Abstract
Nursing educators should equip nursing students with sufficient knowledge about coronavirus disease 2019 (COVID-19), perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, self-efficacy, and behavioral intention in order to prevent the spread of COVID-19.
The purpose of this study was to use the health belief model to elucidate nursing students’ relationships between knowledge about COVID-19, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, self-efficacy, and behavioral intention.
A cross-sectional survey design was adopted and purposive sampling was utilized. A total of 361 nursing students participated in the study. Quantitative analysis was employed for all data analysis.
The findings showed that the nursing students had the following mean scores on knowledge of COVID-19 9.43 [standard deviation (SD)1.19], perceived susceptibility 19.41 (SD2.68), perceived severity 20.31 (SD 4.09), perceived benefits 26.52 (SD 4.08), perceived barriers 15.17 (SD5.88), cues to action 3.30 (SD1.70), self-efficacy 17.68 (SD2.83), and behavioral intention 18.46 (SD2.33). Nursing students’ demographic background, knowledge of COVID-19, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy explained 58.1% of the variance in behavioral intention (R2 = 0.581, F = 29.775, P < .001).
Nursing educators can increase nursing students’ knowledge of COVID-19, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy as effective means of health promotion to improve their behavioral intention to prevent the spread of COVID-19.
Keywords: behavioral intention, COVID-19, health beliefs model, nursing students, self-efficacy
1. Introduction
Since the occurrence of the coronavirus disease (COVID-19) in Wuhan, Hubei Province, China on December 1, 2019, many of millions of people globally have experienced deleterious effects. COVID-19 has a very high risk of human-to-human transmission,[1,2] is widely diagnosed (14,012,449 people worldwide; 454 people in Taiwan), can be both severe and fatal (mortality 596,158 people worldwide 4.25%; 7 people in Taiwan),[3] and causes serious physical, psychological, emotional, and social trauma.[4–6] Relevant knowledge about COVID-19,[7] and related health beliefs, self-efficacy, and preventive behaviors, is critically important to decrease the rate of infection, reduce the mortality rate, and maintain peoples’ health and quality of life.[8–10]
COVID-19 is an atypical coronavirus, with an incubation period of 1 to 14 day or a delay of several weeks to several months. It constitutes a human-to-human droplet and contact infection.[11–14] It is also possible to develop COVID-19 with symptoms or asymptomatically.[15,16] Symptoms may include chest tightness, headache, difficulty breathing, fever >38°C, sneezing, runny nose, stuffy nose, cough, nausea, abdominal pain, diarrhea, muscle ache, fatigue, and general weakness, among others.[17–21] Furthermore, people commonly experience major associated physical, psychological, emotional, and social issues, including insomnia, stress, anxiety, depression, social support and coping problems, well-being issues, and burnout in daily life.[22,23] In addition to the need for people to be cognizant of these symptoms and related impacts of COVID-19, it is also urgent that people understand the demonstrated effectiveness of certain personal self-preventive measures, such as frequently washing one's hands, measuring one's body temperature, wearing a mask,[24] avoiding entering and exiting crowded locations, opening doors and windows to circulate air, using hand sanitizer with 60% to75% alcohol content, and wiping commonly used surfaces with bleach.[17–19]
The structure of the health belief model regarding implementing and sustaining healthy behaviors includes the following: perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and cues to action. Personal behaviors and health beliefs are adopted by individuals in daily life. In order to maintain and promote peoples’ health, healthy behaviors are significant, and produce important impacts on peoples’ health beliefs to practice healthy behaviors and maintain a healthy life. People's health and diseases are related to health beliefs in terms of perceived susceptibility, severity, benefits, and barriers of the diseases, and are manifested in preventive behaviors and behavioral intention.[25–27]
Self-efficacy, in our context, refers to personal effectiveness in using personal health beliefs and behaviors to achieve health goals in daily life. People high in self-efficacy generally hold the belief that, through their own effects, they can achieve desired health results in an effective manner. One of the reasons why the dimension of self-efficacy is so critical in the consistent performance of healthy behaviors is that individuals’ typically face operational barriers when they attempt to perform those healthy behaviors. As a consequence, they need both self-confidence and will-power, that is, self-efficacy to persist through those barriers, reinforce their health beliefs, and implement practical actions to reach their health goals.[25]
Based on the growing global impact of COVID-19, the health belief model is utilized to understand the health beliefs, self-efficacy, and preventive behaviors of nursing students with respect to COVID-19. Indeed, it is hoped that the model can be employed to assess whether nursing students are actually implementing and promoting personal health beliefs, self-efficacy, and preventive behaviors in their patients’ daily lives.[26–30] It is the responsibility of nursing educators to equip nursing students with thorough knowledge about COVID-19, and accurate health beliefs about the perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, self-efficacy, and behavioral intention[26–30] in order to prevent the spread of this infectious disease both locally and globally.
