Abstract
Using a factor mixture model (FMM) approach, this study examined if SAD could be subtyped by distinct risk profiles, and whether these subtypes predicted different manifestations of the disorder. We derived risk profiles from neurotic temperament (NT), positive temperament (PT), and autonomic arousability (AA), which are hypothesized to be important in the maintenance of anxiety disorders such as SAD. In our sample of 758 SAD outpatients, a two-class FMM solution fit the data best. Class 1 was characterized by very low PT whereas PT in Class 2 was substantially higher. The two classes differed to a lesser extent on NT, but were virtually equivalent on AA. Class 1 had significantly more males, individuals with depressive disorders, generalized SAD, and higher SAD severity. Class 2 had more individuals with performance subtype SAD. These findings provide initial support for distinct risk profiles within SAD that may be predictive of its clinical expression.
Keywords: social anxiety disorder, risk profiles, factor mixture modeling
Social anxiety disorder (SAD) is characterized by fear or avoidance of at least one social situation where the individual may be scrutinized by others (American Psychiatric Association, 2013). These social situations almost always provoke fear or anxiety and are avoided or endured with intense fear. Individuals with SAD are afraid that they will display anxiety symptoms or act in a way that will be negatively evaluated. The 12-month prevalence of SAD in the United States is around 7% and the median age of onset is 13 years (Kessler et al., 2005, 2012; Ruscio et al., 2008).
Because of considerable heterogeneity in the expression of SAD (e.g., in the number and types of feared social situations), there have been several attempts to subtype this disorder. These efforts are most apparent in the specifiers that have accompanied various DSM definitions of SAD. For instance, in DSM-III-R (American Psychiatric Association, 1987), a “generalized” specifier was introduced, defined as having fears in most social situations (cf. American Psychiatric Association, 2000). Thereafter, researchers augmented the generalized specifier introduced in DSM-III-R with additional SAD subtypes such as “non-generalized,” and “discrete.” Perhaps due to its higher clinical severity and complications (e.g., comorbidity), the generalized subtype is most common in clinical settings (e.g., Turner, Beidel, Dancu, & Keys, 1986), whereas public speaking fears (e.g., “discrete” SAD) are more prevalent in the general population (Pollard & Henderson, 1988). However, due to the lack of specificity in DSM regarding the types or number of situations necessary for the generalized specifier, researchers adopted their own operational definitions (Heimberg, Holt, Schneier, Spitzer, & Liebowitz, 1993; Stemberger, Turner, Beidel, & Calhoun, 1995). In DSM-5 (APA, 2013) the “generalized” specifier was removed and replaced with a “performance only” specifier which emphasized the type of feared situations rather than the number of situations. Based on a meta-analytic review of 18 studies, it was concluded that a performance only subtype does exist (Blöte, Kint, Miers, & Westenberg, 2009). Three of these studies were clinical studies, while the rest utilized community samples. Another study of treatment-seeking youth (Kerns, Comer, Pincus, & Hofmann, 2013) found that 35.2% of outpatients met criteria for non-generalized SAD, but none of them would have been assigned the performance only specifier. These results may further attest to the types of SAD presentations that are more and less common in treatment-seeking samples (i.e., predominance of “generalized” SAD, performance only subtype less frequent).
Many years before the DSM-5, it was proposed that performance only SAD could be distinguished from a second subtype, “social interaction anxiety” (Mattick & Clarke, 1998). Situations such as dating, communicating with others, and being assertive require interacting with others. On the other hand, performance situations such as giving a speech or playing a musical instrument in public do not involve one-on-one social interaction and generally only involve being observed. Most individuals are rarely required to engage in performance situations. However, interacting with others occurs in nearly every public situation. Given the importance and regularity of social interactions in daily life, social interaction anxiety is more likely to be generalized (present in many different situations) and cause more significant interference in multiple life domains such as social and occupational functioning. It is likely that this difficulty would be more closely linked to and have higher comorbidity with depression due to shared cognitive risk factors such as low self-confidence and poor self-esteem.
Rather than focusing solely on variations in the manifestation of a given disorder (e.g., the number or type of symptoms), it may be useful to determine whether heterogeneity in symptom expression emanates from different patterns of risk1. In addition to its conceptual implications (e.g., individuals with a given disorder do not necessarily share identical risk factors), the explication of robust, distinct risk profiles may have considerable clinical value in predicting the ultimate expression of a disorder and its complications, course, and treatment response. A few dimensional risk factors have been linked to the severity, etiology, and maintenance of SAD as well as other anxiety and mood disorders (e.g., Brown, 2007). Two of the most prominent diatheses are neuroticism (NT) and extraversion or positive temperament (PT) (Fanous, Gardner, Prescott, Cancro, & Kendler, 2002; Hettema, Prescott, & Kendler, 2004; Viken, Rose, Kaprio, & Koskenvuo, 1994). These dimensions are considered components of a general biological vulnerability for emotional disorders, which includes stable and genetically based dispositions to experience negative emotions (Barlow, 2000; Suárez, Bennett, Goldstein, & Barlow, 2009). NT is associated with mood and anxiety disorders to varying degrees, with generalized anxiety disorder (GAD) and depression having the strongest association, and specific phobia the weakest (Brown, 2007; Brown, Chorpita, & Barlow, 1998; Mineka, Watson, & Clark, 1998; Watson, Gamez, & Simms, 2005). Whereas NT is present in all emotional disorders, low PT is uniquely associated with unipolar depression and SAD (Brown & Barlow, 2009; Clark, Watson, & Mineka, 1994; Mineka et al., 1998).
In the context of putative risk dimensions, it is also important to consider SAD’s placement in the structure of psychopathology. Psychological disorders are primarily grouped into two large categories: internalizing disorders, including anxiety and mood disorders (characterized in part by high NT), and externalizing disorders, which entail disorders involving maladaptive, externally focused behaviors such as conduct and substance use disorders (Caspi et al., 2014). Based on factor analytic evidence, researchers have proposed separating internalizing disorders into bipolar, distress, and fear disorders (e.g., L. A. Clark & Watson, 2006; Watson, 2005). Distress disorders include major depression, persistent depressive disorder, GAD, and posttraumatic stress disorder (PTSD). The fear disorders include panic disorder, agoraphobia, SAD, and specific phobia (Watson, 2005). A key unifying feature of this latter category is autonomic arousal (AA), which along with negative affect (NT) and positive affect (PT), is one of the core dimensions of the tripartite risk model of anxiety and depression (Clark et al., 1994). AA is characterized by symptoms such as shortness of breath, trembling/shaking, and rapid heart rate (Brown & McNiff, 2009). These symptoms are clearly related to those experienced during a panic attack (APA, 2013). According to DSM-5 (American Psychiatric Association, 2013), panic attacks can be associated with any disorder, but are more often experienced in panic disorder, PTSD, SAD, and specific phobias (Brown, Campbell, Lehman, Grisham, & Mancill, 2001).
However, research using clinical samples has not found a strong relationship between SAD and AA. Previous studies in clinical samples have found that PTSD and panic disorder/agoraphobia were the only DSM-IV anxiety disorder constructs to have significant direct effects on AA, whereas GAD, SAD, and obsessive-compulsive disorder did not (Brown et al., 1998; Brown & McNiff, 2009). On the whole, in clinical samples SAD has either been uncorrelated or inversely associated with AA and with disorders that are characterized by high AA such as PTSD and panic disorder (Brown, Campbell, et al., 2001; Conway & Brown, 2018). As discussed below, the discrepant findings regarding AA in SAD may stem from the analysis of samples in which relatively distinct SAD subgroups are unwittingly combined in the same sample.
