Abstract
Background
The aim of this study was to examine the trends in impairment regarding activities of daily living (ADL), physical performance, and cognitive function among the oldest-old (those aged 80 and older) in China between 1998 and 2014.
Methods
We used data on 34,297 oldest-old individuals from the seven waves of the Chinese Longitudinal Healthy Longevity Study. We estimated age, period, and cohort effects on the prevalence of self-reported ADL impairment, tested physical performance and cognitive function impairment using the age–period–cohort model.
Results
Regarding age, the prevalence of ADL, physical performance, and cognitive function impairment were highest in the centenarians, but they did not increase with age in this population. Among the literate subgroup, the prevalence of cognitive impairment increased more rapidly with age than that in the illiterate subgroup. Regarding period, the prevalence of self-reported and tested physical impairment slowly increased between 1998 and 2014, but cognitive impairment remained stable. Regarding cohort, ADL impairment continuously decreased. However, physical and cognitive impairment remained stable after a brief decline in the early birth cohorts.
Conclusions
The results suggest that the age effect is still the most obvious effect regarding several types of functional impairment. The likelihood of a younger person experiencing functional impairment may not change significantly, but ADL is likely to be amenable to improvement resulting from improved medical and social care. Therefore, increased care for the oldest-old may considerably improve their quality of life, particularly regarding their basic ADL.
Keywords: Cognition, Physical performance, Longevity, Age, period, cohort model
Population aging is a major social problem faced by all countries. China, a country with a developing economy, is one of the countries with the highest rate of population aging. Improving the quality of life of the aging population and reducing the social burden have become major issues. In particular, a rapidly growing number of the oldest-old (those aged 80 and older) need more daily assistance and medical care (1,2). Therefore, the study of physical and mental health among the oldest-old has important significance.
In recent decades, due to the development of the economy and medical care, life expectancy has constantly increased. The burden of disease and dysfunction will probably also increase due to longevity, so more investment in socioeconomic and medical care was needed (3,4). Researches on period effects showed that, among older individuals in the United States, Sweden, Spain, and Japan, physical and cognitive impairment have tended to worsen to a greater extent in more recent years than in earlier years (5–9). However, other studies have shown opposite results, and overall health has also improved in the U.S. older adult population (10,11). Studies on the older adult population in China have found that the prevalence of impairment in activities of daily living (ADL) and instrumental activities of daily living (IADL) has decreased significantly from the 1990s to the 2000s (12–14), and cognitive impairment and Alzheimer’s disease prevalence have also decreased (15,16). However, these previous studies rarely adjusted for the age–period–cohort (APC) effect. Each aspect of APC contributes uniquely to the study of population health. Aging has an obvious relationship with population health, period captures the burden of morbidity, disability, and mortality in the entire population at a given time, and cohort reflects the health of successive generations and is an important dimension for understanding how population health is changing over time. Overall, failure to isolate APC trends can lead to substantial bias and provides an incomplete picture of population health trends (17).
Several studies on the health status of older adult populations have explored some of the effects of APC, but there are still deficiencies. A study of National Health and Nutrition Examination Survey (NHANES) data demonstrated that ADL and IADL impairment increased with time after controlling for age and cohort effects (18). However, this study did not identify cohort trends, and the mean age (71.6 years) was too young for the study population to be a good representative of the oldest-old. In the National Health Interview Survey (NHIS), adjusted cohort trends for both outcomes showed continual increases across successive cohorts (19). A study among older Chinese adults in Hong Kong found that the prevalence of ADL impairment increased from 2003 to 2012, but there was no significant difference between the different birth cohorts (20). The ages of these study populations ranged from 65 to 86 years old, so the study populations also did not represent the oldest-old.
After a literature search, we found that large-scale studies on the APC trend of functional impairment among the oldest-old population are scarce. Therefore, we analyzed survey data from the seven waves of the Chinese Longitudinal Healthy Longevity Study (CLHLS), the world’s largest oldest-old cohort, using the APC model to analyze ADL, physical performance, and cognitive function impairment trends among the Chinese oldest-old from 1998 to 2014.
Methods
Study Design and Participants
This study draws on data of the oldest-old participants (those aged 80–109 years) of the 1998, 2000, 2002, 2005, 2008, 2011, and 2014 waves of the CLHLS. The CLHLS is a nationwide survey conducted in a randomly selected half of the counties and cities in 22 of the 31 provinces, covering approximately 85% of the total population of China. The CLHLS attempted to interview all centenarians who voluntarily agreed to participate in the study in the sampled counties and cities. The CLHLS also adopted a targeted random-sample design to ensure representativeness through interviews with approximately equal numbers of male and female nonagenarians, octogenarians, and young-old (aged 65–79 years) living near the centenarians. This design serves our aim of investigating determinants of healthy longevity of different age and gender groups who live in the same social and natural environment well (21). The CLHLS was initially designed to facilitate international comparative analyses, and its questionnaire was translated from the instruments of the Danish longevity survey analyzed by Christensen and colleagues (22).
Variables
All CLHLS surveys used almost the same ascertainment and assessment protocols. No proxy was used for objective questions such as assessment of cognitive function and physical performance. The survey was administered in the homes of participants by trained interviewers.
Activities of daily living
The ADL functional status of six daily activities, eating, dressing, transferring, using the toilet, bathing, and continence, were used to measure the elders’ status of independence in daily living. A score of 0 was given to participants needing assistance with the activity, and a score of 1 indicated no help was needed by the participants, resulting in a range of 0–6 for total ADL scores. ADL is a good measurement of functional capacity and a proxy of health status widely used in healthy aging studies (22–24). In this study, we followed the ADL capacity group classification widely adopted in the other studies on the oldest-old: if none or one of the six ADL activities is impaired, the oldest-old is classified as “normal”; if two or more activities are impaired, the oldest-old is classified as having “ADL impairment.” The proportions of the six ADL impairment and the overall impairment prevalence in different ages, gender, residence type, and educational background subgroups are described in Supplementary Tables 1 and 2.
Physical performance measured by three tests
Self-reported subjective measures of ADL impairment have been criticized for their potential to be affected by both differences in the availability of associated facilities and perceptions of the participants. Objective performance-based tests are highly recommended as complementary measures in examining physical functions (25–27). In the Chinese older adult population, objective performance-based tests have been recently valued as important complementary measures for routine ADL assessment and have helped to clarify the intrinsic physiological impairment of older adult individuals and the environmental barriers of their daily activities (28,29).
