Abstract
Purpose of review
Botulinum neurotoxin A (BoNT/A), or Botox, is a popular option for overactive bladder (OAB) and neurogenic bladder (NGB) with or without incontinence. This review aims to discuss the clinical outcomes of BoNT in adult and pediatric bladder conditions, and introduces the potential benefit of novel, engineered neurotoxins beyond BoNT/A.
Recent findings
A large volume of evidence supports the use of Botox for OAB (to reduce urgency, frequency and incontinence episodes), and for NGB (to decrease incontinence and improve bladder capacity and detrusor pressures). Botox is now also Food & Drug Administration (FDA)-approved for pediatric neurogenic detrusor overactivity. However, urinary retention, diminished response over time and treatment failures are prevalent issues with Botox. Modifying natural BoNTs or forming chimeric toxins are alternatives to BoNT/A that may have higher efficacy and lower side-effect profile. One example is BoNT/Bmy-ww. This novel engineered toxin binds to a more commonly expressed synaptotagmin receptor, with potentially more potent paralytic effect and less capacity for systemic diffusion.
Summary
Novel engineered neurotoxins may be the next frontier in OAB and NGB therapy.
Keywords: botulinum neurotoxin, engineered neurotoxin, neurogenic bladder, overactive bladder
INTRODUCTION
Since their Food & Drug Administration (FDA) approval 7 years ago, botulinum neurotoxins (BoNTs) have gained immense popularity in the treatment of overactive and neurogenic bladder (NGB). Supported by an abundance of clinical efficacy data, Botox is now a mainstay in treatment algorithms in both European and American Urologic Society Guidelines. BoNTs are a family of highly potent toxins, and as humans are not routinely vaccinated against BoNTs, these toxins can be used for therapeutic purposes [1■]. There are seven BoNT serotypes, but in urology, treatment of overactive bladder (OAB) or neurogenic bladder (NGB) has most commonly relied on onabotulinumtoxinA (BoNT/A), known as Botox (Allergan, Irvine, CA). Other commercially available BoNT/A products for the bladder include Dysport (Ipsen, Slough, UK) and Xeomin (Merz Pharma, Frankfurt, Germany).
In this review, we briefly discuss the clinical use of BoNT for the bladder and highlight the limitations therein. We then discuss toxin mechanisms and receptor targets, so as to introduce the potential of novel, engineered neurotoxins beyond BoNT/A.
CLINICAL INDICATIONS AND OUTCOMES
The two most well-studied indications for BoNT/A have been for bladder-level conditions. The first, OAB (urgency, frequency and nocturia, with or without incontinence), has significant negative impacts on quality of life and sexual function [2-5]. In a recent study of over 9000 women, bothersome OAB was found in half of women aged 55–64, with incidence increasing with advancing age and BMI [6]. Guidelines for OAB treatment recommend a tiered approach of options with increasing invasiveness, reversibility and side-effect profile [7■]. For patients who are refractory to behavioral therapy, oral anti-muscarinic or α-3 agonist agents, whether because of noncompliance from side-effects or from a lack of clinical response, third-tier options include detrusor BoNT/A administration [8]. The aim is to target sensory and motor nerve endings running under the luminal surface of the bladder wall [9].
Numerous studies have shown the efficacy and cost-effectiveness of BoNT/A, even as a first-line agent [10]. Since the initial clinical work by Schurch et al. [11], several placebo-controlled trials have been conducted to validate the efficacy and tolerability of BoNT/A [12-16]. As a whole, patients have reduced urgency, frequency, incontinence episodes, nocturia and pad usage, [17,18■], as well as improved urodynamic parameters [15]. Importantly, quality of life, sexual function and satisfaction improved with treatment compared to placebo [19,20], with the majority of patients opting for retreatment with injections if needed [21].
The second FDA-approved indication for BoNT/A is in detrusor overactivity incontinence from an underlying neurologic condition. Management of the lower urinary tract in the setting of spinal cord injury, spinal dysraphism or degenerative neurologic disease [i.e. multiple sclerosis (MS)] employs the same principles as anticholinergic manipulation in OAB. The goals of NGB management are to achieve a low pressure, high-volume reservoir without incontinence and to maintain safe intravesical pressures to preserve renal function, and reduce the morbidity of NGB [22].
Although the spectrum of lower urinary tract dysfunction ranges from detrusor level (areflexia and hyperreflexia) to bladder outlet level (incompetent, fixed or dyssynergic sphincter) problems, BoNT/A has been most effective in improving detrusor overactivity and compliance [23]. For those patients with persistent incontinence between catheterizations, or with bothersome OAB symptoms, BoNT/A injections provide urinary continence, enhanced bladder capacity and lower detrusor pressures on urodynamics, with minimal side-effects and high patient satisfaction [11]. These findings were validated and reproduced in several randomized, placebo-controlled trials, with injections of 200–300U [24,25,26■,27]. In one international, multicenter, double-blind placebo-controlled trial studying NGB-related detrusor overactivity, injections of 200–300U of BoNT/A decreased the mean incontinence episodes by 21–23 per week (from a baseline of 32 episodes), compared to a 9 episode per week reduction in the placebo group. Bladder capacity and detrusor pressures improved as well, and the treatment effect lasted approximately 250 days before a request for retreatment [26■]. These trials, among others, also showed an improvement in quality of life [26■,28]. As seen in OAB treatment, therapeutic benefit of BoNT/A wears off over time, requiring repeat injections. In addition, not all patients respond to BoNT/A for symptom or detrusor pressure improvement, whether from tolerance against the medication or from unwanted side-effects.
