Abstract
Purpose:
Current literature disagrees on whether fertility counseling decreases or increases decision regret among young breast cancer survivors. This study investigates whether fertility counseling provided to pre-menopausal breast cancer patients regarding infertility due to treatment is associated with decision regret post-treatment, and how that relationship is moderated by information adequacy.
Methods:
Breast cancer patients aged 18–35 listed in the Pennsylvania cancer registry as diagnosed between 2007 and 2012 were surveyed. Basic descriptive analyses were conducted, and linear regression models were estimated.
Results:
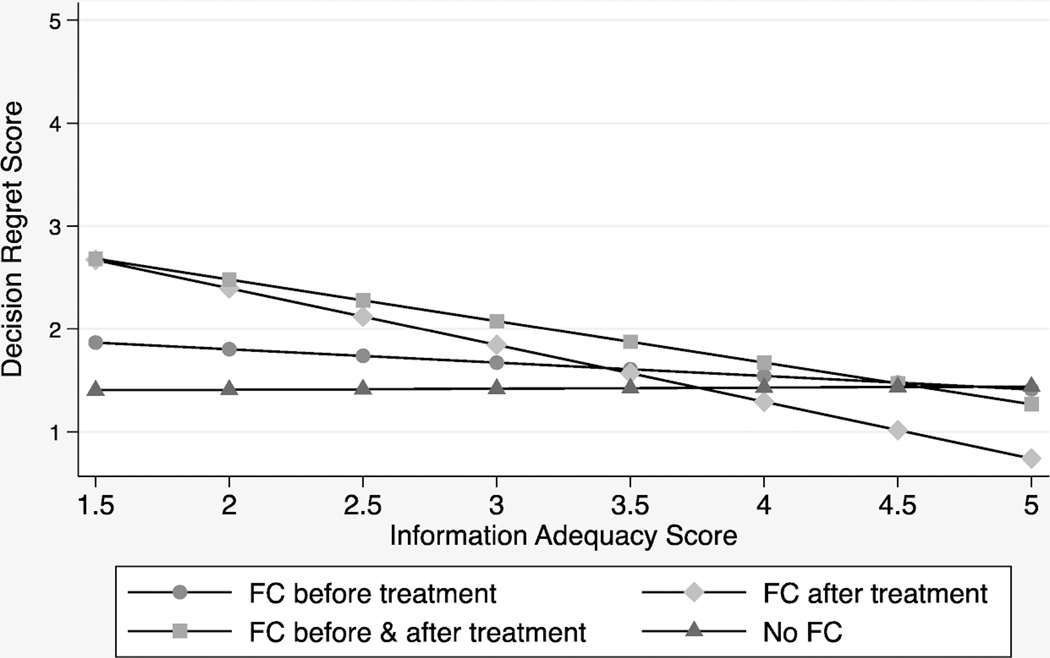
Receipt of fertility counseling was not directly associated with decision regret. However, as fertility information adequacy increased, decision regret significantly decreased among women who received fertility counseling after finishing treatment or before and after finishing treatment. On average, a woman who receives fertility counseling before and after treatment with an information adequacy score of 1.5 had a regret score of 2.68. In contrast, a woman who received fertility counseling before and after treatment who had a fertility information adequacy score of 5 had a regret score of only 1.26 on average.
Conclusion:
Information adequacy is a significant moderator in the relationship between fertility counseling and decision regret. This suggests a possible explanation for disagreement in the literature regarding the benefits of fertility counseling and highlights the need for an increased focus on the adequacy of the information provided.
Implications for Cancer Survivors:
Fertility counseling should be pursued for young adult breast cancer patients and survivors, provided that their satisfaction with the information received is monitored and remains high.