Three objective physical performance tests were administered in the CLHLS surveys. The first task involved standing from a sitting position in a chair. This test has three outcome levels: “can without using arms” (coded as 1), “can using arms” (coded as 0.5), and “cannot” (coded as 0). The second task was to pick up a book from the floor, and respondents were classified as “can while standing” (coded as 1), “can while sitting” (coded as 0.5), and “cannot” (coded as 0). The last task tested whether the respondent could turn approximately 360° without help (yes vs. no, coded as 1 or 0). If all three test scores were 1, the participant was classified as “normal,” and if one of the test scores was not 1, the participant was classified as having “physical performance impairment.” The proportions of individuals with a score of <1 for each of the three physical performance tests and the overall impairment prevalence in different ages, gender, residence type, and educational background subgroups are described in Supplementary Tables 1 and 3.
Cognitive function measured by Mini-Mental State Examination
The Mini-Mental State Examination (MMSE), a global assessment of cognitive function (22,30), was adapted to the Chinese cultural context and was carefully tested in a pilot survey (31). The testing protocol includes 24 items regarding orientation, registration, attention, calculation, recall, and language, with a total score ranging from 0 to 30. Following the practice widely adopted in other studies, we used the MMSE cutoffs to define cognitive function as severe impairment (0–17), mild impairment (18–23), normal (24–27), and maximum (28–30). For the MMSE, the questions could not be answered by a proxy. If the MMSE score was ≥24, the participant was classified as “normal,” and if the score was <24, the participant was classified as having “cognitive impairment.” The rates of cognitive impairment regarding each MMSE subsection and overall cognitive impairment prevalence in different age, gender, residence type, and educational background subgroups are described in Supplementary Tables 1 and 4. In addition, the mean and SD of MMSE scores in the different subgroups are shown in Supplementary Table S5.
The rates of missing values for the variables analyzed in this study were mostly <1%. Due to such low missing data rates, we did not impute the missing values. In the statistical analyses, we excluded the cases with missing values. Comparisons between samples with missing values and samples with complete data can be found in Supplementary Table S6.
Age, period, and birth cohort
Individual ages were available for all respondents, and the respondents were divided into groups of 3-year age intervals (80–82 to 107–109 years). Periods were established using the year of each survey (1998–2014). The birth cohorts were established by subtracting individual ages from the survey years, and then the values were grouped into 3-year categories (1888–1890 to 1929–1931 years).
Sociodemographic variables
We estimated the APC models separately by gender (male or female), residence type (urban or rural), and educational background (literate [received ≥1 year of any formal education] and illiterate [received <1 year of formal education]).
Statistical Analyses
We examined the differences among survey waves regarding the distribution of ADL, physical, and cognitive impairment prevalence by gender, age, residence type, and educational background. Thereafter, we used an intrinsic estimator (IE, represented by β) for the APC analyses, using the approach developed by Yang and colleagues (32–34). Briefly, this method has the advantage that the structure of the design matrix (the numbers of age groups and time periods) does not affect the estimates. The IE employs a special principal components regression that removes the influence of the null space of the design matrix on the estimator. In addition, prior constraints that are often used in conventional analyses to obtain uniquely identified APC parameters (eg, fixing the effects of two or more age groups) are not necessary. The IE can be used to estimate generalized linear models with age, period, and cohort effects. Given that the numbers of individuals with impairment are non-negative counts that can be considered to have a Poisson distribution, log linear models were estimated. The log of the exposure (population with impairment) entered the model (with a coefficient constrained to be 1), which resulted in the estimation of the prevalence. We used the publicly available add-on file for the IE algorithm in Stata software version 15.0 (35). We also estimated the APC effects by gender, residence type, and educational background. A two-tailed p < 0.05 was regarded as significant.
Results
Demographic Distribution of Functional Impairment at Each Wave
The characteristics of the participants are given in Table 1. The study consisted of 34,297 participants in all cross-sectional surveys. There was a higher proportion of females (from 57.0% to 61.4%) than males in the surveys. Individual ages ranged from 80 to 109 years old. The mean age of each wave was between 90.87 (2014) and 92.82 (2008) years old. The crude prevalence of ADL impairment ranged from 18.8% to 24.1%, physical impairment ranged from 28.8% to 44.2%, and cognitive impairment ranged from 38.7% to 52.8%. Cognitive impairment remained the most common impairment. Supplementary Tables 1–3 show the demographic distributions of ADL, physical and cognitive impairment prevalence. Females had a higher impairment burden at each wave. The rural population had a similar ADL and physical impairment burden but a higher cognitive impairment burden than the urban population.
Table 1.
