Abstract
Policy Points.
Persistent communication inequalities limit racial/ethnic minority access to life‐saving health information and make them more vulnerable to the effects of misinformation.
Establishing data collection systems that detect and track acute gaps in the supply and/or access of racial/ethnic minority groups to credible health information is long overdue.
Public investments and support for minority‐serving media and community outlets are needed to close persistent gaps in access to credible health information.
Keywords: health equity, health policy, health disparities, health promotion
Emerging evidence shows that covid‐19 exacts a disproportionate burden of morbidity and mortality on racial/ethnic minority groups. 1 Several explanations have been proposed to account for this disparity. These include living conditions (e.g., overrepresentation in densely populated areas that restricts social distancing), work circumstances (e.g., working in essential industries without paid sick leave or the ability to work remotely), and limited access to health care services. 2 , 3 , 4 The social determinants of health are thus coming once again into focus as the public health community works to mitigate the pandemic's devastating effects. At the same time, the scope and scale of the disruptions caused by COVID‐19 also draw attention to the persistent and systemic gaps affecting racial/ethnic minority groups’ access to health information owing to the lack of a robust communication infrastructure. We define the communication infrastructure as the established mediated and interpersonal communication channels (e.g., news and social media, communication campaigns and advertising, community engagement and outreach activities, and interactions between provider and patient), formal and informal communication networks, and information and communication technology enabling members of a particular social group to receive, share, engage with, and act on health information. Given the persistent digital divide in racial/ethnic minorities’ access to health information and the disproportionally higher prevalence of low health and digital literacy within these groups, 5 our intention is to make the case for considering the communication infrastructure as a social determinant of health and to discuss the potential implications of this for public health policy and practice.
Communication in a Social Determinants of Health Framework
Research on the differential impact of COVID‐19 on racial/ethnic minority groups is only now beginning to emerge. But there already is evidence that communication‐related disparities may be playing an important role in this context. A recent study of the American public's response to COVID‐19 found that a greater percentage of African American (39%) and Hispanic adults (30%) indicated needing a lot more information about COVID‐19 compared to whites (22%). 6 The same study also found that African American and Hispanic adults were significantly less likely than whites to be aware of critical information regarding the spread and treatment of COVID‐19. These communication‐related disparities were found to be associated with African American and Hispanic adults’ greater reliance on social media as a key source of information on this topic.
Growing concerns that misinformation regarding COVID‐19 is disproportionally affecting members of racial/ethnic minority groups 7 , 8 prompted a call from the CDC to public health professionals to ensure that communications about COVID‐19 and its impact on different populations is frequent, transparent, and credible. 1 This recommendation, we note, is typical of the limited conception of health communication within the existing social determinants of health framework, 9 namely, as a tool to inform and influence health‐related decisions and actions. 10 , 11 While sometimes overlooked, health communication also has an important role in stimulating broader societal changes, policies, and social investments that target social and economic inequalities and shape public opinion and policy discourse regarding the effects of the social determinants of health on health disparities. 12 , 13 In addition, communication can be a powerful tool for empowering and enabling disadvantaged social groups to mobilize and engage in collective actions to address health disparities caused by the social determinants of health. 14 Using health communication in these additional ways, however, requires a robust communication infrastructure that supports regular interactions and information exchanges among members of a particular community or social group and other stakeholders in the external environment (e.g., systems, outside communities, and social groups).
We are proposing that differential access to a robust communication infrastructure is effectively a social determinant of health. That is, we see communities and social groups with greater access to a robust communication infrastructure benefiting from having more opportunities to acquire and exchange critical health information 15 and to organize and mobilize as a community to cope with health‐related challenges and/or advocate for systemic change. 16 Much of this is a reflection of the persistent digital divide (e.g., poor access to and utilization of digital information due to limited broadband access among racial/ethnic minority and rural populations), which complicates the task of launching an adequate response to the devastating effects of COVID‐19 on these communities. 17 At the same time, we recognize that communication inequalities (i.e., differences in the generation, manipulation, and distribution of information among social groups) also stem from differences in the capacity to access, understand, appraise, and use health information. There is a well‐established association between low levels of health and digital literacy and poor health outcomes among racial/ethnic minority groups that impact the capacity of people to seek, process, comprehend, and act on health information. 18 , 19 , 20 But it is ultimately the existing available communication infrastructure that determines their opportunities to do so, including opportunities to connect with others and mobilize as a community to address common health‐related risks and challenges.
