Abstract
The objective of this study was to ascertain changes in symptoms of patients with borderline personality disorder undergoing psychodynamic day treatment with a duration of 9 months and the factors that predict clinical outcome or dropouts from the program.
In an observational study, demographic characteristics (age, number of psychiatric hospitalizations, number of suicide attempts, current involvement in work or study activities), day doses of antipsychotic and antidepressant medication, psychiatric symptoms, and social functioning (Health of the Nation Outcome Scales), and symptoms of dissociation (Dissociative Experiences Scale) were assessed in patients at the beginning of treatment (N = 105). Further, psychiatric symptoms and social functioning were assessed at 3 stages: beginning of the program, end of the program, and 1-year follow-up. To study the differences between baseline values and values at the end of the treatment and follow-up values, the Wilcoxon signed-rank test was used. To discover baseline factors related to the effect of the treatment, Spearman correlation coefficients were calculated. To evaluate the differences between patients who completed the program (N = 67) and patients who dropped out (N = 38), differences in baseline factors between both groups were compared, using the Mann–Whitney test for independent samples.
Improvement in symptoms (Health of the Nation Outcome Scales – version for external evaluators) at the end of the therapy (N = 67, P < .001) and at the 1-year follow-up (N = 46, P < .001) was found. Experience of an intimate relationship was positively related to clinical improvement at follow-up examinations (P < .001). Predictors of dropout included a higher number of psychiatric hospitalizations (P = .004), suicide attempts (P = .004), more severe pretreatment symptoms (P = .002), and symptoms of dissociation (P = .046).
The results indicate that a psychodynamic day treatment is feasible for the treatment of less clinically disturbed patients with a history of intimate relationships. Patients with a higher number of previous psychiatric hospitalizations, more suicide attempts in the past, more severe pretreatment symptoms, and symptoms of dissociation are more likely not to complete the program.
Keywords: borderline personality disorder, dropout predictors, outcome predictors, psychodynamic day clinic
1. Introduction
Borderline personality disorder (BPD) is a condition that seriously damages interpersonal relationships and causes severe psychiatric symptoms demanding long-term treatment, with psychotherapy as a priority.[1] Although there is widening research supporting the effect of specialized psychotherapeutic methods in BPD, such as transference focused psychotherapy, mentalization-based treatment (MBT), dialectical behavior therapy (DBT), schema-focused therapy,[2] less attention has been paid to traditional psychotherapeutic programs for BPD, such as a psychodynamic day treatment which is clinically widespread, at least in some countries.[3] Prior studies[4–7] have shown some promise for this treatment model, but further study is needed specifically to explore several areas that have not been considered earlier (shorter treatment duration, treatment provided by qualified psychotherapists, and treatment among a homogenous group of individuals with BPD). In this respect, this study aimed to identify whether a large cohort of participants exposed to psychodynamic day treatment for a duration of 9 months, led by qualified psychotherapists, can demonstrate within-person change over time in a homogenous sample of BPD patients. In addition, the present study aimed to track treatment outcomes on the subjective level from patients at the end of the treatment and the follow-up assessment.
Within the context of treatment, a knowledge of the predictors of treatment outcome could enable clinicians to choose a more appropriate form of therapy for a specific patient. However, results of studies researching outcome variables in psychotherapies in BPD are heterogenous and the only consistent predictors of therapeutic change might be the severity of pretreatment symptoms and the quality of the therapeutic alliance.[8–10] While these studies researched treatment programs other than a psychodynamic day program, the question remains whether this type of program could be advantageous for cases with a higher severity of the disorder. The results of studies examining the symptom of severity as a predictor of outcome in psychodynamic psychotherapies other than the daily program are inconsistent: patients with a higher symptom severity of BPD benefited more from MBT treatment than from being involved in structured clinical management.[11] Similarly, severely disturbed patients profited more from the MBT program than from a psychodynamic group-based treatment program, whereas the outcome was comparable between both programs in less severely disturbed patients.[12] On the other hand, lower pretreatment severity predicted a better outcome in psychodynamic object relations psychotherapy than in DBT, while for patients with higher pretreatment severity, there was no significant difference in outcome between both psychotherapies.[13]
In spite of a series of past studies researching pretreatment factors in the treatment of BPD patients, to the best of our knowledge, no study has assessed the symptoms of dissociation in these patients before psychodynamic psychotherapy. Dissociation occurs in about two-thirds of people suffering from BPD, in the form of depersonalization, derealization, absorption, or amnesia. Around 26% to 40% of these belong to “severe dissociators” with a Dissociative Experiences Scale (DES) score of more than 30. Severe dissociators show comorbidity with other dissociative disorders; they have the most severe symptoms and require the most medical care.[14–16] In this context, dissociation is considered as a barrier to clinical improvement in psychotherapy, especially with respect to absorption or imaginative involvement.[17] In psychotherapy for BPD patients, other than psychodynamic, dissociation as a pretreatment predictor gives mixed results.[8] Kleindienst et al[10] found a significant correlation between higher pretreatment DES scores and a worse outcome in DBT.
Specifically, for psychodynamic psychotherapy, the presence of a minimal level of quality of object relations observable as sustained object relations is supposed as being necessary for good treatment outcome.[18] However, instability in interpersonal relationships in relation to identity disturbance is a core feature of BPD patients.[19] Therefore, the experience of a stable relationship may also predict the outcome of therapy.
In this respect, the second aim of this study is to identify baseline factors that could be associated with clinical improvement in this treatment modality (pretreatment symptoms’ severity, symptoms of dissociation, and experience of adult sustained object relations in a patient).
Successful psychotherapeutic treatment for BPD is also hindered by relatively high dropout rates. The proportion of dropouts ranges from 24% to 37% in day clinics for personality disorders.[20,21] For psychotherapies specific to BPD, the average dropout rate was calculated in a meta-analysis of 41 studies and was found to be 29% for long-term therapies (more than 1 year), and 25% for shorter therapies.[22] Previous psychiatric hospitalization, younger age, and fewer contacts with health and social services were found to be pretreatment predictors of premature treatment termination in day treatment programs for personality disorders.[21] The meta-analysis of various psychotherapeutic approaches for BPD did not show any significant sociodemographic or pretreatment variables predicting dropout, with the exception of higher impulsivity, lower suicidality, and some motivational characteristics.[22] On the other hand, problems caused by the symptoms of dissociation and especially of higher absorption may also apply to dropout, because absorption may hinder involvement in therapeutic relationships.
However, to the best of our knowledge, the pretreatment predictors of dropout in a psychodynamic day treatment program for BPD have not been studied. Therefore, the aim of this study is to identify baseline factors that could be associated with dropout from this treatment modality. Consistent with previous studies, it was assumed that younger age, a higher number of psychiatric hospitalizations, lower number of previous suicide attempts, and higher pretreatment symptoms’ severity might be associated with noncompletion of the psychotherapeutic program. It was also supposed that the presence of pretreatment work or study activities as an indicator of overall motivation may be associated with the completion of the program. On the other hand, it was assumed that more severe dissociation symptoms may be associated with not completing the program as a hindrance of involvement in therapeutic relationships.
