Abstract
Background
: Suicide reports during the COVID pandemic is an increasing cause for concern. However, there is a limited understanding of suicide among individuals with positive/suspected COVID diagnosis specifically. Hence, this study, using online newspaper reports, aimed to determine factors influencing suicide among individuals withCOVID-19 infection status.
Methodology
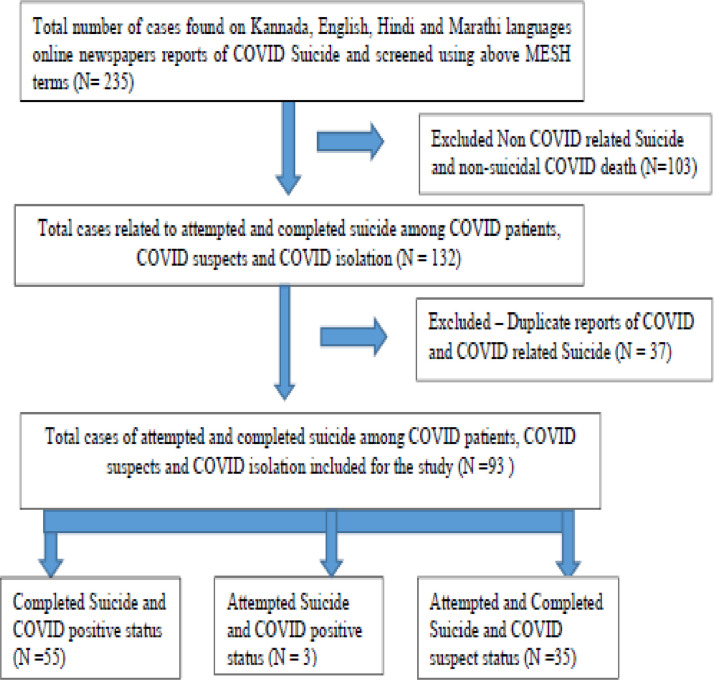
: Information regarding positive/suspected COVID related suicide was obtained from online newspapers published in 4 languages between 30th Jan 2020 to 16th August 2020 using google news aggregator. Of 235 online identified, 93 were eligible for analysis after the exclusion and analysed using descriptive statistics.
Results
: Median Age of COVID related suicide victims was 45 years (range 15 - 80) wherein 61.3% belonged to 30-59 year age group, and 75.3% were males. 50% of suicides occurred within the first week of COVID diagnosis confirmation, and 50% suicides occurred at COVID centres. Hanging (53.8%) was the commonest method of suicide, followed by jumping (12.9%).
Conclusion
: Higher risk for suicide was observed among male gender and those with positive/suspected COVID infection within the first week, while receiving treatment in COVID care centres. Hanging and jumping were the two commonest methods. The above highlight an urgent need to integrate suicide preventive strategies into standard care protocols of COVID-19 positive and suspected cases.
Keywords: COVID, Suicide, Online, Print media, Newspaper
1. Introduction
Suicide is a major public health concern. National Institute of Mental Health (NIMH) defines suicide as death caused by self-directed injurious behaviour with intent to die as a result of the behaviour. (NIMH October 6, 2020) Suicide occurs throughout the lifespan and was the second leading cause of death among 15-29 year-olds globally in 2016. (Suicide August 28, 2020) World Health Organisation (WHO) reported that many suicides occur during a crisis such as a pandemic. A review of the literature shows an increased rate of suicidal deaths during current COVID-19 pandemic, which is similar to previous scientific studies on suicide rate during the Influenza, MERS and Severe SARS outbreaks. (Wasserman, 1992, Chan et al., 2006, Singh, 2020). The proposed reasons for a greater rate of suicides in COVID- 19 pandemic include lockdowns, quarantining, social isolation and associated abrupt change in lifestyle, discrimination/stigma about having or contracting COVID-19 infection, migration, economic stress, decreased access to community and religious support, infodemic about COVID-19, and mental health problems. The prevailing uncertainty regarding future has led individuals to catastrophise and experience an overwhelming sense of dread and panic. (Usher et al., 2020, Shoib et al., 2020) Furthermore, exacerbating the above are incorrect inferences drawn by individuals from various media platforms, including television, radio and newspapers, wherein rapidly disseminating COVID-19 related information exaggerate the unpredictable nature, course and outcome of this pandemic. An unfortunate associated outcome is myths and misinformation arising from limited or selective information leading to a misunderstanding of suicide-related news which has a potential for triggering copycat suicides rather than preventing further suicides, also called the “Werther Effect”. (Shalvee, 2020, Stack, 2003, Hawton and Williams, 2002)
Till date, there are five published articles on COVID-19 related suicides from India. Sheikh et al studied 32 suicide cases reported in the period from January to April 2020 and noted that the maximum cases were reported from the state of Uttar Pradesh, most committed suicide in their homes, and surprisingly most of them were COVID negative. (Shoib et al., 2020) Rajkumar found 23 cases of suicides reported from March to April 2020, while D'souza et al found 69 suicide cases which were reported in March to May 2020. (Rajkumar, 2020, Dsouza et al., 2020) . Singh et al., identified three waves of suicide during various stages of lockdown and urged for a national suicide prevention strategy in India on a large-scale level (Singh, 2020). Ahamed et al., studied 23 reports of alcohol withdrawal-related suicides during the lockdown and brought out the need for measures to prevent suicides as well the