Abstract
Background:
Ulnar collateral ligament (UCL) injuries of the elbow are uncommon in the general population but prevalent in the athletic community, particularly among baseball players. Platelet-rich plasma (PRP) injection therapy has become a popular nonoperative adjuvant treatment for such injuries to help reduce recovery time and avoid surgery.
Purpose/Hypothesis:
To analyze patient outcomes by injury severity and identify injury types that responded most favorably and unfavorably to PRP treatment. It was hypothesized that PRP therapy would prove to be most beneficial in the treatment of lower-grade, partial UCL tears and less effective in the treatment of more severe, complete UCL tears.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A cohort of 50 patients with UCL injuries in their dominant elbow, diagnosed by MRI (magnetic resonance imaging) arthrogram, underwent PRP therapy in conjunction with an established rehabilitation program. UCL injuries were classified by MRI as low-grade partial tear (Type I), high-grade partial tear (Type II), complete tear (Type III), or tear in more than 1 location (Type IV).
Results:
In total, 24 of 39 (61.5%) Type I and II tears, 3 of 3 (100%) Type III tears, and 1 of 8 (12.5%) patients with Type IV tears responded to UCL PRP injection therapy and were able to return to play without surgery. Ten patients required subsequent UCL PRP injections, of which 3 (30%) were able to return to sport without surgery.
Conclusion:
PRP treatment for Types I and II UCL tears shows great promise when combined with physical therapy and a rehabilitation program. Type III UCL tears demonstrated a high rate of success, although with low cohort numbers. Type IV UCL tears did not appear to respond well to PRP injection therapy and often required surgical intervention or cessation of sport. Therefore, PRP treatment does not appear to be appropriate for patients with complete Type IV UCL tears but may enhance recovery and improve outcomes in throwing athletes with Types I, II, and III UCL injuries.
Keywords: platelet-rich plasma, ulnar collateral ligament, ultrasound, baseball
Elbow ulnar collateral ligament (UCL) injuries have seen a rise in incidence and prevalence in recent years. The majority of these injuries are seen in overhead throwing athletes, particularly baseball pitchers, due to the repetitive valgus forces placed on the elbow during overhead throwing.4,5,7–9 This prevalence has resulted in a high volume of these athletes seeking treatment recommendations for these often debilitating injuries.7,9,12,14,16,27 Patients with partial tears are often managed nonoperatively with rest, supportive measures (eg, anti-inflammatory drugs), and physical therapy, while more severe injuries often require surgical intervention.7,9,12,14–16,26,27 Over the past 20 years, UCL reconstruction techniques have been well-studied and refined, typically producing good outcomes and high return-to-play (RTP) rates.7,16,17,27 However, current treatment protocols and outcome data are significantly lacking for nonoperative management of UCL injuries. There is neither a clear consensus on the types of injuries best managed nonoperatively nor a precedence for likely outcomes of such treatments.
The first study to evaluate nonoperative management of UCL injuries administered a 4-month homogeneous-rehabilitation protocol to 31 overhead athletes with UCL injuries and observed an RTP rate of 42%.27 This study included athletes from a variety of sports but lacked a UCL injury grading system, which ultimately limited its applicability. Another evaluated the use of magnetic resonance imaging (MRI) to predict the outcomes of baseball players after they had sustained a UCL injury.20 Of the 39 athletes assessed, 12 (31%) responded to at least 6 weeks of conservative rehabilitation and avoided reconstructive surgery.20 Upon consideration of MRI, 84% of the 12 were found to have low-grade or intact UCLs.20 Of the patients who required surgical intervention, 82% were found to have high-grade or complete UCL tears on MRI.20 These studies demonstrate not only the capability of nonoperative techniques in managing UCL injuries but also the necessity of utilizing an injury-grading system, which helps to select the most effective treatment modality and avoid unnecessary delays in an athlete’s recovery.
