Abstract
Notch is an evolutionary, conserved, cell–cell signaling pathway that is central to several biological processes, from tissue morphogenesis to homeostasis. It is therefore not surprising that several genetic mutations of Notch components cause inherited human diseases, especially cardiovascular disorders. Despite numerous efforts, current in vivo models are still insufficient to unravel the underlying mechanisms of these pathologies, hindering the development of utmost needed medical therapies. In this perspective review, we discuss the limitations of current murine models and outline how the combination of microphysiological systems (MPSs) and targeted computational models can lead to breakthroughs in this field. In particular, while MPSs enable the experimentation on human cells in controlled and physiological environments, in silico models can provide a versatile tool to translate the in vitro findings to the more complex in vivo setting. As a showcase example, we focus on Notch-related cardiovascular diseases, such as Alagille syndrome, Adams–Oliver syndrome, and cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL).
Impact statement
In this review, a comprehensive overview of the limitations of current in vivo models of genetic Notch cardiovascular diseases is provided, followed by a discussion over the potential of microphysiological systems and computational models in overcoming these limitations and in potentiating drug testing and modeling of these pathologies.
Keywords: ex vivo, in vitro, in silico, Notch, cardiovascular
Introduction
Notch is a signaling pathway that relies on direct cell–cell interaction for its activation. Notch ligands (Dll1, Dll4, Jag1, and Jag2) presented at the surface of a cell interact with membrane-bound Notch receptors (Notch1–4) of another adjoining cell. The ligand–receptor interaction results in proteolytic processing of the Notch receptor, releasing the active signaling unit of the receptor, the Notch intracellular domain (NICD). Upon its release into the cytoplasm, the NICD translocates into the nucleus where it binds RBPJk, thereby inducing transcription of target genes and activation of transcriptional programs. This contributes to the determination of cell fate and regulation of tissue development and homeostasis.
In the cardiovascular system, Notch controls heart morphogenesis as well as blood vessel formation1–3 and homeostasis.4,5 Concurrently, mutations in different Notch ligands or receptors can cause several pathologies such as congenital heart defects (CHDs) and diseases such as Alagille syndrome (ALGS), Adams–Oliver syndrome (AOS), calcific aortic valve disease (AoVD), and cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL).3,6
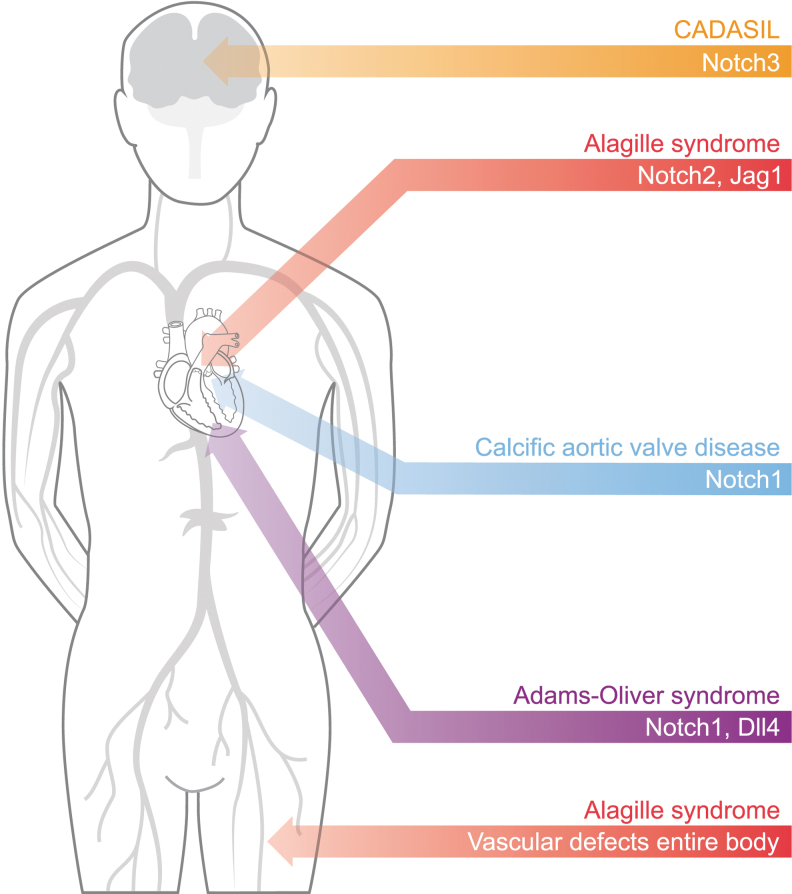
ALGS, AOS, and CADASIL are autosomal dominant diseases that display cardiovascular symptoms.3,6 Each of these diseases is associated with mutations in genes coding for different Notch components (Fig. 1). ALGS is a multisystemic pediatric disease caused by mutations in JAG1 or NOTCH2. The vascular complications include spontaneous bleeding, aneurysms, moyamoya syndrome, renal stenosis, and dilation of carotid arteries,7,8 as well as different CHDs such as tetralogy of Fallot, pulmonary stenosis, ventricular septal defects, and patent ductus arteriosus.9
FIG. 1.
Mutation of Notch signaling components can cause different congenital pathologies, especially within the cardiovascular system. Notch3 mutations lead to CADASIL, which mainly affects the brain vasculature. Notch1 mutations cause heart diseases as they are associated with both calcific AoVD and AOS, with the latter also caused by Dll4 mutations. Finally, mutations of Jag1 or Notch2 can lead to ALGS that presents vascular defects throughout the body and heart defects. ALGS, Alagille syndrome; AOS, Adams–Oliver syndrome; AoVD, aortic valve disease; CADASIL, cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy.
Mutations in NOTCH1 are associated with aberrant morphogenesis of the aortic valves, occurrence of AoVD,10 and AOS.11 This latter syndrome is also caused by mutations in DLL4,12 RBPJk,13 and other Notch-modifying genes. Despite AOS mainly manifesting through terminal transverse limb defects and scalp aplasia cutis, several AOS patients also display CHDs.14,15 CADASIL is a vascular dementia syndrome caused by mutations in NOTCH3, resulting in degeneration of vascular smooth muscle cells (VSMCs) and white matter, together with ischemic strokes.16 Unfortunately, current treatments cannot cure these diseases and only aim at mitigating the symptoms. To overcome this limitation and develop new regenerative therapeutic strategies, further understanding of the underlying molecular mechanisms is required.
Despite several efforts, current in vivo disease models fall short of replicating the actual human disease characteristics, which suggests that fundamental differences between species are present in this context. At the same time, the inherent complexity of in vivo models complicates the identification of the exact molecular mechanisms involved, thereby hindering the development of new therapies. In this perspective review, after summarizing current in vivo models of Notch-related cardiovascular diseases, we propose that their limitations could be overcome by combining engineered in vitro models, providing a controlled environment to investigate specific aspects of the pathologies, together with in silico models, providing a digital twin for the in vivo setting.