need to reduce the high level of alcohol dependence among the people (Ahmed et al., 2020). While these studies provided information pertaining to victims' sociodemographic details, the mode, and the place of committing suicide obtained from the media reports, they largely focused on various potential triggers for suicidal events from available online media reports. These studies' findings were fairly consistent, reporting higher rates among males, hanging being the commonest mode with fear of contagion as the most common cause. Adding to this, Griffiths and Mamun reported three completed and one attempted suicide pacts in the context of COVID-19 in India and 2 cases outside India. (Griffiths and Mamun, 2020) However, there is a lack of literature comparing suicides in the context of COVID-19 positive status to COVID-19 suspected suicides (defined as suicide among high-risk or those suspected to have the COVID-19) with specific relevance to a place of suicide and timeline of occurrence of suicides in relation to COVID-19 testing/care status.
Hence, this study, using online newspaper reports, aimed to identify the temporal correlation of COVID-19 infection status and related factors influencing suicide risk.
2. Methodology
We conducted a “Google news aggregator search” of online newspapers from 30th January 2020 to 16th August 2020, published in India. News reported in 4 languages, including English, Hindi, and two vernacular languages (Kannada and Marathi), were collected from regional and national news platforms to ensure the inclusion of all appropriate COVID-19 cases. We chose English and Hindi online print media, representing the largest circulation and readers in India. Also, we chose two regional vernacular languages (Kannada and Marathi), as the convenience of researcher Lingua. Two authors (MNS and MP) independently searched google with 'news' as a filter, using the terms 'Suicide', 'India', 'Corona', 'COVID-19,' 'Self-harm,' and 'Names of all Indian States and Union Territories' (e.g. Karnataka, Tamil Nadu, Maharashtra, etc). To avoid multiple entries of each incident the information was re-evaluated and jointly reassessed to confirm the same prior to final inclusion in the datasheet. Additionally, careful examination of sociodemographic data and suicide-related information of COVID-19 individuals was undertaken to avoid duplication.
For the study, we defined “COVID-19 suicides” reported in online print media into two groups. One group was "COVID-19 Positive Suicide," in which suicide was committed by a person with verified COVID-19 Positive status. Another group was "COVID-19 suspected suicide" in which a person with a high risk of COVID-19 infection committed suicide (primary contacts positive for COVID-19 or experiencing influenza like disease (ILI) symptoms awaiting COVID results or stigma of contracting COVID infection awaiting results). The Flow chart-1 provides details of the selection process of COVID-19 positive/suspected suicides. A total of 235 online newspaper articles of COVID-19 suicide were screened and identified using the above MESH terms. Of these, 103 were Non COVID-19 related suicide and non-suicidal COVID-19 death and hence excluded from the study. A total of 132 articles were included in the study. Out of 132, 37 articles were deemed to be reports of the same incident, as inferred from the sociodemographic details and other circumstances surrounding the event, and hence were merged. Two articles were related to general non-specific information and preventive measures in the context of COVID-19 related suicides, rather than specific incidents, and hence excluded. Finally, for the given period, the total number of suicides related to positive/suspected COVID was 93. Out of these, 58 suicides were among individuals who had tested positive for the infection. In the remaining group (35), six individuals had tested negative, and 26 had not got themselves tested. For the remaining 3, no details of testing were mentioned and were thus considered under COVID-19 negative suicides. The data were obtained using a semi-structured proforma which included age, gender, marital status, employment, workplace, suicide notes, the relationship between positive/suspected COVID status with time to suicide, the method used, and location of suicide. Data were analysed using descriptive statistics and spearman correlation.
