Abstract
Noninvasive continuous arterial pressure monitoring may be clinically useful in patients who require continuous blood pressure monitoring in situations where arterial catheter placement is limited. Many previous studies on the accuracy of the noninvasive continuous blood pressure monitoring method reported various results. However, there is no research on the effectiveness of noninvasive arterial pressure monitoring during one-lung ventilation. The purpose of this study was to compare arterial blood pressure obtained through invasive method and noninvasive method by using ClearSight during one-lung ventilation.
In this retrospective observational study, a total of 26 patients undergoing one-lung ventilation for thoracic surgery at a single institution between March and July 2019 were recruited. All patients in this study were cannulated on their radial artery to measure continuously invasive blood pressures and applied ClearSight on the ipsilateral side of the cannulated arm. We compared and analyzed the agreement and trendability of blood pressure recorded with invasive and noninvasive methods during one-lung ventilation.
Blood pressure and pulse rate showed a narrower limit of agreement with a percentage error value of around 30%. In addition, the tracking ability of each measurement could be determined by the concordance rate, all of which were below acceptable limits (92%).
In noninvasive arterial blood pressure monitoring using ClearSight, mean blood pressure and pulse rate show acceptable agreement with the invasive method.
Keywords: ClearSight, noninvasive continuous arterial pressure monitoring, one-lung ventilation, thoracic surgery
1. Introduction
Intraoperative hypotension is associated with postoperative complications and increased mortality; therefore, continuously invasive blood pressure monitoring during surgery with potential hemodynamic changes is considered to be essential.[1] Especially, thoracic surgery is one of the surgeries in which severe hemodynamic changes can occur, so continuous blood pressure monitoring is essential. Arterial catheter cannulation allows continuous blood pressure monitoring, but often causes postoperative cannula site pain and, in rare cases, complications such as infection, bleeding, thrombus formation, ischemic injury, and nerve damage.[2]
ClearSight (Edwards Lifesciences Corp., Irvine, California) recently introduced a non-invasive monitoring instrument that can continuously measure hemodynamic factors such as arterial pressure, CO, and cardiac parameters using finger cuffs.[3] ClearSight, formerly known as Nexfin, makes measurements by calculating the arterial pressure wave form using the volume clamp method.[4,5] This is done by measuring the finger arterial pressure by placing the inflatable cuff on the middle phalanx. The volume clamp method is a method of obtaining arterial pressure by a photoelectric plethysmograph and automatic algorithm by applying varying counter-pressures to maintain a constant volume in the pulsating artery.[6] The finger arterial pressure calculated by this method is converted into brachial artery pressure using a general algorithm.[6] The cardiac output is obtained by the pulse contour method and is updated every 20 seconds.[7]
The accuracy and trend of noninvasive arterial pressure measurement using ClearSight during the third trimester of pregnancy, carotid endarterectomy, non-cardiac surgery, and abdominal aortic aneurysm surgery have been studied.[6,8–10] Previous studies on the accuracy of the continuous blood pressure monitoring method reported conflicting results.[9,11–19] However, there is no research on the accuracy and effectiveness of ClearSight in thoracic surgery requiring one-lung ventilation. Although this new non-invasive hemodynamic monitoring method may not completely replace conventional arterial catheterization, it is necessary to study whether it can be used in simple surgeries, such as pneumothorax, or in situations where arterial catheter placement is limited. The purpose of this study was to compare arterial blood pressure obtained through invasive method and noninvasive method by using ClearSight during one-lung ventilation and analyze the trend and accuracy between 2 measurement methods using the Bland-Altman analysis method.[20,21]
2. Methods
2.1. Study population
The protocol of this retrospective observational study was approved by the Institutional Review Board of Kyung Hee University Hospital (KHUH 2020-04-053) and met the guidelines of the Declaration of Helsinki. The informed consent of individual patient was waived by our local ethical committee. We retrospectively included the patients in whom noninvasive arterial pressure was measured by ClearSight and invasive arterial pressure was measured simultaneously during one-lung ventilation for thoracic surgery at our institution between March and July 2019. Patients were excluded if they underwent emergency surgery, had prior arterial cannulation in the upper extremities or thorax, atrial fibrillation, peripheral vascular disease, a history of upper arm vascular surgery. All clinical data were obtained from the electronic medical records system of the institution.