In Vivo Mouse Models for Notch-Associated Diseases
In vivo animal models are generally the most reliable in mimicking the complexity of human organisms. As such, they have been widely adopted to screen for the effects of Notch mutations. However, although ALGS, AOS, AoVD, and CADASIL are caused by autosomal dominant mutations, cardiovascular phenotypes are not obvious in mice presenting targeted disruption of one allele in the associated Notch genes,17–19 except for Dll4 in AOS.20–22 This limitation suggests that murine models are not fully reliable in this case as mice might have differences or compensatory mechanisms masking the effects of Notch mutations.
For example, mice most likely exhibit a different hemodynamic environment compared to humans, which can influence Notch responses to mechanics.23 Furthermore, mouse models have a short life span and different hallmarks of aging, which affect the possibility to mimic the temporal features of Notch-related diseases, including the fact that the first symptoms of CADASIL start to become evident in young adults16 despite the Notch-related mutation being present since birth. Nevertheless, a few animal models replicate some details of cardiovascular Notch-related diseases and thus provide valuable information on the disease etiology.
Mice carrying an array of different Notch mutations have been proposed as ALGS models.24–29 While mice heterozygous for either Jag1 or Notch2 cannot mimic the disease,17,19 double heterozygous mice (Jag1dDSL/+Notch2del1/+) can recapitulate several ALGS symptoms, including cardiac defects.24 However, ALGS is known to arise from single mutations in JAG1 and, more rarely, NOTCH2. Recently, Andersson et al.27 have described a novel mouse (Jag1Ndr/Ndr) with a phenotype mimicking ALGS in humans. The proposed mutation renders JAG1 hypomorphic, both inhibiting signaling through NOTCH1 and hindering activation of NOTCH2 and NOTCH3.27 This new model suggests that ALGS may result from Notch mutations causing partial loss of function, leading to reduced Notch activity. Overall, not only do these findings highlight the importance of understanding the specific roles of different Notch components in human physiology but they also point to the necessity of further analyzing Notch dose sensitivity.
Several mouse models of CADASIL, expressing mutant variants of NOTCH3 with altered numbers of cysteines, partially recapitulate the CADASIL phenotype. These mice exhibit the characteristic deposition of granular osmiophilic material and accumulation of NOTCH3, but no evident brain lesions30,31 (for a review, see32). Differently, introduction and overexpression of NOTCH3R169C into mice in a heterozygous state successfully created a phenotype also displaying white matter degeneration.33 This model has recently led to new findings suggesting that CADASIL is caused by Notch3 gain-of-function mutations that cause increased NAPDH oxidase 5 activation and consequential endoplasmic reticulum stress.34 Similar hypermorphic associations have been made with mutant Notch3 and NF-κB signaling, aggravating vascular remodeling and inflammation.35 However, this NOTCH3R169C model required excessive overexpression of the mutant protein, above endogenous levels,33 and whether CADASIL is caused by loss- or gain-of-function mutations is still strongly debated.32,36,37 Future studies should aim at clarifying this point, in addition to identifying the mechanisms causing CADASIL symptoms to start appearing in young adults and mainly in the brain region. Characterizing the temporal progression and localization of the disease might lead to development of strategies for early diagnosis and treatments.
Mice heterozygous for either Notch1 or RBPJk can mimic the human phenotype of AoVD to some extent. In particular, Notch1+/− mice show enhanced valve calcification and activation of alkaline phosphatase.38 RBPJk+/− mice display greater cardiac impairment, including thickened, calcified valve leaflets, macrophage infiltration, and collagen deposition, as well as activation of procalcific and profibrotic signaling pathways.39 Moreover, RBPJk+/− mice also have upregulated levels of Runx2,39 a transcription factor promoting osteoblast fate and heavily upregulated in human AoVD.40 The seemingly important role of RBPJk39 suggests that AoVD is a result of generally disrupted Notch transcriptional activation, which, given the results with the Notch1 mice,38 mainly occurs through Notch1, although other receptors must be involved. Unfortunately, Notch1+/−, RBPJk+/−, and Dll4+/− mice are, however, not representative models of AOS as they do not display the terminal transverse limb defects and scalp aplasia cutis characteristic of AOS. It has been proposed that vascular defects would be the main drivers of AOS,41,42 and mice with induced inhibition of Notch activity display loss of VSMC coverage and hemorrhage in different regions of the developing brain and limbs.41 In conclusion, animal models of Notch-associated cardiovascular diseases are currently not completely satisfactory; therefore, alternative and complementary strategies are necessary.
In Vitro Microphysiological Systems
Failure to meet the expectations of drug development and drug screening incentives has driven the development of microphysiological systems (MPSs) or organs-on-chips that recapitulate the function of human organs.43 MPSs can also aid in elucidating molecular mechanisms underlying human pathologies and the identification of therapeutic targets. As described above, this can be difficult in animal models, which may not reflect human pathophysiology and where dynamic molecular signaling events and complex cell–microenvironment interactions are difficult to capture. This is especially true for the cardiovascular system, where changes in hemodynamics can critically affect Notch signaling.23 Furthermore, many of the Notch-associated cardiovascular disorders listed above are rare disorders.44
Identifying molecular therapeutic targets and treating rare disease patients are huge challenges due to the limited amount of data available and the lack of relevant model systems. Fewer than around 5% of around 7000 currently identified rare diseases have effective drug therapies,45 and modeling rare disease has high potential to overcome this issue. Complex and rare diseases can be modeled in MPSs46 using cells from patient donors, either from primary or induced stem cell sources, or using genetic tools to induce a disease phenotype that can be studied in vitro against an isogenic background.