One potential subgroup, which corresponds closely but not exactly with the performance subtype in DSM-5, could be comprised primarily by individuals whose SAD is defined by fears of a limited set of social situations (e.g., public speaking, assertiveness). Because these circumscribed fears stem from a situationally specific fear of negative evaluation, these individuals would be less likely to have a generalized negative concept of themselves. Thus, these individuals would evidence lower NT and higher PT, perhaps to a degree that approximates the higher range of functioning seen in individuals without emotional disorders (or patients with specific phobias of circumscribed situations or objects; cf. Brown, Chorpita, Korotitsch, & Barlow, 1997). However, persons in this subgroup may have elevated AA, particularly in the presence of their feared situation.
A second potential subgroup is likely to have an SAD that emanates from and is maintained by the same risk factors found in the mood disorders: i.e., high NT and low PT (cf. Brown, 2007; Naragon-Gainey, Gallagher, & Brown, 2013). Unlike the first subgroup, these individuals experience more ubiquitous social anxiety, including with various forms of one-on-one social interaction (e.g., initiating conversations, talking with authority figures), which may be due to a general sense of low self-confidence and self-worth. However, as is also the case with the mood disorders, high AA is not associated with these SAD presentations (cf. Brown et al., 1998; Brown & McNiff, 2009). Indeed, the inconsistent relationships between SAD and AA that have been reported in the literature may be due to the admixture of these subgroups (e.g., the relationship between SAD and AA is attenuated in outpatient samples where generalized SAD is predominant; however, this relationship is stronger in community-based samples where discrete or performance SAD is more common).
There is significant evidence supporting this hypothesized second subgroup. Compared to other anxiety disorders, previous research found that depression (DSM-IV major depressive disorder and dysthymia) and SAD had the highest comorbidity with each other (Brown, Campbell et al., 2001). Researchers have suggested that high negative affect and low positive affect are crucial components of SAD and depressive disorders (Gross & Jazaieri, 2014; Hofmann, Sawyer, Fang, & Asnaani, 2012). Socially anxious individual reported higher levels of trait negative affect (i.e., NT; Watson, Clark, & Carey, 1988) and higher intensity of negative affect on a given day (Farmer & Kashdan, 2014) compared to those with low social anxiety. The latter is especially true in situations involving potential social threat (e.g., Kashdan & Farmer, 2014). Compared to controls, depressed individuals reported higher trait-level (Clark et al., 1994; Watson et al., 1988) and daily (Bylsma, Taylor-Clift, & Rottenberg, 2011; Mor et al., 2010) negative affect. As aforementioned, SAD is characterized with low positive affect, unlike other anxiety disorders (Brown et al., 1998). Socially anxious individuals demonstrated lower trait-level and daily positive affect than those with low social anxiety (Kashdan & Steger, 2006). A large-scale meta-analysis also demonstrated that social anxiety is related to low positive affect, even after controlling for depression (Kashdan, 2007). Another meta-analysis concluded that depressed individuals demonstrate less emotional reactivity to positive stimuli than controls (Bylsma, Morris, & Rottenberg, 2008) and have difficulty sustaining positive affect across time (e.g., Heller et al., 2009). Thus, it is clear that depression and SAD share strong connections with trait positive and negative affect (i.e., PT and NT), which we hypothesize will result in a subgroup of SAD with similar risk factors as depression.
With these issues in mind, this paper used factor mixture modeling (FMM) to evaluate whether distinct risk profiles exist in SAD among treatment seeking-outpatients. Based on previous research on SAD subtypes and the aforementioned conceptual reasoning, we hypothesized that FMM would explicate two classes reflecting two separate risk profiles. The first class would evidence a profile characterized by high NT, low PT, and low AA. Members of this class would be more likely to experience generalized social anxiety due to low self-confidence and poor self-esteem, and would share a similar risk profile to depressed individuals due to the shared importance of NT and PT to both SAD and depression. The second class would be characterized by low NT, high PT, and high AA, which is more descriptive of an anxiety or fear subtype. Instead of an SAD that is driven by a generalized neurotic and introverted temperament, the members of this class are more apt to experience situational fearfulness and arousal, especially in circumscribed situations such as performing or speaking in front of others.
Method
Participants
The sample consisted of 758 individuals who were seeking treatment at an outpatient treatment clinic for anxiety and related disorders. Participants were predominantly Caucasian (86.3%; African-American = 4.9%, Asian = 8.0%, Other = 0.7%) and 54.6% were female. The mean age for the sample was 31.15 (SD = 11.68, range = 18 to 87). All participants were diagnosed with social anxiety disorder (SAD) using the Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L; Di Nardo, Brown, & Barlow, 1994). The ADIS-IV-L is a semi-structured interview used for diagnosing and obtaining severity ratings for anxiety, mood, somatoform, and substance use disorders. Screens for other disorders such as psychotic disorders are also included. The interview has demonstrated good to excellent reliability for diagnosing anxiety and mood disorders (Brown, Di Nardo, Lehman, & Campbell, 2001). In this sample, the most common current disorders other than SAD were: mood disorders (major depressive disorder, dysthymia, depressive disorder not otherwise specified; 38.5%), generalized anxiety disorder (32.5%), panic disorder (13.6%), obsessive-compulsive disorder (12.5%), and specific phobia (10.9%).
Measures and Indicators Used in Factor Mixture Model (FMM)
The study used five questionnaires to assess three dimensions of risk: NT, PT, and AA. As discussed earlier, NT and PT are dimensions of temperament that have been shown to be very important in the etiology and maintenance of emotional disorders. The NEO-Five Factor Inventory (NEO-FFI; Costa & McCrae, 1992), Eysenck Personality Questionnaire (EPQ; Eysenck & Eysenck, 1975), and Behavioral Inhibition/Activation Scales (BIS/BAS; Carver & White, 1994) were used to assess NT and PT. The neuroticism scores from the NEO-FFI and EPQ, as well as the BIS score were used as indicators of NT. The extraversion scores from the NEO-FFI and EPQ and the BAS score were the indicators of PT. The Beck Anxiety Inventory (BAI; Beck & Steer, 1990) and Anxiety subscale from the Depression Anxiety Stress Scales (DASS; Lovibond & Lovibond, 1996) were used as indicators of autonomic arousal (cf. Brown & McNiff, 2009). Of note, the BAI and DASS Anxiety scales were rescored to only include items inquiring about physiological symptoms of AA (e.g., removing cognitive fear items such as “fear of dying” from the BAI; cf. Brown & McNiff, 2009). Additionally, the short form version of the EPQ was utilized (Eysenck & Eysenck, 1975). Each of these questionnaires is well-established and has been shown to have excellent psychometric properties in previous research.
Validation Measures
Both clinician ratings and self-report measures were used to validate the classes that were explicated by FMM. With regard to clinical ratings, ADIS-IV-L diagnoses and clinician-rated fear of various social situations were used to validate the classes. During the ADIS-IV-L, clinicians assessed the presence and severity of key and associated symptoms of each disorder on a dimensional scale (0-8 ratings). These dimensional ratings were assigned regardless of whether a formal clinical diagnosis was being considered. In the Social Anxiety Disorder section of the ADIS-IV-L, interviewers made dimensional ratings of patients’ fear of 13 social situations, ranging from 0 (no fear) to 8 (very severe fear). A sum of these 13 ratings was used as an indicator of SAD severity. In addition, the resulting classes were compared on the presence of performance and generalized SAD subtypes. Generalized subtype was defined by whether or not the ADIS-IV-L interviewer assigned this DSM-IV specifier when making the SAD diagnosis. Because the performance only subtype did not exist before DSM-5, it was constructed in this data set by separating the 13 ADIS-IV-L social situations into performance (i.e., participating at meetings/classes, talking in front of a group/formal speaking, eating in public, using public restrooms, and writing in public) and interaction situations. Participants who only endorsed performance situations at a clinically significant level (i.e., situational fear ratings of 4 or higher) were deemed to have the performance SAD subtype.