The Communication Infrastructure as a Social Determinant of Health
Our proposed conceptual model of the communication infrastructure as a social determinant of health (see Figure 1) positions the communication infrastructure as a critical bridge between health outcomes and the information environment. The model aims to highlight the ways in which the knowledge and information gaps caused by the unequal distribution of information harm the ability of disadvantaged groups and communities to obtain, process, organize, and act on health information. In proposing this model, our primary concern is with those elements of the communication infrastructure that can be modified to decrease communication inequalities and improve the capacity of individuals and communities to navigate and cope with health disparities.
Figure 1.
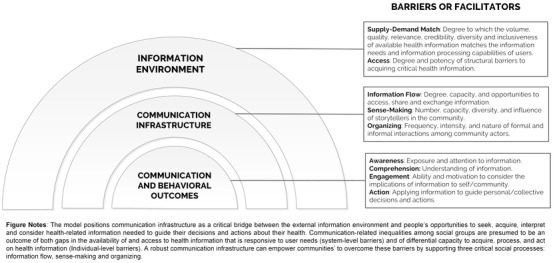
Conceptual Model of the Communication Infrastructure as a Social Determinant of Health
The figure's outer layer represents the complex and dynamic information environment of health‐related issues. The health information needs of different communities and social groups are diverse and dynamic, and their ability to access credible, inclusive, and relevant (or hyperlocal) health information can significantly impact their ability to respond to health‐related challenges. 21 For example, much of the health information regarding COVID‐19 has not been tailored to racial/ethnic minority groups’ consumption and use, despite the urgency of combating the spread of misinformation and the disproportionate risk that COVID‐19 poses for minority populations. 7 , 8 This issue has been plaguing the CDC's early response to COVID‐19 when it started to compile morbidity and mortality data by racial/ethnic group once it was pressured to do so by civil rights and public health advocates. 22 For this reason, the model in Figure 1 identifies the degree of alignment between the supply of and demand for health information as an important source of information and communication inequalities that affect health outcomes among disadvantaged social groups. Besides the gaps between supply and demand, the model also identifies, as a source of communication inequalities, the structural barriers preventing disadvantaged groups and communities from obtaining access to available health information.
The inner most layer represents the communication and behavioral outcomes needed to promote health‐related decisions and behaviors. 10 These include awareness and comprehension of relevant health information, engagement with information (i.e., processing and considering the information and recommendations), and acting accordingly. Generally speaking, the likelihood that these groups and communities will adopt the desirable health behavior is a function of their capacity, opportunity, and motivation to act on relevant health information. 23 According to the model, the communication infrastructure available to connect actors to relevant health information from the broader information environment as well as to information circulating within their community or social group has a critical role in this regard.
Role and Functions of the Communication Infrastructure as a Social Determinant of Health
Our model depicts the communication infrastructure as a critical bridge between the health information environment and the communication and behavioral outcomes experienced by members of a particular community or social group. A community's communication infrastructure consists of the formal and informal communication channels, networks, and vehicles that enable routine interactions between community members and other stakeholders in the external environment. We argue that a robust communication infrastructure not only has a broad reach into the community but also provides the community with hyperlocal and responsive health information. Therefore, a robust communication infrastructure is integral to community members’ information and interaction routines.
Our model also treats the communication infrastructure, rather than the information environment, 24 as a social determinant of health, since social groups’ opportunities to connect with and influence the supply of relevant health information depend critically on the capacity of the communication infrastructure. This particular conception draws on the logic of several contemporary health communication theories—including the communication infrastructure theory (CIT), 14 structural influence model (SIM), 11 , 25 and communication theory of knowledge brokering26—that seek to explicitly link communication inequalities with health disparities. Collectively, these models recognize that communication inequalities partially mediate the effects of social determinants of health on health outcomes but that they are mostly a function of differences in opportunities to seek, receive, and exchange health information. These opportunities in turn are determined by the relative robustness of the communication infrastructure available to support information flow, sense making, and organizing that facilitate members’ acquisition, processing, and use of relevant health information and to empower community mobilization.
