Abstract
Background and Objectives
More studies are needed to assess the long‐term safety profile and clinical outcomes of lasers and energy‐based devices to treat the symptoms associated with vulvovaginal atrophy. This study evaluated a series of three fractional CO2 laser treatments to the vulva and vagina with a 1‐year follow‐up in a postmenopausal population.
Study Design/Materials and Methods
In this prospective, self‐controlled, open‐label clinical study, 18 postmenopausal females with atrophic vaginitis received 3 monthly treatments to the vulva and vagina with a fractional CO2 laser system and 1‐, 3‐, 6‐, and 12‐month follow‐up. Investigators used the Vaginal Health Index (VHI) to assess changes in vaginal elasticity, fluid volume, vaginal pH, epithelial integrity, and moisture. Sexual function at each timepoint was subject‐reported, using the validated Female Sexual Function Index (FSFI).
Results
Treatment of the vulva and vagina in postmenopausal women with fractional CO2 laser resurfacing resulted in statistically significant improvements as compared with baseline at all post‐treatment and follow‐up intervals to 12 months in VHI and FSFI (P ≤ 0.003 and P ≤ 0.03, respectively). Mean total VHI score increased from a baseline of 11.8–22.8 (93.2% improved) at 6‐month follow‐up (P = 0.0002) slightly decreasing to 21.4 (81.4% improved) at 12‐month follow‐up post‐treatment (P = 0.0003). Mean FSFI Scores increased from a baseline of 17.9–26.3 (46.9% improvement) at 12‐month follow‐up post‐treatment (P ≤ 0.0048). Cohort analysis revealed restoration of normal or near‐normal (23–25) VHI following laser treatment in the recently menopausal (1–3 years) greatly exceeded that of the >3 years postmenopausal population and the difference was statistically significant (P ≤ 0.05). Normal/near‐normal VHI at 3‐, 6‐, and 12‐month post‐treatment was 88%, 88%, and 63% in the recently postmenopausal cohort, as compared with 30%, 40%, and 10% of the >3 years postmenopausal group (P ≤ 0.05). Patient satisfaction following treatment was rated as high at 94% at 12‐month follow‐up. Safety findings demonstrated no‐to‐slight discomfort in the majority of subjects and transient erythema and edema, with no adverse events associated with treatment.
Conclusion
Fractional CO2 laser treatment of the vulva and vagina resulted in statistically significant improvements in VHI and FSFI compared with baseline in postmenopausal population that were sustained to 12‐month follow‐up. Restoration of normal VHI was observed in a statistically significant greater percentage in the recently postmenopausal cohort (1–3 years) as compared with postmenopausal cohort of >3 years, suggesting that early intervention is correlated with improved outcomes. Lasers Surg. Med. © 2020 Wiley Periodicals, Inc.
Keywords: fractional CO2 laser, menopause, genitourinary, vagina, vulvovaginal atrophy, laser
BACKGROUND
At present, an accumulating body of evidence suggests safety and efficacy of laser and energy‐based devices for the treatment of women's genitourinary conditions [1, 2, 3, 4]. More clinical studies are needed to assess the long‐term safety profile and clinical outcomes of the lasers and energy‐based devices to treat the symptoms associated with vulvovaginal atrophy (VVA) [2, 3, 4]. The European Vulvovaginal Epidemiological Survey (EVES) recently determined the prevalence of VVA confirmed by gynecological assessment among all postmenopausal women as 81.3% and the prevalence of at least one VVA symptom at 92.8% [5]. The VVA diagnosis and symptom presence were dependent upon age and time since menopause, suggesting that early therapeutic intervention may be important [5].
The current study evaluated a series of three fractional CO2 laser treatments to the vagina and vulva to investigate whether study findings from another site, recently published in the literature, for 1‐year outcome in a postmenopausal population were reproducible [6]. In the course of the study, a difference in vaginal health and sexual function outcomes was observed in the recently postmenopausal versus the >3 years postmenopausal group. The results of the study and cohort analysis are reported here and contribute to our fund of knowledge on this highly prevalent genitourinary disorder affecting postmenopausal women and the potential importance of early intervention.
PATIENTS AND METHODS
The study was approved by an Institutional Review Board (Salus IRB, Protocol DHF 19731, Clinical Study of the CO2RE Laser Device Performance for Vaginal Atrophy Treatments; ClinicalTrials.gov Identifier: NCT02704741). A total of 18 subjects were enrolled and treated at a private research clinic in the United States (Dr. Alexiades) and are the basis of this clinical evaluation. All 18 patients completed a series of three fractional CO2 laser treatments and were assessed at 1‐, 3‐, 6‐, and 12‐month follow‐up after the treatment series.
Treatment Intervention
The CO2RE system is FDA‐cleared (K181523) and indicated for use in surgical applications requiring the ablation, vaporization, excision, incision, and coagulation of soft tissue in medical specialties including aesthetic surgery (dermatology and plastic surgery), podiatry, gynecology, neurosurgery, orthopedics (soft tissue), and arthroscopy (knee). The CO2RE Intima is CE‐marked for the treatment of vulvovaginal atrophy (VVA) and vaginal rejuvenation.
Device Description
The CO2RE laser system (Candela Corporation, Wayland, MA) is a second‐generation fractional carbon dioxide (CO2) system that emits light at a wavelength of 10.6 μm, which is readily absorbed by water in the tissue. The CO2 gas tube is radiofrequency (RF)‐excited and air‐cooled. The system has a programmable two‐axis scanning laser beam that allows the physician to select the density coverage from a selection of predetermined patterns, of various sizes, based on the skin area to be treated. The fractional CO2RE system has different modes for resurfacing, surgical and four different ablative treatment modes, coagulating at depths of up to 900 μm with Deep Mode [7].