Flow Chart 1.
Flow Chart 1 - Shows the COVID Suicide case selection process from the online newspaper
3. Results
A total of 93 COVID-19 suicides were examined, among them, 58 were among COVID-19 positive patients, and 35 were COVID-19 suspected individuals. Table-1 shows the comparison between COVID-19 positive and COVID-19 suspected suicides. There was no difference between groups noted in terms of age, gender, and suicide methods adopted among COVID-19 positive patients and suspected individuals. The sample's median age was 45 years (range 15-80) and 75% were males. Interestingly, the online newspaper reports mentioned that only eight individuals had a pre-existing medical illness (chronic kidney disease being the commonest) and 4 had psychiatric conditions. The mode of suicide was noted in 84% cases, out of which 54% was hanging, making it the most common modality used, followed by jumping from height 12.9%. Other lesser common modalities include drowning 3.2%, slitting throat/wrist 4.2%, and poisoning 4.2%.
Of the 35 COVID-19 suspected individuals, 26 had not undergone any test for COVID-19. Importantly, six individuals who underwent testing committed suicide before receiving their COVID-19 report, and later they were found to be negative. For the remaining 3, no details of testing were mentioned and considered under COVID-19 negative suicides.
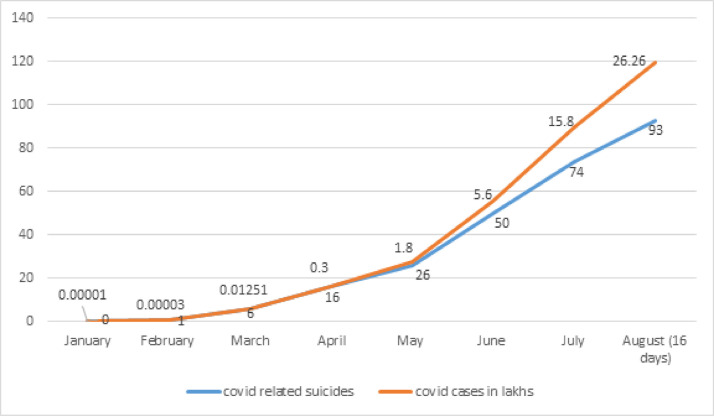
Figure 2 depicts the relationship of total COVID cases with COVID related suicides. There was a strong positive correlation between a number of COVID cases with COVID related suicides with R=0.979 (p<0.001).
Figure 2.
Graph depicting the relation of total COVID cases with COVID related suicides
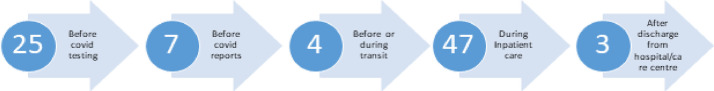
Figure 3 shows a timeline of the occurrence of suicide in relation to COVID testing/care status. The study showed that nearly 50% of individuals committed suicide happened while they were institutionalised (COVID Hospital or Quarantine Centres), while 36 % committed while they were at home, for the rest details were not available. 50% of suicide happened in the first week of COVID positive status. Furthermore, two individuals ended lives while they were being transported to an institution right after their COVID-19 results. One couple and one cancer survivor committed suicide after getting discharged from the hospital.
Figure 3.
Timeline of occurrence and number of suicides in relation with COVID testing/care status
4. Discussion
In the current COVID pandemic, our study compared the COVID-19 positive and COVID-19 suspected suicides with respect to age, gender, place of suicide, and timeline of occurrence of suicides in relation to COVID-19 testing/care status as well as trends associated with overall COVID-19 infection rates. The findings highlight that majority of COVID related suicides occur in males and those belonging to the middle age group. Most COVID patients committed suicide while they were away from families, in isolation (COVID hospital, Quarantine centres, transit to the hospital) and during the first week of COVID positive status. No differences were noted in terms of age, gender, and suicide methods adopted among those with a COVID-19 positive status compared to those having a COVID-19 suspected status. Additionally, we have observed the COVID-19 related suicide rate was 16.7 per 1,00,000 population, which is well above the national average of averahe 10.2 per 1,00,000 population(Accidental Deaths & Suicides in India - 2019 September 6, 2020). Findings also highlight a strong positive correlation between a number of COVID cases with COVID related suicides. On comparing the state-wise distribution of our sample, Karnataka had the maximum proportion (20%) of reported suicides, followed by Maharashtra (11.6%) & Bihar (10.5%). This is comparable with National Crime Record Bureau (NCRB) data regarding Karnataka & Maharashtra in the top 5 states in suicide for the last five consecutive years (2014-2019). It's noteworthy that these two states have the highest number of COVID-19 infections in the country.
