Abstract
Giardia lamblia (also referred to as Giardia intestinalis and Giardia duodenalis) is the most common intestinal parasite in the world, affecting approximately 200 million people annually. Symptoms of Giardia include foul-smelling diarrhea, abdominal cramping, bloating, gas, and nausea. Although usually self-limiting, Giardia can progress to dehydration, malnutrition, and failure to thrive, especially in immunocompromised individuals. Early diagnosis and treatment is imperative to prevent and control infection of Giardia. Infectious Disease Society of America diagnostic guidelines recommend obtaining stool studies to diagnose Giardia; when stool studies are negative but suspicion remains high, duodenal aspirate microscopy is the only alternative diagnostic strategy suggested. We report a patient diagnosed incidentally with Giardia from a duodenal biopsy specimen obtained during a workup for a gastrointestinal bleed. There are limited cases of Giardia diagnosed by duodenal biopsy reported in the literature. We review studies that suggest duodenal biopsy can be a very sensitive strategy for the diagnosis of Giardia.
Keywords: Giardia lamblia, Giardia intestinalis, Giardia duodenalis, Giardiasis, Giardia, duodenum, duodenal biopsy
Introduction
Giardia lamblia is the most common intestinal parasite worldwide.1 Giardia is transmitted fecal to orally, most often by ingestion of contaminated food or water.2 Symptoms usually appear 1 to 3 weeks after exposure and include abdominal pain, large volume watery and foul-smelling diarrhea, nausea, flatulence, and bloating.2 Giardia usually clears on its own; however, some cases can lead to malnutrition, failure to thrive, and growth retardation.2 Immunocompromised individuals and undernourished children from developing countries are more susceptible to serious manifestations of untreated Giardia.3,4 Due to unsafe watery supply, sanitation, and hygiene, the prevalence of Giardia in the developing world is estimated to be 20% to 30%.3,4 In industrialized countries, prevalence is estimated to be 2% to 5%.3,4 Patients at most risk from industrialized countries include those who work in childcare settings, backpackers, and campers.1
In clinical settings, Giardia is most often diagnosed by stool antigen detection or nucleic acid amplification testing (NAAT), consistent with Infectious Disease Society of America (IDSA) diagnostic guidelines.5 IDSA guidelines recommend duodenal aspirate microscopy when stool studies are nondiagnostic but suspicion for Giardia remains high.6 Duodenal biopsy is not a common tool to diagnose Giardia. We report a patient who presented with diarrhea and bright red blood per rectum; he underwent an esophagogastroduodenoscopy (EGD) with duodenal biopsy in the workup of a gastrointestinal bleed. His biopsy specimen incidentally revealed Giardia trophozoites adherent to the duodenal mucosa.
Case Presentation
A 59-year-old man with history of alcoholic cirrhosis, chronic hepatitis C, and hepatocellular carcinoma presented with 2 weeks of abdominal distention, watery diarrhea, and prior to arrival, a half cup of bright red blood per rectum. He did not endorse recent travel, camping, backpacking, working in childcare settings, or exposure to animals. On arrival, he was mildly tachycardic, and physical examination was notable for moderate ascites. Early laboratory findings were notable for a leukocytosis of 12 800/mm3, hemoglobin of 10.1 g/dL, from a baseline of 14.8 g/dL, and an acutely elevated lactate of 3.5 mmol/L. Liver function tests were baseline. Stool leukocytes, stool culture, and Clostridium difficile toxin were negative. Abdominal ultrasound confirmed a small amount of ascites not amenable for paracentesis. He was given an empiric dose of ceftriaxone for spontaneous bacterial peritonitis and taken for EGD and colonoscopy for a suspected gastrointestinal bleed.
Esophagogastroduodenoscopy was significant for a few nonbleeding healing ulcers in the gastric antrum. Findings were otherwise normal. Biopsies were obtained from the duodenal bulb (Figure 1) and mid duodenum (Figure 2) to rule out celiac disease. Colonoscopy was significant for a small, nonbleeding cecal angiectasia, polyps in the cecum, ascending colon and rectum, and internal hemorrhoids. He was discharged the next day after spontaneous resolution of his symptoms. His duodenal biopsy specimens later revealed superficially adherent Giardia trophozoites over a backdrop of normal villous architecture. He was treated outpatient with 2 g of tinidazole.