Study Design
This prospective, investigational IRB‐approved study was conducted at one USA clinic, as part of a multi‐center clinical study. Study enrollment took place from June 2017 through April 2018 (ClinicalTrials.gov Identifier: NCT0270474). Study participants included postmenopausal women presenting to the clinic with symptoms of VVA (vaginal dryness, irritation, soreness, or dyspareunia associated with this condition). Study inclusion criteria included: healthy female ≥35 years of age; absence of menstruation ≥12 months; seeking treatment for vaginal atrophy; unresponsive to or dissatisfied with previous local estrogen therapy (with a washout period for the use of hormone replacement therapy, either systemic or local, within the 6 months prior to study enrollment); desire to maintain sexual activity and currently experiencing sexual activity at least once a month; normal cell cytology, PAP smear with HPV PCR; negative urinalysis and normal internal and external vaginal examination. Exclusion criteria included: prior vaginal reconstructive surgery or treatment for vaginal tightening within the past 12 months; previous laser or RF treatment within the prior 6 months; prolapse stage ≥II, according to the pelvic organ prolapse quantification (ICS‐POP‐Q) system (to exclude advanced prolapse for which first‐line treatments are invasive); acute or recurrent urinary tract infections; active genital infections; undiagnosed vaginal bleeding; anticoagulation medications or non‐steroidal anti‐inflammatory agents 1 week prior to and after the treatment course (to avoid peri‐ and post‐operative bleeding); use of hormone therapy, immunosuppressive medications or use of systemic corticosteroid therapy 6 months prior to or during the course of the study; history of heat‐induced herpes virus infection; acute or recurrent urinary tract infection or herpes virus infection; history of or active malignancy in the past 5 years; electrical implants; immunosuppressive illness; suffering from hormonal imbalance or any serious disease or chronic condition that could interfere with study compliance; lymphatic disorders; suffering from significant conditions in the treated area, inflammatory conditions, or lacerations or abrasions in the treated area; keloids or hypertrophic scarring; history of epidermal or dermal disorders including collagen vascular disease or vasculitis; use of isotretinoin in preceding 6 months; dysplastic nevi in the area; pregnant and or breastfeeding. The study protocol was approved by the Salus Institutional Review Board, and informed written consent was obtained from all study subjects.
Study Procedure
Postmenopausal women were treated to the vulva (extravaginally) and vagina (internally) with a fractional CO2 laser (CO2RE Intima; Candela Corporation, Wayland, MA). Subjects underwent a series of three‐monthly treatments, according to the study treatment protocol. A gynecological exam of the vaginal canal for evidence of active infection and of the vestibule and introitus for signs of injury or bleeding was performed prior to each treatment and at each follow‐up interval. An examination of the vulvar skin was also done to examine for characteristic color changes and signs of atrophy. Treatment to the vagina was performed using the following settings with the internal handpiece: square 7.8 × 7.8 mm pattern with Deep Mode, fractional density of 5% and energy level of 50 mJ and fluence of 283 J/cm2. The handpiece was inserted into the vagina (up to 10 cm). Mineral oil was applied for reduced friction upon insertion into the introitus. The handpiece was positioned with contact to the vagina and was rotated to apply 12 pulses at each 1‐cm marking (application of laser energy at 3–10‐cm depths). The vaginal canal was treated with a single pass. Anesthesia was not used for internal treatment to the vagina.
Vulvar (external) treatments were performed with a separate handpiece, using Deep Mode and the hexagon or square pattern. A layer (approximately 1 g) of topical 5% lidocaine anesthetic gel was applied to the labia minora and majora just prior to external treatment. Single passes were administered at energy level of 50 mJ and 5% fractional density. Subjects received three treatments at an interval of 3–4 weeks between treatment. Patients were recommended to avoid coital sexual activity and tampon use for at least 7 days after treatment.
Study Assessments
The Vaginal Health Index (VHI), a quantitative assessment of vaginal health, was performed by the investigator to assess changes in vaginal elasticity, fluid volume, vaginal pH level, epithelial integrity, and moisture after treatment and at follow‐ups (1, 3, 6, and 12 months) after the final treatment compared with baseline. The VHI scale ranges from 5 (severe) to 25 (normal) across all five parameters [8].
The Female Sexual Functional Index (FSFI) questionnaire, a 19‐item questionnaire developed as a brief, multidimensional, self‐reported instrument for assessing the key dimensions of sexual function in women was completed by the subjects at baseline and at follow‐up [9].
A visual analog scale from 0 (no pain) to 10 (worst possible pain) was used to measure discomfort associated with probe insertion, probe rotation/retraction, and laser application.
RESULTS
Baseline Characteristics
Demographics and VHI parameters at baseline are summarized in Tables 1 and 2. Mean age was 54 ± 7 years with a range of 44–64 years. Most of the subjects were Caucasian (n = 16, 89%). The majority had Fitzpatrick skin type I or II (n = 15, 83%). The VHI at baseline was 11.8 ± 3.55 (range 7–20). Eighteen postmenopausal females (mean age, 53 ± 7 years; range, 40–64 years) were enrolled and treated. Ten subjects were postmenopausal >3 years (range 3–16 years) and eight subjects postmenopausal <3 years.
Table 1.
Demographic Characteristics: The Prevalence of Characteristics of the Study Population, Including Race and Skin Type, Are Listed
| Number | Percent | |
|---|---|---|
| Number of subjects | 18 | 100 |
| Race | ||
| American Indian or Alaska Native | 1 | 6 |
| Middle culture | 1 | 6 |
| Caucasian (white) | 16 | 89 |
| Skin type | ||
| ST I | 7 | 39 |
| ST II | 8 | 44 |
| ST III | 1 | 6 |
| ST IV | 2 | 11 |
| ST V | 0 | 0 |
| ST VI | 0 | 0 |
Table 2.
VHI Parameters at Baseline: Baseline Data Including Age, Weight and VHI Parameters For the Study Population Are Listed
| Age (years) | Weight (kg) | Vaginal elasticity | Vaginal fluid volume (pooling of secretions) | Vaginal pH level | Vaginal epithelial integrity | Vaginal moisture (coating) | Total VHI | |
|---|---|---|---|---|---|---|---|---|
| Mean | 54 | 58 | 2.44 | 2.28 | 1.67 | 2.78 | 2.67 | 11.83 |
| SD | 7 | 5 | 0.78 | 1.02 | 0.84 | 1.00 | 1.08 | 3.55 |
| Variance | 44 | 24 | 0.61 | 1.04 | 0.71 | 1.01 | 1.18 | 12.62 |
| Minimum | 44 | 48 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 7.00 |
| Maximum | 64 | 64 | 4.00 | 5.00 | 4.00 | 4.00 | 5.00 | 20.00 |
| N | 18 | 18 | 18 | 18 | 18 | 18 | 18 | 18 |
SD, standard deviation; VHI, Vaginal Health Index.
Treatment Findings
All 18 subjects underwent three treatments with fractional CO2 laser using both the internal handpiece for the vagina (internal procedure) and the standard fractional handpiece for the vulva (external procedure). A total of 54 sessions were conducted. The mean duration was 6 minutes for internal treatment and 7 minutes for external treatment.
Safety Findings
A total of 54 treatments were performed. Self‐reported VAS pain scores were recorded on a scale of 0 = no pain to 10 = worst possible pain. The mean reported discomfort/pain levels were 1.9 ± 2.0 (probe insertion), 1.7 ± 2.2 (probe movement), and 1.2 ± 1.7 (laser application) (Table 3). Most of the subjects reported on none to minimal discomfort for probe insertion (65%), probe movement (74%), and laser application (80%) (Fig. 1).