The Social Interaction Anxiety Scale (SIAS; Mattick & Clarke, 1998) and Albany Panic and Phobia Questionnaire (APPQ; Rapee, Craske, & Barlow, 1994) were used as self-report validation measures. The APPQ measures fear of activities that may elicit strong internal bodily sensations (interoceptive fear), locations that may elicit panic-like symptoms (agoraphobia), and social situations. If classes differed significantly on levels of AA, it was posited that they might also differ on APPQ scores because individuals with higher AA would likely endorse stronger interoceptive and agoraphobic fear.
Data Analysis
This study followed the FMM methodology described in Clark et al. (2013). Clark et al. recommended starting with factor analysis and latent class analysis models to help determine the number of classes and the factors to use when specifying the FMMs. Factor analysis, latent class analysis, and FMM analysis were conducted in Mplus 7.1 (L. K. Muthén & Muthén, 1998-2013). The models were estimated using robust maximum likelihood (MLR), which also accommodated missing data (covariance coverage for the indicators ranged from 94.1 to 99.9%). The fit of the factor analytic models was evaluated using the root mean square error of approximation (RMSEA) and its 90% confidence interval, the Tucker-Lewis index (TLI), the comparative fit index (CFI), and the standardized root mean square residual (SRMR). In accordance with the recommendations of Hu and Bentler (1999), the following guidelines were used to define acceptable model fit: RMSEA values close to or below 0.06, CFI and TLI values close to or above .95, and SRMR values close to or below .08. Additionally, standardized residuals and modification indices were used to identify any localized areas of strain in the solutions.
For the latent class analyses and FMMs, the following statistics were considered in class enumeration and comparative model fit evaluation: log-likelihood, Akaike information criterion (AIC), Bayes information criterion (BIC), entropy, and the Lo-Mendell Rubin adjusted likelihood ratio test (LMR) were considered in choosing best-fitting solutions. Smaller log-likelihood, AIC, and BIC values, higher entropy, and significant LMR are indicative of better-fitting models (Lo, Mendell, & Rubin, 2001; Raftery, 1995). Prior research has shown that the BIC is a particularly robust indicator of model fit (Nylund, Asparouhov, & Muthén, 2007), so it was prioritized in class enumeration. In addition to model fit comparisons, solutions were evaluated by the size and interpretability of the resulting classes.
After the number of the factors and classes were ascertained, we analyzed four FMMs that varied in their degree of measurement invariance. FMM type 1 (FMM-1) estimated all factor means in each class, held intercepts and loadings to equality, and set the factor covariances to zero. FMM-2 allowed both factor means and factor covariance matrix to vary between classes, while still holding factor loadings and intercepts to equality. FMM-3 allowed the factor covariance matrix and intercepts to vary, held the factor loadings to equality, and fixed factor means to zero. Finally, in FMM-4, the factor means were fixed to zero and all other elements (intercepts, loadings, and factor covariances) were allowed to vary across classes. The best solution was selected using fit indices.
Results
Factor Analysis and Latent Class Analysis
Given the strong conceptual and empirical basis for a tripartite model of risk (i.e., NT, PT, and AA, cf. Brown et al., 1998; Clark et al., 1994), a three-factor confirmatory factor analysis was performed. This model fit the data well, χ2 (17) = 70.13, p < .001, SRMR = .04, RMSEA = 0.06 (90% CI = 0.05 to 0.08), TLI = 0.96, CFI = .97. The standardized residuals and modification indices did not indicate any substantively salient areas of localized strain. Thus, only three-factor solutions were considered in the FMMs. The factor loadings for each indicator were large and statistically significant (range of loadings = .54 to .96, ps < .001). The PT factor was significantly correlated with NT (r = −.38, p < .001) and AA was significantly correlated with NT (r = .35, p < .001). However, the PT and AA factors were not significantly correlated (r = .01, p = .812).
Latent class analyses were performed to determine the maximum number of classes to test in the FMMs. Because of differing metrics, the observed scores for the eight indicators were converted to T-scores to foster interpretability. The indicators were then submitted to latent class analyses entailing one to eight classes (because there were eight indicators). BIC and AIC values did not plateau and continued to decrease as the number of classes increased (see Table S1 in Supplemental Material available online). However, entropy was highest, indicating good class discrimination, for the two and four class solutions. Only the solutions with two through five classes had significant or near significant LMR values, which suggested that the appropriate number of classes was within this range.
The factor scores for the latent variables from the three-factor confirmatory factor analysis were estimated and exported for further latent class analysis. These additional analyses were conducted to foster the interpretability of the FMMs, given that the FMMs would be based on the three factors. Guided by the results of the 8-indicator latent class analyses, latent class models using two through five classes were tested (see Table S1 in Supplemental Material available online). Fit statistics indicated that AIC and BIC values continued to decrease while the number of classes increased. However, the difference in BIC from Class 3 to Class 4 was very small, indicating no appreciable improvement in model fit with the added class. Entropy was highest for the two class solution, indicating the best class differentiation. Only the two and five class solutions had significant LMR p-values, while the three class solution approached significance.
To evaluate the interpretability of the classes, the mean factor estimates from the three-factor latent class analyses described above were graphed (see Figure S1 in Supplemental Material available online). The two and three class solutions were the most distinct and interpretable, as the classes in the four and five class solutions were differences of degree rather than kind. For example, in the four class model, Class 1 and 2 had the same risk profile, with Class 2 having slightly higher NT, PT, and AA. This was also the case for Classes 2 and 3 and Classes 4 and 5 in the five class solution. This suggests that these classes were not categorically distinct, but differed only on the degree of risk severity. Moreover, the sizes of some classes were small in the four and five class solutions, (as low as 31). These are likely to be subsets of the larger groups found in the two and three class solutions, and not distinct groups. Given that the two class and three class solutions were the most interpretable and had significant or near significant LMR p-values, FMMs were conducted using three factors and two and three classes.
Factor Mixture Models
Each of the four types of FMMs outlined in Clark et al. (2013) was conducted for two- and three-class solutions, with three factors (see Table 1). Table 1 also provides the fit indices for the best models from the factor analysis and latent class analysis along with the factor mixture solutions. Both the two-and three-class models for FMM-4 and the three-class model for FMM-3 produced negative variances for one or more latent variables, so these solutions were not considered further. Based on the BIC and LMR, FMM-2 for two classes was deemed the best-fitting solution. Although the two class solutions for FMM-1, FMM-2, and FMM-3, as well as the FMM-1 three class solution, had significant LMR values, the FMM-2 two class solution had the lowest BIC. The two class FMM-2 and FMM-3 models fit the data roughly the same, but FMM-2 was more parsimonious. When compared to the best models from the factor and latent class analysis, the FMM-2 two class solution had the lowest AIC and BIC. Because the measurement parameters (factor loadings and indicator intercepts) were equivalent between classes in the FMM-2 model, the factor scores for the classes could be compared.
Table 1.
