Abstract
Background
Cessation of elective procedures and lower bed capacity during the COVID-19 pandemic have led to a rise in the waiting lists for surgery, but it is unclear if workload has recovered sufficiently to account for this backlog. We describe the change in neurosurgical workload at a tertiary neurosciences center in the United Kingdom after the first pandemic wave in comparison with the months before and during the first wave.
Methods
A retrospective review of theatre records and electronic referrals—between December 1, 2019, and August 31, 2020—was performed. The months of December 2019–February 2020 were designated as pre-COVID months and March–May 2020 were designated as COVID months. The time period from June to August 2020 was designated as post-wave months. Statistical analyses were performed on SPSS v22 (IBM).
Results
Referrals declined from 572 in January to a nadir of 352 in April before a steady rise to August. Referral volumes for degenerative spinal disease and traumatic brain injuries showed a statistically significant change during the year. On average, 212 procedures per month were performed in the pre-COVID months, 167 procedures per month during COVID months, and 232 procedures per month in the post-wave months. The number of patients on the waiting list for scheduled operations rose from March (785 patients) onward to a peak of 997 patients in July.
Conclusions
In the aftermath of COVID-19, higher referral volumes and operative procedures were apparent in the post-wave months as services returned to normal. With the expectation of a second wave of infections, it is unclear whether this will be sustainable.
Key words: COVID-19, Neurosurgery, Pandemics, Physicians' Practice Patterns, Referral and consultation, Workload
Introduction
The United Kingdom (UK) was severely affected by the first wave of the COVID-19 pandemic during the months of March–May 2020. As part of the national response to prioritize health care resources and reduce transmission, all elective operations were canceled1 and a nationwide lockdown2 was enforced in March. With the infection rates seemingly under control, the lockdown was gradually lifted3 in June and surgical services planned to return to “normality.”4 , 5
Worldwide, neurosurgeons had to contend with a drastic fall in operating volume,6, 7, 8 referrals,9 bed capacity,10 earnings,11 , 12 and a rise in illness13, 14, 15 during the pandemic. Furthermore, the cancellation of elective procedures has led to a significant increase in the waiting lists for surgery,16 and it is unclear if workload—after the lockdown was eased—has escalated sufficiently to be able to account for the backlog.17 Moreover, limited evidence is available from the neurosurgical literature on the recovery patterns seen in operative and referral volumes as the pandemic has eased.
Our aim is to describe the change in neurosurgical workload during the 3 months after the first pandemic wave (June–August 2020, inclusive) in comparison with before (December 2019–February 2020, inclusive) and during the first wave (March–May 2020, inclusive), as services returned to normal, in a tertiary neurosciences center in the UK.
Materials and Methods
Study Setting
Our institution is a Level I trauma center in England and offers neurosurgical services to a population of over 3 million people.18 A total of 71 inpatient neurosurgical beds are spread over 2 wards and a day surgery unit. Four neurosurgical operating theatres are run on weekdays, including a dedicated emergency theatre.
During the first wave, 1 inpatient 31-bedded ward was converted to a “COVID-19” ward and only 2 operating theatres were in use—1 for emergencies and 1 for pooled urgent and semielective cases. After the lockdown was lifted, both wards and the full complement of operating theatres were gradually brought into use. All patients admitted on an elective and emergency basis undergo testing for COVID-19 and are isolated until the results are available. Emergent and semiurgent procedures, in the context of a pending test result, were performed with adequate personal protective measures, and the patients were treated as if they were COVID-positive.
Data Collection
A retrospective review of theatre records and electronic referrals—between December 1, 2019, and August 31, 2020—was performed. Duplicate referrals were excluded. The months of December 2019–February 2020 were designated as pre-COVID months and March–May 2020 were designated as COVID months for comparison with the included dataset. The study period of June–August 2020 was designated as post-wave months.
