Abstract
Background
Investigations demonstrated a decrease of admissions for myocardial infarction (MI) during the CoronaVirus Disease-19 (COVID-19) outbreak. No study has evaluated the time required to reverse this downward curve of MI admissions.
Methods
This is a retrospective analysis on patients (N = 2415) admitted to the Emergency Departments for acute MI in nine Italian centers. Primary endpoint was the incidence rates (IRs) of MI admissions in the post-lockdown COVID-19 period (case-period: from May 4 to July 12, 2020) vs. the following control periods: January 1–February 19, 2020 (pre-lockdown period); February 20–May 3, 2020 (intra-lockdown period); May 4–July 12, 2019 (inter-year non-COVID-19 period).
Results
IR of admissions for MI in the post-lockdown period was higher than the intra-lockdown period (IR ratio, IRR: 1.60, 95% CI 1.42–1.81; p = 0.0001), was lower than the pre-lockdown period (IRR: 0.86, 0.77–0.96; p = 0.009) and similar to the inter-year non-COVID-19 period (IRR: 0.96, 0.87–1.07; p = 0.47). Within the case period, the increase in MI admissions was more pronounced in earlier vs later weeks (IRR 1.19, 95% CI 1.02–1.38, p = 0.024) and, compared to the inter-year control period, was significant for non ST-segment elevation MI (IRR: 1.25, 95% CI 1.08–1.46, p = 0.004), but was not observed for ST-segment elevation MI (STEMI), where hospitalizations were reduced (IRR 0.76, 95% CI 0.65–0.88, p = 0.0001).
Conclusions
Our study first indicates an increase in the number of admissions for MI after the removal of the national lockdown for COVID-19 in Italy. This increase was prevalent in the first weeks following the lockdown removal, but was under-represented in STEMI patients.
Key-words: COVID-19, Viral pandemic, Hospitalizations, Myocardial infarction
1. Introduction
Investigations demonstrated a significant decrease of admissions for acute coronary syndrome during the CoronaVirus Disease-19 (COVID-19) outbreak, [[1], [2], [3], [4]] possibly due to underestimation of symptoms, negative psychological response, including anxiety, depression and social isolation, as well as distrust of in-hospital anti-COVID-19 protocols and consequent fear of post-admission contagion. [5] In Italy this reduction was particularly evident during the national lockdown, that was decreed on March 8, 2020. Notably, a concomitant increase in the number of cases of out-of-hospital cardiac arrest during the COVID-19 pandemic was observed in Italy. [6] We evaluated the over time course of the hospitalization rates for myocardial infarction (MI) after the national lockdown in Italy.
2. Methods
This is a retrospective analysis performed in 9 Italian tertiary hub centers with on-site cath–lab availability 24 h per day/7 days per week/365 days per year, serving a total population of 911.000 people. Epidemiological data of consecutive patients admitted for MI at the participating hospitals were anonymously extracted from each hospital's electronic database and checked for accuracy by study investigators. The following intra-year control periods were considered: January 1–February 19, 2020 (pre-lockdown COVID-19 period); February 20–May 3, 2020 (intra-lockdown COVID-19 period). The case-period was defined as the time from May 4 to July 12, 2020 (post-lockdown COVID-19 period). A comparison between post-lockdown COVID-19 period and the same time-frame in 2029 (inter-year control period) was also performed. Primary endpoint was the incidence rate (IR) of admissions for MI, either ST-segment elevation (STEMI) and non ST-segment elevation myocardial infarction (NSTEMI), in the case-period vs. each of the control periods. IRs of admissions for MI were calculated by dividing the number of cumulative events by the number of days for each time period. Incidence rate ratios (IRRs) comparing the case-period with each of the control periods were calculated by Poisson regression. Sub-analyses for MI subtypes (STEMI, NSTEMI) were also performed. The case-period was further segmented in an earlier time-frame [from May 4 to June 3, 2020 (i.e. when limited social containing measures and restrictions of economic activities were still maintained)] and a later time-frame [from June 4 to July 12, 2020]. Moreover, the weekly number of admissions for MI from January 1 to July 12, 2020 was assessed together with a Local Polynomial Regression smoothing (LOESS) curve and 95% CI.
