Supplemental Digital Content is available in the text.
Keywords: canagliflozin, cardiomyopathy, COVID-19, heart failure, Kansas City Cardiomyopathy Questionnaire
Background:
The expense of clinical trials mandates new strategies to efficiently generate evidence and test novel therapies. In this context, we designed a decentralized, patient-centered randomized clinical trial leveraging mobile technologies, rather than in-person site visits, to test the efficacy of 12 weeks of canagliflozin for the treatment of heart failure, regardless of ejection fraction or diabetes status, on the reduction of heart failure symptoms.
Methods:
One thousand nine hundred patients will be enrolled with a medical record-confirmed diagnosis of heart failure, stratified by reduced (≤40%) or preserved (>40%) ejection fraction and randomized 1:1 to 100 mg daily of canagliflozin or matching placebo. The primary outcome will be the 12-week change in the total symptom score of the Kansas City Cardiomyopathy Questionnaire. Secondary outcomes will be daily step count and other scales of the Kansas City Cardiomyopathy Questionnaire.
Results:
The trial is currently enrolling, even in the era of the coronavirus disease 2019 (COVID-19) pandemic.
Conclusions:
CHIEF-HF (Canagliflozin: Impact on Health Status, Quality of Life and Functional Status in Heart Failure) is deploying a novel model of conducting a decentralized, patient-centered, randomized clinical trial for a new indication for canagliflozin to improve the symptoms of patients with heart failure. It can model a new method for more cost-effectively testing the efficacy of treatments using mobile technologies with patient-reported outcomes as the primary clinical end point of the trial.
Registration:
URL: https://www.clinicaltrials.gov; Unique identifier: NCT04252287.
Although cardiovascular disease remains the leading cause of death in the United States, wide-spread concerns have arisen about the costs, inefficiencies, and complexities of clinical trials. These costs, as well as barriers to regulatory approval, have dramatically attenuated the introduction of new cardiovascular treatments.1 As such, there have been calls for novel strategies to lower the costs of clinical trials.2,3 A large component (up to 50%) of these costs are the burden of data collection on sites, which has increased 3.6-fold from 1990 to 2010.4 In response to the growing demands to make clinical trials more efficient, novel study designs have been implemented, from leveraging existing registries as the backbone of data collection5 to the use of electronic health records to identify, enroll, randomize and follow-up eligible patients.6
An additional significant threat to clinical trials is prolonged patient enrollment and deviations from planned follow-up in executing clinical trials. The ongoing coronavirus disease 2019 (COVID-19) global pandemic has proven to be a cataclysmic event for the conduct of clinical trials, significantly disrupting patient enrollment as patients and providers are all fearful of the risks of in-person site visits. Both the US Food and Drug Administration7 and a Heart Failure (HF) Collaboratory Statement8 have highlighted the need to prioritize the safety and well-being of HF trial participants and research team members, even if sacrificing protocol adherence.
Against this backdrop of a call for more efficient and cost-effective clinical trials and the need to maximize patient safety and convenience, we designed the CHIEF-HF trial (Canagliflozin: Impact on Health Status, Quality of Life and Functional Status in Heart Failure), which sought to directly engage participants without in-person contact. An unplanned benefit of our trial design was its relevance and feasibility during the COVID-19 pandemic, which had major disruptive consequences on traditional clinical trials. This report describes the novel methodological features of this decentralized trial.
Methods
Evolving Role of Sodium-Glucose Cotransporter 2 Inhibitors in HF
Sodium-glucose cotransporter 2 inhibitors (SGLT2i), which lower plasma glucose concentrations via increased urinary glucose excretion, are a class of medications originally developed for the treatment of type 2 diabetes. They were also postulated to have a potential benefit in the treatment of HF.9,10 Several large cardiovascular outcome trials, and one large kidney outcome trial, have demonstrated robust and consistent reductions in the risk of hospitalization for HF in patients with type 2 diabetes.11,12 However, the overwhelming majority of patients in these studies did not have a history of HF, and those that did were not well-characterized. Therefore, although these trials established the efficacy of SGLT2i in preventing incident HF in high-risk patients, whether they could also treat patients with established HF was not well established until recently.
In the DAPA-HF trial (Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure), a global randomized outcome trial of dapagliflozin versus placebo in 4744 patients with HF and reduced ejection fraction (EF),13 patients treated with dapagliflozin (as compared with placebo) experienced a significant 26% relative risk reduction in the primary composite outcome of cardiovascular death or hospitalization for HF, a benefit that emerged early and was consistent in both patients with and without type 2 diabetes.14 The recent publication of the EMPEROR-Reduced trial (Empagliflozin Outcome Trial in Patients with Chronic Heart Failure and a Reduced Ejection Fraction), which also demonstrated a significant reduction in cardiovascular death and HF hospitalizations, further emphasized the potential benefits of SGLT2i on clinical events.15 In addition, both DAPA-HF and EMPEROR-reduced significantly improved HF-related symptoms, as measured by the Kansas City Cardiomyopathy Questionnaire (KCCQ).15,16 The health status (symptoms, physical limitations, and quality of life) benefits of an SGLT2i were also addressed in DEFINE-HF (Dapagliflozin Effects on Biomarkers, Symptoms and Functional Status in Patients With HF With Reduced Ejection Fraction)—the first randomized placebo-controlled trial of an SGLT2i that included the KCCQ as a part of the composite primary outcome.17 In that study, dapagliflozin significantly improved symptoms, physical limitations, and quality of life in patients with symptomatic HF with reduced EF after 12 weeks of treatment. Furthermore, fewer patients treated with dapagliflozin (versus placebo) experienced a deterioration in health status, and significantly more patients treated with dapagliflozin had small, moderate, and large improvements in their health status. Collectively, these data support the benefits of dapagliflozin to improve the health status of patients with HF with reduced EF, but none of these agents are currently indicated for the clinical improvement in HF symptoms or for use in patients with HF with preserved EF (HFpEF). CHIEF-HF was designed to test the efficacy of canagliflozin on the health status outcomes of a broad spectrum of patients with HF.