BoNT/A use in pediatric patients with neurogenic detrusor overactivity (NDO) was approved by the FDA in June 2020. In general, cohort studies using BoNT/A in pediatrics, for indications similar to adult patients, have produced promising results [29-31]. However, outcomes have not been as successful as in adults. For refractory OAB, children receiving weight-based doses of BoNT/A expectedly have improvements in bladder capacity, a decrease in urinary frequency and incontinence episodes, as well as satisfaction [32-34]. Repeat injections are safe [35], and long-term follow up of up to 35.4 months, across multiple cohorts, showed that a third of patients respond completely, whereas the rest require continued oral anticholinergic therapy or repeated injections to control their symptoms, despite initial BoNT/A injection.
In the pediatric myelomeningocele patient with NGB, studies have shown that BoNT/A may offset or delay the need for augmentation enterocystoplasty in patients with unsafe detrusor pressure or refractory detrusor overactivity incontinence [36-38]. As a composite, 293 pediatric spina bifida patients across 12 publications were analyzed in a systematic review by the French Referral Network of Spina Bifida [39]. Rates of incontinence resolution ranged from 32 to 100%, detrusor pressures decreased by 32–54%, cystometric capacities increased from 27 to 162% and compliance improved from 28 to 176%. A multicenter, randomized, double-blind study that supported the recent FDA approval of BoNT/A for urinary incontinence in patients with NDO showed a decrease in mean incontinence episodes by 1.0–1.4 from a baseline of 2.5–3.5 per day, and first morning catheterization (or capacity) increased by 20–60 mL at week 2, and up to 70 mL by week 6. More than two thirds of patients had a positive response to a single injection at 6 and 12 weeks. Detrusor pressures decreased, especially with higher doses (12cmH2O decrease at 50U, 20cmH2O at 100U and 25cmH2O at 200U), and retreatment requests ranged from 24 to 30 weeks (unpublished data).
ISSUES WITH BOTULINUM NEUROTOXIN A
Although well tolerated overall, BoNT/A is not without adverse outcomes, such as urinary tract infection, urinary retention and gross hematuria [40]. Urinary retention is a toxin-specific result, and often necessitates temporary intermittent catheterization until toxicity subsides. For the sensate patient, this is problematic. In adult idiopathic and refractory OAB, 100U of BoNT/A causes a retention rate of 5–10%, with increasing rates from dose escalation [16,18■,41■]. Very few patients report signs of systemic toxicity (dry mouth, dysphagia, impaired vision and muscle weakness), and when present, are usually self-limiting [42]. In the MS population, however, 7–10% of patients had bothersome muscle weakness, compared to 3.8% on placebo [26■]. For adult spinal cord injury patients, this rate was 0–1%, but the relative risk of weakness compared to placebo was 2.59 (95% CI, 1.36–4.91, P = 0.004) [43].
Long-term data show a durable response to treatment of OAB at 3 months, with 93% of patients reporting continued response. However, this percentage diminishes to 67% and 20%, at 6 and 9 months, respectively [14]. In other reports of more than 5-year follow up, 70% of patients had discontinued treatment; 27% because of insufficient therapeutic effect or tachyphylaxis, and 43% from tolerability issues. Seventy-nine percentage stopped treatment after the first injection, and 19% after the second injection [44].
Pediatric NGB treatment with BoNT/A does not appear as durable as in adults. In the nonneurogenic, idiopathic OAB child, only 30–60% respond to their first injection, with the rest needing at least a second injection at 6 months because of partial or no response [34,45]. In some studies, 40% of children remained symptomatic even after initial BoNT/A injection, and those with poor compliance do not have satisfactory improvement to incontinence [46]. In fact, up to 21.7% of low compliance bladders are deemed as nonresponders [47]. Failure rates of BoNT/A were 28.9% after 7 years of follow up, with only 58% of patients still undergoing treatment at that time. Those prone to failure had severe NDO [48]. Unpublished data from our institution show only a 38% composite improvement rate in incontinence and/or urodynamic parameters for patients with spinal dysraphism.
In a 2018 study, half of first-time responders only had clinical symptom improvement, without urodynamic changes. The remaining 34% did have predictable capacity and compliance improvement after one injection, which was unfortunately not seen in those with poor compliance. At a follow up of 3.7 years, 43.4% of patients (23 of 53) had to undergo augmentation [49]. Khan et al. [50] report a 27% rate of augmentation enterocystoplasty for pediatric NGB as well. Animal models with NGB suggest that BoNT/A still helps with reduction in fibrosis and muscle hyperplasia, explaining the effect seen in some patients [51,52].
In general, reasons for treatment failure may include issues with Botox storage, reconstitution, administration or inadequate dosing. The problem may also be specific to BoNT/A for bladder-level disorders. Management of nonresponders is troublesome, and may include subjecting patients to repeat injections, switching BoNT/A preparations (i.e. abo-, ona-BoNT/A), or serotypes (i.e. BoNT/B), adding multiple anticholinergic agents or proceeding to more definite treatment, such as diversion or augmentation [53,54]. Adding subsequent bladder injections does not increase efficacy. Alternatives to direct injections of BoNTs via transurethral electromotive drug administration have had mixed, and nonreproducible, results [55,56]. Anatomically, the urothelial layer is semi-impermeable, which may reduce efficacy rates. To bypass this, promising techniques like ion triggered liposomal delivery systems are currently under trial.