Table 3.
Discomfort/Pain Level During Treatment: The VAS Scores for Probe Insertion, Probe Movement and Laser Application Were Recorded for Each Subject and Data Presented
| Probe insertion level NSR | Probe movement level NSR | Laser application‐level NSR | |
|---|---|---|---|
| Mean | 1.9 | 1.7 | 1.2 |
| SD | 2.0 | 2.2 | 1.7 |
| Variance | 4.0 | 4.9 | 3.0 |
| Minimum | 0 | 0 | 0 |
| Maximum | 7.0 | 9.0 | 8.0 |
| N | 54 | 54 | 54 |
SD, standard deviation; VAS, visual analog scale.
Fig. 1.
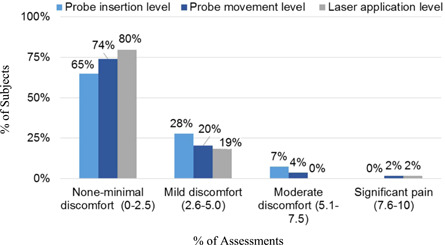
Percentage of subjects with discomfort/pain during treatment: the distribution of percentage of subjects with none‐minimal, mild, moderate and significant pain scores are presented for probe insertion, probe movement, and laser application.
Immediate treatment responses were limited to transient and mild erythema visible at the introitus and vulva, which were present following 67% and 30% of the treatment sessions, respectively, and resolved without any intervention by the 1‐week safety evaluation. No adverse events related to the treatment were observed during the study course. There were no treatment complications observed.
Investigator Measured (VHI) Findings
Point VHI improvement
VHI was assessed at each study visit, which includes quantitative measurements such as pH. All subjects showed improvement after a single treatment, with an average VHI improvement of 5.9 ± 3.3 points (range 2–15) (Table 4 and Figs. 2 and 3). Average improvement in vaginal health increased with successive treatments to 11.0 ± 3.0 points’ improvement at the 6‐month follow‐up. Improvement was maintained through the 12‐month follow‐up with a slight decrease between the 6‐ and 12‐month follow‐ups (Table 4 and Fig. 2).
Table 4.
Point Improvement in Vaginal Health Index From Baseline in Total Postmenopausal Subject Population
| Post Tx.1 | Post Tx.2 | 1 m FU | 3 m FU | 6 m FU | 12 m FU | |
|---|---|---|---|---|---|---|
| Mean | 5.9 | 8.6 | 10.3 | 10.7 | 11.0 | 9.6 |
| SD | 3.3 | 3.5 | 3.0 | 3.1 | 3.0 | 3.3 |
| Variance | 10.8 | 12.1 | 8.8 | 9.4 | 8.8 | 11.1 |
| Minimum | 2 | 4 | 5 | 3 | 4 | 0 |
| Maximum | 15 | 15 | 15 | 15 | 15 | 13 |
| N | 18 | 18 | 18 | 18 | 18 | 18 |
| P value* | 0.0002 | 0.0002 | 0.0002 | 0.0002 | 0.0002 | 0.0003 |
SD, standard deviation.
Wilcoxon signed‐rank test for single group median.
Fig. 2.
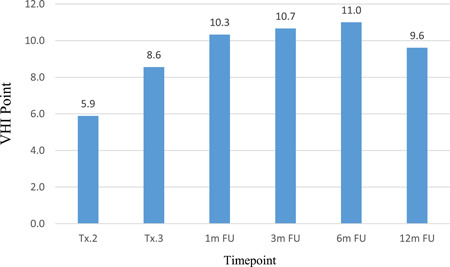
Point Improvement in Vaginal Health Index (VHI) from baseline in postmenopausal subject population*: the mean point improvement in VHI over baseline is presented in the treated subject population for each follow‐up timepoint (see Table 4). All point improvements were statistically significant, *P < 0.0003.
Fig. 3.
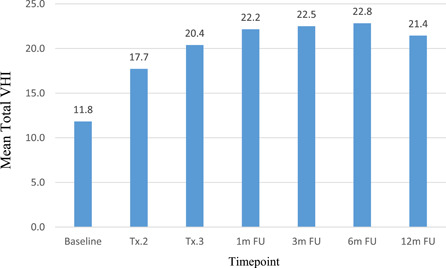
Average Total Vaginal Health Index (VHI) score by visit in postmenopausal subject population: the mean total VHI for the entire postmenopausal study population at baseline, following each treatment and at the 1‐, 3‐, 6‐, and 12‐month follow‐up timepoints is shown (see Table 4).
Mean total VHI scores
All 18 patients showed a statistically significant improvement in the VHI score (P ≤ 0.0003) at each post‐treatment timepoint and at 3‐, 6‐, and 12‐month follow‐up intervals, with mean VHI scores of 22.5, 22.8, and 21.4, respectively, as compared with baseline mean VHI score of 11.8 (P ≤ 0.0003) (Fig. 3). All 18 patients showed a statistically significant improvement in the VHI score at the 3‐, 6‐, and 12‐month follow‐up with mean scores of 22.5 (range 19–25), 22.8 (range 19–25), and 21.4 (range 17–25), respectively, as compared with baseline mean of 11.8 (range 7–20). Sustained VHI outcomes to 12‐month follow‐up in both cohorts with a slight decrease in VHI scores between the 6‐ and 12‐month follow‐up timepoints (Fig. 3). Mean total VHI score was 11.8 at baseline and following treatment increased to 22.8 (93.2% improved) at the 6‐month follow‐up (P = 0.0002) with a slight decrease to 21.4 (81.4% improved) at 12‐month follow‐up (P = 0.0003).
VHI parameters
High percentages of subjects showed improvement in each of the five parameters comprising the VHI score at each study visit (Table 5). Most subjects experienced improvement in elasticity, pH, and other VHI parameters (ranging from 78% for moisture to 100% for epithelial integrity) sustained to 12 months after treatment. VHI parameters improved with each treatment, with restoration of pH in the normal range in the majority and improvement in epithelial integrity improved in all 18 subjects after two treatments which remained improved for all subjects throughout the follow‐up phase (Table 5).
Table 5.