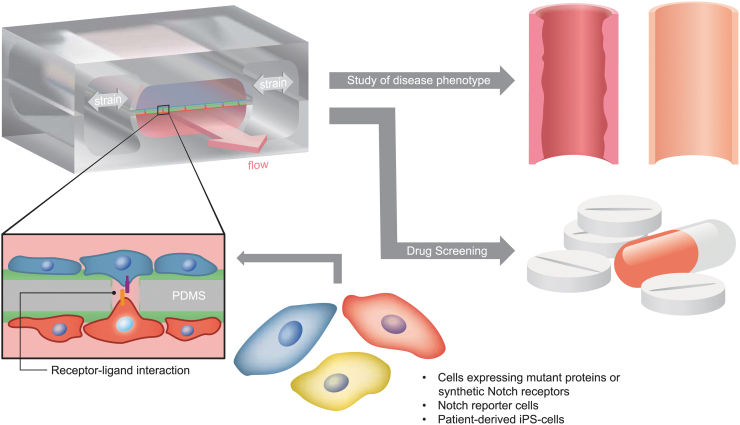
The Hutchinson–Gilford progeria syndrome (HGPS) is a rare genetic condition that is caused by a mutation in the Lamin A gene. Recently, a tissue-engineered blood vessel model of HGPS using induced pluripotent stem cell (iPSC)-derived endothelial cells identified the role of the endothelium in HGPS.47 Other rare diseases that have been modeled using iPSCs and organ-on-chip technologies include hereditary hemorrhagic telangiectasia, Rett syndrome, Alpers–Huttenlocher syndrome (as reviewed by Low and Tagle46), and Barth syndrome, where a heart-on-chip technology provided new insights into the pathogenesis.48 For all these reasons, we expect that the MPS will be a game changer also in the investigation of genetic Notch disorders as it could be adopted to study disease-mimicking cells and test drugs under physiologically relevant conditions (Fig. 2).
FIG. 2.
Microphysiological systems mimicking specific features of the cellular environment can enable the study of diseases caused by Notch mutations. For example, patient-derived or other human cells can be inserted in microfluidic devices mimicking the layer separation between endothelial cells and VSMCs, which is evident in blood vessels not only in terms of location but also stimuli (shear stress and cyclic stretch for endothelial cells and only cyclic stretch for VSMCs). These devices provide platforms where Notch interactions can be efficiently quantified, thereby enabling the controlled investigation of disease phenotypes and drug screening with donors' cells (the scheme of the microfluidic device is adapted from Ref. van Engeland et al.61). VSMC, vascular smooth muscle cell.
As described in the sections above, most of the genetic Notch cardiovascular disorders seem to arise from defects in blood vessels, which are in turn caused by incorrect temporal changes in Notch dosage,27 mediated by the interactions between multiple Notch ligands and receptors,27,38,39 each having a specific role. To elucidate these mechanisms, therefore, techniques able to engineer cells expressing different (ratios of) Notch ligands and receptors in a controlled manner should be adopted, and MPSs should enable long-term culture of cells in environments mimicking the structure, components, and stimuli of blood vessels.
Possible disease-mimicking cells might be obtained through synthetic biology and cellular engineering, which have already helped in elucidating Notch signaling networks and the impact of receptor–ligand specificity on signaling dynamics.49,50 Notch signaling dynamics is important for tissue development and morphogenesis,49,51,52 and Notch signaling dose and specific receptor–ligand interactions affect cell fate53,54 and physiology.20 Advances in synthetic biology, stem cell, and organoid technologies, as well as gene editing, combined with advanced microengineering of humanized model systems, will drive cutting-edge translational research.
Within vascular biology, three-dimensional (3D), ex vivo vascular networks have been useful to study the impact of Notch signaling dynamics on tissue morphogenesis and malformation,55 but these systems lack the impact of mechanics. Coupling dynamic molecular activity and mechanics to tissue pathology, to understand the interrelationship between biochemical regulation and mechanical impact on cardiovascular disease, requires real-time monitoring of molecular and cellular activities in humanized physiological systems and control over hemodynamic parameters. In vitro models with simplified mechanical characteristics or reduced tissue complexity, ex vivo microfluidic channels, and cellular strain platforms have all been used to study the mechanosensitivity of Notch in vascular cells.4,56–59 The complexity of these systems should be gradually increased to more closely mimic the physiological environment.
The hemodynamic environment of blood vessels consists of both shear stress (due to blood flow) and circumferential stretch (due to blood pressure). The tissue is layered, multicellular, and 3D. While simple microfluidic or strain devices can be employed to assess the impact of mechanics on Notch, more complex models and tissue-engineered constructs are a step closer toward mimicking the complexity in vivo. Perfused, self-organized vascular systems in 3D gels have helped in elucidating novel mechanisms of Notch in vascular barrier functions.60
We recently developed a vessel wall on a chip, mimicking the physiological cell composition, organization, and hemodynamic environment of the arterial vessel wall, to study the impact of simultaneous shear stress and strain on endothelial-VSMC signaling in tissue remodeling.61 A bioreactor that independently combined shear stress and stretch was developed to study the development of vascular grafts,62 and another bioreactor with a controlled, pressurized tissue system was developed to study the long-term effect of constant strain versus constant stress on tissue growth.63
In sum, several bioreactors and MPSs have already been developed and hold great promise in mimicking several aspects of genetic Notch cardiovascular disorders. The modeling of disease states on MPSs opens new avenues for understanding molecular mechanisms of pathologies and potential treatments of Notch-linked vascular disease. These models will provide insight into complexity, dose sensitivity, and receptor–ligand specificity of Notch signaling in cardiovascular tissue and especially in relation to changes in tissue mechanics and hemodynamics.
In Silico Models Bridging In Vitro and In Vivo Models
Although MPSs enable the investigation of human diseases with human donor cells and the investigation of isolated stimuli acting on them, in vitro findings remain challenging to translate to in vivo settings, where several biological processes interact, creating feedback loops with counterintuitive results. This conceptual gap between in vitro and in vivo models may be bridged by in silico models, providing digital twins of in vivo conditions and analytic tools for understanding the systemic consequences of single biological mechanisms.
In silico models have a wide range of applications within the investigation of vascular diseases and associated treatments. For example, computational fluid dynamics models can potentiate the optimization of in vitro systems64–66 and analysis of the effects of vascular network geometry on hemodynamics.67–69 Not only can these models compute the shear stress experienced by endothelial cells and other cell types in vitro70–72 or in human pathologic conditions73 but they can also be adopted to optimize surgical strategies for Notch-related diseases such as ALGS.74–76
Similarly, computational models are widely adopted to compute the local strain experienced by cardiovascular cells resulting from blood pressure-induced tissue deformation,77–79 both for idealized and patient-specific geometries.80,81 Coupled with this, an increasing number of modeling approaches include the possibility to simulate cell behavior in response to chemo-mechanical cues within cardiovascular tissues.82 Given the growing evidence of Notch mechanosensitivity, the capability of computational models to analyze cellular mechanical stimuli will be increasingly crucial for the study of Notch-related diseases. To this aim, these biomechanical models have to be coupled with in silico Notch models.