The desire to minimize RTP time has led many clinicians to implement adjuvant therapies into their nonoperative approach to managing UCL injuries. Typically used in conjunction with a rehabilitation program, platelet-rich plasma (PRP) injections have become a popular adjunct and demonstrated effectiveness in a range of musculoskeletal pathologies.10–12,21–23,25,26 Although relatively new, PRP has been adopted by many physicians, quickly emerging as a popular conservative management modality. According to a survey conducted by the American Shoulder and Elbow Society, 36% of members responded that they routinely use PRP in the management of UCL injuries.18 While PRP literature remains limited due to it still being in its infancy, current data do allude to its potential benefits.12,25,27 In 2016, a study examined the effectiveness of PRP therapy in the treatment of high-level throwers with UCL insufficiency.12 This study found that 73% of 44 baseball players, having previously failed a course of conservative treatment, experienced excellent outcomes after PRP injection.12 Another study achieved similar results, assessing the recovery of 34 patients with partial UCL tears or increased UCL signal on MRI following a single ultrasound (US)-guided PRP injection.25 An RTP rate of 88% at a mean of 3 months was observed, which is in contrast to surgical reconstruction of the UCL that often permits an RTP rate of 90% at a mean timeframe of 9 to 12 months.12,25 Several studies have reported RTP rates between 73% and 96% with the use of PRP, demonstrating its utility in the management of UCL injuries.11,12,25 However, there remains a lack of evidence supporting the types and severities of UCL injuries that may respond most favorably or unfavorably to PRP therapy. Thus, the decision regarding whether to utilize PRP in the treatment of a particular UCL injury can be subjective rather than evidence-based.
The purpose of this study was to assess the effectiveness of PRP therapy as a conservative nonoperative treatment for UCL injuries. More specifically, this study aimed to analyze patient outcomes by injury severity and identify injury types that responded most favorably and unfavorably to PRP treatment. It was hypothesized that PRP therapy would be most beneficial in the treatment of lower-grade, partial UCL tears and less effective in the treatment of more severe, complete UCL tears.
Methods
Approval was obtained from the institutional review board. The charts of 61 throwing athletes between 16 and 44 years of age, who had previously undergone PRP therapy for a UCL injury in their dominant elbow between April 2010 and January 2014, were reviewed retrospectively. Charts were identified using the Current Procedural Terminology diagnosis code 24346 (UCL) and treatment code 0232 T (PRP). Patients were eligible for inclusion if they had at least 6 months of in-person follow-up after their PRP injection. Patients with a history of neurological pathology or UCL reconstructive surgery were not eligible for inclusion. Of the 61 patients selected, 11 were unable to be contacted for follow-up and thus excluded from the study. The patient population was made up of all throwing athletes, whose level of play ranged from low (ie, high school) to high level (ie, collegiate and professional).
Participants received a grading of their elbow MRI by a single sports medicine, fellowship-trained orthopaedic surgeon (P.W.J.), utilizing an established grading system.19 This system categorized UCL injuries into 4 distinct groups defined by the criteria outlined in Table 1.
Table 1.
Description of the MRI-based UCL Injury Classification Systema
| UCL Injury Classification on MRI | Description |
|---|---|
| Type I | Edema in UCL only; low-grade, partial tear (Figure 1A) |
| Type II | Partial tear of UCL; no extravasation of fluid on arthrogram; high-grade, partial tear (Figure 1B) |
| Type III | Complete, full-thickness tear of the UCL with extravasation of fluid on arthrogram (Figure 1C) |
| Type IV | Tear/pathology in more than 1 location on the UCL (ie, ulna and humerus) (Figure 1D) |
| Subset | H (humerus), U (ulna), and M (midsubstance) further denotes injury location |
aMRI, magnetic resonance imaging; UCL, ulnar collateral ligament.
Figure 1.