Factor Mixture Model Comparisons
| Model | Log- Likelihood |
Parameters | AIC | BIC | Adj. BIC | Entropy | LMR p value |
|---|---|---|---|---|---|---|---|
| Factor Analysis | |||||||
| 3 factor | −16663.623 | 27 | 33381.247 | 33506.275 | 33420.539 | ||
| Latent Class Analysis | |||||||
| 2 class | −21854.825 | 25 | 43759.651 | 43875.418 | 43796.033 | .863 | .0000 |
| 3 class | −21624.082 | 34 | 43316.164 | 43473.608 | 43365.643 | .839 | .0009 |
| Factor Mixture Analysis | |||||||
| 2 class, 3 factor | |||||||
| FMM-1 | −17287.839 | 25 | 34625.678 | 34741.445 | 34662.059 | .863 | .0000 |
| FMM-2 | −16552.561 | 37 | 33179.122 | 33350.457 | 33232.967 | .740 | .0001 |
| FMM-3 | −16540.629 | 42 | 33165.257 | 33359.746 | 33226.378 | .858 | .0008 |
| FMM-4 | * | ||||||
| 3 class, 3 factor | |||||||
| FMM-1 | −17077.600 | 29 | 34213.201 | 34347.490 | 34255.403 | .831 | .0022 |
| FMM-2 | −16540.629 | 47 | 33142.238 | 33359.880 | 33210.635 | .598 | .1559 |
| FMM-3 | * | ||||||
| FMM-4 | * | ||||||
Note.
resulted in negative latent variable variances. The bolded solution was determined to be the best fitting and most interpretable. AIC = Akaike information criterion; BIC = Bayesian information criterion; Adj. BIC = Adjusted Bayesian information criterion; LMR = Lo-Mendell-Rubin adjusted likelihood ratio test p value.
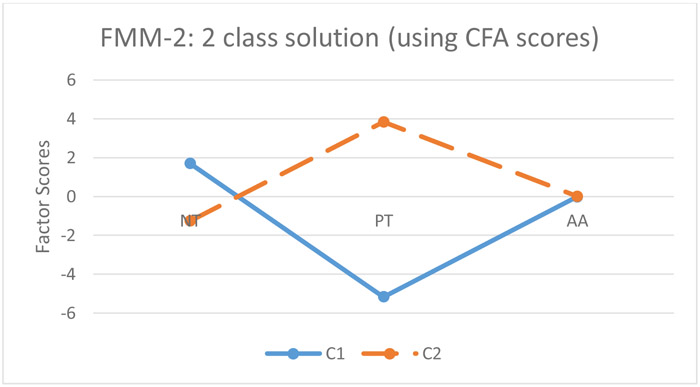
The exported CFA factor scores were used to graph the relative standing on the three latent dimensions for the two classes from the FMM-2 solution (Figure 1). There were 323 individuals in the first class and 435 in the second class. The average probabilities of class membership were .842 for Class 1 and .990 for Class 2, indicating good discrimination. As can be seen in Figure 1, although the classes differed to some degree on NT (but were virtually the same on AA), they were distinguished primarily by higher versus lower levels of PT. To foster the interpretation of the classes, the observed means of NT, PT, and AA were examined using the marker indicator of each factor (NEO-FFI neuroticism, NEO-FFI extraversion, and DASS Anxiety subscale). The combined gender, community sample norms from the NEO manual (Costa & McCrae, 1992) were used to interpret the class means on neuroticism and extraversion in relation to a normative sample. Although Class 1’s NEO-FFI neuroticism score was slightly, albeit significantly higher, than Class 2 (Ms = 35.67 and 32.56, respectively; p < .001), both classes would be characterized as having very high neuroticism based on a cutscore of 30 or above in the normative sample. On NEO-FFI extraversion, scores below 19 signify very low extraversion and scores from 25 to 30 are considered average extraversion scores. The classes had significantly different levels of extraversion (p < .001), with Class 1 having very low extraversion (15.77) and Class 2 having nearly average extraversion (24.87). Based on normative data from a large non-clinical sample in the United Kingdom (Henry & Crawford, 2005), the DASS Anxiety means (using the full scale) were around the 79th percentile for both classes, and there were no differences in AA between the two groups (Ms = 6.74 and 6.40, p = .31)2.
Figure 1. Factor Score Means for Two Class, FMM-2.
Note. NT = neurotic temperament, PT = positive temperament; AA = autonomic arousal; C1 = Class 1; C2 = Class 2.
To interpret the classes in relation to other relevant disorders, the observed means (see Table S2 in Supplemental Material available online) were also compared to scores of patients in this study who had a principal depressive disorder, principal SAD, or principal panic disorder. Class 1 had a mean NEO-FFI neuroticism score of 35.67 (SD = 6.53), NEO-FFI extraversion score of 15.77 (5.79), and a DASS Anxiety score of 6.74 (4.47). Class 2 had a mean NEO-FFI neuroticism score of 32.56 (8.30), NEO-FFI extraversion score of 24.87 (6.60), and a DASS Anxiety score of 6.40 (4.35). Patients with a principal depressive disorder diagnosis (n = 117) had a mean NEO-FFI neuroticism score of 35.20 (6.60), NEO-FFI extraversion score of 21.50 (7.79), and a DASS Anxiety score of 6.50 (4.32). Those with principal SAD (n = 385) had a mean NEO-FFI neuroticism score of 32.88 (8.23), NEO-FFI extraversion score of 20.53 (7.78), and a DASS-Anxiety score of 5.92 (4.11). The average scores for patients with panic disorder (n = 260) were 27.93 (8.82), 27.07 (7.62), and 9.28 (4.87) for NEO-FFI neuroticism, extraversion, and DASS-Anxiety, respectively. Thus, Class 1 had similar levels of NT (p = .51) and AA (p = .62) as those who had a principal depressive disorder, but even lower PT scores (p < .001, d = 0.84). Class 2 had similar levels of NT (p = .58) and AA (p = .11) compared to individuals with principal SAD, but significantly higher PT scores (p < .001, d = 0.60). Both classes had a level of AA considerably lower than that seen in panic disorder (Class 1 p < .001, d = 0.54); Class 2 p < .001, d = 0.62).
Class Validation
The interpretability and validity of the two latent classes were further evaluated by regressing class membership onto clinically relevant covariates using the three-step approach available in Mplus. This method estimates the mixture model, creates a variable representing most likely class membership, and then estimates the regression parameters for the covariates adjusting for classification uncertainty (Vermunt, 2010). The Mplus commands R3Step and BCH were used for categorical and continuous covariates, respectively.
The regression models were conducted to test for class differences in sex, age, presence of any depressive disorder, panic disorder, whether SAD was the principal diagnosis, SAD severity (sum of the 13 social situation fear ratings from the ADIS-IV-L), SIAS score, and the three subscale scores of the APPQ. There were no significant differences in age between classes (p = .49). Compared to Class 2, Class 1 had significantly more males (p = .003; 51.7% vs. 40.7%), more individuals with depressive disorders (p < .001; 47.7% vs. 31.7%) and with SAD as their principal diagnosis (p < .001; 66.6% vs. 49.9%) (see Table 2), and higher clinician-rated SAD severity (p < .001) (see Table 3). As seen in Table 3, Class 1 also endorsed higher self-reported scores of social interaction anxiety as measured by the SIAS (p < .001) and stronger fear of social (p < .001) and agoraphobic (p = .04) situations as measured by the APPQ. Thus, the classes differed significantly on all outcomes except for APPQ Interoceptive fear and the presence of a panic disorder diagnosis.
Table 2.
Logistic Regressions of Class Membership onto Covariates
| Variable | Estimate | SE | Est/SE | p value | Odds Ratio |
|
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Sex | 0.535 | 0.178 | 2.997 | .003 | 1.707 | |
| Comorbidities | ||||||
| Any Depressive Disorder Diagnosis | 0.804 | 0.181 | 4.438 | <.001 | 2.234 | |
| Panic Disorder diagnosis | −0.106 | 0.262 | −0.403 | .687 | 0.899 | |
| SAD principal diagnosis | 0.848 | 0.191 | 4.434 | <.001 | 2.335 | |
| Generalized Subtype | 1.536 | 0.235 | 6.530 | <.001 | 4.646 |
Table 3.