Identifying those who may not respond to a second injection, particularly in children, is important for a decision algorithm. Brain-derived neurotrophic factor, as a urinary marker, may potentially identify which patients have failed initial Botox therapy, without the need for invasive urodynamics, which would be helpful to redirect treatment strategy [57].
NOVEL, ENGINEERED TOXINS BEYOND BOTULINUM NEUROTOXIN A
Advances in novel, engineered toxins beyond BoNT/A may hold a more promising solution. Ultimately, the aim is to have a toxin that has a longer duration of effect (thereby reducing the need for repeated cystoscopy), with minimal side-effects or systemic diffusion, at the lowest possible dose.
Understanding the BoNT mechanism and receptor targets is critical to the development of novel toxins. Briefly, BoNTs are produced by anaerobic spore-forming Clostridium and related species, and the overall structure comprises of a 150-kDa protoxin with three functional domains: a 50-kDa zinc protease domain comprises the N-terminal light chain, and a translocation and receptor binding domain constitutes the C-terminal 100-kDa heavy chain [1■]. Normally, parasympathetic, nicotinic efferent fibers via the pelvic nerve (S2–S4) release acetylcholine to induce bladder contractions. In the myogenic theory of OAB, irregular or excessive release of acetylcholine onto the detrusor smooth muscle fibers is considered, in part, the underlying issue. With BoNT/A injections, the toxin binds to receptors at the presynaptic membrane and enters neurons via receptor-mediated endocytosis. Once inside the endosome, acidic conditions trigger conformational changes to the toxin, leading to translocation of the light chain across the endosomal membrane into the cytosol. There, the active light chain cleaves SNARE proteins (either syntaxin 1, SNAP-25, or VAMP1–3 depending on the BoNT serotype), which prohibits synaptic vesicles from fusing with the presynaptic membrane and releasing neurotransmitters [58]. This results in smooth muscle relaxation.
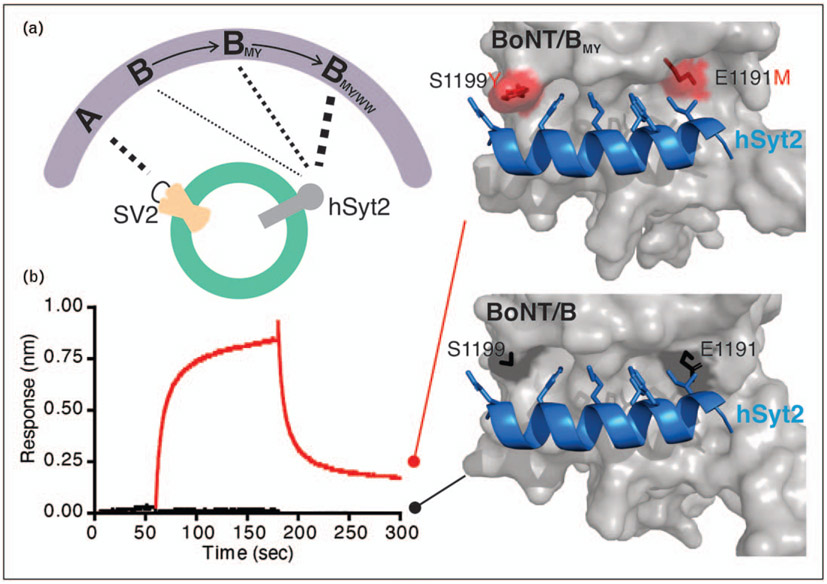
There are two main receptors for BoNT on the presynaptic terminal. The first are gangliosides, and the second are protein-based receptors, including synaptic vesicle protein 2 (SV2) or synaptotagmin 1 and 2 (Syt-1 and Syt-2) [59■,60-66]. These receptors are located on the synaptic vesicle, and when fused with the presynaptic membrane during neurotransmitter release, they are temporarily exposed to the synaptic cleft. This transient exposure allows BoNT binding and entry into the neuron via endocytosis. BoNT/Abinds Sv2, whereas BoNT/B binds Syt-1 or -2 (Fig. 1a). Expression of a specific receptor can vary in different tissues and neurons, which dictates the tissue sensitivity to BoNT.
FIGURE 1.
Engineering of BoNT/B to enhance receptor binding. (a) Evolution of BoNT/B engineering to gain higher binding affinity to human Syt-2. Unlike BoNT/A, which adopts SV2 as receptor, BoNT/B enters neurons by targeting Syt-1 and Syt-2. The thickness of band between toxin and receptor correlates to the degree of interaction. (b) Demonstration of enhancement of interaction between BoNT/Bmy and human Syt-2 on a molecular level. Biolayer interferometry assays show significant increase in the interaction between BoNT/B and human Syt-2 by introducing two mutations (E1191M/S1199Y), whereas naturally occurring BoNT/B exhibits minimal interaction. The enhancement of binding between BoNT/Bmy and human Syt-2 is endued through hydrophobic interactions generated by mutated amino acids, along with substituting two residues in a loop region of BoNT/B to tryptophan.
The structure–function relationship between BoNT serotypes and their receptors is an important prerequisite to developing novel toxins. Attempts to improve BoNT/A have already been conducted. López de la Paz et al. [67] modified BoNT/A to improve its half-life, and Stone et al. [68] created a BoNT/A formulated in a novel fashion to limit the extent of diffusion beyond the site of injection. However, there are other toxin serotypes available, targeting other receptors besides SV2, with potentially more dramatic improvements.