Based on the background and the aims described in this Introduction, the following hypotheses were postulated in this study:
-
1.
a homogenous sample of BPD patients completing a psychodynamic day program for a duration of 9 months shows within-person change in symptoms and interpersonal functioning at the end of the treatment and at the follow-up assessment 1 year after completion of the program;
-
2.
baseline pretreatment symptoms’ severity, symptoms of dissociation, and experience of adult sustained object relations in a patient are associated with clinical improvement in the program;
-
3.
the group of patients who dropped out of the program differs from the group of completers of the program in the following baseline factors: higher number of previous psychiatric hospitalizations, lower number of previous suicide attempts, lower presence of work or study activities, higher pretreatment symptoms’ severity, and more severe symptoms of dissociation.
This study should contribute to answering the question: “What treatment for whom?” That is, to help identify the characteristics of BPD in patients in whom we could expect a greater benefit from the treatment and who are more likely to complete the program. This issue is particularly important, given the relatively high proportion of BPD patients who do not complete therapeutic programs and the focus on those groups of BPD patients who can be expected to have the best possible outcome of the treatment.
In the following Materials and Methods section, the sample, its inclusion, and exclusion criteria will be described, followed by a description of the therapeutic program. Thereafter, the psychometric measures used in the study will be stated. This is followed by mention of how the data in the sample were collected. Next follows a description of the data analysis and statistical methods used in this study. The article concludes with the usual division into sections: Results, Discussion, and Conclusions.
2. Materials and methods
2.1. Participants
The participants for this study were patients from a daily group psychotherapeutic treatment program for BPD at the ESET Psychotherapeutic and Psychosomatic Clinic in Prague. The Clinic's admitting psychiatrist was responsible for the decision to enroll the patients in the treatment program. The participants were asked to sign an informed consent form for participation in the study. This study was approved by the Ethical Committee of ESET Clinic. Patients who had been diagnosed with BPD based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV, TR),[23] and who entered the treatment program from January 1, 2008 until August 31, 2017 were included. The diagnosis of BPD in patients was confirmed using a semistructured interview for BPD, Structured Clinical Interview for DSM Disorders-II.[24] It was also required that patients should simultaneously have fulfilled the criteria for emotionally unstable personality disorder (F60.3 diagnosis according to International Classification of Diseases 10th Revision).[25] Exclusion criteria were organic illnesses involving the central nervous system, substance and/or alcohol use disorders (based on medical record and self-report), mental retardation (IQ Raven lower than 90),[26] also comprising conditions affecting the ability to fill out the assessments for these medical reasons, and refusal to sign the informed consent.
The following demographic data for the sample were gathered: age, sex, level of education, length of psychiatric treatment, number of psychiatric hospitalizations, number of suicide attempts. The presence of a current or previous relationship or marriage was also ascertained among the participants, as well as the current involvement in study or work activities. The demographic data were collected with the aid of semistructured interviews conducted by a nurse and were recorded in a pre-prepared form. Current prescription data, dates of previous suicide attempts, psychiatric hospitalizations, and length of psychiatric treatment from self-reports by the patients were also obtained. These data were checked in the medical records. Current daily doses of antipsychotic medication in equivalents of chlorpromazine, and antidepressant medication in equivalents of fluoxetine, were calculated for all participants.[27–29]
2.2. Therapeutic program
The day clinic schedule consisted of a daily psychotherapeutic program in a half-open group of 6 to 9 participants. The half-open group implied that new patients could enter the group and stay there for a certain length of time. The group consisted of newcomers and existing members who had been part of the group for some time; group members joined and left the group at different times. The treatment lasted for 9 months for every patient. Patients entered and left the program individually throughout the year. The therapy took place every day except the weekend. All treatment decisions during the therapeutic program were made as routine clinical care. The basis of the program was group psychodynamic psychotherapy, which lasted for 2 to 3 hours daily (13 hours weekly). The group psychotherapy was based on “here and now” group interaction and was adapted to work with BPD patients.[30] Group dynamics were directed to the effort of understanding and dealing with relationships between therapists and patients, mutual relationships among patients, and for the promotion of the self-concept of patients. An essential element of the therapeutic process was the elaboration of transference and counter-transference, containment of patients’ feelings, interpretation of projective mechanisms and mental contents, linking current experience with past experiences, and creating awareness of immature defense mechanisms of behavior. The group provided a safe space for the creation of more mature defense mechanisms. A further essential point was the creation of a group history and culture, and the involvement of patients in the comanagement of the group. Continuous and consistent work with group rules and a therapeutic contract was another important area of focus. Physical aggression or substance misuse were not tolerated. In the case of a suspicion of substance misuse, a patient was obligated to undergo regular assessments of urine toxicology at weekly intervals. Patients were eliminated from the program not only if they were found to be intoxicated at a session, but also for any substance misuse occurring between sessions. Patients were required to attend at least 80% of the total sessions in each month. The therapy was terminated for patients who broke any fundamental rules, and another form of treatment was then offered to them. The therapist was the guarantor of creating and maintaining the boundaries within the group, the framework and confidence needed for group work, and interpreting and promoting interpersonal processes in the group, including self-identification of group members. The nondirective and facilitative style of the therapist characterized by his neutrality and objectivity facilitates self-growth and self-regulation of the patients.[31]
Additional therapeutic activities included: practical training (shopping, cooking, dishwashing, dining) – 5 hours per week; social skills training (including role modeling and nonverbal techniques) – 2 hours per week; bibliotherapy – 1 hour per week; music therapy – 1 hour per week; physical exercise – 1 hour per week; and occupational therapy – 1 hour per week. All the additional activities were included within the framework of the psychodynamic program, that is, the content of these interactions was worked through in psychodynamic groups. Attendance was counted as overall attendance in the program (at least 80%) including both therapy sessions and additional activities.
The group sessions were conducted by 1 clinical psychologist and 1 nurse. The additional activities were organized by the nurse.[32] The clinical psychologist and nurse were trained in psychodynamic group psychotherapy. The therapeutic team obtained regular bi-monthly external supervision by a clinical psychologist trained in psychoanalysis and group analysis. The same supervisor, clinical psychologist, and nurse attended to the patients throughout the duration of the study.
2.3. Psychometric measures
Symptomatology and the social functioning of patients were measured with the Health of the Nation Outcome Scales (HoNOS).[33] The scale includes 12 items (overactive, aggressive, disruptive, or agitated behavior; nonaccidental self-injury; problem-drinking or drug-taking; cognitive problems; physical illness or disability problems; problems associated with hallucinations or delusions; problems with depressed mood; other mental and behavioral problems; problems with relationships; problems with activities of daily living; problems with living conditions; problems with occupation and activities). Higher scores on the HoNOS indicated more severe symptoms and deficits in functioning. Cut-off scores, which have been used in previous research,[34] are 12 points for distinguishing very severe from severe mental illness and 7 points for distinguishing severe from mild mental illness. Two versions of the scale are available, the version for external evaluators and the self-rating version for patients. Both versions were translated into the Czech language (Cronbach's alpha 0.797; test-retest reliability after 1 week, r = 0.85).[35] The scale for external evaluators of HoNOS was completed by clinicians who went through a training in this method including checking interrater reliability.
