Abstract
Background: Shorter sleep duration and lower sleep quality have been previously associated with greater obesity risk among adult samples. Food insecurity has also been found to impact sleep patterns and obesity. Yet few studies have explored associations between sleep, food insecurity, and obesity in adolescent populations, who may have more irregular sleep patterns. Thus, the objectives of this study were to determine associations between measures of sleep, food insecurity, and weight status.
Methods: Data were obtained from the Family Life, Activity, Sun, Health, and Eating (FLASHE) Study, an online cross-sectional study of parent and adolescent (12–17-year old) dyads. Participants were drawn from a Consumer Opinion Panel representative of the general population of the United States with respect to sex, education, income, age, household size, and region. First, multinomial logistic regression analyses were conducted to determine associations between sleep measures (adolescent-reported average nighttime sleep duration, having a regular bedtime, and having difficulty staying asleep), food insecurity (a validated two-item parent-reported measure), and weight status (being underweight, of healthy weight, overweight, and obese). Weight status was based upon adolescent BMI z-scores using Centers for Disease Control and Prevention growth charts using information from parent report of adolescent height and weight and adolescent-reported age and sex among adolescents (N = 1544). Conditional process models were also fitted to the data to determine whether food insecurity moderates the associations between sleep measures and weight status, and to determine whether the association between food insecurity and weight status is mediated by average sleep duration.
Results: Compared to those with food security, a greater percentage of those with food insecurity reported having difficulties staying asleep and a longer average sleep duration. Multinomial logistic regression models demonstrated that having a regular bedtime was associated with lower odds of having obesity, having difficulties staying asleep was associated with greater odds of being underweight, and having food insecurity was associated with greater odds of being overweight. Conditional process models demonstrated that food insecurity did not moderate associations between sleep measures and weight status and that average nighttime sleep duration did not mediate the association between food insecurity and weight status.
Conclusions: This is one of the first studies to examine associations between sleep, food insecurity, and weight status among adolescents. Results provide additional support for the need to uncover mechanisms for how sleep and food insecurity affect pediatric obesity using longitudinal data.
Keywords: adolescents, food insecurity, obesity, sleep, weight status
Introduction
Pediatric obesity is a growing public health concern. Rates of pediatric obesity are increasing and have had serious consequences on the health care system1 and the health and well-being of individuals and society.2 Recent estimates suggest that more than 330 million children and adolescents between the ages of 5 and 19 years worldwide are overweight (i.e., BMI >85th percentile and <95th percentile) or obese (i.e., BMI >95th percentile on sex- and age-specific growth charts).3 Pediatric obesity is associated with increased susceptibility to psychological disorders (e.g., depression), chronic health disorders (e.g., cardiovascular disease), and a higher risk of 13 types of cancers in adulthood.4–6 Importantly, pediatric obesity prevalence is the highest among adolescents (12–19 years of age) at 20.6%, relative to 13.9% of 2–5 year olds and 18.4% of 6–11 year olds.7 Adolescence is an especially critical period of development,8 marked by psychological, behavioral, and emotional shifts with direct and indirect implications for weight.9 It is also a time during which personal autonomy for many health habits are formed, which influence metabolic and physiological changes that track into adulthood.10,11 Given the strong associations between adolescent and adult obesity,12 obtaining a better understanding on how different factors interact to influence pediatric obesity—especially during adolescence—is necessary for prevention of obesity and obesity-associated morbidities in adulthood.
Prior literature suggests that enhancing sleep may be an effective strategy toward preventing and treating pediatric obesity.13 While rates of pediatric obesity have increased, nocturnal sleep duration has continued to decline.14 Furthermore, adolescents are not achieving sufficient sleep length,15 which is recommended to be between 8 and 10 hours per night.16 Recent meta-analyses suggest that adolescents not meeting recommended sleep guidelines are at 58%–89% increased risk for developing overweight/obesity.17 Short sleep duration may influence obesity through physiological and behavioral changes occurring in response to sleep deprivation. For example, experimental studies involving adult participants suggest that sleep deprivation may lead to endocrine and hormonal changes associated with increased hunger and appetite, motivation to eat, and food intake.18,19 Shorter sleep duration may also be associated with obesity through increases in higher energy intake from snacks20 and main meals.21
Another important factor that may contribute to the development of obesity, especially among those from lower socioeconomic backgrounds, is food insecurity.22 Food insecurity is defined as a disruption of food intake or eating patterns because of a lack of money or other resources.23 Food insecurity is linked to increased weight in adulthood, and higher rates of being overweight and obese are found among adults from lower-income backgrounds experiencing food insecurity.24–28 Among adult samples, food insecurity is associated with poorer sleep outcomes,29 as well as greater obesity risk.30 One study utilizing data from the National Health Interview Survey found a positive and direct relationship between food insecurity and short sleep duration and trouble falling asleep, among adults with obesity. In the same study, having trouble falling asleep and short sleep duration were found to partially mediate the relationship between food insecurity and obesity.31 Results from other studies suggest that food insecurity in adulthood may also be associated with poorer sleep quality.29,32–34 For example, a recent study of college students demonstrates that food insecurity is related to fewer days of enough sleep and increased BMI. This study also found that food insecurity was related to fewer days of enough sleep, which was related to increased BMI.35
However, the relationship between food insecurity and sleep may not be limited to the developmental period of emerging adulthood. One study of preschool-aged children attending Head Start in Pennsylvania found that food insecurity was associated with suboptimal sleep quality, but not sleep duration.36 Food insecurity may also have differential effects by sex, as one study using data from the National Longitudinal Study of Adolescent Health found that food insecurity was associated with increased BMI in young adult women, but not men.30 Another study using data from the third National Health and Nutrition Examination Survey (NHANES III) found that food insufficiency was negatively associated with overweight status in younger girls.37
Meanwhile, results from prior studies investigating the relationship between food insecurity and obesity among children and adolescents are mixed.38–43 Data from the National Health and Nutrition Examination Survey (1992–2002) suggest that associations may differ according to age, as children from food-insecure households are more likely to be at risk for being overweight if they are between the ages of 12 and 17 years.41 One study of predominantly Hispanic, fifth-grade children and their mothers found that food insecurity was negatively associated with child BMI, but not associated with food intake.39 Another study of adolescents 10–15 years of age and their mothers who participated in the Welfare, Children, and Families: A Three-City Study found no direct association between food insecurity and overweight or obesity.44
Collectively, the existing literature has focused on associations between sleep and obesity or food insecurity and obesity separately, but has not examined the associations between sleep, food insecurity, and obesity all together. In addition, much of the existing literature focuses on samples of adults or younger children, while less is known about the developmental period of adolescence. Therefore, the objective of this study is to determine (1) the associations between sleep characteristics (i.e., average nighttime sleep duration, having a regular bedtime, and having difficulties staying asleep) and weight status (i.e., being underweight, of normal weight, overweight, and obese), (2) whether food insecurity moderates the association between sleep measures and weight status, and (3) whether the association between food insecurity and weight status is mediated by sleep. Since prior studies have suggested that associations between sleep, food insecurity, and obesity may differ by sex, we also sought to determine whether the associations between sleep measures, food insecurity, and weight status were moderated by sex.