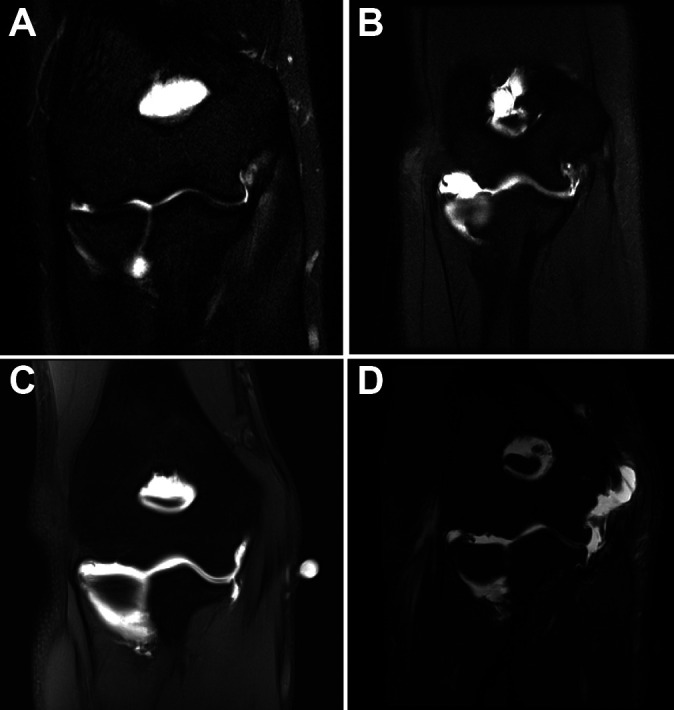
(A) MRI demonstrating a Type IH injury. (B) MRI demonstrating a Type IIH injury. (C) MRI of Type IIIU injury. (D) MRI of Type IV injury. MRI, magnetic resonance imaging.
Follow-up was conducted 2 years after each participant’s final injection. A single investigator (P.W.J.), who was blinded to the results of the MRI grading process, contacted each patient via telephone to evaluate functional outcome. Patients were asked a series of follow-up questions from a script written by lead investigators (P.W.J. and J.R.A.) to determine the level of recovery and classify each patient into 1 of 4 pre-established functional outcome categories. If symptoms remained after 7 months of therapy following PRP injection, it was reasonably assumed that maximal improvement had been achieved. The 4 categories were defined as follows:
Full recovery (ie, pain-free) and return to preinjury level of play.
Return to preinjury level of play without the need for surgical correction, but recovery lasted at least 6 months and potentially required additional conservative treatments (eg, additional PRP injections and/or extended physical therapy).
Return to preinjury level of play but required surgical correction within 5 years of the initial injection despite conservative management.
Inability to return to preinjury level of play despite conservative management and surgical correction.
The PRP was prepared according to Anz et al.1 Whole blood was drawn from the patient’s antecubital fossa via venipuncture with a 60-mL syringe preloaded with 10 mL of sodium citrate anticoagulant (EmCyte Corporation, Fort Myers, Florida). The blood was processed at the point of care with a dual-spin protocol/disposable (PurePRP; EmCyte) to produce leukocyte-rich PRP (LR-PRP). LR-PRP is monocyte/lymphocyte-rich and neutrophil-poor. The sample was loaded into a disposable cylinder and centrifuged for 1.5 minutes at 3800 rpm, producing a 2-layer soft stack that consisted of a platelet plasma layer suspended over a red cell layer. The top platelet plasma suspension layer was aspirated off until red blood cells entered the aspiration pipe. The aspirate was then loaded into a second disposable cylinder and centrifuged for 5 minutes at 3800 rpm. This second round of centrifugation resulted in a platelet-poor plasma (PPP) top layer and platelet buffy coat at the bottom of the cylinder. The PPP was aspirated off, leaving behind approximately 7 mL of pure PRP. The platelet buffy coat and plasma were resuspended into the remaining plasma by swirling the cylinder, and the final 7 mL of PRP was aspirated into the injection syringe.
Cell and platelet concentrations were not measured due to this study taking place prior to the issuance of guidelines for minimal reporting of biologic product studies.24 However, a 7-mL sample of PurePRP has been shown to contain a platelet concentration of approximately 1300 × 106 per mL, white blood cell concentration of 14.7 × 106 per mL, monocyte concentration of 2.3 × 106 per mL, and lymphocyte concentration of 11.9 × 106 per mL.1 The EmCyte PurePRP systems estimate a mean platelet capture efficiency rate of 76%.1
Immediately after PRP production, a single sports medicine physician (P.W.J.) used US to locate the UCL and a sterile 25-guage needle with 3 to 5 mL of 1% lidocaine to anesthetize the injured area. After anesthetization, the inactivated LR-PRP was injected using a sterile 22-guage needle into the pathologic section of the UCL under musculoskeletal US guidance and following standard sterile injection procedure.