Dissociative symptoms were assessed using the DES.[36] DES is a 28-item self-report questionnaire that evaluates the frequencies of various experiences of dissociative phenomena in everyday life. The score for each item ranges from 0 to 100 and the mean of all item scores is calculated as the DES score. Higher scores on the DES indicate a higher level of dissociation. For a thorough assessment of dissociative symptoms, we analyzed three factors of the DES that focused on: absorption, amnesia related to dissociative states, amnesia related to dissociative states, and depersonalization/derealization.[37] In the present study, we used the Czech version of the DES that, similar to the original English version, displays high reliability and internal consistency (Cronbach's alpha 0.92; test-retest reliability after 1 week, r = 0.91).[38,39]
2.4. Data collection
The patients were assessed 3 times during the study:
-
1.
When entering the program (demographic data, daily doses of medications, HoNOS, DES);
-
2.
At the end of the program (HoNOS); and
-
3.
After 1 year from completion of the program (HoNOS). See Figure 1.
Figure 1.
Assessment time points. Note: B – baseline assessments (demographic data, daily doses of medications, HoNOS, Dissociative Experiences Scale); E – assessment at the end of the treatment (HoNOS); F – follow-up assessment (HoNOS). HoNOS = Health of the Nation Outcome Scales.
2.5. Data analysis
To assess clinical improvement in the patients who underwent the psychodynamic day treatment program, a pre-post design was used. The assessed variables (both versions of HoNOS) were compared to study the differences between baseline values and values at the end of the treatment. Then a similar comparison between baseline values and follow-up values was used. For the psychometric comparisons, a non-parametric statistical test, the Wilcoxon signed-rank test was used, because the data from the psychometric measures were not normally distributed (HoNOS for external evaluators at baseline and at the end of the treatment, Lilliefors test P < .05).
To discover possible baseline factors which might be related to the effect of the treatment, Spearman correlation coefficients between the sum of differences of the values of HoNOS for external evaluators and HoNOS for self-evaluation (baseline values minus values at follow-up examinations) and baseline factors (experience of an intimate relationship/marriage/living as a couple, dissociative symptoms measured by DES, pretreatment symptom severity measured by HoNOS for external evaluators) were calculated. To prevent Type II error, which would disable the rejection of the null hypothesis that the differences in HoNOS values are not linked to baseline factors, a power analysis was performed, and the effect sizes characterizing differences between means and correlation coefficients were assessed. Regrettably, a multiple regression analysis instead of Spearman correlation coefficients could not be used, because some of the variables did not have a normal distribution of values (Kolmogorov–Smirnov tests for experience of an intimate relationship: d = 0.492, P < .01; Shapiro–Wilk test for DES: W = 0.921, P < .01).
To evaluate the differences between patients who completed the program and patients who dropped out, differences in baseline factors (age, number of psychiatric hospitalizations, number of suicide attempts, current involvement in work or study activities, HoNOS – version for external evaluators, and dissociative symptoms measured by DES) were compared between both groups, using the Mann–Whitney test for independent samples.
All statistical analyses were performed using the Statistica software package (version 6).
3. Results
A total of 105 patients who signed the informed consent and fulfilled the inclusion and exclusion requirements (24 males and 81 females) was obtained. In the sample, 53 patients (50%) had other co-occurring clinical diagnoses, apart from BPD (the numbers may overlap): 8 patients (8%) had one other personality disorder; 12 patients (11%) had more than one other personality disorder; 2 patients (2%) had a gender identity disorder; 15 patients (14%) had an affective disorder; 20 patients (19%) had an anxiety disorder, and 3 patients (3%) had eating disorders. The patients had spent an average of 9.7 years (SD = 8) in psychiatric treatment with 1.9 hospitalizations (SD = 2.2) and 2.2 suicide attempts (SD = 4.7). The mean daily dosage of antipsychotic medication in equivalents of chlorpromazine was 63 mg (SD = 156), and of antidepressants in equivalents of fluoxetine was 35 mg (SD = 32). The mean age of the patients was 31.2 years (SD = 8.4). On an average, the patients had received education for 11.8 years (SD = 2.5). Among the patients, 21.2% had a current or previous intimate relationship or marriage, and 49% of the patients were currently involved in work or study activities.
Out of the original sample of 105 patients, 38 did not complete the psychotherapeutic program (premature departures, noncompliance with the rules of attendance). Of the remaining 67 patients, 21 could not be reached for the follow-up assessment. Therefore, complete data (at baseline, at the end of the treatment, and at the follow-up evaluation) for 46 patients were obtained (See Fig. 2). Table 1 shows the demographic characteristics at baseline for the whole sample, including those who completed the program (completers), those who dropped out (dropouts), and those who provided the follow-up data.
Figure 2.
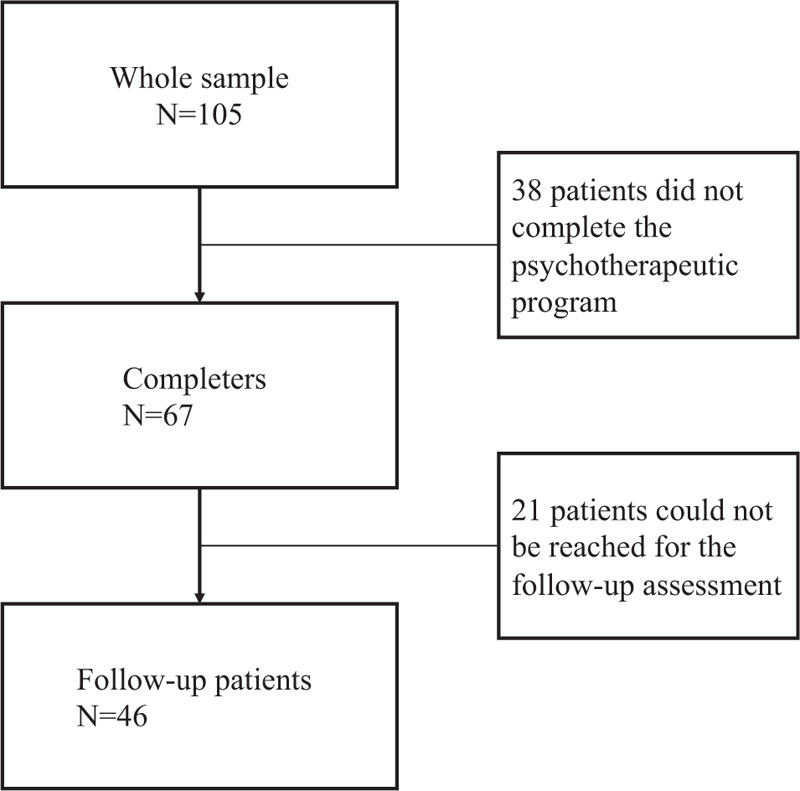
Participant flow chart.
Table 1.