Patient demographics, time and date of referral, referral diagnoses, and procedure types were captured on an Excel (Microsoft; Redmond, Washington, USA) spreadsheet. Referral diagnoses were categorized thus: 1) traumatic brain injuries (including acute subdural hematomas); 2) degenerative spinal diseases of the whole spine (including suspected or confirmed cauda equina syndrome); 3) intracranial and intradural spinal tumors; 4) spontaneous intra cerebral hemorrhage or ischemic stroke; 5) spontaneous subarachnoid hemorrhage and other neurovascular lesions (arteriovenous malformations, arteriovenous fistulae, unruptured aneurysms, etc.); 6) chronic subdural hematomas and subdural collections or hygromas; 7) hydrocephalus or shunt-related; 8) postoperative complications; 9) spinal fractures; 10) infections of the central nervous system (not postoperative); 11) Chiari or other hindbrain anomalies; 12) pituitary lesions; 13) congenital spinal lesions or spinal dysraphism; 14) congenital cranial lesions; and 15) spontaneous or traumatic cerebrospinal fluid leak. Operations were categorized as either cranial, including functional procedures, or spinal procedures.
Statistical analyses were performed on SPSS v22 (IBM; Armonk, New York, USA). Differences between monthly volumes were evaluated by χ2 goodness-of-fit tests; statistical significance was set at the 95% level (P = 0.05). Post hoc testing was performed using the Bonferroni correction.
Results
Referral Volume
In total, 1674 electronic referrals were received during the study period (June–August 2020). Median age was 60 years, and 52.4% of referred patients were female.
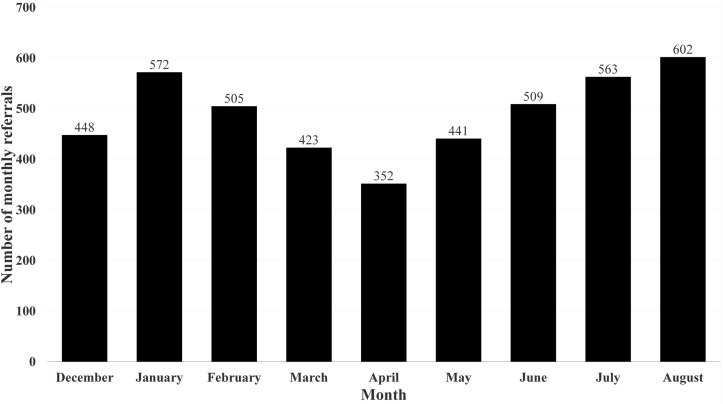
Figure 1 illustrates the total referrals received per month in the pre-COVID months, COVID months, and the current study period.
Figure 1.
Total referrals per month before (December–February), during (March–May), and after (June–August) the first wave of the COVID-19 pandemic.
There was a statistically significant difference in the referral volumes from December 2019 to August 2020 (χ2(8) = 107.793; P < 0.001) whereby referrals had declined in number from January onward to a nadir of 352 per month in April—at the height of the first wave—before the steady rise to August.
Referral volumes in the COVID months were lower than the pre-COVID month low of 448 per month in December, whereas referral volume in August was higher than the pre-COVID month high of 572 in January. In particular, the number of referrals received by our department progressively increased in number from June to August (χ2(2) = 7.817; P = 0.02), peaking at 602 referrals in August.
After categorizing referral volumes into the 3 time periods (pre-COVID months, COVID months, post-wave months), post hoc testing using the Bonferroni correction demonstrated statistically significant differences in referral volumes between each time period (pre-COVID months vs. COVID months, P < 0.001; pre-COVID months vs. post-wave months, P = 0.027; COVID months vs. post-wave months, P < 0.001).