2. Purpose
The purpose of this study was to use the health belief model to explore nursing students’ relationships between knowledge about COVID-19, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, self-efficacy, and behavioral intention.
3. Methods
3.1. Design
A cross-sectional survey design was adopted in this study.
3.2. Framework
The framework of this study was constructed to survey the demographic background of nursing students in terms of school system, gender, age, religious beliefs, health status, diet, movement, and reading of COVID-19 information, in relation to COVID-19 knowledge, as well as the relationships between the health beliefs model on perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, self-efficacy, and behavioral intention (Fig. 1).
Figure 1.
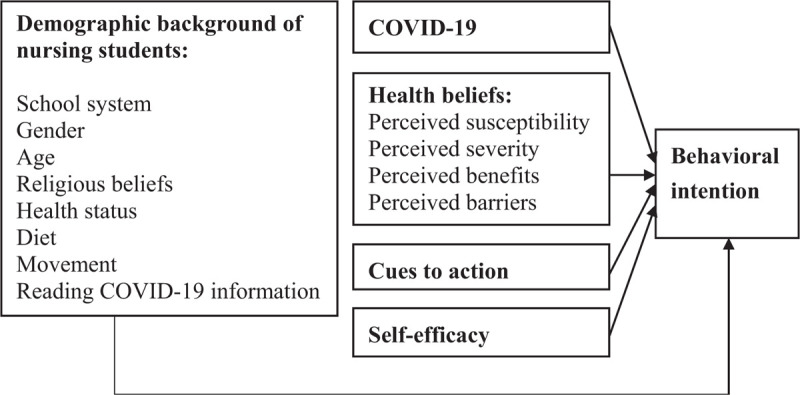
Indicated the demographic background of nursing students, COVID-19, health beliefs, cues to action, and self-efficacy to predict behavioral intention.
3.3. Participants
According to Krejcie and Morgan, the samples of the study were required 346 nursing students.[31] The study was no criteria in inclusion and exclusion. A total of 361 nursing students participated in the survey study. Purposive sampling was used in the study. The 361 nursing students comprised, at the university level: 200 in a 5-year program; 45 in a 4-year program; and 116 in a 2-year program.
3.4. Ethical considerations
This survey study of nursing students was authorized by the Institutional Review Board / Ethics Committee of Mennonite Christian Hospital (IRB No. 20–04-008) in Taiwan, ROC. All nursing students participated voluntarily in answering the questionnaires about demographic background, cues to action, COVID-19 knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and behavioral intention.