Due to the importance of Notch in numerous contexts, many in silico models of this signaling pathway have been proposed,83 usually to investigate the effects of different Notch ligand–receptor relationships on the resulting cellular phenotypic patterns.84–89 For example, modeling studies have uncovered that spatial patterns of cells with two alternating phenotypes can arise both from Notch lateral inhibition,84 defined as downregulation of Notch ligands in receiving cells after Notch activation, and from cis-inhibition,85 that is, the mutual exclusion of Notch receptor–ligand pairs within a single cell without Notch activation. Similarly, simulations have been crucial to understand the effects of filopodia,90,91 cell area and size,88 mechanics,4,92,93 and cell connectivity89 on Notch signaling dynamics and consequential tissue patterning. To our knowledge, there are currently no computational studies simulating Notch signaling in genetic Notch cardiovascular disorders. Nevertheless, we envision that combining and extending the features of the existing Notch in silico models will provide great versatility and opportunities for investigation of Notch-related diseases and for acceleration of targeted drug development and approval as it is also suggested and currently occurs in other fields.94,95
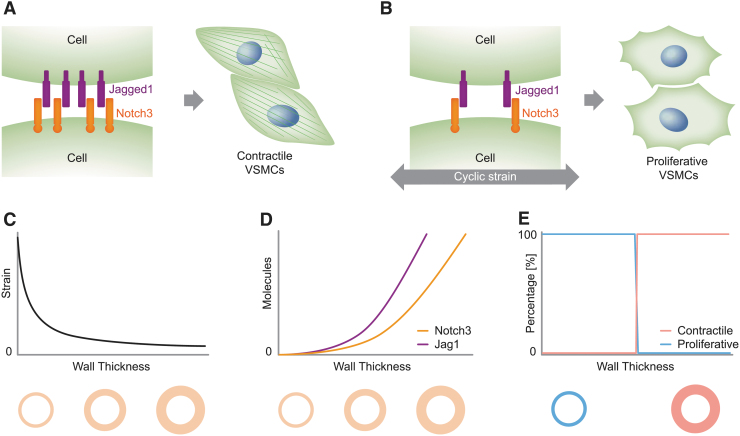
For example, our group has recently proposed a computational model for Notch signaling in blood vessels, which might have several applications in investigating CADASIL and ALGS.4 By accounting for Notch3-Jag1 signaling and their sensitivity to cyclic strain, this model identified Notch mechanosensitivity as a possible key factor of blood vessel homeostasis4 (see Fig. 3 for a scheme). The predictive potential of this model is supported by further experiments from our group.93 Future studies could adopt and extend this model to unravel the underlying mechanisms of CADASIL.
FIG. 3.
In silico models can translate in vitro findings to the in vivo setting. For example, in vitro studies have shown that the phenotype of VSMCs is strongly influenced by Notch signaling and mechanics: (A) high Notch activation corresponds to contractile VSMCs; (B) cyclic strain downregulates the expression of Notch3 and Jag1, and low levels of Notch correspond to proliferative VSMCs. By accounting for the fact that (C) the strain in arteries decreases with wall thickness and, consequently, (D) Notch3 and Jag1 expression levels increase with arterial thickness, (E) a recent computational model4 predicted that Notch mechanosensitivity can induce a phenotypic switch of VSMCs from proliferative to contractile for a specific wall thickness, thereby suggesting a mechanism that regulates the arterial homeostatic thickness (A and B are adapted from Ref. Loerakker and Ristori82).
In fact, the proposed Notch circuit model could be extended to investigate the possible effects that CADASIL-induced accumulation of the Notch3 extracellular domain96 has on Notch signaling and vascular homeostasis. Moreover, if coupled with simulations of blood vessel mechanics during aging, the model might shed light on the effects that age-related modifications have on Notch3-Jag1 signaling and, in turn, on the appearance of CADASIL symptoms in young adults.16 Finally, the Notch circuit model could be extended to include other Notch receptors, with different effects and behaviors, thereby enabling the investigation of ALGS dose sensitivity and Notch receptor specificity, which was discussed in the section on in vivo mouse models.
Conditional for their success, computational models need to be tightly coupled to experiments, which are strictly necessary for the model-informed development and validation. In fact, it is increasingly clear that each Notch ligand and receptor has its own specific role and regulation,49,50,54 which depend on the environment and, most likely, cell type. For example, Notch activation by Dll1 and Dll4 has different effects.49 Similarly, the activity of the enzymes, manic and lunatic fringe, is known to reduce Jag1-Notch2 binding97 and, on the opposite, increase Jag1-Notch1 binding events.98,99 On the one hand, accounting for these types of distinctions is not important for the quality of computational studies analyzing Notch signaling in general; on the other hand, it is crucial for the reliability of simulations of more specific biological phenomena, such as Notch-related diseases. Similarly, Notch3 activity might have location-dependent roles as it has opposite effects in the progression of arterial and pulmonary hypertension.100,101 Therefore, fully reliable in silico models can be attained only by informing their development with targeted experiments that analyze the specific cell type and specific Notch proteins. Future efforts in this field should thus aim at potentiating the interplay between experiments and simulations by establishing more rigorous methods for the calibration and validation of in silico models based on cell experiments.
Conclusion and Outlook
Unfortunately, current animal models of Notch-associated cardiovascular diseases are still not fully satisfactory. Although (in some cases) they have helped in understanding whether these pathologies result from loss- or gain-of-function Notch mutations, this information is still not enough for development of drugs targeting the disease instead of the symptoms. To this aim, fully understanding the molecular pathways involved is necessary. Achieving such understanding solely with animal models is challenging, if not impossible, not only because of their incapability to fully recapitulate Notch-related diseases but also because of their complexity. A further challenge stems from potential species differences. In general, the insufficient contribution of animal models is also highlighted by the disproportionate number of drugs that positively pass animal trials, but fail to reach the clinical setting due to negative results in humans.102 Alternative and complementary strategies are therefore necessary.
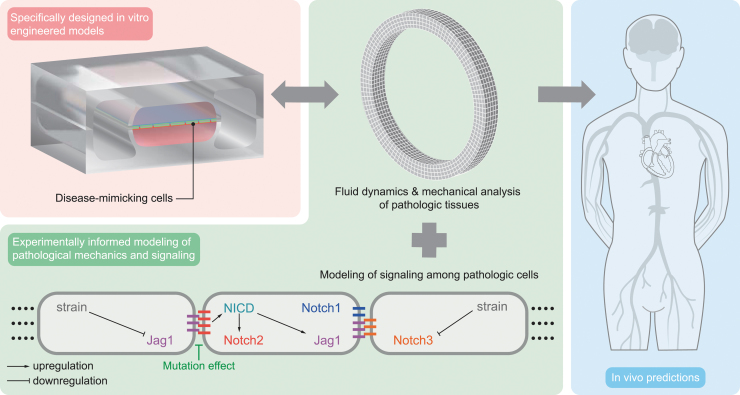
We expect that the combination between MPSs and computational models will significantly aid our understanding of Notch signaling mechanisms in cardiovascular disorders and will potentiate the development of targeted treatments (Fig. 4). MPSs provide controlled environments mimicking isolated features of human physiology, where patient-derived or other human cells can be directly cultured and relatively easily tested and imaged. Computational models can integrate findings from different experiments and predict their consequences in vivo, where multiple phenomena interact over a long time period. Therefore, these two approaches complement each other and could lead to breakthroughs in the field of Notch-related cardiovascular diseases.