Keywords: breast cancer, survivorship, counseling, fertility
Introduction
The receipt of a breast cancer diagnosis is a stressful time that requires patients to make difficult treatment-related decisions in a short amount of time.[1,2] These decisions affect the odds of entering remission and, among pre-menopausal women, the odds of conceiving a child and carrying a pregnancy to term once treatment has ended.[3] Balancing the need for aggressive treatment with the desire to have children is a difficult task, and decision regret can have long-term consequences for the emotional wellbeing of young breast cancer survivors.[4,5]
Women in their reproductive years (aged less than 50) account for more than 20% of all breast cancer cases.[6]. If caught at a local or regional stage, the 5-year survival rate for young women diagnosed with breast cancer is greater than 85%.[7] With such promising odds, quality of life post-treatment is an important consideration for survivors. However, the survivorship literature finds that patients diagnosed in young adulthood have unique stressors compared to those diagnosed later in life.[8,9] Many young patients may not have formed permanent partnerships, finished their education, settled into careers, or had children. Fertility is a particularly important factor to consider as it may often signal a return to normality.[10] Unfortunately, the desire for children may not surface until years after treatment is completed,[10] but the odds of an unassisted pregnancy post-treatment are very low, thus, the ability to conceive is best safeguarded before treatment has begun.[11]
Even when preservation treatments are discussed with younger patients, they are not always an option due to the necessity for urgent treatment or for financial reasons.[12] For example, embryo cryopreservation is the most established form of fertility preservation, but the process for obtaining the embryos can take up to two weeks from the beginning of the menstrual cycle,[13] which could delay necessary treatment later than many doctors would advise. Other types of fertility preservation are being investigated, but they are less established and often have lower success rates.[13]
Unfortunately, prior studies reveal low patient awareness of the infertility risks associated with cancer treatment.[9] Qualitative research suggests that many women undergoing chemotherapy are concerned about the effects of treatment on their fertility, but were unsure how to discuss this issue with their doctors.[14] Instead, they waited for the doctor to initiate the discussion, or did not have the discussion at all.[14] High levels of fertility concerns during treatment have been shown to be associated with regret, depression and poor emotional wellbeing during remission;[15,16] and at least one study has shown that approximately half of the women who were concerned about their fertility during treatment did not feel that these concerns were fully addressed.[17] Previous research on breast cancer screening and hormone replacement therapy shows that patients who report receiving adequate information prior to treatment also report higher levels of satisfaction post-treatment and decreased levels of regret.[18,19] However, the literature investigating the relationship between fertility counseling and emotional wellbeing among young adult breast cancer patients has come to differing conclusions.[20] In some cases fertility counseling is associated with a decrease in regret[21] and improved quality of life.[12] In other cases, those who receive fertility counseling have higher levels of reproductive concerns after cancer compared to those who do not receiving counseling.[20] One paper found that among women who received counseling, more in-depth counseling was associated a decrease in reproductive concerns,[22] but there is currently no study examining how the quality of information presented to women who receive counseling may influence their regret scores relative to women who do not receive counseling. Thus, it is not clear if women who receive fertility counseling have improved emotional wellbeing relative to women who do not. This is uncomfortable, because not disclosing all of the information regarding the effects of treatment is unethical, even if it leads to depression or regret, but it is hard to advocate for fertility counseling when the results may not be positive.
To address this gap in the literature, this study examines whether fertility counseling provided to pre-menopausal breast cancer patients is associated with decreased decision regret post-treatment and whether the effects of fertility counseling receipt are influenced by information adequacy. Previous studies have addressed the quality of cancer related fertility information available online.[23] To our knowledge,, this is the first study to analyze patient rated information adequacy influences in the relationship between fertility counseling receipt and regret among young adult breast cancer survivors. The analysis is guided by two hypotheses. First, because our measure of fertility counseling is very general and leaves room for considerable variation in adequacy, we hypothesize that the direct relationship between counseling and regret will be positive, because concerns may be raised but not fully addressed within the counseling sessions. Second, we hypothesize that as information adequacy increases, regret will decrease among women who receive fertility counseling at any time point.
Methods
Data Collection
In September of 2015, we mailed out an original survey on the topic of fertility counseling among reproductive-aged breast cancer survivors. The sampling frame consisted of breast cancer survivors living in Pennsylvania who were diagnosed with breast cancer between the years 2007 – 2012, were between the ages of 18–35 at the time of diagnosis. In the United States, the collection and release of cancer registry data is organized by each individual state. We received our data from the Pennsylvania cancer registry and in designing our sampling strategy had to balance several concerns. First, we wanted to set our age of diagnosis between 18–35 to try and capture as many women who may have hoped to have children post-treatment as possible. We also wanted to maximize our chances of surveying women who had completed treatment as women may feel differently about their ability to conceive once they are no longer concerned with surviving their diagnosis and are ready to move toward ‘normality’.[10] These criteria combined with a concern for a large enough sample size led us to set our diagnosis window of 2007–2012