Methods
Data Source and Study Procedures
Data were obtained from the Family Life, Activity, Sun, Health, and Eating (FLASHE) Study. FLASHE is a cross-sectional, internet-based study that was conducted by the National Cancer Institute between April and October 2014. The sample was drawn from a Consumer Opinion Panel representative of the United States population, based upon sex, education, income, age, household size, and region. FLASHE contains responses to survey questions from parent-child dyads, focused on diet, physical activity, sleep, sun safety, and tobacco use, as well as questions related to household characteristics and sociodemographic data.45 More detailed information on recruitment, enrollment, and survey response are reported elsewhere.46,47
Briefly, a parent/caregiver and their adolescent (12–17 years of age) were enrolled and then randomly selected to a Survey-Only group (i.e., received the web-based survey instruments only) or a Motion Study group (i.e., received the same web-based surveys plus an accelerometer worn by the adolescent). Approximately 39% (or N = 1945 dyads) of 5027 dyads who were invited to participate in FLASHE were enrolled.45 Parents were asked to complete informed consent forms for their participation and their adolescents' participation. Adolescents were asked to complete an assent form for their participation. A total of 1890 parent-adolescent dyads had complete survey data available. Only adolescents who had information on BMI and sleep measures were included in our analytic sample (N = 1544). All FLASHE data collection materials and procedures were reviewed and approved by the US Government's Office of Management and Budget, National Cancer Institute (NCI)'s Special Studies Institutional Review Board, and Westat's Institutional Review Board. Study procedures were conducted in accordance with ethical standards set by the Helsinki Declaration of 1975.
Measures
Sleep
In this study, we investigated three adolescent-reported sleep characteristics: average nighttime sleep duration, having a regular bedtime, and having difficulties staying asleep. Average nighttime sleep duration (in hours) was determined by subtracting morning wake time from bedtime. Having a regular bedtime was measured by the following question: “Do you have a regular bedtime?” with responses being yes or no. Difficulty staying asleep was measured by question: “Do you generally have trouble staying asleep at night?” with responses being yes or no.
Weight status
Weight status was categorized into being underweight, of healthy weight, overweight, and obese. This was determined by calculating adolescent BMI z-score using CDC growth charts, based upon parent report of the adolescent's height and weight and adolescent-reported age and sex. Weight status category was defined by the percentile range, as follows: underweight, <5th percentile; healthy weight, 5th percentile to <85th percentile; overweight, 85th to <95th percentile; and obese, 95th percentile or greater.48
Food insecurity
Food insecurity was measured using a validated, two-item screener.49 Parents were asked to indicate whether the following statements were never true, sometimes true, or often true: “Within the past 12 months, we worried whether our food would run out before we got money to buy more” and “Within the past 12 months, the food we bought just didn't last and we didn't have money to get more.” Each of these parent-reported items was dichotomized [i.e., never true (0) vs. sometimes true/often true (1)]. Affirmative (i.e., sometimes true/often true) response to either question was indicative of food insecurity, while negative responses (i.e., never true) to both questions was indicative of food security. Prior studies demonstrate that this two-item screener provides a sensitivity of 97% and specificity of 83%, in determining food insecurity.49
Covariates
Included in this analysis were the following covariates, which prior literature has demonstrated to be associated with pediatric obesity: youth factors, such as age (in years), race/ethnicity (Hispanic, black, white, and other race/ethnicity), and parent factors, such as parent weight status (underweight/healthy weight, overweight, and obese, based on BMI thresholds) and parent education (less than high school, high school degree or General Education Diploma (GED), some college, but not a college degree, 4-year college degree, or higher).50–52
Statistical Methods
Descriptive statistics are reported as frequencies and means [standard deviations (SDs)]. Chi-square analyses (for having a regular bedtime and having difficulties staying asleep) and t-tests (for average sleep duration) were conducted to determine whether there were differences across sleep measures by the presence/absence of food insecurity. Then, a set of multinomial logistic regression models was fit to the data to determine associations between sleep measures and weight status. Unadjusted logistic regression models with average sleep duration, having a regular bedtime, and having difficulties staying asleep predicting weight status category were fit to the data first, followed by logistic regression models adjusting for covariates.
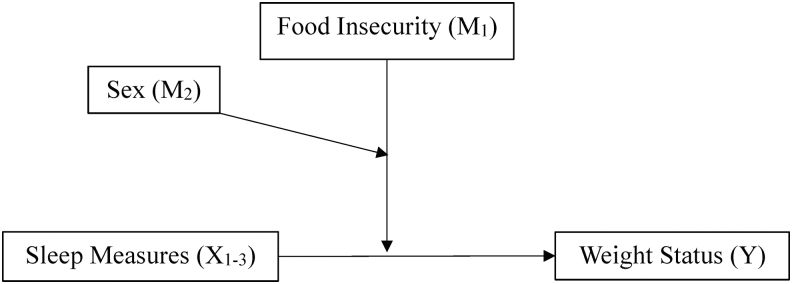
Then, conditional process models were implemented to investigate associations between each sleep measure and weight status and test whether these associations were moderated by food insecurity and sex. Separate models were fit to the data for each sleep measure (e.g., mean-centered average nighttime sleep duration, having a regular bedtime, and having difficulties staying asleep). Continuous predictors were centered at their means (Aiken and West, 1991)74 before computing the interaction term and all terms were entered into the model together. Conditional process models included effects of predictors (X1–3; mean-centered average nighttime sleep duration, having a regular bedtime, or having difficulties staying asleep) on the outcome (Y; weight status) by the moderators (M1,2; food insecurity status and sex). Models controlled for the effects of age, race/ethnicity, as well as parent weight status, education, and income, and interactions between sleep measures, food insecurity, and sex (Fig. 1). Statistical significance was determined by a critical p-value of <0.05.
Figure 1.
Conditional process model: association between Sleep Measures and Weight Status, Moderated by Food Insecurity and Sex. Note. Sleep measures include mean-centered sleep duration (X1), having a regular bedtime (X2), and having difficulties sleeping (X3). This model is adjusted for the effects of each sleep measure, as well as the following covariates: adolescent-reported age, sex, and race/ethnicity, as well as parent-reported weight status, education, and income. Results for this model (reflective of Model 3 in Hayes53) are shown in Table 3.
