Abstract
Background:
Reducing the number of pitches thrown is regarded as the most effective way to prevent throwing injuries in youth baseball pitchers. However, few studies have compared the effectiveness of limiting the pitch count versus the limiting the number of innings pitched in terms of elbow injuries.
Hypothesis:
We hypothesized that, compared with inning limits, pitch count limits would lead to greater decreases in elbow pain, range of motion deficits, positive moving valgus stress test results, and the risk of capitellar osteochondritis dissecans (OCD).
Study Design:
Cohort study; Level of evidence, 3.
Methods:
This study retrospectively reviewed baseball pitchers aged 8 to 12 years in 2017 and 2018. Inning and pitch count limits in games were set to a daily maximum of 7 innings in 2017 and 70 pitches in 2018. Elbow pain, range of motion, and moving valgus stress test results were evaluated. The presence of capitellar OCD was assessed on ultrasonographic and radiographic images.
Results:
A total of 352 pitchers in 2017 and 367 pitchers in 2018 participated. The mean pitch count per game was lower in the pitch count limit (CL) group (52.5 ± 16.0) than in the inning limit (IL) group (98.2 ± 19.5) (P < .001). Compared with the IL group, the CL group had significantly lower rates of elbow pain (40.9% vs 31.9%, respectively; P = .01) and reduced flexion (19.0% vs 10.6%, respectively; P = .001). Multivariate analysis revealed a significant association between elbow pain and age in both the IL and the CL groups (P < .0001 and P = .02, respectively) and between OCD and elbow pain in the CL group (P = .04).
Conclusion:
A pitch count limit of ≤70 pitches per day for baseball pitchers ≤12 years could be more protective against elbow pain and reduced flexion than a limit of ≤7 innings per day, but it may not be effective for reducing the risk of capitellar OCD.
Keywords: pitch count, baseball, pitcher, prevention, OCD
Throwing injuries in young baseball players are a serious problem.32 Such injuries become evident at higher competition levels and are caused by cumulative, recurrent microtrauma from the repetitive, dynamic, overhead motion used in throwing.2,10,23 Epidemiological research has increasingly focused on throwing-related risk factors for injuries in youth and adolescent players.8,11,26,30,35,40 Some studies investigating elbow injuries in both pitchers and nonpitchers have shown that the incidence of elbow injuries is significantly higher in pitchers than in nonpitchers.11,21,26,30 Several risk factors, including skeletal immaturity, high pitch count, pitch type, pitch velocity, throwing mechanics, loss of shoulder motion, and elbow torque, have been shown to increase a pitcher’s risk of injuries.3,8,11,19,23,40 Based on these findings, several primary prevention strategies have been considered. Limiting the pitch count is regarded as the most effective way to prevent throwing injuries.7,17,40
The USA Baseball Medical and Safety Advisory Committee (MSAC) guidelines were developed in 2006 to provide recommendations for limiting the pitch count.42 Little League Baseball subsequently replaced its original inning limits with pitch count limits per game based on athlete age.1 Erickson et al4 suggested that compliance with recommended pitch count limits may be protective against subsequent ulnar collateral ligament reconstruction (UCLR). However, in a survey examining the understanding of and compliance with the USA Baseball MSAC pitching guidelines, Fazarale et al6 found that only 43% of coaches correctly answered questions about pitch count recommendations, even though 73% reported following established pitching rules.
The Japanese Society of Clinical Sports Medicine recommended limits of 50 pitches per day and 200 pitches per week in baseball players aged ≤12 years in 1995.16 Yukutake et al45 showed that, although the level of knowledge of recommendations in Japan was similar to that in the United States, compliance levels were far lower. The Japan Rubber Baseball Association established a pitching regulation that limited youth players to at most 7 innings per day in 2012. However, pitchers sometimes had pitch counts of ≥100 while remaining within the limit of 7 innings. In 2018, the Tokushima Prefecture branch of the Japan Rubber Baseball Association changed its pitch limit regulation to ≤70 pitches per day in pitchers ≤12 years.
The primary objective of this study was to compare the effectiveness of limiting the pitch count versus limiting the number of innings in terms of elbow injuries. Our hypothesis was that, compared with inning limits, pitch count limits would lead to greater decreases in elbow injuries.
Methods
The study protocol was approved by the institutional review board at our institution, and all parents and coaches provided informed consent. This cross-sectional, observational study involved baseball pitchers aged 8 to 12 years who participated in a regional summer championship for youth baseball teams in July 2017 and 2018. None of the participants had thrown curveballs or sliders; all had thrown fastballs or change-ups.