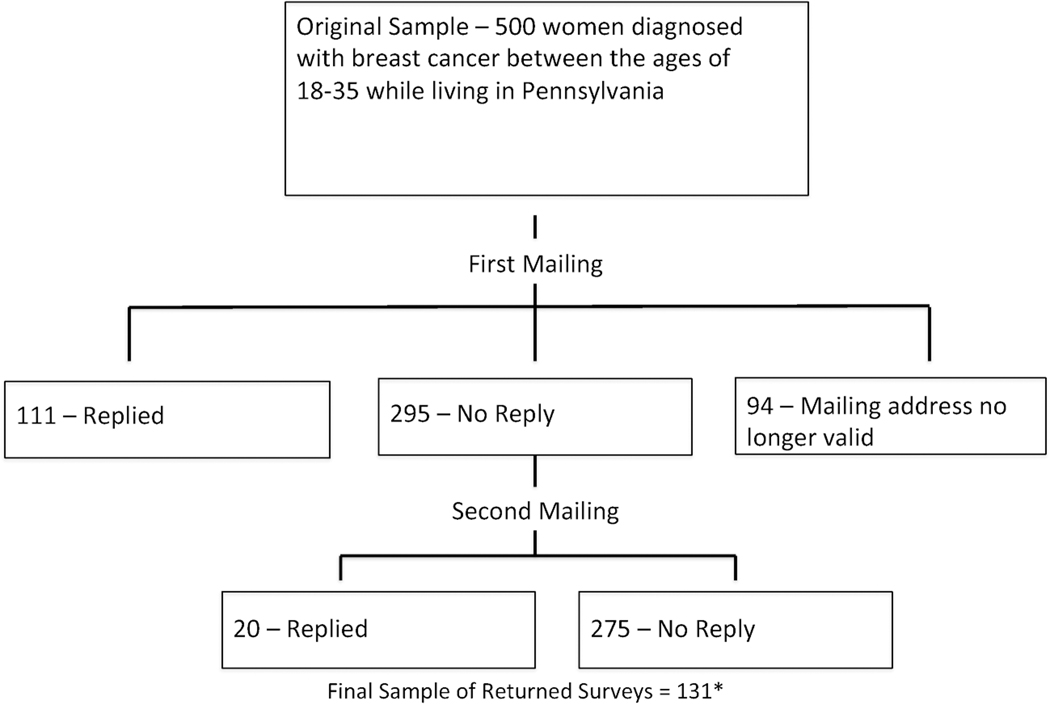
These selection criteria returned a sample of 860 women. Due to budget constraints, a random sample of 500 women was chosen from the original 860 using the sample command in STATA 13. There was no significant difference in age at diagnosis between women who were randomly selected relative to those who were not. A survey was then mailed to each woman in the sample in September of 2015 along with a pre-paid return envelope. Of these surveys (Figure 1), 111 were returned with the survey filled out, 94 were returned by the post office due to having outdated addresses, and 295 were not returned. A second, identical survey was sent out in January of 2016 to all 295 women who had not returned completed surveys. An additional 20 surveys were returned after the second mailing. Of the 406 surveys with valid addresses, 131 were returned, yielding a response rate of 32%, which is similar to other studies utilizing mail out surveys with one follow up.[24,25] A $2 bill was enclosed with both mail outs as a small incentive for returning the survey. Of the 131 surveys that were returned, three surveys had to be dropped; two were dropped because the respondents wrote a note to use in the margins of the survey that indicated that they did not have breast cancer and a third survey was dropped due to the respondent circling multiple answers for each question. Respondents were slightly older than non-responders 32.3 vs. 31.6 for non-responders (p<.05). There was no difference in time of diagnosis.
Figure 1.
Survey Response Flow Chart
* An additional 3 Surveys were dropped; 2 because the respondent indicated she did not have breast cancer and 1 because the respondent circled multiple answers to each question. Final N = 128
Measures
The dependent variable of interest is decision regret related to the woman’s breast cancer treatment choices. Regret was measured utilizing a four item scale adapted from the medical decision making literature.[26] This scale is measured continuously from 1 to 5 and has been validated among breast cancer patients.[26] The mean of all four items was calculated and scored such that higher scores indicate higher levels of regret. Preliminary analyses showed that this measure has a Cronbach’s Alpha of .91. A list of regret questionnaire items is located in Appendix A.
There are two independent variables of interest – receipt of fertility counseling and information adequacy. In this study, fertility counseling is defined as any conversation with a health care provider regarding post-treatment fertility. There are two survey questions inquiring about fertility counseling. The first question asked, “[a]fter your diagnosis, but before you started your cancer treatment, did you talk about potential trouble having children due to your cancer treatment with any of your healthcare providers (primary care doctor, cancer doctor, oncologist, radiologist, surgeon, nurse)?” and the second question asked, “[a]fter you finished your cancer treatment, were you ever informed by a doctor that you may have trouble conceiving a child?” inquiring whether fertility counseling was given post-treatment. Both questions are coded as yes/no. Utilizing these two questions a four level measure of fertility counseling was created as follows: 1 = Received Fertility Counseling Before Beginning Treatment, 2 = Received Fertility Counseling After Finishing Treatment, = 3 Received Fertility Counseling Before and After Treatment, and 4 = Did Not Receive Fertility Counseling. Fertility counseling receipt was represented in multivariate analyses by 3 dummy variables, where Did Not Receive Fertility Counseling was the omitted category.
The information adequacy scale was adapted from two previously validated studies in the medical decision making literature investigating information adequacy regarding flu vaccine [15] and prophylactic breast cancer surgery [21].[19,27] Participants were asked to complete 12 items measured on a likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The list of information adequacy questions began with a prompt of, “In regards to the effects of your cancer treatment on your fertility would you say…” Exploratory analyses revealed that the mean value of questions which specifically referenced childbearing such as, “I wanted more information about how my breast cancer treatment may affect having children,” were significantly lower than the mean value questions that did not contain this additional prompt such as, “I wanted clearer advice about my breast cancer treatment.” Thus, it was decided that the questions would be divided into two categories: fertility information adequacy and general information adequacy. The measures were entered into the model separately. All questions are scored on a likert scale from 1 (strongly disagree) to 5 (strongly agree) and are analyzed continuously. A full list of questions is located in appendix B and questions requiring reverse coding are marked with an asterisk.
Control variables for current age, education (≤ HS/some college or Associate Degree/Bachelor’s Degree/Graduate Degree or higher), race (recoded as either white or non-white), current marital status (married/not married), self-rated health (excellent/very good/good/fair/poor), family income range ($0–34,999/$35,000–49,999/$50,000–74,999/$75,000–99,999/$100,000 or more) and receipt of fertility preservation treatment were also entered into the model. To measure fertility preservation respondents were asked, “Did you choose to undergo any type of fertility preservation treatment, like freezing eggs, prior to your breast cancer treatment?” Responses were coded as yes/no. All variables were self-reported. All analyses were run using STATA version 13. This study was approved by the University Park IRB at the Pennsylvania State University (STUDY00001163).