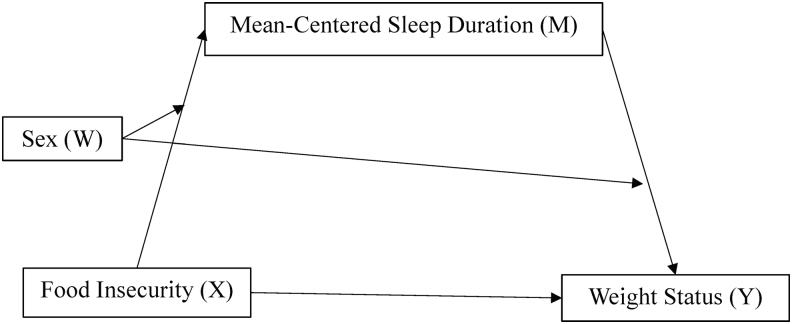
Conditional process models were also implemented to investigate associations between food insecurity and weight status and test whether this association was mediated by mean-centered average nighttime sleep duration and moderated by sex. These conditional process models included the effects of the predictor (X, food insecurity) on the outcome (Y, weight status) through the mediator (M, mean-centered sleep duration) and moderator (W, sex). Models controlled for the effects of age, race/ethnicity, as well as parent weight status, education, and income (Fig. 2). Like the other conditional process models, statistical significance was determined by a critical p-value of <0.05. Given that average sleep duration is one of the most common sleep measures found in the extant literature17 and that conditional process models cannot provide estimates for models where mediators are dichotomous,53 only mediation by mean-centered sleep duration is reported. All statistical analyses were conducted in SAS v9.4, with the PROCESS macro being applied for conditional process analyses.53
Figure 2.
Conditional process model: association between Food Insecurity and Weight Status, Mediated by Mean-Centered Sleep Duration and Moderated by Sex. Note. This model is adjusted for the following covariates: adolescent-reported age, sex, and race/ethnicity, as well as parent-reported weight status, education, and income. Results for this model (reflective of Model 59 in Hayes53) are shown in Table 4.
Results
Sample characteristics are shown in Table 1. Adolescents were on average 14.5 years of age (SD = 1.6). Half of the sample was female (50%) and most were white (64%). Approximately 27% of adolescents and 61% of parents were overweight or obese. Almost half (42%) of parents had earned a 4-year college degree or higher. Approximately 35% of adolescents lived in food-insecure households. Regarding sleep, most adolescents (61%) had a regular bedtime and 13% reported having difficulties staying asleep. Adolescents slept on average 9.0 hours (SD = 1.3) per night.
Table 1.
Sample Characteristics by Parent-Reported Food Insecurity (N = 1544)
| Adolescents | Total |
Food secure (N = 1094) |
Food insecure (N = 422) |
p | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Sleep measures | |||||||
| Has a regular bedtime | 0.716 | ||||||
| No | 565 | 38.9 | 411 | 39.3 | 154 | 38.2 | |
| Yes | 885 | 61.1 | 636 | 60.7 | 249 | 61.8 | |
| Has difficulty staying asleep | <0.001 | ||||||
| No | 1307 | 86.9 | 966 | 88.9 | 341 | 81.8 | |
| Yes | 197 | 13.1 | 121 | 11.1 | 76 | 18.2 | |
| Weight status | <0.001 | ||||||
| Underweight | 69 | 4.5 | 54 | 4.9 | 15 | 3.6 | |
| Healthy weight | 1034 | 68.2 | 780 | 71.3 | 254 | 60.2 | |
| Overweight | 224 | 14.8 | 147 | 13.5 | 77 | 18.2 | |
| Obese | 189 | 12.5 | 113 | 10.3 | 76 | 18.0 | |
| Sex | 0.359 | ||||||
| Male | 770 | 49.9 | 539 | 49.3 | 219 | 51.9 | |
| Female | 774 | 50.1 | 555 | 50.7 | 203 | 48.1 | |
| Race/Ethnicity | <0.001 | ||||||
| Hispanic | 150 | 9.9 | 96 | 8.9 | 54 | 13.0 | |
| Black | 243 | 16.2 | 154 | 14.2 | 89 | 21.3 | |
| White | 969 | 64.6 | 731 | 67.4 | 238 | 57.1 | |
| Other | 139 | 9.3 | 103 | 9.5 | 36 | 8.6 | |
| Mean | SD | Mean | SD | Mean | SD | p | |
| Age, years (range: 12–17 years) | 14.5 | 1.6 | 14.5 | 1.6 | 14.4 | 1.7 | 0.856 |
| Average sleep duration, hours | 9.0 | 1.3 | 8.9 | 1.2 | 9.1 | 1.4 | 0.014 |
| Parents | N | % | N | % | N | % | p |
| Weight status | <0.001 | ||||||
| Underweight | 19 | 1.3 | 12 | 1.1 | 7 | 1.7 | |
| Healthy weight | 558 | 37.2 | 445 | 41.0 | 113 | 27.3 | |
| Overweight | 456 | 30.4 | 340 | 31.3 | 116 | 28.0 | |
| Obese | 467 | 31.1 | 289 | 26.6 | 178 | 43.0 | |
| Education | <0.001 | ||||||
| Less than high school | 20 | 1.3 | 7 | 0.6 | 13 | 3.1 | |
| High school degree or GED | 251 | 16.6 | 161 | 14.8 | 90 | 2.5 | |
| Some college but not a college degree | 527 | 34.9 | 353 | 32.4 | 174 | 41.5 | |
| Four-year college degree or higher | 711 | 47.1 | 569 | 52.2 | 142 | 33.9 | |
| Income | <0.001 | ||||||
| $0–$99,999 | 1178 | 78.7 | 792 | 73.3 | 386 | 92.8 | |
| $100,000 or more | 319 | 21.3 | 289 | 26.7 | 30 | 7.2 | |
p-Values reflect comparisons between adolescents living within food-secure and food-insecure households.
GED, General Education Diploma; SD, standard deviation.
Statistically significant differences were found across adolescent-reported average nighttime sleep duration and having difficulties staying asleep by parent-reported food insecurity status. Adolescents living in food-insecure households slept on average 0.2 hours longer than adolescents living in food-secure households. A greater percentage of adolescents living in food-insecure households reported having difficulties staying asleep (18%), when compared to adolescents living in food-secure households (11%). There were no statistically significant differences in adolescents having a regular bedtime across parent-reported food insecurity status (62% of adolescents living in food-insecure and 61% of adolescents living in food-secure households had a regular bedtime). Race/ethnicity, parent weight status, parent education, and parent income also differed by food insecurity status. A greater percentage of adolescents living in food-insecure households were Hispanic (13%) and black (21%), had parents who were either overweight (28%) or had obesity (43%), and had parents who attained less than a high school education (3%) and earned an income of <$100,000 (93%).