3. Results
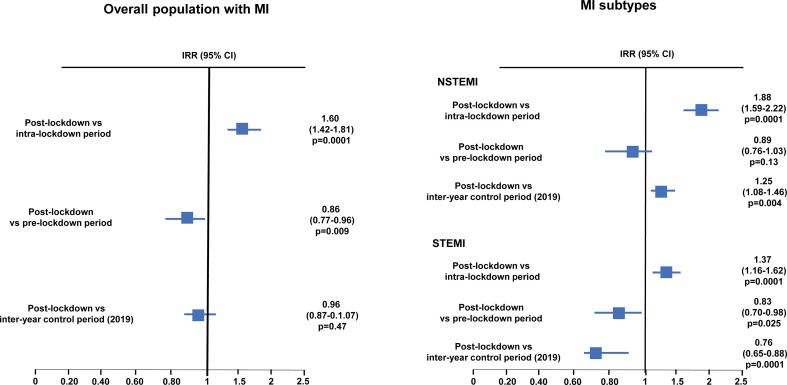
A total of 2415 patients hospitalized for MI were included. IRs for MI were 11.3/day in the pre-lockdown period, 6.1/day in the intra-lockdown period, 9.8/day in the post-lockdown period and 10.1/day in the inter-year non-COVID-19 period. The IR of admissions for MI in the post-lockdown period was higher than the intra-lockdown period (IRR: 1.60, 95% CI 1.42–1.81; p = 0.0001), was lower than the pre-lockdown period (IRR: 0.86, 0.77–0.96; p = 0.009) and similar to the inter-year non-COVID-19 period (IRR: 0.96, 0.87–1.07; p = 0.47) (Fig. 1 ).
Fig. 1.
IRRs of hospitalizations for MI in the case period vs control periods in the overall population and according to MI subtypes.
CI = Confidence interval; IRR = Incidence rate ratio; MI = Myocardial infarction; NSTEMI = Non ST-segment elevation myocardial infarction; STEMI = ST-segment elevation myocardial infarction.
The analysis according to the type of MI (Fig. 1) revealed that the IR of admissions for NSTEMI was 6.0/day in the pre-lockdown period, 2.8/day in the intra-lockdown period, 5.3/day in the post-lockdown period and 4.3/day in the inter-year non-COVID-19 period. The IR of admissions for NSTEMI in the post-lockdown period was significantly increased compared to the intra-lockdown period (IRR: 1.88, 95% CI 1.59–2.22, p = 0.0001), reaching values similar to the pre-lockdown period (IRR: 0.89, 95% CI 0.76–1.03, p = 0.13) and being even higher than the inter-year non-COVID-19 period (IRR: 1.25, 95% CI 1.08–1.46, p = 0.004).
The IR of admissions for STEMI was 5.3/day in the pre-lockdown period, 3.2/day in the intra-lockdown period, 4.4/day in the post-lockdown period and 5.9/day in the inter-year non-COVID-19 period. The IR of admissions for STEMI in the post-lockdown period was significantly higher than the intra-lockdown (IRR: 1.37, 95% CI 1.16–1.62, p = 0.0001), but remained lower than the pre-lockdown period (IRR: 0.83, 95% CI 0.70–0.98, p = 0.025) and the inter-year non-COVID-19 period (IRR: 0.76, 95% CI 0.65–0.88, p = 0.0001).