Results
Table 1 presents descriptive statistics for the full sample and by receipt of fertility counseling. More than two-thirds (72%) of the women surveyed received fertility counseling at some point. There are no statistically significant differences at the p<.05 level between the sample of women who received fertility counseling and those who did not. However, the women who received fertility counseling had a higher regret score (1.67) than women who did not (1.38) and the difference is marginally significant (p=.07). Women who received fertility counseling also had slightly higher scores on the fertility information adequacy scale (3.75 compared 3.48), where higher scores indicated increased information adequacy. This group, however, did not have higher scores on the general information adequacy scale (3.88 vs. 4.06). Women who did not receive counseling from a healthcare provider reported getting information from printed brochures, web pages and family friends. Some also said that did not receive any information at all or that they did not know/preferred not to answer. Also, a greater proportion of women who reported receiving fertility counseling had a graduate degree or higher compared to women not receiving fertility counseling (32% vs. 17%).
Table 1.
Descriptives of the Full and Analytic Samples
| Full Sample | Received Counseling | Did Not Receive Counseling | |||||
|---|---|---|---|---|---|---|---|
| Variable | % or Mean (SE) | Number of Obs. | % or Mean (SE) | Number of Obs. | % or Mean (SE) | Number of Obs. | p-value |
| Regret | 1.59 (.07) | 104 | 1.67 (.09) | 75 | 1.38 (.12) | 29 | 0.07 |
| Fertility Counseling | |||||||
| Received Fertility Counseling | |||||||
| Before Beginning Treatment | 26.92% | 28 | -- | -- | |||
| Received Fertility Counseling | |||||||
| After Finishing Treatment | 8.65% | 9 | -- | -- | |||
| Received Fertility Counseling | |||||||
| Before and After Treatment | 37% | 38 | -- | -- | |||
| Did not Receive Fertility | |||||||
| Counseling | 27.88% | 29 | -- | -- | |||
| Fertility Information Adequacy | 3.68 (.09) | 104 | 3.75 (.10) | 75 | 3.48 (.18) | 29 | 0.18 |
| General Information Adequacy | 3.93 (.08) | 104 | 3.88 (.10) | 75 | 4.06 (.13) | 29 | 0.32 |
| Had Fertility Preservation | |||||||
| Treatment | |||||||
| Yes | 8.65% | 9 | 12.00% | 9 | 0.00% | 0 | 0.50 |
| No | 91.35% | 95 | 88.00% | 66 | 100.00% | 29 | |
| Age (at the time of the survey) | 37.69 (.33) | 104 | 37.69 (.35) | 75 | 37.69 (.75) | 29 | 0.99 |
| Age (at the time of diagnosis) | 32.14 (.27) | 104 | 32.19 (30) | 75 | 32.03 | 29 | 0.74 |
| Education | |||||||
| High School or Less | 14.42% | 15 | 13.33% | 10 | 17.24% | 5 | 0.48 |
| Associates or Some College | 29.81% | 31 | 29.33% | 22 | 31.03% | 9 | |
| Bachelor’ s Degree | 27.88% | 29 | 25.33% | 19 | 34.48% | 10 | |
| Graduate Degree or Higher | 27.88% | 29 | 32.00% | 24 | 17.24% | 5 | |
| Race | |||||||
| White | 81.73% | 85 | 79.31% | 62 | 82.67% | 23 | 0.69 |
| Other | 18.27% | 19 | 20.69% | 13 | 17.33% | 6 | |
| Married | |||||||
| Yes | 70.19% | 73 | 72.00% | 54 | 65.52% | 19 | 0.51 |
| No | 29.81% | 31 | 28.00% | 21 | 34.48% | 10 | |
| Combined Family Income | |||||||
| $0 - $34,999 | 18.27% | 19 | 14.67% | 11 | 27.59% | 8 | 0.21 |
| $35,000 - $49,999 | 9.62% | 10 | 12.00% | 9 | 3.45% | 1 | |
| $50,000 - $74,999 | 21.15% | 22 | 24.00% | 18 | 13.79% | 4 | |
| $75,000 - $99,999 | 18.27% | 19 | 20.00% | 15 | 13.79% | 4 | |
| $100,000 and over | 32.69% | 34 | 29.33% | 22 | 41.38% | 12 | |
| Self-Rated Health | 3.62 (.09) | 104 | 3.69 (.10) | 75 | 3.41 (.19) | 29 | 0.16 |
Table 2 displays the results from linear regressions analyzing the relationship between fertility counseling and regret. Model 1 shows the bivariate relationship between fertility counseling and regret. There is a .89 point increase in regret when fertility counseling is received after treatment (p<.01). In Model 2, controls were added to the model and fertility counseling is no longer a significant predictor of a woman’s regret score. Fertility information adequacy is also not significantly associated with regret. However, for each one point increase in general information adequacy, there is .53 point decrease in regret (p<.001).
Table 2.