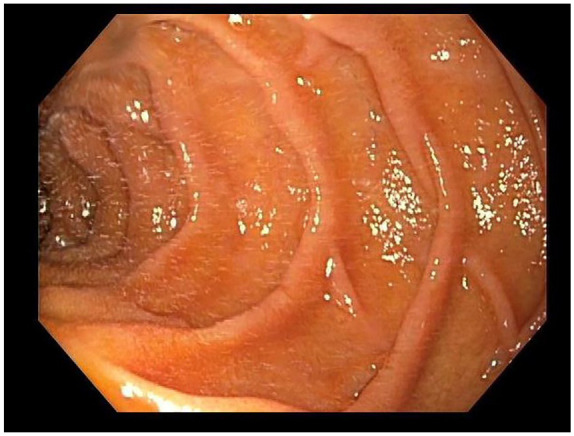
Figure 1.

Duodenal bulb, region from which where the first biopsy was obtained.
Figure 2.
Mid duodenum, region from which where the second biopsy was obtained.
Discussion
Several stool-based assays are used to diagnose Giardia. Stool antigen tests and NAAT are the most commercially available and rapid assays used in clinical settings.7 Stool antigen testing is ideal when Giardia is specifically suspected, such as in outbreak scenarios.7 NAAT, or DNA polymerase chain reaction (PCR) testing, is better suited when evaluating for multiple potential causes of infectious diarrhea, as PCR panels can detect bacterial, viral, and parasitic pathogens.7 Although Giardia trophozoites and cysts can be identified by stool microscopy, this is a timely and insensitive method that sometimes requires examination of up to 3 stool specimens.7 Sensitivity is approximately 60% to 80% with 1 stool specimen, 80% to 90% with 2 samples, and over 90% with 3 samples.5 Sensitivity is affected by severity of diarrhea due to dilution of the parasite.5
According to IDSA guidelines, duodenal aspirate microscopy can be pursued in patients with suspected Giardia, Strongyloides, Crystoisopora, or Microsporidia infection but negative stool studies.6 Duodenal aspirate microscopy is sensitive because trophozoites are abundant in proximal small bowel and recognized easily because of their motility.8 The clear and liquid appearance of aspirate fluid also facilitates recognition of trophozoites.8 Only 2 to 3 mL of duodenal fluid is required for this technique.8 Two drops can be placed on a clean glass slide and examined under low-power magnification (×100) for diagnosis; 4 negative specimens are usually sufficient to rule out Giardia infection.8 Duodenal aspirate microscopy has few contraindications or complications.8
Duodenal biopsy is a less practiced method of Giardia identification and not included in IDSA diagnostic guidelines.6 Diagnosis requires careful examination of several biopsy sections. Trophozoites are usually appreciated on the surface of duodenal mucosa; however, there are some reports of Giardia invading intestinal mucosa.8 Recognition of trophozoites is often time consuming because not all sections will contain parasite.8 Additionally, Giardia can be misidentified as host cell when only part of the trophozoite is seen.8 Histological changes associated with Giardia are nonspecific and cannot be used to establish a diagnosis.8 The characteristic appearance of a Giardia trophozoite is a pear-shaped organism with paired flagella and nuclei.9
All 3 methods have their uses and limitations. Multiple studies have compared the efficacy of duodenal biopsy with stool studies and duodenal aspirate microscopy. Gupta et al reported 161 children with Giardia, all cases diagnosed by duodenal aspirate were also diagnosed by duodenal biopsy, suggesting duodenal biopsy has noninferior diagnostic sensitivity to duodenal aspirate microscopy.10 Watson et al reported 3 cases of Giardia diagnosed by duodenal biopsy; only one of those cases was confirmed by duodenal aspirate microscopy.11 Wahnschaffe et al reported 16 patients with Giardia diagnosed by stool testing; 8 cases were confirmed by duodenal biopsy but only 3 by duodenal aspirate.12 Kamath and Murugasu reported 21 children with suspected Giardia, duodenal biopsy confirmed infection in 12, while duodenal aspirate and stool microscopy were positive in only 10 and 6, respectively.8 These studies suggest that duodenal biopsy has the potential to be more sensitive in diagnosing Giardia than the more accepted methods.