After treatment, all patients were instructed to protect the injection site, use only gentle-passive range of motion (ROM), and avoid nonsteroidal anti-inflammatory drugs for 6 weeks after injection. Patients were also prescribed physical therapy and a detailed rehabilitation protocol, per the senior author’s traditional protocol. This protocol consisted of the following: a gradual increase in light-passive ROM and isometric exercise for the first 2 weeks after injection; the initiation of active ROM at the wrist by week 3; a gradual buildup in strengthening exercises, while avoiding valgus forces on the elbow during weeks 4 to 7; the introduction of upper extremity plyometrics, as tolerated, and an interval hitting program in week 8; and the initiation of a light tossing program during week 9. Patients who were without pain and had been cleared by a physician in week 9 were graduated to full throwing programs under the guidance of their physical therapist or athletic trainer.
Statistical analysis consisted of calculating the mean age and standard deviation for all participants as well as their mean duration of in-person follow-up. Participants were stratified by injury and functional outcome classification. Severe Type IV injuries were stratified separately from Type I to III injuries to preserve the clinical significance of our results. An odds ratio (OR), confidence interval, and P value were calculated comparing successful (Groups A and B) and unsuccessful (Groups C and D) outcomes for partial tears (Type I or II) of humeral versus ulnar origin, and partial tears (Type I or II) versus complete tears (Type III or IV). For participants who received more than 1 injection or underwent surgical reconstruction, the mean duration between injections as well as from their final injection to surgery was calculated.
Results
Of the 50 patients included in this study, 48 were male and 2 were female. There was a mean age of 20 ± 6 years at the time of injury (Table 2). Of the participants, 48 were baseball players and 2 were javelin throwers, whose level of play ranged from high school to professional. All 11 excluded patients were male baseball players, whose level of play ranged from high school to professional level. The mean length of in-person follow-up from the time of each participant’s initial PRP injection to their final appointment was 183.6 days (26.2 weeks).
Table 2.
Distribution of Ulnar Collateral Ligament (UCL) Injuries Based on MRI Classification
| UCL Injury Type | n (%) |
|---|---|
| IH | 18 (36) |
| IU | 5 (10) |
| IIH | 9 (18) |
| IIU | 7 (14) |
| IIIH | 3 (6) |
| IIIU | 0 (0) |
| IV | 8 (16) |
| Total | 50 |
Treatment of Groups A and B were considered to be successful, while treatment of Groups C and D were considered to be unsuccessful. Twenty-six athletes (52%) received outcome classifications consistent with Groups A and B, while 24 (48%) athletes were classified into either Group C or D (Table 3).
Table 3.
Distribution of Patients Classified by Functional Outcome After Treatment
| Outcome Classification | n (%) |
|---|---|
| A | 15 (30) |
| B | 11 (22) |
| C | 2 (4) |
| D | 22 (44) |
| Total | 50 |
Overall, 26 athletes (52%) were eventually able to return to their baseline function of performance with PRP treatment, physical therapy, and a rehabilitation program, receiving outcome classifications of either A or B. Twenty-four athletes (48%) received an outcome classification of either C or D, indicating they were either able to return to their preinjury level of play with the addition of surgical correction (Group C) or unable to return to their preinjury level of play despite undergoing PRP treatment, physical therapy, rehabilitation, and surgical correction (Group D).
Of the 42 athletes with a Type I, II, or III injury, 59.5% eventually returned to baseline and were therefore considered part of outcome categories A and B. Additionally, 40.5% of patients eventually required surgery or retirement, thus falling into outcome groups C and D (Table 4).
Table 4.
Distribution of Type I, II, and III Ulnar Collateral Ligament (UCL) Injuries by Outcome Classification
| Type I, II, and III UCL Injury | n (%) |
|---|---|
| Conservative treatment (groups A + B) | 25 (59.5) |
| Surgical treatment (groups C + D) | 17 (40.5) |
| Total | 42 |
Of the 8 patients with Type IV UCL injuries, 7 did not respond favorably to PRP treatment, physical therapy, and rehabilitation and eventually required surgical reconstruction or retirement (Table 5).