Regulatory Shifts in Clinical End Points
Marked change has occurred in the Food and Drug Administration’s perspectives on clinical end points in HF trials for drug approval, including endorsement that patient-reported outcomes of reduced symptoms and improved function could support regulatory approval.18 Moreover, the Food and Drug Administration’s Center for Drug Evaluation and Research recently qualified the KCCQ as a clinical outcome assessment for drug approval and marketing.19 Collectively, the availability of a patient-reported outcome to serve as an approvable outcome in clinical trials, coupled with the availability of mobile technologies to collect these data, have created an unprecedented opportunity to perform clinical trials at lower costs and with more efficiency than would otherwise be possible. Because of this, the CHIEF-HF trial was designed with the primary outcome being the Total Symptom Score of the KCCQ to capture the benefits of canagliflozin over placebo on patients’ shortness of breath, fatigue, orthopnea, and edema.
Study Hypothesis
The primary hypothesis of the study is that canagliflozin is superior to placebo in improving HF symptoms within 12 weeks of treatment, as assessed by the KCCQ Total Symptom Score.
Study Methodology
CHIEF-HF was designed to be a decentralized (ie, no face-to-face visits) US study with direct engagement of patients through a study website, electronic informed consent, direct home delivery of study medication, completion of the primary end point by a mobile application, and a Fitbit Versa 2 (San Francisco, CA) to monitor activity. Although clinical events were not included as a primary end point in this 3-month trial, these will be captured through claims data or patient self-report during the active 12-week treatment phase and the following 6 months. Collectively, this design allowed for the elimination of in-person site visits, a critical feature in enabling the study to launch in the midst of the COVID-19 pandemic and for reassuring participants who might be leery of coming to a hospital or clinic.
The study was designed, in conjunction with an Executive Steering Committee, by Janssen Scientific Affairs, LLC (Titusville, NJ) and PRA Health Sciences (PRA, Raleigh, NC). PRA is also leading the trial operations (with oversight by Janssen), including the creation of the web platform and mobile application (the primary means of data collection), randomization and drug delivery, and facilitating a virtual study coordinating center to support participant onboarding, questions, shipping the Fitbit and supplies, confirming receipt, and drug compliance. The organization of the study infrastructure is provided in Figure 1. The authors declare that all supporting data are available within the article.
Figure 1.
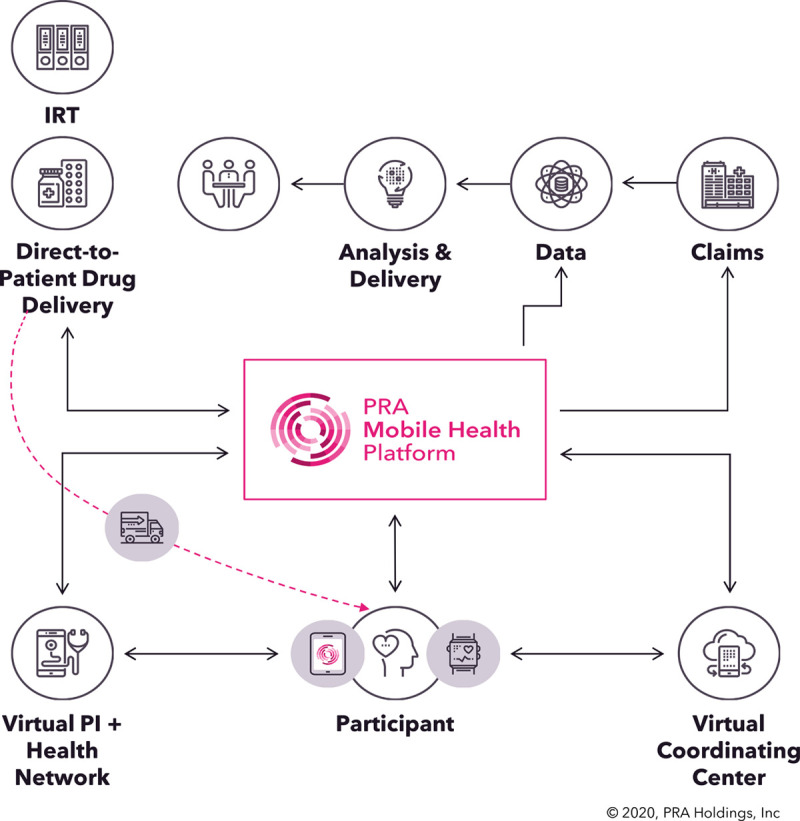
Overview of study infrastructure. (1) At the center of the trial is the participant, who is offered participation by their provider/health network and opts in after learning more on a central recruitment website. (2) Once their eligibility is verified by their health network, they interact with the Mobile Health Platform (mHP) to eConsent and complete a baseline KCCQ. (3)Upon KCCQ score review for eligibility, the participant is randomized through an Interactive Response Technology (IRT) system, which triggers direct-to-patient drug delivery. (4) The participant is also be shipped a Welcome Kit, including the Fitbit, from the Virtual Coordinating Center, which serves as participant liaison throughout the study for technology set-up and troubleshooting, call center support, safety reporting, and compliance monitoring. (5) All patient source data (ePROs, medication diaries) are collected via the mHP study app and Fitbit. (6) Upon consent and randomization, a token will be applied to patients to collect medical and prescription insurance claims. (7) All data will be integrated in and normalized within the PRA data cloud and translated into Study Data Tabulation Model (SDTM) data sets for analysis and submission to the FDA. IRT indicates Interactive Response Technology.
Funding Sources
Funding for this study has been provided by Janssen Scientific Affairs and PRA Health Sciences.
Participant Inclusion and Exclusion Criteria and Process for Confirming Participant Eligibility
Potential participants are screened at participating US health systems, who all agreed to the use of a central Institutional Review Board (Advarra, Columbia MD). The complete inclusion and exclusion criteria are provided in the Data Supplement. In brief, participants must be 18 years or older with a diagnosis of HF, regardless of EF, to be eligible, irrespective of whether they have diabetes or not. A diagnosis of HF for potential participants with a left ventricular EF of ≤40% was established by a primary diagnosis of HF or at least 2 medical visits (including virtual) with a diagnostic code for HF. For patients with a left ventricular EF >40%, use of a loop diuretic or an aldosterone-receptor blocker was also required to improve diagnostic specificity. To support the mobile data collection of the KCCQ and to provide study support, patients were required to own a smartphone compatible with the app (either a Samsung S7 Galaxy or Apple iPhone 6 or later and the Fitbit), speak and read English, and be willing to wear a Fitbit for 9 months.