Percentage Subjects With Improvement in Vaginal Health Index Parameters Versus Baseline
| Tx.2 | Tx.3 | 1 m FU | 3 m FU | 6 m FU | 12 m FU | |
|---|---|---|---|---|---|---|
| (n = 18) (%) | (n = 18) (%) | (n = 18) (%) | (n = 18) (%) | (n = 18) (%) | (n = 18) (%) | |
| Elasticity | 94 | 94 | 100 | 89 | 89 | 89 |
| Fluid volume | 89 | 94 | 94 | 94 | 94 | 94 |
| Vaginal pH level | 78 | 83 | 94 | 94 | 100 | 83 |
| Epithelial integrity | 83 | 100 | 100 | 100 | 100 | 100 |
| Moisture (coating) | 78 | 89 | 94 | 94 | 89 | 78 |
Cohort Analysis: VHI of Recently Postmenopausal (1–3 Years) Versus Postmenopausal >3 Years
Mean total VHI scores
Study subjects enrolled were postmenopausal for a range of 1–13 years at baseline prior to treatment. Ten (56%) of the 18 subjects were postmenopausal for greater than 3 years (>3 years menopausal cohort) with a range of up to 13 years, while eight subjects (44%) were postmenopausal for 1–3 years (recently menopausal cohort).
At baseline, mean total VHI score was 14.3 for the recently postmenopausal cohort as compared to 9.9 for the >3 years postmenopausal cohort (P = 0.008). Average total VHI score was significantly different between the two study cohorts at baseline and remained significantly different until the 6‐ and 12‐month follow‐ups when the differences were no longer significant between the two groups (Table 6).
Table 6.
VHI Score by Visit for Recently Menopausal (1–3 Years) and >3 Years Menopausal Cohorts
| Baseline | Tx.2 | Tx.3 | 1 m FU | 3 m FU | 6 m FU | 12 m FU | |
|---|---|---|---|---|---|---|---|
| Recently menopausal (1–3 years) | |||||||
| Mean | 14.3 | 21.3 | 23.0 | 24.1 | 23.5 | 23.6 | 22.6 |
| SD | 3.5 | 3.8 | 3.1 | 1.7 | 2.0 | 1.6 | 2.3 |
| Minimum | 10 | 15 | 16 | 20 | 19 | 20 | 19 |
| Maximum | 20 | 25 | 25 | 25 | 25 | 25 | 25 |
| N | 8 | 8 | 8 | 8 | 8 | 8 | 8 |
| Menopausal >3 years | |||||||
| Mean | 9.9 | 14.9 | 18.3 | 20.6 | 21.7 | 22.2 | 20.5 |
| SD | 2.2 | 3.1 | 3.4 | 3.3 | 1.7 | 1.7 | 2.2 |
| Minimum | 7 | 11 | 13 | 15 | 19 | 19 | 17 |
| Maximum | 14 | 21 | 24 | 25 | 24 | 25 | 25 |
| N | 10 | 10 | 10 | 10 | 10 | 10 | 10 |
| P value* | 0.008 | 0.004 | 0.014 | 0.012 | 0.034 | 0.057 | 0.105 |
SD, standard deviation; VHI, Vaginal Health Index.
Wilcoxon rank‐sum test (Mann–Whitney U test) for unpaired data.
In each cohort, the mean VHI score increased following each treatment and was sustained to the 6‐month follow‐up with slight decrease between the 6‐ and 12‐month intervals (Fig. 4). The mean total VHI scores following treatment were higher for the recently postmenopausal cohort as compared to the >3‐year postmenopausal cohort (Fig. 4). For the recently postmenopausal cohort, the total VHI score increased from a baseline of 14 to an average of 23–25 following the second treatment and throughout the follow‐up period. For the >3 years postmenopausal cohort, the VHI score increased from an average baseline score of 10 to an average of 18–22 before declining at the 12‐month follow‐up (Fig. 4).
Fig. 4.
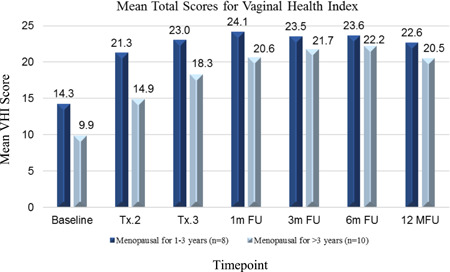
Mean total Vaginal Health Index (VHI) by menopausal status cohort: the mean total VHI for the early postmenopausal and >3 years postmenopausal cohorts are presented at baseline, following treatment, and at each follow‐up timepoint (see Table 6). Differences between cohorts statistically significant through 3‐month follow‐up, *P < 0.05.
Restoration of normal/near‐normal VHI scores
The restoration of normal or near‐normal VHI (score of 23–25) was observed in a statistically significant greater percentage in the recently postmenopausal cohort (1–3 years) as compared with postmenopausal cohort of >3 years following the first two treatments and at 1‐, 3‐, and 12‐month follow‐up timepoints (P ≤ 0.05) (Fig. 5). Comparison of the two cohorts, 88% of recently postmenopausal attained normal or near‐normal VHI at 3 and 6 months and 63% maintained this level to 12 months follow‐up, as compared with a maximum of 40% of the >3 years postmenopausal group at 6 months that diminished to 10% by the 12‐month interval (Fig. 5 and Table 7).
Fig. 5.
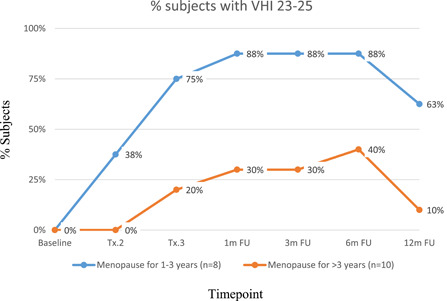
Percentage (%) of subjects with normal or near‐normal Vaginal Health Index (VHI) score of 23–25 at each timepoint: the percentage of subjects with normal or near‐normal VHI scores (23–25) in the recently postmenopausal and >3 years postmenopausal cohorts at baseline, following treatment and at the 1‐, 3‐, 6‐, and 12‐month follow‐up timepoints are shown (see Table 7). Differences statistically significant at treatment 3, and 1‐, 3‐, and 12‐month follow‐up, *P < 0.05.
Table 7.