The pitching limit in all official games during the whole season was set to a daily maximum of 7 innings in 2017 and 70 pitches in 2018. In 2018, the rule was that a pitcher must throw no more than 70 pitches per game unless more was necessary to complete a batter’s plate appearance. Pitches thrown or signaled for the purpose of effecting an intentional walk were not counted against the overall pitch limits. If a pitcher reached the maximum number of pitches in a game during a batter’s plate appearance, the pitcher was allowed to continue until the end of that plate appearance. Official pitch counts were collected at each game by a designated scorekeeper.
Player information was collected using a questionnaire, followed by a physical examination and ultrasonographic and radiographic examinations to investigate the presence of capitellar osteochondritis dissecans (OCD). The questionnaires were distributed to team coaches, who asked players to complete them with the assistance of their coach and/or parents. The questionnaire asked players specifically whether they had any history of elbow pain during the season, where “elbow pain” was defined as any condition resulting in elbow pain lasting ≥1 week. Any injury that occurred via a mechanism such as trauma, including abrasions, bruising, dislocations, and fractures, was excluded. The questionnaire also gathered data on the player’s age, height, weight, whether the athlete was concomitantly playing as a catcher, number of months that the athlete had been playing baseball, and total number of maximum-effort pitches per day and per week in practice. The completed questionnaires, including written confirmation of the participant’s understanding of the questions, were returned by mail and reviewed by the first author (T.M.) for accuracy of the information provided. If inaccurate information was found, we followed up to obtain the correct information.
The physical examination included measurements of elbow range of motion and the moving valgus stress test. Reduced flexion/extension was regarded as positive if the difference between the throwing and nonthrowing elbows was more than 5°. The throwing elbow of each participant was examined by ultrasonography on the playing field. Ultrasonography of the lateral aspect of the elbow was performed by an orthopaedic surgeon with 5 years of experience performing elbow ultrasonography (T.I.) or by an ultrasound technician with 6 years of experience performing elbow imaging (S.N.). Both examiners were blinded to all clinical data.
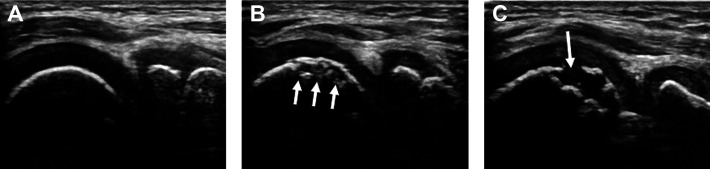
All ultrasound images were obtained using the following equipment: a sonographic diagnostic imaging system (Fazone M; Zonare Medical Systems) with a 5- to 10-MHz linear array transducer (Fazone CB; Fujifilm), a portable ultrasonographic system (MyLab Five; Esaote) with a 6- to 18-MHz linear array transducer, or an ultrasonographic system (M-Turbo; SonoSite) with a 6- to 13-MHz linear array transducer. Anterior views were acquired with the participant seated and the elbow fully extended. Posterior views were acquired with the elbow fully flexed to obtain an adequate view of the anterior aspect of the capitellum. Subchondral surface irregularity, a break in continuity of the echo line, or a double floor line in the subchondral bone of the capitellum was regarded as an irregularity (Figure 1).14,18,29
Figure 1.
Ultrasonographic images of the humeral capitellum of the right elbow. (A) A healthy capitellum showing a smooth echo line in the subchondral bone. (B) Subchondral surface irregularity (arrows). (C) A break in continuity of the echo line (arrow).
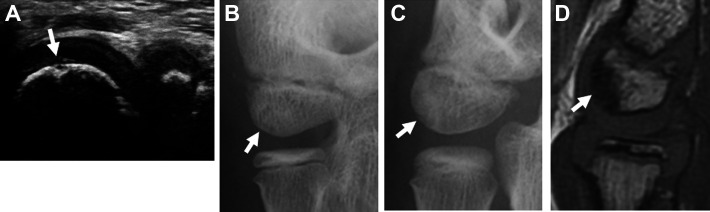
Players found to have an irregularity on the ultrasonographic examination were advised to undergo a radiographic examination. Radiography of the elbow was performed in the anteroposterior direction with the elbow extended and flexed at 45° as well as in the lateral and oblique directions. A board-certified musculoskeletal radiologist with 10 years of experience (S.T.) then compared the radiographic and ultrasonographic findings and confirmed the presence of capitellar OCD. OCD appears as a radiolucent area in the subchondral bone on the anterior aspect of the capitellum, in contrast to Panner disease, which is characterized by decreased size and irregular ossification of the entire capitellum.20 For players in whom the radiographic findings were normal or showed only subtle changes, magnetic resonance imaging was recommended to confirm OCD (Figure 2).