FIG. 4.
Example of workflow. Specifically designed in vitro engineered models are adopted to mimic the in vivo environment and test disease-mimicking cells. The in vitro experiments inform the development of computational models of tissue mechanics and Notch signaling as perturbed by the genetic mutation under investigation. The computational model predictions can be validated with further in vitro experiments, completing the cycle of model information and validation. Ideally, this process should lead to increased model credibility and reliable in vivo predictions (the scheme of the microfluidic device is adapted from Ref. van Engeland et al.61).
Future MPSs should aim at more closely mimicking the complexity of human tissues and conditions while keeping their advantages in terms of control. Further complexity and physiological relevance may be achieved by including more features of the systemic environment, such as gradients of nutrients, gasses, cytokines, hormones, circulating cells, and other relevant cell types, and by tuning the composition and organization of the extracellular matrix. Ideally, this should be performed following a modular design so that complexity can be increased or decreased depending on the research question. Such an approach should also be followed by computational models to increase their versatility and enable their application in different contexts.
Importantly, given the long timescale features of Notch-related diseases and tissue morphogenesis, growth, and remodeling more in general, both MPSs and computational models should reach the potential to recapitulate long-term organ function, enabling long-term cell culture on the one hand and long-term simulations with contained computational costs on the other hand. Reaching these goals remains challenging and requires engineering skills that are not yet widely accessible. To fill this gap, we need to develop new tools and a new framework where expertise in cell biology, molecular biomedicine, engineering, and computational biology is combined. To facilitate communication and the exchange of information and tools between these different disciplines, common hybrid international conferences should be organized and strategies should be optimized to increase the accessibility of tissue chip technology and computational models. For this latter aim, these technologies should be accurately validated and commercialized for community-wide access.
In conclusion, the coupling and further development of MPSs and computational models may accelerate the investigation of genetic Notch cardiovascular disorders and could provide new, personalized medicine approaches as drugs may be tested directly on patient-derived cells within MPSs mimicking the human physiology and disease. The potential of this coupling is currently largely unexplored in this field and therefore, despite the challenges ahead, we envision that the interplay between these two approaches will lead to accelerated drug discovery and an increased approval rate, in addition to facilitating the transition from care, where only symptoms are treated, to cure, where disease causes are targeted.
Acknowledgment
The ICMS Animation Studio is gratefully acknowledged for providing the artwork.
Disclosure Statement
No competing financial interests exist.
Funding Information
This work has been supported by the Academy of Finland, project numbers 218062 and 33041, and the ERC-CoG 771168-ForceMorph to C.M.S., by the Swedish Cultural Foundation in Finland to M.S., and by the research program, NWO Rubicon, which is (partly) financed by the Dutch Research Council (NWO), with project number 019.183EN.025 to T.R.
References
- 1. del Monte, G., Casanova, J.C., Guadix, J.A., et al. Differential Notch signaling in the epicardium is required for cardiac inflow development and coronary vessel morphogenesis. Circ Res 108, 824, 2011 [DOI] [PubMed] [Google Scholar]
- 2. Luxán G, D'Amato, G., MacGrogan, D., and de la Pompa, J.L.. Endocardial Notch signaling in cardiac development and disease. Circ Res 118, e1, 2016 [DOI] [PubMed] [Google Scholar]
- 3. Mašek, J., and Andersson, E.R.. The developmental biology of genetic Notch disorders. Development 144, 1743, 2017 [DOI] [PubMed] [Google Scholar]
- 4. Loerakker, S., Stassen, O.M.J.A., Ter Huurne, F.M., Boareto, M., Bouten, C.V.C., and Sahlgren, C.M.. Mechanosensitivity of Jagged-Notch signaling can induce a switch-type behavior in vascular homeostasis. Proc Natl Acad Sci U S A 115, E3682, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dou, G.-R., Wang, Y.-C., Hu, X.-B., et al. RBP-J, the transcription factor downstream of Notch receptors, is essential for the maintenance of vascular homeostasis in adult mice. FASEB J 22, 1606, 2008 [DOI] [PubMed] [Google Scholar]
- 6. Chapman, G., Moreau, J.L.M., Eddie, I.P., et al. Functional genomics and gene-environment interaction highlight the complexity of congenital heart disease caused by Notch pathway variants. Hum Mol Genet 29, 566, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Vandriel, S.M., Ichord, R.N., and Kamath, B.M.. Vascular manifestations in alagille syndrome. In: Kamath, B., and Loomes, K., eds. Alagille Syndrome. Cham, Switzerland: Springer, 2018, pp. 91–102 [Google Scholar]
- 8. Lykavieris, P., Crosnier, C., Trichet, C., Meunier-Rotival, M., and Hadchouel, M.. Bleeding tendency in children with Alagille syndrome. Pediatrics 111, 167, 2003 [DOI] [PubMed] [Google Scholar]
- 9. Emerick, K.M., Rand, E.B., Goldmuntz, E., Krantz, I.D., Spinner, N.B., and Piccoli, D.A.. Features of Alagille syndrome in 92 patients: frequency and relation to prognosis. Hepatology 29, 822, 1999 [DOI] [PubMed] [Google Scholar]
- 10. Garg, V., Muth, A.N., Ransom, J.F., et al. Mutations in NOTCH1 cause aortic valve disease. Nature 437, 270, 2005 [DOI] [PubMed] [Google Scholar]
- 11. Southgate, L., Sukalo, M., Karountzos, A.S.V., et al. Haploinsufficiency of the NOTCH1 receptor as a cause of adams-oliver syndrome with variable cardiac anomalies. Circ Cardiovasc Genet 8, 572, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Meester, J.A.N., Southgate, L., Stittrich, A.-B., et al. Heterozygous loss-of-function mutations in DLL4 cause Adams-Oliver Syndrome. Am J Hum Genet 97, 475, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hassed, S.J., Wiley, G.B., Wang, S., et al. RBPJ mutations identified in two families affected by Adams-Oliver syndrome. Am J Hum Genet 91, 391, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Meester, J.A.N., Verstraeten, A., Alaerts, M., Schepers, D., Van Laer, L., and Loeys, B.L.. Overlapping but distinct roles for NOTCH receptors in human cardiovascular disease. Clin Genet 95, 85, 2019 [DOI] [PubMed] [Google Scholar]