Percentage of Subjects With Normal or Near‐Normal Vaginal Health Index (VHI) (23–25) at Each Timepoint
| % Subjects with normal or near‐normal VHI (23–25) | |||||||
|---|---|---|---|---|---|---|---|
| Baseline | Tx.2 | Tx.3 | 1 m FU | 3 m FU | 6 m FU | 12 m FU | |
| Menopause for 1–3 years (n = 8) | 0% | 38% | 75% | 88% | 88% | 88% | 63% |
| Menopause for >3 years (n = 10) | 0% | 0% | 20% | 30% | 30% | 40% | 10% |
| P value (Fisher's exact test) | 0.07 | 0.05 | 0.02 | 0.02 | 0.07 | 0.04 | |
FSFI
The aggregated FSFI score is a sum of weighted answers for each of the 19 items in the questionnaire, with a maximum score 36.0 (high level of sexual functional) and minimum score of 2.0 (low level of sexual functional). At baseline, average FSFI for the 18 subjects was 17.9 ± 9.2 (range 2.0–32.0). Improvements in total FSFI scores were statistically significant compared with baseline after each treatment and at each follow‐up timepoint (Fig. 6 and Table 8). Following the first treatment, 78% (14/18) of subjects experienced improvement with a mean of 2.7 points’ improvement (Fig. 7 and Table 9). At the 3‐month follow‐up, the improvement rate increased to 89% (16/18) with a mean improvement level of 8.2 points. The rate of improvement remained stable (89%, 16/18) at the 12‐month follow‐up with mean improvement of 8.3 points. Although the rate was the same, comparing scores by subject revealed that two subjects who did not experience improvement at the 3‐month follow‐up did experience improvement at the 12‐month follow‐up, while another two subjects experienced a decline. The remaining 14 subjects experienced relatively stable scores at the 12‐month follow‐up (Figs. 6, 7 and Tables 8, 9).
Fig. 6.
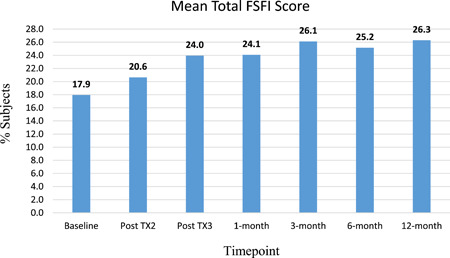
Mean Female Sexual Functional Index (FSFI) at baseline and following fractional CO2 laser treatment: the mean FSFI scores at baseline, following treatment and at 1‐, 3‐, 6‐, and 12‐month follow‐up timepoints are shown for the postmenopausal study population (see Table 8). FSFI improvements statistically significant post TX3 through 12‐month follow‐up, *P < 0.05.
Table 8.
Mean FSFI at Baseline and Following Fractional CO2 Laser Treatment
| Total FSFI scores | Baseline | Post TX2 | Post TX3 | 1‐month | 3‐month | 6‐month | 12‐month |
|---|---|---|---|---|---|---|---|
| Mean | 17.9 | 20.6 | 24.0 | 24.1 | 26.1 | 25.2 | 26.3 |
| SEM | 2.2 | 2.6 | 2.3 | 2.4 | 1.9 | 2.3 | 1.9 |
| SD | 9.2 | 10.9 | 9.8 | 10.1 | 8.2 | 9.8 | 8.2 |
| Variance | 84.8 | 118.9 | 96.9 | 102.3 | 67.0 | 97.0 | 66.7 |
| Coef. Var. | 0.5 | 0.5 | 0.4 | 0.4 | 0.3 | 0.4 | 0.3 |
| Minimum | 2 | 3.2 | 3.2 | 2 | 5.8 | 4.4 | 2.9 |
| Maximum | 32 | 32.9 | 33.6 | 34.8 | 34.5 | 35.4 | 34.8 |
| Sum | 323 | 371.5 | 431.1 | 433.3 | 470.2 | 452.8 | 473.2 |
| N | 18 | 18 | 18 | 18 | 18 | 18 | 18 |
| P value* | NA | 0.1635 | 0.0233 | 0.0256 | 0.0018 | 0.0082 | 0.0048 |
FSFI, Female Sexual Functional Index; SD, standard deviation; SEM, standard error of the mean.
Wilcoxon rank‐sum test (Mann–Whitney U test) for unpaired data.
Fig. 7.
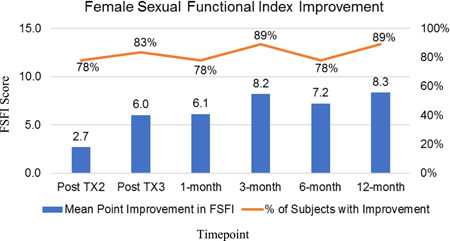
Point improvement in Female Sexual Functional Index (FSFI): the point improvement in FSFI scores at baseline, following treatment and at 1‐, 3‐, 6‐, and 12‐month follow‐up timepoints are shown for the postmenopausal study population. The orange graph indicates the percentage of subjects with a point‐improvement FSFI response at each timepoint (see Tables 8 and 9). FSFI point improvements statistically significant post TX3 through 12‐month follow‐up, *P < 0.03.
Table 9.
Point Improvement in FSFI
| Mean point improvement in FSFI | Post TX2 | Post TX3 | 1‐month | 3‐month | 6‐month | 12‐month |
|---|---|---|---|---|---|---|
| Mean | 2.7 | 6.0 | 6.1 | 8.2 | 7.2 | 8.3 |
| SEM | 2.4 | 2.3 | 2.4 | 2.2 | 2.3 | 2.1 |
| SD | 10.2 | 9.9 | 10.1 | 9.3 | 9.8 | 8.9 |
| Variance | 103.8 | 99.6 | 102.6 | 86.1 | 95.2 | 79.2 |
| Coef. Var. | 3.8 | 1.7 | 1.6 | 1.1 | 1.3 | 1.1 |
| Minimum | −19.4 | −17.6 | −18.8 | −10.7 | −10.9 | −3.5 |
| Maximum | 27.2 | 28.1 | 24.9 | 28.1 | 30.2 | 29.6 |
| Sum | 48.5 | 108.1 | 110.3 | 147.2 | 129.8 | 150.2 |
| N | 18 | 18 | 18 | 18 | 18 | 18 |
| Post TX2 | Post TX3 | 1‐month | 3‐month | 6‐month | 12‐month | |
| Mean point improvement in FSFI | 2.7 | 6.0 | 6.1 | 8.2 | 7.2 | 8.3 |
| % of subjects with Improvement | 78% | 83% | 78% | 89% | 78% | 89% |
FSFI, Female Sexual Functional Index; SD, standard deviation; SEM, standard error of the mean.
Cohort Analysis: FSFI Improvement for Recently Menopausal (1–3 Years) Versus Menopausal >3 Years
Mean FSFI scores increased in both cohorts following each treatment and continued to demonstrate sustained improvement during the follow‐up interval. Mean total FSFI scores at baseline were 22.4 for the recently menopausal cohort as compared with 14.4 for the >3‐year postmenopausal cohort, though the difference did not reach statistical significance (P = 0.056) (Table 10). At the 12‐month timepoint, the mean FSFI was 27.5 for the recently menopausal and 25.3 for the >3 year postmenopausal. The differences in FSFI following each treatment and at each follow‐up timepoint as compared to baseline were statistically significant within each cohort (Table 10).