2.2. Anesthesia and perioperative management
Anesthesia was induced with propofol 1.5 to 2.5 mg/kg bolus and remifentanil continuous infusion. After a bolus injection of rocuronium 1.0 mg/kg, a double-lumen tube was intubated for one-lung ventilation and the optimal position of the tube was confirmed using fiberoptic bronchoscopy. If the result of a modified Allen test is negative, the radial artery of the wrist in the contralateral side of surgery was cannulated after induction of anesthesia. The finger cuff of ClearSight was attached to the mid-phalanx of the index or middle finger, ipsilateral to the radial artery catheter. The patient's position was changed from supine position to lateral decubitus so that the surgical field faced upwards. When patients are positioned laterally as for thoracic surgery, the position of the transducers (Edwards Lifesciences, Irvine, California) of the invasive blood pressure measurement and ClearSight were adjusted to the same as the level of the right atrium (RA) in order to correct the significant hydrostatic gradient in blood pressure according to the difference in the level of 2 measuring positions. Anesthesia was maintained during surgery with anesthetic drugs such as propofol, remifentanil, and rocuronium. During surgery, propofol was adjusted to maintain proper anesthetic depth while monitoring the levels of the bispectral index.
2.3. Clinical variables and perioperative variables
Demographic variables recorded included patient age, sex, weight, height, and body mass index (BMI). Preoperative variables included previous medical history, including hypertension and diabetes mellitus. Intraoperative data included anesthesia time, surgery time, one-lung ventilation time, and hemodynamic parameters including pulse rate (PR), systolic arterial blood pressure (SAP), diastolic arterial blood pressure (DAP), mean arterial blood pressure (MAP). Of all the data measured in this study, only the data measured during one-lung ventilation were compared and analyzed. Because variation and artifacts that occur due to posture change occur during other times, one-lung ventilation data was used for data analysis to ensure reliability of measured data. The purpose of this study was to verify the agreement between the 2 measurement methods during one-lung ventilation.
2.4. Sample size and clinical data
In a study of patients in the third trimester, there was controversy over the sample size because the Bland-Altman method is not a statistical test.[8] There is no established concept for the appropriate number of patients or the number of measurements required in studies comparing repeated measurements.[22] Compared to the previous study using ClearSightTM that basically analyzed about 3000 pairs of data, over 8400 pairs of data used in our study is considered to be a sufficient sample size for interpreting the results.[19,22]
2.5. Statistical analysis
Categorical variables are expressed as numbers and percentages, and continuous variables as means and standard deviations (SD). Patients’ hemodynamic data were compared using paired t tests. All statistical analyses were performed using “R” statistical software (R ver. 3.5.1.), with P <.05 considered statistically significant. The Bland–Altman method was used to quantify agreement.[20,21] Bias (mean difference between the noninvasive method and the invasive method) represents the systematic error between methods, and precision (SD of the bias) represents the random error or variability between techniques. In this study, it was considered acceptable if the bias was less than 5 mmHg according to the Association for the Advancement of Medical Instrumentation guidelines.[9,18] Limits of agreement (LOA) were calculated as bias ± 2 standard deviation (SD) and defined the range in which 95% of the differences between methods were expected to fall. The percentage error was calculated as the ratio of 2SD of the bias to the mean parameter of the invasive method. The percentage error was considered clinically acceptable, and the noninvasive method (ClearSight) was regarded as interchangeable with the invasive method, if results were below 30%, as proposed by Critchley et al. Bias, LOA, and percentage error between 2 methods were calculated for all data.[23]
3. Results
3.1. Participants
A total of 30 patients undergoing thoracic surgery requiring one-lung ventilation were recruited during the study period, 2 of whom were excluded for cardiac arrhythmia and 2 others were excluded for rejecting consent. Of the 26 patients, 14 underwent wedge resection and the last patients underwent lobectomy or segmentectomy. Fourteen patients who underwent wedge resection were operated with VATS, and all other patients underwent open procedure through thoracotomy (Table 1). Of the 9427 paired measures of the invasive and noninvasive methods from 26 patients, 8408 measures were used for the final analysis, with the exception of double missing and measurement errors (Fig. 1). The mean age of study patients is 61.9 years, and 21 of 26 patients (more than 80%) were male patients. Patients’ demographic and operative characteristics are shown in Table 1.