3.5. Instruments
The instrument of this study was self-designed and used a health belief model[25,26,27] constructed by the authors. The questionnaire included nursing students’ demographic background in terms of school system, gender, age, religious beliefs, health status, diet, movement, reading COVID-19 information, cues to action (television, broadcast, news, network, health care workers, poster promotion, school promotion, promotional car, and others). The questionnaire comprised 42-items, containing: knowledge about COVID-19 (items 1–11), and relationships between the health beliefs model on perceived susceptibility (items 12–16), perceived severity (items 17–22), perceived benefits (items 23–28), perceived barriers (items 29–34), self-efficacy (items 35–38), and behavioral intention (items 39–42). Items 1 to 11 on the questionnaire were answered by “true” and “false” responses, while a 5-point Likert-type scale was used for items 12 to 42. The content validity index of the questionnaire on the 7-part measure, including COVID-19 knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and behavioral intention was 0.85 to 0.92 as established by 5 experts. The reliabilities of the preliminary test on the 7-part measure (n = 83) were as follows: COVID-19 knowledge had a Kuder–Richardson reliability−20 of 0.38; perceived susceptibility had a Cronbach α of 0.71; perceived severity had a Cronbach α of 0.84; perceived benefits had a Cronbach α of 0.94; perceived barriers had a Cronbach α of 0.92; self-efficacy had a Cronbach α of 0.96; and behavioral intention had a Cronbach α of 0.96. The reliabilities of the 7-part measure (n = 361) were as follows: COVID-19 knowledge had a Kuder–Richardson reliability−20 of 0.46; perceived susceptibility had a Cronbach α of 0.61; perceived severity had a Cronbach α of 0.84; perceived benefits had a Cronbach α of 0.96; perceived barriers had a Cronbach α of 0.91; self-efficacy had a Cronbach α of 0.96; and behavioral intention had a Cronbach α of 0.96.
3.6. Data collection
The researcher administered a questionnaire to 400 nursing students, and explained that the questionnaire was used to survey nursing students’ demographic background, cues to action, and relationships between COVID-19 knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and behavioral intention in a university. Each of the 400 nursing students could decide to fill out the survey questionnaires completely or incompletely. Nursing students self-responded to the 42-item questions regarding COVID-19 knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and behavioral intention. 361 (90.25%) of the questionnaires were completely finished by nursing students and 39 (9.75%) of the questionnaires were either incomplete or unreturned. The researcher collected a total of 361 questionnaires from May 25 to May 29, 2020.
3.7. Data analysis
Quantitative analysis was employed for all data analysis. The Statistical Package for the Social Sciences 23.0 statistical package was used to analyze all data in the research. The data analysis of the study included percentages, frequencies, means, standard deviations (SDs), single sample t test, Spearman rho correlation, and multiple hierarchical regression analysis.
4. Results
4.1. Demographic background
Nursing students included 200 (55.40%) in a 5-year program, 45 (12.50%) in a 4-year program, and 116 (32.10%) in a 2-year program (Table 1). Concerning gender distribution, 39 (10.80%) were males and 322 (89.20%) were females (Table 1). In terms of age distribution, the nursing students included 216 (59.80%) 20-years-old and 145 (40.20%) who were above 20-years-old (Table 1). Regarding religious beliefs, there were 178 (49.30%) nursing students with no religious beliefs and 183 (50.70%) with religious beliefs (Table 1). Concerning health status, 193 (53.50%) nursing students had an ordinary health status and 168 (46.50%) had a very good health status (Table 1). In terms of diet, 117 (32.40%) nursing students ate a normal diet without in 3 meals and 244 (67.60%) ate a normal diet in 3 meals (Table 1). Regarding movement, 259 (71.70%) nursing students had no regular movement, and 102 (28.30%) had regular movement (Table 1). Concerning reading COVID-19 information, 55 (15.20%) of the nursing students had done no reading and 306 (84.80%) had done some reading (Table 1).
Table 1.