Table 10.
FSFI Score by Visit for Recently Menopausal (1–3 years) and >3 years Menopausal Cohorts
| Baseline | Tx.2 | Tx.3 | 1 m FU | 3 m FU | 6 m FU | 12 m FU | |
|---|---|---|---|---|---|---|---|
| Recently menopausal (1–3 years) | |||||||
| Mean | 22.4 | 23.8 | 22.6 | 23.2 | 26.7 | 24.4 | 27.5 |
| SD | 8.1 | 12.5 | 12.7 | 13.4 | 9.1 | 11.1 | 6.6 |
| Minimum | 7 | 3.2 | 3.2 | 2 | 5.8 | 5.6 | 17.2 |
| Maximum | 32 | 32.9 | 33.6 | 34.8 | 33.3 | 34.2 | 34.8 |
| N | 8 | 8 | 8 | 8 | 8 | 8 | 8 |
| Menopausal >3 years | |||||||
| Mean | 14.4 | 18.1 | 25.1 | 24.8 | 25.7 | 25.8 | 25.3 |
| SD | 8.8 | 9.3 | 7.3 | 7.2 | 7.8 | 9.3 | 9.5 |
| Minimum | 2 | 3.8 | 10.8 | 11.1 | 8.2 | 4.4 | 2.9 |
| Maximum | 26.2 | 32.4 | 33.3 | 34.1 | 34.5 | 35.4 | 34.8 |
| N | 10 | 10 | 10 | 10 | 10 | 10 | 10 |
| P value* | 0.056 | 0.197 | 0.824 | 0.564 | 0.624 | 1.00 | 0.657 |
FSFI, Female Sexual Functional Index; SD, standard deviation; SEM, standard error of the mean.
Wilcoxon rank‐sum test (Mann–Whitney U test) for unpaired data.
While the FSFI scores were higher at baseline and during the treatment phase for the recently postmenopausal cohort, the difference between the two cohorts did not attain statistical significance at baseline or during the trial. FSFI improvements were greater for the menopausal >3 years group, but did not attain statistically significance at follow‐up intervals (Table 10 and Fig. 8).
Fig. 8.
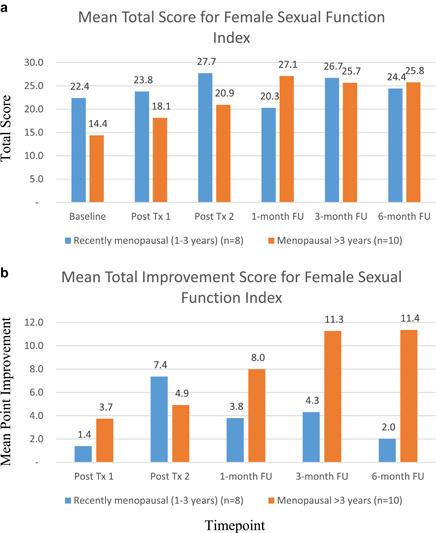
Mean Female Sexual Function Index (FSFI) by menopausal status cohort: the mean (A) and point improvement (B) FSFI scores for the recently postmenopausal and >3 years postmenopausal cohorts at baseline, following treatment and at 1‐, 3‐, 6‐, and 12‐month follow‐up timepoints are shown (see Table 10).
Subject Satisfaction Assessments
Subjects rated their satisfaction with treatment using a 5‐point Likert scale (−2 = Very unsatisfied; −1 = Unsatisfied; 0 = Uncertain; 1 = Satisfied; 2 = Very satisfied) at each of the follow‐up visits. At the 1‐, 3‐, and 12‐month follow‐ups, 94% (17 subjects) reported satisfaction (satisfied or very satisfied) with treatment outcome, while one subject was “neutral” (Table 11). At the 6‐month follow‐up, most subjects (86%, 16/18) were satisfied with treatment outcome, while one subject (7%) had no opinion (“neutral”) and one subject (7%) was unsatisfied (Table 11A). Cohort analysis revealed similar high satisfaction rates and no statistically significant difference detected between the recently (<3 years) postmenopausal versus >3 years postmenopausal duration (Table 11B and Fig. 10).
Table 11.
Subject Satisfaction Distribution by Visit: Subjects Rated Their Satisfaction With Treatment Using a 5‐Point Likert Scale (−2 = Very Unsatisfied; −1 = Unsatisfied; 0 = Uncertain; 1 = Satisfied; 2 = Very Satisfied) at Each of the Follow‐Up Visits
| A. Satisfaction total subject population | |||||
| 1 m FU (n = 18) | 3 m FU (n = 18) | 6 m FU (n = 18) | 12 m FU (n = 18) | ||
| Unsatisfied | 0% | 0% | 6% | 0% | |
| Neutral | 6% | 6% | 11% | 6% | |
| Satisfied | 94% | 94% | 83% | 94% | |
| B. Subject satisfaction by the 2 cohorts (>3 years menopausal vs. ≤3 years): | ||||||||
| Both cohorts had similar high satisfaction rates (no significant difference—see P‐values below): | ||||||||
| Menopausal > 3 years (n = 10) | Recently menopausal (1‐3 years) (n = 8) | |||||||
| 1‐month FU | 3‐month FU | 6‐month FU | 12‐month FU | 1‐month FU | 3‐month FU | 6‐month FU | 12‐month FU | |
| Very dissatisfied | 0% | 0% | 10% | 0% | 0% | 0% | 0% | 0% |
| Dissatisfied | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% |
| Uncertain | 0% | 10% | 10% | 10% | 13% | 0% | 13% | 0% |
| Very satisfied | 40% | 20% | 30% | 20% | 13% | 38% | 38% | 50% |
| Satisfied | 60% | 70% | 50% | 70% | 75% | 63% | 50% | 50% |
| % satisfied | 100% | 90% | 80% | 90% | 88% | 100% | 88% | 100% |
| Satisfaction rate | 1‐month FU | 3‐month FU | 6‐month FU | 12‐month FU |
| Menopausal >3 years (n = 10) | 100% | 90% | 80% | 90% |
| Recently menopausal (1–3 years) (n = 8) | 88% | 100% | 88% | 100% |
| P value (Fisher's exact test) | 0.4444 | 1.0000 | 1.0000 | 1.0000 |
Fig. 10.