In this study, the median age of the sample was 45 years (range 15-80) and 61% of suicides occurred among those aged 30 - 60 years, in comparison to NCRB (Accidental Deaths & Suicides in India - 2019 September 6, 2020), wherein young adults (18-45years) formed the majority (66.9%). The study by Shoib et al., in contrast to our findings, indicates that the majority of suicides occurred in the young adult group (18-35 years of age), but this was limited to reporting from January to April 2020 (Shoib et al., 2020) The higher suicide rate in middle age group might have been due to a) COVID-19 infection rate being higher among middle-age group individuals, b) they were more vulnerable to develop uncertainty and panic about future, resulting in anxiety and depression, leading to anomic suicides in the current pandemic. (Menon et al., 2018) The male gender accounts for the majority of suicide in our study, which is comparable to 2019 NCRB data (Accidental Deaths & Suicides in India - 2019 September 6, 2020) and other previous COVID-related suicide studies. The study found that the mode of suicide was reported in 84% cases, and hanging was the most common method comparable to NCRB-2019 data. The jumping from height was more in COVID-19 related suicide, which is consistent with study findings from Philip et al., and Shoib et al., (Shoib et al., 2020, Rajkumar, 2020) Given that higher rates of infections occurred in urban settings in India, having the greater presence of high rise buildings could explain easier access to this means and a hence more increased rate of jumping as a mode of committing suicide in comparison with NCRB data.
Our study found that more than 50% of suicides occurred in an institutional setting, which was consistent with study findings from Philip et al (Rajkumar, 2020). Additionally of note, the current study identified that majority of suicides occurred in the first week of COVID positive status and individuals had expressed either a fear of death by COVID-19, extreme isolation at institutional or stigma associated with COVID-19. Stigma related to COVID infection is faced by patients, healthcare workers, and survivors of the disease and their unaffected family members, having been extensively reported in India and cause for serious concern given the above fatalities. (Coronavirus | How life changes post COVID-19 recovery - The Hindu September 27, 2020, Indian doctors being evicted from homes over coronavirus fears | Coronavirus outbreak | The Guardian n.d. September 27, 2020) There was a report of a middle-aged man killing himself because his family members had tested positive and being ostracised by neighbours who blamed them for spreading infection. (ಕೊರೊನಾ: ನೆರೆಮನೆಯವರ ಅವಮಾನಕ್ಕೆ ನೊಂದು ವ್ಯಕ್ತಿ ಆತ್ಮಹತ್ಯೆ- Kannada Prabha n.d. September 27, 2020) In another incident, an extended suicide was noted, wherein one young man consumed poison along with the wife and child, due to the fear that he has been a source of the infection to his family. (Karnataka, September 27, 2020) Both cases illustrate the influence of stigma and discrimination in the context of COVID positive/suspected infection leading to unnecessary loss of lives. World Health Organisation (WHO) and Ministry of Health and Family Welfare (MoHFW), Government of India have identified lack of adequate information, fear of the disease, and rumours/misinformation as the major contributory factors. It may be necessary to formulate proactive strategies that can overcome the same. (MoHFW 2020, Coronavirus Disease September 2, 2020)
As social stigma and uncertainty regarding illness outcome arising from COVID-19 are associated with the higher rate of suicides, health professionals must provide attention, evaluate and closely monitor for emergent suicide risk concurrently with regular COVID clinical care. So, all patients at the time of undergoing testing and particularly over the 7-10 days after receiving a positive test result as well as on admission to care centres should get screened for stigma, apprehension, monitoring for self-harm risk, and suicidal ideas. (1) Additionally, patients in COVID care centre/isolation/quarantine centre need to be encouraged to regularly use the telephonic /internet-based modalities to stay socially connected with significant others whilst in physical isolation, ensure adequate sleep, undertake medically supervised exercise regimens and relaxation/ meditation strategies. It is vital to ensure and convey community and family support for those in isolation/quarantine, by providing all needs are attended to and proactively stay “socially connected” to the individual. New initiatives like a) Peer-based support, including scheduled group interactions among institutionalised patients and health workers, can be encouraged using the buddy system and displaying posters with helpline numbers. (Pfefferbaum and North, 2020, Bagcchi, 2020); b) Telemedicine can be a useful tool to improve the accessibility of mental health care during COVID. (Thirthalli et al., 2020); c) Where resources permit, additional display of awareness through audio, videos, the chart can be made using positive stories of those who have recovered from COVID-19 and using authentic information with the website of MoHFW, Govt. of India, or the WHO. (MoHFW 2020, The United Nations Children's Fund 2020); d) opportunities for recreational activities that help maintain the morale of the patients. (Sher, 2020, Sher, 2020) and e) COVID care Centres (CCC) and hospitals would benefit from incorporating additional structural safety measures to reduce the mode of suicide like jumping and hanging by restricting access to means.