Mean Comparisons of Covariates between Classes
| Variable | Class 1 Mean |
Class 1 SE |
Class 2 Mean |
Class 2 SE |
χ2 | p value | |
|---|---|---|---|---|---|---|---|
| Demographics | |||||||
| Age | 31.602 | 0.792 | 30.892 | 0.560 | 0.471 | 0.49 | |
| SAD Descriptors | |||||||
| SAD Severity |
48.154 | 0.957 | 34.793 | 0.677 | 114.372 | <.001 | |
| Self-Reports | |||||||
| SIAS | 62.298 | 0.828 | 41.557 | 0.764 | 288.676 | <.001 | |
| APPQS | 42.138 | 0.985 | 28.023 | 0.654 | 126.558 | <.001 | |
| APPQA | 16.156 | 0.858 | 13.861 | 0.581 | 4.33 | .04 | |
| APPQI | 8.778 | 0.626 | 7.985 | 0.437 | 0.949 | .33 |
Note. SAD = social anxiety disorder; SIAS = Social Interaction Anxiety Scale; APPQS = Albany Panic and Phobia Questionnaire Social Fear Scale; APPQA = Albany Panic and Phobia Questionnaire Agoraphobia Scale; APPQI = Albany Panic and Phobia Questionnaire Interoceptive Scale.
In the full sample, 27 patients feared performance situations only, whereas 471 patients were classified as having generalized SAD. Out of 27 performance-only SAD individuals, only two of them were in Class 1, and the other 25 were in Class 2. Due to the small number of performance subtype individuals (27 in total, two in class 1 and 25 in class 2), the three-step approach in Mplus was not able to calculate an accurate estimate. Fisher’s Exact Test (p < .001) was used instead. There were significantly more patients with generalized SAD in Class 1 (see Table 2). Of the 471 patients with generalized SAD, 250 (77.40%) were in Class 1 whereas 221 (51.16%) were in Class 2.
Analyses Excluding Depressed Patients
As in most treatment-seeking clinical samples, depression was prevalent in our overall sample (38.5%). Thus, it is possible that mood disorder comorbidity contributed to the resulting extracted classes. This issue is particularly relevant given that the risk profile observed in Class 1 is the same as what would be expected for individuals with mood disorders (i.e., high NT, low PT). To address this issue, the analyses were re-conducted excluding participants with any current depressive disorder diagnosis (total N was reduced to 466). As before, a three-factor confirmatory factor analysis was performed, and the model fit the data well, χ2 (17) = 48.29, p < .001, SRMR = .03, RMSEA = 0.06 (90% CI = 0.04 to 0.08), TLI = 0.96, CFI = .97.
To foster the interpretability of the classes, the factor scores for the latent variables from the three-factor confirmatory factor analysis were estimated and exported for latent class analysis. In accordance with previous findings, latent class models using two through five classes were tested. Fit statistics indicated that AIC and BIC values continued to decrease while the number of classes increased3. As before, entropy was highest for the two-class solution, indicating the best class differentiation. Only the two and three class solutions had significant LMR p values, while the five-class solution approached significance. Additionally, both the four and five class solution had classes that contained less than 30 individuals. Thus, FMMs were conducted using three factors and two and three classes.
Both the two-and three-class models for FMM-4 produced negative variances for a latent variable, so these solutions were not considered further. Based on the BIC and LMR, FMM-3 for two classes was deemed the best-fitting solution. Although the three-class solution for FMM-3 had a lower BIC value, the LMR p value was non-significant. FMM-1 for the two-class solution had a significant LMR value, but a higher BIC value. The two class, FMM-3 solution also had the highest entropy (.865) across all the FMMs. The measurement parameters (factor loadings and indicator intercepts) were equivalent between classes in the FMM-3 model, allowing for the between-class comparison of factor scores.
The exported CFA factor scores were compared using t-tests. The means were as follows for Class 1 and Class 2, respectively: −7.58 and 1.79 for NT, 2.29 and −.54 for PT, and −.44 and .10 for AA. The two groups differed significantly on NT (p < .001), PT (p < .001), and AA (p = .023). There were 89 individuals in the first class and 377 in the second class. Attesting to favorable discrimination, the average probabilities of class membership were .880 for Class 1 and .980 for Class 2, and the classification probabilities of the most likely class memberships for the two classes were .914 and .972, respectively.
Overall, these re-analyses produced results that were similar to the full sample analyses, with the best solution being comprised of two classes that were differentiated primarily by NT and PT. However, the two classes now differed most markedly on NT. The classes continued to differ minimally on AA. Although the two classes continued to significantly differ on PT this difference was less pronounced than in the full sample analysis, likely due to the removal of patients with depression from the sample, which would eliminate many patients with low PT.
Discussion
The aims of this study were to determine if there are distinct patterns of risk within SAD and whether these risk profiles predict variations in the expression of this disorder. FMM of three latent dimensions of risk (NT, PT, AA) explicated two risk profile classes. The two classes differed on NT and PT in the expected manner, but did not differ on AA. The smaller class (Class 1) was in accord with our prediction that there is a subgroup of persons with SAD who share the risk dimensions found in the mood disorders. Indeed, as in the mood disorders, this class was characterized by high NT and low PT (cf. Brown, 2007; Naragon-Gainey et al., 2013) and had observed scores more similar to patients with a principal depressive disorder diagnosis than patients with a principal SAD. Because of these shared risk factors and the dysfunctional cognitions that accompany high NT and low PT (e.g., low self-confidence; cf. Brown & Naragon-Gainey, 2013), it was posited that the SAD of individuals in this class would tend to be more generalized and severe, and more often accompanied by comorbid depression. Consistent with these predictions, the rates of generalized SAD and co-occurring mood disorders, and the overall severity of SAD were found to be significantly higher in Class 1 than in Class 2.
The second class identified by FMM was comprised of persons with SAD who evidenced significantly higher PT. Based on community sample norms (Costa & McCrae, 1992), NT was still very high in this class. On the other hand, this class did not evidence a clinically significant deficit in PT (i.e., average NEO-FFI extraversion scores approximated the normal range relative to the community sample). We hypothesized that depressogenic factors would be less germane and predominant in this class, and that persons with this risk profile would be more likely to have a SAD that is defined by apprehension and avoidance of more circumscribed or performance type situations (e.g., public speaking, assertiveness) rather than a more generalized disorder that also encompasses fears of social interaction. However, about half of this class still had generalized SAD, indicating that generalized SAD is not uniformly associated with low PT. This finding may also be due to the fact that generalized SAD is much more common in treatment-seeking populations. Along these lines, although this subtype was relatively uncommon in this treatment-seeking outpatient sample, virtually all of the cases with performance type SAD resided in Class 2 (25 of 27, 92.6%). This result may lend some support for the inclusion of the performance type specifier in DSM-5 by suggesting that in addition to having fewer complications (e.g., less mood disorder comorbidity), persons with performance type SAD have a distinct risk profile. In fact, provided that the SAD does not occur in the context of comorbid disorders, individuals with this risk profile may be more apt to function at a level that approximates the normal range (e.g., although avoidant of musical performance because of the feared consequences of an unexpected panic attack, a person with SAD may be otherwise extraverted and function well in all other life areas). This might be particularly true for the performance type of SAD given the focal nature of the social fears. Nevertheless, it is important to note that the two classes explicated by FMM did not correspond to subgroups that could be distinguished simply by the type or number of social fears. The fact that the majority of patients in Class 2 did not have performance type SAD, and that many patients (over 20%) in Class 1 did not have generalized SAD, suggests that the two risk profiles are not inherently associated with a given form of SAD presentation.