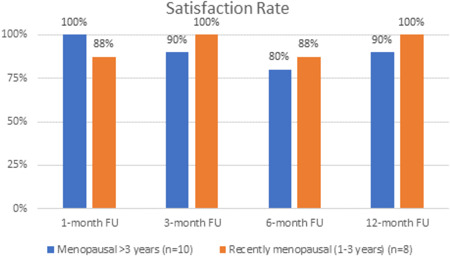
Subject satisfaction rate per cohort.
Comparison to Published Clinical Study
Similar improvement in VHI score over baseline was observed in previously published findings in a study cohort of 40 postmenopausal subjects at an alternate clinical site employing the same protocol. Average baseline VHI of 11.8 ± 3.6 (range, 7–20) and 11.3 ± 3.2 (range, 5–18) for 18‐patient study and 40‐patient study, respectively. Similar improvements in mean VHI were observed at each post‐treatment and follow‐up intervals between the two studies (Fig. 9).
Fig. 9.
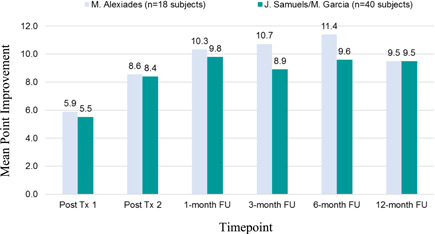
Comparison of mean Vaginal Health Index (VHI)‐point improvement to recently published results [6]: the current study is one of a multi‐center clinical trial evaluating the safety and efficacy of three fractional CO2 laser treatments on vulvovaginal atrophy. A comparison of the mean VHI point improvements between clinical sites are shown.
DISCUSSION
Fractional CO2 laser treatment of the vulva and vagina in a postmenopausal population resulted in statistically significant improvements in VHI and FSFI post‐treatment and at all follow‐up intervals to 12 months (P ≤ 0.003 and P ≤ 0.03, respectively). Mean total VHI score across the study population was 11.8 at baseline and following treatment increased to 22.8 (93.2% improved) at the 6‐month follow‐up (P = 0.0002) with a slight decrease to 21.4 (81.4% improved) at 12‐month follow‐up (P = 0.0003). Mean FSFI Scores also increased from a baseline of 17.9–26.3 (46.9% improvement) at 12‐month follow‐up post‐treatment (P ≤ 0.0048). Though improvements in VHI decreased slightly between the 6‐ and 12‐month follow‐up intervals, FSFI improvements were sustained. Patient satisfaction was reported as high at 94% at the 12‐month follow‐up. Safety findings demonstrated no to slight discomfort in the majority of subjects and transient erythema and edema post‐treatment, with no adverse events associated with treatment.
During the course of the clinical trial, it was discovered that the recently postmenopausal subjects attained normal or near‐normal VHI at a higher rate than those >3 years postmenopausal, prompting the performance of a cohort analysis. Restoration of normal or near‐normal (23–25) VHI following treatment occurred in a statistically significant greater percentage of the recently postmenopausal cohort (1–3 years) as compared with postmenopausal cohort of >3 years, suggesting that early intervention is correlated with optimal outcomes (P ≤ 0.05). The difference between the two cohorts was large: 88% of recently postmenopausal attained normal or near‐normal VHI at 3 and 6 months and 63% maintained this level to 12 months follow‐up, as compared with a maximum of 40% of the >3 years postmenopausal group at 6 months that diminished to 10% by the 12‐month interval (P ≤ 0.05; Fig. 5 and Table 7). The difference in attainment of normal/near‐normal VHI may be explained in part by differences in mean baseline VHI scores. The recently postmenopausal cohort had a baseline VHI of 14 which rose to 23–25 following the second treatment and throughout the follow‐up period; in contrast, the >3 years postmenopausal cohort had a baseline of 10 that rose to 18–22 before declining at 12 months. Early intervention with fractional CO2 laser vulvovaginal treatment may have restored normal/near‐normal VHI due to the fact that the baseline VHI of the recently menopausal cohort was of lesser severity, requiring fewer treatments to attain normal or near‐normal scores. The initial response rate between the two cohorts was similar, as the rate of VHI increase following the first treatment was 49.12% and 50.51% for the recently and the >3 years postmenopausal cohorts, respectively; however, the response rate decreased with each successive treatment as VHI approached normalcy. It is possible that additional treatments in the >3 years postmenopausal population would continue to improve VHI scores towards the normal/near‐normal range and this will require further study.
Early intervention in menopause resulting in improved outcomes has support from the gynecologic published literature. The Kronos Early Estrogen Prevention Study (KEEPS) has demonstrated that treatment of recently postmenopausal women improved sexual function [10]. In another published report from KEEPS, recently menopausal women had similar and substantial reductions in hot flashes and night sweats with lower than conventional doses of oral or transdermal estrogen [11]. These reductions were sustained over 4 years [11]. An 80‐subject study of non‐ablative fractional laser resurfacing of vagina and vulva observed that the two subjects who demonstrated inferior outcomes were of advanced age (76 and 79 years old) and two others had experienced early (<40 years of age) menopause, suggesting that there may be a finite window of opportunity for optimizing outcomes [12]. A study of fractional Er:YAG laser treatment of stress urinary incontinence (SUI) in a postmenopausal population demonstrated that an age‐dependent impact on SUI severity and efficacy of treatment [13]. Predictive modeling was tested and showed SUI improvement following treatment for subjects 47.5 years or younger [13]. A study comparing surgically‐induced versus physiologic menopause showed a greater improvement from fractional CO2 laser treatment of VVA symptoms in the former group which had a mean age of 5 years younger, once again suggesting that the difference in efficacy may be due to proximity to menopause [14]. The current report is the first of which we are aware that directly demonstrates a statistically significant difference in attainment of normal or near‐normal VHI in a recently postmenopausal cohort (1–3 years) as compared with postmenopausal cohort of >3 years. The findings presented here indicate that there is a critical window of opportunity in the recently postmenopausal timeframe to treat in order to restore normal or near‐normal vaginal health.
The current findings reproduce the long‐term follow‐up reported following vaginal and vulvar treatment with fractional CO2 laser from other clinical trials, demonstrating long‐term improvements in VHI and FSFI to 12‐month follow‐up. Our findings are compared with those of another group utilizing the same protocol, demonstrating that the outcomes are reproducible (Fig. 9) [6]. Athanasiou et al. [15] also reported sustained improvements in FSFI and VVA symptoms to 12‐month follow‐up following three‐to‐five treatments with fractional CO2 laser. In that study, increasing treatment numbers from three to four or five yielded additional improvements in symptoms and signs of genitourinary syndrome of menopause [15]. The current fractional CO2 laser and treatment protocol has also been reported to yield improvements in SUI [16].