Figure 2.
Images of osteochondritis dissecans with a subtle change on radiograph of the right elbow. (A) Ultrasonographic image obtained during initial screening (posterior long-axis view). A subchondral surface irregularity (arrow) is present on the capitellum. (B) Anteroposterior radiograph with the elbow flexed at 45° and (C) oblique radiograph obtained at the initial examination show only a subtle change (arrow). (D) Sagittal T1-weighted magnetic resonance imaging shows low signal intensity in the subchondral bone of the capitellum (arrow).
Data Analysis
The interobserver variability of the 2 ultrasound examiners was preliminarily determined using the same images for 100 randomly selected patients. The interobserver reliability of the ultrasonographic examination was assessed using the kappa statistic.22 The kappa coefficient for interobserver agreement was graded as follows: ≤0.20, slight; 0.21 to 0.40, fair; 0.41 to 0.60, moderate; 0.61 to 0.80, substantial; and >0.80, almost perfect.
The data of the participants who followed the inning limit (IL group: ≤7 innings per day) and of those who followed the pitch count limit (CL group: ≤70 pitches per day) were statistically analyzed using SPSS software Version 20.0 (IBM). Univariate analyses were performed using the chi-square test for categorical variables and the Mann-Whitney U test for continuous variables. The level of statistical significance was set at P < .05.
We investigated the following potential risk factors for elbow pain: age, the Rohrer index (10 × weight/[height 3]), concomitantly playing as a catcher, number of months playing baseball in a lifetime, and adherence to maximum-effort pitches per day (≤50) and per week (≤200) in practice. To analyze the influence of elbow pain, participants were divided into 2 groups: those with negative elbow pain versus those with positive elbow pain for ≥1 week. The potential risk factors for OCD that were investigated were the same as those for elbow pain and also included elbow pain. Participants were divided into 2 groups: those who were negative versus those who were positive for OCD. The data were analyzed using multivariate logistic regression analysis and are shown as odds ratios (ORs) with 95% CIs. All statistical analyses were performed using SAS software Version 9.4 (SAS Institute). The critical value for statistical significance was set at P < .05.
Results
Of 115 teams, 90 (78.3%) were enrolled in this study with approval from parents and coaching staff. Players from these teams completed the questionnaire. A total of 352 pitchers in 2017 and 367 pitchers in 2018 participated. Of the 367 pitchers who participated in 2018, there were 145 pitchers (39.5%) who had participated in 2017. The mean pitch count per game in the CL group (52.5 ± 16.0) was significantly lower than in the IL group (98.2 ± 19.5) (P < .001). There were no statistically significant differences between the 2 groups in age, height, weight, length of baseball experience, concomitantly playing as a catcher, or adherence to pitch count limits in practice (Table 1).
Table 1.
Baseline Characteristics of Pitchersa
| IL Group (n = 352) | CL Group (n = 367) | P | |
|---|---|---|---|
| Age, y | 10.7 ± 1.0 | 10.7 ± 0.9 | .93 |
| Height, cm | 142.9 ± 8.5 | 142.9 ± 8.2 | .93 |
| Weight, kg | 36.8 ± 8.1 | 36.6 ± 7.6 | .86 |
| Length of baseball experience, mo | 37.4 ± 13.7 | 38.6 ± 13.9 | .32 |
| Concomitantly playing as catcher, n (%) | 143 (40.6) | 166 (45.2) | .23 |
| Adherence to daily pitch count limit in practice (≤50 pitches), n (%) | 252 (71.6) | 242 (65.9) | .11 |
| Adherence to weekly pitch count limit in practice (≤200 pitches), n (%) | 309 (87.8) | 324 (88.3) | .91 |
| Pitch count per game | 98.2 ± 19.5 | 52.5 ± 16.0 | <.001 |
aValues are reported as mean ± SD unless otherwise indicated. Bolded P value indicates a statistically significant difference between groups (P < .05). CL, pitch count limit; IL, inning limit.
The prevalence of elbow pain within 12 months (31.9%) and of reduced flexion (10.6%) was significantly lower in the CL group than in the IL group (40.9% [P = .01] and 19.0% [P = .001], respectively). There were no statistically significant differences in the prevalence of reduced extension or positive moving valgus stress test results between the 2 groups (Table 2).
Table 2.
Elbow Pain, Range of Motion, and Moving Valgus Stress Test Resultsa
| IL Group (n = 352) | CL Group (n = 367) | P | |
|---|---|---|---|
| Elbow pain | 144 (40.9) | 117 (31.9) | .01 |
| Reduced extension | 36 (10.2) | 26 (7.1) | .15 |
| Reduced flexion | 67 (19.0) | 39 (10.6) | .001 |
| Positive moving valgus stress test finding | 54 (15.3) | 54 (14.7) | .84 |
| OCD | 6 (1.7) | 9 (2.5) | .61 |
aValues are reported as n (%). Bolded P values indicate a statistically significant difference between groups (P < .05). CL, pitch count limit; IL, inning limit; OCD, osteochondritis dissecans.