Notably, neuron expression of Syt-1/2 is greater than SV2, so targets to Syt (such as BoNT/B) could theoretically be more effective [69]. This concept has been confirmed by a chimeric toxin approach, for instance, where a part of BoNT/A receptor-binding domain is replaced with the corresponding region of BoNT/B. This chimeric toxin has a four-fold increase in potency on mouse diaphragm paralysis compared with natural BoNT/A [70]. Among the two Syt receptors, Syt-2 is the dominant receptor for BoNT/B at the neuromuscular junction [71]. However, human Syt-2 has a residue difference at the binding site that weakens the receptor–toxin interaction [64,72]. As such, 60–100-fold greater doses of BoNT/B are required to reach the therapeutic efficacy of BoNT/A for paralyzing skeletal muscles. This undoubtedly increases side-effects, systemic diffusion, and potentially neutralizing antibody formation. No doubt, when used for OAB, natural BoNT/B showed less efficacy and a shorter duration of response [73-75]. As natural BoNT/B suffers from low potency toward human Syt-2 receptors, the creation of an engineered toxin that improves binding of BoNT/B to its receptor would drastically improve efficacy.
In 2017, Tao et al. [76■■] developed a novel, engineered toxin that restores high affinity binding to human Syt-2 receptors, termed BoNT/Bmy [77■■]. This mutant toxin contains changes at two amino acids within its receptor-binding domain (E1191M/S1199Y), which compensates for the residue change seen in human Syt-2 (Fig. 1b). In addition, this mutant toxin also showed enhanced binding to human Syt-1 as well [76■■]. The effectiveness of this mutant toxin is further validated recently using a humanized mouse model, in which the toxin binding region of Syt-2 is replaced with the human Syt-2 sequence. As expected, natural BoNT/B showed a lower potency than BoNT/A for paralyzing skeletal muscles in humanized mice, whereas BoNT/Bmy showed a much-enhanced potency than natural BoNT/B, reaching levels similar to BoNT/A [77■■].
Most recently, an additional improvement of BoNT/B binding to neurons has been achieved by introducing mutations that augment toxin binding to lipid membranes [78■■]. It was found that BoNT/B contains a loop structure within its receptor-binding domain, which is located between the Syt and ganglioside receptor [79,80]. This loop is in an ideal location that may interact with cell membranes. The sequence of natural BoNT/B within this loop, however, is less than ideal for interacting with lipid membranes. By changing two amino acids located at the tip of this loop with tryptophan, a mutant toxin (designated BoNT/Bww) was created [78■■]. Without altering the overall structure, BoNT/Bww enhances binding to neurons by adding a third interaction with the cell surface besides binding to gangliosides and Syt receptors. This newly enhanced binding to lipid membranes itself is not strong enough to result in nonspecific binding of toxins to other cell types, as stable binding to cells still requires the cobinding to gangliosides and Syt receptors. On the contrary, the lipid membrane interaction can retain the mutant toxin onto neuronal surfaces longer than natural BoNT/B, thus elevating entry of the mutant toxin into neurons and reducing toxin diffusion.
A composite mutant toxin containing both mutations, BoNT/Bmy-ww, has also been created. In-vivo studies of rodents injected with BoNT/Bmy-ww revealed less body weight loss (a surrogate for systemic diffusion and toxicity), along with a far longer paralytic effect compared with BoNT/Bmy (23 days compared to 15 days) [78■■]. These important residue changes provide key advantages, allowing for less toxin to be injected, reducing the chance of triggering an immune response and enhancing the binding by allowing more toxin to enter the pre-synaptic membrane efficiently.
The role of novel toxins to OAB and NGB management lies in that BoNT/Bmy shows a higher potency than BoNT/A for paralyzing bladder tissues [77■■]. In contrast to skeletal muscles, where Syt-2 is the dominant receptor, Syt-1 appears to be the major BoNT/B receptor in the bladder. Therefore, future improvement in enhancing BoNT/B binding to human Syt-1 may further improve the efficacy of BoNT/B on bladder tissues. Finally, improved BoNT/B receptor-binding domain can be utilized to replace the receptor-binding domain of BoNT/A to generate a chimeric toxin that can combine the advantage of BoNT/A and BoNT/B.
In addition to the classic BoNTs, in 2017, a novel BoNT-like toxin was characterized, termed BoNT/X. Its light chain not only cleaves VAMP at a site unique from other BoNTs, but it is also capable of cleaving noncanonical additional VAMP family proteins, such as VAMP4, 5 and Ykt6 that no other BoNTs can cleave [81]. More recently, another novel BoNT-like toxin was isolated from Enterococcus faecium, the first non-clostridial toxin of its kind. Named BoNT/En, this also cleaves VAMP at a unique site, and it is the only toxin known that can simultaneously cleave both VAMP and SNAP-25 [82]. These BoNT-like toxins do not appear to target mammalian neurons, but chimeric toxins can be created by replacing their receptor-binding domains with the receptor-binding domain of a classic BoNT. The resulting chimeric toxins have been shown to paralyze mice efficiently, providing a way to utilize the unique capability of these BoNT-like toxins for modulating neuronal activities, although their therapeutic potential remains to be explored.
CONCLUSION
Management of refractory OAB, or detrusor overactivity incontinence in NGB patients, currently relies on BoNT/A therapy. Most nonneurogenic patients benefit greatly from detrusor injections, with minimal side-effects, but the result in NGB is less durable, especially in children. Engineered toxins, such as BoNT/Bmy-ww, have enhanced efficacy that may serve as next-generation options in the management algorithm of OAB and NGB patients.