The difference reported here in the efficacy of fractional CO2 laser treatment in signs and symptoms of vulvovaginal atrophy (VHI) between the two groups based upon menopausal duration may be explained by differences in baseline severity and/or differences in response rate. One possible explanation for the findings presented here is that observation that the baseline VHI is greater for the recently (<3 years) postmenopausal group. Therefore, assuming a similar response rate, attainment of normal or near‐normal VHI would be expected to occur in the recently postmenopausal cohort in fewer treatments. An alternative explanation is that the response rate to treatment diminishes with increased postmenopausal duration. This may be possibly due to the size, density, or responsivity of the target cell population, such as the fibroblast and vascular endothelial populations, in the lamina propria. It is possible that there is greater response to these target cells in the early stages of menopause, but that this population may dwindle as menopause progresses. These data suggest but do not demonstrate definitively that there may be a critical window period where intervention will achieve normalcy in VHI. In contrast, while fractional CO2 laser treatment was shown to improve female sexual function by the FSFI scale, a statistically significant difference in FSFI between the two cohorts was not detected. These findings suggest that the postmenopausal duration had less of an adverse impact on the therapeutic efficacy of fractional CO2 laser treatment of female sexual function as compared to vulvovaginal atrophy.
CONCLUSIONS
Fractional CO2 laser treatment resulted in improvements in mean scores and point improvements of vulvovaginal health using validated and objective scales were statistically significant and sustained to 12‐month follow‐up. The findings reported here demonstrated that postmenopausal duration has an impact on the efficacy of fractional CO2 laser treatment of the vulva and vagina for restoration of normal or near‐normal genitourinary health and that early intervention improves outcomes. These findings need to be reproduced, but offer insight into a potentially critical therapeutic window for this highly prevalent genitourinary disorder among postmenopausal women.
ACKNOWLEDGMENT
Thank you to Doran Rozen, Sarvar Kothavala, Shlomit Mann and Konika Patel for their invaluable assistance with this study.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
REFERENCES
- 1. Tadir Y, Gaspar A, Lev‐Sagie A, et al. Light and energy‐based therapeutics for genitourinary syndrome of menopause: Consensus and controversies. Lasers Surg Med 2017;49(2):137–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tadir Y, Iglesia C, Alexiades M, Davila GW, Guerette N, Gaspar A. Energy‐based treatment for gynecologic conditions including genitourinary syndrome of menopause: Consensus, controversies, recommendations, and FDA clearance. Lasers Surg Med 2019;15:315–317. [DOI] [PubMed] [Google Scholar]
- 3. Alexiades M. Lasers and energy‐based devices for Women's Genitourinary Health: Scientific and clinical evidence and FDA clearance. J Drugs Dermatol 2018;17(11):1155. [PubMed] [Google Scholar]
- 4. Alexiades M. Device‐based treatment for vaginal wellness. Semin Cutan Med Surg 2018;37(4):226–232. 10.12788/j.sder.2018.052 [DOI] [PubMed] [Google Scholar]
- 5. Palacios S, Nappi RE, Bruyniks N, Particco M, Panay N, EVES Study Investigators . The European Vulvovaginal Epidemiological Survey (EVES): Prevalence, symptoms and impact of vulvovaginal atrophy of menopause. Climacteric 2018;21(3):286–291. 10.1080/13697137.2018.1446930 [DOI] [PubMed] [Google Scholar]
- 6. Samuels JB, Garcia MA. Treatment to external labia and vaginal canal with CO2 laser for symptoms of vulvovaginal atrophy in postmenopausal women. Aesthet Surg J 2019;39(1):83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hurliman E, Zelickson B, Kenkel J. n‐Vivo histological analysis of a fractional CO2 laser system intended for treatment of soft tissue. J Drugs Dermatol 2017;16(11):1085–1090. [PubMed] [Google Scholar]
- 8. Bachmann G. Urogenital ageing: An old problem newly recognized. Maturitas 1995;22(Suppl. 1):S1–S5. [DOI] [PubMed] [Google Scholar]
- 9. Rosen R, Brown C, Heiman J, Leib S. The Female Sexual Function Index (FSFI): A multidimensional self‐report instrument for the assessment of female sexual function. J Sex Marital Ther 2000;26:191–208. [DOI] [PubMed] [Google Scholar]
- 10. Taylor HS, Tal A, Pal L, et al. Effects of oral vs transdermal estrogen therapy on sexual function in early postmenopause: Ancillary study of the Kronos Early Estrogen Prevention Study (KEEPS). JAMA Intern Med 2017;177(10):1471–1479. 10.1001/jamainternmed.2017.3877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Santoro N, Allshouse A, Neal‐Perry G, et al. Longitudinal changes in menopausal symptoms comparing women randomized to low‐dose oral conjugated estrogens or transdermal estradiol plus micronized progesterone versus placebo: The Kronos Early Estrogen Prevention Study. Menopause 2017;24(3):238–246. 10.1097/GME.0000000000000756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dodero D, Frascani F, Angelucci M, et al. Histological modifications of postmenopausal vaginal mucosa after regenerative solid state laser treatment: A multicenter study. Int J Womens Health Wellness 2019;5:099. 10.23937/2474-1353/1510099 [DOI] [Google Scholar]
- 13. Fistonic N, Fistonic I, Lukanovic A, Gustek S, Turina SB, Franic D. First assessmentof short‐term efficacy of Er:YAG laser treatment on stress urinary incontinence in women: Prospective cohort study. Climacteric 2015;18(Suppl 1):37–42. [DOI] [PubMed] [Google Scholar]
- 14. Pagano I, Gieri S, Nocera F, et al. Evaluation of the CO2 laser therapy on vulvo‐vaginal atrophy (VVA) in oncological patients: Preliminary results. J Cancer Ther 2017;8:452–463. 10.4236/jct.2017.85039 [DOI] [Google Scholar]
- 15. Athanasiou S, Pitsouni E, Grigoriadis T, et al. Microablative fractional CO2 laser for the genitourinary syndrome of menopause up to 12‐month results. Menopause 2019;26(3):248–255. 10.1097/GME.0000000000001206 [DOI] [PubMed] [Google Scholar]
- 16. Palacios S, Ramirez M. Efficacy of the use of fractional CO2RE intima laser treatment in stress and mixed urinary incontinence. Eur J Obstet Gynecol Reprod Biol 2020;244:95–100. 10.1016/j.ejogrb.2019.10.048 [DOI] [PubMed] [Google Scholar]