The kappa coefficient for interobserver reliability of the ultrasonographic examinations was 0.82 (95% CI, 0.82-0.17; P < .001), indicating almost-perfect agreement. In the IL group, ultrasonography revealed irregularities in the subchondral bone of the capitellum in 7 of 352 players (2.0%), and all agreed to undergo radiography. Of these 7 players, 6 (85.7%) had OCD. In the CL group, ultrasonography revealed irregularities in the subchondral bone of the capitellum in 10 of 367 players (2.7%), and all agreed to undergo radiography. Of these 10 players, 9 (90.0%) had OCD. There were no statistically significant differences in the prevalence of OCD between the 2 groups (Table 2).
Potential risk factors associated with elbow pain in the IL and CL groups are summarized in Table 3. In the IL group, multivariate analysis revealed a significant association between elbow pain and age (OR, 1.87 [95% CI, 1.43-2.47]) but no significant association between elbow pain and length of baseball experience, Rohrer index, concomitantly playing as a catcher, or adherence to daily and weekly maximum-effort pitch count limits in practice. In the CL group, multivariate analysis revealed a significant association between elbow pain and age (OR, 1.42 [95% CI, 1.05-1.93]) but no significant association between elbow pain and length of baseball experience, Rohrer index, concomitantly playing as a catcher, or adherence to daily and weekly maximum-effort pitch count limits in practice.
Table 3.
Risk Factors for Elbow Paina
| IL Group | CL Group | |||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| Age | 1.87 (1.43-2.47) | <.0001 | 1.42 (1.05-1.93) | .02 |
| Length of baseball experience (>1 mo) | 1.02 (1.00-1.04) | .08 | 1.02 (1.00-1.04) | .07 |
| Rohrer index | 0.99 (0.98-1.01) | .23 | 1.01 (1.00-1.03) | .16 |
| Concomitantly playing as catcher | 1.16 (0.72-1.86) | .54 | 1.28 (0.81-2.04) | .29 |
| Adherence to daily pitch count limit | 1.02 (0.76-1.36) | .91 | 0.95 (0.69-1.30) | .74 |
| Adherence to weekly pitch count limit | 1.05 (0.76-1.44) | .77 | 1.30 (0.94-1.81) | .12 |
aBolded P values indicate a statistical significance (P < .05). CL, pitch count limit; IL, inning limit; OR, odds ratio.
The potential risk factors associated with OCD in the 2 groups are summarized in Table 4. In the IL group, multivariate analysis revealed no significant association between OCD and age, length of baseball experience, Rohrer index, concomitantly playing as a catcher, adherence to daily and weekly maximum-effort pitch count limits in practice, or elbow pain. In the CL group, multivariate analysis revealed a significant association between OCD and elbow pain (OR, 5.77 [95% CI, 1.29-40.42]) but not between OCD and age, length of baseball experience, Rohrer index, concomitantly playing as a catcher, or adherence to daily and weekly maximum-effort pitch count limits in practice.
Table 4.
Risk Factors for OCDa
| IL Group | CL Group | |||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| Age | 2.35 (0.77-8.81) | .15 | 0.98 (0.33-2.91) | .96 |
| Length of baseball experience (>1 mo) | 1.01 (0.95-1.09) | .71 | 1.06 (1.00-1.14) | .07 |
| Rohrer index | 1.03 (0.99-1.07) | .11 | 1.02 (0.98-1.06) | .25 |
| Concomitantly playing as catcher | 0.98 (0.16-5.76) | .98 | 1.16 (0.29-5.04) | .83 |
| Adherence to daily pitch count limit | 0.43 (0.07-2.49) | .32 | 1.82 (0.41-10.34) | .45 |
| Adherence to weekly pitch count limit | 1.12 (0.15-23.63) | .92 | 0.68 (0.12-5.47) | .67 |
| Elbow pain | 1.02 (0.17-6.05) | .99 | 5.77 (1.29-40.42) | .04 |
aBolded P value indicates a statistical significance (P < .05). CL, pitch count limit; IL, inning limit; OCD, osteochondritis dissecans; OR, odds ratio.