Referral Patterns by Diagnosis
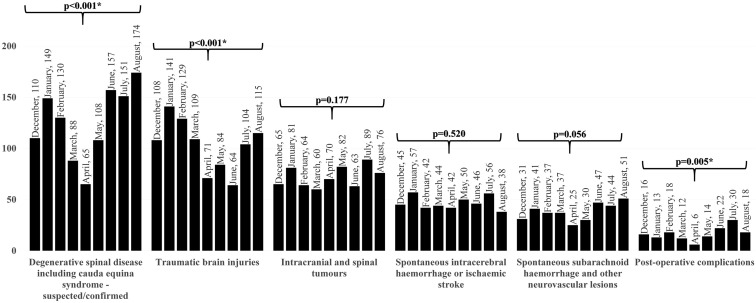
Figure 2 illustrates the change in referral volume by the 5 commonest diagnoses across the year, from the pre-COVID months, through the COVID months, and the current study period.
Figure 2.
Bar chart comparing the monthly referral volumes from December till August, for the 5 commonest diagnoses. Statistical significance in the differences in referral volumes between December and August is depicted above the bars and is highlighted with an asterisk where P < 0.05.
Between June and August, referrals for traumatic brain injuries increased by 79.7%, whereas referrals for intracranial/intradural tumors and degenerative spinal diseases rose by 20.6% and 10.8%, respectively. Referrals for hydrocephalus/shunt-related problems and subarachnoid hemorrhage also increased by 32.0% and 8.5%, respectively, between June and August. Referrals for degenerative spinal diseases were higher in all the post-wave months in comparison with pre-COVID months. Similarly, referrals for stroke syndromes, subarachnoid hemorrhage, and postoperative complications were also higher in all the post-wave months compared with the pre-COVID months. Intracranial and intradural spinal tumor referrals were also more commonly seen in July and August in comparison with the pre-COVID months. On the other hand, referrals for traumatic brain injuries were lower in all the post-wave months compared with pre-COVID months.
Comparing referral volume from December till August showed a statistically significant change in referral numbers for degenerative spinal diseases, traumatic brain injuries, and postoperative complications (Figure 2).
Operative Volumes and Waiting List
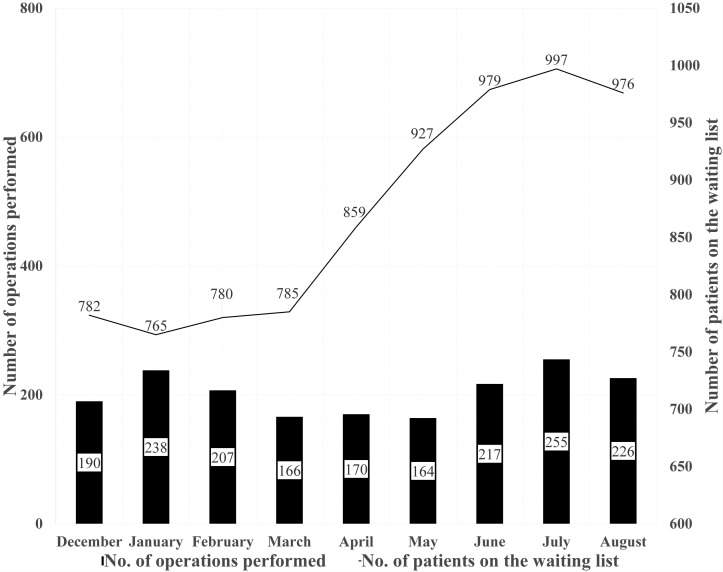
Figure 3 illustrates the total operations performed per month and the number of patients on the waiting list in the pre-COVID months, COVID months, and the current study period.
Figure 3.
A graph demonstrating the pattern in total operative volume (black bars) and the number of patients on the waiting list (black line) during the pre-COVID months (December–February), COVID months (March–May), and post-wave months (June–August).