- 15. Stittrich, A.-B., Lehman, A., Bodian, D.L., et al. Mutations in NOTCH1 cause Adams-Oliver syndrome. Am J Hum Genet 95, 275, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang, M.M. CADASIL. Handb Clin Neurol 148, 733, 2018 [DOI] [PubMed] [Google Scholar]
- 17. Xue, Y., Gao, X., Lindsell, C.E., et al. Embryonic lethality and vascular defects in mice lacking the Notch ligand Jagged1. Hum Mol Genet 8, 723, 1999 [DOI] [PubMed] [Google Scholar]
- 18. Swiatek, P.J., Lindsell, C.E., del Amo, F.F., Weinmaster, G., and Gridley, T.. Notch1 is essential for postimplantation development in mice. Genes Dev 8, 707, 1994 [DOI] [PubMed] [Google Scholar]
- 19. Hamada, Y., Kadokawa, Y., Okabe, M., Ikawa, M., Coleman, J.R., and Tsujimoto, Y.. Mutation in ankyrin repeats of the mouse Notch2 gene induces early embryonic lethality. Development 126, 3415, 1999 [DOI] [PubMed] [Google Scholar]
- 20. Duarte, A., Hirashima, M., Benedito, R., et al. Dosage-sensitive requirement for mouse Dll4 in artery development. Genes Dev 18, 2474, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Krebs, L.T., Shutter, J.R., Tanigaki, K., Honjo, T., Stark, K.L., and Gridley, T.. Haploinsufficient lethality and formation of arteriovenous malformations in Notch pathway mutants. Genes Dev 18, 2469, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gale, N.W., Dominguez, M.G., Noguera, I., et al. Haploinsufficiency of delta-like 4 ligand results in embryonic lethality due to major defects in arterial and vascular development. Proc Natl Acad Sci U S A 101, 15949, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stassen, O.M.J.A., Ristori, T., and Sahlgren, C.M.. Notch in mechanotransduction: from molecular mechanosensitivity to tissue mechanostasis. J Cell Sci 21;133(24):jcs250738, 2020 (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McCright, B., Lozier, J., and Gridley, T.. A mouse model of Alagille syndrome: Notch2 as a genetic modifier of Jag1 haploinsufficiency. Development 129, 1075, 2002 [DOI] [PubMed] [Google Scholar]
- 25. Tsai, H., Hardisty, R.E., Rhodes, C., et al. The mouse slalom mutant demonstrates a role for Jagged1 in neuroepithelial patterning in the organ of Corti. Hum Mol Genet 10, 507, 2001 [DOI] [PubMed] [Google Scholar]
- 26. Vrijens, K., Thys, S., De Jeu, M.T., et al. Ozzy, a Jag1 vestibular mouse mutant, displays characteristics of Alagille syndrome. Neurobiol Dis 24, 28, 2006 [DOI] [PubMed] [Google Scholar]
- 27. Andersson, E.R., Chivukula I V, Hankeova, S., et al. Mouse model of Alagille syndrome and mechanisms of Jagged1 missense mutations. Gastroenterology 154, 1080, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Thakurdas, S.M., Lopez, M.F., Kakuda, S., et al. Jagged1 heterozygosity in mice results in a congenital cholangiopathy which is reversed by concomitant deletion of one copy of Poglut1 (Rumi). Hepatology 63, 550, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Adams, J.M., Huppert, K.A., Castro, E.C., et al. Sox9 is a modifier of the liver disease severity in a mouse model of Alagille syndrome. Hepatology 71, 1331, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Monet-Leprêtre, M., Bardot, B., Lemaire, B., et al. Distinct phenotypic and functional features of CADASIL mutations in the Notch3 ligand binding domain. Brain 132(Pt 6), 1601, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ruchoux, M.M., Domenga, V., Brulin, P., et al. Transgenic mice expressing mutant Notch3 develop vascular alterations characteristic of cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Am J Pathol 162, 329, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ayata, C. CADASIL: experimental insights from animal models. Stroke 41(10 Suppl), S129, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Joutel, A., Monet-Leprêtre, M., Gosele, C., et al. Cerebrovascular dysfunction and microcirculation rarefaction precede white matter lesions in a mouse genetic model of cerebral ischemic small vessel disease. J Clin Invest 120, 433, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Neves, K.B., Harvey, A.P., Moreton, F., et al. ER stress and Rho kinase activation underlie the vasculopathy of CADASIL. JCI insight 4, e131344, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ling, C., Liu, Z., Song, M., et al. Modeling CADASIL vascular pathologies with patient-derived induced pluripotent stem cells. Protein Cell 10, 249, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rutten, J.W., Boon, E.M.J., Liem, M.K., et al. Hypomorphic NOTCH3 alleles do not cause CADASIL in humans. Hum Mutat 34, 1486, 2013 [DOI] [PubMed] [Google Scholar]
- 37. Moccia, M., Mosca, L., Erro, R., et al. Hypomorphic NOTCH3 mutation in an Italian family with CADASIL features. Neurobiol Aging 36, 547.e5, 2015 [DOI] [PubMed] [Google Scholar]
- 38. Nigam, V., and Srivastava, D.. Notch1 represses osteogenic pathways in aortic valve cells. J Mol Cell Cardiol 47, 828, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Nus, M., MacGrogan, D., Martínez-Poveda, B., et al. Diet-induced aortic valve disease in mice haploinsufficient for the Notch pathway effector RBPJK/CSL. Arterioscler Thromb Vasc Biol 31, 1580, 2011 [DOI] [PubMed] [Google Scholar]
- 40. Garg, V. Molecular genetics of aortic valve disease. Curr Opin Cardiol 21, 180, 2006 [DOI] [PubMed] [Google Scholar]
- 41. Chang, L., Noseda, M., Higginson, M., et al. Differentiation of vascular smooth muscle cells from local precursors during embryonic and adult arteriogenesis requires Notch signaling. Proc Natl Acad Sci U S A 109, 6993, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Patel, M.S., Taylor, G.P., Bharya, S., et al. Abnormal pericyte recruitment as a cause for pulmonary hypertension in Adams-Oliver syndrome. Am J Med Genet A 129A, 294, 2004 [DOI] [PubMed] [Google Scholar]
- 43. Bhatia, S.N., and Ingber, D.E.. Microfluidic organs-on-chips. Nat Biotechnol 32, 760, 2014 [DOI] [PubMed] [Google Scholar]
- 44. Rare Disease Database. https://rarediseases.org/for-patients-and-families/information-resources/rare-disease-information/ Accessed October29, 2020
- 45. Global Genes. Rare diseases: facts and statistics. https://globalgenes.org/rare-facts/ Accessed October29, 2020