Sample demographic and clinical data.
| Whole sample N = 105 | SD | Completers N = 67 | SD | Dropouts N = 38 | SD | Follow-up patients N = 46 | SD | |
| AGE | 31.2 | 8.4 | 31.33 | 8.53 | 31 | 8.14 | 32.11 | 8.79 |
| EDU | 11.8 | 2.5 | 12.03 | 2.5 | 11.25 | 2.33 | 12.17 | 2.6 |
| TREAT | 9.7 | 8 | 9.19 | 8.42 | 10.54 | 7.16 | 9.7 | 9.09 |
| HOSP | 1.9 | 2.2 | 1.41 | 1.89 | 2.79 | 2.38 | 1.52 | 2.11 |
| SUI | 2.2 | 4.7 | 1.2 | 2.91 | 4.22 | 6.65 | 0.93 | 1.8 |
| COM | 50 | 48 | 55 | 43 | ||||
| EC | 63 | 156 | 51.93 | 118.71 | 82.3 | 205.3 | 37.78 | 70.97 |
| EF | 35 | 32 | 34.01 | 31.54 | 37.65 | 33.71 | 34.29 | 29.89 |
| DES | 21.71 | 14.75 | 20.21 | 15.17 | 26.69 | 11.96 | 20.13 | 15.48 |
| HoNOS (E) | 17.8 | 4.21 | 16.7 | 3.66 | 19.78 | 4.42 | 16.35 | 4.05 |
AGE = mean age, COM = percentage of patients with comorbid mental disorders, DES = Dissociation Experience Scale (mean of total scores), EC = day dosage of antipsychotic medication in equivalents of chlorpromazine (mean in mg), EDU = level of education (mean in years), EF = day dosage of antidepressants in equivalents of fluoxetine (mean in mg), HoNOS(E) = version of HoNOS for external evaluators (mean of total scores), HOSP = number of previous hospitalizations (mean), SUI = number of suicide attempts (mean), TREAT = years of previous treatment (mean).
Results of the comparisons are shown in Figure 3 and Table 2. At the end of the treatment, there was a significant decrease in values compared to the baseline data (total score = 16.70, SD = 3.66 vs total score = 11.97, SD = 3.72, Cohen's d = 1.28) in the version for external evaluators (Z = 5.69, P < .001), but not in the self-rating version of HoNOS (Z = 1.67, P = .10). Here, the HoNOS score decreased only nonsignificantly (15.37, SD = 6.04 vs 13.91, SD = 6.74). The differences in HoNOS for external evaluators were significant in all items (overactive, aggressive, disruptive or agitated behavior: Z = 3.94, P < .001; nonaccidental self-injury: Z = 4.57, P < .001; cognitive problems: Z = 2.68, P = .01; problems of depressed mood: Z = 5.40, P < .001; other mental and behavioral problems: Z = 5.27, P < .001; problems with relationships: Z = 5.04, P < .001; problems with daily living activities: Z = 2.30, P = .02; problems with living conditions: Z = 2.08, P = .04). The exceptions were items of problem drinking or drug-taking: Z = 1.47, P = .14; physical illness or disability problems: Z = 0.31, P = .76; problems of hallucinations or delusions: Z = 0.41, P = .68; and problems with occupation and activities: Z = 0.71, P = .48. In the follow-up comparisons, both versions of HoNOS showed significant improvements (Z = 4.90, P < .001; respectively Z = 2.66, P = .008). The total score in HoNOS decreased in the version for external evaluators (16.35, SD = 4.05 vs 10.85, SD = 5.42, Cohen's d = 1.15), as well as in the version for self-evaluation (16.02, SD = 6.04 vs 13.17, SD = 0.56, Cohen's d = 0.66). In both versions of HoNOS, items of other mental and behavioral problems (anxiety, sleeping problems) (Z = 5.04, P < .001, respectively Z = 2.05, P = .04), and problems with relationships (Z = 4.87, P < .001, respectively Z = 3.45, P = .001) showed significant improvement. Moreover, in the version for external evaluators, items of overactive, aggressive, disruptive, or agitated behavior (Z = 3.29, P = .001); nonaccidental self-injury (Z = 3.39, P = .001); and problems of depressed mood (Z = 4.78, P < .001) were also significantly improved.
Figure 3.
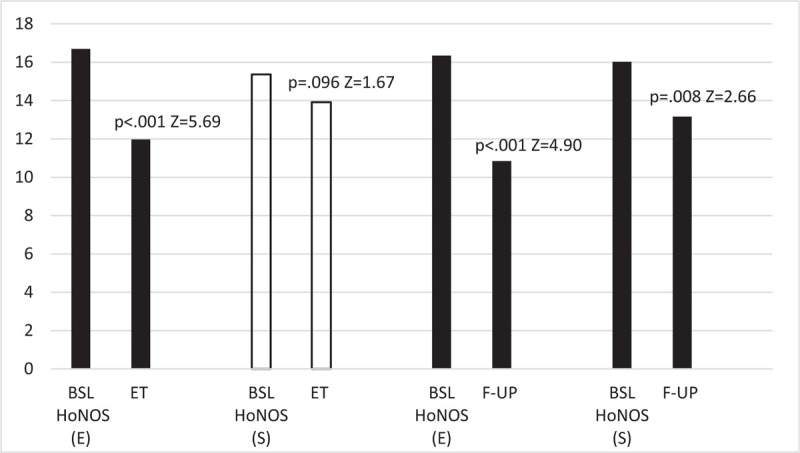
Symptoms and social functioning in borderline personality disorder patients: A comparison of Wilcoxon test Z values at baseline with values at the end of the treatment (N = 67) and at follow-up (N = 46) in the total score of HoNOS. Note: Columns with values of P < 0.05 are colored; BSL = total scores at baseline, ET = total scores at the end of the treatment, F-UP = follow-up total scores, HoNOS(E) = version of HoNOS for external evaluators, HoNOS(S) = self-rating version of HoNOS, Z = Wilcoxon test Z.
Table 2.
Symptoms and social functioning in BPD patients: A comparison of Wilcoxon test Z values at baseline with values at the end of the treatment (N = 67), and at follow-up (N = 46) in individual items of HoNOS.
| HoNOS (E) | HoNOS (S) | HoNOS (E) | HoNOS (S) | |||||
| N = 67 | N = 67 | N = 46 | N = 46 | |||||
| Wilcoxon test | Wilcoxon test | Wilcoxon test | Wilcoxon test | |||||
| Z | P-value | Z | P-value | Z | P-value | Z | P-value | |
| Total | 5.69 | <.001 | 1.67 | .01 | 4.9 | <.001 | 2.66 | .008 |
| BEH | 3.94 | <.001 | 1.15 | .25 | 3.29 | .001 | 1.95 | .05 |
| INJ | 4.57 | <.001 | 0.23 | .82 | 3.39 | .001 | 0.41 | .69 |
| DRI | 1.47 | .14 | 0.41 | .68 | 1.58 | .16 | 0.49 | .63 |
| COG | 2.68 | .01 | 1.9 | .06 | 1.59 | .11 | 1.74 | .08 |
| PHYS | 0.31 | .76 | 1.02 | .31 | 0.55 | .58 | 0.26 | .79 |
| HA-DE | 0.41 | .68 | 1 | .32 | 1.46 | .14 | 1.72 | .01 |
| DEP | 5.4 | <.001 | 1.35 | .18 | 4.78 | <.001 | 1.85 | .06 |
| OTH | 5.27 | <.001 | 0.11 | .91 | 5.04 | <.001 | 2.05 | .04 |
| REL | 5.04 | <.001 | 1.91 | .06 | 4.87 | <.001 | 3.45 | .001 |
| ACT | 2.3 | .02 | 1.89 | .06 | 1.7 | .09 | 1.8 | .07 |
| LIV | 2.08 | .04 | 0.96 | .34 | 0.43 | .67 | 0.28 | .78 |
| OCC | 0.71 | .48 | 0.93 | .10 | 0.64 | .53 | 0.88 | .38 |
Values at P < .05 are bold; ACT = problems with daily living activities, BEH = overactive, aggressive, disruptive, or agitated behavior, COG = cognitive problems, DEP = problems of depressed mood, DRI = problem-drinking or drug-taking, HA-DE = problems of hallucinations or delusions, HoNOS(E) = version of HoNOS for external evaluators, HoNOS(S) = self-rating version of HoNOS, INJ = non-accidental self-injury, LIV = problems with living conditions, OCC = problems with occupation and activities, OTH = other mental and behavioral problems, PHYS = physical illness or disability problems, REL = problems with relationships.