Table 5.
Distribution of Type IV Ulnar Collateral Ligament (UCL) Injuries by Outcome Classification
| Type IV UCL Tears | n (%) |
|---|---|
| Conservative treatment (groups A + B) | 1 (12.5) |
| Surgical treatment (groups C + D) | 7 (87.5) |
| Total | 8 |
An OR of successful (Group A and B) to unsuccessful (Groups C and D) outcomes for Type IH and Type IIH versus Type IU and Type IIU injuries was determined to be 1.04 (P = .957; 95% CI, 0.261-4.13). An OR of successful (Groups A and B) to unsuccessful (Groups C and D) outcomes for Type I and II injuries versus Type III and IV injuries was calculated to be 3.83 (P = .074; 95% CI, 0.879-16.7).
Ten athletes received more than 1 PRP injection with a mean interinjection time of 156 days (range, 14-519 days). Of the 10 athletes, 7 underwent reconstructive UCL surgery, despite receiving multiple injections. Overall, 19 of the 50 athletes underwent surgical UCL reconstruction with a mean time of 208 days (range, 56-789 days) from PRP injection to surgery.
Discussion
Upon examination of Type IV UCL pathology in isolation, we observed a dismal 12.5% success rate, which was consistent with a number of studies that reported higher rates of nonoperative treatment failure in players with high-grade (complete or partial) tears on MRI.7,12,15,20,27 Meanwhile, exclusion of Type IV UCL injuries resulted in an overall increase in outcome success from 52% to 59.5%. This further reinforces the current understanding that PRP use in severe UCL injuries may have minimal clinical benefit.2,7,12,14,15,26 In such cases, immediate surgical intervention may ultimately prevent avoidable recovery time and expense. This is further illustrated by the OR that demonstrated patients with less severe (Type I or II) UCL injuries were 3.83 times more likely to return to their preinjury baseline than those with more severe (Type III or IV) injuries. Of note, examining lower-grade UCL injuries in isolation demonstrated a slight decrease in RTP rates in Type III (66.7%), Type II (62.5%), and Type I (56.5%) injuries, which can likely be explained by the small sample size of this study, as the difference in overall outcomes was marginal. Nevertheless, the RTP rates observed in this study surpass an initial report demonstrating a 42% RTP rate when a homogeneous rehabilitation program was used in the treatment of throwing athletes from various sports.27 These RTP rates also surpass those seen in a more recent report that examined outcomes of a rehabilitation program used in professional baseball players and demonstrated an RTP rate of 57%.7
In addition to the degree of injury, tear location has also been shown to affect outcome and RTP.7,17 Injury to the humeral origin may be most common in UCL injuries as suggested by the anatomical distribution of injuries in this study and several others.7,16,17,19,20,28 Edematous or low-grade, partial tear UCL injuries at the humeral origin (Type IH) were by far the most common type of UCL injury observed in this study (36%). Furthermore, humeral-origin tears comprised 69.2% of partial tears and 54% of all tears observed, which is consistent with a previous study that reported humeral-origin pathology of the UCL to be most common in patients undergoing primary surgical repair.28 This is clinically significant because both humeral- and ulnar-sided injuries are amenable to surgical and nonoperative interventions, but proximal tears generally have better outcomes.7,17 The calculated OR of 1.04 indicates a negligible practical difference in outcomes between these 2 sites of injury after receiving PRP therapy and rehabilitation. However, this value was not statistically significant (P = .957), which is likely explained by the small sample size of this study.
Twenty-four patients did not respond to PRP treatment when combined with physical therapy and rehabilitation. Of those 24 patients, 10 were unable to return to their preinjury level of play and 19 underwent subsequent UCL reconstructive surgery. The mean time from PRP injection to surgery was approximately 7 months. However, this ranged from 56 to 789 days, which was likely multifactorial with the patient’s age, level of competition, future career prospects, and response to rehabilitation. All of these factors likely contributed to the decision to pursue surgical intervention.