The classes did not differ on AA or on panic disorder comorbidity, which is at odds with our prediction that there is a subgroup of persons whose SAD is characterized in part by higher levels of autonomic arousal. In fact, both classes also had mild to moderate AA scores (see Table S2 in Supplemental Material available online) that were well below the level of AA seen in panic disorder. In tandem with prior evidence (e.g., Brown & McNiff 2009), these findings bolster questions about the relevance of AA to SAD as a whole (i.e., AA may not be germane to even some SAD presentations). These results, along with findings indicating that, at the diagnostic level, SAD is not positively correlated with panic disorder/agoraphobia and specific phobia in clinical samples (Brown, Campbell, et al., 2001; Conway & Brown, 2018) challenge the notion that SAD should be subclassified as a fear disorder in internalizing-externalizing structural models of psychopathology (e.g., Watson, 2005). Rather, the current findings suggest that SAD may not fall neatly into either the fear or distress disorder subcategories. The fact that the majority of outpatients with SAD have a risk profile based on the same vulnerability dimensions found in mood disorders (Class 1), coupled with prior evidence attesting to the differential aggregation of SAD-mood disorder comorbidity (e.g., Brown, Campbell, et al., 2001), would lend support for the classification of SAD as a distress disorder. However, this classification would not seem to apply to a second distinct subgroup of outpatients (Class 2) whose SAD is less related to these risk factors (i.e., PT in normal range), but is unrelated to AA as well (perhaps also negating a fear disorder categorization).
It is possible that the lack of elevations and class differences on AA was because our indicators of this construct (BAI, DASS Anxiety) operate more as measures of generalized arousability than as measures of situation-specific anxiety. Previous research indicates that SAD is not characterized by chronic hyperarousal, as is found in panic disorder and PTSD (e.g., Brown & McNiff, 2009). This is likely due to the fact that, unlike PTSD and panic disorder where anxious arousal is triggered by internal cues (e.g., bodily sensations, intrusive recollections), fear reactions in SAD are elicited by external cues that can be more readily escaped or avoided. Under this conceptualization, one might argue that AA should be higher in persons with SAD who have generalized or social interaction fears because their feared situations are more pervasive and less easy to avoid. However, this assertion would be countered by the finding that AA was not elevated in Class 1 participants. The fact that the two classes had virtually the same levels of AA supports the notion that the classes emerging from the FMM analyses did not differ simply on the basis of general symptom severity.
Given the possibility that the presence of current mood disorders affected the resulting classes in the full sample analyses, the factor analytic, factor score latent class, and mixture models were re-conducted excluding patients with comorbid depression. A similar three-factor, two-class solution was obtained although the classes were more strongly differentiated by NT than by PT in the reduced sample analysis. These results bolster the notion that the full sample analyses were not unduly impacted by mood disorder comorbidity, although the removal of patients with depression somewhat mitigated the distinguishability of the two classes on PT. This is likely due in part to the fact that SAD often shares the same risk factors with mood disorders (i.e., high NT, low PT; e.g., Brown et al., 1998). To an immeasurable degree, the exclusion of cases with depression likely eliminated patients whose SAD-mood disorder comorbidity emanated from the same risk factors, thereby reducing the separation of Class 1 and Class 2 on PT, which is a risk factor unique to SAD and mood disorders. In addition to the results of these re-analyses, other findings suggest that mood disorder comorbidity was not primarily responsible for the final latent class solution in the full sample. For instance, although the rate of depression was significantly higher in Class 1 in the full sample analyses, mood disorders were prevalent in both classes (47.7% vs. 31.7%). Moreover, the majority of patients in Class 1 (52.3%) did not have a current mood disorder, despite having a risk profile (high NT and low PT) that was in accord with the theoretical risk profile of mood disorders.
Nevertheless, although we have posited that some individuals with SAD have a risk profile that places them at higher risk for developing subsequent mood disorders (i.e., Class 1), this could not be directly tested in the current sample with pre-existing depression diagnoses. Given that the age of SAD onset usually precedes the onset of mood disorders by several years (cf. Brown et al., 2001), it would be of interest to determine the extent to which these risk profiles are replicated in samples of children or adolescents with SAD who have yet to develop comorbid depression.
Time-series research should be done to evaluate if risk profiles predict the longitudinal course and treatment response of SAD, and do so more strongly than symptom-based SAD types (e.g., performance, generalized) or risk dimensions in isolation. Given previous findings that individuals with lower neuroticism and higher extraversion have better treatment outcomes (e.g., Bush et al., 2004; Quilty et al., 2008; Spek, Nyklícek, Cuijpers, & Pop, 2008; Wolitzky-Taylor, Arch, Rosenfield, & Craske, 2012), it seems plausible that persons with a Class 1 risk profile would have a worse prognosis than persons in Class 2. Individuals with the Class 1 risk profile may be more likely to have comorbid depression and longstanding negative core-beliefs that are more resistant to treatment and less likely to spontaneously resolve. Findings attesting to the heterogeneity of SAD point to the possibility that individuals should not receive the same treatment simply because of their diagnosis. Knowledge of an individual’s risk profile may improve treatment planning and help clinicians to better tailor therapy. For example, patients with SAD with a Class 2 risk profile (i.e., higher PT) may benefit more from pure exposures, whereas patients with a risk profile along the lines of Class 1 risk profile may require more cognitive restructuring around negative self-cognitions. Because various forms of SAD symptom presentations were found in both classes (e.g., although more common in Class 1, many patients with generalized SAD resided in Class 2), it may not be optimal to base these treatment decisions solely on the number or type of feared social situations. Thus, risk profiles may provide important additional information about treatment planning for SAD.
Moreover, it would be informative to evaluate whether the genetic liabilities of SAD vary as a function of the risk profile. Whereas NT and PT are unquestionably heritable (e.g., Bouchard & McGue, 2003; Jang, Livesley, & Vernon, 1996), the current findings suggest that the relevance of these risk dimensions to SAD differ among affected individuals. If latent classes of risk indeed have distinct genetic profiles, then the gene associations reported in previous studies of SAD would be weakened or obscured. In general, dimension-based profile approaches to risk and disorder classification (e.g., Rosellini & Brown, 2014) may produce stronger genetic associations than have been found in prior research which has focused predominantly on disorders in isolation while ignoring comorbidity and underlying dimensions of risk.
The replicability of these classes, both longitudinally and within other samples, should be tested. Due to the cross-sectional nature of these data, it is yet to be seen whether SAD individuals’ risk profiles change over the course of their illness and lifetimes. There has been some evidence that neuroticism and extraversion can change as a result of treatment (e.g., Carl, Gallagher, Sauer-Zavala, Bentley, & Barlow, 2014), and examining patients before and after treatment would help establish the nature and stability of these classes. Additionally, although this study examined the latent profiles of variables construed to be dimensions of disorder risk, the study focused on patients with pre-existing disorders. Thus, the directionality of SAD risk profile relationships could not be addressed (e.g., profiles may have emanated from variations in the expression of SAD or from diagnostic comorbidity). Also, the composition of the sample and study measures could have strongly influenced the extracted profiles. For example, in addition to the influence of mood disorder comorbidity, the latent class structure may have differed if the performance type of SAD was better represented in the sample.