Table 3 shows the Spearman correlation coefficients, which indicate the relationship between the differences in HoNOS scores and baseline factors. A significant positive correlation was found in the baseline factor of experience of an intimate relationship (R = 0.43; P < .001). Correlations between the values of HoNOS at baseline (version for external evaluators) (R = 0.18; P = .57) and DES (R = 0.1; P = .65) were nonsignificant.
Table 3.
Spearman correlation coefficients of the differences in HoNOS scores and baseline factors (N = 46).
| R | Refined Fisher Z | P-value | |
| Experience of a relationship | 0.43 | 0.84 | <.001 |
| HoNOS(E) | 0.18 | 0.23 | .57 |
| DES | 0.1 | 0.09 | .65 |
Values at P < .05 are in bold; DES = Dissociative Experiences Scale (mean), HoNOS(E) = version of HoNOS for external evaluators at baseline, R = Spearman correlation coefficient.
Table 4 shows the statistical comparison between baseline values of patients who completed the program (completers) and patients who dropped out during the program (dropouts). The dropout patients differed significantly from those who completed the program with regard to a higher number of psychiatric hospitalizations (Z = -2.94, P < .01) and suicide attempts (Z = -3.12, P < .01), in higher pretreatment symptom severity measured by HoNOS for external evaluators (Z = -3.12, P < .01), and in higher values of symptoms of dissociation measured by DES (Z = -2.00, P < .05). Concerning the factors of DES, only the factor of depersonalization/derealization was significant (Z = -2.13, P < .05). The other 2 factors achieved only nonsignificant values, the factor of absorption (Z = 0.17, P = .17), and the factor of amnesia (Z = -0.65, P = .52).
Table 4.
Statistical comparison between patients who completed the program (completers) and those who dropped out (dropouts) using the Mann-Whitney test.
| Completers | Dropouts | |||
| N = 67 | N = 38 | Z | P | |
| Age | 31.33 | 31 | 0.18 | .85 |
| Number of psychiatric hospitalizations | 1.41 | 2.79 | -2.94 | .004 |
| Suicide attempts | 1.2 | 4.22 | -3.12 | .004 |
| Work or study activity | 0.57 | 0.33 | 2.25 | .05 |
| HoNOS (E) | 16.7 | 19.78 | -3.12 | .002 |
| DES | 20.21 | 26.69 | -2 | .046 |
Values at P < .05 are in bold; age, number of psychiatric hospitalizations, suicide attempts are indicated in mean value. Experience of work or study activity is shown in proportions of the sample. DES = Dissociative Experiences Scale (mean), HoNOS(E) = version of HoNOS for external evaluators (mean).
4. Discussion
In pursuit of the first hypothesis of this study, it was found that a day group psychodynamic treatment program for the duration of 9 months might improve symptoms and interpersonal functioning in patients of BPD completing the program. The changes are observable on both objective and subjective levels at the 1-year follow-up after the treatment. Improvements on both these levels show equivalent results in general psychiatric symptoms and interpersonal functioning. However, at the end of the treatment, improvement was noticeable only on the objective level. A reason why a response was missing on the subjective level might be that at the end of the treatment patients went through the arduous process of termination, in which they faced separation anxiety, fear of abandonment, and loss of the therapy which is crucial for relationships in BPD and may reinforce subjectively perceived difficulties, despite objective gains in the therapy.[40] Generally, this finding is in accordance with the overall efficacy of psychodynamic psychotherapy, which shows that maintaining therapeutic gains and continuation of improvement even after the end of treatment may be based on the target of fostering the inner resources and capacities of patients before symptom changes.[41] More specifically, this regularity was proven in recent research on a group of BPD patients. Gullestad et al[42] showed that, in a 36-month follow-up, outpatient psychodynamic psychotherapy was superior to an intensive psychodynamic day treatment program, but after 6 years this superiority was reversed in favor of an intensive psychodynamic program.[6]
Employing the cut-off scores of HoNOS, the results of this study represent a clinically meaningful change from very severe to severe mental illness. The effect sizes indicate moderate to larger effects, which were similar to the 36-month evaluation of psychodynamic group therapy for BPD in the study of Gullestad et al[42] (mean effect size 1.23), but lower than the 6-year follow-up of a day psychodynamic treatment program followed by individual or group psychotherapy in the study of Antonsen et al[6] (mean effect size 1.66).
With regard to the second hypothesis that baseline pretreatment symptoms’ severity, symptoms of dissociation, and experience of adult sustained object relations in a patient are associated with clinical improvement in the program, results of the study confirmed only 1 significant predictor – experience of an intimate relationship – with a positive correlation to treatment outcome.
Previous studies did not identify marital status as a significant predictor of the outcome in BPD.[8] However, this study used a broader definition of the demographic variable as the experience of an intimate relationship, that is, past or present experience of marriage or living as a couple. This positive correlation with the outcome at this point might reflect the importance of adult experiences and relationships in the formation of personality.[43] These experiences could also be productively used in therapy. Specifically, disturbance in intimate relationships seems to be related to dysfunctional attachment patterns in BPD patients and these relationships may be influenced by the severity of BPD symptoms.[44] Moreover, inability to form stable intimate relationships may in part result from lower mentalizing abilities and impaired cognitive or affective empathy in this clinical group.[45] At least a certain level of these functions is a prerequisite for successful psychodynamic psychotherapy.
In this study, pretreatment symptom severity was not confirmed as a predictor of outcome of the therapy. Results of the studies researching this predictor showed heterogeneous results, with no difference between psychodynamic and cognitive-behavioral approaches.[8] Findings of newer studies of psychodynamic approaches in BPD concerning pretreatment symptom severity are still ambiguous.[46,47] Theoretically, more severe psychiatric symptoms can elevate hyperarousal in patients and, conversely, reduce inhibitory control which may induce immature ways of mentalization, thus hampering working-through in psychotherapy.[11] However, the different impact of symptom intensity on therapy outcome may be related to the formation of patient trust in a particular psychotherapeutic program and its therapist. In the absence of trust, the capacity for change in the patients may be reduced, hand in hand with the reduced capacity for learning from experience from the therapeutic process.[48]
Dissociation was not shown to be a negative predictor of outcome, as was previously found in DBT therapy.[10] The reason for this finding might be that psychodynamic psychotherapy could positively influence dissociation with its emphasis on integration of the whole mental content.[49] Corresponding to this, association techniques that are connected with a psychodynamic approach and which help to build narratives of recent interpersonal relations and to verbalize emotions, have been found to be significantly correlated with improvements in dissociative symptoms.[50]
The dropout rate in the present study was 36% (38/105), which is slightly higher than the average (25%) reported in day treatment programs for personality disorders[21] or in psychotherapies for BPD patients with a duration of less than 12 months.[22] However, a variance of completion rates in the aforementioned meta-analysis covered an entire range between 50% and 100%.