Demographic background of nursing students.
| N = 361 | Items | Frequency | Percentage |
| School system | 1. 5-year program | 200 | 55.40% |
| 2. 4-year program | 45 | 12.50% | |
| 3. 2-year program | 116 | 32.10% | |
| Gender | 1. Male | 39 | 10.80% |
| 2. Female | 322 | 89.20% | |
| Age | 1. 20-years-old | 216 | 59.80% |
| 2. Above 20-years-old | 145 | 40.20% | |
| Religious beliefs | 1. No religious beliefs | 178 | 49.30% |
| 2. Religious beliefs | 183 | 50.70% | |
| Health status | 1. Ordinary health status | 193 | 53.50% |
| 2. Very good health status | 168 | 46.50% | |
| Diet | 1. Normal diet without 3 meals | 117 | 32.40% |
| 2. Normal diet in 3 meals | 244 | 67.60% | |
| Movement | 1. No regular movement | 259 | 71.70% |
| 2. Regular movement | 102 | 28.30% | |
| Reading COVID-19 information | 1. No reading | 55 | 15.20% |
| 2. Reading | 306 | 84.80% |
4.2. Cues to action for nursing students
In the study, nursing students’ cues to action included 353 (97.80%) from television, 56 (15.50%) broadcast, 82 (22.70%) news, 227 (62.90%) network, 142 (39.30%) health care workers, 105 (29.10%) poster promotion, 199 (55.10%) school promotion, 24 (6.60%) promotional car, and 3 (0.80%) others (Table 2).
Table 2.
Cues to action for nursing students.
| N = 361 | Items | Frequency | Percentage |
| Cues to action | 1. Television | 353 | 97.80% |
| 2. Broadcast | 56 | 15.50% | |
| 3. News | 82 | 22.70% | |
| 4. Network | 227 | 62.90% | |
| 5. Health care workers | 142 | 39.30% | |
| 6. Poster promotion | 105 | 29.10% | |
| 7. School promotion | 199 | 55.10% | |
| 8. Promotional car | 24 | 6.60% | |
| 9. Others | 3 | 0.80% |
4.3. Nursing student's mean scores
The results of the study showed that the nursing students had the following mean scores on knowledge of COVID-19 9.43 (SD1.19); perceived susceptibility 19.41 (SD2.68); perceived severity 20.31 (SD 4.09); perceived benefits 26.52 (SD 4.08); perceived barriers 15.17 (SD5.88); cues to action 3.30 (SD1.70); self-efficacy 17.68 (SD2.83); and behavioral intention 18.46 (SD2.33) (Table 3).
Table 3.
Nursing student's mean scores.
| N = 361 | Items | Mean | SD |
| Knowledge | 11 | 9.43 | 1.19 |
| Perceived susceptibility | 5 | 19.41 | 2.68 |
| Perceived severity | 6 | 20.31 | 4.09 |
| Perceived benefits | 6 | 26.52 | 4.08 |
| Perceived barriers | 6 | 15.17 | 5.88 |
| Cues to action | 9 | 3.30 | 1.70 |
| Self-efficacy | 4 | 17.68 | 2.83 |
| Behavioral intention | 4 | 18.46 | 2.33 |
4.4. Spearman rho correlation analysis results
Spearman rho correlation analysis results are presented in Table 4. It was found that 361 nursing students’ COVID-19 knowledge was positively correlated with self-efficacy, r = .162 (P < .01), and behavioral intention, r = .158 (P < .01). In addition, nursing students’ perceived susceptibility was positively correlated with perceived severity, r = .279 (P < .01), perceived benefits, r = .325 (P < .01), self-efficacy, r = .236 (P < .01), and behavioral intention, r = .279 (P < .01). Moreover, nursing students’ perceived severity was positively correlated with perceived benefits, r = .158 (P < .01), and perceived barriers, r = .193 (P < .01). Furthermore, nursing students’ perceived benefits were positively correlated with perceived barriers, r = −.237 (P < .01), self-efficacy, r = .451 (P < .01), and behavioral intention, r = .525 (P < .01). Nursing students’ perceived barriers were positively correlated with self-efficacy, r = −.224 (P < .01), and behavioral intention, r = −.352 (P < .01). Nursing students’ cues to action were also positively correlated with self-efficacy, r = .104 (P < .05). Finally, nursing students’ self-efficacy was positively correlated with behavioral intention, r = .667 (P < .01).
Table 4.