Those with any of the following within the timeframe listed before enrollment were excluded: currently taking an SGLT2i, having a history of diabetic ketoacidosis or type 1 diabetes, acute decompensated HF, advanced kidney disease (glomerular filtration rate <30 mL/min or on dialysis), a diagnosis of recent hypotension, a history of atraumatic amputation or critical limb ischemia, planned major surgery, left ventricular assist device implantation, known allergy to canagliflozin, or pregnant, planning to become pregnant, or breastfeeding during the study.
To engage participants, sites are encouraged to develop a computable phenotype for the inclusion and exclusion criteria and to screen their electronic health record for potentially eligible participants. A range of options for contacting potentially eligible participants are available for sites to adapt, based on their patient population and EHR capabilities. These include email, patient portal communications through the electronic medical record, traditional post, and phone calls. These invitations, all approved by the Central Institutional Review Board, encourage potential participants to visit the study website, to read and observe a video describing the study, and, if interested, to complete an initial set of screening questions confirming initial eligibility. If these criteria are met, potential participants opt-in to be contacted and evaluated for further eligibility. Participants who opt-in are then assessed by their respective health network for a full eligibility review before being scheduled for a virtual eConsent call. This process reduces time invested by the sites so they only focus on those individuals interested in study participation. Candidates passing this initial screening are then invited to download the app in preparation for the virtual informed consent call with a member of their health network authorized to obtain consent for CHIEF-HF and an independent observer from the virtual study coordinating call center. Once consent is obtained, the participant completes the KCCQ-23 to ensure that they have an Overall Summary score of ≤80 and are sufficiently symptomatic to have the potential to improve from treatment. The use of the KCCQ as an entry criterion ensures that patients are symptomatic and overcomes the well-documented limitations of relying upon clinician-assigned New York Heart Association classification.20 Once participants meet all study criteria, they are randomized by the Virtual Investigator.
Study Protocol and Execution
CHIEF-HF is a randomized, double-blind, placebo-controlled, decentralized, interventional, superiority study. Once participants with confirmed HF diagnoses undergo the virtual informed consent process, provide documented consent to participate, and are determined to have a KCCQ Overall Summary score of ≤80, they undergo central randomization, stratified by the type of HF (HF with reduced EF [HFrEF] and HFpEF), to either canagliflozin 100 mg or placebo for 12 weeks of drug exposure, followed by unblinding and a 6-month observational data collection period without study drug. Data collection throughout the study, as well as the assessment of medication compliance and reminders for study assessments, are being collected by the study-specific app. Examples of selected screenshots are shown in Figure 2.
Figure 2.
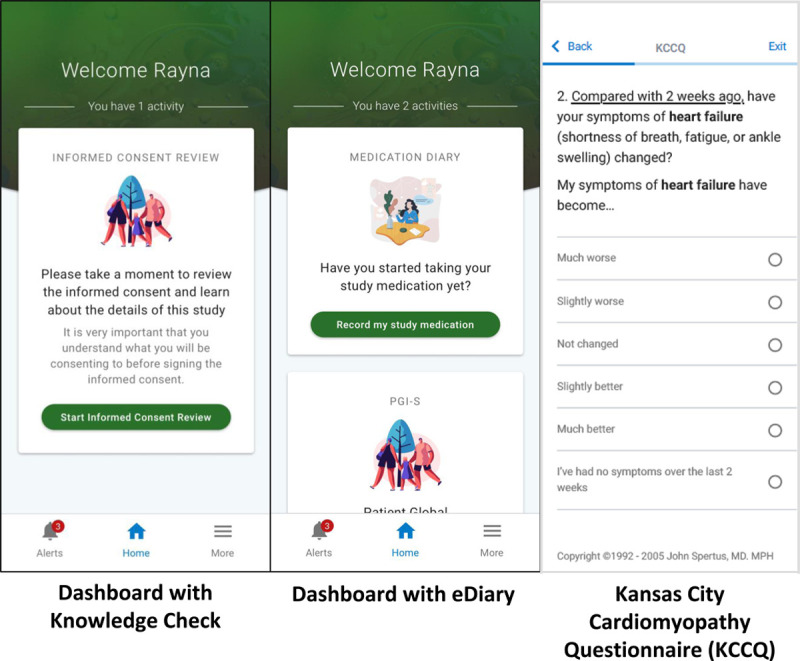
Sample screenshots of data collection app. KCCQ indicates Kansas City Cardiomyopathy Questionnaire. PGIs, Patient Global Impression - Severity
The app includes an electronic version of the KCCQ-23 that has been converted to an electronic format following the ISPOR ePRO (International Society for Pharmacoeconomics and Outcomes Research electronic Patient Reported Outcome) Good Research Practices Task Force recommendations.21 The app also collects participants’ global assessments of change, their perceptions of the HF symptom severity, as well as a participant satisfaction survey at the completion of the trial to gain patients’ perspectives of participating in this decentralized study. It also passively collects daily Fitbit data to directly quantify participants’ physical activity, including step count and floors climbed. The primary outcome, the KCCQ, will be collected at baseline, weeks 2, 4, 6, and 12, and again at months 6 and 9, with the 12-week assessment (the duration of randomized, double-blind drug exposure) being the primary outcome. The study will continue for an additional 6 months without any protocol-mandated treatment to collect participant follow-up in a real-world setting, including whether or not they begin open-label SGLT2i treatment. Figure 3 provides an overview of the study design.
Figure 3.