Regarding the third hypothesis of this study, comparison of the dropout sample and regular participants revealed significant differences in a more severe course of the disorder among dropout patients such as a higher number of psychiatric hospitalizations, and more severe pretreatment general psychiatric symptoms as well as symptoms of dissociation. On the contrary, the number of previous suicide attempts was significantly higher in the dropout sample than we expected. According to our assumptions, despite work or study activities being higher in the completers’ group, this difference was not significant. It was also not possible to prove a difference in the age of the participants between the 2 groups.
Concerning the higher number of psychiatric hospitalizations, it can be hypothesized that a more pronounced history of psychiatric treatment bears a stronger stigma and labeling, and that those patients do not wish to be subjected to psychiatric or psychotherapeutic care for a long time.[51,52] A higher number of hospitalizations as a predictor of dropout from day treatment with mixed personality disorders was also found in a previous study by Ogrodniczuk et al.[21] This suggested the possibility that patients who were accustomed to using hospitalization as an escape from the demands of daily living, feel more stressed under the conditions of a day treatment program and tend to terminate it prematurely.
Previous studies showed contradictory results regarding suicidal history as a dropout predictor in BPD. In inpatient DBT, it was shown both as a negative predictor[51] and as a positive predictor.[53] It was also found as a positive predictor in general psychiatric practice.[54] Argument for this difference between these findings and those of other studies might be that different therapeutic interventions more or less specifically target suicidal behavior of patients. Hence, patients involved in less specifically targeted programs may feel that the program is not tailored to them and drop out early.[54] This explanation may be reflected in the higher suicide rates in the dropout group in our study, because the psychodynamic day program is not specifically targeted in this regard.
Concerning the symptoms of dissociation, to the best of our knowledge, this variable has not been studied as a dropout factor in BPD treatment. Significant difference in the factor for depersonalization/derealization of DES might indicate problems in the formation of a therapeutic relationship in dropout patients.
Some research findings from other studies indicate that there might be a common cluster of BPD patients with more frequent hospitalizations, suicide attempts, more severe psychiatric symptoms, and even symptoms of dissociation. A subpopulation of BPD patients with frequent suicide attempts suffers from more severe psychopathology,[55] and especially from more severe depressive symptoms and a feeling of hopelessness.[56] BPD patients with higher levels of dissociation are at high risk of self-injury, suicide attempts, and more frequent hospitalization. They need complex treatment with a stabilization phase that precedes the actual therapy.[57] In this context, it is also important to mention that dissociation in BPD has frequently been reported in relation to childhood trauma and correlates with several kinds of caregivers’ malfunction and with childhood abuse.[14] Interestingly, significant associations between childhood maltreatment, depressive symptoms, and higher suicidal risk have been found in psychiatric patients predominantly with bipolar disorder and major depression.[58] Thus it could also be assumed that exposure to abuse and neglect as a child may also increase the risk to develop suicidality in BPD patients. Another area that could be investigated for relationships similar to major affective disorder are extreme sensory processing patterns in the form of hypersensitivity or hyposensitivity, which are related to impulsivity, alexithymia, depression, and hopelessness in this group of disorders.[59] Involvement of sensory perception is also strongly implicated in the emotional processes of BPD patients. Hyposensitivity or hypersensitivity may be “trait” markers of BPD individuals with depression. Interventions should refer to the individual unique sensory profiles and their behavioral and functional impact in the real-life context.
Although work or study activities were only insignificantly lower in the dropout group, it can be assumed that this difference may also be related to procrastination in those who do not complete the program. Recently, a significant association has been found between procrastination and lower self-efficacy, negative perfectionism, and narcissism in a nonclinical sample.[60]
Age of participants, unlike in several other studies[61–63] was not found to differ between the groups. A possible explanation for lower age in the dropout groups is that patients only become conscious of long-standing and severe interpersonal problems with age, and therefore become more motivated to stay in the therapy.[63] This apparently did not play much of a role in the sample of this study, with an average age of 31.2 years.
Using the design of a cohort group is a limitation of the present study which, unlike a randomized control trial, cannot prove cause and effect. There was also no control for factors other than specific psychotherapy which could influence the outcome, for example, common factors of the therapy and/or therapeutic aspects of the treatment milieu. In addition, it was also not verified whether the nonpsychodynamic elements of the treatment (occupational therapy, practical training, social skills training) influenced the outcome. This study is also limited by the fact that not all patients who completed the treatment could be reached for follow-up assessment. The most common reason was a change of contact information, mostly due to the relocation of patients. Relocation might have been associated with greater symptom severity which was one significant predictor of dropout found in our study, in which BPD patients often relate to instability of relationships, including the place of residence.
Further research is needed to address the dissociation symptoms as a dropout predictor in the therapy of BPD patients. As the findings of relationship experience and symptoms of dissociation in this study show, in addition to sociodemographic variables, variables related to psychological functioning and life experience should be included in research as possible predictors of outcome or dropout.
5. Conclusions
A day psychodynamic treatment program of the duration of 9 months might be influential in improving symptoms and interpersonal functioning in patients with BPD completing the program. However, given the demands on the education of therapists, the duration of therapy, and the economic costs, it is necessary to know which group of patients with BPD will benefit best from this program. Knowledge of the predictors of treatment outcome and dropout may well help, in particular since psychotherapeutic treatment in patients with BPD is accompanied by relatively high dropouts. This study provides insights into these predictors. Previous experience of intimate relationships has been shown to be a predictor of improvement in therapy, but it has not been confirmed that the severity of psychiatric symptoms or symptoms of dissociation can be this kind of predictor. The dropout from the program was related to factors such as a higher number of previous psychiatric hospitalizations, more suicide attempts in the past, more severe pretreatment symptoms, and symptoms of dissociation. On the contrary, the dropout did not appear to be associated with the age of the patients and the higher presence of study or work activities. Taken together, the results of this study show that a psychodynamic day program is more feasible for patients with lower levels of clinical disturbance (less frequently hospitalized, milder psychiatric and dissociation symptoms, and fewer suicide attempts) with regard to the possibility of dropout. At the same time, this program is more suitable for patients with a positive history of intimate relationships, given the better outcome of treatment. This finding is also in concordance with previous studies.[11,12] The results of this study mainly have a practical impact for clinicians to better understand which patients with BPD to enroll in a psychodynamic day program. However, the findings of this study are also limited by this type of observational study, not taking into account all the factors that may affect the outcome of treatment, and the lower participation of patients in the follow-up assessment. There is a need to focus further studies on this area and also to involve more candidate predictors in the assessment, mainly from the field of psychosocial factors and interpersonal relationships.
Author contributions
Conceptualization: Ondrej Pec.
Data curation: Jan Pec.
Formal analysis: Petr Bob.
Methodology: Petr Bob.
Supervision: Irena Ludvikova.
Writing – original draft: Ondrej Pec.
Writing – review & editing: Ondrej Pec, Petr Bob, Irena Ludvikova.
Footnotes
Abbreviations: BPD = borderline personality disorder, DBT = dialectical behavior therapy, DES = Dissociative Experiences Scale, DSM = Diagnostic and Statistical Manual of Mental Disorders, HoNOS = Health of the Nation Outcome Scales, MBT = mentalization based treatment.