As shown in Table 2, unadjusted multinomial logistic regression models demonstrated a statistically significant association between having a regular bedtime and lower odds of having obesity [odds ratio (OR) = 0.72, 95% confidence interval (95% CI): 0.52 to 0.99]. This association remained significant, even after adjusting for covariates (OR = 0.62, 95% CI: 0.43 to 0.90). Food insecurity was also associated with greater odds of being overweight (OR = 1.56, 95% CI: 1.13 to 2.15) and having obesity (OR = 1.96, 95% CI: 1.40 to 2.74). The association between food insecurity and greater odds of being overweight remained statistically significant after adjusting for covariates (OR = 1.40, 95% CI: 1.00 to 2.00), while the association between food insecurity and greater odds of having obesity did not (OR = 1.37, 95% CI: 0.95 to 1.99).
Table 2.
Associations between Sleep Measures, Food Insecurity, and Weight Status, Unadjusted and Adjusted for Covariates
| Unadjusted models |
Adjusted modelsa |
|||||
|---|---|---|---|---|---|---|
| Underweight, OR (95% CI) | Overweight, OR (95% CI) | Obese, OR (95% CI) | Underweight, OR (95% CI) | Overweight, OR (95% CI) | Obese, OR (95% CI) | |
| Mean-centered sleep duration | 1.05 (0.86 to 1.28) | 0.96 (0.85 to 1.09) | 0.95 (0.84 to 1.08) | 1.06 (0.86 to 1.32) | 0.93 (0.82 to 1.06) | 0.92 (0.80 to 1.06) |
| Has a regular bedtime (reference: no) | 1.71 (0.95 to 3.06) | 0.98 (0.72 to 1.34) | 0.72 (0.52 to 0.99) | 1.65 (0.90 to 3.03) | 0.88 (0.63 to 1.24) | 0.62 (0.43 to 0.90) |
| Has difficulties staying asleep (reference: no) | 1.68 (0.85 to 3.32) | 1.36 (0.89 to 2.08) | 1.48 (0.95 to 2.30) | 2.03 (1.01 to 4.10) | 1.27 (0.80 to 2.00) | 1.40 (0.86 to 2.27) |
| Food insecurity (reference: no) | 0.81 (0.44 to 1.50) | 1.56 (1.13 to 2.15) | 1.96 (1.40 to 2.74) | 0.86 (0.45 to 1.62) | 1.40 (1.00 to 2.00) | 1.37 (0.95 to 1.99) |
The reference category for adolescent weight status is healthy weight. Bold text indicates statistical significance at p-value <0.05.
Analyses are adjusted for the following covariates: youth-reported age, youth-reported sex, youth-reported race/ethnicity, parent self-reported weight status, parent-reported education, and parent-reported income.
CI, confidence interval; OR, odds ratio.
Adjusted multinomial logistic regression models also demonstrated statistically significant associations between having difficulties staying asleep and food insecurity status with adolescent weight status. Adolescents who reported having difficulties staying asleep had higher odds of being underweight (OR = 2.03, 95% CI: 1.01 to 4.10).
Table 3 displays results from conditional process models for the association between sleep measures and weight status, moderated by food insecurity status and sex (i.e., Models 1–3). Results demonstrated that food insecurity was not related to adolescent weight status across any of the models [Model 1: β = 0.18, standard error (SE) = 0.13, p = 0.184; Model 2: β = 0.02, SE = 0.22, p = 0.925; and Model 3: β = 0.10, SE = 0.15, p = 0.496]. Having a regular bedtime was negatively associated with adolescent weight status across all models (Model 1: β = −0.12, SE = 0.04, p = 0.006; Model 2: β = −0.31, SE = 0.15, p = 0.391; and Model 3: β = −0.12, SE = 0.04, p = 0.003). In addition, age was negatively associated with adolescent weight status and parent weight status was positively associated with adolescent weight status in all models. Interactions between sleep measures, food insecurity status, and sex were not statistically significant, except for the interaction between having difficulties staying asleep and sex predicting weight status (β = 0.34, SE = 0.15, p = 0.030). Although not statistically significant, having difficulties staying asleep was associated with greater weight status among males (β = 0.32, SE = 0.19, p = 0.087) and lower weight status among females (β = −0.064, SE = 0.16, p = 0.709).
Table 3.
Associations between Sleep Measures and Weight Status, Moderated by Food Insecurity and Sex
| Model 1: mean-centered sleep duration→weight status |
Model 2: has a regular bedtime→weight status |
Model 3: has difficulty staying asleep→weight status |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | p | Estimate | SE | p | Estimate | SE | p | |
| Constant | 2.56 | 0.26 | <0.001 | 2.71 | 0.27 | <0.001 | 2.67 | 0.26 | <0.001 |
| Food insecurity | 0.18 | 0.13 | 0.184 | 0.02 | 0.22 | 0.925 | 0.10 | 0.15 | 0.496 |
| Mean-centered sleep duration | −0.05 | 0.06 | 0.372 | −0.03 | 0.02 | 0.108 | −0.02 | 0.02 | 0.125 |
| Has a regular bedtime | −0.12 | 0.04 | 0.006 | −0.31 | 0.15 | 0.039 | −0.12 | 0.04 | 0.003 |
| Has difficulty staying asleep | 0.04 | 0.06 | 0.546 | 0.04 | 0.06 | 0.511 | −0.55 | 0.27 | 0.040 |
| Sleep measure × food insecurity | −0.01 | 0.10 | 0.900 | 0.24 | 0.28 | 0.392 | 0.71 | 0.41 | 0.086 |
| Sleep measure × sex | 0.01 | 0.04 | 0.866 | 0.13 | 0.09 | 0.176 | 0.34 | 0.15 | 0.030 |
| Food insecurity × sex | −0.05 | 0.09 | 0.543 | 0.07 | 0.14 | 0.632 | 0.00 | 0.09 | 0.976 |
| Sleep measure × parent insecurity × sex | 0.04 | 0.06 | 0.499 | −0.18 | 0.18 | 0.319 | −0.39 | 0.25 | 0.123 |
| Age | −0.03 | 0.01 | 0.020 | −0.03 | 0.06 | 0.016 | −0.03 | 0.04 | 0.003 |
| Sex | −0.06 | 0.05 | 0.182 | −0.15 | 0.07 | 0.056 | −0.10 | 0.04 | 0.052 |
| Race/ethnicity | −0.02 | 0.06 | 0.524 | −0.02 | 0.03 | 0.478 | −0.02 | 0.03 | 0.424 |
| Parent weight status | 0.22 | 0.02 | <0.001 | 0.22 | 0.02 | <0.001 | 0.22 | 0.02 | <0.001 |
| Parent education | −0.05 | 0.02 | 0.090 | −0.05 | 0.03 | 0.069 | −0.05 | 0.03 | 0.086 |
| Parent income | −0.09 | 0.05 | 0.086 | −0.08 | 0.05 | 0.117 | −0.09 | 0.05 | 0.091 |
| R2 | 0.10 | 0.10 | 0.10 | ||||||
| F | 10.84 | 10.73 | 10.98 | ||||||
| p | <0.001 | <0.001 | <0.001 | ||||||
Bold text indicates statistical significance at p-value <0.05.