- 46. Low, L.A., and Tagle, D.A.. Tissue Chips to aid drug development and modeling for rare diseases. Expert Opin orphan drugs 4, 1113, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Atchison, L., Abutaleb, N.O., Snyder-Mounts, E., et al. iPSC-derived endothelial cells affect vascular function in a tissue-engineered blood vessel model of Hutchinson-Gilford Progeria syndrome. Stem Cell Rep 14, 325, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wang, G., McCain, M.L., Yang, L., et al. Modeling the mitochondrial cardiomyopathy of Barth syndrome with induced pluripotent stem cell and heart-on-chip technologies. Nat Med 20, 616, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Nandagopal, N., Santat, L.A., LeBon, L., Sprinzak, D., Bronner, M.E., and Elowitz, M.B.. Dynamic ligand discrimination in the Notch signaling pathway. Cell 172, 869, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Tveriakhina, L., Schuster-Gossler, K., Jarrett, S.M., et al. The ectodomains determine ligand function in vivo and selectivity of DLL1 and DLL4 toward NOTCH1 and NOTCH2 in vitro. Elife 7, e40045, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Shimojo, H., Ohtsuka, T., and Kageyama, R.. Oscillations in notch signaling regulate maintenance of neural progenitors. Neuron 58, 52, 2008 [DOI] [PubMed] [Google Scholar]
- 52. Theodoris, C.V., Li, M., White, M.P., et al. Human disease modeling reveals integrated transcriptional and epigenetic mechanisms of NOTCH1 haploinsufficiency. Cell 160, 1072, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mazzone, M., Selfors, L.M., Albeck, J., et al. Dose-dependent induction of distinct phenotypic responses to Notch pathway activation in mammary epithelial cells. Proc Natl Acad Sci U S A 107, 5012, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Benedito, R., Roca, C., Sörensen, I., et al. The Notch ligands Dll4 and Jagged1 have opposing effects on angiogenesis. Cell 137, 1124, 2009 [DOI] [PubMed] [Google Scholar]
- 55. Ubezio, B., Blanco, R.A., Geudens, I., et al. Synchronization of endothelial Dll4-Notch dynamics switch blood vessels from branching to expansion. Elife 5, 1, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Mack, J.J., Mosqueiro, T.S., Archer, B.J., et al. NOTCH1 is a mechanosensor in adult arteries. Nat Commun 8, 1620, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Driessen, R.C.H., Stassen, O.M.J.A., Sjöqvist, M., et al. Shear stress induces expression, intracellular reorganization and enhanced Notch activation potential of Jagged1. Integr Biol (Camb) 10, 719, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Souilhol, C., Li, X., Canham, L., et al. JAG1-NOTCH4 mechanosensing drives atherosclerosis. bioRxiv 2020. [Epub ahead of print]; DOI: 10.1101/2020.05.15.097931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Sonnen, K.F., Lauschke, V.M., Uraji, J., et al. Modulation of phase shift between Wnt and Notch signaling oscillations controls mesoderm segmentation. Cell 172, 1079.e12, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Polacheck, W.J., Kutys, M.L., Yang, J., et al. A non-canonical Notch complex regulates adherens junctions and vascular barrier function. Nature 552, 258, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. van Engeland, N.C.A., Pollet, A.M.A.O., den Toonder, J.M.J., Bouten, C.V.C., Stassen, O.M.J.A., and Sahlgren, C.M.. A biomimetic microfluidic model to study signalling between endothelial and vascular smooth muscle cells under hemodynamic conditions. Lab Chip 18, 1607, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. van Haaften, E.E., Wissing, T.B., Rutten, M.C.M., et al. Decoupling the effect of shear stress and stretch on tissue growth and remodeling in a vascular graft. Tissue Eng Part C Methods 24, 418, 2018 [DOI] [PubMed] [Google Scholar]
- 63. van Kelle, M.A.J., Oomen PJA, Bulsink, J.A., et al. A bioreactor to identify the driving mechanical stimuli of tissue growth and remodeling. Tissue Eng Part C Methods 23, 377, 2017 [DOI] [PubMed] [Google Scholar]
- 64. Hutmacher, D.W., and Singh, H.. Computational fluid dynamics for improved bioreactor design and 3D culture. Trends Biotechnol 26, 166, 2008 [DOI] [PubMed] [Google Scholar]
- 65. Mehrian, M., Guyot, Y., Papantoniou, I., et al. Maximizing neotissue growth kinetics in a perfusion bioreactor: an in silico strategy using model reduction and Bayesian optimization. Biotechnol Bioeng 115, 617, 2018 [DOI] [PubMed] [Google Scholar]
- 66. Zhao, F., van Rietbergen, B., Ito, K., and Hofmann, S.. Flow rates in perfusion bioreactors to maximise mineralisation in bone tissue engineering in vitro. J Biomech 79, 232, 2018 [DOI] [PubMed] [Google Scholar]
- 67. LaDisa, J.F.J., Olson, L.E., Douglas, H.A., Warltier, D.C., Kersten, J.R., and Pagel, P.S.. Alterations in regional vascular geometry produced by theoretical stent implantation influence distributions of wall shear stress: analysis of a curved coronary artery using 3D computational fluid dynamics modeling. Biomed Eng Online 5, 40, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Ghaffari, S., Leask, R.L., and Jones, E.A.V.. Simultaneous imaging of blood flow dynamics and vascular remodelling during development. Development 142, 4158, 2015 [DOI] [PubMed] [Google Scholar]
- 69. Vardhan, M., Gounley, J., Chen, S.J., Kahn, A.M., Leopold, J.A., and Randles, A.. The importance of side branches in modeling 3D hemodynamics from angiograms for patients with coronary artery disease. Sci Rep 9, 1, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Guyot, Y., Smeets, B., Odenthal, T., et al. Immersed boundary models for quantifying flow-induced mechanical stimuli on stem cells seeded on 3D scaffolds in perfusion bioreactors. PLoS Comput Biol 12, e1005108, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Melke, J., Zhao, F., van Rietbergen, B., Ito, K., and Hofmann, S.. Localisation of mineralised tissue in a complex spinner flask environment correlates with predicted wall shear stress level localisation. Eur Cell Mater 36, 57, 2018 [DOI] [PubMed] [Google Scholar]
- 72. Driessen, R., Zhao, F., Hofmann, S., Bouten, C., Sahlgren, C., and Stassen, O.. Computational characterization of the dish-in-a-dish, a high yield culture platform for endothelial shear stress studies on the orbital shaker. Micromachines 11, 1, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Ardakani, V.G., Tu, X., Gambaruto, A.M., et al. Near-wall flow in cerebral aneurysms. Fluids 4, 1, 2019 [Google Scholar]
- 74. Yang, W., Feinstein, J.A., and Vignon-Clementel, I.E.. Adaptive outflow boundary conditions improve post-operative predictions after repair of peripheral pulmonary artery stenosis. Biomech Model Mechanobiol 15, 1345, 2016 [DOI] [PubMed] [Google Scholar]