Table 1.
Demographic and intraoperative data.
| Variable | Number (percentage) or mean ± SD |
| Number of patients | 26 |
| Demographics | |
| Age (year) | 61.9 ± 13.9 |
| Sex (male) | 21 (80.8%) |
| Clinical characteristics | |
| Height (cm) | 162.9 ± 8.2 |
| Weight (kg) | 64.4 ± 9.3 |
| BMI (kg/m2) | 24.3 ± 3.4 |
| Medical history | |
| HTN | 11 (42.3%) |
| DM | 10 (38.5%) |
| Type of surgery | |
| Thoracotomy | 12 (46.2%) |
| VATS | 14 (53.8%) |
| Intraoperative data | |
| Anesthesia time (min) | 138.1 ± 56.8 |
| Surgery time (min) | 91.7 ± 52.9 |
| OLV time (min) | 74.1 ± 48.1 |
SD = standard deviation, BMI = body mass index, HTN = hypertension, DM = diabetes mellitus, VATS = video-assisted thoracic surgery, OLV = one-lung ventilation.
Figure 1.
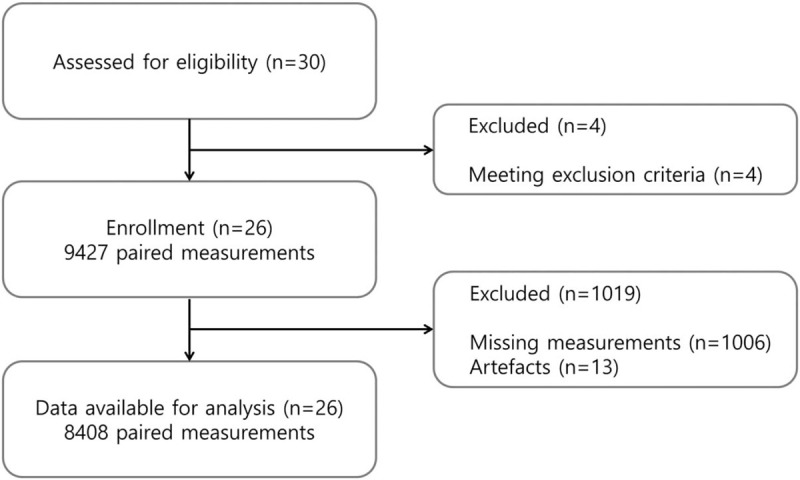
Study flow chart.
3.2. Analyses of agreement
Bland–Altman analysis was used to find out the accuracy of the measured values according to invasive and noninvasive methods (Fig. 2). The biases, percentage error, and LOA for each variable are shown in Table 2. The bias of SAP was −5.18 mmHg and limits of agreement for SAP was −37.81 to 27.45 mmHg with percentage error of 31.01% showing an overestimation of SAP with ClearSight. The bias of DAP was 5.16 mmHg and limits of agreement for DAP was −12.41 to 22.72 mmHg with percentage error of 27.14% showing an underestimation of DAP with ClearSight. The bias of MAP was 1.05 mmHg and limits of agreement was −18.85 to 20.95 mmHg with percentage error of 25.23% showing a slightly underestimation of MAP with ClearSight. The bias of PR was 0.21 mmHg and limits of agreement for PR showed the narrowest LOA from −8.22 to 8.63 mmHg, and the least percentage error value of 11.65% reflected the most accurate predictive performance with ClearSight.
Figure 2.
