Abstract
Stroke outcome considerably varies between stroke patients and often cannot be predicted. Now, Gendrun and colleagues investigated the suitability of blood neurofilament light chain proteins (NFL) as a biomarker of neuronal damage. High NFL levels correlated with brain injury, functional outcome and mortality following all major types of stroke. These data raise hope to revolutionize future prognosis and management of stroke patients.
Keywords: Biomarker, neurofilament, stroke, ischemia, neuronal damage
Main text
Stroke is a leading cause of disability and death worldwide. Over 13.7 million strokes occur each year, and one in four people over 25 years will experience a stroke in their lifetime.1 The presence of life-saving medicines allows timely intervention and significantly decreased mortality following stroke.2 On the other hand, overall stroke outcome can vary considerably between individual patients from asymptomatic and non-disabling to permanent-disability or death. Current clinical measures include the assessment through an experienced stroke clinician and are supplemented with advanced neuroimaging such as magnetic resonance imaging (MRI) and computed tomography (CT) to determine the injured stroke area and brain damage. However, this advanced healthcare infrastructure is inaccessible for many patients especially in low and middle-income countries and/or in rural regions. Although clinical assessments provide important insight into overall stroke severity, they are often crude and have only moderate correlation with actual brain tissue damage and long-term outcome.3 Thus, potential easily available blood biomarkers (see here for an overview of biomarkers 4) are urgently needed to guide individualized stroke patient treatment. Now, research by Gendron and colleagues 5 identified elevated levels of Neurofilament light chain protein (NFL) in multiple cohorts of stroke patients and raise hope towards a universal prognostic blood biomarker for brain injury.
While blood biomarkers such as troponin have revolutionized the prognosis and management of myocardial infarction (MI), the development of blood biomarkers for stroke faces difficulties. Strokes tend to be a more heterogeneous condition than ischemic heart diseases. Contrary to MI that is mainly caused by atherosclerosis, causes of stroke also include small- and large vessel disease, cardioembolism, dissections and rare coagulopathies. Moreover, the blood-brain barrier (BBB) considerably reduces the release of brain tissue proteins into the blood circulation after stroke, delaying the release of glial and neuronal proteins. So far, a variety of individual prognostic blood biomarkers have been identified that indicate neuronal damage, inflammation or BBB disruption. Also panels of biomarkers have been suggested to predict stroke outcome. However, most of the studies on blood markers reside still in an exploratory phase, and therefore used rather small cohorts and only few were controlled for potential confounding factors.
Among others, NFLs have emerged as promising prognostic biomarkers in stroke.6,7 Since NFL proteins are major structural components of neurons, release of NFL can be directly related to neuronal damage. Previously, cerebrospinal fluid concentrations of NFL have been associated with neuronal damage. However, the more recent development of ultrasensitive assays allowed also its quantification in the blood serum.6 As a consequence, the use of NFL as a marker of neuronal damage became feasible in diseases where lumbar puncture is not part of the clinical routine, such as stroke. Given the heterogeneous pathology of stroke, few initial studies concentrated on the correlation between elevated NFL blood levels to outcomes of specific subtypes of stroke. Although most findings were encouraging, interstudy discrepancies revealed the need for more intensive investigations to verify NFL as a universal blood biomarker for all major types of stroke.
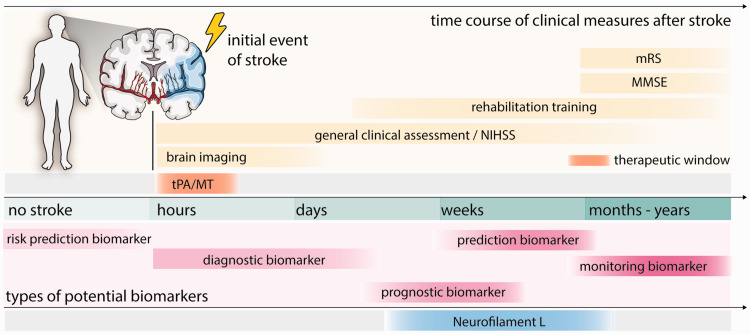
Here, Gendron and colleagues5 undertook a comprehensive study to investigate the suitability of blood NFL as a uniform blood biomarker to predict the degree of neuronal damage and mortality. The authors generated a large multi-cohort dataset of stroke patients categorized in acute cerebral infarction (ACI, N = 227), subarachnoid hemorrhage (SAH, N = 58) and intracerebral hemorrhage (ICH, N = 169). Their findings indicate elevated levels of neurofilament light (NFL) across all major types of stroke. Differences in blood NFL between patients and control were most evident at 9–20 days following stroke onset. Interestingly, elevated NFL blood levels also correlated with infarct volume, which was determined using CT-based scores. To determine neurological, functional and cognitive status of stroke patients at the time of blood withdrawal, a panel of standard clinical measures were performed consisting of the National Institutes of Health Stroke Scale (NIHSS), the modified Rankin Scale (mRS), and the Mini-Mental State Examination (MMSE). In all stroke groups, higher blood NFL levels were associated with a worse performance for all the three tests. Strikingly, increased plasma NFL serums collected within 20 days following stroke were also able to reliably predict poor functional recovery three and six months following stroke and indicated an increased all-cause mortality within the first three years (Figure 1).