Discussion
This study showed that a pitch count limit of ≤70 pitches per day for baseball pitchers ≤12 years could be more protective against elbow pain and reduced flexion than a limit of ≤7 innings per day. A unique aspect of the study was the comparison of the elbow injury rate under an inning limit versus a pitch count limit. Few surveys of this nature have been performed among youth baseball players. Another unique aspect was that the study involved Japanese participants. In 1983, Iwase et al15 retrospectively examined 1932 Japanese youth baseball players ≤12 years. They reported that the prevalence of radiographic abnormalities in pitchers and fielders was 38% and 10%, respectively, and that the average maximum-effort pitches/throws per day in pitchers and fielders was 147 and 56, respectively. They recommended a maximum of 50 pitches per day and 200 pitches per week. The Japanese Society of Clinical Sports Medicine adopted these recommendations in 1995.16 In a prospective study, Matsuura et al31 examined the same recommendations in youth players without elbow pain and found that the recommendations were appropriate. However, in 2012, the Japan Rubber Baseball Association established a pitching rule for youth players that was based on a limit of 7 innings rather than on a pitch count limit. The present study found that the mean pitch count per pitcher per game was 98.2 in 2017 (Table 1). The Tokushima Prefecture branch of the Japan Rubber Baseball Association judged that a rule change from the inning limit to a pitch count limit was necessary. Therefore, in 2018, this branch changed the rule to a pitch count limit of ≤70 pitches per day for players ≤12 years. The choice of 70 pitches was a compromise between sports medicine providers and coaches.
The principal findings of this investigation were that a history of elbow pain in the past year and reduced flexion were significantly lower in the CL group than in the IL group. Our data indicate that the pitch count limit of ≤70 pitches per day was more protective against elbow injuries than the limit of ≤7 innings per day. A higher pitch count requires a repetitive, dynamic, overhead-throwing motion. As a result, it is thought that a higher pitch count causes a higher incidence of elbow pain and reduced flexion. A few studies have examined the effectiveness of pitch count limits. Erickson et al4 sought to determine whether Little League Baseball World Series pitchers continued on to play professional baseball and whether these professional players underwent UCLR. Only 10% of 638 pitchers progressed to professional play, and the results suggested that compliance with pitch limit recommendations may be protective against subsequent UCLR.4 Compared with their study, most pitchers were nonelite in our study. Although the daily maximum pitch count limit in our study (70 pitches) was lower than that of Erickson et al4 (85 pitches), there were no statistically significant differences in reduced extension or positive moving valgus stress test results between the IL and CL groups (Table 2). Our study did not address some issues, including pitches thrown per season,23,24 bullpen sessions or warm-up throws,43 days of rest, and showcases. These factors might have affected the results. Also, a decision is needed on the number of pitches that youth players may actually make in a season.
Age was strongly associated with elbow pain in this study, but length of baseball experience was not. There may have been a type II error in the results for the length of baseball experience because the P values were almost <.05. The relationship between age and risk of arm problems and/or injuries has been frequently reported, with older age shown to be associated with a higher incidence of arm pain.23,26,40 This increase was found to occur during a 3- to 4-year time frame between the ages of 8 and 12 years, which might have important implications. It is possible that older players are more skillful.8,24,34 Older players are also likely to be stronger and capable of generating greater loads on the joint/soft tissue structures than younger players. A further hypothesis focuses on secondary ossification centers,24 which start to ossify between the ages of 2 and 11 years and do not fuse to the long bones until as late as 17 years of age. There may be up to 6 secondary ossification centers present in the elbow of a 12-year-old boy. These centers are the most vulnerable points in the young elbow and can become inflamed and irritated by the pitching motion.24
Our study did not find a significant association between concomitantly playing as a catcher and experiencing elbow pain. Other Japanese studies have reported risk factors associated with elbow pain including playing as a pitcher and catcher.25,40 In a study on pitchers, Fleisig et al8 showed that those who concomitantly played as a catcher became injured more frequently, but this trend was not statistically significant. Concomitantly playing as a catcher was shown not to be a risk factor for UCLR by Erickson et al.4 Recently, in a systematic review and meta-analysis involving adolescent baseball pitchers, Salamh et al37 also found that playing catcher as a secondary position was not a statistically significant risk factor for elbow injuries.
Although pitch limit recommendations may be protective against elbow injuries,5,31 these limits are meaningless without strict compliance. In previous studies, coaches in the United States correctly answered 43% of questions regarding pitch counts and rest periods, whereas only 28% of coaches in Japan complied with the recommendations.6,45 Adherence to daily or weekly pitch count limits in practice (65.9%-88.3%) in our study was higher than in other studies, and we found no correlation between adherence to pitch count limits and elbow pain. In a study on Little League pitchers, Pytiak et al36 found that 28% of the pitchers experienced pain during the season, even though the league fully complied with pitch count regulations. They pointed to year-round play as the reason. In fact, the players in our study played year-round, which might explain why no correlation was found between adherence to pitch count limits and elbow pain.