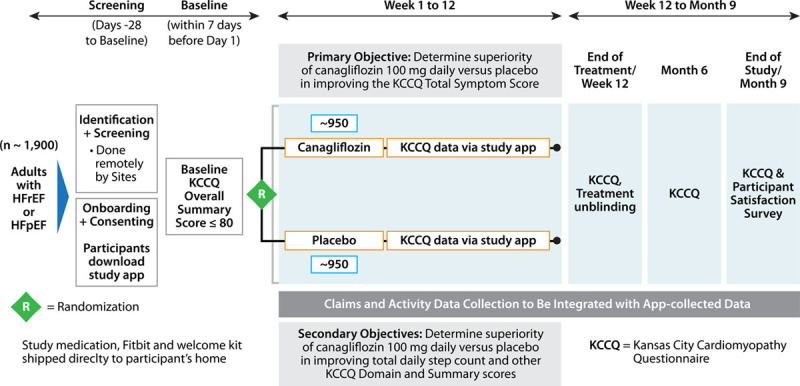
Overview of study design. HFpEF indicates heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; and KCCQ, Kansas City Cardiomyopathy Questionnaire.
Study Outcomes
The primary assessment of efficacy is the 23-item KCCQ, which has extensive data supporting its validity, reliability, sensitivity to clinical change, and association with other clinical events, such as HF hospitalization and death.22–27 The primary outcome of the CHIEF-HF study is the Total Symptom score of the KCCQ. The Total Symptom score is comprised of 7 items, 4 assessing symptom frequency, and 3 symptom severity or burden over the past 2 weeks and ranges from 0 to 100 points.
Secondary outcomes include a comparison of daily step counts acquired from the Fitbit, followed by these additional domain scores of the KCCQ: Physical Limitation, Quality of Life, the Clinical Summary (the average of Physical Limitation and Total Symptom scores), and the Overall Summary (the average of the Physical Limitation, Total Symptom, Social Functioning, and Quality of Life domains) scores. Exploratory analyses also include patients’ global ratings of change and symptom severity, health care resource utilization, daily floors climbed, and time to clinical events, including time to first HF hospitalization or death, as well as their satisfaction with the decentralized nature of the study. Adverse event reporting will also be collected through patient self-report.
An all-payer database (https://symphonyhealth.prahs.com/) will be used to monitor clinical events and health care utilization, exploratory end points for this short-term trial, and to confirm patient eligibility. PRA (Symphony Health) has compiled a database of US medical and prescription claims that cover over 300 million patients across all diagnoses, contains over 90% coverage of prescriptions dispensed, is geographically representative and covers all payer types (Medicaid, Medicare, and Commercial Insurers). PRA’s patient claims data include some important patient demographics (gender, age), payer, as well as administrative diagnosis, treatment, and procedure codes that include date and location of service and physician name and address. Each deidentified patient in the data is assigned a longitudinally stable unique identifier that allows PRA to track deidentified patients longitudinally over time and across locations of care. PRA’s encrypted anonymized patient key links patient activities across many data sources to ensure individual patient-level data are anonymous and protected; consistent with US Health Insurance Portability and Accountability Act.
Despite the potential of the Symphony Health database, there are potential limitations due to the origin of claims data being transactional in nature. Specifically, deaths that occur outside of the hospital may be missed, if not captured by payers. Also, while extensive, PRA’s claims data may not capture complete activity of every enrolled patient. These caveats are documented in the claims data analysis plan, along with the recommendation of complementing patient activity captured through claims data by patient-reported outcomes and site’s electronic medical records. Importantly, the primary analyses of changes in KCCQ scores are collected directly from the patients as part of the trial.
Analytic Approach and Power
Analyses will be performed by intention to treat, with group allocation based upon randomization, regardless of actual use of assigned medications. For the primary outcome, a mixed effect model of repeated measures, adjusting for study intervention (the primary variable of interest), stratification (HFrEF versus HFpEF), time by study intervention, and baseline KCCQ Total Symptom score will be performed. Although statistical significance of this comparison with least-square means will test the primary hypothesis, the mean treatment group difference is not as clinically interpretable as the proportion of patients who clinically improve or worsen.28 To support the clinical interpretability of the observed mean differences, the proportion of patients who have a clinically small, but significant, moderate to large, and large to very large change in their health status, as defined by KCCQ changes of 5, 10, and 20 points, respectively, will be performed.23,29–31 Mortality in this short-duration trial is expected to be low and to be comparable between groups and will be ignored in the primary analyses of mean differences in changes in KCCQ Total Symptom scores, but can be included in the responder analyses by assigning them to the lowest response (greatest deterioration) category. Should there be a >5% mortality rate and if it is unequally distributed between treatment arms, then joint modeling of survival and health status will be performed.32 The key secondary end point of step counts will be compared, if the primary analysis is significant at <5% type I error, using a 2-sided t test. The additional secondary end points of other KCCQ scores will be conducted in the same fashion as the primary outcome, using the baseline score of each domain in the model.
Sample size was determined for the primary outcome by using a 2-sample t test for continuous measures. The group mean differences of the KCCQ Total Symptom score that have been defined as clinically meaningful range from 3 to 5 points.29–31 Accordingly, the study was powered to detect a 3-point change with 95% power, assuming a type 1 error of 5%, and a potential dropout rate of 5%. This led to a target sample size of 1900 patients, randomized 1:1 to canagliflozin or placebo.
Discussion
Demonstrating treatment benefit, ideally through the conduct of randomized clinical trials, is the foundation for advancing patient care. Yet, the cost and complexity of current clinical trials is proving to be a great impediment.1,2,33 A report by the Eastern Research Group examining key drivers for reducing the costs of cardiovascular phase 3 and 4 clinical trials identified lower-cost facilities or at-home testing (up to 10%–13% cost reduction), use of mobile technologies (up to 6%–14% cost reduction), use of electronic health records (up to 3-8% cost reduction) and simplified protocols (up to 2%–4% reduction) as the most important opportunities for improving the efficiency of clinical trials.34,35 By incorporating all of these features, CHIEF-HF has embraced multiple strategies to model a more efficient approach to generating clinical trial evidence. It is also completely aligned with the recommendations of the National Academy of Medicine, which recommends directly engaging health care systems in the research enterprise.33 Although designed before the onset of the COVID-19 pandemic, the novel design of CHIEF-HF highlights the urgency to explore novel approaches to generating evidence and possible benefits of innovative study design.