Suicide has been a major public health issue for many decades and now it has grabbed further attention during the COVID-19 pandemic in India. Early identification of risk factors and prevention of suicide is essential during a pandemic, and it's critical to continue those measures further into the post-pandemic times. However, to tackle such a rapidly growing and multifaceted problem, no single strategy is likely to work best. So, there is a need to implement a national strategy to prevent suicide as advocated by the National Mental Health Policy (NMHP). It talks about screening programs for suicide prevention, gatekeeper training, restriction of access to means, media strategies for suicide prevention and suicide hotline/helpline at national, regional, and community levels. (Manoranjitham et al., 2006, National_Health_Mental_Policy.pdf, 2014) Adding to that, the recent Mental Health Care Act (MHCA), 2017; Section 115, subsection 2 advocates that the appropriate Government shall have a duty to provide care, treatment and rehabilitation to a person, having severe stress and who attempted to commit suicide, to reduce the risk of recurrence of attempt to commit suicide. (MoHFW, 2017) Even though it was partially addressed under mental health policy and act, a separate national suicide prevention policy is non-existent in India compared to other LAMIC countries such as Sri Lanka, Bhutan, Bulgaria and Uruguay. Hence the Government should consider drawing a national suicide prevention policy by involving sectors like health, education, social welfare, police, and the judiciary in the planning and organisation policy and services to prevent suicide.
This study is a first of its kind to compare the COVID-19 positive and COVID-19 suspected suicides, place of suicide, and timeline of suicides in relation to COVID-19 testing/care status and trends associated with overall COVID-19 infection rates. The study also offers insights into variations in risk associated with COVID-19 related suicides comparing findings to NCRB 2019 data on suicides in India. The data extraction and subsequent study findings derived were from objective facts stated in reports rather than subjective or presumptive information, allowing for more accurate interpretation. This study has few limitations, such as a) Study being restricted to information extracted from newspaper reports, given the absence of any other official or reliable source of data related to suicides during the COVID-19; b) There might have been an underestimation of actual suicide burden during the COVID-19 pandemic, as well as study lacked coverage of other important factors that may contribute to suicide risk during this vulnerable period; c) Authenticity and reliability of reports from online newspapers may be questionable given subjective and objective components of reports. It may not be demarcated leading to a misrepresentation of actual context and facts, which was partly attenuated by focusing on objective facts rather than conjecture and d) Study chose only two regional vernacular languages (Kannada and Marathi) based on convenience of researcher lingua. Hence specific findings may be restricted to regions covered that may not be reflective for all states of India and generalisation of the findings is not assured.
5. Conclusion
The COVID-19 related suicide rates are well above the national average suicide rate highlighting an urgent need to address the same. The heightened risk for COVID-19 related suicide is within the first week of diagnosis while receiving treatment in COVID-19 care setting and male gender. Hanging and jumping were the two most common methods used. This study's findings emphasised the need to incorporate multi-level and inter sectorial suicide prevention strategies during COVID-19 care by clinicians, public health officials, and administrators. The study also offered specific COVID-19 infection status-related suicide risk factors that can provide much-needed directions for implementing effective strategies.
6. Author statement file
Relevant CRediT roles:
All authors contributed in conceptualization, data curation, formal analysis, investigation, designing the methodology, writing and revising the draft, reviewing and editing the draft.
Table 1.