Spearman rho correlation analysis results.
| N = 361 | COVID-19 knowledge | Perceived susceptibility | Perceived severity | Perceived benefits | Perceived barriers | Cues to action | Self-efficacy | Behavioral intention |
| COVID-19 knowledge | 1 | |||||||
| Perceived susceptibility | .084 | 1 | ||||||
| Perceived severity | .092 | .279∗∗ | 1 | |||||
| Perceived benefits | .068 | .325∗∗ | .158∗∗ | 1 | ||||
| Perceived barriers | −.020 | .034 | .193∗∗ | −.237∗∗ | 1 | |||
| Cues to action | .026 | −.019 | .053 | .051 | −.092 | 1 | ||
| Self-efficacy | .162∗∗ | .236∗∗ | .075 | .451∗∗ | −.224∗∗ | .104∗ | 1 | |
| Behavioral intention | .158∗∗ | .279∗∗ | .067 | .525∗∗ | −.352∗∗ | .094 | .667∗∗ | 1 |
4.5. Multiple hierarchical regression analysis results
In model 1, nursing students’ demographic background regarding school system, gender, age, religious beliefs, health status, diet, movement, and reading COVID-19 information explained 5.2% of the variance in behavioral intention (R2 = 0.052, F = 2.118, P < .05) (Table 5). Table 5 shows the data on the health status (B = 0.210, t = 3.706, P < .001), and it can be seen that nursing students had a very good health status with the highest impact on their behavioral intention.
Table 5.
Multiple hierarchical regression analysis results.
| Model 1 | Model 2 | |||
| Standardized coefficients | t values | Standardized coefficients | t values | |
| Variables | Beta distribution | Beta distribution | ||
| Constant | 67.695∗∗∗ | 5.446∗∗∗ | ||
| School system | ||||
| Four-year program | −.004 | −.050 | .012 | .209 |
| Two-year program | .031 | .337 | −.008 | −.131 |
| Gender | ||||
| male | −.078 | −1.471 | −.001 | −.037 |
| Age | ||||
| Above 20-years-old | −.037 | −1.368 | −.033 | −.492 |
| Religious beliefs | ||||
| No religious beliefs | −.065 | −1.244 | −.011 | −.309 |
| Health status | ||||
| Very good health status | .210 | 3.706∗∗∗ | .059 | 1.560 |
| Diet | ||||
| Normal diet without 3 meals | −.004 | −.069 | −.012 | −.323 |
| Movement | ||||
| Regular movement | −.003 | −.046 | −.022 | −.590 |
| Reading COVID-19 information | ||||
| No reading | −.018 | −.337 | .072 | 1.967 |
| COVID-19 knowledge | .047 | 1.290 | ||
| Perceived susceptibility | .093 | 2.315∗ | ||
| Perceived severity | −.007 | −.193 | ||
| Perceived benefits | .274 | 6.446∗∗∗ | ||
| Perceived barriers | −.151 | −4.008∗∗∗ | ||
| Cues to action | .044 | 1.203 | ||
| Self-efficacy | .480 | 11.513∗∗∗ | ||
| R2 = 0.052 | F = 2.118∗ | R2 = 0.581 | F = 29.775∗∗∗ | |
| ΔR2 = 0.529 | ΔF = 62.019∗∗∗ | |||
In model 2, the results of this study showed that nursing students’ demographic background regarding school system, gender, age, religious beliefs, health status, diet, movement, reading COVID-19 information, COVID-19 knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy explained 58.1% of the variance in behavioral intention (R2 = 0.581, F = 29.775, P < .001) (Table 5).
Nursing students’ demographic background concerning school system, gender, age, religious beliefs, health status, diet, movement, and reading COVID-19 information were controlled, COVID-19 knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy explained 52.9% of the variance in behavioral intention (R2 = 0.529, ΔF = 62.019, P < .001) (Table 5).