KEY POINTS.
BoNT/A (Botox) is widely accepted in the treatment of overactive and NGB, but outcomes are variable, and a large portion of patients fail to respond to treatment.
Novel botulinum toxins may offer an alternative to BoNT/A. Toxins engineered through select residue changes, or the characterization of new and chimeric toxins, have higher potency, efficacy and less side-effects in preclinical studies.
These next-generation toxins may be suitable for urologic indications, and warrant further, expeditious evaluation.
Acknowledgements
The authors would like to thank Dr Rosalyn Adam for her guidance with the review.
Financial support and sponsorship
This work was supported by the National Institutes of Health (NIH) T32 Grant [DK060442–16], American Urologic Association & Urology Care Foundation Research Scholar Award and the Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction Chemodenervation Grant. In addition, M.D. acknowledges support from the NIH [R01NS080833 and R21NS106159], and M.D. holds the Investigator in the Pathogenesis of Infectious Disease award from the Burroughs Wellcome Fund.
Footnotes
Conflicts of interest
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
■ of special interest
■■ of outstanding interest
- 1. ■.Dong M, Masuyer G, Stenmark P. Botulinum and tetanus neurotoxins. Annu Rev Biochem 2019; 88:811–837.This review provides a state-of-the-art summary of botulinum and tetanus neurotoxins, both naturally occuring and engineered, with a focus on toxin structure, mechanisms and potential therapeutic applications.
- 2.Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 2010; 29:4–20. [DOI] [PubMed] [Google Scholar]
- 3.Coyne KS, et al. The impact of urinary urgency and frequency on health-related quality of life in overactive bladder: results from a National Community Survey. Value Health 2004; 7:455–463. [DOI] [PubMed] [Google Scholar]
- 4.Balzarro M, Rubilotta E, Mancini V, et al. Impact of Overactive Bladder-Wet Syndrome on Female Sexual Function: A Systematic Review and Meta-Analysis. Sex Med Rev 2019; 7:565–574. [DOI] [PubMed] [Google Scholar]
- 5.Kim A, et al. Health related quality of life in patients with side-effects after antimuscarinic treatment for overactive bladder. Low Urin Tract Symptoms 2017; 9:171–175. [DOI] [PubMed] [Google Scholar]
- 6.Robinson D, Åkervall S, Wagg A, et al. Prevalence and predictors of overactive bladder in nonpregnant nulliparous women below 65 years of age. Int Urogynecol J 2018; 29:531–537. [DOI] [PubMed] [Google Scholar]
- 7. ■.Gormley EA, et al. Diagnosis and treatment of overactive bladder (nonneurogenic) in adults: AUA/SUFU guideline. J Urol 2012; 188(6 Suppl): 2455–2463.This society guideline on nonneurogenic detrusor activity provides comprehensive evidence on the management and treatment outcomes for patients, via a tiered approach to therapy.
- 8.Amundsen CL, et al. Two-year outcomes of sacral neuromodulation versus onabotulinumtoxinA for refractory urgency urinary incontinence: a randomized trial. Eur Urol 2018; 74:66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Purves JT, et al. A three dimensional nerve map of human bladder trigone. Neurourol Urodyn 2017; 36:1015–1019. [DOI] [PubMed] [Google Scholar]
- 10.Shepherd JP, Carter-Brooks CM, Chermanksy C. A cost-effectiveness analysis of onabotulinumtoxin A as first-line treatment for overactive bladder. Int Urogynecol J 2018; 29:1213–1219. [DOI] [PubMed] [Google Scholar]
- 11.Schurch B, Stöhrer M, Kramer G, et al. Botulinum-A toxin for treating detrusor hyperreflexia in spinal cord injured patients: a new alternative to anticholinergic drugs? Preliminary results. J Urol 2000; 164:692–697. [DOI] [PubMed] [Google Scholar]
- 12.Flynn MK, Amundsen CL, Perevich M, et al. Outcome of a randomized, double-blind, placebo controlled trial of botulinum A toxin for refractory overactive bladder. J Urol 2009; 181:2608–2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brubaker L, et al. Refractory idiopathic urge urinary incontinence and botulinum A injection. J Urol 2008; 180:217–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuo HC. Comparison of effectiveness of detrusor, suburothelial and bladder base injections of botulinum toxin a for idiopathic detrusor overactivity. J Urol 2007; 178:1359–1363. [DOI] [PubMed] [Google Scholar]
- 15.Sahai A, Khan MS, Dasgupta P. Efficacy of botulinum toxin-A for treating idiopathic detrusor overactivity: results from a single center, randomized, double-blind, placebo controlled trial. J Urol 2007; 177:2231–2236. [DOI] [PubMed] [Google Scholar]
- 16.Nitti VW, et al. OnabotulinumtoxinA for the treatment of patients with overactive bladder and urinary incontinence: results of a phase 3, randomized, placebo controlled trial. J Urol 2017; 197:S216–S223. [DOI] [PubMed] [Google Scholar]
- 17.Cui Y, et al. Botulinum toxin-A injections for idiopathic overactive bladder: a systematic review and meta-analysis. Urol Int 2013; 91:429–438. [DOI] [PubMed] [Google Scholar]
- 18. ■.Dmochowski R, et al. Efficacy and safety of onabotulinumtoxinA for idiopathic overactive bladder: a double-blind, placebo controlled, randomized, dose ranging trial. J Urol 2010; 184:2416–2422.This clinical trial highlights the efficacy and side-effect profile of human intravesical use of Botox for idiopathic OAB. Importantly, this trial reveals the dose-dependent relationship between rates of urinary retention and escalating doses of Botox.