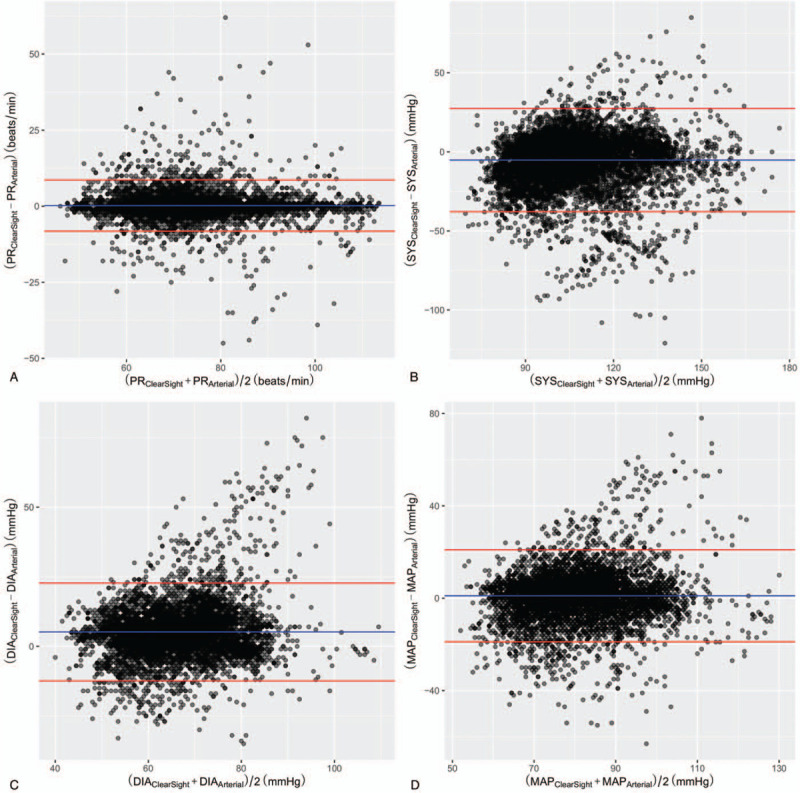
Bland–Altman plot for arterial blood pressure measurements with bias and 95% limits of agreement. Bland–Altman plot showing accuracy (A) between PRClearSight and PRArterial, (B) between SYSClearSight and SYSArterial, (C) between DIAClearSight and DIAArterial, and (D) between MAPClearSight and MAPArterial. PR = pulse rate, SYS = systolic blood pressure, DIA = diastolic blood pressure, MAP = mean arterial blood pressure.
Table 2.
Comparison of hemodynamic measurements between the invasive method and ClearSight.
| Variable | Invasive method | ClearSight | Percentage error | Bias | LOA |
| PR | 73.68 ± 12.37 | 73.88 ± 12.27 | 11.65 | 0.21 | −8.22 to 8.63 |
| Blood pressure; mmHg | |||||
| Systolic | 109.93 ± 17.18 | 104.76 ± 18.29 | 31.01 | −5.18 | −37.81 to 27.45 |
| Diastolic | 63.45 ± 9.50 | 68.61 ± 10.78 | 27.14 | 5.16 | −12.41 to 22.72 |
| Mean | 79.95 ± 11.46 | 80.99 ± 12.47 | 25.23 | 1.05 | −18.85 to 20.95 |
Values are presented as mean ± standard deviation.
LOA = limits of agreement, PR = pulse rate.
3.3. Analyses of trendability
A 4-quadrant plot was used to analyze the trendability of each hemodynamic variable (Fig. 3). The ratio of data located in the upper right or lower left quadrant of the 4-quadrant plot is defined as the concordance rate.[23] The respective concordance rates for PR, SAP, DAP, and MAP were 90.3, 53.8, 51.7, and 42.8%. These concordance rates were below 92%, suggested by the cut off value in the previous study.[23] In order to analyze the degree of agreement between the changes in the 2 methods, the polar plot is expressed around a horizontal line of 90 degrees in terms of the angle between the line of identity (“Y = X”) and the vector of each data and the magnitude of the vector as the radius of polar plot (Fig. 4). Therefore, it is considered that the data formed by the angle of the vector in the polar plot is within 30 degrees from the horizontal line is valid.
Figure 3.