Table 5 presents the data on perceived susceptibility (B = 0.093, t = 2.315, P < .05), perceived benefits (B = 0.274, t = 6.446, P < .001), perceived barriers (B = 0.151, t = −4.008, P < .001), and self-efficacy (B = 0.480, t = 11.513, P < .001). It can be seen that nursing students’ high self-efficacy, high perceived benefits, low perceived barriers, and high perceived susceptibility had the highest sequential impact on their behavioral intention.
5. Discussion
According to the World Health Organization, COVID-19 is currently an epidemic and infective disease,[32] is inflicting serious damage on people physically, psychologically, emotionally, and socially,[33] and threatens the world economy.[34] Since many millions of people are suffering from COVID-19 globally, effective preventing measures are critical. Washing one's hands and wearing a face mask are demonstrably correlated with a lower rate of spread of COVID-19, and constitute effective ways to prevent the infectious disease among community residents.[35,36] COVID-19 preventive measures are major components of health literacy in health promotion.[37,38] This study aimed to elucidate nursing students’ COVID-19 knowledge, health beliefs, self-efficacy, and behavioral intention.
The findings indicated that nursing students’ cues to action included television, broadcast, news, network, health care workers, poster promotion, school promotion, promotional car, and others. The results of this study demonstrated that television is the best communication tool, network is the second-best, and school promotion is the third-best for nursing students concerning COVID-19 preventive measures.
In addition, nursing students’ mean scores were as follows: COVID-19 knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, self-efficacy, and behavioral intention. All nursing students’ health beliefs associated with all items on the mean scores indicated good healthy beliefs concerning COVID-19 knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, self-efficacy, and behavioral intention.
From the Spearman rho correlations analysis, all nursing students’ COVID-19 knowledge was positively correlated with health beliefs, self-efficacy, and behavioral intention. The findings also demonstrated that all nursing students possessed COVID-19 knowledge, evaluated their health beliefs, increased individuals’ self-efficacy, and practiced behavioral intention for preventing the spread of COVID-19.
Nursing students’ demographic background regarding school system, gender, age, religious beliefs, health status, diet, movement, reading COVID-19 information, including health beliefs about COVID-19 knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy explained 58.1% of the variance in behavioral intention. In accordance with a previous study,[39] practicing self-efficacy is strongly associated with behavioral intention. Our study offers the same findings as that study concerning implementing public health strategies to increase COVID-19 knowledge and health beliefs regarding physical, psychological, emotional, and social health promotion. Peoples’ positive coping, positive responses, and job satisfaction strengthen psychological prevention[40] and psychological health, which are associated with physical, emotional, and social health for avoiding COVID-19 infection.[41,42]
6. Limitations
The limitations of this study are that the participants were limited to 361 nursing students in 200 five-year, 45 four-year, and 116 two-year nursing education programs at a university. This study may have limited the data that were collected all 361 nursing students. In addition, all participants were limited to nursing students in the Department of Nursing at a University in Kaohsiung City, Taiwan, ROC.
7. Conclusions
This study found that nursing students’ mean scores were as follows: COVID-19 knowledge 9.43, perceived susceptibility 19.41, perceived severity 20.31, perceived benefits 26.52, perceived barriers 15.17, cues to action 3.30, self-efficacy 17.68, and behavioral intention 18.46. Nursing students’ demographic background, COVID-19 knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy explained 58.1% of the variance in behavioral intention. Therefore, nursing educators can increase COVID-19 knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy for nursing students as effective health promotion strategies to improve their behavioral intention and prevent the spread of COVID-19 locally and globally.
Author contributions
Conceptualization: Fu-Ju Tsai.
Data curation: Fu-Ju Tsai.
Formal analysis: Fu-Ju Tsai, Cheng-Yu Chen.
Funding acquisition: Fu-Ju Tsai.
Investigation: Fu-Ju Tsai.
Methodology: Fu-Ju Tsai, Yih-Jin Hu, Cheng-Yu Chen, Gwo-Liang Yeh.