CHIEF-HF builds upon the slow evolution of novel clinical trials. A large advance was the leveraging of ongoing clinical registries as the foundation for data collection, such that randomization of treatments could be done with minimal additional data collection.5 The recent publication of the ADAPTABLE (Aspirin Dosing: A Patient-centric Trial Assessing Benefits and Long-Term Effectiveness) trial methodology highlighted the use of electronic health records to identify, enroll, randomize, and follow eligible patients.6 Although CHIEF-HF similarly uses computable phenotypes to identify potentially eligible participants and refer them to a website for additional information about the trial, it also introduces a placebo-controlled randomized design, as opposed to the open-label, dose-finding research question of ADAPTABLE. Although both CHIEF-HF and ADAPTABLE are using claims data without adjudication to define clinical events, ADAPTABLE required a very large trial with which to be adequately powered for these events, whereas the primary outcome of CHIEF-HF is patient-reported symptoms, as captured by the extensively-validated KCCQ. In fact, the growing acceptance of patient-reported outcomes, including the recently qualified KCCQ, can be a harbinger of future such studies to accelerate the conduct of more affordable clinical trials to inform the benefits of new treatments.
There are sure to be unanticipated challenges with CHIEF-HF. For example, current standards for Good Clinical Practice require that a disinterested party be present to witness the informed consent process. This requires a rather cumbersome process of coordinating a time during which a potential participant, a site investigator, and an observer from the coordinating center can simultaneously be available to review the consent form, address questions, and confirm the identity of the participant with dual authentication, before obtaining an electronic signature. As comfort grows with virtual clinical trials, this process may be simplified by having patients view an online video and provide an electronic signature to the electronic consent and only arrange a video conference with the site investigator if the potential participants have additional questions. In addition, the use of electronic activity monitors, although not new, is still early in their evolution, and defining the completeness of data capture and the interpretability of results require further study. Finally, requiring a smartphone and the ability to read and understand English can minimize the diversity of the CHIEF-HF population, although if CHIEF-HF is successful, future studies can consider making smartphones available, providing cards for data, and translating the platform to different languages.
An additional potential challenge with CHIEF-HF is the growing body of evidence showing improved survival or reduced hospitalizations with the use of SGLT2i for patients with HF.13,15 Although some might consider it unethical, in light of these data, to randomize patients to placebo, the sponsor and steering committee felt that this was reasonable based on several streams of logic. First, the half of enrolled patients assigned to placebo would only be exposed to inactive drug for 3 months, after which they could openly take an SGLT2i. Second, the proactive screening process could accelerate their identification and recognition by the health care system that they are candidates of an SGLT2i at the conclusion of the 12-week trial. Finally, and most importantly, the translation of data, even as compelling as that of DAPA-HF and EMPEROR-Reduced,13,15 to clinical practice is notoriously slow and inefficient. In fact, a contemporary HF registry reported that even among patients with diabetes, <5% are treated with SGLT2i.36 By being enrolled in CHIEF-HF, all patients will have been identified as potential candidates for treatment and educated about the potential benefits of treatment so that their providers could consider adding these medications to their HF regimen.
CHIEF-HF also provides an example of moving away from simply enrolling a subset of patients based on their EF. This approach was chosen because although patients are clearly aware of their symptoms, function, and quality of life, they are not aware of their left ventricular physiology. Focusing the primary outcome on patients’ health status, for which the KCCQ’s validity and prognostic ability has been shown to be similar in patients with HFrEF and HFpEF, further supports the appropriateness of combining these HF phenotypes in a patient-centered trial.23 Moreover, evidence is accumulating that the clinical benefits of SGLT2i is similar in patients with both HFrEF and HFpEF, as seen in the recent SOLOIST-WHF (Effect of Sotagliflozin on Cardiovascular Events in Patients With Type 2 Diabetes Post Worsening Heart Failure) trial, although the KCCQ data has not yet been published.37 Although the expectation is of similar benefits across the spectrum of HF, randomization is stratified by EF and formal tests of an interaction of treatment benefit by HFrEF and HFpEF will establish this more definitively.
In light of the growing therapeutic options for HF treatment to reduce hospitalizations and mortality,13,15,38–41 improving patients’ health status, their symptoms, function, and quality of life, may become a distinguishing feature in deciding which treatment might be started after beta-blockade and inhibition of the renin-angiotensin-aldosterone axis. Trials, like CHIEF-HF, which explicitly quantify these benefits have the ability to provide important information for clinicians to support shared decision-making with patients.42 Moreover, innovations in the conduct of such trials, such as the methods exemplified in CHIEF-HF, can model ways to more efficiently generate evidence and accelerate the evidence-base of guidelines and care in many other therapeutic areas.43
Sources of Funding
Funding for this study has been provided by Janssen Scientific Affairs and PRA Health Sciences.