Capitellar OCD does not occur frequently but, if advanced, could entail prolonged absence from sports activity.28,33 Our study found no statistically significant differences in the prevalence of OCD between the IL and CL groups (see Table 2). Repetitive throwing is considered one of the main etiological factors for capitellar OCD. However, a study showed that starting baseball earlier in life, a greater number of years played, and more training hours indicating repetitive valgus stress were not significantly associated with capitellar OCD.27 Taken together, these findings suggest that the cause of capitellar OCD likely includes a combination of repetitive microtrauma and internal factors such as ischemia12 and a genetic predisposition.9,39 In the present cross-sectional study, OCD in the CL group was significantly associated with elbow pain. However, in a prospective study, Matsuura et al27 demonstrated that elbow pain was not associated with OCD. They also reported that age of 10 to 11 years was the only factor significantly associated with an increased risk of capitellar OCD,27 although the current study did not find that age was significantly associated with OCD. Their findings and the fact that the present study had a cross-sectional design indicate the need for further longitudinal, multiregional studies to reach a firm conclusion regarding the association between age or elbow pain and capitellar OCD.
Although this study adds new information, it has several limitations. The first limitation is participant selection. Of 367 pitchers who participated in 2018, there were 145 pitchers (39.5%) who participated in 2017. If pitchers experienced elbow pain in the first year, some of them may have modified their playing style and tried as much as possible not to pitch. As a result, players’ experience in the first year would have affected the results in the second year. Similarly, pitchers in the second year had experienced higher pitch counts in the previous season, which may have contributed to loss of motion and the presence of OCD. The second limitation is the retrospective cohort design and the fact that the results were self-reported by young participants. Recall bias may have been introduced when the players were asked about their history of elbow pain. The study may also have yielded more robust information if the questionnaire had covered information such as the characteristics and intensity of elbow pain and the time taken to return to baseball. Recall bias was also likely present because some coaches were the ones who reported the maximum-effort pitch count per day and week in practice, even though they reported that they did not always keep track of pitch counts. The third limitation is that we did not study other potential risk factors such as physical conditioning and pitching mechanics. The physical examination did not include factors such as glenohumeral internal rotation deficit, loss of full range of motion at the shoulder, humeral retroversion, and scapular dysfunction. Greater emphasis is now placed on variations in these physical factors13,38,41,44 as potential contributors to an increased risk of injuries. Fourth, radiographs were obtained only from players with positive ultrasonographic findings, raising the possibility of false-negative results. Finally, because all the players were from a single geographic region in Japan, the generalizability of the findings to other populations or geographic areas is unknown. Future multicenter studies are needed to draw firm conclusions on pitch count limits in youth baseball players.
Conclusion
This study’s results indicated that a pitch count limit of ≤70 pitches per day in baseball players ≤12 years could be more protective against elbow pain and reduced flexion than a limit of ≤7 innings per day. However, continued research is necessary to establish evidence-based strategies for optimizing the pitch count limit for youth baseball pitchers while minimizing pitching-related injuries.
Acknowledgment
The authors thank Takenobu Iwase, MD, and Shinji Kashiwaguchi, MD, from the Department of Orthopaedic Surgery, Tokushima National Hospital, for their assistance with initial project planning and the study design.
Footnotes
Final revision submitted September 24, 2020; accepted October 23, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Tokushima University Hospital.