Project administration: Fu-Ju Tsai, Yih-Jin Hu.
Resources: Fu-Ju Tsai, Yih-Jin Hu.
Software: Fu-Ju Tsai.
Supervision: Yih-Jin Hu, Cheng-Yu Chen, Chie-Chien Tseng, Gwo-Liang Yeh, Jin-Fong Cheng.
Validation: Yih-Jin Hu, Cheng-Yu Chen, Chie-Chien Tseng, Gwo-Liang Yeh, Jin-Fong Cheng.
Visualization: Yih-Jin Hu, Cheng-Yu Chen, Chie-Chien Tseng, Gwo-Liang Yeh, Jin-Fong Cheng.
Writing – original draft: Fu-Ju Tsai.
Writing – review & editing: Fu-Ju Tsai, Yih-Jin Hu.
Corrections
When originally published, the section heading 3.1 Design was incorrectly printed as 3.1 2.1 Design. It has since been corrected.
Footnotes
Abbreviations: COVID-19 = coronavirus disease 2019, SD= standard deviation.
How to cite this article: Tsai FJ, Hu YJ, Chen CY, Tseng CC, Yeh GL, Cheng JF. Using the health belief model to explore nursing students’ relationships between COVID-19 knowledge, health beliefs, cues to action, self-efficacy, and behavioral intention: a cross-sectional survey study. Medicine. 2021;100:11(e25210).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
P < .05.
P < .01.
P < .05.
P < .001.
References
- [1].Awadasseid A, Wu Y, Tanaka Y, et al. Initial success in the identification and management of the coronavirus disease 2019 (COVID-19) indicates human-to-human transmission in Wuhan, China. Int J Biol Sci 2020;16:1846–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Riou J, Althaus CL. Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020. Euro Surveill 2020;25:2000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Taiwan centers for disease control (2020). COVID-19. Available at: https://www.cdc.gov.tw/ [assessed July 18, 2020] [Google Scholar]
- [4].Dey SK, Rahman MM, Siddiqi UR, et al. Analyzing the epidemiological outbreak of COVID-19: a visual exploratory data analysis approach. J Med Virol 2020;92:632–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Madabhavi I, Sarkar M, Kadakol N. COVID-19: a review. Monaldi Arch Chest Dis 2020;90: 10.4081/monaldi.2020.1298. doi:10.4081/monaldi.2020.1298. [DOI] [PubMed] [Google Scholar]
- [6].Harapan H, et al. Coronavirus disease 2019 (COVID-19): a literature review. J Infect Public Health 2020;13:667–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Jia Q, et al. Analysis of knowledge bases and research hotspots of coronavirus from the perspective of mapping knowledge domain. Medicine 2020;99:e20378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Chena Z, et al. High-resolution computed tomography manifestations of COVID-19 infections in patients of different ages. Eur J Radiol 2020;1–6. www.elsevier.com/locate/ejrad [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kanga L, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun 2020;1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Verity R, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis 2020; 10.1016/S1473-3099(20)30243-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Wang Y, Wang Y, Chen Y, et al. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol 2020;92:568–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Sifuentes-Rodríguez E, Palacios-Reyes D. COVID-19: the outbreak caused by a new coronavirus. Bol Med Hosp Infant Mex 2020;77:47–53. [DOI] [PubMed] [Google Scholar]
- [13].Whittaker A, Anson M, Harky A. Neurological manifestations of COVID-19: a systematic review and current update. Acta Neurol Scand 2020;142:14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Singhal T. A review of coronavirus disease-2019 (COVID-19). Indian J Pediatr 2020;87:281–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Wang L, Wang Y, Ye D, et al. Review of the 2019 novel coronavirus (SARS-CoV-2) based on current evidence. Int J Antimicrob Agents 2020;55:105948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Sun P, Lu X, Xu C, et al. Understanding of COVID-19 based on current evidence. J Med Virol 2020;92:548–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Keesara S, Jonas A, Schulman K. Covid-19 and health care's digital revolution. N Engl J Med 2020;1–3. [DOI] [PubMed] [Google Scholar]