SE, standard error.
Table 4 displays results from the conditional process model for the association between food insecurity status and weight status, mediated by mean-centered sleep duration and moderated by sex. Results indicate that food insecurity was not associated with either mean-centered sleep duration (β = 0.12, SE = 0.07, p = 0.109) or weight status (β = 0.17, SE = 0.14, p = 0.206) and that mean-centered sleep duration was not associated with weight status (β = −0.06, SE = 0.04, p = 0.229). Also, the effect of food insecurity status on adolescent weight status did not differ by sex (interaction between food security and sex: β = −0.04, SE = 0.09, p = 0.610). Having a regular bedtime was positively associated with mean-centered sleep duration (β = 0.43, SE = 0.07, p < 0.001) and negatively associated with adolescent weight status (β = −0.13, SE = 0.04, p = 0.003). Having difficulties staying asleep was not associated with mean-centered sleep duration (β = 0.09, SE = 0.10, p = 0.340) or adolescent weight status (β = 0.04, SE = 0.06, p = 0.176).
Table 4.
Food Insecurity (X) Predicting Weight Status (Y), Mediated by Mean-Centered Sleep Duration (M), Including Moderation Effect by Sex
| Mean-centered sleep duration (M) |
Weight status (Y) |
|||||
|---|---|---|---|---|---|---|
| Estimate | SE | p | Estimate | SE | p | |
| Constant | 2.61 | 0.42 | <0.001 | 2.58 | 0.26 | <0.001 |
| Food insecurity (X) | −0.08 | 0.23 | 0.732 | 0.17 | 0.14 | 0.206 |
| Mean-centered sleep duration | — | — | — | −0.06 | 0.05 | 0.229 |
| Mean-centered sleep duration × sex | — | — | — | 0.02 | 0.03 | 0.467 |
| Food insecurity × sex | 0.14 | 0.15 | 0.351 | −0.04 | 0.09 | 0.610 |
| Has a regular bedtime | 0.43 | 0.07 | <0.001 | −0.13 | 0.04 | 0.003 |
| Has difficulty staying asleep | 0.09 | 0.10 | 0.388 | 0.04 | 0.06 | 0.500 |
| Age | −0.15 | 0.02 | <0.001 | −0.03 | 0.01 | 0.019 |
| Sex | 0.03 | 0.04 | 0.467 | −0.06 | 0.05 | 0.176 |
| Race/ethnicity | 0.03 | 0.04 | 0.487 | −0.02 | 0.03 | 0.483 |
| Parent weight status | −0.10 | 0.04 | 0.011 | 0.22 | 0.02 | <0.001 |
| Parent education | −0.12 | 0.04 | 0.006 | −0.05 | 0.03 | 0.079 |
| Parent income | −0.19 | 0.08 | 0.022 | −0.08 | 0.05 | 0.108 |
| R2 | 0.10 | 0.10 | ||||
| F | 15.56 | 12.39 | ||||
| p | <0.001 | <0.001 | ||||
Bold text indicates statistical significance at p-value <0.05. Direct effect = 0.11, p = 0.017; indirect effect = −0.003, bootstrapped 95% CI (−0.014 to 0.001).
Discussion
This study is one of the first to comprehensively examine associations between sleep, food insecurity, and weight status during adolescence. Results demonstrate statistically significant differences in adolescent-reported sleep measures according to parent-reported food insecurity status, such that adolescents living in food-insecure households report higher frequencies of having difficulties staying asleep and greater average sleep duration. A greater percentage of parents who have obesity, earned less than a high school education, and an income of <$100,000 have adolescents living in food-insecure households. Adolescents living in food-insecure households were also found to have higher odds of being overweight, relative to adolescents living in food-secure households. Having a regular bedtime was associated with lower odds of having obesity, while having difficulties staying asleep was associated with greater odds of being underweight. Some associations were not statistically significant in unadjusted multinomial logistic regression models, but became statistically significant after adjusting for covariates (e.g., having a regular bedtime and greater odds of being underweight), which may signal that one or more of the covariates is related to sleep and/or weight status in some way. Furthermore, it is possible that there may be other factors to consider in the associations between sleep, food insecurity, and obesity outside of dietary intake, such as depression. When examining how sleep measures, food insecurity, and weight status may be related using conditional process models, food insecurity did not moderate the association between sleep measures and weight status. In addition, average nighttime sleep duration was not found to mediate the relationship between food insecurity and weight status. Unlike other studies,30 sex did not moderate any associations between sleep measures, food insecurity, and weight status.
These results provide additional support for the need to uncover mechanisms for how sleep and food insecurity effect pediatric obesity, especially during adolescence. Poor sleep is increasingly common among adolescents, as only 20% get sufficient sleep on school nights.54 This is problematic, especially given the results of recent meta-analyses and systematic reviews,55–57 which describe associations between short sleep duration and obesity incidence. According to previous studies, the mechanisms by which sleep duration might affect obesity include dietary intake, as it relates to increased hunger and appetite,58,59 irregular eating habits, and snacking between meals,60 which have been previously associated with short sleep duration. Although less prevalent in existing studies, other aspects of sleep have also been associated with obesity both cross-sectionally and longitudinally.61 For example, a review of pediatric sleep and overweight/obesity conducted by Hart et al. found associations between sleep duration, quality, and timing and BMI and body fat percentage.13 Although, a more recent review of the literature conducted by Krietsch et al. reveals considerable variability in findings linking pediatric sleep with weight-related factors, such dietary intake and altered eating behaviors, and hormones regulating hunger/satiety,62 such as leptin and ghrelin.62–65
Results from our study demonstrated associations between having a regular bedtime and lower odds of having obesity. These findings align with results from the Millennium Cohort Study, a longitudinal study of children from the United Kingdom, which found that inconsistent bedtimes at the age of 3 were associated with later obesity at age 11.66 Children and adolescents who have regular bedtime routines have been found to have earlier bedtimes, sleep more, fall asleep faster, and experience fewer sleep disturbances due to nighttime awakenings.67 Studies have demonstrated that those with obesity are also more likely to report insomnia or difficulty with sleep, even after controlling for sociodemographic and behavioral factors.68,69 Our study results also showed an association between having difficulties staying asleep and increased odds of being underweight. To our knowledge, this association has not been described elsewhere and will require additional examination. However, results from our study and that of others suggest that improving sleep through the implementation of consistent bedtimes and reduced sleep disturbances may be a prudent pediatric obesity prevention strategy.