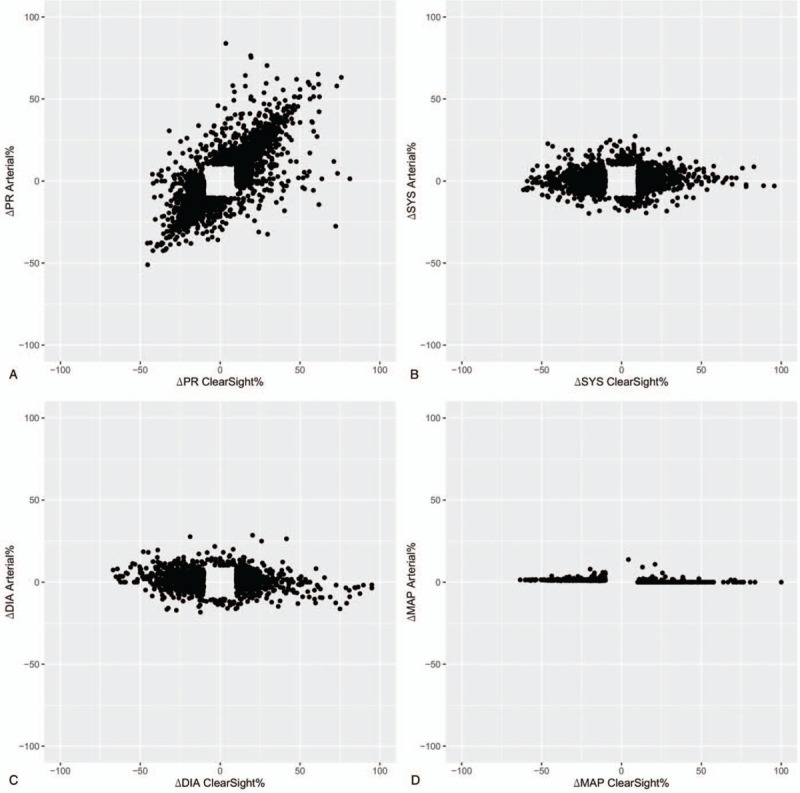
Four quadrant plot showing trendability (A) between PRClearSight and PRArterial, (B) between SYSClearSight and SYSArterial, (C) between DIAClearSight and DIAArterial, and (D) between MAPClearSight and MAPArterial. PR = pulse rate, SYS = systolic blood pressure, DIA = diastolic blood pressure, MAP = mean arterial blood pressure.
Figure 4.
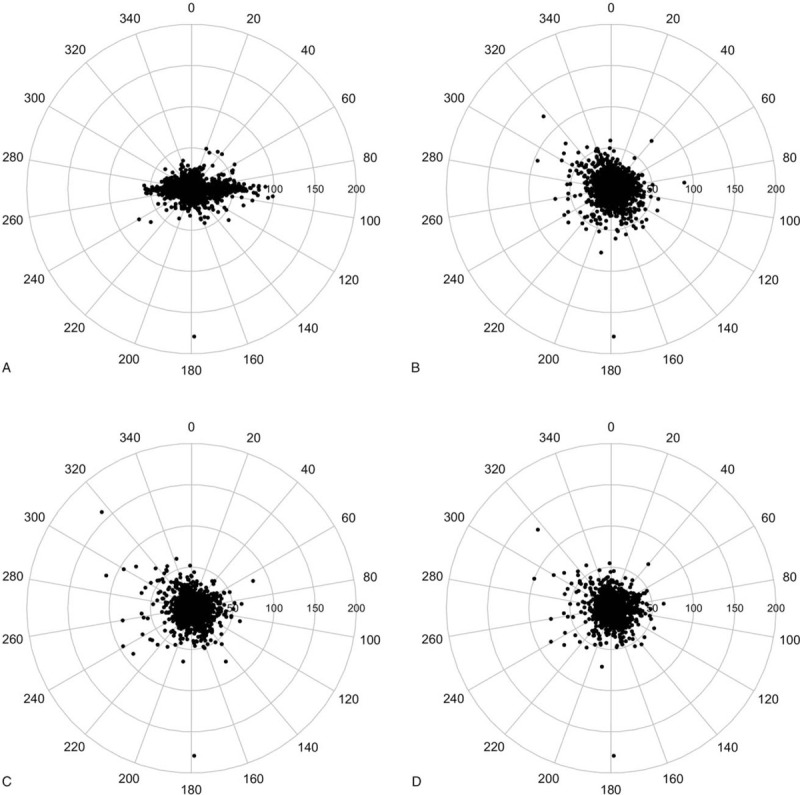
Polar plot to analyze the degree of agreement in the changes in the measurements (A) for PRClearSight compared with PRArterial, (B) for SYSClearSight compared with SYSArterial, (C) for DIAClearSight compared with DIAArterial, and (D) for MAPClearSight compared with MAPArterial. PR = pulse rate, SYS = systolic blood pressure, DIA = diastolic blood pressure, MAP = mean arterial blood pressure.