- [18].Peyrin-Biroulet L. Will the quality of research remain the same during the COVID-19 pandemic? Clin Gastroenterol Hepatol 2020;1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Turer RW, et al. Electronic personal equipment: a strategy to protect emergency department providers in the age of COVID-19. Am Med Inform Assoc 2020;1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun 2020;109:102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Phan T. Novel coronavirus: from discovery to clinical diagnostics. Infect Genet Evol 2020;79:104211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Nochaiwong S, et al. Mental health circumstances among healthcare workers and general public under the pandemic situation of COVID-19 (HOME-COVID-19). Medicine 2020;99:26.e20751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Tu ZH, He JW, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: a cross-sectional study. Medicine 2020;99:26.e20769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Gao Q, et al. The epidemiological characteristics of 2019 novel coronavirus diseases (COVID-19) in Jingmen, Hubei, China. Medicine 2020;99:23.e20605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. JOSSEY-BASS A Wiley Imprint 2008;http://www.josseybass.com [Google Scholar]
- [26].Nobiling BD, Maykrantz SA. Exploring perceptions about and behaviors related to mental illness and mental health service utilization among college students using the health belief model (HBM). Am J Health Edu 2017;48:306–19. [Google Scholar]
- [27].Mukhtar S. Mental health and emotional impact of COVID-19: applying health belief model for medical staff to general public of Pakistan. Brain Behav Immun 2020;87:28–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Jimeneza T, et al. Fatalism in the context of COVID-19: perceiving coronavirus as a death sentence predicts reluctance to perform recommended preventive behaviors. SSM Population Health 2020;11:100615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Honarvar B, et al. Knowledge, attitudes, risk perceptions, and practices of adults toward COVID-19: a population and field-based study from Iran. Int J Public Health 2020; 10.1007/s00038-020-01406-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Cvetkovic VM, et al. Preparedness and preventive behaviors for a pandemic disaster caused by COVID-19 in Serbia. Int J Environ Res Public Health 2020;17:4124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Krejcie RV, Morgan DW. Determining sample size for research activities. Edu Psychol Meas 1970;30:607–10. [Google Scholar]
- [32].Sohrabi C, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg 2020;76:71–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Lima CKT, et al. The emotional impact of coronavirus 2019-nCoV (new coronavirus disease). Psychiatry Res 2020;287:112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Peixoto PS, Marcondes D, Peixoto C, et al. Modeling future spread of infections via mobile geolocation data and population dynamics. An application to COVID-19 in Brazil. PloS One 2020; 10.1371/journal.pone.0235732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Lin YH, Liue CH, Chiug YC. Google searches for the keywords of “wash hands” predict the speed of national spread of COVID-19 outbreak among 21 countries. Brain Behav Immun 2020; 10.1016/j.bbi.2020.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Chen X, et al. Hand hygiene, mask-wearing behaviors and its associated factors during the COVID-19 epidemic: a cross-sectional study among primary school students in Wuhan, China. Int J Environ Res Public Health 2020;17:2893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Bernard SS, et al. First cases of coronavirus disease 2019 (COVID-19) in France: surveillance, investigations and control measures. Euro Surveill 2020;25:2000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Lin C, et al. Policy decisions and use of information technology to fight COVID-19, Taiwan. Emerg Infect Dis 2020;26:1506–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Lee M, You M. Psychological and behavioral responses in South Korea during the early stages of coronavirus disease 2019 (COVID-19). Int J Environ Res Public Health 2020;25,17:2977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Wang YX, et al. Factors associated with post-traumatic stress disorder of nurses exposed to corona virus disease 2019 in China. Medicine 2019;99:26.e20965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Cao W, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res 2020;287:112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Zhou SJ. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry 2020;29:749–58. [DOI] [PMC free article] [PubMed] [Google Scholar]