A total of 698 procedures were performed during the study period between June and August, inclusive. On average, 212 procedures per month were performed in the pre-COVID months, 167 procedures per month during COVID months, and 232 procedures per month in the post-wave months. The χ2 goodness-of-fit testing revealed a statistically significant difference in the number of operations performed per month between December and August (χ2(8) = 43.277; P < 0.001). Post hoc testing using the Bonferroni correction showed a statistically significant difference between operative volumes in the pre-COVID months and COVID months (P < 0.001), and between COVID months and post-wave months (P < 0.001). During the study period, operations increased from a nadir of 164 in May to a peak of 255 in July. The number of operations performed during any of the post-wave months was higher than that in the COVID months and any of the pre-COVID months (except January).
There was also a significant difference in the number of patients on the waiting list for scheduled operations between December and August (χ2(8) = 87.897; P < 0.001). Post hoc testing demonstrated statistically significant differences in the number of patients on the waiting list between all 3 time periods (pre-COVID months vs. COVID months, P = 0.002; pre-COVID months vs. post-wave months, P < 0.001; COVID months vs. post-wave months, P < 0.001).
The number of patients on the waiting list rose continuously from March (785 patients) onward to a peak of 997 patients in July—an increase of 27.0%. This contrasted with the much slower rise in the waiting list from January till March (2.61% increase). Furthermore, 63 operations were postponed between March and May and subsequently added to the backlog of patients awaiting surgery in the post-wave months.
Discussion
We have described the workload changes at a busy neurosurgical department in the UK in the aftermath of the first wave of the COVID-19 pandemic.
Spinal Neurosurgery
As expected, with the resumption of normal activity, referral and operative volumes increased in the post-wave months of June–August. Multiple authors have commented on the drastic fall in spinal presentations during the COVID months.19, 20, 21, 22 Reluctance or difficulty in seeking medical attention and cessation of manual labor activities may be relevant factors in the fall in spinal pathologies. Cancellation of elective spinal surgeries23 during the pandemic was associated with an increase in the surgical waiting list backlog, and the steep rise in referrals in the post-wave months may reflect this cohort seeking our services to alleviate their symptoms.
Trauma
The pandemic and associated lockdown restrictions were associated with a drop in road traffic accidents.24 , 25 Consequently, referrals for traumatic head injuries were low during the COVID months, and although the referral volumes have increased in the post-wave months, they have yet to reach the same volumes as the pre-COVID months. This could reflect altered working patterns as the public may have continued to work from home despite the relaxation of travel restrictions. Higher unemployment rates26 because of the pandemic may have also reduced road traffic. The study period, in normal circumstances, is also the university and school holiday season during which there is a lower incidence of road traffic accidents anyway.
Other Relevant Referral Patterns
The fall in stroke presentations during the pandemic is well described,27 and the rise in these referrals during the post-wave months is likely to represent a recovery in the stroke presentation rates. Referrals for postoperative complications demonstrated a significant change across the year from December to August, and more referrals in this category were seen in the post-wave months compared with the pre-COVID months. This could reflect operated patients' reluctance to attend hospital during the pandemic for what may be perceived as a trivial wound issue.
Changes in Operative Volume
With the backlog of operations vastly increased (Figure 3), post-pandemic operating volumes need to be much higher to help clear the elective surgery waiting list.17 However, limitations in, and competition for, theatre space, staff sickness, and the risk of postoperative COVID-19 infection5 , 28 will likely mean that operative volumes will not be able to reach the levels required to help clear the backlog over the next several months and the waiting list may continue to increase.
Since the start of the COVID-19 pandemic, neurosurgical workload has changed considerably with higher referral numbers and operative procedures undertaken in the post-wave months as services return to normal. With the expectation of a second wave of infections29 , 30—especially as schools and universities reopen31—it is unclear whether this will be sustainable. Future work should involve multicenter collaborative efforts to identify similarities, if any, in workload patterns at other neurosurgical centers in order to develop a common strategy for the referrals and operative backlog that threatens to swamp neurosurgery in the post-COVID world.
Strengths and Limitations
This study is, to the best of our knowledge, the first to describe the changes in referral and operative volumes in neurosurgery as the COVID-19 pandemic wanes. Patterns described here can be useful and act as a reference for future pandemic planning. Limitations include the retrospective nature of the study while the accuracy of data extraction from databases can be limited by suboptimal data input.