Disclosures
Dr Spertus is the principal investigator of grants from National Institutes of Health (NIH), Abbott Vascular, and the American College of Cardiology Foundation; is a consultant to Janssen, Novartis, Amgen, Myokardia, AstraZeneca, Bayer, and Merck; serves on the Scientific Advisory Board of United Healthcare and the Board of Directors for Blue Cross Blue Shield of Kansas City; owns the copyright to the Kansas City Cardiomyopathy Questionnaire (KCCQ), Seattle Angina Questionnaire and Peripheral Artery Questionnaire; and has an equity interest in Health Outcomes Sciences. Dr Butler is a consultant to Abbott, Adrenomed, Arena Pharma, Array, Amgen, Applied Therapeutics, Astra Zeneca, Bayer, BerlinCures, Boehringer Ingelheim, Corvia, Cardior, CVRx, Eli Lilly, FIRE1, Foundry, G3 Pharma, Imbria, Impulse Dynamics, Innolife, Janssen, LivaNova, Luitpold, Medtronic, Merck, Novartis, Novo Nordisk, Relypsa, Roche, SC Pharma, Sanofi, Sequana Medical, V-Wave Limited, Vifor. Dr Lingvay has received research funding, advisory/consulting fees and/or other support from Novo Nordisk, Eli Lilly, Sanofi, Astra Zeneca, Boehringer Ingelheim, Janssen, Intercept, Intarcia, TARGETPharma, Merck, Pfizer, Novartis, GI Dynamics, Mylan, Mannkind, Valeritas, Zealand Pharma. Dr Lanfear has received research grants from National Heart, Lung, and Blood Institute (NHLBI), Amgen, Bayer, Critical Diagnostics, and Janssen; has participated in collaborative research with Somalogic; is a consultant for Amgen, Janssen (CHIEF Steering Committee), Ortho Diagnostics, and Duke Clinical Research Institute (Novartis). Dr Abbate has received research grant support from Janssen; is a consultant to Janssen. Dr Kosiborod has received research grants from AstraZeneca and Boehringer Ingelheim; is a consultant and/or advisory board member for Amarin, Applied Therapeutics, AstraZeneca, Amgen, Bayer, Boehringer Ingelheim, Janssen, Eli Lilly, Merck (Diabetes), Novartis, Novo Nordisk, Sanofi, Vifor. C. Fawcett is an employee of PRA Health Sciences. Drs Birmingham, Whang and Burton are employees of Janssen Scientific Affairs, LLC. Dr Januzzi is supported by the Hutter Family Professorship; is a Trustee of the American College of Cardiology; has received grant support from Applied Therapeutics and Novartis; has received consulting income from Abbott, Janssen, Novartis, Pfizer, Merck, and Roche Diagnostics; participates in clinical end point committees/data safety monitoring boards for Abbott, AbbVie, Amgen, Bayer, CVRx, Janssen, and Takeda. Dr Damaraju is an employee of Janssen Research & Development, LLC.
Supplementary Material
Nonstandard Abbreviations and Acronyms
- CHIEF-HF
- Canagliflozin: Impact on Health Status, Quality of Life and Functional Status in Heart Failure
- DAPA-HF
- Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure
- DEFINE-HF
- Dapagliflozin Effects on Biomarkers, Symptoms and Functional Status in Patients With HF With Reduced Ejection Fraction
- EF
- ejection fraction
- EMPEROR-Reduced
- Empagliflozin Outcome Trial in Patients with Chronic Heart Failure and a Reduced Ejection Fraction
- HF
- heart failure
- HFpEF
- HF with preserved EF
- HFrEF
- HF with reduced EF
- KCCQ
- Kansas City Cardiomyopathy Questionnaire
- SGLT2i
- sodium-glucose cotransporter 2 inhibitor
This manuscript was sent to Kenneth B. Margulies, MD, Senior Guest Editor, for review by expert referees, editorial decision, and final disposition.
The Data Supplement is available at https://www.ahajournals.org/doi/suppl/10.1161/CIRCHEARTFAILURE.120.007767.
For Sources of Funding and Disclosures, see page 402.
Contributor Information
Mary C. Birmingham, Email: mbirming@its.jnj.com.
Javed Butler, Email: butlzih@gmail.com.
Ildiko Lingvay, Email: ildiko.lingvay@utsouthwestern.edu.
David E. Lanfear, Email: dlanfea1@hfhs.org.
Antonio Abbate, Email: antonio.abbate@vcuhealth.org.
Mikhail N. Kosiborod, Email: mkosiborod@saint-lukes.org.
Christina Fawcett, Email: FawcettChristina@prahs.com.
C.V. Damaraju, Email: cdamara1@its.jnj.com.
James L. Januzzi, Email: JJANUZZI@PARTNERS.ORG.
References
- 1.Fordyce CB, Roe MT, Ahmad T, Libby P, Borer JS, Hiatt WR, Bristow MR, Packer M, Wasserman SM, Braunstein N, et al. Cardiovascular drug development: is it dead or just hibernating? J Am Coll Cardiol. 2015;65:1567–1582. doi: 10.1016/j.jacc.2015.03.016 [DOI] [PubMed] [Google Scholar]
- 2.Lauer MS, Gordon D, Wei G, Pearson G. Efficient design of clinical trials and epidemiological research: is it possible? Nat Rev Cardiol. 2017;14:493–501. doi: 10.1038/nrcardio.2017.60 [DOI] [PubMed] [Google Scholar]
- 3.Antman EM, Harrington RA. Transforming clinical trials in cardiovascular disease: mission critical for health and economic well-being. JAMA. 2012;308:1743–1744. doi: 10.1001/jama.2012.14841 [DOI] [PubMed] [Google Scholar]
- 4.Berndt E, Cockburn I. Price indices for clinical trial research: a feasibility study. Working Paper 18918. 2013;37 [Google Scholar]
- 5.Fröbert O, Lagerqvist B, Gudnason T, Thuesen L, Svensson R, Olivecrona GK, James SK. Thrombus aspiration in ST-elevation myocardial infarction in scandinavia (TASTE trial). A multicenter, prospective, randomized, controlled clinical registry trial based on the Swedish angiography and angioplasty registry (SCAAR) platform. Study design and rationale. Am Heart J. 2010;160:1042–1048. doi: 10.1016/j.ahj.2010.08.040 [DOI] [PubMed] [Google Scholar]
- 6.Marquis-Gravel G, Roe MT, Robertson HR, Harrington RA, Pencina MJ, Berdan LG, Hammill BG, Faulkner M, Munoz D, Fonarow GC, et al. Rationale and design of the aspirin dosing-a patient-centric trial assessing benefits and long-term effectiveness (ADAPTABLE) trial. JAMA Cardiol. 2020;5:598–607. doi: 10.1001/jamacardio.2020.0116 [DOI] [PubMed] [Google Scholar]