References
- 1. American Sports Medicine Institute. Position statement for adolescent baseball pitchers. Accessed November 17, 2017. http://www.asmi.org/research.php?page=research§ion=positionStatement
- 2. Andrews JR, Fleisig GS. Preventing throwing injuries. J Orthop Sports Phys Ther. 1998;27(3):187–188. [DOI] [PubMed] [Google Scholar]
- 3. Anz AW, Bushnell BD, Griffin LP, Noonan TJ, Torry MR, Hawkins RJ. Correlation of torque and elbow injury in professional baseball pitchers. Am J Sports Med. 2010;38(7):1368–1374. [DOI] [PubMed] [Google Scholar]
- 4. Erickson BJ, Chalmers PN, Axe MJ, Romeo AA. Exceeding pitch count recommendations in Little League baseball increases the chance of requiring Tommy John surgery as a professional baseball pitcher. Orthop J Sports Med. 2017;5(3):2325967117695085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Erickson BJ, Harris JD, Tetreault M, Bush-Joseph C, Cohen M, Romeo AA. Is Tommy John surgery performed more frequently in Major League Baseball pitchers from warm weather areas? Orthop J Sports Med. 2014;2(10):2325967114553916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fazarale JJ, Magnussen RA, Pedroza AD, Kaeding CC, Best TM, Classie J. Knowledge of and compliance with pitch count recommendations: a survey of youth baseball coaches. Sports Health. 2012;4(3):202–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fleisig GS, Andrews JR. Prevention of elbow injuries in youth baseball pitchers. Sports Health. 2012;4(5):419–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fleisig GS, Andrews JR, Cutter GR, et al. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med. 2011;39(2):253–257. [DOI] [PubMed] [Google Scholar]
- 9. Gardiner TB. Osteochondritis dissecans in three members of one family. J Bone Joint Surg Br. 1955;37(1):139–141. [DOI] [PubMed] [Google Scholar]
- 10. Grana WA, Rashkin A. Pitcher’s elbow in adolescents. Am J Sports Med. 1980;8(5):333–336. [DOI] [PubMed] [Google Scholar]
- 11. Harada M, Takahara M, Mura N, Sasaki J, Ito T, Ogino T. Risk factors for elbow injuries among young baseball players. J Shoulder Elbow Surg. 2010;19(4):502–507. [DOI] [PubMed] [Google Scholar]
- 12. Haraldsson S. On osteochondrosis deformas juvenilis capituli humeri including investigation of intra-osseous vasculature in distal humerus. Acta Orthop Scand Suppl. 1959;38:1–232. [PubMed] [Google Scholar]
- 13. Hibberd EE, Oyama S, Myers JB. Increase in humeral retrotorsion accounts for age-related increase in glenohumeral internal rotation deficit in youth and adolescent baseball players. Am J Sports Med. 2014;42(4):851–858. [DOI] [PubMed] [Google Scholar]
- 14. Iwame T, Matsuura T, Suzue N, Tamaki S, Yokoyama K, Sairyo K. Two-year follow-up study of subchondral surface irregularities of the capitellum on ultrasonography in baseball players under the age of 10 years. Skeletal Radiol. 2017;46(11):1499–1505. [DOI] [PubMed] [Google Scholar]
- 15. Iwase T, Otomune T, Kuge A. Epidemiology of Little League elbow [in Japanese]. Seikeigeka MOOK. 1983;27:61–82. [Google Scholar]
- 16. Japanese Society of Clinical Sports Medicine. Guideline for youth baseball players. Accessed October 17, 2012. https://www.rinspo.jp/pdf/proposal_03-1.pdf
- 17. Kerut EK, Kerut DG, Fleisig GS, Andrews JR. Prevention of arm injury in youth baseball pitchers. J La State Med Soc. 2008;160(2):95–98. [PubMed] [Google Scholar]
- 18. Kida Y, Morihara T, Kotoura Y, et al. Prevalence and clinical characteristics of osteochondritis dissecans of the humeral capitellum among adolescent baseball players. Am J Sports Med. 2014;42(8):1963–1971. [DOI] [PubMed] [Google Scholar]
- 19. Klingele KE, Kocher MS. Little League elbow: valgus overload injury in the paediatric athlete. Sports Med. 2002;32(15):1005–1015. [DOI] [PubMed] [Google Scholar]
- 20. Kobayashi K, Burton KJ, Rodner C, Smith B, Caputo AE. Lateral compression injuries in the pediatric elbow: Panner’s disease and osteochondritis dissecans of the capitellum. J Am Acad Orthop Surg. 2004;12(4):246–254. [DOI] [PubMed] [Google Scholar]
- 21. Krajnik S, Fogarty KJ, Yard EE, Comstock RD. Shoulder injuries in US high school baseball and softball athletes, 2005-2008. Pediatrics. 2010;125(3):497–501. [DOI] [PubMed] [Google Scholar]
- 22. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 23. Lyman S, Fleisig GS, Andrews JR, Osinski ED. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30(4):463–468. [DOI] [PubMed] [Google Scholar]
- 24. Lyman S, Fleisig GS, Waterbor JW, et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001;33(11):1803–1810. [DOI] [PubMed] [Google Scholar]