Comparison between COVID-19 positive and COVID-19 suspected Suicides
| Variable | COVID-19 positive suicides (N = 58) | COVID-19 suspected suicides (N = 35) | COVID related Suicide [COVID Positive suicides + COVID Suspected Suicides] (N = 93) | |
|---|---|---|---|---|
| Total number of cases | 58 | 35 | 93 | |
| Mean Age in years | 47.3 | 41 | 44.8 | |
| Age in years | <18 | 1 (1.7%) | 0 | 1 (1.1%) |
| 18-29 | 6 (10.3%) | 6 (17.1%) | 12 (12.9%) | |
| 30-44 | 15 (25.86%) | 12 (34.3%) | 27 (29%) | |
| 45-59 | 19 (32.7%) | 11 (31.4 %) | 30 (32.3%) | |
| 60 & above | 12 (20.68%) | 0 | 12 (13.7%) | |
| Missing Data | 5 (8.6%) | 6 (17.1%) | 11 (11.8%) | |
| Gender | Male | 40 (68.9 %) | 30 (85.7%) | 70 (75.3%) |
| Female | 15 (25.86%) | 5 (14.3%) | 20 (21.5 %) | |
| Missing data | 3 (5.1%) | 0 | 3 (3.2%) | |
| Gender Ratio | 73:27 | 86:14 | 78:22 | |
| Method of Suicide | Hanging | 31 (53.4%) | 19 (54.3 %) | 50 (53.8%) |
| Jumping | 10 (17.2%) | 2 (5.7 %) | 12 (12.9%) | |
| Poison consumption | 1 (1.7%) | 3 (8.6 %) | 4(4.3%) | |
| Drowning | 2 (3.4%) | 1 (2.9 %) | 3(3.2%) | |
| Burns | 0 | 2 (5.7 %) | 2 (2.1%) | |
| Train/vehicle | 0 | 1 | 1(1.07%) | |
| Missing Data | 10 (17%) | 5 (14.3%) | 15(16.1%) | |
Declaration of Competing Interest
All authors declare no conflict of interest
References
- Ahmed S., Khaium M.O., Tazmeem F. COVID-19 lockdown in India triggers a rapid rise in suicides due to the alcohol withdrawal symptoms: Evidence from media reports. The International journal of social psychiatry. 2020;66(8):827–829. doi: 10.1177/0020764020938809. [DOI] [PubMed] [Google Scholar]
- NIMH » Suicide n.d. https://www.nimh.nih.gov/health/statistics/suicide.shtml (accessed October 6, 2020).
- Suicide n.d. https://www.who.int/health-topics/suicide#tab=tab_1 (accessed August 28, 2020).
- Wasserman IM. The Impact of Epidemic, War, Prohibition and Media on Suicide: United States, 1910–1920. Suicide Life-Threatening Behav. 1992;22:240–254. doi: 10.1111/j.1943-278X.1992.tb00231.x. [DOI] [PubMed] [Google Scholar]
- Chan SMS, Chiu FKH, Lam CWL, Leung PYV, Conwell Y. Elderly suicide and the 2003 SARS epidemic in Hong Kong. Int J Geriatr Psychiatry. 2006;21:113–118. doi: 10.1002/gps.1432. [DOI] [PubMed] [Google Scholar]
- Singh GP. Lockdown and 3 Waves of Suicide in India During the COVID-19 Pandemic. Prim Care Companion CNS Disord. 2020;22 doi: 10.4088/PCC.20com02794. [DOI] [PubMed] [Google Scholar]
- Usher K, Durkin J, Bhullar N. The COVID-19 pandemic and mental health impacts. Int J Ment Health Nurs. 2020;29:315–318. doi: 10.1111/inm.12726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoib S, Nagendrappa S, Grigo O, Rehman S, Ransing R. Factors associated with COVID-19 outbreak-related suicides in India. Asian J Psychiatr. 2020;53:2018–2020. doi: 10.1016/j.ajp.2020.102223. [DOI] [PubMed] [Google Scholar]
- Shalvee Sambhav S. Role of mass media and communication during pandemic. Int J Creat Res Thoughts. 2020;8 3786–1790. [Google Scholar]
- Stack S. Media coverage as a risk factor in suicide. J Epidemiol Community Health. 2003;57:238–240. doi: 10.1136/jech.57.4.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Williams K. Influences of the media on suicide. Br Med J. 2002;325:1374–1375. doi: 10.1136/bmj.325.7377.1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar RP. Suicides related to the COVID-19 outbreak in India: A pilot study of media reports. Asian J Psychiatr. 2020;53 doi: 10.1016/j.ajp.2020.102196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dsouza DD, Quadros S, Hyderabadwala ZJ, Mamun MA. Aggregated COVID-19 suicide incidences in India: Fear of COVID-19 infection is the prominent causative factor. Psychiatry Res. 2020;290:17–20. doi: 10.1016/j.psychres.2020.113145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths MD, Mamun MA. COVID-19 suicidal behavior among couples and suicide pacts: Case study evidence from press reports. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113105. [DOI] [PubMed] [Google Scholar]
- Accidental Deaths & Suicides in India - 2019 | National Crime Records Bureau n.d. https://ncrb.gov.in/en/accidental-deaths-suicides-india-2019 (accessed September 6, 2020).