- 7.US Food and Drug Administration. FDA guidance on conduct of clinical trials of medical products during COVID-19 pandemic 2020;2020 [Google Scholar]
- 8.Abraham W, Fiuzat M, Psotka M, O’Connor C. Heart failure collaboratory statement on clinical trials in the landscape of COVID-19. JACC. 2020;8:423–425. doi: 10.1016/j.jchf.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Butler J, Hamo CE, Filippatos G, Pocock SJ, Bernstein RA, Brueckmann M, Cheung AK, George JT, Green JB, Januzzi JL, et al. ; EMPEROR Trials Program. The potential role and rationale for treatment of heart failure with sodium-glucose co-transporter 2 inhibitors. Eur J Heart Fail. 2017;19:1390–1400. doi: 10.1002/ejhf.933 [DOI] [PubMed] [Google Scholar]
- 10.Packer M, Anker SD, Butler J, Filippatos G, Zannad F. Effects of sodium-glucose cotransporter 2 inhibitors for the treatment of patients with heart failure: proposal of a novel mechanism of action. JAMA Cardiol. 2017;2:1025–1029. doi: 10.1001/jamacardio.2017.2275 [DOI] [PubMed] [Google Scholar]
- 11.Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, et al. ; EMPA-REG OUTCOME Investigators. Empagliflozin, cardiovascular outcomes, and mortality in Type 2 diabetes. N Engl J Med. 2015;373:2117–2128. doi: 10.1056/NEJMoa1504720 [DOI] [PubMed] [Google Scholar]
- 12.Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR; CANVAS Program Collaborative Group. Canagliflozin and cardiovascular and renal events in Type 2 diabetes. N Engl J Med. 2017;377:644–657. doi: 10.1056/NEJMoa1611925 [DOI] [PubMed] [Google Scholar]
- 13.McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, Ponikowski P, Sabatine MS, Anand IS, Bělohlávek J, et al. ; DAPA-HF Trial Committees and Investigators. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008. doi: 10.1056/NEJMoa1911303 [DOI] [PubMed] [Google Scholar]
- 14.Petrie MC, Verma S, Docherty KF, Inzucchi SE, Anand I, Belohlavek J, Bohm M, Chiang CE, Chopra VK, de Boer RA, et al. Effect of dapagliflozin on worsening heart failure and cardiovascular death in patients with heart failure with and without diabetes. JAMA. 2020;323:1353–1368. doi: 10.1001/jama.2020.1906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, Januzzi J, Verma S, Tsutsui H, Brueckmann M, et al. ; EMPEROR-Reduced Trial Investigators. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383:1413–1424. doi: 10.1056/NEJMoa2022190 [DOI] [PubMed] [Google Scholar]
- 16.Kosiborod MN, Jhund PS, Docherty KF, Diez M, Petrie MC, Verma S, Nicolau JC, Merkely B, Kitakaze M, DeMets DL, et al. Effects of dapagliflozin on symptoms, function, and quality of life in patients with heart failure and reduced ejection fraction: results from the DAPA-HF trial. Circulation. 2020;141:90–99. doi: 10.1161/CIRCULATIONAHA.119.044138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nassif ME, Windsor SL, Tang F, Khariton Y, Husain M, Inzucchi SE, McGuire DK, Pitt B, Scirica BM, Austin B, et al. Dapagliflozin effects on biomarkers, symptoms, and functional status in patients with heart failure with reduced ejection fraction: the DEFINE-HF trial. Circulation. 2019;140:1463–1476. doi: 10.1161/CIRCULATIONAHA.119.042929 [DOI] [PubMed] [Google Scholar]
- 18.Food and Drug Administration. Treatment for Heart Failure: Endpoints for Drug Development Guidance for Industry. 2019. August 3, 2020
- 19.U.S. Food and Drug Administration. Clinical Outcome Assessments (COA) Qualification Submissions Office of Cardiology H, Endocrinology, and Nephrology (OCEHM) Division of Cardiovascular and Nephrology (DCN). DDT COA #000084: Kansas City Cardiomyopathy Questionnaire (KCCQ). 2020. August 3, 2020
- 20.Tran AT, Chan PS, Jones PG, Spertus JA. Comparison of patient self-reported health status with clinician-assigned New York Heart Association classification. JAMA Netw Open. 2020;3:e2014319. doi: 10.1001/jamanetworkopen.2020.14319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coons SJ, Gwaltney CJ, Hays RD, Lundy JJ, Sloan JA, Revicki DA, Lenderking WR, Cella D, Basch E; ISPOR ePRO Task Force. Recommendations on evidence needed to support measurement equivalence between electronic and paper-based patient-reported outcome (PRO) measures: ISPOR ePRO Good Research Practices Task Force report. Value Health. 2009;12:419–429. doi: 10.1111/j.1524-4733.2008.00470.x [DOI] [PubMed] [Google Scholar]
- 22.Green CP, Porter CB, Bresnahan DR, Spertus JA. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol. 2000;35:1245–1255. doi: 10.1016/s0735-1097(00)00531-3 [DOI] [PubMed] [Google Scholar]
- 23.Pokharel Y, Khariton Y, Tang Y, Nassif ME, Chan PS, Arnold SV, Jones PG, Spertus JA. Association of serial Kansas City cardiomyopathy questionnaire assessments with death and hospitalization in patients with heart failure with preserved and reduced ejection fraction: a secondary analysis of 2 randomized clinical trials. JAMA Cardiol. 2017;2:1315–1321. doi: 10.1001/jamacardio.2017.3983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spertus JA, Jones PG. Development and validation of a short version of the Kansas City cardiomyopathy questionnaire. Circ Cardiovasc Qual Outcomes. 2015;8:469–476. doi: 10.1161/CIRCOUTCOMES.115.001958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kosiborod M, Soto GE, Jones PG, Krumholz HM, Weintraub WS, Deedwania P, Spertus JA. Identifying heart failure patients at high risk for near-term cardiovascular events with serial health status assessments. Circulation. 2007;115:1975–1981. doi: 10.1161/CIRCULATIONAHA.106.670901 [DOI] [PubMed] [Google Scholar]