Information Flow
The communication infrastructure is important to enabling the efficient and effective flow of health information: the degree, capacity, and opportunity of a group or community to access, share, and exchange timely, relevant, and accurate health information. Social networks help provide or supplement health information that is difficult to access, particularly when mainstream channels are limited or blocked to members of a particular group 27 or when formal communication channels collapse in times of crisis. 28 Intermediaries (or knowledge brokers) such as local journalists, community‐based organizations (CBO), public libraries, and places of worship are critical to supporting the flow of information, as they perform several crucial functions: awareness (drawing attention to relevant health information), accessibility (making health information more comprehensible to users), engagement (connecting health information to the unique problems and challenges faced by the community), linkage (connecting and coordinating information dissemination activities in the community), and mobilization (advocating for specific individual and collective actions based on available health information). 26 For example, past research has consistently found that African Americans prefer and trust local news as a source of credible health information. 27 , 29 However, systemic public disinvestments have devastated the local news media market and created coverage gaps, particularly in rural areas, thereby reducing the availability of relevant and credible health information to residents and their capacity to engage and act on such information. 30
Sense Making
A robust communication infrastructure also is critical to support the ability of groups and communities to make sense of health information. The ways in which health information is presented, interpreted, and contextualized have considerable influence on how people process, use, and act on this information. 12 In particular, research highlights the significance of geoethnic media, community‐based organizations, and other communication channels that support the storytelling network (everyday conversations and stories created and shared by members). 31 By producing and sharing hyperlocal accounts of how the community is being affected by and coping with health‐related challenges, storytellers make health information both more understandable and actionable. 14 For example, access to a storytelling network among African American and Hispanic adults in Los Angeles was found to predict greater knowledge of breast cancer and diabetes, as well as a greater likelihood of seeking screening for breast cancer and diabetes. 16 Similarly, stories about police brutality that circulated on social media were instrumental in crystalizing the African American community's identity and mobilizing members into protest and activism, including the evolution of the Black Lives Matter movement. 32 In this way, by sharing the same story via multiple communication channels and by being picked up by institutional actors, a robust communication infrastructure can facilitate the flow of locally produced health information and knowledge into the larger information environment that surrounds health issues. 26
Organizing
A robust communication infrastructure can also support high levels of social integration in communities and groups by connecting members to one another and to the collective problems they face. Specifically, communities that can maintain rich, diverse, and inclusive cross‐cutting communication and structured mechanisms and opportunities for public discussion are more likely to recognize real problems, develop solutions, and work with stakeholders on their implementation and evaluation. 28 Beyond having a positive effect on community members’ awareness, knowledge, and motivation to act on health recommendations, 33 such communicative social capital has also been shown to increase trust and collective efficacy to seek and use health information 27 , 34 and has also been associated with community mobilizing efforts to satisfy unmet information needs. 35 For example, town hall meetings can be an effective tool for engaging community members in conversations about health problems that require a coordinated response and active community participation. 36 Moreover, a robust communication infrastructure that uses both formal and informal channels/networks to engage diverse groups in the community is key to mobilizing members into collective action such as organizing to collect unwanted or unneeded pain medicine. 37 In addition, emerging evidence shows that a robust communication infrastructure can build resilience against the spread and adverse effects of misinformation. 38
Overall, therefore, considerable research supports the proposition that a robust communication infrastructure can be activated to improve information flow, sense making, and organizing, all of which are needed to support knowledge mobilization. 14 The relative robustness of a communication infrastructure acts as a social determinant of health in that it separates groups and communities that are better equipped and prepared to respond to health challenges from those that are less resilient. Furthermore, while there is little doubt that differences in the communication infrastructure stem in part from the effect of other social determinants of health, the communication infrastructure is unique in that it can be improved and used to enhance knowledge acquisition and knowledge mobilization that empower individuals and communities to navigate and cope with health challenges.