Despite these aforementioned limitations, the present study is the first to determine if SAD could be subtyped on the basis of latent risk profiles. Our FMM results and subsequent concurrent validity analyses provide strong initial evidence for the potential utility of subclassifying patients with emotional disorders on the basis of distinct profiles of risk. More so than the symptom expression of the condition itself, these risk profiles may greatly inform our understanding of psychological disorders’ etiology, course, complications, and treatment response. Accordingly, risk profiles of this nature should have a prominent role in future classification systems that aim to supplant nosologies based on unitary categories (e.g., DSM-5) with dimensional approaches that emphasize patterns of functioning across an array of transdiagnostic features (e.g., Brown & Barlow, 2009; Rosellini & Brown, 2019).
Supplementary Material
Acknowledgments
The authors thank Anthony J. Rosellini for his comments on this manuscript. This research was funded by a grant from the National Institute of Mental Health (R01 MH039096; PI: Brown).
Footnotes
Disclosure Statement
The authors declare no conflicts of interest with respect to the authorship or the publication of this article.
The term “risk” is used throughout this paper in reference to these constructs which are putative vulnerability factors for emotional disorders (cf. Clark, Watson, & Mineka, 1994). The reader should keep in mind that this is not a study of disorder risk per se given the use of a clinical sample (see Discussion).
In order to compare our class means to norms, we utilized the full DASS Anxiety scale scores.
The complete results of these re-analyses are available upon request.
References
- American Psychiatric Association. (1987). Diagnostic and statistical manual of mental disorders : DSM-III-R. (3rd ed., rev..). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders : DSM-IV-TR. (4th ed., text revision..). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders : DSM-5. (5th ed..). Washington, DC: Author. [Google Scholar]
- Barlow DH (2000). Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory. American Psychologist, 55, 1247–1263. [DOI] [PubMed] [Google Scholar]
- Beck AT, & Steer RA (1990). Manual for the Beck Anxiety Inventory. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Blöte AW, Kint MJW, Miers AC, & Westenberg PM (2009). The relation between public speaking anxiety and social anxiety: A review. Journal of Anxiety Disorders, 23, 305–313. https://doi.Org/10.1016/j.janxdis.2008.11.007 [DOI] [PubMed] [Google Scholar]
- Bouchard TJ, & McGue M (2003). Genetic and environmental influences on human psychological differences. Journal of Neurobiology, 54, 4–45. 10.1002/neu.10160 [DOI] [PubMed] [Google Scholar]
- Brown TA (2007). Temporal course and structural relationships among dimensions of temperament and DSM-IV anxiety and mood disorder constructs. Journal of Abnormal Psychology, 116, 313–328. https://doi.Org/10.1037/0021-843X.116.2.313 [DOI] [PubMed] [Google Scholar]
- Brown TA, & Barlow DH (2009). A proposal for a dimensional classification system based on the shared features of the DSM-IV anxiety and mood disorders: Implications for assessment and treatment. Psychological Assessment, 21, 256–271. 10.1037/a0016608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, & Mancill RB (2001). Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology, 110, 585–599. 10.1037/0021-843X.110.4.585 [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, & Barlow DH (1998). Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology, 107, 179–192. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Korotitsch W, & Barlow DH (1997). Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behaviour Research and Therapy, 35, 79–89. [DOI] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, & Campbell LA (2001). Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology, 110, 49–58. 10.1037/0021-843X.110.1.49 [DOI] [PubMed] [Google Scholar]
- Brown TA, & McNiff J (2009). Specificity of autonomic arousal to DSM-IV panic disorder and posttraumatic stress disorder. Behaviour Research and Therapy, 47, 487. https://doi.Org/10.1016/j.brat.2009.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, & Naragon-Gainey K (2013). Evaluation of the unique and specific contributions of dimensions of the triple vulnerability model to the prediction of DSM-IV anxiety and mood disorder constructs. Behavior Therapy, 44, 277–292. https://doi.Org/10.1016/j.beth.2012.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush T, Rutter C, Simon G, Von Korff M, Katon WJ, Walker EA, … Ludman E (2004). Who benefits from more structured depression treatment? International Journal of Psychiatry in Medicine, 34, 247–258. 10.2190/LF18-KX2G-KT79-05U8 [DOI] [PubMed] [Google Scholar]
- Bylsma LM, Morris BH, & Rottenberg J (2008). A meta-analysis of emotional reactivity in major depressive disorder. Clinical Psychology Review, 28, 676–691. https://doi.Org/10.1016/j.cpr.2007.10.001 [DOI] [PubMed] [Google Scholar]
- Bylsma LM, Taylor-Clift A, & Rottenberg J (2011). Emotional reactivity to daily events in major and minor depression. Journal of Abnormal Psychology, 120, 155–167. 10.1037/a0021662 [DOI] [PubMed] [Google Scholar]
- Carl JR, Gallagher MW, Sauer-Zavala SE, Bentley KH, & Barlow DH (2014). A preliminary investigation of the effects of the unified protocol on temperament. Comprehensive Psychiatry, 55, 1426–1434. https://doi.Org/10.1016/j.comppsych.2014.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, & White TL (1994). Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS Scales. Journal of Personality and Social Psychology, 67, 319–333. 10.1037/0022-3514.67.2.319 [DOI] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, … Moffitt TE (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2, 119–137. 10.1177/2167702613497473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, & Watson D (2006). Distress and fear disorders: An alternative empirically based taxonomy of the “mood” and “anxiety” disorders. British Journal of Psychiatry, 189, 481–483. 10.1192/bjp.bp.106.03825 [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D, & Mineka S (1994). Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology, 103, 103–116. 10.1037/0021-843X.103.1.103 [DOI] [PubMed] [Google Scholar]
- Conway CC, & Brown TA (2018). Evaluating dimensional models of psychopathology in outpatients diagnosed with emotional disorders: A cautionary tale. Depression and Anxiety, 35, 898–902. 10.1002/da.22740 [DOI] [PubMed] [Google Scholar]
- Costa PT, & McCrae RR (1992). NEO PI-R professional manual. Odessa, FL: Psychological Assessment Resources, Inc. [Google Scholar]
- Di Nardo PA, Brown TA, & Barlow DH (1994). Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Eysenck HJ, & Eysenck SBG (1975). Manual of Eysenck Personality Questionnaire. London: Hodder and Stoughton. [Google Scholar]
- Fanous A, Gardner CO, Prescott CA, Cancro R, & Kendler KS (2002). Neuroticism, major depression and gender: a population-based twin study. Psychological Medicine, 32, 719–728. [DOI] [PubMed] [Google Scholar]
- Farmer AS, & Kashdan TB (2014). Affective and self-esteem instability in the daily lives of people with generalized social anxiety disorder. Clinical Psychological Science, 2, 187–201. 10.1177/2167702613495200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ, & Jazaieri H (2014). Emotion, emotion regulation, and psychopathology: an affective science perspective. Clinical Psychological Science, 2, 387–401. 10.1177/2167702614536164 [DOI] [Google Scholar]
- Heimberg RG, Holt CS, Schneier FR, Spitzer RL, & Liebowitz MR (1993). The issue of subtypes in the diagnosis of social phobia. Journal of Anxiety Disorders, 7, 249–269. 10.1016/0887-6185(93)90006-7 [DOI] [Google Scholar]