The interpretation of this study’s results is primarily limited by its small sample size and lack of a control group due to it being a retrospective observational study. The study’s small sample size significantly limits its power, which likely explains the lack of statistical significance demonstrated by the calculated OR. The lack of a control group makes it difficult to discern between the benefits of PRP therapy versus physical therapy and the rehabilitation protocol. Thus, it is not possible to accurately quantify the improvements and successes seen in this patient cohort.
This study also lacked uniformity in its patient cohort. Baseball players made up the overwhelming majority of the cohort, with only 2 participants being javelin throwers. This delineation between baseball and nonbaseball players is of importance because player position and sport have been shown to influence RTP.5,7,12 However, it is unlikely that the overall results of this study would have varied significantly if the 2 javelin throwers were excluded, because this demographic made up a miniscule portion of the patient population. Furthermore, they are considered high-velocity throwers and likely test the integrity and healing response of a PRP injection similarly to that of baseball players. This study’s patient cohort also included players from a broad range of competitive levels and different positions, which have been demonstrated to affect RTP rates and timeframes.7–9,12,13,16,17
The functional outcome classification system used in this study took into account whether each participant achieved RTP within 6 months, but exact timing was not recorded. Knowing each player’s exact RTP time would allow for comparison with the outcomes observed using other conservative management techniques. Furthermore, participants rarely lived within reasonable proximity to the clinic and were often dependent on their local physical therapist, athletic trainer, coach, or parent to ensure proper completion of their assigned rehabilitation protocol. Patients received detailed protocols and frequent demonstrations before their departure, but programs may have lacked uniformity in close follow-up and assistance. Thus, there was a potential for variability between the different physical therapy regimens and return to throwing protocols carried out by each participant. Additionally, the 2 javelin throwers were instructed to participate in all aspects of the prescribed rehabilitation protocol with the exception of the interval hitting program. It is unlikely this would significantly affect their recovery given that it was only 1 part in an extensive protocol, but it does introduce a degree of variability.
This study utilized a detailed PurePRP EmCyte protocol to prepare PRP, which includes estimates of PurePRP properties and concentrations. However, cell analysis was not conducted to verify the accuracy of these estimates due to this study’s being completed before the issuance of guidelines for minimal reporting of biologic product studies.24 For this reason, recipient comorbidities were not documented, which may have affected the results of this study. Consideration of these factors is potentially necessary for the replication and extrapolation of these results.
Local anesthetics were administered prior to PRP injection, which is a widely debated topic when it comes to PRP therapy. One study showed an in vitro reduction in platelet aggregation when local anesthetics (eg, lidocaine) were combined with PRP.3 Another observed decreased in vitro tenocyte proliferation when PRP was combined with local anesthetics.6 Before PRP injection, patients were locally anesthetized, using 1% lidocaine, superficially and down into the UCL substance to minimize patient discomfort. Volumes greater than 3 mL were used, which is slightly greater than the aforementioned studies and may explain the discrepancy in success rates.6,25 These studies indicate that the presence of local anesthetics may compromise the potential benefits of PRP therapy, but both were conducted in vitro and transposition of their results to in vivo human tissue is limited. Therefore, future investigation is warranted.
Conclusion
PRP treatment of Types I and II UCL tears shows great promise when combined with physical therapy and a rehabilitation program. Type III UCL tears demonstrated a high rate of success, although with low cohort numbers. Type IV UCL tears did not appear to respond well to PRP injection and often required surgical intervention or cessation of sport. Therefore, PRP treatment does not appear to be appropriate for patients with complete, Type IV UCL tears but may enhance recovery and improve outcomes in throwing athletes with Type I, II, and III UCL injuries.