- 25. Matsuura T, Chosa E, Tajika T, et al. Correlation between playing position, elbow physical findings and elbow pain in elementary school baseball players: results of a multi-regional study in Japan. J Orthop Sci. 2020;25(1):122–126. [DOI] [PubMed] [Google Scholar]
- 26. Matsuura T, Iwame T, Suzue N, Arisawa K, Sairyo K. Risk factors for shoulder and elbow pain in youth baseball players. Phys Sportsmed. 2017;45(2):140–144. [DOI] [PubMed] [Google Scholar]
- 27. Matsuura T, Iwame T, Suzue N, et al. Cumulative incidence of osteochondritis dissecans of the capitellum in preadolescent baseball players. Arthroscopy. 2019;35(1):60–66. [DOI] [PubMed] [Google Scholar]
- 28. Matsuura T, Kashiwaguchi S, Iwase T, Takeda Y, Yasui N. Conservative treatment for osteochondrosis of the humeral capitellum. Am J Sports Med. 2008;36(5):868–872. [DOI] [PubMed] [Google Scholar]
- 29. Matsuura T, Suzue N, Iwame T, Nishio S, Sairyo K. Prevalence of osteochondritis dissecans of the capitellum in young baseball players: results based on ultrasonographic findings. Orthop J Sports Med. 2014;2(8):2325967114545298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Matsuura T, Suzue N, Kashiwaguchi S, Arisawa K, Yasui N. Elbow injuries in youth baseball players without prior elbow pain: a 1-year prospective study. Orthop J Sports Med. 2013;1(5):2325967113509948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Matsuura T, Suzue N, Kashiwaguchi S, Iwase T, Arisawa K, Yasui N. Prospective study of elbow pain and verification of guideline in schoolchild baseball players [in Japanese]. Jpn J Orthop Sports Med. 2012;32:242–247. [Google Scholar]
- 32. Melugin HP, Leafblad ND, Camp CL, Conte S. Injury prevention in baseball: from youth to the pros. Curr Rev Musculoskelet Med. 2018;11(1):26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mihara K, Tsutsui H, Nishinaka N, Yamaguchi K. Nonoperative treatment for osteochondritis dissecans of the capitellum. Am J Sports Med. 2009;37(2):298–304. [DOI] [PubMed] [Google Scholar]
- 34. Olsen SJ, 2nd, Fleisig GS, Dun S, Loftice J, Andrews JR. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34(6):905–912. [DOI] [PubMed] [Google Scholar]
- 35. Otoshi K, Kikuchi S, Kato K, et al. Age-specific prevalence and clinical characteristics of humeral medial epicondyle apophysitis and osteochondritis dissecans: ultrasonographic assessment of 4249 players. Orthop J Sports Med. 2017;5(5):2325967117707703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Pytiak AV, Stearns P, Bastrom TP, et al. Are the current Little League pitching guidelines adequate? A single-season prospective MRI study. Orthop J Sports Med. 2017;5(5):2325967117704851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Salamh P, Jones E, Bashore M, Liu X, Hegedus EJ. Injuries and associated risk factors of the shoulder and elbow among adolescent baseball pitchers: a systematic review and meta-analysis. Phys Ther Sport. 2020;43:108–119. [DOI] [PubMed] [Google Scholar]
- 38. Shanley E, Kissenberth MJ, Thigpen CA, et al. Preseason shoulder range of motion screening as a predictor of injury among youth and adolescent baseball pitchers. J Shoulder Elbow Surg. 2015;24(7):1005–1013. [DOI] [PubMed] [Google Scholar]
- 39. Stougaard J. Familial occurrence of osteochondritis dissecans. J Bone Joint Surg Br. 1964;46:542–543. [PubMed] [Google Scholar]
- 40. Takagishi K, Matsuura T, Masatomi T, et al. Shoulder and elbow pain in elementary school baseball players: the results from a nation-wide survey in Japan. J Orthop Sci. 2017;22(4):682–686. [DOI] [PubMed] [Google Scholar]
- 41. Trakis JE, McHugh MP, Caracciolo PA, Busciacco L, Mullaney M, Nicholas SJ. Muscle strength and range of motion in adolescent pitchers with throwing-related pain: implications for injury prevention. Am J Sports Med. 2008;36(11):2173–2178. [DOI] [PubMed] [Google Scholar]
- 42. USA Baseball. Youth baseball pitching injuries. Accessed December 1, 2013. https://www.usabaseball.com/news/youth-baseball-pitching-injuries/c-246193056
- 43. Wahl EP, Pidgeon TS, Richard MJ. Youth baseball pitch counts vastly underestimate high-effort throws throughout a season. J Pediatr Orthop. 2020;40(7):e609–e615. [DOI] [PubMed] [Google Scholar]
- 44. Whiteley RJ, Adams RD, Nicholson LL, Ginn KA. Reduced humeral torsion predicts throwing-related injury in adolescent baseballers. J Sci Med Sport. 2010;13(4):392–396. [DOI] [PubMed] [Google Scholar]
- 45. Yukutake T, Yamada M, Aoyama T. A survey examining the correlations between Japanese Little League baseball coaches’ knowledge of and compliance with pitch count recommendations and player elbow pain. Sports Health. 2013;5(3):239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]