- Menon V, Subramanian K, Selvakumar N, Kattimani S. Suicide prevention strategies: An overview of current evidence and best practice elements. Int J Adv Med Heal Res. 2018;5:43. doi: 10.4103/ijamr.ijamr_71_18. [DOI] [Google Scholar]
- Coronavirus | How life changes post COVID-19 recovery - The Hindu n.d. https://www.thehindu.com/sci-tech/health/life-after-recovery-from-coronavirus-stigma-and-anxiety/article32702257.ece (accessed September 27, 2020).
- Indian doctors being evicted from homes over coronavirus fears | Coronavirus outbreak | The Guardian n.d. https://www.theguardian.com/world/2020/mar/30/indian-doctors-being-evicted-from-homes-over-coronavirus-fears (accessed September 27, 2020).
- ಕೊರೊನಾ: ನೆರೆಮನೆಯವರ ಅವಮಾನಕ್ಕೆ ನೊಂದು ವ್ಯಕ್ತಿ ಆತ್ಮಹತ್ಯೆ- Kannada Prabha n.d. https://www.kannadaprabha.com/karnataka/2020/jul/21/covid-ve-man-commits-suicide-after-humiliation-from-neighbors-424191.html (accessed September 27, 2020).
- Dharwad: ಧಾರವಾಡ: ನಾಲ್ಕು ವರ್ಷದ ಪುತ್ರಿಗೆ ಕೊರೊನಾ ಪಾಸಿಟಿವ್ ಎಂಬ ಭೀತಿ, ಪತ್ನಿ, ಮಗಳಿಗೆ ವಿಷ ನೀಡಿ ಆತ್ಮಹತ್ಯೆ - man gives poison to wife, kid, commits suicide in dharwad | Vijaya Karnataka n.d. https://vijaykarnataka.com/news/dharawada/man-gives-poison-to-wife-kid-commits-suicide-in-dharwad/articleshow/77164564.cms (accessed September 27, 2020).
- MoHFW Govt.ofIndia. The Mental Healthcare Act -2017. 2017:51. https://www.indiacode.nic.in/handle/123456789/2249?view_type=browse&sam_handle=123456789/1362 2017. accessed October 17, 2020. [Google Scholar]
- MoHFW . 2020. Guide to address stigma associated with COVID-19. GoI. [Google Scholar]
- Coronavirus Disease . September 2, 2020. COVID-19) Situation Reports.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports n.d. accessed. [Google Scholar]
- Pfefferbaum B, North CS. Mental Health and the Covid-19 Pandemic. N Engl J Med. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis. 2020;20:782. doi: 10.1016/S1473-3099(20)30498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thirthalli J, Manjunatha N, Math SB. Unmask the mind! Importance of video consultations in psychiatry during COVID-19 pandemic. Schizophr Res. 2020 doi: 10.1016/j.schres.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The United Nations Children's Fund Social stigma associated with the coronavirus disease (COVID-19) 2020;5 [Google Scholar]
- Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM An Int J Med. 2020:1–6. doi: 10.1093/qjmed/hcaa202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher L. Are COVID-19 survivors at increased risk for suicide? Acta Neuropsychiatr. 2020:13059. doi: 10.1017/neu.2020.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manoranjitham S, Jayakaran R, Jacob K. Suicide in India: The need for a national policy. Indian J Psychiatry. 2006;48:72. doi: 10.4103/0019-5545.31626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National_Health_Mental_Policy.pdf MoHFW G. Gov India; 2014. Minist Heal Fam Welfare. [Google Scholar]