- 19.Fowler CJ, et al. OnabotulinumtoxinA improves health-related quality of life in patients with urinary incontinence due to idiopathic overactive bladder: a 36-week, double-blind, placebo-controlled, randomized, dose-ranging trial. Eur Urol 2012; 62:148–157. [DOI] [PubMed] [Google Scholar]
- 20.Miotla P, et al. Impact of intravesical onabotulinumtoxinA on sexual function in women with OAB. Neurourol Urodyn 2017; 36:1564–1569. [DOI] [PubMed] [Google Scholar]
- 21.Mühlstädt S, et al. Quo vadis botulinum toxin: normative constraints and quality of life for patients with idiopathic OAB? Front Surg 2018; 5:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cameron AP, Rodriguez GM, Schomer KG. Systematic review of urological followup after spinal cord injury. J Urol 2012; 187:391–397. [DOI] [PubMed] [Google Scholar]
- 23.Wyndaele JJ, et al. Neurologic urinary incontinence. Neurourol Urodyn 2010; 29:159–164. [DOI] [PubMed] [Google Scholar]
- 24.Schurch B, et al. Botulinum toxin type a is a safe and effective treatment for neurogenic urinary incontinence: results of a single treatment, randomized, placebo controlled 6-month study. J Urol 2005; 174:196–200. [DOI] [PubMed] [Google Scholar]
- 25.Reitz A, et al. European experience of 200 cases treated with botulinum-A toxin injections into the detrusor muscle for urinary incontinence due to neurogenic detrusor overactivity. Eur Urol 2004; 45:510–515. [DOI] [PubMed] [Google Scholar]
- 26. ■.Ginsberg D, et al. Phase 3 efficacy and tolerability study of onabotulinumtoxinA for urinary incontinence from neurogenic detrusor overactivity. J Urol 2012; 187:2131–2139.The data from this important clinical trial support the use of intravesical injections of Botox for NGB, in improving detrusor pressures and incontinence episodes.
- 27.Cruz F, et al. Efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: a randomised, double-blind, placebo-controlled trial. Eur Urol 2011; 60:742–750. [DOI] [PubMed] [Google Scholar]
- 28.Chancellor MB, et al. OnabotulinumtoxinA improves quality of life in patients with neurogenic detrusor overactivity. Neurology 2013; 81:841–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hassouna T, Gleason JM, Lorenzo AJ. Botulinum toxin A’s expanding role in the management of pediatric lower urinary tract dysfunction. Curr Urol Rep 2014; 15:426. [DOI] [PubMed] [Google Scholar]
- 30.Marte A, et al. Effectivenessof botulinum-Atoxin for the treatment of refractory overactive bladder in children. EurJ Pediatr Surg 2010; 20:153–157. [DOI] [PubMed] [Google Scholar]
- 31.Scheepe JR, Blok BF, ‘t Hoen LA. Applicability of botulinum toxin type A in paediatric neurogenic bladder management. Curr Opin Urol 2017;27:14–19. [DOI] [PubMed] [Google Scholar]
- 32.Bayrak O, Sadioglu E, Sen H, et al. Efficacy of onabotulinum toxin A injection in pediatric patients with nonneurogenic detrusor overactivity. Neurourol Urodyn 2017; 36:2078–2082. [DOI] [PubMed] [Google Scholar]
- 33.El-Dakhakhny AS, El-Karamany TM, El-Atrebi M, Gharib T. Efficacy and safety of intradetrusor onabotulinumtoxinA injection for managing paediatric non-neurogenic overactive bladder: a prospective case-series study. Arab J Urol 2019; 17:143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ingham J, Angotti R, Lewis M, Goyal A. Onabotulinum toxin A in children with refractory idiopathic overactive bladder: medium-term outcomes. J Pediatr Urol 2019; 15:32.e1–32.e5. [DOI] [PubMed] [Google Scholar]
- 35.Sekerci CA, Tanidir Y, Garayev A, et al. Clinical and urodynamic results of repeated intradetrusor onabotulinum toxin A injections in refractory neurogenic detrusor overactivity: up to 5 injections in a cohort of children with myelodysplasia. Urology 2018; 111:168–175. [DOI] [PubMed] [Google Scholar]
- 36.Schulte-Baukloh H, Herholz J, Bigalke H, et al. Results of a BoNT/A antibody study in children and adolescents after onabotulinumtoxin A (Botoxâ) detrusor injection. Urol Int 2011; 87:434–438. [DOI] [PubMed] [Google Scholar]
- 37.Riccabona M, et al. Botulinum-A toxin injection into the detrusor: a safe alternative in the treatment of children with myelomeningocele with detrusor hyperreflexia. J Urol 2004; 171:845–848. [DOI] [PubMed] [Google Scholar]
- 38.Kajbafzadeh AM, et al. Intravesical injection of botulinum toxin type A: management of neuropathic bladder and bowel dysfunction in children with myelomeningocele. Urology 2006; 68:1091–1096. [DOI] [PubMed] [Google Scholar]
- 39.Hascoet J, et al. Outcomes of intra-detrusor injections of botulinum toxin in patients with spina bifida: a systematic review. Neurourol Urodyn 2017; 36:557–564. [DOI] [PubMed] [Google Scholar]
- 40.Leu R, Stearns GL. Complications of Botox and their management. Curr Urol Rep 2018; 19:90. [DOI] [PubMed] [Google Scholar]
- 41. ■.Nitti VW, et al. Durable efficacy and safety of long-term onabotulinumtoxinA treatment in patients with overactive bladder syndrome: final results of a 3.5-year study. J Urol 2016; 196:791–800.This clinical trial provides a large base of evidence toward Botox efficacy in idiopathic OAB.