4. Discussion
Until now, the usefulness of blood pressure measurement using a noninvasive method needs to be verified in various clinical situations. Furthermore, recently, noninvasive hemodynamic monitoring devices using finger cuffs such as ClearSight have been developed and applied to clinical trials, especially to critically ill patients.[24] Therefore, the results of the study for monitoring arterial pressure using ClearSight are different depending on the clinical situation and various research environments, so there is still lack of evidence showing the accuracy and clinical usefulness of ClearSight.
In this study, we investigated the accuracy and trendability of noninvasive method using ClearSight in patients undergoing thoracic surgery requiring one-lung ventilation by comparing ClearSight-derived arterial blood pressure monitoring with a conventional invasive method. Through our study, it was found that the mean blood pressure and pulse rate had statistically significant agreement between the 2 methods, and although SAP and DAP did not have an acceptable agreement between 2 methods, they showed almost close to the acceptable level of agreement. To the best of our knowledge, this is the first study to investigate the accuracy and usefulness of a noninvasive arterial blood pressure monitoring using ClearSight in thoracic surgery during one-lung ventilation.
Previous studies have attempted to determine the accuracy of arterial pressure monitoring using ClearSight.[9,19,25] In a previous study, there was a study comparing blood pressure measured using the continuous noninvasive method and the invasive method on patients undergoing carotid surgery.[9,19] The study reported that the bias of minus values for the blood pressure values such as SAP, DAP, and MAP reflected the result of overestimation with ClearSight.[9,19] On the other hand, various bias values were observed from negative to positive in our study. Only MAP and PR values showed the degree of agreement that satisfied the Association for the Advancement of Medical Instrumentation criteria, and SAP and DAP exceeded the reference values. This was similar to that reported in previous studies.[25] This result is probably because the waveform obtained through ClearSight is the brachial blood pressure from a specific algorithm, and the waveform obtained by the invasive method is the radial blood pressure, so this difference is thought to have influenced the bias. As it goes from aorta to the peripheral blood vessel, the arterial pressure waveform changes shape due to reflection and blood flow resistance.[9] As the systolic blood pressure becomes larger and the diastolic blood pressure becomes smaller, the pulse pressure increases.[9] Therefore, this fact is somewhat consistent with the results of measuring the bias in which SAP is larger and DAP is smaller. Therefore, it may be reasonable to compare MAP in the blood pressure comparison of the 2 measurement methods. In fact, it was confirmed that the results showed similar degree of agreement in MAP. In this study, the authors compared the accuracy and trendability of the values of continuous arterial pressure variables monitored using the invasive arterial cannulation and those obtained using the noninvasive ClearSight method in thoracic surgery that requires one-lung ventilation. This study is similar to the previous study in that it attempts to determine the accuracy and consistency of ClearSight. However, this study is intended to examine its usefulness in other surgical types.
As mentioned above, arterial catheter insertion can cause several complications. Although arterial catheter insertion is not recommended to simple pneumothorax surgery in young healthy patients, continuous blood pressure monitoring is possible with ClearSite. In simple pneumothorax surgery, future studies will be needed to determine whether continuous blood pressure monitoring lowers the incidence of hypotension compared to NIBP. Additionally, ClearSight may be helpful in cases where it is difficult to mount an arterial catheter, such as shock patients, patients with coagulation disorders, and patients requiring vascular protection due to dialysis.[22]
Our study has some limitations. First of all, this study has limitations due to the analysis based on the data collected retrospectively. Since the data were collected retrospectively, it was more limited than the prospective study to control various variables that influence the measurement. We tried to overcome the limitations of the retrospective study to some extent by selecting the patient group and the necessary data in consideration of the exclusion criteria used in the previous prospective study.[9] However, prospective studies will be needed for more reliable and accurate conclusions in the future. The limitations of this study may be the bias between the blood pressure measured by ClearSight measured on different arms and the blood pressure measured by the invasive method and the difference in measurement due to the lateral position. However, we tried to reduce this measurement bias by placing the transducers of 2 methods at the same level of RA. Moreover, it was difficult to know whether the value of hemodynamic parameters such as cardiac output and stroke volume through this study, which can be measured by ClearSight, are reliable. For a more accurate comparative study, it is more appropriate to verify the accuracy and usefulness of ClearSight in monitoring other hemodynamic parameters such as cardiac output and stroke volume by comparing it with a more reliable method by measuring the cardiac output using echocardiography or invasive pulmonary arterial catheterization. Another limitation of the study is that the total sample size is small. However, since the previous study to investigate the accuracy of ClearSight was conducted in a group of 20 to 30 patients, we believe that the sample size of 26 patients in our study is not small.[6,9,26] In addition, the number of hemodynamic data of over 8000 used in the analysis is much larger than the previous studies, so it seems to be a sufficient amount of data for analysis.[6,9,26]
5. Conclusion
In noninvasive arterial blood pressure monitoring using ClearSight, mean blood pressure and pulse rate shows acceptable agreement with the invasive method. Although arterial blood pressure monitoring using ClearSightTM is limited in use when there is peripheral vascular disease or when blood samples for arterial blood gas analysis have to be drawn, this study showed some usefulness in clinical use of ClearSight instead of conventional arterial pressure monitoring through arterial cannulation in thoracic surgery requiring one-lung ventilation. However, in the future, it is necessary to evaluate the accuracy of noninvasive arterial blood pressure monitoring under various surgical conditions in order to broaden the indications of that in the anesthesia monitoring part.