Characteristics of Chinese Adults 80 Years of Age or Older in Seven Wave Survey in CLHLS
| Characteristic | 1998 | 2000 | 2002 | 2005 | 2008 | 2011 | 2014 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 8,938) | (n = 11,123) | (n = 11,128) | (n = 10,620) | (n = 12,238) | (n = 6,503) | (n = 3,848) | ||||||||
| Mean age, y | 92.25 | 91.27 | 92.57 | 92.76 | 92.82 | 92.13 | 90.87 | |||||||
| Genders | ||||||||||||||
| Male | 3,563 | 39.9% | 4,624 | 41.6% | 4,389 | 39.4% | 4,183 | 39.4% | 4,726 | 38.6% | 2,628 | 40.4% | 1,656 | 43.0% |
| Female | 5,375 | 60.1% | 6,499 | 58.4% | 6,739 | 60.6% | 6,437 | 60.6% | 7,512 | 61.4% | 3,875 | 59.6% | 2,192 | 57.0% |
| Age, y | ||||||||||||||
| 80–82 | 1,179 | 13.2% | 1,602 | 14.4% | 1,192 | 10.7% | 828 | 7.8% | 1,243 | 10.2% | 695 | 10.7% | 570 | 14.8% |
| 83–85 | 1,092 | 12.2% | 1,556 | 14.0% | 1,390 | 12.5% | 1,102 | 10.4% | 1,173 | 9.6% | 905 | 13.9% | 541 | 14.1% |
| 86–88 | 946 | 10.6% | 1,341 | 12.1% | 1,271 | 11.4% | 1,523 | 14.3% | 1,326 | 10.8% | 797 | 12.3% | 615 | 16.0% |
| 89–91 | 1,023 | 11.4% | 1,567 | 14.1% | 1,280 | 11.5% | 1,588 | 15.0% | 1,917 | 15.7% | 806 | 12.4% | 505 | 13.1% |
| 92–94 | 915 | 10.2% | 1,271 | 11.4% | 1,432 | 12.9% | 1,312 | 12.4% | 1,653 | 13.5% | 905 | 13.9% | 409 | 10.6% |
| 95–97 | 806 | 9.0% | 851 | 7.7% | 928 | 8.3% | 1,037 | 9.8% | 1,069 | 8.7% | 708 | 10.9% | 422 | 11.0% |
| 98–100 | 1,494 | 16.7% | 1,230 | 11.1% | 1,391 | 12.5% | 1,185 | 11.2% | 1,356 | 11.1% | 485 | 7.5% | 250 | 6.5% |
| 101–103 | 1,153 | 12.9% | 1,261 | 11.3% | 1,648 | 14.8% | 1,354 | 12.7% | 1,677 | 13.7% | 618 | 9.5% | 231 | 6.0% |
| 104–106 | 252 | 2.8% | 360 | 3.2% | 500 | 4.5% | 571 | 5.4% | 661 | 5.4% | 439 | 6.8% | 183 | 4.8% |
| 107–109 | 78 | 0.9% | 84 | 0.8% | 96 | 0.9% | 120 | 1.1% | 163 | 1.3% | 145 | 2.2% | 122 | 3.2% |
| Residence | ||||||||||||||
| Urban | 3,373 | 37.7% | 5,808 | 52.2% | 4,981 | 44.8% | 4,663 | 43.9% | 4,716 | 38.5% | 2,178 | 33.5% | 1,231 | 32.0% |
| Rural | 5,565 | 62.3% | 5,315 | 47.8% | 6,147 | 55.2% | 5,957 | 56.1% | 7,522 | 61.5% | 4,325 | 66.5% | 2,617 | 68.0% |
| Education | ||||||||||||||
| Illiteracy | 6,036 | 67.5% | 7,167 | 64.4% | 7,567 | 68.0% | 7,360 | 69.3% | 8,760 | 71.6% | 4,450 | 68.4% | 2,472 | 64.2% |
| Literacy | 2,902 | 32.5% | 3,956 | 35.6% | 3,561 | 32.0% | 3,260 | 30.7% | 3,478 | 28.4% | 2,053 | 31.6% | 1,376 | 35.8% |
| Activities of daily living | ||||||||||||||
| Normal | 6,781 | 75.9% | 8,773 | 78.9% | 8,411 | 75.6% | 8,406 | 79.2% | 9,934 | 81.2% | 4,983 | 76.6% | 2,995 | 77.8% |
| Impairment | 2,119 | 23.7% | 2,317 | 20.8% | 2,669 | 24.0% | 2,210 | 20.8% | 2,303 | 18.8% | 1,515 | 23.3% | 845 | 22.0% |
| Missing | 38 | 0.4% | 33 | 0.3% | 48 | 0.4% | 4 | <0.1% | 1 | <0.1% | 5 | <0.1% | 8 | 0.2% |
| Physical performance | ||||||||||||||
| Normal | 6,363 | 71.2% | 7,691 | 69.1% | 6,885 | 61.9% | 6,530 | 61.5% | 6,826 | 55.8% | 3,945 | 60.7% | 2,350 | 61.1% |
| Impairment | 2,446 | 27.4% | 3,362 | 30.2% | 4,164 | 37.4% | 4,060 | 38.2% | 5,405 | 44.2% | 2,539 | 39.0% | 1,485 | 38.6% |
| Missing | 129 | 1.4% | 70 | 0.6% | 79 | 0.7% | 30 | 0.3% | 7 | <0.1% | 19 | 0.3% | 13 | 0.3% |
| Cognitive function | ||||||||||||||
| Normal | 4,737 | 53.0% | 6,395 | 57.5% | 5,236 | 47.1% | 5,244 | 49.4% | 5,374 | 43.9% | 3,145 | 48.4% | 2,006 | 52.1% |
| Impairment | 4,105 | 45.9% | 4,684 | 42.1% | 5,884 | 52.9% | 5,376 | 50.6% | 6,864 | 56.1% | 3,322 | 51.1% | 1,839 | 47.8% |
| Missing | 96 | 1.1% | 44 | 0.4% | 8 | <0.1% | 0 | 0 | 0 | 0 | 36 | 0.6% | 3 | <0.1% |
Notes: Data are years, cases or proportion %. Activities of daily living (ADL) measured by six questions, physical performance measured by three tests and cognitive function measured by Mini-Mental State Examination (MMSE).