Implications for Research, Policy, and Practice
If we accept the premise that the communication infrastructure is a social determinant of health, then the next logical step is to identify potential policy levers and structural interventions that can ensure that all people and communities have access to hyperlocal health information when they need it and in a format that helps them comprehend, deliberate, and act on that information. Based on the preceding discussion we propose three general targets for universal interventions: (1) improving the supply of and access to relevant and credible health information, 9 (2) improving the flow of and engagement with health information, and (3) improving the capacity of individuals and institutions to act on health information.
Target 1: Improving the Supply of and Access to Health Information
The first step toward closing communication inequalities is establishing national and local surveillance systems (e.g., “infodemiology”) that track and monitor the information needs of different social groups, assess the degree to which available information matches their needs, and provide policymakers and practitioners with the knowledge needed to implement appropriate and effective strategies that target identified information inequalities. In principle, infodemiology is akin to tracking and monitoring the epidemiology of diseases and other health‐related factors. 39 Infodemiology could also involve the mining of website and social media user data to serve as population health metrics. 39 Sentiment analysis of user‐generated content in online forums and social media groups is an example of a strategy that is increasingly employed to this end. 40 Another example is the COVID‐19 Consortium for Understanding the Public's Policy Preferences Across States (COVIDstates.org), which has been tracking public knowledge of and attitudes toward the COVID‐19 response and making this information publicly available. 41
The next step is increasing the production and distribution of hyperlocal information that is responsive to community‐specific information needs. This can be accomplished, in part, by renewing public investments in local journalism, an important source of hyperlocal information. 30 As the COVID‐19 pandemic unfolds, local news outlets keep communities updated on recent public health recommendations, local incidence of COVID‐19 cases, location of testing sites, and other valuable information related to mitigation and reopening efforts—all while experiencing public disinvestments, loss of advertising revenues, and eliminating subscription paywalls to allow free access to critical health information. 42 For example, recognizing the value of local journalism as a vital information source, New Jersey decided to invest public funds in rebuilding the state local news infrastructure. 43
A third strategy is to build the capacity of key intermediaries to verify, filter, and curate health information. Trusted CBOs and patient advocacy groups such as the American Cancer Association and the National Alliance on Mental Illness have a reputable brand, organizational resources, and a network of relationships that can be leveraged to this end. By partnering with local public health experts and policymakers to create information hubs and community outreach programs, 44 these groups can significantly improve their ability to serve the information needs of diverse constituents while also advocating for policy solutions. The growing body of research on research‐practice partnerships can be a useful resource for building and sustaining this type of relationship. 45
Target 2: Improving the Flow of and Engagement With Health Information
While communication research has traditionally focused on developing, testing, and implementing effective message strategies to increase the likelihood that target audiences will pay attention to and process health information, there is a growing interest in how intermediaries might improve the flow of and engagement with health information. 26 As noted earlier, because of the central position they occupy in the communication infrastructure, their reputation and credibility as a source of information, and their ability to leverage organizational resources and practical knowledge, intermediaries are well positioned to connect diverse groups of audiences with relevant and credible health information. Although public education is already a key mission of intermediaries, they may lack the power to communicate effectively about health issues with diverse groups of stakeholders and target audiences. Equipping intermediaries with communication training and providing them with various forms of expert and technical support thus has significant potential to improve their efficacy. For example, training local journalists to report on health and creating mechanisms (e.g., seminars, expert directories) to connect with public health experts can support their capacity to produce and distribute hyperlocal health information. 46 In‐person and virtual town hall meetings organized by community groups to discuss health issues is another example of a potentially effective mechanism to engage members of disadvantaged groups in information exchange while also learning about their unique information needs. 36 Information flow and public engagement can be supported as well by better coordinating resources and activities among intermediaries who are active on the same issue or in the same health policy space through communication and information technologies. 28
Target 3: Improving the Capacity to Convert Health Information Into Actions
Clear, relevant, and timely communication can significantly increase the likelihood that health information will be translated into personal change and collective action. 47 The choice of what to say, to whom, how, and when is therefore consequential not only to make it more likely to result in the desired behavioral outcome but also to avoid unintended effects on audiences. Many actors who communicate regularly with disadvantaged populations about health issues lack the resources and tools needed to collect the surveillance and analytics data of the type that governments and corporations routinely use to inform their outreach and strategic communication efforts. The most critical barrier to utilizing these data is such organizations’ capacity to clean, analyze, and appropriately interpret such data. Short of identifying sources of funding for these organizations, one potentially cost‐effective way of overcoming this barrier is investing in publicly available tools like interactive data dashboards that track changes in public awareness, knowledge, perceptions, and intention to act on health issues. 44 For example, the Connect2HealthFCC Mapping Broadband Health in America platform (https://www.fcc.gov/health/maps) allows users to generate customized maps showing broadband access, adoption, and speed alongside various health measures (e.g., obesity, diabetes, and physician access) in every US state and county. Another potentially useful strategy is establishing publicly accessible and easily searchable clearinghouses of useful communication resources and evidence‐based communication practices, similar to the US Institute of Educational Sciences’ What Works Clearinghouse (https://ies.ed.gov/ncee/wwc/).