Author contributions
Conceptualization: Sang-Wook Lee, Sangho Lee, Hyungtae Kim, Yun-Jong Kim, Mihyeon Kim, Jeong-Hyun Choi.
Data curation: Hyungtae Kim, Yun-Jong Kim, Mihyeon Kim, Jeong-Hyun Choi.
Formal analysis: Sang-Wook Lee, Sangho Lee, Jeong-Hyun Choi.
Methodology: Sang-Wook Lee, Jeong-Hyun Choi.
Supervision: Jeong-Hyun Choi.
Visualization: Sang-Wook Lee.
Writing – original draft: Sang-Wook Lee, Jeong-Hyun Choi.
Writing – review & editing: Sang-Wook Lee, Sangho Lee, Hyungtae Kim, Yun-Jong Kim, Mihyeon Kim, Jeong-Hyun Choi.
Footnotes
Abbreviations: AAMI = Association for the Advancement of Medical Instrumentation, BMI = body mass index, DAP = diastolic arterial blood pressure, LOA = limits of agreement, MAP = mean arterial blood pressure, PR = pulse rate, RA = right atrium, SAP = systolic arterial blood pressure, SD = standard deviation.
How to cite this article: Lee SW, Lee S, Kim H, Kim YJ, Kim M, Choi JH. Accuracy of noninvasive continuous arterial pressure monitoring using ClearSight during one-lung ventilation. Medicine. 2021;100:11(e25152).
This study was approved by the Institutional Review Board of Kyung Hee University Hospital (KHUH 2020-04-053). The informed consent of individual patient was waived by the Institutional Review Board of Kyung Hee University Hospital.
The authors have no funding and conflicts of interests to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Walsh M, Devereaux PJ, Garg AX, et al. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology 2013;119:507–15. [DOI] [PubMed] [Google Scholar]
- [2].Monk TG, Bronsert MR, Henderson WG, et al. Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery. Anesthesiology 2015;123:307–19. [DOI] [PubMed] [Google Scholar]
- [3].Scheer B, Perel A, Pfeiffer UJ. Clinical review: complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine. Crit Care 2002;6:199–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Clement RP, Vos JJ, Scheeren TWL. Minimally invasive cardiac output technologies in the ICU: putting it all together. Curr Opin Crit Care 2017;23:302–9. [DOI] [PubMed] [Google Scholar]
- [5].Penaz J, Voigt A, Teichmann W. Contribution to the continuous indirect blood pressure measurement. Z Gesamte Inn Med 1976;31:1030–3. [PubMed] [Google Scholar]
- [6].Sumiyoshi M, Maeda T, Miyazaki E, et al. Accuracy of the ClearSight system in patients undergoing abdominal aortic aneurysm surgery. J Anesth 2019;33:364–71. [DOI] [PubMed] [Google Scholar]
- [7].Wesseling KH, Jansen JR, Settels JJ, et al. Computation of aortic flow from pressure in humans using a nonlinear, three-element model. J Appl Physiol 19851993;74:2566–73. [DOI] [PubMed] [Google Scholar]
- [8].Duclos G, Hili A, Resseguier N, et al. Clearsight use for haemodynamic monitoring during the third trimester of pregnancy - a validation study. Int J Obstet Anesth 2018;36:85–95. [DOI] [PubMed] [Google Scholar]
- [9].Noto A, Sanfilippo F, De Salvo G, et al. Noninvasive continuous arterial pressure monitoring with Clearsight during awake carotid endarterectomy: a prospective observational study. Eur J Anaesthesiol 2019;36:144–52. [DOI] [PubMed] [Google Scholar]
- [10].Maheshwari K, Khanna S, Bajracharya GR, et al. A randomized trial of continuous noninvasive blood pressure monitoring during noncardiac surgery. Anesth Analg 2018;127:424–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Hofhuizen C, Lansdorp B, van der Hoeven JG, et al. Validation of noninvasive pulse contour cardiac output using finger arterial pressure in cardiac surgery patients requiring fluid therapy. J Crit Care 2014;29:161–5. [DOI] [PubMed] [Google Scholar]