Our study also contributes to the existing literature by exploring the relationship between sleep measures, food insecurity, and weight status in more comprehensive statistical models. To date, existing research has focused primarily on food insecurity and sleep36,70 or food insecurity and obesity.28 Extant research examining the relationship between food insecurity and sleep finds that food insecurity is associated with insufficient sleep and insomnia70 and suboptimal sleep quality.36 Meanwhile, literature on food insecurity and pediatric obesity reveals mixed associations.38–43 Recent reviews of the literature suggest that mixed findings may be attributed to differences in the ages of sample populations and participation in food assistance.28,71
The results from this study suggest that sleep and food insecurity are independently related to pediatric obesity and that attributes of sleep may differ by food insecurity status. However, the mechanisms by which sleep and food insecurity influence pediatric obesity remain unclear. Sleep was not an explanatory factor in our study. Furthermore, the association between food insecurity and longer sleep duration that we found in our study was in the opposite direction of what was expected, based on prior research.31 One study conducted using data from Norway by Sivertsen et al. found that being underweight was associated with shorter sleep duration and suggested that being underweight was related to poorer sleep outcomes in a way that was similar to being overweight and obese. The effect also seemed to differ according to sex. While females had demonstrated a curvilinear relationship between BMI and sleep duration, males demonstrated a linear relationship.72 Unfortunately, we are unable to replicate and/or explain these findings without the collection of longitudinal data and information on other measures, such as eating behaviors, energy intake, and depression. Thus, more research is needed to confirm these findings and examine other potential individual- and family-level factors influencing pediatric obesity not yet explored in this work.
Limitations and Strengths
A few limitations of our study should be considered. This study was conducted utilizing cross-sectional data from the FLASHE Study. The use of cross-sectional survey data does not allow for any investigation into causality between sleep and obesity. In addition, measures were self-reported. The dichotomous response options for two of the sleep measures (i.e., having a regular bedtime and having difficulty staying asleep) did not allow for a detailed level of specificity present with more continuous measures. Similarly, we utilized a validated, two-item screener for measuring parent-reported food insecurity.49 A more comprehensive measure such as the 18-item Household Food Security Survey73 could be used in future studies. Added to this, the data presented here do not include information from the FLASHE Motion Study, which is not currently available to the public. Having these data would offer an important opportunity to explore the research question using a more objective measurement of sleep. Future studies may want to look toward validating existing survey data on sleep with that of accelerometer data, which may be made available in the future. Finally, although efforts were made to recruit a balanced sample, the FLASHE parent sample included more individuals who were highly educated.31 This survey was also administered online, suggesting that there may be potential selection bias of participants (i.e., those who have access to the internet). Thus, results might not be generalizable to other populations with other characteristics.
Despite these limitations, the study also has strengths worth mentioning. First, the FLASHE Study includes a broad scope of correlates,30 which were included in our analyses. In addition, the FLASHE study includes a large sample of adolescents—an underrepresented population, especially in studies of sleep, food insecurity, and obesity. Most studies have focused on characterizing the relationships between sleep, food insecurity, and obesity among adults and young children. Our study also expands upon the existing literature, which primarily focuses on average sleep duration and obesity,56,71 by including other sleep measures not commonly investigated in other studies (e.g., having a regular bedtime and having difficulties staying asleep). We were also able to explore potential interactions between sleep, food insecurity, and sex on weight status, which has not been previously investigated in other studies.
Conclusions
Results of this study provide information on the relationships between sleep, food insecurity, and adolescent obesity. Longitudinal data and experimental studies focused on sleep, food insecurity, and weight status are needed to better understand the potential mechanisms and directionality of these relationships. Specifically, cohort studies investigating developmental trajectories, duration, and chronicity of sleep behaviors would be useful in determining how these measures of sleep present across development. Understanding the conditions under which sleep promotes or inhibits pediatric obesity across different environments (e.g., within food-secure vs. food-insecure households) will add to our understanding of obesity and obesity-related morbidities in adulthood.
Authors' Contributions
E.K.D., G.A.B., and E.L.A. conducted the literature search. E.K.D. performed the data analysis and generation of figures. E.K.D., A.J.K., E.L.A., and B.F.F. contributed to the data interpretation. All authors were involved in the study design, writing, and final approval of the submitted and published versions of this article.