Age, Period, and Cohort Effects on Functional Impairment
Age effects
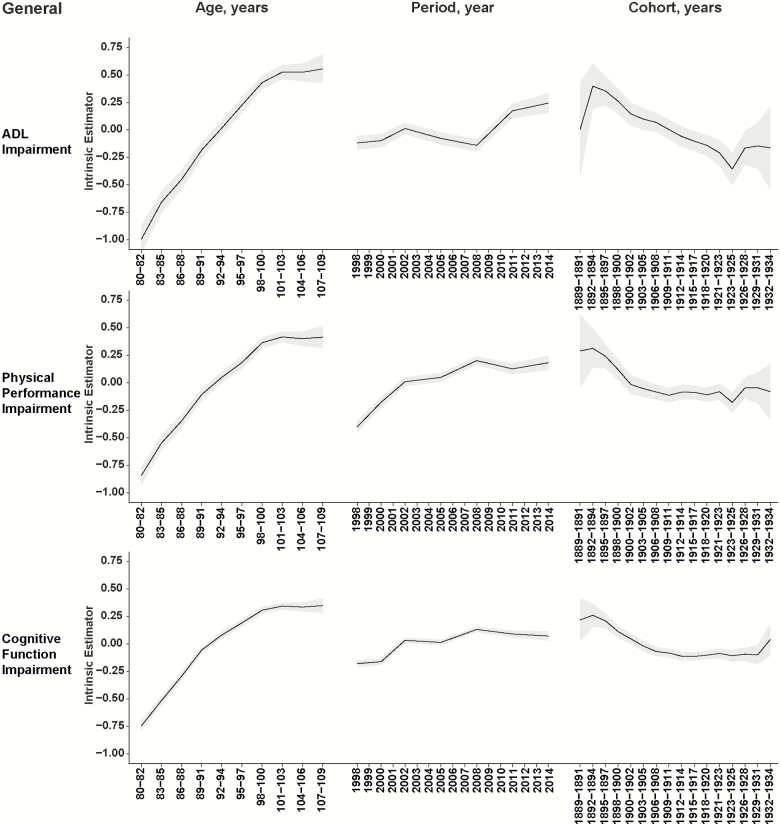
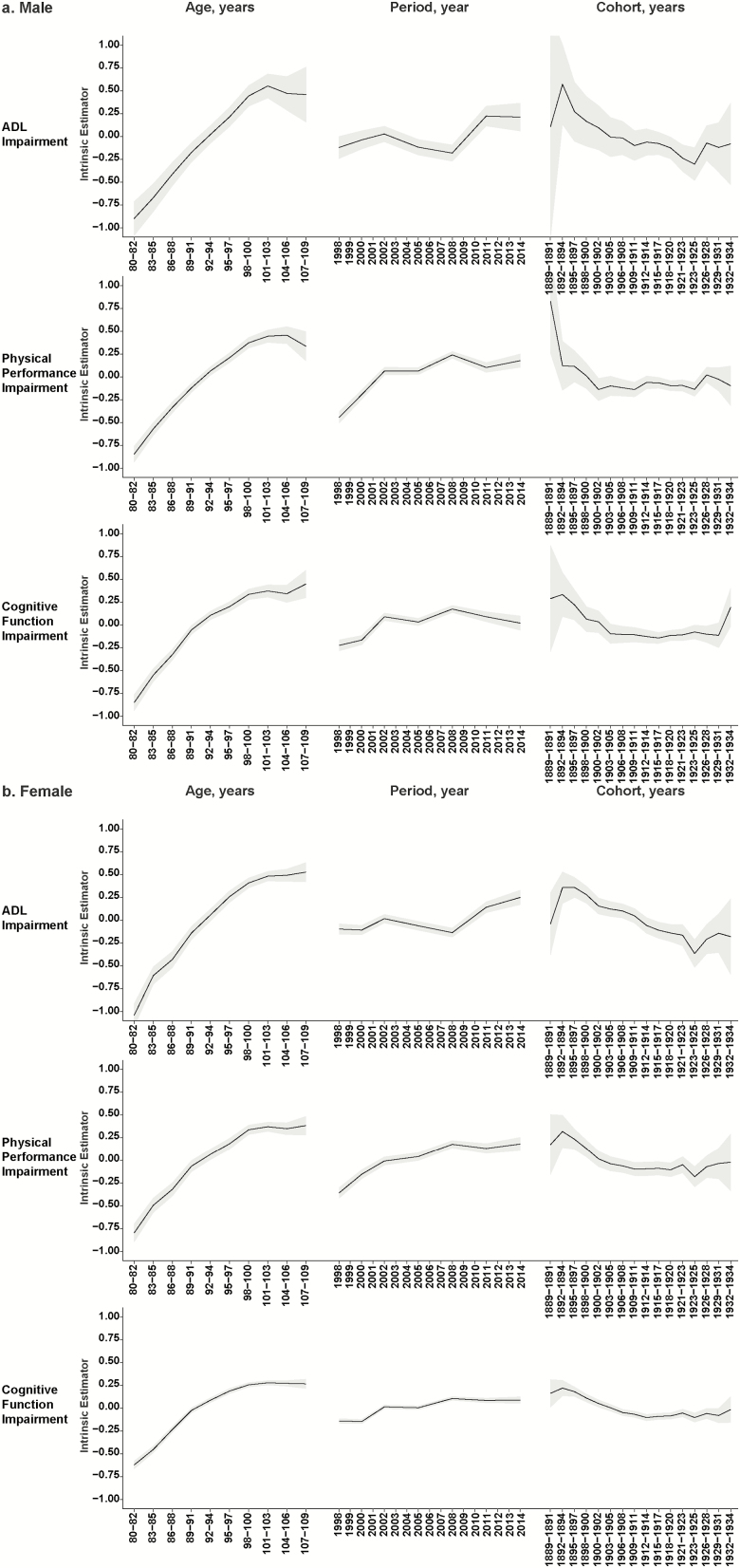
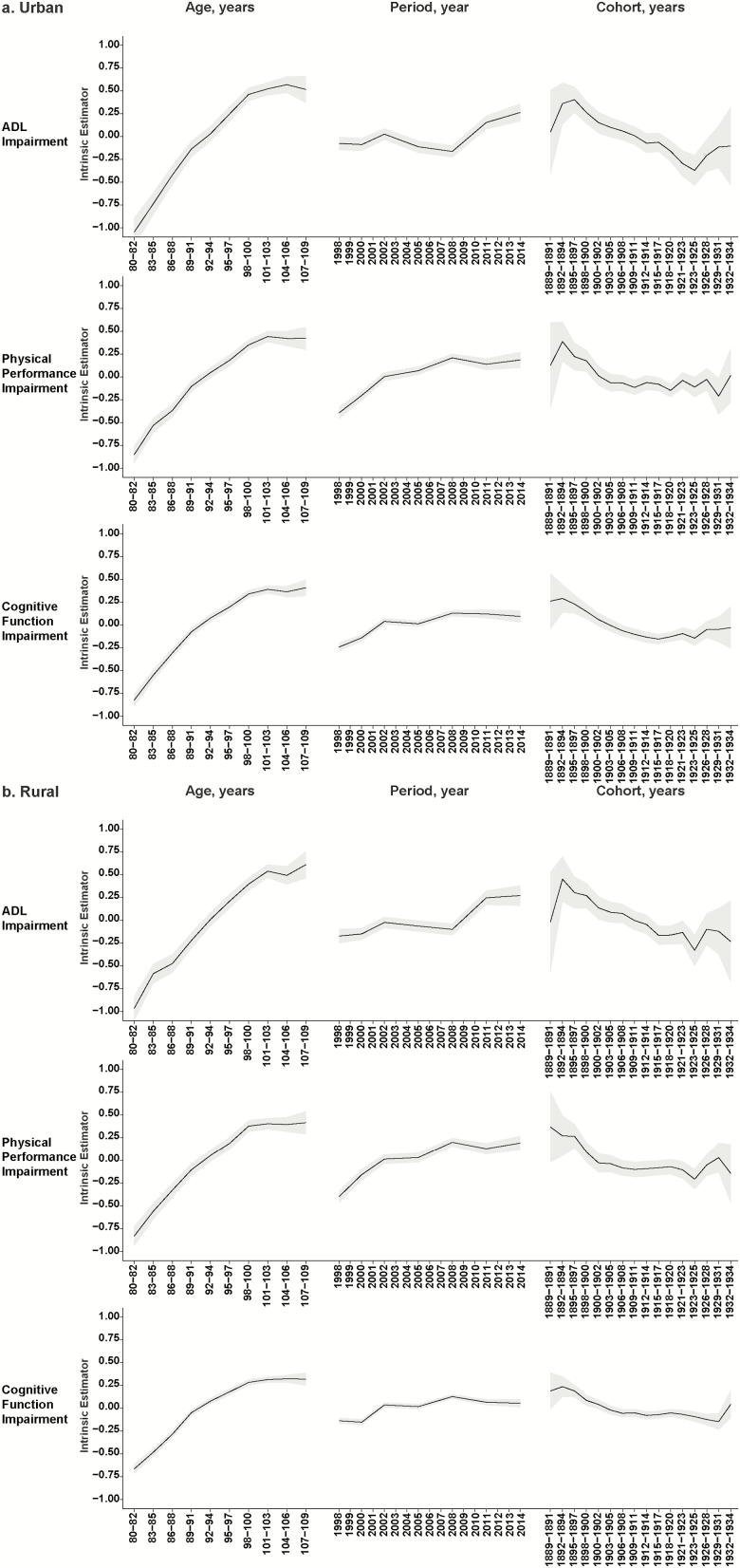
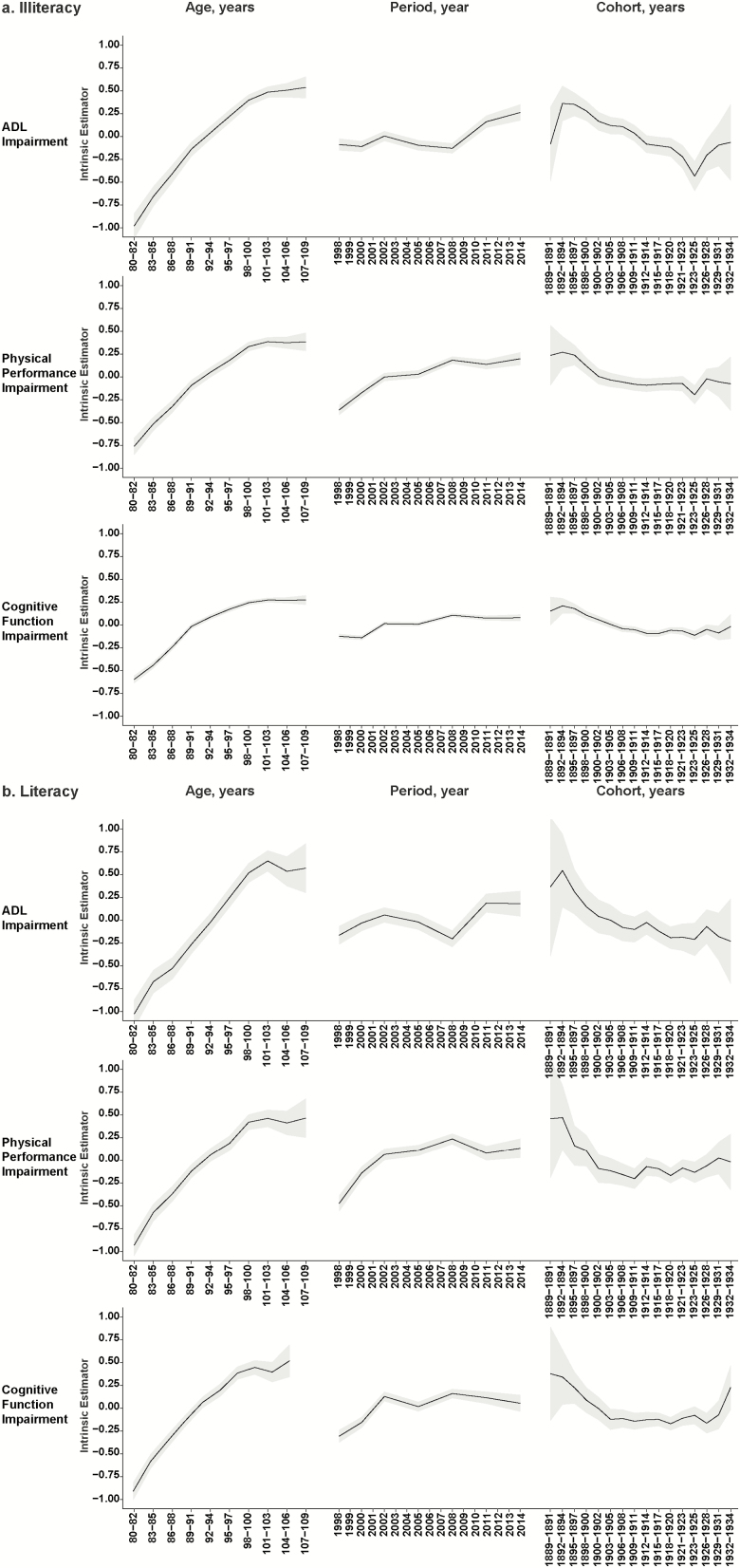
ADL, physical performance, and cognitive impairment increased rapidly between the ages of 80 and 100. However, after the age of 100 years, the impairment burden did not continue to increase and remained stable (ADL impairment: β = 0.52–0.55; physical impairment: β = 0.40–0.42; cognitive impairment: β = 0.38–0.39). This means that in the age group after 100 years old, the burden of ADL, physical performance, and cognitive impairment was about 1.71, 1.51, and 1.41 times higher, respectively, than the burden for all ages combined (Figure 1). Almost the same trend was observed in the subsequent analyses of different genders, location types, and educational backgrounds. Among them, the ADL and physical impairment burden in males decreased after 104–106 years old. In addition, the rapid deterioration of cognitive function with age was more severe in the male, urban, and literate subgroups (Figures 2–4).
Figure 1.
Age, period, and cohort effects on ADL, physical performance, and cognitive function impairment prevalence in the Chinese oldest-old general population. The intrinsic estimator (IE) estimate is the mean change in impairment associated with an age–period–cohort (APC) group relative to the mean of all APC groups combined. Solid lines, IE estimates; gray bands, 95% confidence intervals.
Figure 2.