Full Models Investigating the Relationship Between Fertility Counseling, Information Adequacy and Regret (N=104)
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| Variable | β | SE | β | SE | β | SE |
| Fertility Counseling | ||||||
| Received Fertility Counseling Before Beginning Treatment | 0.24 | (0.19) | 0.16 | (0.15) | 0.67 | (0.52) |
| Received Fertility Counseling After Finishing Treatment | 0.89** | (0.27) | 0.27 | (0.22) | 2.11* | (0.96) |
| Received Fertility Counseling Before and After Treatment | 0.19 | (0.17) | 0.29 | (0.15) | 1.90** | (0.71) |
| Did not Receive Fertility Counseling | -- | -- | -- | |||
| Fertility Information Adequacy | −0.11 | (0.09) | 0.01 | (0.11) | ||
| Fertility Information Adequacy * Received Fertility Counseling Before Beginning Treatment | −0.14 | (0.14) | ||||
| Fertility Information Adequacy * Received Fertility Counseling After Finishing Treatment | −0.56* | (0.26) | ||||
| Fertility Information Adequacy * Received Fertility Counseling Before and After Treatment | −0.42* | (0.18) | ||||
| Fertility Information Adequacy * Did not Receive Fertility Counseling | -- | |||||
| General Information Adequacy | −0.53*** | (0.11) | −0.43*** | (0.11) | ||
| Had Fertility Preservation Treatment | ||||||
| Yes | −0.01 | (0.21) | −0.14 | (0.22) | ||
| No | -- | -- | ||||
| Age (at the time of the survey) | 0.02 | (0.02) | 0.02 | (0.02) | ||
| Education | 0.04 | (0.06) | 0.07 | (0.06) | ||
| Race | ||||||
| White | −0.01 | (0.15) | −0.04 | (0.15) | ||
| Other | -- | -- | ||||
| Married | ||||||
| Yes | 0.13 | (0.15) | 0.12 | (0.15) | ||
| No | -- | -- | ||||
| Combined Family Income | 0.01 | (0.05) | −0.14 | −0.05 | ||
| Self-Rated Health | −0.09 | (0.06) | −.08 | (0.06) | ||
| Constant | 1.38*** | (0.13) | 3.24*** | (0.84) | 2.31* | (0.92) |
p<.05
p<.01
p<.001
Model 3 displays the results of the full model that interacts receipt of fertility counseling with fertility information adequacy. In this model, general information adequacy still significantly decreases regret by .43 points (p<.001) and fertility information adequacy is significantly associated with the relationship between fertility counseling and regret. This relationship is displayed graphically in Figure 2. The lines representing women who received fertility counseling before and after treatment and those receiving fertility counseling after treatment only are both downward sloping. This indicates that these women’s regret levels are considerably reduced when they received more adequate fertility information compared to women experiencing the same temporal patterns of fertility counseling but receiving less adequate information.
Fig 2.
The Relationship between Fertility Counseling and Information Adequacy with Decision Regret
Discussion
Support for the hypotheses posed by this paper are mixed. The first hypothesis posited that women who received fertility counseling at any time point would have higher regret scores relative to women who did not receive counseling. This hypothesis was based upon previous research showing that young adult breast cancer patients who received fertility counseling prior to beginning treatment had increased reproductive concerns relative to patients who did not receive counseling.[20] This hypothesis was partially supported. In the bivariate model, receipt of fertility counseling after treatment was significantly associated with an increase in regret. This relationship was no longer significant once controls were entered into the model, which suggests that other factors including information adequacy influence feelings of regret. This brings us to our second hypothesis, which is that regret scores will decrease as fertility information adequacy increases.
The second hypothesis was also partially supported. Information adequacy influences the relationship between fertility counseling and regret among women who only received fertility counseling after finishing treatment or received counseling both pre- and post-treatment. It must be stressed that we did not ask about the content of the conversations. We only asked if the conversation happened and how satisfied the woman was with the information she received. One of the explanations put forth to explain the phenomenon of increased reproductive concerns among women receiving fertility counseling is that these women have a deeper understanding of the possible harm that chemotherapy and radiation can pose to their future childbearing goals.[20] Thus, it is possible that the women who received counseling had the greatest understanding of their potential fertility problems moving forward. What is important to note, however, is that awareness of potential fertility problems can be raised without a deeper conversation regarding fertility goals and potential avenues to reach these goals. It is possible that some information was given, but it was not enough information or the type of information the patient felt she needed. Thus, the adequacy component is important since reproductive possibilities vary greatly between women depending on age and the type of cancer treatment they received.[28] The significant relationship between information adequacy and fertility counseling in the full model suggests that a conversation regarding fertility, provided it is high quality, is helpful as the woman moves into survivorship. This may be especially true for young adult women as they begin to think about marriage and family post-treatment.[29] Intervention studies have found that women respond positively to the inclusion of psychologists in discussions of fertility preservation and post-treatment fertility goals.[5] While oncologists and gynecologists focus on the physical body, a psychologist may be better equipped to handle the emotions surrounding fertility, which encompass sexuality, body image, and female identity alongside the ability to conceive.[4,30,31]
Currently, the evidence regarding the positive impacts of fertility counseling on emotional is mixed. Some studies have found that fertility counseling decreases reproductive concerns[22] and improves quality of life among breast cancer survivors,[21] but there are also conflicting findings suggesting that fertility counseling can actually increase reproductive concerns post-treatment.[20] This study sought to bridge the gap between these studies by positing that just having the fertility conversation may not be enough to sufficiently allay a woman’s fears as she enters survivorship. Rather, the content and quality of the information presented as well as the woman’s understanding of that information may play a vital role in whether or not fertility counseling can improve a woman’s quality of life post-treatment. Thus, the comparison between those women who receive counseling and those who do not is absolutely key in determining if fertility counseling can be done without decreasing emotional wellbeing.