Conclusions
We report the change in the referral patterns, operative volumes, and the waiting list in the pre-COVID, COVID, and post-wave months, and these patterns are indicative of the likely workload for the future as services return to normal. The volume of referrals, especially for degenerative spinal diseases, and the operative volumes increased as patients returned to seek our services.
CRediT authorship contribution statement
Ahmed Nabil ElGhamry: Conceptualization, Methodology, Investigation, Formal analysis, Writing - original draft. Nithish Jayakumar: Conceptualization, Methodology, Investigation, Formal analysis, Writing - original draft, Visualization. Mohamed Youssef: Methodology, Investigation, Validation, Writing - review & editing. Syed Shumon: Methodology, Investigation, Validation, Writing - review & editing. Patrick Mitchell: Conceptualization, Methodology, Writing - review & editing, Supervision.
Footnotes
Conflict of interest statement: The author declares that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.BBC News £350bn to help UK firms, while operations delayed. March 17, 2020. https://www.bbc.com/news/uk-51933410 Available at:
- 2.Stewart H., Mason R., Dodd V. Boris Johnson orders UK lockdown to be enforced by police. The Guardian. March 23, 2020. https://www.theguardian.com/world/2020/mar/23/boris-johnson-orders-uk-lockdown-to-be-enforced-by-police Available at:
- 3.BBC News Coronavirus: lockdown to be relaxed in England as 2m rule eased. June 23, 2020. https://www.bbc.co.uk/news/uk-53152416 Available at:
- 4.NHS England NHS roadmap to safely bring back routine operations. https://www.england.nhs.uk/2020/05/nhs-roadmap/ Available at:
- 5.Royal College of Surgeons Recovery of surgical services during and after COVID-19. https://www.rcseng.ac.uk/coronavirus/recovery-of-surgical-services/ Available at:
- 6.Patel P.D., Kelly K.A., Reynolds R.A., et al. Tracking the volume of neurosurgical care during the coronavirus disease 2019 pandemic. World Neurosurg. 2020;142:e183–e194. doi: 10.1016/j.wneu.2020.06.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jean W.C., Ironside N.T., Sack K.D., Felbaum D.R., Syed H.R. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir (Wien) 2020;162:1229–1240. doi: 10.1007/s00701-020-04342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bajunaid K., Alatar A., Alqurashi A., et al. The longitudinal impact of COVID-19 pandemic on neurosurgical practice. Clin Neurol Neurosurg. 2020;198:106237. doi: 10.1016/j.clineuro.2020.106237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jayakumar N., Kennion O., Villabona A.R., Paranathala M., Holliman D. Neurosurgical referral patterns during the coronavirus disease 2019 pandemic: a United Kingdom experience. World Neurosurg. 2020;144:e414–e420. doi: 10.1016/j.wneu.2020.08.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mathiesen T., Arraez M., Asser T., et al. A snapshot of European neurosurgery December 2019 vs. March 2020: just before and during the Covid-19 pandemic. Acta Neurochir (Wien) 2020;162:2221–2233. doi: 10.1007/s00701-020-04482-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Venkataram T., Goyal N., Dash C., et al. Impact of the COVID-19 pandemic on neurosurgical practice in India: results of an anonymized national survey. Neurol India. 2020;68:595–602. doi: 10.4103/0028-3886.289004. [DOI] [PubMed] [Google Scholar]
- 12.Sivakanthan S., Pan J., Kim L., Ellenbogen R., Saigal R. Economic impact of COVID-19 on a high-volume academic neurosurgical practice. World Neurosurg. 2020;143:e561–e566. doi: 10.1016/j.wneu.2020.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaurasia B., Deora H., El-Ghandour N.M.F., et al. In memoriam: a memoir for our fallen “heroes. Neurosurgery. 2020;87:854–856. [Google Scholar]