- [12].Martina JR, Westerhof BE, de Jonge N, et al. Noninvasive arterial blood pressure waveforms in patients with continuous-flow left ventricular assist devices. ASAIO J 2014;60:154–61. [DOI] [PubMed] [Google Scholar]
- [13].Hohn A, Defosse JM, Becker S, et al. Non-invasive continuous arterial pressure monitoring with Nexfin does not sufficiently replace invasive measurements in critically ill patients. Br J Anaesth 2013;111:178–84. [DOI] [PubMed] [Google Scholar]
- [14].Monnet X, Picard F, Lidzborski E, et al. The estimation of cardiac output by the Nexfin device is of poor reliability for tracking the effects of a fluid challenge. Crit Care 2012;16:R212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Fischer MO, Avram R, Carjaliu I, et al. Non-invasive continuous arterial pressure and cardiac index monitoring with Nexfin after cardiac surgery. Br J Anaesth 2012;109:514–21. [DOI] [PubMed] [Google Scholar]
- [16].Martina JR, Westerhof BE, van Goudoever J, et al. Noninvasive continuous arterial blood pressure monitoring with Nexfin(R). Anesthesiology 2012;116:1092–103. [DOI] [PubMed] [Google Scholar]
- [17].Stover JF, Stocker R, Lenherr R, et al. Noninvasive cardiac output and blood pressure monitoring cannot replace an invasive monitoring system in critically ill patients. BMC Anesthesiol 2009;9:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Vos JJ, Poterman M, Mooyaart EA, et al. Comparison of continuous non-invasive finger arterial pressure monitoring with conventional intermittent automated arm arterial pressure measurement in patients under general anaesthesia. Br J Anaesth 2014;113:67–74. [DOI] [PubMed] [Google Scholar]
- [19].Heusdens JF, Lof S, Pennekamp CW, et al. Validation of non-invasive arterial pressure monitoring during carotid endarterectomy. Br J Anaesth 2016;117:316–23. [DOI] [PubMed] [Google Scholar]
- [20].Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307–10. [PubMed] [Google Scholar]
- [21].Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat 2007;17:571–82. [DOI] [PubMed] [Google Scholar]
- [22].Tanioku T, Yoshida A, Aratani Y, et al. Validation of noninvasive continuous arterial pressure measurement by ClearSight system during induction of anesthesia for cardiovascular surgery. BMC Anesthesiol 2020;20:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Critchley LA, Lee A, Ho AM. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg 2010;111:1180–92. [DOI] [PubMed] [Google Scholar]
- [24].Ameloot K, Palmers PJ, Malbrain ML. The accuracy of noninvasive cardiac output and pressure measurements with finger cuff: a concise review. Curr Opin Crit Care 2015;21:232–9. [DOI] [PubMed] [Google Scholar]
- [25].Ilies C, Grudev G, Hedderich J, et al. Comparison of a continuous noninvasive arterial pressure device with invasive measurements in cardiovascular postsurgical intensive care patients: a prospective observational study. Eur J Anaesthesiol 2015;32:20–8. [DOI] [PubMed] [Google Scholar]
- [26].Boisson M, Poignard ME, Pontier B, et al. Cardiac output monitoring with thermodilution pulse-contour analysis vs. non-invasive pulse-contour analysis. Anaesthesia 2019;74:735–40. [DOI] [PubMed] [Google Scholar]