It should also be noted that the definition of “fertility counseling” in this study is broad and general. Previous research has concluded that the materials presented to women during fertility counseling varies quite a bit and may not always be satisfactory.[32,33] Therefore, we decided on a very basic measure of fertility counseling to simply identify if the conversation took place and used the information adequacy measure as a proxy of how in depth the conversation may have been. Information adequacy was also purposely created as a general measure of the woman’s perception of the information she received rather than as an objective measure of the number and types of materials presented to her. The questions asked in the survey were written such that information quality between women who had a conversation with a provider regarding fertility and those who did not could be compared. The survey did not ask about specific materials presented or topics discussed – it only asked if the woman, “wanted more information about how breast cancer may affect having children, “ or if the woman, “was aware of the of the ways that my breast cancer could be treated and how each of the treatment options would affect childbearing.” It is quite possible that women who did receive counseling wanted more information while women who did not receive counseling felt their information was adequate and vice versa.
This study is meant as a first step in assessing the relationship between information adequacy and fertility counseling and cannot speak to the proper methods of improving communication between providers and patients regarding fertility. The survey was cross-sectional by design, and is subject to the weaknesses inherent in any survey that is given at only one time point. Fertility intentions have been shown to change as a woman progresses through treatment[34] and it is possible that regret and information adequacy scores will change as a woman moves farther away from the time of her treatment. When respondents are asked to recall how they felt or thought about a subject at an earlier time, especially something as sensitive as infertility, their response is subject to recall bias and may be unreliable. Future research should aim to measure information quality and regret at multiple time points in the cancer treatment continuum. In addition, in an attempt to keep the survey focused we did not ask additional questions regarding spouse/partner feelings during and after treatment. While this was outside the scope of our study, partner attitudes can significantly influence how a woman feels about her treatment[31,35] and future work should investigate how this impacts the relationship between information adequacy and decision regret.
In addition, this was a mail out survey and only sampled women who were treated in Pennsylvania. It is possible that women who did not respond or did not receive the survey due to changing addresses may be different in an important way from the women who completed and returned the surveys. The sample size is small, which may decrease the external validity. However, the likelihood of significant findings is reduced as the sample size decreases, which suggests that the relationship between information adequacy and fertility counseling is strong and worth pursuing further. These results also lend further support to studies suggesting that psychologists be incorporated into oncofertility care, as they may be able to better assess patient needs informational and decision-making needs.[30] Overall, this study offers insight into an unresolved issue in the breast cancer survivorship literature[20,22] and highlights the need for an increased focus on the content of fertility counseling as we move forward and seek to improve the quality of life of young adult breast cancer survivors.
Funding & Acknowledgments:
This work was supported by the Susan G. Komen Foundation Post-Baccalaureate Training Program in Disparities Research (grant number KG101424). This publication was also made possible in part by Grant TL1TR002531 (T. Hurley, PI) from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Award.
Appendix A: Decision Regret Questions Utilized in the Breast Cancer & Fertility Survey.
When thinking about your cancer treatment and the effects that it had on both your survival and your fertility, how would you rate the following statements (circle one):
| Strongly Disagree | Disagree | Neither Agree Nor Disagree | Agree | Strongly Agree | |
|---|---|---|---|---|---|
| a) My breast cancer treatment choice was the right decision* | 1 | 2 | 3 | 4 | 5 |
| b) I regret the breast cancer treatment choice that was made | 1 | 2 | 3 | 4 | 5 |
| c) I would go for the same breast cancer treatment if I had to do it over again* | 1 | 2 | 3 | 4 | 5 |
| d) My breast cancer treatment decision was a wise one | 1 | 2 | 3 | 4 | 5 |
Indicates the question was reverse coded for analysis
Appendix B: Information Adequacy Questions Utilized in the Breast Cancer & Fertility Survey.