Another productive venue of capacity‐building interventions for eliminating information and communication inequalities is the translation of complex health information into an accessible form. 48 Public health communication is too often motivated by the goal of disseminating guidelines or prescriptions for evidence‐based actions. Such guidelines inform people about what to do to minimize potentially serious health risks but not how to do it or how to implement the recommendations. For example, people may know that they should be tested for COVID‐19 when they experience certain symptoms, but they may not know how and where to get tested if such information is not provided. Universal guidelines (e.g., protocols for safely reopening schools and businesses once COVID‐19 infections are declining) are often not universally applicable. Guidelines must therefore be adapted to account for the unique constraints and circumstances of the recommended action. Encouraging intermediaries to focus their efforts on communicating about the how, when, and where of health recommendations can increase adherence to recommended actions. 37 In addition, successfully translating guidelines into actionable propositions requires establishing collaborations between health experts and community storytellers.
Discussion
Robust communication infrastructures are essential to ensuring that all people and communities have an equal opportunity to acquire and use the critical health information they need to make informed health‐related decisions. Research has demonstrated that social groups and communities with a robust communication infrastructure are better equipped and prepared to cope with health stressors and crises than communities that do not—most notably, members of immigrant groups, racial and ethnic minorities, and rural populations who struggle to acquire and act on critical health information. In this sense, the communication infrastructure can and should be understood as a social determinant of health. Systemic efforts to map and track information and communication inequalities are long overdue and can be a powerful tool for guiding policy and public investments in building the national and local communication infrastructure that can support equal access to and use of credible health information and mitigate the spread and adverse effects of misinformation. We see a significant opportunity to build on existing public investments and scale promising structural interventions that can ensure that all people and all groups benefit from a healthy, equitable, and inclusive information environment that can support effective responses to current and future public health challenges.
Funding/Support: None.
Conflict of Interest Disclosures: Both authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest. No conflicts were reported.
References
- 1. Centers for Disease Control and Prevention (CDC) . COVID‐19 in racial and ethnic minority groups. 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html. Accessed May, 04, 2020.
- 2. Almsay S, Yan H, Holcombe M. Coronavirus hitting some African American communities extremely hard. CNN. April 6, 2020.
- 3. Maryland Department of Health. Coronavirus disease 2019 (COVID‐19) outbreak . https://coronavirus.maryland.gov. 2020. Accessed April 10, 2020.
- 4. Levenson E. Why black Americans are at higher risk for coronavirus. CNN. April 7, 2020.
- 5. Smith B, Magnani JW. New technologies, new disparities: the intersection of electronic health and digital health literacy. Int J Cardiol. 2019;292:280‐282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ballew M, Bergquist P, Goldberg M, et al. American public responses to COVID‐19. New Haven, CT: Yale University and George Mason University, Yale Program on Climate Change Communication; 2020. [Google Scholar]
- 7. Martin R. S.C. senator says getting COVID‐19 information to African Americans will “save lives.” NPR. April 4, 2020.
- 8. Scott E. 4 reasons coronavirus is hitting black communities so hard. Washington Post. April 10, 2020.