- 26.Soto GE, Jones P, Weintraub WS, Krumholz HM, Spertus JA. Prognostic value of health status in patients with heart failure after acute myocardial infarction. Circulation. 2004;110:546–551. doi: 10.1161/01.CIR.0000136991.85540.A9 [DOI] [PubMed] [Google Scholar]
- 27.Joseph SM, Novak E, Arnold SV, Jones PG, Khattak H, Platts AE, Dávila-Román VG, Mann DL, Spertus JA. Comparable performance of the Kansas City cardiomyopathy questionnaire in patients with heart failure with preserved and reduced ejection fraction. Circ Heart Fail. 2013;6:1139–1146. doi: 10.1161/CIRCHEARTFAILURE.113.000359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spertus JA, Jones PG, Sandhu AT, Arnold SV. Interpreting the Kansas City cardiomyopathy questionnaire in clinical trials and clinical care: JACC state-of-the-art review. J Am Coll Cardiol. 2020;76:2379–2390. doi: 10.1016/j.jacc.2020.09.542 [DOI] [PubMed] [Google Scholar]
- 29.Spertus J, Peterson E, Conard MW, Heidenreich PA, Krumholz HM, Jones P, McCullough PA, Pina I, Tooley J, Weintraub WS, et al. ; Cardiovascular Outcomes Research Consortium. Monitoring clinical changes in patients with heart failure: a comparison of methods. Am Heart J. 2005;150:707–715. doi: 10.1016/j.ahj.2004.12.010 [DOI] [PubMed] [Google Scholar]
- 30.Dreyer RP, Jones PG, Kutty S, Spertus JA. Quantifying clinical change: discrepancies between patients’ and providers’ perspectives. Qual Life Res. 2016;25:2213–2220. doi: 10.1007/s11136-016-1267-9 [DOI] [PubMed] [Google Scholar]
- 31.Butler J, Khan MS, Mori C, Filippatos GS, Ponikowski P, Comin-Colet J, Roubert B, Spertus JA, Anker SD. Minimal clinically important difference in quality of life scores for patients with heart failure and reduced ejection fraction. Eur J Heart Fail. 2020;22:999–1005 [DOI] [PubMed] [Google Scholar]
- 32.Spertus JV, Hatfield LA, Cohen DJ, Arnold SV, Ho M, Jones PG, Leon M, Zuckerman B, Spertus JA. Integrating quality of life and survival outcomes in cardiovascular clinical trials. Circ Cardiovasc Qual Outcomes. 2019;12:e005420. doi: 10.1161/CIRCOUTCOMES.118.005420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Institute of Medicine.. Envisioning a Transformed Clinical Trials Enterprise in the United States: Establishing an Agenda for 2020: Workshop Summary. 2012. The National Academies Press; [PubMed] [Google Scholar]
- 34.Sertkaya A, Wong HH, Jessup A, Beleche T. Key cost drivers of pharmaceutical clinical trials in the United States. Clin Trials. 2016;13:117–126. doi: 10.1177/1740774515625964 [DOI] [PubMed] [Google Scholar]
- 35.Sertkaya A, Birkenback A, Berlind A, Eyraud J. Examination of clinical trial costs and barriers for drug development July 25, 2014. https://aspe.hhs.gov/report/examination-clinical-trial-costs-and-barriers-drug-development
- 36.Vaduganathan M, Fonarow GC, Greene SJ, DeVore AD, Kavati A, Sikirica S, Albert NM, Duffy CI, Hill CL, Patterson JH, et al. Contemporary treatment patterns and clinical outcomes of comorbid diabetes mellitus and HFrEF: the CHAMP-HF registry. JACC Heart Fail. 2020;8:469–480. doi: 10.1016/j.jchf.2019.12.015 [DOI] [PubMed] [Google Scholar]
- 37.Bhatt DL, Szarek M, Steg PG, Cannon CP, Leiter LA, McGuire DK, Lewis JB, Riddle MC, Voors AA, Metra M, et al. ; SOLOIST-WHF Trial Investigators. Sotagliflozin in patients with diabetes and recent worsening heart failure. N Engl J Med. 2021;384:117–128. doi: 10.1056/NEJMoa2030183 [DOI] [PubMed] [Google Scholar]
- 38.Armstrong PW, Pieske B, Anstrom KJ, Ezekowitz J, Hernandez AF, Butler J, Lam CSP, Ponikowski P, Voors AA, Jia G, et al. ; Victoria Study Group. Vericiguat in patients with heart failure and reduced ejection fraction. N Engl J Med. 2020;382:1883–1893 [DOI] [PubMed] [Google Scholar]
- 39.McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, et al. ; PARADIGM-HF Investigators and Committees. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993–1004. doi: 10.1056/NEJMoa1409077 [DOI] [PubMed] [Google Scholar]
- 40.Swedberg K, Komajda M, Böhm M, Borer JS, Ford I, Dubost-Brama A, Lerebours G, Tavazzi L; SHIFT Investigators. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010;376:875–885. doi: 10.1016/S0140-6736(10)61198-1 [DOI] [PubMed] [Google Scholar]
- 41.Teerlink JR, Felker GM, McMurray JJ, Solomon SD, Adams KF, Jr, Cleland JG, Ezekowitz JA, Goudev A, Macdonald P, Metra M, et al. ; COSMIC-HF Investigators. Chronic oral study of myosin activation to increase contractility in heart failure (COSMIC-HF): a phase 2, pharmacokinetic, randomised, placebo-controlled trial. Lancet. 2016;388:2895–2903. doi: 10.1016/S0140-6736(16)32049-9 [DOI] [PubMed] [Google Scholar]
- 42.Rumsfeld JS, Alexander KP, Goff DC, Jr, Graham MM, Ho PM, Masoudi FA, Moser DK, Roger VL, Slaughter MS, Smolderen KG, et al. ; American Heart Association Council on Quality of Care and Outcomes Research, Council on Cardiovascular and Stroke Nursing, Council on Epidemiology and Prevention, Council on Peripheral Vascular Disease, and Stroke Council. Cardiovascular health: the importance of measuring patient-reported health status: a scientific statement from the American Heart Association. Circulation. 2013;127:2233–2249. doi: 10.1161/CIR.0b013e3182949a2e [DOI] [PubMed] [Google Scholar]
- 43.Tricoci P, Allen JM, Kramer JM, Califf RM, Smith SC., Jr. Scientific evidence underlying the ACC/AHA clinical practice guidelines. JAMA. 2009;301:831–841. doi: 10.1001/jama.2009.205 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