In regards to the effects of your cancer treatment on your fertility would you say (circle one):
| Strongly Disagree | Disagree | Neither Agree Nor Disagree | Agree | Strongly Agree | |
|---|---|---|---|---|---|
| a) I am satisfied with the information I received about breast cancer treatment and childbearinga | 1 | 2 | 3 | 4 | 5 |
| b) I knew the pros and cons of the effects my breast cancer treatment on my future childbearinga | 1 | 2 | 3 | 4 | 5 |
| c) I wanted more information about how my breast cancer treatment may affect having childrena* | 1 | 2 | 3 | 4 | 5 |
| d) I wanted clearer advice about my breast cancer treatmentb* | 1 | 2 | 3 | 4 | 5 |
| e) I made a well informed choice regarding my breast cancer treatmentb | 1 | 2 | 3 | 4 | 5 |
| f) I was aware the of the ways that my breast cancer could be treated and how each of the treatment options would affect childbearinga | 1 | 2 | 3 | 4 | 5 |
| g) I felt I knew the benefits of my breast cancer treatmentb | 1 | 2 | 3 | 4 | 5 |
| h) I felt I knew the risks and side effects of my breast cancer treatment on childbearinga | 1 | 2 | 3 | 4 | 5 |
| i) It was hard to decide if the benefits of the breast cancer treatment were more important to me than the risks of not having a childa* | 1 | 2 | 3 | 4 | 5 |
| j) The breast cancer treatment decision was hard for me to makeb* | 1 | 2 | 3 | 4 | 5 |
| k) I was unsure what to do in regards to my breast cancer treatmentb* | 1 | 2 | 3 | 4 | 5 |
| l) It was clear what breast cancer treatment choice was best for meb | 1 | 2 | 3 | 4 | 5 |
indicates that this question was used to measure information adequacy related to fertility
indicates that this question was used to measure information adequacy related to general information
Indicates the question was reverse coded for analysis
Footnotes
Conflict of Interest: Dr. Angela G. Campbell & Dr. Marianne Hillemeier declare that they have no conflicts of interest to disclose. Informed consent was obtained from all individual participants included in the study. The authors have full control of all primary data and agree to release it to the journal for review if requested. This work was supported by the Susan G. Komen Foundation Post-Baccalaureate Training Program in Disparities Research [grant number KG101424].
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Contributor Information
Angela G. Campbell, Indiana University School of Medicine, Pediatric Health Services Research, 410 West 10th Street, Suite 2000, Indianapolis, IN 46202.
Marianne Hillemeier, The Pennsylvania State University.
References:
- 1.Al-Ghazal SK, Fallowfield L, Blamey RW. Comparison of psychological aspects and patient satisfaction following breast conserving surgery, simple mastectomy and breast reconstruction. Eur J Cancer. 2000. October;36(15):1938–43. [DOI] [PubMed] [Google Scholar]
- 2.Sheehan J, Sherman KA, Lam T, Boyages J. Association of information satisfaction, psychological distress and monitoring coping style with post-decision regret following breast reconstruction. Psycho-Oncology J Psychol Soc Behav Dimens Cancer. 2007;16(4):342–51. [DOI] [PubMed] [Google Scholar]
- 3.Benedict C, Thom B, Teplinsky E, Carleton J, Kelvin JF. Family-building After Breast Cancer: Considering the Effect on Adherence to Adjuvant Endocrine Therapy. Clin Breast Cancer. 2017. June;17(3):165–70. [DOI] [PubMed] [Google Scholar]
- 4.Logan S, Perz J, Ussher JM, Peate M, Anazodo A. A systematic review of patient oncofertility support needs in reproductive cancer patients aged 14 to 45 years of age. Psycho-oncology. 2018;27(2):401–9. [DOI] [PubMed] [Google Scholar]
- 5.Logan S, Perz J, Ussher JM, Peate M, Anazodo A. Systematic review of fertility-related psychological distress in cancer patients: informing on an improved model of care. Psycho-oncology. 2019;28(1):22–30. [DOI] [PubMed] [Google Scholar]
- 6.Breast Cancer Facts & Figures 2017–2018. American Cancer Society; 2017. [Google Scholar]
- 7.Keegan TH, Ries LA, Barr RD, Geiger AM, Dahlke DV, Pollock BH, et al. Comparison of cancer survival trends in the United States of adolescents and young adults with those in children and older adults. Cancer. 2016;122(7):1009–16. [DOI] [PubMed] [Google Scholar]
- 8.Zebrack BJ. Psychological, Social, and Behavioral Issues for Young Adults With Cancer. Cancer. 2011. May 15;117(10):2289–94. [DOI] [PubMed] [Google Scholar]
- 9.Crawshaw MA, Glaser AW, Hale JP, Sloper P. Male and female experiences of having fertility matters raised alongside a cancer diagnosis during the teenage and young adult years. Eur J Cancer Care (Engl). 2009. July;18(4):381–90. [DOI] [PubMed] [Google Scholar]
- 10.Schmidt R, Richter D, Sender A, Geue K. Motivations for having children after cancer–a systematic review of the literature. Eur J Cancer Care (Engl). 2016;25(1):6–17. [DOI] [PubMed] [Google Scholar]
- 11.Lambertini M, Peccatori FA. Fertility Preservation and Pregnancy After Breast Cancer. In: Breast Cancer in Young Women. Springer; 2020. p. 167–76. [Google Scholar]
- 12.Deshpande NA, Braun IM, Meyer FL. Impact of fertility preservation counseling and treatment on psychological outcomes among women with cancer: A systematic review. Cancer. 2015. August 11;121(22):3938–47. [DOI] [PubMed] [Google Scholar]