Age, period, and cohort effects on ADL, physical performance, and cognitive function impairment prevalence in the Chinese oldest-old male (a) and female (b) populations. The intrinsic estimator (IE) estimate is the mean change in impairment associated with an age–period–cohort (APC) group relative to the mean of all APC groups combined. Solid lines, IE estimates; gray bands, 95% confidence intervals.
Figure 3.
Age, period, and cohort effects on ADL, physical performance, and cognitive function impairment prevalence in the Chinese oldest-old urban (a) and rural (b) populations. The intrinsic estimator (IE) estimate is the mean change in impairment associated with an age–period–cohort (APC) group relative to the mean of all APC groups combined. Solid lines, IE estimates; gray bands, 95% confidence intervals.
Figure 4.
Age, period, and cohort effects on ADL, physical performance, and cognitive function impairment prevalence in the Chinese oldest-old illiteracy (a) and literacy (b) populations. The intrinsic estimator (IE) estimate is the mean change in impairment associated with an age–period–cohort (APC) group relative to the mean of all APC groups combined. Solid lines, IE estimates; gray bands, 95% confidence intervals.
Period effects
ADL, physical performance, and cognitive impairment prevalence gradually increased with the period. The peak ADL impairment was in 2014 (β = 0.24, 95% confidence interval [CI]: 0.16, 0.33), the peak physical impairment was in 2008 (β = 0.20, 95% CI: 0.17, 0.24), and the peak cognitive impairment was in 2008 (β = 0.13, 95% CI: 0.11, 0.15; Figure 1). In the gender, location type, and educational background subgroups, the period effect exhibited almost the same trend. Among them, the trends of physical and cognitive impairment changed more smoothly in the female and illiterate subgroups (Figures 2–4).
Cohort effects
ADL, physical performance, and cognitive impairment all rapidly declined, followed by stabilization. Among them, ADL impairment had the most fluctuations. The birth cohort of 1892–1894 had the highest prevalence of ADL impairment (β = 0.40, 95% CI: 0.20, 0.60). Thereafter, the prevalence declined in all cohorts through to the 1923–1925 cohort, which had the lowest values (β = −0.36, 95% CI: −0.50, −0.21). After that, the prevalence increased slightly and then remained stable. For the birth cohorts between 1892 and 1894 and 1900–1902, there was a rapid decline in the physical impairment prevalence from its peak (β = 0.31, 95% CI: 0.14, 0.49). Since then, the prevalence remained stable. Moreover, cognitive impairment exhibited nearly the same trend, that is, the highest impairment rate was in the 1892–1894 cohort (β = 0.26, 95% CI: 0.16, 0.36) followed by a decline across the cohorts through to the 1906–1908 cohort (β = −0.07, 95% CI: −0.11, −0.03), after which the prevalence remained unchanged (Figure 1). In the subgroup analyses, the cohort effect exhibited almost the same trend, but the IE values had greater volatility and wide CIs in the male, urban, and literate subgroups. In addition, in the literate subgroup, IE values remained stable from the first cohort to the 1903–1905 cohort, whereas in the illiterate subgroup, they remained stable until the 1912–1914 cohort (Figures 2–4).
Discussion
The CLHLS is a nationwide survey conducted in a randomly selected half of the counties and cities in 22 of the 31 provinces of China, covering approximately 85% of the total population of China. In the present study, we used the APC model to analyze data regarding functional impairment in the world’s largest oldest-old cohort for the first time. Regarding the age effect, we demonstrated that the ADL, physical, and cognitive impairment burden rapidly increased with age but remained stable in the centenarians. Self-reported ADL and objective physical performance impairment rates slowly increased between 1998 and 2014, but cognitive impairment remained stable, except for a period of decline in ADL impairment between 2002 and 2008. In addition, the ADL impairment rate continually declined across birth cohorts, while the physical and cognitive impairment rates remained unchanged for a long period of time after a sharp decline. These trends were similar in gender, location type, and educational background subgroups. Furthermore, we found that females had a higher rate of ADL, physical, and cognitive impairment, which may be due to females having a longer life expectancy. A higher burden of ADL, physical, and cognitive impairment was observed in rural regions, which is closely related to the socioeconomic status and access to medical care of these regions.
The results of the APC model analysis showed that age had a significant effect on the ADL, physical, and cognitive impairment burden. These impairments rapidly became very common with age, consistent with general knowledge and the results of previous studies. However, because the mortality rate increased with age, the overall burden remained stable, especially among centenarians. The period effect remained relatively stable, followed by a gradual rise. We speculated that this may be due to an increase in the overall life expectancy of the population, which means that the life expectancy of the population with impairments was extended, resulting in an increase in the overall impairment burden. This is also consistent with previous studies (20,36). The ADL impairment rate reached its lowest point in 2008, when looking at the period effect. The main reason we considered was that, unlike physical performance and cognitive function (objective indicators of the abilities of older individuals), ADL is more affected by medical care and life nursing. With the increased investment in medical care in a certain historical period, the burden of ADL impairment was improved. In addition, the improvement of ADL impairment occurred in more birth cohorts. These findings suggest that the overall burden of disability may increase to some extent in the future, indicating an increase in long-term care demand.
In contrast, the cohort effect was more complex. ADL impairment was significantly lower in the late-born population, consistent with the results based on the same cohort (27) but different from the results of other populations, such as in the United States and Hong Kong, that showed that the cohort effect appeared to remain stable or to increase (18–20). We speculate that multiple reasons may explain these findings. First, there were large differences in the socioeconomic conditions of the early-born populations between these studies; the Chinese mainland was undergoing great social and economic turbulence during the early-born individuals’ lives. After this period, ADL impairment improved. Second, the age of the population included in these studies was not completely consistent. CLHLS contained more people aged >80. This group had a higher prevalence of ADL impairment and was more sensitive to the progress of life care brought about by socioeconomic development, suggesting that the burden of ADL impairment may decrease in more recent birth cohorts. Third, the burden of physical and cognitive impairment gradually became stable after a brief decline in the early-born cohorts, which more objectively indicated that the physical and mental state of older individuals was less affected by improved resources and family care. As two indicators reflecting the physical activity of the oldest-old, objective physical impairment, and self-reported ADL impairment showed similar trends, indicating the reliability of the results. These results suggest that, unlike people born in a period of extreme resource scarcity and social turmoil, the physical and cognitive function of older people born at different times in peaceful eras will be stable, which is consistent with a previous study (37). However, this result was different from an earlier study based on the CLHLS (27). This may be due to the criteria we used to assess impairment or due to unspecific scores, which may mean that our results are more sensitive to the respondents’ impairment status (impairment vs no impairment) without considering the severity. As the tested items were the most basic daily and thinking activities, slight issues will have a great impact on the quality of life, it is reasonable to use such impairment status criteria. Finally, we used the APC model, which may more independently reflect the birth cohort effect by adjusting for the age and period effects (which exhibit significant collinearity with the birth cohort effect). In the gender, location type and educational background subgroups, the period effect showed almost the same trend. Perhaps due to the differences in sample size between pairs of subgroups, the 95% CIs were smaller in the female, rural, and illiterate subgroups, and the trends were more stable and smoother. It was worth noting that the age effect on cognitive impairment burden in the male and urban subgroups, and especially in the literate subgroup, increased more rapidly with age. In addition, in the illiterate subgroup, the cognitive improvement of later-born population occurred in a longer period of time. We speculated that the reason may be that education may enable the oldest-old to have better cognitive function at a relatively young age, but with the increase of age, cognitive function irresistibly deteriorates, which leads to a rapid increase in the burden of cognitive impairment in the population under good education and economic conditions. This also highlights the urgency and importance of research on cognitive function among the older adults.