- 42.Bauer RM, et al. Patient-reported side effects of intradetrusor botulinum toxin type a for idiopathic overactive bladder syndrome. Urol Int 2011; 86:68–72. [DOI] [PubMed] [Google Scholar]
- 43.Cheng T, et al. Efficacy and safety of onabotulinumtoxinA in patients with neurogenic detrusor overactivity: a systematic review and meta-analysis of randomized controlled trials. PLoS One 2016; 11:e0159307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marcelissen TA, Rahnama’i MS, Snijkers A, et al. Long-term follow-up of intravesical botulinum toxin-A injections in women with idiopathic overactive bladder symptoms. World J Urol 2017; 35:307–311. [DOI] [PubMed] [Google Scholar]
- 45.Uçar M, Akgül AK, Parlak A, et al. Noninvasive evaluation of botulinum-A toxin treatment efficacy in children with refractory overactive bladder. Int Urol Nephrol 2018; 50:1367–1373. [DOI] [PubMed] [Google Scholar]
- 46.Kask M, Rintala R, Taskinen S. Effect of onabotulinumtoxinA treatment on symptoms and urodynamic findings in pediatric neurogenic bladder. J Pediatr Urol 2014; 10:280–283. [DOI] [PubMed] [Google Scholar]
- 47.Zeino M, Becker T, Koen M, et al. Long-term follow-up after botulinum toxin A (BTX-A) injection into the detrusor for treatment of neurogenic detrusor hyperactivity in children. Cent European J Urol 2012; 65:156–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Joussain C, et al. Long-term outcomes and risks factors for failure of intradetrusor onabotulinumtoxin A injections for the treatment of refractory neurogenic detrusor overactivity. Neurourol Urodyn 2018; 37:799–806. [DOI] [PubMed] [Google Scholar]
- 49.Hascoet J, et al. Intradetrusor injections of botulinum toxin type A in children with spina bifida: a multicenter study. Urology 2018; 116:161–167. [DOI] [PubMed] [Google Scholar]
- 50.Khan MK, et al. Botulinum toxin injection in the pediatric population with medically refractory neuropathic bladder. J Pediatr Urol 2016; 12:. [DOI] [PubMed] [Google Scholar]
- 51.Temeltas G, Tikiz C, Dagci T, et al. The effects of botulinum-A toxin on bladder function and histology in spinal cord injured rats: is there any difference between early and late application? J Urol 2005; 174:2393–2396. [DOI] [PubMed] [Google Scholar]
- 52.Tinay I, Tanidir Y, Cikler E, et al. Intradetrusor botulinum neurotoxin A (BoNT-A) injections decrease bladder fibrosis secondary to partial urethral obstruction in the male rat model. Neurourol Urodyn 2012; 31:564–570. [DOI] [PubMed] [Google Scholar]
- 53.Doherty A, Hennessey DB, Onggo JR, et al. Modifications to Botulinum toxin A delivery in the management of detrusor overactivity recalcitrant to initial injections: a review. World J Urol 2019; 37:891–898. [DOI] [PubMed] [Google Scholar]
- 54.Peyronnet B, et al. Failure of botulinum toxin injection for neurogenic detrusor overactivity: switch of toxin versus second injection of the same toxin. Int J Urol 2015; 22:1160–1165. [DOI] [PubMed] [Google Scholar]
- 55.Koh C, Melling CV, Jennings C, et al. Efficacy of electromotive drug administration in delivering botulinum toxin a in children with neuropathic detrusor overactivity-outcomes of a pilot study. J Pediatr Urol 2019; 15:552.e1–552.e8. [DOI] [PubMed] [Google Scholar]
- 56.Sharifi-Rad L, Ladi-Seyedian SS, Nabavizadeh B, et al. Intravesical electromotive botulinum toxin type A. Urology 2019. doi: 10.1016/j.urology.2019.06.033. [DOI] [PubMed] [Google Scholar]
- 57.Sekerci CA, et al. Value of urinary brain-derived neurotrophic factor levels on the assessment of botulinum toxin type A treatment for neurogenic detrusor overactivity in children with myelodysplasia. J Urol 2019; 201:174–180. [DOI] [PubMed] [Google Scholar]
- 58.Aoki KR, Guyer B. Botulinum toxin type A and other botulinum toxin serotypes: a comparative review of biochemical and pharmacological actions. Eur J Neurol 2001; 8(Suppl 5):21–29. [DOI] [PubMed] [Google Scholar]
- 59. ■.Dong M, Richards DA, Goodnough MC, et al. Synaptotagmins I and II mediate entry of botulinum neurotoxin B into cells. J Cell Biol 2003; 162:1293–1303.Although Botox (botulinum neurotoxin A) uses SV2 as its receptor on the neurons, botulinum neurotoxin B uses synaptotagmin as the target protein receptor. This article provides the evidence for this discovery and paves the way for novel toxins that target the synaptotagmin receptor.