Footnotes
Final revision submitted September 22, 2020; accepted October 23, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: A.K.M. has received consulting fees from Novartis. J.G.H. has received consulting fees from Avanos, Ferring, Fidia Pharma, Fujifilm, Sonosite, and Tenex. P.W.J. is a paid employee of PerfectACL App and has received consulting fees from DePuy Mitek, RTI Surgical Inc, and Amend Medical Inc. J.R.A. has received royalties from Biomet Sports Medicine; is a paid employee for Biomet Sports Medicine, Bauerfiend, Theralase, MiMedx, and Physiotherapy Associates; has received consulting fees from Biomet Sports Medicine, Bauerfiend, Theralase, and MiMedx; holds stock or stock options in Patient Connection and Connective Orthopaedics; and is on the board of FastHealth Corporation. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Baptist Hospital Institutional Review Board.
References
- 1. Anz AW, Hubbard R, Rendos NK, Everts PA, Andrews JR, Hackel JG. Bone marrow aspirate concentrate is equivalent to platelet-rich plasma for the treatment of knee osteoarthritis at 1 year: a prospective, randomized trial. Orthop J Sports Med. 2020;8(2):232596711990095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Arner JW, Chang ES, Bayer S, Bradley JP. Direct comparison of modified Jobe and docking ulnar collateral ligament reconstruction at midterm follow-up. Am J Sports Med. 2019;47(1):144–150. [DOI] [PubMed] [Google Scholar]
- 3. Bausset O, Magalon J, Giraudo L, et al. Impact of local anaesthetics and needle calibres used for painless PRP injections on platelet functionality. Muscles Ligaments Tendons J. 2014;4(1):18–23. [PMC free article] [PubMed] [Google Scholar]
- 4. Camp CL, Conte S, D’Angelo J, Fealy SA. Epidemiology of ulnar collateral ligament reconstruction in Major and Minor League Baseball pitchers: comprehensive report of 1429 cases. J Shoulder Elbow Surg. 2018;27(5):871–878. [DOI] [PubMed] [Google Scholar]
- 5. Camp CL, Dines JS, van der List JP, et al. Summative report on time out of play for Major and Minor League Baseball: An analysis of 49,955 injuries from 2011 through 2016. Am J Sports Med. 2018;46(7):1727–1732. [DOI] [PubMed] [Google Scholar]
- 6. Carofino B, Chowaniec DM, McCarthy MB, et al. Corticosteroids and local anesthetics decrease positive effects of platelet-rich plasma: an in vitro study on human tendon cells. Arthroscopy. 2012;28(5):711–719. [DOI] [PubMed] [Google Scholar]
- 7. Chauhan A, McQueen P, Chalmers PN, et al. Nonoperative treatment of elbow ulnar collateral ligament injuries with and without platelet-rich plasma in professional baseball players: a comparative and matched cohort analysis. Am J Sports Med. 2019;47(13):3107–3119. [DOI] [PubMed] [Google Scholar]
- 8. Ciccotti MG, Pollack KM, Ciccotti MC, et al. Elbow injuries in professional baseball: epidemiological findings from the Major League Baseball Injury Surveillance System. Am J Sports Med. 2017;45(10):2319–2328. [DOI] [PubMed] [Google Scholar]
- 9. Conte SA, Fleisig GS, Dines JS, et al. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am J Sports Med. 2015;43(7):1764–1769. [DOI] [PubMed] [Google Scholar]
- 10. Cugat R, Cuscó X, Seijas R, et al. Biologic enhancement of cartilage repair: the role of platelet-rich plasma and other commercially available growth factors. Arthroscopy. 2015;31(4):777–783. [DOI] [PubMed] [Google Scholar]
- 11. Deal JB, Smith E, Heard W, O’Brien MJ, Savoie FH. Platelet-rich plasma for primary treatment of partial ulnar collateral ligament tears: MRI correlation with results. Orthop J Sports Med. 2017;5(11):2325967117738238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dines JS, Williams PN, ElAttrache N, et al. Platelet-rich plasma can be used to successfully treat elbow ulnar collateral ligament insufficiency in high-level throwers. Am J Orthop (Belle Mead NJ). 2016;45(5):296–300. [PubMed] [Google Scholar]