How to cite this article: Pec O, Bob P, Pec J, Ludvikova I. Psychodynamic day treatment program for borderline personality disorder: factors that predict outcome and dropout: an observational study. Medicine. 2021;100:11(e25186).
The authors report no conflicts of interest.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Gunderson JG. Clinical practice. Borderline personality disorder. N Engl J Med 2011;364:2037–42. [DOI] [PubMed] [Google Scholar]
- [2].Stoffers JM, Völlm BA, Rücker G, et al. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst Rev 2012;2012:CD005652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Kallert TW, Glöckner M, Priebe S, et al. A comparison of psychiatric day hospitals in five European countries. Implications of their diversity for day hospital research. Soc Psychiatry Psychiatr Epidemiol 2004;39:777–88. [DOI] [PubMed] [Google Scholar]
- [4].Bateman A, Fonagy P. Effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. Am J Psychiatry 1999;156:1563–9. [DOI] [PubMed] [Google Scholar]
- [5].Bateman A, Fonagy P. Treatment of borderline personality disorder with psychoanalytically oriented partial hospitalization: an 18-month follow-up. Am J Psychiatry 2001;158:36–42. [DOI] [PubMed] [Google Scholar]
- [6].Antonsen BT, Kvarstein EH, Urnes Ø, et al. Favorable outcome of long-term combined psychotherapy for patients with borderline personality disorder: six-year follow-up of a randomized study. Psychother Res 2017;27:51–63. [DOI] [PubMed] [Google Scholar]
- [7].Arnevik E, Wilberg T, Urnes Ø, et al. Psychotherapy for personality disorders: Short-term day hospital psychotherapy versus outpatient individual therapy - a randomized controlled study. Eur Psychiatry 2009;24:71–8. [DOI] [PubMed] [Google Scholar]
- [8].Barnicot K, Katsakou C, Bhatti N, et al. Factors predicting the outcome of psychotherapy for borderline personality disorder: a systematic review. Clin Psychol Rev 2012;32:400–12. [DOI] [PubMed] [Google Scholar]
- [9].Bohus M, Haaf B, Simms T, et al. Effectiveness of inpatient dialectical behavioral therapy for borderline personality disorder: a controlled trial. Behav Res Ther 2004;42:487–99. [DOI] [PubMed] [Google Scholar]
- [10].Kleindienst N, Limberger MF, Ebner-Priemer UW, et al. Dissociation predicts poor response to dialectal behavioral therapy in female patients with borderline personality disorder. J Pers Disord 2011;25:432–47. [DOI] [PubMed] [Google Scholar]
- [11].Bateman A, Fonagy P. Impact of clinical severity on outcomes of mentalisation-based treatment for borderline personality disorder. Br J Psychiatry 2013;203:221–7. [DOI] [PubMed] [Google Scholar]
- [12].Kvarstein EH, Pedersen G, Folmo E, et al. Mentalization-based treatment or psychodynamic treatment programmes for patients with borderline personality disorder - the impact of clinical severity. Psychol Psychother 2019;92:91–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sahin Z, Vinnars B, Gorman BS, et al. Clinical severity as a moderator of outcome in psychodynamic and dialectical behavior therapies for borderline personality disorder. Personal Disord 2018;9:437–46. [DOI] [PubMed] [Google Scholar]
- [14].Korzekwa MI, Dell PF, Links PS, et al. Dissociation in borderline personality disorder: a detailed look. J Trauma Dissociation 2009;10:346–67. [DOI] [PubMed] [Google Scholar]
- [15].Zanarini MC, Frankenburg FR, Jager-Hyman S, et al. The course of dissociation for patients with borderline personality disorder and Axis II comparison subjects: a 10-year follow up. Acta Psychiatr Scand 2008;118:291–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Zanarini MC, Jager-Hyman S. Dell PF, O’Neil JA. Dissociation in borderline personality disorder. Dissociation and the Dissociative Disorders. DSM-V and Beyond. New York, NY: Routledge; 2009. 487–93. [Google Scholar]
- [17].Spitzer C, Barnow S, Freyberger HJ, et al. Dissociation predicts symptom-related treatment outcome in short-term inpatient psychotherapy. Aust N Z J Psychiatry 2007;41:682–7. [DOI] [PubMed] [Google Scholar]
- [18].Lagerlöf S, Sigrell B. A Discussion of models for the selection of patients for supervised psychoanalysis. J Clin Psychoanal 1999;8:149–72. [Google Scholar]
- [19].Kernberg OF. Identity: recent findings and clinical implications. Psychoanal Q 2006;75:969–1003. [DOI] [PubMed] [Google Scholar]
- [20].Karterud S, Pedersen G, Bjordal E, et al. Day treatment of patients with personality disorders: experiences from a Norwegian treatment research network. J Pers Disord 2003;17:243–62. [DOI] [PubMed] [Google Scholar]
- [21].Ogrodniczuk JS, Joyce AS, Lynd LD, et al. Predictors of premature termination of day treatment for personality disorder. Psychother Psychosom 2008;77:365–71. [DOI] [PubMed] [Google Scholar]
- [22].Barnicot K, Katsakou C, Marougka S, et al. Treatment completion in psychotherapy for borderline personality disorder - a systematic review and meta-analysis. Acta Psychiatr Scand 2011;123:327–38. [DOI] [PubMed] [Google Scholar]
- [23].American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed (Text Revised). New York: American Psychiatric Association; 2001 [Google Scholar]
- [24].First MB, Gibbon M, Spitzer RL, et al. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). Washington, DC: American Psychiatric Press, Inc; 1997. [Google Scholar]
- [25].World Health Organization. International Statistical Classification of Diseases and Related Health Problems (10th revision, edition 2010). Geneva: World Health Organization; 2010 [Google Scholar]
- [26].Raven JC. Guide to the Standard Progressive Matrices. London, UK: HK Lewis; 1960. [Google Scholar]
- [27].Atkins M, Burgess A, Bottomley C, et al. Chlorpromazine equivalents: a consensus of opinion for both clinical and research applications. Psychiatric Bulletin 1997;21:224–6. [Google Scholar]
- [28].Hayasaka Y, Purgato M, Magni LR, et al. Dose equivalents of antidepressants: Evidence-based recommendations from randomized controlled trials. J Affect Disord 2015;180:179–84. [DOI] [PubMed] [Google Scholar]
- [29].Woods SW. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J Clin Psychiatry 2003;64:663–7. [DOI] [PubMed] [Google Scholar]
- [30].Behr H, Hearst L. Behr H, Hearst L. The symptom in its group context. Group-analytic Psychotherapy. A Meeting of Minds. London, UK: Whurr; 2005. 66–80. [Google Scholar]
- [31].Lappalainen PH. Conflicts as triggers of personal growth: post-traumatic growth in the organizational setup. SciMed 2019;1: doi: 10.28991/SciMedJ-2019-0103-2 [Google Scholar]
- [32].Mohd-Nor N, Bit-Lian Y, Knowledge. Attitude and practices of standard precaution among nurses in Middle-East Hospital. SciMed 2019;1: doi: 10.28991/SciMedJ-2019-0104-4 [Google Scholar]