- 9. Healthy People 2020 . Social determinants of health. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. Accessed June 10, 2020.
- 10. McCormack L, Sheridan S, Lewis M, Boudewyns V, Melvin C, Kistler C . Communication and dissemination strategies to facilitate the use of health‑related evidence. Rockville, MD: Agency for Healthcare Research and Quality; 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Viswanath K, Emmons KM. Message effects and social determinants of health: its application to cancer disparities. J Commun. 2006;56(Suppl.1):S238‐S264. [Google Scholar]
- 12. Niederdeppe J, Bu LQ, Borah P, Kindig DA, Robert SA. Message design strategies to raise public awareness of social determinants of health and population health disparities. Milbank Q. 2008;86(3):481‐513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dorfman L, Wallack L. Moving nutrition upstream: the case for reframing obesity. J Nutr Education Behav. 2007;39(Suppl.2):S45‐S50. [DOI] [PubMed] [Google Scholar]
- 14. Wilkin HA. Exploring the potential of communication infrastructure theory for informing efforts to reduce health disparities. J Commun. 2013;63(1):181‐200. [Google Scholar]
- 15. Van Winkle B, Carpenter N, Moscucci M. Why aren't our digital solutions working for everyone? AMA J Ethics. 2017;19(11):1116‐1124. [DOI] [PubMed] [Google Scholar]
- 16. Kim Y‐C, Moran MB, Wilkin HA, Ball‐Rokeach SJ. Integrated connection to neighborhood storytelling network, education, and chronic disease knowledge among African Americans and Latinos in Los Angeles. J Health Commun. 2011;16(4):393‐415. [DOI] [PubMed] [Google Scholar]
- 17. Ramsetty A, Adams C. Impact of the digital divide in the age of COVID‐19. J Am Med Inform Assoc. 2020;27(7):1147‐1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mantwill S, Monestel‐Umaña S, Schulz PJ. The relationship between health literacy and health disparities: a systematic review. PLOS ONE. 2015;10(12):e0145455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stormacq C, Van den Broucke S, Wosinski J. Does health literacy mediate the relationship between socioeconomic status and health disparities? Integrative review. Health Promotion Inter. 2018;34(5):e1‐e17. [DOI] [PubMed] [Google Scholar]
- 20. Kontos E, Bennett GG, Viswanath K. Barriers and facilitators to home computer and internet use among urban novice computer users of low socioeconomic position. J Med Internet Res. 2007;9(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kreuter MW, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav. 2003;27(1):S227‐S232. [DOI] [PubMed] [Google Scholar]
- 22. Eligon J, Burch ADS. Questions of bias in COVID‐19 treatment add to the mourning for black families. New York Times. May, 20, 2020. https://www.nytimes.com/2020/05/10/us/coronavirus-african-americans-bias.html.
- 23. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Sci. 2011;6(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rice L, Sara R. Updating the determinants of health model in the information age. Health Promotion Inter. 2019;34(6):1241‐1249. [DOI] [PubMed] [Google Scholar]
- 25. Ackerson LK, Viswanath K. The social context of interpersonal communication and health. J Health Commun. 2009;14(Supp.1):5‐17. [DOI] [PubMed] [Google Scholar]
- 26. Yanovitzky I, Weber MS. News media as knowledge brokers in public policymaking processes. Commun Theory. 2019;29(2):191‐212. [Google Scholar]
- 27. Matsaganis MD, Wilkin HA. Communicative social capital and collective efficacy as determinants of access to health‐enhancing resources in residential communities. J Health Commun. 2015;20(4):377‐386. [DOI] [PubMed] [Google Scholar]
- 28. Hossain L, Kuti M. Disaster response preparedness coordination through social networks. Disasters. 2010;34(3):755‐786. [DOI] [PubMed] [Google Scholar]
- 29. Friedland L, Napoli P, Ognyanova K, Weil C, Wilson EJ III. Review of the literature regarding critical information needs of the American public. Unpublished manuscript submitted to the Federal Communications Commission. https://transition.fcc.gov/bureaus/ocbo/Final_Literature_Review.pdf2012. Accessed January 21, 2021. [Google Scholar]