- 75. Yang, W., Hanley, F.L., Chan, F.P., Marsden, A.L., Vignon-Clementel, I.E., and Feinstein, J.A.. Computational simulation of postoperative pulmonary flow distribution in Alagille patients with peripheral pulmonary artery stenosis. Congenit Heart Dis 13, 241, 2018 [DOI] [PubMed] [Google Scholar]
- 76. Silva Vieira, M., Arthurs, C.J., Hussain, T., Razavi, R., and Figueroa, C.A.. Patient-specific modeling of right coronary circulation vulnerability post-liver transplant in Alagille's syndrome. PLoS One 13, 1, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Holzapfel, G.A., and Ogden R.W.. Constitutive modelling of arteries. Proc R Soc A 466, 1551, 2010 [Google Scholar]
- 78. Oomen, P.J.A., Loerakker, S., van Geemen, D., et al. Age-dependent changes of stress and strain in the human heart valve and their relation with collagen remodeling. Acta Biomater 29, 161, 2016 [DOI] [PubMed] [Google Scholar]
- 79. Sacks, M.S., Drach, A., Lee, C.-H., et al. On the simulation of mitral valve function in health, disease, and treatment. J Biomed Eng 141,0708041, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Mansi, T., Voigt, I., Georgescu, B., et al. An integrated framework for finite-element modeling of mitral valve biomechanics from medical images: application to MitralClip intervention planning. Med Image Anal 16, 1330, 2012 [DOI] [PubMed] [Google Scholar]
- 81. van Disseldorp, E.M.J., Petterson, N.J., Rutten, M.C.M., van de Vosse, F.N., van Sambeek, M.R.H.M., and Lopata, R.G.P.. Patient specific wall stress analysis and mechanical characterization of abdominal aortic aneurysms using 4D ultrasound. Eur J Vasc Endovasc Surg 52, 635, 2016 [DOI] [PubMed] [Google Scholar]
- 82. Loerakker, S., and Ristori, T.. Computational modeling for cardiovascular tissue engineering: the importance of including cell behavior in growth and remodeling algorithms. Curr Opin Biomed Eng 15, 1, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Binshtok, U., and Sprinzak, D.. Modeling the Notch response. Adv Exp Med Biol 1066, 79, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Collier, J.R., Monk, N.A., Maini, P.K., and Lewis, J.H.. Pattern formation by lateral inhibition with feedback: a mathematical model of delta-notch intercellular signalling. J Theor Biol 183, 429, 1996 [DOI] [PubMed] [Google Scholar]
- 85. Sprinzak, D., Lakhanpal, A., Lebon, L., et al. Cis-interactions between Notch and Delta generate mutually exclusive signalling states. Nature 465, 86, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Boareto, M., Jolly, M.K., Lu, M., Onuchic, J.N., Clementi, C., and Ben-Jacob, E.. Jagged–Delta asymmetry in Notch signaling can give rise to a Sender/Receiver hybrid phenotype. Proc Natl Acad Sci U S A 112, E402, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Luna-Escalante, J.C., Formosa-Jordan, P., and Ibañes, M.. Redundancy and cooperation in Notch intercellular signaling. Development 145, dev154807, 2018 [DOI] [PubMed] [Google Scholar]
- 88. Shaya, O., Binshtok, U., Hersch, M., et al. Cell-cell contact area affects Notch signaling and Notch-dependent patterning. Dev Cell 40, 505, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Ristori, T., Stassen, O.M.J.A., Sahlgren, C.M., and Loerakker, S.. Lateral induction limits the impact of cell connectivity on Notch signaling in arterial walls. Int J Numer Method Biomed Eng 36, e3323, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Bentley, K., Gerhardt, H., and Bates, P.A.. Agent-based simulation of notch-mediated tip cell selection in angiogenic sprout initialisation. J Theor Biol 250, 25, 2008 [DOI] [PubMed] [Google Scholar]
- 91. Cohen, M., Georgiou, M., Stevenson, N.L., Miodownik, M., and Baum, B.. Dynamic filopodia transmit intermittent Delta-Notch signaling to drive pattern refinement during lateral inhibition. Dev Cell 19, 78, 2010 [DOI] [PubMed] [Google Scholar]
- 92. Riahi, R., Sun, J., Wang, S., Long, M., Zhang, D.D., and Wong, P.K.. Notch1-Dll4 signalling and mechanical force regulate leader cell formation during collective cell migration. Nat Commun 6, 1, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. van Engeland, N.C.A., Suarez Rodriguez, F., Rivero-Müller, A., et al. Vimentin regulates Notch signaling strength and arterial remodeling in response to hemodynamic stress. Sci Rep 9, 12415, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Kameo, Y., Miya, Y., Hayashi, M., Nakashima, T., and Adachi, T.. In silico experiments of bone remodeling explore metabolic diseases and their drug treatment. Sci Adv 6, eaax0938, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Geris, L. In silico tools predict effects of drugs on bone remodelling. Nat Rev Rheumatol 16, 475, 2020 [DOI] [PubMed] [Google Scholar]
- 96. Joutel, A., Andreux, F., Gaulis, S., et al. The ectodomain of the Notch3 receptor accumulates within the cerebrovasculature of CADASIL patients. J Clin Invest 105, 597, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Shimizu, K., Chiba, S., Saito, T., Kumano, K., Takahashi, T., and Hirai, H.. Manic fringe and lunatic fringe modify different sites of the Notch2 extracellular region, resulting in different signaling modulation. J Biol Chem 276, 25753, 2001 [DOI] [PubMed] [Google Scholar]
- 98. Yang, L.T., Nichols, J.T., Yao, C., Manilay, J.O., Robey, E.A., and Weinmaster, G.. Fringe glycosyltransferases differentially modulate Notch1 proteolysis induced by Delta1 and Jagged1. Mol Biol Cell 16, 927, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Kakuda, S., Haltiwanger, R.S., Kakuda, S., and Haltiwanger, R.S.. Short article deciphering the fringe-mediated Notch code: identification of activating and inhibiting sites allowing discrimination between ligands short article deciphering the fringe-mediated Notch code: identification of activating and inhibiting sit. Dev Cell 40, 193, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Li, X., Zhang, X., Leathers, R., et al. Notch3 signaling promotes the development of pulmonary arterial hypertension. Nat Med 15, 1289, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Boulos, N., Helle, F., Dussaule, J.-C., et al. Notch3 is essential for regulation of the renal vascular tone. Hypertens (Dallas, Tex 1979) 57, 1176, 2011 [DOI] [PubMed] [Google Scholar]
- 102. Norman GA Van. Limitations of animal studies for predicting toxicity in clinical trials. JACC Basic Transl Sci 4, 845, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]