- [33].Wing JK, Curtis RH, Beevor AS. HoNOS: Health of the Nation Outcome Scales: Report on Research and Development July 1993-December 1995. London, UK: Royal College of Psychiatrists; 1996. [Google Scholar]
- [34].Barbato A, Agnetti G, D’Avanzo B, et al. Outcome of community-based rehabilitation program for people with mental illness who are considered difficult to treat. J Rehabil Res Dev 2007;44:775–84. [DOI] [PubMed] [Google Scholar]
- [35].Pec O, Cechova D, Pecova J, et al. HoNOS (Health of the Nations Outcome Scales) - an adaptation of the tool for the assessment of symptoms and social functions in serious mentally ill in the Czech conditions and its use. [HoNOS (Hodnocení zdravotního stavu) - adaptace nástroje na hodnocení symptom a sociálních funkcí u závažně duševně nemocných v českých podmínkách a jeho použití]. Ceska Slov Psychiatr 2009;105:245–9. [Google Scholar]
- [36].Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis 1986;174:727–35. [DOI] [PubMed] [Google Scholar]
- [37].Waller NG, Putnam FW, Carlson EB. Types of dissociation and dissociative types: a taxometric analysis of dissociative experiences. Psychol Methods 1996;1:300–21. [Google Scholar]
- [38].Bob P. Dissociation processes and their measurement. [Disociativni procesy a jejich mereni] Ceska Slov Psychiatr 2000;96:301–9. [Google Scholar]
- [39].Ptacek R, Bob P, Paclt I. Dissociative experiences scale - Czech version. [Skala disociativnich zkuseností - ceska verze ] Cesk Psychol 2006;50:262–72. [Google Scholar]
- [40].Goldstein WN. Dynamically oriented psychotherapy with borderline patients. Am J Psychother 1997;51:14–30. [DOI] [PubMed] [Google Scholar]
- [41].Shedler J. The efficacy of psychodynamic psychotherapy. Am Psychol 2010;65:98–109. [DOI] [PubMed] [Google Scholar]
- [42].Gullestad FS, Wilberg T, Klungsøyr O, et al. Is treatment in a day hospital step-down program superior to outpatient individual psychotherapy for patients with personality disorders? 36 months follow-up of a randomized clinical trial comparing different treatment modalities. Psychother Res 2012;22:426–41. [DOI] [PubMed] [Google Scholar]
- [43].Colarusso CA, Nemiroff RA. Some observations and hypotheses about the psychoanalytic theory of adult development. Int J Psychoanal 1979;60:59–71. [PubMed] [Google Scholar]
- [44].Hill J, Stepp SD, Wan MW, et al. Attachment, borderline personality, and romantic relationship dysfunction. J Pers Disord 2011;25:789–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Jeung H, Herpertz SC. Impairments of interpersonal functioning: empathy and intimacy in borderline personality disorder. Psychopathology 2014;47:220–34. [DOI] [PubMed] [Google Scholar]
- [46].Wrege JS, Busmann M, Meyer AH, et al. Impulsiveness in borderline personality disorder predicts the long-term outcome of a psychodynamic treatment programme. Clin Psychol Psychother 2020. 1–9. doi: 10.1002/cpp.2526. [DOI] [PubMed] [Google Scholar]
- [47].Euler S, Nolte T, Constantinou M, et al. Interpersonal problems in borderline personality disorder: associations with mentalizing, emotion regulation, and impulsiveness. J Pers Disord 2019. 1–7. doi: 10.1521/pedi_2019_33_427. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- [48].Fonagy P, Luyten P, Allison E. Epistemic petrification and the restoration of epistemic trust: a new conceptualization of borderline personality disorder and its psychosocial treatment. J Pers Disord 2015;29:575–609. [DOI] [PubMed] [Google Scholar]
- [49].Wehle D. Plunge into the abyss: creativity and trauma psychodynamic group. Group 2016;40:197–221. [Google Scholar]
- [50].Goldman GA, Gregory RJ. Relationships between techniques and outcomes for borderline personality disorder. Am J Psychother 2010;64:359–71. [DOI] [PubMed] [Google Scholar]
- [51].Rüsch N, Schiel S, Corrigan PW, et al. Predictors of dropout from inpatient dialectical behavior therapy among women with borderline personality disorder. J Behav Ther Exp Psychiatry 2008;39:497–503. [DOI] [PubMed] [Google Scholar]
- [52].Aubeeluck ND, Luximon-Ramma A. The burdens of family caregivers of schizophrenia in mauritius. SciMed 2020;2: doi: 10.28991/SciMedJ-2020-0203-2. [Google Scholar]
- [53].Krüger C, Röepke S, Kliem S. Reasons for premature termination of dialectical behavior therapy for inpatients with borderline personality disorder. Behav Res Ther 2014;60:46–52. [DOI] [PubMed] [Google Scholar]
- [54].DePanfilis C, Marchesi C, Cabrino C, et al. Patient factors predicting early dropout from psychiatric outpatient care for borderline personality disorder. Psychiatry Res 2012;200:422–9. [DOI] [PubMed] [Google Scholar]
- [55].Marcinko D, Bilić V, Pivac N, et al. Serum cholesterol concentration and structured individual psychoanalytic psychotherapy in suicidal and non-suicidal male patients suffering from borderline personality disorder. Coll Antropol 2011;35: Suppl 1: 219–23. [PubMed] [Google Scholar]
- [56].Pérez S, Marco JH, García-Alandete J. Comparison of clinical and demographic characteristics among borderline personality disorder patients with and without suicidal attempts and non-suicidal self-injury behaviors. Psychiatry Res 2014;220:935–40. [DOI] [PubMed] [Google Scholar]
- [57].Korzekwa MI, Dell PF, Pain C. Dissociation and borderline personality disorder: an update for clinicians. Curr Psychiatry Rep 2009;11:82–8. [DOI] [PubMed] [Google Scholar]
- [58].Pompili M, Innamorati M, Lamis DA, et al. The associations among childhood maltreatment, “male depression” and suicide risk in psychiatric patients. Psychiatry Res 2014;220:571–8. [DOI] [PubMed] [Google Scholar]
- [59].Serafini G, Gonda X, Canepa G, et al. Extreme sensory processing patterns show a complex association with depression, and impulsivity, alexithymia, and hopelessness. J Affect Disord 2017;210:249–57. [DOI] [PubMed] [Google Scholar]
- [60].Jahani HJG, Ehsanikenari A, Sharif AS. Role of self-efficacy and negative perfectionism in the prediction of procrastination of narcissistic personality: a study on non-clinical subjects. Emerg Sci J 2018;2:388–99. [Google Scholar]
- [61].Crawford MJ, Price K, Gordon F, et al. Engagement and retention in specialist services for people with personality disorder. Acta Psychiatr Scand 2009;119:304–11. [DOI] [PubMed] [Google Scholar]
- [62].Smith TE, Koenigsberg HW, Yeomans FE, et al. Predictors of dropout in psychodynamic psychotherapy of borderline personality disorder. J Psychother Pract Res 1995;4:205–13. [PMC free article] [PubMed] [Google Scholar]
- [63].Thormählen B, Weinryb RM, Norén K, et al. Patient factors predicting dropout from supportive-expressive psychotherapy for patients with personality disorders. Psychother Res 2003;13:493–509. [DOI] [PubMed] [Google Scholar]