- 30. Napoli PM, Stonbely S, McCollough K, Renninger B. Local journalism and the information needs of local communities: toward a scalable assessment approach. Journalism Pract. 2017;11(4):373‐395. [Google Scholar]
- 31. Kim Y‐C, Jung J‐Y, Ball‐Rokeach SJ. “Geo‐ethnicity” and neighborhood engagement: a communication infrastructure perspective. Political Commun. 2006;23(4):421‐441. [Google Scholar]
- 32. Ray R, Brown M, Fraistat N, Summers E. Ferguson and the death of Michael Brown on Twitter: #BlackLivesMatter, #TCOT, and the evolution of collective identities. Ethnic Racial Stud. 2017;40(11):1797‐1813. [Google Scholar]
- 33. Domínguez S, Arford T. It is all about who you know: social capital and health in low‐income communities. Health Sociol Rev. 2010;19(1):114‐129. [Google Scholar]
- 34. Basu A, Dutta MJ. The relationship between health information seeking and community participation: the roles of health information orientation and efficacy. Health Commun. 2008;23(1):70‐79. [DOI] [PubMed] [Google Scholar]
- 35. Carlson BA, Neal D, Magwood G, Jenkins C, King MG, Hossler CL. A community‐based participatory health information needs assessment to help eliminate diabetes information disparities. Health Promotion Pract. 2006;7(Suppl.3):213S‐222S. [DOI] [PubMed] [Google Scholar]
- 36. Bejarano WA. Analyzing town hall meetings to identify information gaps in the opioid crisis. Drug Alcohol Dependence. 2019;197:164‐167. [Google Scholar]
- 37. Yanovitzky I. A multiyear assessment of public response to a statewide drug take‐back and disposal campaign, 2010 to 2012. Health Education Behav. 2017;44(4):590‐597. [DOI] [PubMed] [Google Scholar]
- 38. Swire‐Thompson B, Lazer D. Public health and online misinformation: challenges and recommendations. Annu Rev Public Health. 2020;41(1):433‐451. [DOI] [PubMed] [Google Scholar]
- 39. Eysenbach G. Infodemiology and infoveillance: framework for an emerging set of public health informatics methods to analyze search, communication and publication behavior on the internet. J Med Internet Res. 2009;11(1):e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Yang F‐C, Lee AJT, Kuo S‐C. Mining health social media with sentiment analysis. J Med Syst. 2016;40(11):236. [DOI] [PubMed] [Google Scholar]
- 41. Ognyanova K, Lazer D, Robertson RE, Wilson C. Misinformation in action: fake news exposure is linked to lower trust in media, higher trust in government when your side is in power. Harvard Kennedy School Misinformation Rev. June 2, 2020. [Google Scholar]
- 42. Nossel S, Vilk V. As we confront a pandemic, U.S. state and federal government must support local news. Slate . March 27, 2020. https://slate.com/technology/2020/03/coronavirus-local-news-funding.html. Accessed June 10, 2020.
- 43. Stelter B. New Jersey poised to invest $5 million into local journalism. July 3, 2018. CNN Business. Accessed September 30, 2020.
- 44. Hering JG. Do we need “more research” or better implementation through knowledge brokering? Sustainability Sci. 2016;11(2):363‐369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ovretveit J, Hempel S, Jennifer LM, Brian SM, Lisa VR, David AG. Guidance for research‐practice partnerships (R‐PPs) and collaborative research. J Health Organ Manage. 2014;28(1):115‐126. [DOI] [PubMed] [Google Scholar]
- 46. Friedman DB, Tanner A, Rose ID. Health journalists’ perceptions of their communities and implications for the delivery of health information in the news. J Community Health. 2014;39(2):378‐385. [DOI] [PubMed] [Google Scholar]
- 47. Rimal RN, Lapinski MK. Why health communication is important in public health. B World Health Organ. 2009;87(4):247‐247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Liyanage C, Elhag T, Ballal T, Li Q. Knowledge communication and translation—a knowledge transfer model. J Knowledge Manage. 2009;13(3):118‐131. [Google Scholar]