- 13. Dodson CC, Slenker N, Cohen SB, Ciccotti MG, DeLuca P. Ulnar collateral ligament injuries of the elbow in professional football quarterbacks. J Shoulder Elbow Surg. 2010;19(8):1276–1280. [DOI] [PubMed] [Google Scholar]
- 14. Dugas JR. Ulnar collateral ligament repair: an old idea with a new wrinkle. Am J Orthop (Belle Mead NJ). 45(3):124–127. [PubMed] [Google Scholar]
- 15. Erickson BJ, Bach BR, Verma NN, Bush-Joseph CA, Romeo AA. Treatment of ulnar collateral ligament tears of the elbow: is repair a viable option? Orthop J Sports Med. 2017;5(1):2325967116682211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ford GM, Genuario J, Kinkartz J, Githens T, Noonan T. Return-to-play outcomes in professional baseball players after medial ulnar collateral ligament injuries: comparison of operative versus nonoperative treatment based on magnetic resonance imaging findings. Am J Sports Med. 2016;44(3):723–728. [DOI] [PubMed] [Google Scholar]
- 17. Frangiamore SJ, Lynch TS, Vaughn MD, et al. Magnetic resonance imaging predictors of failure in the nonoperative management of ulnar collateral ligament injuries in professional baseball pitchers. Am J Sports Med. 2017;45(8):1783–1789. [DOI] [PubMed] [Google Scholar]
- 18. Hurwit DJ, Garcia GH, Liu J, Altchek DW, Romeo A, Dines J. Management of ulnar collateral ligament injury in throwing athletes: a survey of the American Shoulder and Elbow Surgeons. J Shoulder Elbow Surg. 2017;26(11):2023–2028. [DOI] [PubMed] [Google Scholar]
- 19. Joyner PW, Bruce J, Hess R, Mates A, Mills FB, Andrews JR. Magnetic resonance imaging–based classification for ulnar collateral ligament injuries of the elbow. J Shoulder Elbow Surg. 2016;25(10):1710–1716. [DOI] [PubMed] [Google Scholar]
- 20. Kim NR, Moon SG, Ko SM, Moon W-J, Choi JW, Park J-Y. MR imaging of ulnar collateral ligament injury in baseball players: value for predicting rehabilitation outcome. Eur J Radiol. 2011;80(3):e422–e426. [DOI] [PubMed] [Google Scholar]
- 21. Lyras DN, Kazakos K, Verettas D, et al. The effect of platelet-rich plasma gel in the early phase of patellar tendon healing. Arch Orthop Trauma Surg. 2009;129(11):1577–1582. [DOI] [PubMed] [Google Scholar]
- 22. Mascarenhas R, Saltzman B, Fortier L, Cole B. Role of platelet-rich plasma in articular cartilage injury and disease. J Knee Surg. 2014;28(1):3–10. [DOI] [PubMed] [Google Scholar]
- 23. Mishra A, Harmon K, Woodall J, Vieira A. Sports medicine applications of platelet rich plasma. Curr Pharm Biotechnol. 2012;13(7):1185–1195. [DOI] [PubMed] [Google Scholar]
- 24. Murray IR, Geeslin AG, Goudie EB, Petrigliano FA, LaPrade RF. Minimum Information for Studies Evaluating Biologics in Orthopaedics (MIBO). J Bone Joint Surg Am. 2017;99(10):809–819. [DOI] [PubMed] [Google Scholar]
- 25. Podesta L, Crow SA, Volkmer D, Bert T, Yocum LA. Treatment of partial ulnar collateral ligament tears in the elbow with platelet-rich plasma. Am J Sports Med. 2013;41(7):1689–1694. [DOI] [PubMed] [Google Scholar]
- 26. Rebolledo BJ, Dugas JR, Bedi A, Ciccotti MG, Altchek DW, Dines JS. Avoiding Tommy John Surgery: what are the alternatives? Am J Sports Med. 2017;45(13):3143–3148. [DOI] [PubMed] [Google Scholar]
- 27. Rettig AC, Sherrill C, Snead DS, Mendler JC, Mieling P. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med. 2001;29(1):15–17. [DOI] [PubMed] [Google Scholar]
- 28. Savoie FH, Trenhaile SW, Roberts J, Field LD, Ramsey JR. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes. Am J Sports Med. 2008;36(6):1066–1072. [DOI] [PubMed] [Google Scholar]