Figure 1.
Time course of stroke and potential blood biomarkers. Current measures of stroke consist of clinical assessments and neuronal imaging to confirm a stroke and initiate enzymatic thrombolysis (tPA) and/or mechanical thrombectomy (MT) treatment. The therapeutic window of the treatments is 4–6.5 hours following stroke. Several days after stroke rehabilitative training begins and can continue for months-years. Regular measures of motor and cognitive abilities are performed to determine long-term effects of stroke e.g. NIHSS, MMSE, mRS. Types of Biomarker: To measure the risk to develop a disease (risk prediction); To confirm the presence of a disease or identify subtypes (diagnosis); to identify probability to develop a clinical event in patients with a disease (prognosis); to predict probability to develop any effect as consequence of clinical intervention (prediction); to monitor the status of a disease and the response to an intervention (monitoring). tPA: tissue plasminogen activator; MT: mechanical thrombectomy, NIHSS: National Institutes of Health Stroke Scale; mRS: modified Rankin Scale; MMSE: Mini-Mental State Examination.
These results encourage the use of NFL as a subacute biomarker to forecast stroke outcome, complications and complement clinical routine in the near future. The additional information might be used to allocate healthcare resources and improve drug development: (1) Patients with elevated NFL levels might be referred to more intensive rehabilitation centers to counteract an unfavorable clinical outcome; and (2) efficacy of novel therapeutics might be assessed based on blood NFL levels. However, high blood NFL levels are not specific for stroke and its release has been also linked with other neurological conditions including multiple sclerosis and traumatic brain injuries.8 Therefore, stroke patients and clinicians may further benefit from recent advancements in the development of risk prediction and diagnostic biomarkers. Increased search for novel blood biomarker after stroke also revealed other promising candidates e.g. hemojuvelin to be an independent predictor of functional outcome after stroke.9 Multilevel omics approaches have revealed a panel of biomarkers to identify the likelihood of developing a stroke or to diagnose and categorize the stroke type in the acute phase.10 Although it is important to note that translating these exciting findings into clinical routine would require further optimization and validation, a panel of diagnostic and prognostic blood biomarkers have definitely great potential to revolutionize stroke management and contribute to individualized precision medicine for stroke patients.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This work was kindly supported by the Mäxi Foundation.
Acknowledgements: The brain cross section in Figure 1 was modified from Servier Medical Art, licensed under a Creative Common Attribution 3.0 Generic License. http://smart.servier.com/.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iD: Ruslan Rust https://orcid.org/0000-0003-3376-3453
References
- 1.GBD 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol 2019; 18: 439–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thomalla G, Simonsen CZ, Boutitie F, et al. MRI-guided thrombolysis for stroke with unknown time of onset. N Engl J Med 2018; 379: 611–622. [DOI] [PubMed] [Google Scholar]
- 3.Menezes Nina M, Ay H, Wang Zhu M, et al. The real estate factor. Stroke 2007; 38: 194–197. [DOI] [PubMed] [Google Scholar]
- 4.García-Gutiérrez MS, Navarrete F, Sala F, et al. Biomarkers in psychiatry: concept, definition, types and relevance to the clinical reality. Front Psychiatry 2020; 11: 432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gendron TF, Badi MK, Heckman MG, et al. Plasma neurofilament light predicts mortality in patients with stroke. Sci Transl Med 2020; 12: eaay1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khalil M, Teunissen CE, Otto M, et al. Neurofilaments as biomarkers in neurological disorders. Nat Rev Neurol 2018; 14: 577–589. [DOI] [PubMed] [Google Scholar]
- 7.Pinter D, Gattringer T, Enzinger C, et al. Longitudinal MRI dynamics of recent small subcortical infarcts and possible predictors. J Cereb Blood Flow Metab 2019; 39: 1669–1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barro C, Chitnis T, Weiner HL.Blood neurofilament light: a critical review of its application to neurologic disease. Ann Clin Transl Neurol.2020; 7: 2508–2523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Young G-H, Tang S-C, Wu V-C, et al. The functional role of hemojuvelin in acute ischemic stroke. J Cereb Blood Flow Metab 2020; 40: 1316–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montaner J, Ramiro L, Simats A, et al. Multilevel omics for the discovery of biomarkers and therapeutic targets for stroke. Nat Rev Neurol 2020; 16: 247–264. [DOI] [PubMed] [Google Scholar]