- 13.Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, et al. Fertility Preservation in Patients With Cancer: ASCO Clinical Practice Guideline Update. J Clin Oncol. 2018;36(19):1994–2001. [DOI] [PubMed] [Google Scholar]
- 14.Gorman JR, Bailey S, Pierce JP, Su HI. How do you feel about fertility and parenthood? The voices of young female cancer survivors. J Cancer Surviv. 2012. June;6(2):200–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gorman JR, Malcarne VL, Roesch SC, Madlensky L, Pierce JP. Depressive symptoms among young breast cancer survivors: the importance of reproductive concerns. Breast Cancer Res Treat. 2010;123(2):477–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Canada AL, Schover LR. The psychosocial impact of interrupted childbearing in long-term female cancer survivors. Psycho-Oncology. 2012;21(2):134–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Partridge AH, Gelber S, Peppercorn J, Sampson E, Knudsen K, Laufer M, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004. October 15;22(20):4174–83. [DOI] [PubMed] [Google Scholar]
- 18.HolmesRovner M, Kroll J, Schmitt N, Rovner DR, Breer ML, Rothert ML, et al. Patient satisfaction with health care decisions: The satisfaction with decision scale. Med Decis Making. 1996. January;16(1):58–64. [DOI] [PubMed] [Google Scholar]
- 19.Oconnor AM. VALIDATION OF A DECISIONAL CONFLICT SCALE. Med Decis Making. 1995. January;15(1):25–30. [DOI] [PubMed] [Google Scholar]
- 20.Young K, Shliakhtsitsava K, Natarajan L, Myers E, Dietz AC, Gorman JR, et al. Fertility counseling before cancer treatment and subsequent reproductive concerns among female adolescent and young adult cancer survivors. Cancer. 2019;125(6):980–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Letourneau JM, Ebbel EE, Katz PP, Katz A, Ai WZ, Chien AJ, et al. Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer. 2012. March 15;118(6):1710–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shah MS, Letourneau JM, Niemasik EE, Bleil M, McCulloch CE, Rosen MP. The role of in-depth reproductive health counseling in addressing reproductive health concerns in female survivors of nongynecologic cancers. J Psychosoc Oncol. 2016;34(4):305–17. [DOI] [PubMed] [Google Scholar]
- 23.De Man AM, Rashedi A, Nelen W, Anazodo A, Rademaker A, De Roo S, et al. Female fertility in the cancer setting: availability and quality of online health information. Hum Fertil. 2020;1–9. [DOI] [PubMed] [Google Scholar]
- 24.Kaplowitz MD, Hadlock TD, Levine R. A comparison of web and mail survey response rates. Public Opin Q. 2004;68(1):94–101. [Google Scholar]
- 25.Kwak N, Radler B. A comparison between mail and web surveys: Response pattern, respondent profile, and data quality. J Off Stat. 2002;18(2):257. [Google Scholar]
- 26.Brehaut JC, O’Connor AM, Wood TJ, Hack TF, Siminoff L, Gordon E, et al. Validation of a decision regret scale. Med Decis Making. 2003. July;23(4):281–92. [DOI] [PubMed] [Google Scholar]
- 27.Stalmeier PFM, Roosmalen MS, Verhoef LCG, Hoekstra-Weebers J, Oosterwijk JC, Moog U, et al. The decision evaluation scales. Patient Educ Couns. 2005. June;57(3):286–93. [DOI] [PubMed] [Google Scholar]
- 28.Barton SE, Najita JS, Ginsburg ES, Leisenring WM, Stovall M, Weathers RE, et al. Infertility, infertility treatment, and achievement of pregnancy in female survivors of childhood cancer: a report from the Childhood Cancer Survivor Study cohort. Lancet Oncol. 2013;14(9):873–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miller LE. Sources of uncertainty in cancer survivorship. J Cancer Surviv. 2012;6(4):431–40. [DOI] [PubMed] [Google Scholar]
- 30.Razzano A, Revelli A, Delle Piane L, Salvagno F, Casano S, Randaccio S, et al. Fertility preservation program before ovarotoxic oncostatic treatments: role of the psychological support in managing emotional aspects. Gynecol Endocrinol. 2014. November 1;30(11):822–4. [DOI] [PubMed] [Google Scholar]
- 31.Miaja M, Platas A, Martinez-Cannon BA. Psychological impact of alterations in sexuality, fertility, and body image in young breast cancer patients and their partners. Rev Invest Clin. 2017;69(4):204–9. [DOI] [PubMed] [Google Scholar]
- 32.Benedict C, Thom B, Friedman DN, Pottenger E, Raghunathan N, Kelvin JF. Fertility information needs and concerns post-treatment contribute to lowered quality of life among young adult female cancer survivors. Support Care Cancer. 2018. July;26(7):2209–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Logan S, Anazodo A. The psychological importance of fertility preservation counseling and support for cancer patients. Acta Obstet Gynecol Scand. 2019;98(5):583–97. [DOI] [PubMed] [Google Scholar]
- 34.Huang S, Tseng L, Lai JC, Lien P, Chen P. Oncofertility to Evidence-Based Practice: Changes in Fertility Intention and Symptom Burden in Reproductive-Age Women With Breast Cancer. Worldviews Evidence-Based Nurs. 2019;16(5):381–8. [DOI] [PubMed] [Google Scholar]
- 35.Logan S, Perz J, Ussher J, Peate M, Anazodo A. Clinician provision of oncofertility support in cancer patients of a reproductive age: A systematic review. Psycho-oncology. 2018;27(3):748–56. [DOI] [PubMed] [Google Scholar]