Funding Information
The FLASHE Study was funded by the National Cancer Institute (NCI) under contract number HHSN261201200039I issued to Westat, Inc. This project has been funded, in whole or in part, with federal funds from NCI, NIH, under contract number HHSN261200800001E (Hennessy). The content of this publication does not necessarily reflect the views or policies of the DHHS, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government. Additional support for this research was provided by the American Heart Association 2020 Institutional Undergraduate Fellowship (PHC 50647, Award No. 20UFEL35320025) to Gabrielle A. Bowen through the Pauley Heart Center at Virginia Commonwealth University and by the National Institutes of Health (Award No. 2T32CA093423) for Elizabeth L. Adams' postdoctoral effort.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Bridger T. Childhood obesity and cardiovascular disease. Paediatr Child Health 2009;14:177–182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Schwarz SW, Peterson J. Adolescent Obesity in the United States: Facts for Policymakers. National Center for Children in Poverty, New York, NY, 2010 [Google Scholar]
- 3. Di Cesare M, Sorić M, Bovet P, et al. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med 2019;17:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity: An evaluation of potential bias. Vital Health Stat 2018;3:1–21 [PubMed] [Google Scholar]
- 5. Rofey DL, Kolko RP, Iosif A-M, et al. A longitudinal study of childhood depression and anxiety in relation to weight gain. Child Psychiatry Hum Dev 2009;40:517–526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. CDC Press Releases [Internet]. CDC. 2016. [Cited November 25, 2020]. Available at https://www.cdc.gov/media/releases/2017/p1003-vs-cancer-obesity.html (Last accessed January16, 2021)
- 7. Lakshman R, Elks CE, Ong KK. Childhood obesity. Circulation 2012;126:1770–1779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Quas JA. Adolescence: A unique period of challenge and opportunity for positive development [Internet]. 2014. [Cited November 25, 2020]. Available at https://www.apa.org/pi/families/resources/newsletter/2014/12/adolescence-development (Last accessed January16, 2021)
- 9. Patton GC, Coffey C, Carlin JB, et al. Overweight and obesity between adolescence and young adulthood: A 10-year prospective cohort study. J Adolesc Health 2011;48:275–280 [DOI] [PubMed] [Google Scholar]
- 10. Tirosh A, Shai I, Afek A, et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med 2011;364:1315–1325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ly W, Graubard BI, Williamson DF, Gail MH. The association between body mass index in adolescence and obesity in adulthood. J Adolesc Health 2008;42:512–518 [DOI] [PubMed] [Google Scholar]
- 12. Wang LY, Chyen D, Lee S, Lowry R. The association between body mass index in adolescence and obesity in adulthood. J Adolesc Health 2008;42:512–518 [DOI] [PubMed] [Google Scholar]
- 13. Hart CN, Cairns A, Jelalian E. Sleep and obesity in children and adolescents. Pediatr Clin North Am 2011;58:715–733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics 2003;111:302–307 [DOI] [PubMed] [Google Scholar]
- 15. Twenge JM, Krizan Z, Hisler G. Decreases in self-reported sleep duration among U.S. adolescents 2009-2015 and association with new media screen time. Sleep Med 2017;39:47–53 [DOI] [PubMed] [Google Scholar]
- 16. National Sleep Foundation. National Sleep Foundation Recommends New Sleep Times [Internet]. SleepFoundation.org. [Cited November 25, 2020]. Available at https://www.sleepfoundation.org/press-release/national-sleep-foundation-recommends-new-sleep-times (Last accessed January16, 2021)
- 17. Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity (Silver Spring) 2008;16:265–274 [DOI] [PubMed] [Google Scholar]
- 18. Mars M, de Graaf C, de Groot CPGM, et al. Fasting leptin and appetite responses induced by a 4-day 65%-energy-restricted diet. Int J Obes 2006;30:122–128 [DOI] [PubMed] [Google Scholar]
- 19. Wren AM, Seal LJ, Cohen MA, et al. Ghrelin enhances appetite and increases food intake in humans. J Clin Endocrinol Metab 2001;86:5992. [DOI] [PubMed] [Google Scholar]
- 20. Nedeltcheva AV, Kessler L, Imperial J, Penev PD. Exposure to recurrent sleep restriction in the setting of high caloric intake and physical inactivity results in increased insulin resistance and reduced glucose tolerance. J Clin Endocrinol Metab 2009;94:3242–3250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brondel L, Romer MA, Nougues PM, et al. Acute partial sleep deprivation increases food intake in healthy men. Am J Clin Nutr 2010;91:1550–1559 [DOI] [PubMed] [Google Scholar]
- 22. Troy LM, Miller EA, Olson S. Hunger and Obesity: Understanding a Food Insecurity Paradigm: Workshop Summary. National Academies Press (US): Washington, DC, 2011 [PubMed] [Google Scholar]
- 23. Trade Reforms and Food Security [Internet]. [Cited November 25, 2020]. Available at www.fao.org/3/y4671e/y4671e00.htm (Last accessed January16, 2021).
- 24. Jones SJ, Frongillo EA. Food insecurity and subsequent weight gain in women. Public Health Nutr 2007;10:145–151 [DOI] [PubMed] [Google Scholar]
- 25. Webb AL, Schiff A, Currivan D, Villamor E. Food Stamp Program participation but not food insecurity is associated with higher adult BMI in Massachusetts residents living in low-income neighbourhoods. Public Health Nutr 2008;11:1248–1255 [DOI] [PubMed] [Google Scholar]
- 26. Gibson D. Food stamp program participation is positively related to obesity in low income women. J Nutr Oxford Academic 2003;133:2225–2231 [DOI] [PubMed] [Google Scholar]
- 27. Leung CW, Villamor E. Is participation in food and income assistance programmes associated with obesity in California adults? Results from a state-wide survey. Public Health Nutr 2011;14:645–652 [DOI] [PubMed] [Google Scholar]
- 28. Larson NI, Story MT. Food insecurity and weight status among U.S. children and families: A review of the literature. Am J Prev Med 2011;40:166–173 [DOI] [PubMed] [Google Scholar]
- 29. Ding M, Keiley MK, Garza KB, et al. Food insecurity is associated with poor sleep outcomes among US adults. J Nutr 2015;145:615–621 [DOI] [PubMed] [Google Scholar]
- 30. Gooding HC, Walls CE, Richmond TK. Food insecurity and increased BMI in young adult women. Obesity (Silver Spring) 2012;20:1896–1901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Narcisse M, Long CR, Felix H, et al. The mediating role of sleep quality and quantity in the link between food insecurity and obesity across race and ethnicity. Obesity (Silver Spring) 2018;26:1896–1901 [DOI] [PubMed] [Google Scholar]
- 32. Liu Y, Njai RS, Greenlund KJ, et al. Relationships between housing and food insecurity, frequent mental distress, and insufficient sleep among adults in 12 US States, 2009. Prev Chronic Dis 2014;11:E37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jordan ML, Perez-Escamilla R, Desai MM, Shamah-Levy T. Household food insecurity and sleep patterns among Mexican adults: Results from ENSANUT-2012. J Immigr Minor Health 2016;18:1093–1103 [DOI] [PubMed] [Google Scholar]