- 14.Sharif S., Amin F., Hafiz M., et al. COVID 19-depression and neurosurgeons. World Neurosurg. 2020;140:e401–e410. doi: 10.1016/j.wneu.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deora H., Mishra S., Tripathi M., et al. Adapting neurosurgery practice during the COVID-19 pandemic in the Indian subcontinent. World Neurosurg. 2020;142:e396–e406. doi: 10.1016/j.wneu.2020.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The Royal College of Surgeons of England Covid ‘wrecking ball’ through NHS waiting times. https://www.rcseng.ac.uk/news-and-events/media-centre/press-releases/covid-wrecking-ball-through-nhs-waiting-times/ Available at:
- 17.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newcastle Hospitals. Trust profile. https://www.newcastle-hospitals.org.uk/about-us/trust-profile.html Available at:
- 19.Brembilla C., Veiceschi P., Fanti A., et al. The eclipse of degenerative spine pathology during COVID-19 pandemic. Neurospine. 2020;17:354–356. doi: 10.14245/ns.2040268.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ham C.H., Moon H.J., Kim J.H., Park Y.-K., Lee T.H., Kwon W.-K. Coronavirus disease (COVID-19) outbreak and its impact on spinal daily practice: preliminary report from a single (regional) university hospital in Republic of Korea. J Korean Neurosurg Soc. 2020;63:407–414. doi: 10.3340/jkns.2020.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Agosti E., Giorgianni A., Locatelli D. Impact of COVID-19 outbreak on spinal pathology: single center first impression. Spinal Cord. 2020;58:726–727. doi: 10.1038/s41393-020-0480-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cofano F., Tartara F., Zenga F., Penner F., Lanotte M., Garbossa D. Letter: Back pain and accesses to emergency departments during COVID-19 lockdown in Italy. Neurosurgery. 2020;87:E211. doi: 10.1093/neuros/nyaa174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mehta A.I., Chiu R.G. COVID-19 non-essential surgery restrictions and spine surgery: a German experience. Spine (Phila Pa 1976) 2020;45:942–943. doi: 10.1097/BRS.0000000000003571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Qureshi A.I., Huang W., Khan S., et al. Mandated societal lockdown and road traffic accidents. Accid Anal Prev. 2020;146:105747. doi: 10.1016/j.aap.2020.105747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cardwell M. Huge drop in car crashes as drivers stay home amid coronavirus lockdown. Express & Star. https://www.expressandstar.com/news/2020/05/04/car-crashes-drop-by-65-per-cent/ Available at:
- 26.Rojas J.-P.F. Coronavirus: unemployment rate climbs as pandemic takes toll. Business News | Sky News. https://news.sky.com/story/coronavirus-unemployment-rate-climbs-as-pandemic-takes-toll-12072250 Available at:
- 27.July J., Pranata R. Impact of the coronavirus disease pandemic on the number of strokes and mechanical thrombectomies: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2020;29:105185. doi: 10.1016/j.jstrokecerebrovasdis.2020.105185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet Lond Engl. 2020;396:27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grech V., Cuschieri S. COVID-19: a global and continental overview of the second wave and its (relatively) attenuated case fatality ratio. https://doi.org/10.1016/j.earlhumdev.2020.105211 [e-pub ahead of print]. Early Hum Dev. [DOI] [PMC free article] [PubMed]
- 30.Zali A., Ashrafi F., Ommi D., Behnam B., Arab-Ahmadi M. The deadly cost of ignorance: the risk of second wave of COVID-19. Asia Pac J Public Health. 2020;32:511–512. doi: 10.1177/1010539520957809. [DOI] [PubMed] [Google Scholar]
- 31.Grech V., Grech E., Borg Myatt J. Holidays over: a review of actual COVID-19 school outbreaks up to September 2020. https://doi.org/10.1016/j.earlhumdev.2020.105206 [e-pub ahead of print]. Early Hum Dev. [DOI] [PMC free article] [PubMed]