Our results provide new insights into the health status of the oldest-old during extensive social and economic changes, but there are still some limitations to our study. Due to the limitations of the model, we did not adjust for other factors, such as family economic conditions, education level, marital status, chronic conditions, and disability. We replaced the scores with binary variables indicating the presence of impairment, which may have caused a loss in information about the severity of the impairments. Furthermore, improved assessment of physical state is urgently needed to more comprehensively describe the living conditions of the older adults before the end of their lives. China is facing the world’s greatest population aging problem. With the increase in average life expectancy, although medical treatments and social security are continually improving, there are still many diseases and unhealthy conditions that result in a heavy social burden.
This study used data from seven population-based survey waves among the oldest-old in China and assessed the prevalence trends of ADL, physical, and cognitive impairment by using the APC model. The results suggest that the age effect is still the most important factor regarding several functional impairments. When the socioeconomic development meets the most basic needs of the population, there is no obvious improvement in the objective physical and cognitive function among the more recently born population cohorts in their old age. However, ADL, which is more sensitive to medical care, may continue to improve. ADL assessment is the standard evaluation for basic activity ability; ADL improvement ensures that the older adults will have dignity in their last period of life. Therefore, economic development that brings more investment in medical care for the older adults is of great significance to them. These measures include providing long-term and acute day-to-day care and access for individuals with disabilities, providing jobs for the older individuals who remain active and providing services and personalized interventions for social and leisure activities. In the future, research on geriatric syndromes in the older adults will continue to expand to wider age groups. In addition, future research should also more stringently control for the potential confounders. Novel effective approaches are required to improve predictions, assessments, and health interventions for the older adult population.
Supplementary Material
Acknowledgments
The Chinese Longitudinal Healthy Longevity Study (CLHLS), which provides data analyzed in this article, is jointly supported by National Natural Sciences Foundation of China (71490732) and the U.S. National Institute of Aging (3P01AG031719-07S1). We thank all interviewees and their families for their voluntary participation in the CLHLS study.
Funding
This work was supported by the National Key Research and Development Program of China (2018YFC2000400 to C.M.), the Construction of High-Level University of Guangdong (G619080438 and G618339167 to C.M.), and the National Natural Sciences Foundation of China (81573207, 71233001, 71490732, and 81573247 to X.M.S.). The funders played no role in the study design or implementation; data collection, management, analysis, or interpretation; manuscript preparation, review, or approval; or the decision to submit the manuscript for publication.
Author Contributions
X.M.S. and C.M. designed the study and drafted the article. P.D.Z. performed the statistical data analysis and worked with Y.B.L. to draft the article. All authors discussed and contributed to the theoretical framework, interpretation of the results, and revised and gave final approval of this manuscript.
Conflict of Interest
None reported.
References
- 1. Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med. 1980;303:130–135. doi:10.1056/NEJM198007173030304 [DOI] [PubMed] [Google Scholar]
- 2. Vaupel JW. Biodemography of human ageing. Nature. 2010;464:536–542. doi:10.1038/nature08984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. 2009;374:1196–1208. doi:10.1016/S0140-6736(09)61460-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Waidmann T, Bound J, Schoenbaum M. The illusion of failure: trends in the self-reported health of the U.S. elderly. Milbank Q. 1995;73:253–287. [PubMed] [Google Scholar]
- 5. Fuller-Thomson E, Yu B, Nuru-Jeter A, Guralnik JM, Minkler M. Basic ADL disability and functional limitation rates among older AMERICANS from 2000–2005: the end of the decline? J Gerontol A Biol Sci Med Sci.. 2009;64:1333–1336. doi:10.1093/gerona/glp130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Parker MG, Schon P, Lagergren M, Thorslund M. Functional ability in the elderly Swedish population from 1980 to 2005. Eur J Ageing. 2008;5:299–309. doi:10.1007/s10433-008-0096-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Palacios-Cena D, Jimenez-Garcia R, Hernandez-Barrera V, Alonso-Blanco C, Carrasco-Garrido P, Fernandez-de-Las-Penas C. Has the prevalence of disability increased over the past decade (2000–2007) in elderly people? A Spanish population-based survey. J Am Med Dir Assoc. 2012;13:136–142. doi:10.1016/j.jamda.2010.05.007 [DOI] [PubMed] [Google Scholar]
- 8. Parker MG, Ahacic K, Thorslund M. Health changes among Swedish oldest old: prevalence rates from 1992 and 2002 show increasing health problems. J Gerontol A Biol Sci Med Sci. 2005;60:1351–1355. doi:10.1093/gerona/60.10.1351 [DOI] [PubMed] [Google Scholar]
- 9. Dodge HH, Buracchio TJ, Fisher GG, et al. Trends in the prevalence of dementia in Japan. Int J Alzheimers Dis. 2012;2012:956354. doi:10.1155/2012/956354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: a systematic review. JAMA. 2002;288:3137–3146. doi:10.1001/jama.288.24.3137 [DOI] [PubMed] [Google Scholar]
- 11. Manton KG. Recent declines in chronic disability in the elderly U.S. population: risk factors and future dynamics. Annu Rev Public Health. 2008;29:91–113. doi:10.1146/annurev.publhealth.29.020907.090812 [DOI] [PubMed] [Google Scholar]