Conclusion
In conclusion, we report a rare case of Giardia diagnosed incidentally by duodenal biopsy. Current IDSA guidelines do not recommend duodenal biopsy for the diagnosis of Giardia; however, multiple studies demonstrate that duodenal biopsy can be a very sensitive diagnostic strategy. Clinicians should consider performing a duodenal biopsy when stool studies and duodenal aspirate microscopy are negative but suspicion for Giardia remains high.
Footnotes
Authors’ Note: Previous presentation: This case was presented in part as a poster at the ACG 2020 Virtual Annual Meeting; October 23 to 28, 2020.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Our institution does not require ethical approval for reporting individual cases reports.
Informed Consent: Informed consent was obtained from the patient for their anonymized information to be published in this article.
ORCID iD: Kevin Groudan  https://orcid.org/0000-0002-9532-2533
https://orcid.org/0000-0002-9532-2533
References
- 1. Zylberberg HM, Green PH, Turner KO, et al. Prevalence and predictors of Giardia in the United States. Dig Dis Sci. 2017; 62:432-440. [DOI] [PubMed] [Google Scholar]
- 2. Einarsson E, Ma’ayeh S, Svärd SG. An up-date on Giardia and giardiasis. Curr Opin Microbiol. 2016;34:47-52. [DOI] [PubMed] [Google Scholar]
- 3. Bartelt LA, Sartor RB. Advances in understanding Giardia: determinants and mechanisms of chronic sequelae. F1000Prime Rep. 2015;7:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Júlio C, Vilares A, Oleastro M, et al. Prevalence and risk factors for Giardia duodenalis infection among children: a case study in Portugal. Parasit Vectors. 2012;5:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hooshyar H, Rostamkhani P, Arbabi M, et al. Giardia lamblia infection: review of current diagnostic strategies. Gastroenterol Hepatol Bed Bench. 2019;12:3-12. [PMC free article] [PubMed] [Google Scholar]
- 6. Shane A, Mody R, Crump J, et al. 2017 Infectious Diseases Society of America clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin Infect Dis. 2017;65:1963-1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dunn N, Juergens AL. Giardiasis. StatPearls; 2020. [PubMed] [Google Scholar]
- 8. Kamath KR, Murugasu R. A comparative study of four methods for detecting Giardia lamblia in children with diarrheal disease and malabsorption. Gastroenterology. 1974;66:16-21. [PubMed] [Google Scholar]
- 9. Garg N, Singh J, Anjum H, et al. Cytopreparation of duodenal biopsy fixative improves detection rate of Giardia in clinically suspected cases. Cytopathology. 2019;30:309-313. [DOI] [PubMed] [Google Scholar]
- 10. Gupta SK, Croffie JM, Pfefferkorn MD, Fitzgerald JF. Diagnostic yield of duodenal aspirate for G lamblia and comparison to duodenal mucosal biopsies. Dig Dis Sci. 2003;48:605-607. [DOI] [PubMed] [Google Scholar]
- 11. Watson D, Sutherland L, Befus A. Giardiasis in endoscopy patients: a comparison of diagnostic techniques. J Clin Gastroenterol. 1989;4:1-4. [Google Scholar]
- 12. Wahnschaffe U, Ignatius R, Loddenkemper C, et al. Diagnostic value of endoscopy for the diagnosis of giardiasis and other intestinal diseases in patients with persistent diarrhea from tropical or subtropical areas. Scand J Gastroenterol. 2007;42:391-396. [DOI] [PubMed] [Google Scholar]