- 34. Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep 2014;37:601–611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Martinez SM, Grandner MA, Nazmi A, et al. Pathways from food insecurity to health outcomes among California University Students. Nutrients 2019;11:1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Na M, Eagleton SG, Jomaa L, et al. Food insecurity is associated with suboptimal sleep quality, but not sleep duration, among low-income Head Start children of pre-school age. Public Health Nutr 2020;23:701–710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Alaimo K, Olson CM, Frongillo EA. Food insufficiency and American school-aged children's cognitive, academic, and psychosocial development. Pediatrics 2001;108:44–53 [PubMed] [Google Scholar]
- 38. Kaiser LL, Melgar-Quinones HR, Lamp CL, et al. Food security and nutritional outcomes of preschool-age Mexican-American children. J Am Diet Assoc 2002;102:924–929 [DOI] [PubMed] [Google Scholar]
- 39. Matheson DM, Varady J, Varady A, Killen JD. Household food security and nutritional status of Hispanic children in the fifth grade. Am J Clin Nutr 2002;76:210–217 [DOI] [PubMed] [Google Scholar]
- 40. Bhattacharya J, Currie J, Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. J Health Econ 2004;23:839–862 [DOI] [PubMed] [Google Scholar]
- 41. Casey PH, Simpson PM, Gossett JM, et al. The association of child and household food insecurity with childhood overweight status. Pediatrics 2006;118:e1406–e1413 [DOI] [PubMed] [Google Scholar]
- 42. Rose D, Bodor J. Household food insecurity and overweight status in young school children: Results from the early childhood longitudinal study. Pediatrics 2006;117:464–473 [DOI] [PubMed] [Google Scholar]
- 43. Gundersen C, Garasky S, Lohman BJ. Food insecurity is not associated with childhood obesity as assessed using multiple measures of obesity. J Nutr 2009;139:1173–1178 [DOI] [PubMed] [Google Scholar]
- 44. Lohman BJ, Stewart S, Gundersen C, et al. Adolescent overweight and obesity: Links to food insecurity and individual, maternal, and family stressors. J Adolesc Health 2009;45:230–237 [DOI] [PubMed] [Google Scholar]
- 45. National Cancer Institute. FLASHE: Family Life, Activity, Sun, Health, and Eating Study [Internet]. National Cancer Institute; Available at https://cancercontrol.cancer.gov/sites/default/files/2020-06/flashe_factsheet.pdf (Last accessed January16, 2021)
- 46. Oh AY, Davis T, Dwyer LA, et al. Recruitment, enrollment, and response of parent–adolescent dyads in the FLASHE study. Am J Prev Med 2017;52:849–855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Nebeling LC, Hennessy E, Oh AY, et al. The FLASHE study: Survey development, dyadic perspectives, and participant characteristics. Am J Prev Med 2017;52:839–848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Growth Charts—Clinical Growth Charts [Internet]. 2019. [Cited November 25, 2020]. Available at https://www.cdc.gov/growthcharts/clinical_charts.htm (Last accessed January16, 2021)
- 49. Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 2010;126:e26–e32 [DOI] [PubMed] [Google Scholar]
- 50. An R, Yang Y, Hoschke A, et al. Influence of neighbourhood safety on childhood obesity: A systematic review and meta-analysis of longitudinal studies. Obes Rev 2017;18:1289–1309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hassapidou M, Papadopoulou SK, Frossinis A, et al. Sociodemographic, ethnic and dietary factors associated with childhood obesity in Thessaloniki, Northern Greece. Hormones (Athens) 2009;8:53–59 [DOI] [PubMed] [Google Scholar]
- 52. Singh GK, Siahpush M, Kogan MD. Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health Aff (Millwood) 2010;29:503–512 [DOI] [PubMed] [Google Scholar]
- 53. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. The Guilford Press: New York, NY, 2013 [Google Scholar]
- 54. Miller AL, Lumeng JC, LeBourgeois MK. Sleep patterns and obesity in childhood. Curr Opin Endocrinol Diabetes Obes 2015;22:41–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: A meta-analysis of prospective studies. Sleep Med 2014;15:1456–1462 [DOI] [PubMed] [Google Scholar]
- 56. Patel SR, Hu FB. Short sleep duration and weight gain: A systematic review. Obesity (Silver Spring) 2008;16:643–653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Cappuccio FP, Taggart FM, Kandala N-B, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008;31:619–626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 2004;141:846–850 [DOI] [PubMed] [Google Scholar]
- 59. Schmid SM, Hallschmid M, Jauch-Chara K, et al. A single night of sleep deprivation increases ghrelin levels and feelings of hunger in normal-weight healthy men. J Sleep Res 2008;17:331–334 [DOI] [PubMed] [Google Scholar]
- 60. Ohida T, Kamal AM, Uchiyama M, et al. The influence of lifestyle and health status factors on sleep loss among the Japanese general population. Sleep 2001;24:333–338 [DOI] [PubMed] [Google Scholar]
- 61. Ogilvie RP, Patel SR. The epidemiology of sleep and obesity. Sleep Health 2017;3:383–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Krietsch KN, Chardon ML, Beebe DW, Janicke DM. Sleep and weight-related factors in youth: A systematic review of recent studies. Sleep Med Rev 2019;46:87–96 [DOI] [PubMed] [Google Scholar]
- 63. Briançon-Marjollet A, Weiszenstein M, Henri M, et al. The impact of sleep disorders on glucose metabolism: Endocrine and molecular mechanisms. Diabetol Metab Syndr 2015;7:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Lundahl A, Nelson TD. Sleep and food intake: A multisystem review of mechanisms in children and adults. J Health Psychol 2015;20:794–805 [DOI] [PubMed] [Google Scholar]
- 65. Hagen EW, Starke SJ, Peppard PE. The association between sleep duration and leptin, ghrelin, and adiponectin among children and adolescents. Curr Sleep Med Rep 2015;1:185–194 [Google Scholar]
- 66. Anderson SE, Sacker A, Whitaker RC, Kelly Y. Self-regulation and household routines at age three and obesity at age eleven: Longitudinal analysis of the UK Millennium Cohort Study. Int J Obes (Lond) 2017;41:1459–1466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Mindell JA, Li AM, Sadeh A, et al. Bedtime routines for young children: A dose-dependent association with sleep outcomes. Sleep 2015;38:717–722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Singareddy R, Vgontzas A, Fernandez-Mendoza J, et al. Risk factors for incident chronic insomnia: A general population prospective study. Sleep Med 2012;13:346–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Pearson NJ, Johnson LL, Nahin RL. Insomnia, trouble sleeping, and complementary and alternative medicine: Analysis of the 2002 National Health Interview Survey Data. Arch Intern Med 2006;166:1775–1782 [DOI] [PubMed] [Google Scholar]
- 70. Poling K, Gallagher R, Hale L, et al. Sleep partially mediates the association between food insecurity and obesity: Roles of short sleep duration, insomnia, and socioeconomic factors. Sleep 2017;40(Suppl 1):A308 [Google Scholar]
- 71. Eisenmann JC, Gundersen C, Lohman BJ, et al. Is food insecurity related to overweight and obesity in children and adolescents? A summary of studies, 1995-2009. Obes Rev 2011;12:e73–e83 [DOI] [PubMed] [Google Scholar]
- 72. Sivertsen B, Pallesen S, Sand L, Hysing M. Sleep and body mass index in adolescence: Results from a large population-based study of Norwegian adolescents aged 16 to 19 years. BMC Pediatr 2014;14:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Gulliford MC, Nunes C, Rocke B. The 18 Household Food Security Survey items provide valid food security classifications for adults and children in the Caribbean. BMC Public Health 2006;6:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Sage: Newbury Park, CA, 1991 [Google Scholar]