- 12. Liang Y, Welmer AK, Moller J, Qiu C. Trends in disability of instrumental activities of daily living among older Chinese adults, 1997–2006: population based study. BMJ Open. 2017;7:e016996. doi:10.1136/bmjopen-2017-016996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liang Y, Song A, Du S, Guralnik JM, Qiu C. Trends in disability in activities of daily living among Chinese older adults, 1997–2006: the China Health and Nutrition Survey. J Gerontol A Biol Sci Med Sci.. 2015;70:739–745. doi:10.1093/gerona/glu204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Feng Q, Zhen Z, Gu D, Wu B, Duncan PW, Purser JL. Trends in ADL and IADL disability in community-dwelling older adults in Shanghai, China, 1998–2008. J Gerontol B Psychol Sci Soc Sci. 2013;68:476–485. doi:10.1093/geronb/gbt012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wu YT, Lee HY, Norton S, et al. Period, birth cohort and prevalence of dementia in mainland China, Hong Kong and Taiwan: a meta-analysis. Int J Geriatr Psychiatry. 2014;29:1212–1220. doi:10.1002/gps.4148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chan KY, Wang W, Wu JJ, et al. Epidemiology of Alzheimer’s disease and other forms of dementia in China, 1990–2010: a systematic review and analysis. Lancet. 2013;381:2016–2023. doi:10.1016/s0140-6736(13)60221-4 [DOI] [PubMed] [Google Scholar]
- 17. Yang Y, Land KC. Age–period–cohort analysis of repeated cross-section surveys: fixed or random effects? Sociol Methods Res. 2008;36:297–326. doi:10.1177/0049124106292360 [Google Scholar]
- 18. Seeman TE, Merkin SS, Crimmins EM, Karlamangla AS. Disability trends among older Americans: National Health and Nutrition Examination Surveys, 1988–1994 and 1999–2004. Am J Public Health. 2010;100:100–107. doi:10.2105/ajph.2008.157388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lin SF, Beck AN, Finch BK, Hummer RA, Masters RK, Master RK. Trends in US older adult disability: exploring age, period, and cohort effects. Am J Public Health. 2012;102:2157–2163. doi:10.2105/AJPH.2011.300602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yu R, Wong M, Chang B, et al. Trends in activities of daily living disability in a large sample of community-dwelling Chinese older adults in Hong Kong: an age-period-cohort analysis. BMJ Open. 2016;6:e013259. doi:10.1136/bmjopen-2016-013259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zeng Y. Towards deeper research and better policy for healthy aging – using the unique data of Chinese Longitudinal Healthy Longevity Survey. China Econ J. 2012;5:131–149. doi:10.1080/17538963.2013.764677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Christensen K, Thinggaard M, Oksuzyan A, et al. Physical and cognitive functioning of people older than 90 years: a comparison of two Danish cohorts born 10 years apart. Lancet. 2013;382:1507–1513. doi:10.1016/S0140-6736(13)60777-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Katz S, Branch LG, Branson MH, Papsidero JA, Beck JC, Greer DS. Active life expectancy. N Engl J Med. 1983;309:1218–1224. doi:10.1056/NEJM198311173092005 [DOI] [PubMed] [Google Scholar]
- 24. Wiener JM, Hanley RJ, Clark R, Van Nostrand JF. Measuring the activities of daily living: comparisons across national surveys. J Gerontol. 1990;45:S229–S237. doi:10.1093/geronj/45.6.s229 [DOI] [PubMed] [Google Scholar]
- 25. Reuben DB, Seeman TE, Keeler E, et al. Refining the categorization of physical functional status: the added value of combining self-reported and performance-based measures. J Gerontol A Biol Sci Med Sci. 2004;59:1056–1061. doi:10.1093/gerona/59.10.m1056 [DOI] [PubMed] [Google Scholar]
- 26. Melzer D, Lan TY, Tom BD, Deeg DJ, Guralnik JM. Variation in thresholds for reporting mobility disability between national population subgroups and studies. J Gerontol A Biol Sci Med Sci. 2004;59:1295–1303. doi:10.1093/gerona/59.12.1295 [DOI] [PubMed] [Google Scholar]
- 27. Zeng Y, Feng Q, Hesketh T, Christensen K, Vaupel JW. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet. 2017;389:1619–1629. doi:10.1016/S0140-6736(17)30548-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Feng Q, Hoenig HM, Gu D, Yi Z, Purser JL. Effect of new disability subtype on 3-year mortality in Chinese older adults. J Am Geriatr Soc. 2010;58:1952–1958. doi:10.1111/j.1532-5415.2010.03013.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Purser JL, Feng Q, Yi Z, Hoenig H. A new classification of function and disability in China: subtypes based on performance-based and self-reported measures. J Aging Health. 2012;24:779–798. doi:10.1177/0898264312444310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. [DOI] [PubMed] [Google Scholar]
- 31. Yi Z, Vaupel JW. Functional capacity and self-evaluation of health and life of oldest old in China. J Soc Issues. 2002;58:733–748. doi:10.1111/1540-4560.00287 [Google Scholar]
- 32. Fu WJ. Ridge estimator in singulah oesiun with application to age-period-cohort analysis of disease rates. Commun Stat Theory Methods. 2000;29:263–278. doi:10.1080/03610920008832483 [Google Scholar]
- 33. Yang Y, Fu WJ, Land KC. A methodological comparison of age-period-cohort models: the intrinsic estimator and conventional generalized linear models. Sociol Methodol. 2004;34:75–110. doi:10.1111/j.0081-1750.2004.00148.x [Google Scholar]
- 34. Yang Y, Schulhofer-Wohl S, Fu WJ, Land KC. The intrinsic estimator for age-period-cohort analysis: what it is and how to use it. AJS. 2008;113:1697–1736. doi:10.1086/587154 [Google Scholar]
- 35. Stata C. Stata statistical software, release 9. College Station, TX: Stata Corporation; 2005. [Google Scholar]
- 36. Luo H, Yu G, Wu B. Self-reported cognitive impairment across racial/ethnic groups in the United States, National Health Interview Survey, 1997–2015. Prev Chronic Dis. 2018;15:E06. doi:10.5888/pcd15.170338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cho J, Martin P, Margrett J, MacDonald M, Poon LW, Johnson MA. Cohort comparisons in resources and functioning among centenarians: findings from the Georgia Centenarian Study. Int J Behav Dev. 2012;36:271–278. doi:10.1177/0165025412439967 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.