- Heller AS, Johnstone T, Shackman AJ, Light SN, Peterson MJ, Kolden GG, … Davidson RJ (2009). Reduced capacity to sustain positive emotion in major depression reflects diminished maintenance of fronto-striatal brain activation. Proceedings of the National Academy of Sciences, 106, 22445–22450. 10.1073/pnas.0910651106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry JD, & Crawford JR (2005). The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology, 44, 227–239. 10.1348/014466505X29657 [DOI] [PubMed] [Google Scholar]
- Hettema JM, Prescott CA, & Kendler KS (2004). Genetic and environmental sources of covariation between generalized anxiety disorder and neuroticism. American Journal of Psychiatry, 161, 1581–1587. https://doi.Org/10.1176/appi.ajp.161.9.1581 [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Fang A, & Asnaani A (2012). Emotion dysregulation model of mood and anxiety disorders. Depression and Anxiety, 29, 409–416. 10.1002/da.21888 [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jang KL, Livesley WJ, & Vernon PA (1996). Heritability of the big five personality dimensions and their facets: a twin study. Journal of Personality, 64, 577–591. [DOI] [PubMed] [Google Scholar]
- Kashdan TB (2007). Social anxiety spectrum and diminished positive experiences: theoretical synthesis and meta-analysis. Clinical Psychology Review, 27, 348–365. https://doi.Org/10.1016/j.cpr.2006.12.003 [DOI] [PubMed] [Google Scholar]
- Kashdan TB, & Farmer AS (2014). Differentiating emotions across contexts: comparing adults with and without social anxiety disorder using random, social interaction, and daily experience sampling. Emotion, 14, 629–638. 10.1037/a0035796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan TB, & Steger MF (2006). Expanding the topography of social anxiety. An experience-sampling assessment of positive emotions, positive events, and emotion suppression. Psychological Science, 17, 120–128. 10.1111/j.1467-9280.2006.01674.x [DOI] [PubMed] [Google Scholar]
- Kerns CE, Comer JS, Pincus DB, & Hofmann SG (2013). Evaluation of the proposed social anxiety disorder specifier change for DSM-5 in a treatment-seeking sample of anxious youth. Depression and Anxiety, 30, 709–715. 10.1002/da.22067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 617–627. https://doi.Org/10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, & Wittchen H-U (2012). Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21, 169–184. 10.1002/mpr.1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y, Mendell NR, & Rubin DB (2001). Testing the number of components in a normal mixture. Biometrika, 88, 767–778. https://doi.Org/10.1093/biomet/88.3.767 [Google Scholar]
- Lovibond SH, & Lovibond PF (1995). Manual for the Depression Anxiety Stress Scales (2nd ed.). Sydney: Psychology Foundation of Australia. [Google Scholar]
- Mattick RP, & Clarke JC (1998). Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy, 36, 455–470. [DOI] [PubMed] [Google Scholar]
- Mineka S, Watson D, & Clark LA (1998). Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology, 49, 377–412. https://doi.Org/10.1146/annurev.psych.49.1.377 [DOI] [PubMed] [Google Scholar]
- Mor N, Doane LD, Adam EK, Mineka S, Zinbarg RE, Griffith JW, … Nazarian M (2010). Within-person variations in self-focused attention and negative affect in depression and anxiety: A diary study. Cognition and Emotion, 24, 48–62. 10.1080/02699930802499715 [DOI] [Google Scholar]
- Muthén LK, & Muthén BO (1998). Mplus User’s Guide (7th ed.). Los Angeles: Author. [Google Scholar]
- Naragon-Gainey K, Gallagher MW, & Brown TA (2013). Stable “trait” variance of temperament as a predictor of the temporal course of depression and social phobia. Journal of Abnormal Psychology, 122, 611–623. 10.1037/a0032997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling, 14, 535–569. 10.1080/10705510701575396 [DOI] [Google Scholar]
- Pollard CA, & Henderson JG (1988). Four types of social phobia in a community sample. Journal of Nervous and Mental Disease, 176, 440–445. [DOI] [PubMed] [Google Scholar]
- Quilty LC, De Fruyt F, Rolland J-P, Kennedy SH, Rouillon PF, & Bagby RM (2008). Dimensional personality traits and treatment outcome in patients with major depressive disorder. Journal of Affective Disorders, 108, 241–250. https://doi.Org/10.1016/j.jad.2007.10.022 [DOI] [PubMed] [Google Scholar]
- Raftery AE (1995). Bayesian model selection in social research. Sociological Methodology, 25, 111–163. 10.2307/271063 [DOI] [Google Scholar]
- Rapee RM, Craske MG, & Barlow DH (1994). Assessment instrument for panic disorder that includes fear of sensation-producing activities: The Albany Panic and Phobia Questionnaire. Anxiety, 1, 114–122. [DOI] [PubMed] [Google Scholar]
- Rosellini AJ, & Brown TA (2014). Initial interpretation and evaluation of a profile-based classification system for the anxiety and mood disorders: Incremental validity compared to DSM-IV categories. Psychological Assessment, 26, 1212–1224. 10.1037/pas0000023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosellini AJ, & Brown TA (2019). The Multidimensional Emotional Disorder Inventory (MEDI): Assessing transdiagnostic dimensions to validate a profile approach to emotional disorder classification. Psychological Assessment, 31, 59–72. https://doi:10.1037/pas0000649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, & Kessler RC (2008). Social fears and social phobia in the USA: Results from the National Comorbidity Survey Replication. Psychological Medicine, 38, 15–28. 10.1017/S0033291707001699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spek V, Nyklícek I, Cuijpers P, & Pop V (2008). Predictors of outcome of group and internet-based cognitive behavior therapy. Journal of Affective Disorders, 105, 137–145. https://doi.Org/10.1016/j.jad.2007.05.001 [DOI] [PubMed] [Google Scholar]
- Stemberger RT, Turner SM, Beidel DC, & Calhoun KS (1995). Social phobia: An analysis of possible developmental factors. Journal of Abnormal Psychology, 104, 526–531. [DOI] [PubMed] [Google Scholar]
- Suárez LM, Bennett SM, Goldstein CR, & Barlow DH (2009). Understanding anxiety disorders from a “triple vulnerability” framework. In Antony MM, Stein MB, Antony MM (Ed), & Stein MB (Ed) (Eds.), Oxford handbook of anxiety and related disorders. (pp. 153–172). New York: Oxford University Press. [Google Scholar]
- Turner SM, Beidel DC, Dancu CV, & Keys DJ (1986). Psychopathology of social phobia and comparison to avoidant personality disorder. Journal of Abnormal Psychology, 95, 389–394. [DOI] [PubMed] [Google Scholar]
- Vermunt JK (2010). Latent class modeling with covariates: Two improved three-step approaches. Political Analysis, 18, 450–469. 10.1093/pan/mpq025 [DOI] [Google Scholar]
- Viken RJ, Rose RJ, Kaprio J, & Koskenvuo M (1994). A developmental genetic analysis of adult personality: Extraversion and neuroticism from 18 to 59 years of age. Journal of Personality and Social Psychology, 66, 722–730. [DOI] [PubMed] [Google Scholar]
- Watson D (2005). Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology, 114, 522–536. https://doi.Org/10.1037/0021-843X.114.4.522 [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Carey G (1988). Positive and negative affectivity and their relation to anxiety and depressive disorders. Journal of Abnormal Psychology, 97, 346–353. [DOI] [PubMed] [Google Scholar]
- Watson D, Gamez W, & Simms LJ (2005). Basic dimensions of temperament and their relation to anxiety and depression: A symptom-based perspective. Journal of Research in Personality, 39, 46–66. https://doi.Org/10.1016/j.jrp.2004.09.006 [Google Scholar]
- Wolitzky-Taylor KB, Arch JJ, Rosenfield D, & Craske MG (2012). Moderators and non-specific predictors of treatment outcome for anxiety disorders: A comparison of cognitive behavioral therapy to acceptance and commitment therapy. Journal of Consulting and Clinical Psychology, 80, 786–799. 10.1037/a0029418 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.