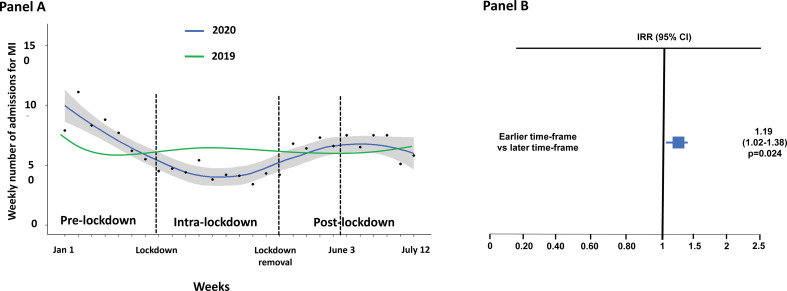
The analysis on the weekly number of admissions for MI by Local Polynomial Regression smoothing (LOESS) is illustrated in Fig. 2 , panel A. The decline of MI admission started before the lockdown and therefore may be related both to the lockdown and the pandemic itself. Within the post-lockdown period, the increase in the number of admissions for MI was more pronounced in the earlier time-frame vs the later time-frame (IR 10.7/day vs 9.0/day; IRR 1.190, 95% CI 1.023–1.382, p = 0.024) (Fig. 2, panel B). In Fig. 2 we also depict that from January 1 to July 12 the rates of MI admission in 2019 remained essentially constant across the whole period.
Fig. 2.
Panel A. Weekly number of admissions for MI in 2020 and 2019. At a Negative Binomial (NB) model, ratio of means and 95% CI for the period May 4–July 12, 2020 were 0.81, 0.50–1.36 (p = 0.402), for the period February 20–May 3, 2020 were 0.68, 0.55–0.83 (p < 0.001). Panel B. Analysis within the case period: IRR of admissions for MI in the earlier time-frame (May 4–June 3, 2020) vs the later time-frame (June 4–July 12, 2020).
CI = Confidence interval; IRR = Incidence rate ratio; MI = Myocardial infarction.
4. Discussion
Our study first indicates an increase in the number of admissions for MI after the removal of the national lockdown for COVID-19 in Italy. Such increase was more pronounced in the first weeks following the lockdown removal. Our findings may be attributable to a decrease in the risk perception in the community, as well as to campaigns from scientific societies addressing that, even in the COVID-19 era: a) patients with symptoms suggestive of acute heart diseases must access the Emergency Departments to receive a prompt diagnosis and potentially lifesaving treatment; b) hospitals were capable to perform urgent cardiac interventions following dedicated pathways to prevent inter-individual viral diffusion. Our results have epidemiological relevance, as they might translate into a reduced number of people with post-acute cardiological issues in the next few months. However, unlike NSTEMI, in the post-lockdown period the hospitalizations for STEMI were still reduced; this is alarming inasmuch as this may be due to a persisting high early, pre-hospital mortality of STEMI patients, as already observed in the early COVID-19 era. [6] However, specific epidemiological studies are welcome to specifically address such issue.
Credit Author Statement
AR: conceptualization; data curation; writing: original draft.
FDA, CC, AB, MM, DT, UB, RV, CM: data curation; writing: review and editing.
MS, MGM, VG, RR, FU, ODF, IP, FF, GS, CM, GC, SL, GDF: writing: review and editing.
DA: formal analysis; writing: review and editing.
GP: conceptualization; formal analysis; methodology; writing: original draft.
Funding
No funding.
Disclosures
No disclosure related to this paper for all authors.
References
- 1.De Filippo O., D’Ascenzo F., Angelini F., et al. Reduced rate of hospital admission for ACS during COVID – 19 outbreak in Northern Italy. N. Engl. J. Med. 2020 Jul 2;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garcia S., Albaghdadi M.S., Meraji P.M., et al. Reduction in ST – segment elevation cardiac catheterization laboratory activations in United States during COVID – 19 pandemic. J. Am. Coll. Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Rosa S., Spaccarotella C., Basso C., et al. Reduction of hospitalization for myocardial infarction in Italy in the COVID – 19 era. Eur. Heart J. 2020 Jun 7;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tam C.F., Cheung K.S., Lam S., et al. Impact of coronavirus disease 19 (COVID 19) outbreak on ST – segment elevation myocardial infarction care in Hong – Kong, China. Circ. Cardiovasc. Qual. Outcomes. 2020;13(4) doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lau J.T., Griffiths S., Choi K.C., Tsui H.Y. Avoidance behaviors and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infect. Dis. 2010 May 28;10:139. doi: 10.1186/1471-2334-10-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baldi E., Sechi G.M., Mare C., et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N. Engl. J. Med. 2020 Apr 29 doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]