- 60.Dong M, et al. SV2 is the protein receptor for botulinum neurotoxin A. Science 2006; 312:592–596. [DOI] [PubMed] [Google Scholar]
- 61.Rummel A, Karnath T, Henke T, et al. Synaptotagmins I and II act as nerve cell receptors for botulinum neurotoxin G. J Biol Chem 2004; 279:30865–30870. [DOI] [PubMed] [Google Scholar]
- 62.Dong M, Tepp WH, Liu H, et al. Mechanism of botulinum neurotoxin B and G entry into hippocampal neurons. J Cell Biol 2007; 179:1511–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dong M, Liu H, Tepp WH, et al. Glycosylated SV2A and SV2B mediate the entry of botulinum neurotoxin E into neurons. Mol Biol Cell 2008; 19:5226–5237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Peng L, et al. Botulinum neurotoxin D-C uses synaptotagmin I and II as receptors, and human synaptotagmin II is not an effective receptor for type B, D-C and G toxins. J Cell Sci 2012; 125:3233–3242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Peng L, Tepp WH, Johnson EA, Dong M. Botulinum neurotoxin D uses synaptic vesicle protein SV2 and gangliosides as receptors. PLoS Pathog 2011; 7:e1002008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mahrhold S, Rummel A, Bigalke H, et al. The synaptic vesicle protein 2C mediates the uptake of botulinum neurotoxin A into phrenic nerves. FEBS Lett 2006;580:2011–2014. [DOI] [PubMed] [Google Scholar]
- 67.López de la Paz M, Scheps D, Jurk M, et al. Rational design of botulinum neurotoxin A1 mutants with improved oxidative stability. Toxicon 2018; 147:54–57. [DOI] [PubMed] [Google Scholar]
- 68.Stone HF, Zhu Z, Thach TQ, Ruegg CL. Characterization of diffusion and duration of action of a new botulinum toxin type A formulation. Toxicon 2011; 58:159–167. [DOI] [PubMed] [Google Scholar]
- 69.Wilhelm BG, et al. Composition of isolated synaptic boutons reveals the amounts of vesicle trafficking proteins. Science 2014; 344: 1023–1028. [DOI] [PubMed] [Google Scholar]
- 70.Rummel A, Mahrhold S, Bigalke H, Binz T. Exchange of the H(CC) domain mediating double receptor recognition improves the pharmacodynamic properties of botulinum neurotoxin. FEBS J 2011; 278:4506–4515. [DOI] [PubMed] [Google Scholar]
- 71.Pang ZP, et al. Synaptotagmin-2 is essential for survival and contributes to Ca2+ triggering of neurotransmitter release in central and neuromuscular synapses. J Neurosci 2006; 26:13493–13504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Strotmeier J, Willjes G, Binz T, Rummel A. Human synaptotagmin-II is not a high affinity receptor for botulinum neurotoxin B and G: increased therapeutic dosage and immunogenicity. FEBS Lett 2012; 586:310–313. [DOI] [PubMed] [Google Scholar]
- 73.Hirst GR, et al. Botulinum toxin B is not an effective treatment of refractory overactive bladder. Urology 2007; 69:69–73. [DOI] [PubMed] [Google Scholar]
- 74.Ghei M, et al. Effects of botulinum toxin B on refractory detrusor overactivity: a randomized, double-blind, placebo controlled, crossover trial. J Urol 2005; 174:1873–1877. [DOI] [PubMed] [Google Scholar]
- 75.Dykstra D, Enriquez A, Valley M. Treatment of overactive bladder with botulinum toxin type B: a pilot study. Int Urogynecol J Pelvic Floor Dysfunct 2003; 14:424–426. [DOI] [PubMed] [Google Scholar]
- 76. ■■.Tao L, et al. Engineered botulinum neurotoxin B with improved efficacy for targeting human receptors. Nat Commun 2017; 8:53.This study introduces the novel mutations to botulinum neurotoxin B (E1191M/S1199Y) that improve its binding capacity to human synaptotamin receptors. This enhanced binding has ~11-fold greater efficacy in blocking neurotransmitter release.
- 77. ■■.Elliott M, et al. Engineered botulinum neurotoxin B with improved binding to human receptors has enhanced efficacy in preclinical models. Sci Adv 2019; 5:eaau7196.In line with the development of novel toxins, this article further studies engineered neurotoxins (rBoNT/B1MY and rBoNT/B1QW) in skeletal and smooth muscle preclinical experiments, and provides the crystal structure of this novel toxin with its synaptotagmin receptor. Evidence in this Science Advances article paves the way for the use of novel toxins in therapeutics.
- 78. ■■.Yin L, et al. Characterization of a membrane binding loop leads to engineering botulinum neurotoxin B with improved therapeutic efficacy. PLoS Biol 2020; 18:e3000618.In this study, an important toxin to receptor binding interaction is characterized and described (termed lipid binding loop), and modified with mutations to enhance the binding capacity of this interaction. The engineered toxin, with improved binding to lipid membranes, has a greater paralytic effect and less toxin diffusion capability, compared to naturally occuring toxins.
- 79.Stern D, et al. A lipid-binding loop of botulinum neurotoxin serotypes B, DC and G is an essential feature to confer their exquisite potency. PLoS Pathog 2018; 14:e1007048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhang S, et al. Structural basis for the unique ganglioside and cell membrane recognition mechanism of botulinum neurotoxin DC. Nat Commun 2017; 8:1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang S, et al. Identification and characterization of a novel botulinum neurotoxin. Nat Commun 2017; 8:14130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhang S, Lebreton F, Mansfield MJ, et al. Identification of a botulinum neurotoxin-like toxin in a commensal strain of Enterococcus faecium. Cell Host Microbe 2018; 23:169–176.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]