Abstract
BACKGROUND AND PURPOSE:
A major concern after emergent intracranial angioplasty in cases of acute stroke with underlying intracranial stenosis is the acute reocclusion of the treated arteries. This study reports the incidence and clinical outcomes of acute reocclusion of arteries following emergent intracranial angioplasty with or without stent placement for the management of patients with acute stroke with underlying intracranial atherosclerotic stenosis.
MATERIALS AND METHODS:
Forty-six patients with acute stroke received emergent intracranial angioplasty with or without stent placement for intracranial atherosclerotic stenosis and underwent follow-up head CTA. Acute reocclusion was defined as “hypoattenuation” within an arterial segment with discrete discontinuation of the arterial contrast column, both proximal and distal to the hypoattenuated lesion, on CTA performed before discharge. Angioplasty was defined as “suboptimal” if a residual stenosis of ≥50% was detected on the postprocedural angiography. Clinical and radiologic data of patients with and without reocclusion were compared.
RESULTS:
Of the 46 patients, 29 and 17 underwent angioplasty with and without stent placement, respectively. Acute reocclusion was observed in 6 patients (13%) and was more frequent among those with suboptimal angioplasty than among those without it (71.4% versus 2.6%, P < .001). The relative risk of acute reocclusion in patients with suboptimal angioplasty was 27.857 (95% confidence interval, 3.806–203.911). Furthermore, a good outcome was significantly less frequent in patients with acute reocclusion than in those without it (16.7% versus 67.5%, P = .028).
CONCLUSIONS:
Acute reocclusion of treated arteries was common after emergent intracranial angioplasty with or without stent placement in patients with acute stroke with intracranial atherosclerotic stenosis and was associated with a poor outcome. Suboptimal results of angioplasty appear to be associated with acute reocclusion, irrespective of whether stent placement was performed.
Intracranial atherosclerotic stenosis (ICAS) is rapidly becoming a major concern worldwide in patients with stroke because Asian, Hispanic, and African populations, which are prone to ICAS, constitute an overwhelming majority of the population of the world.1 Acute stroke caused by an in situ thrombosis at the site of ICAS differs from that caused by cardiogenic embolic occlusion and may not respond to modern mechanical embolectomy procedures such as stent-retriever embolectomy or manual aspiration embolectomy. Few studies have been published hitherto on the optimal treatment plan for patients with acute stroke with underlying ICAS.2–5 Emergent intracranial angioplasty, with or without stent placement, has been recently suggested as an effective treatment option for the management of underlying ICAS following mechanical embolectomy; for example, Yoon et al4 reported a successful revascularization rate of 95% and a favorable outcome rate of 65% with this strategy.
Nevertheless, a major concern after emergent intracranial angioplasty in cases of acute stroke is the acute reocclusion of the treated arteries. Acute reocclusion may occur following intracranial angioplasty or stent placement as a result of platelet activation, adherence, and aggregation triggered by the disruption of vulnerable plaque and endothelial damage; unsuccessful or inadequate pretreatment with antiplatelet drugs; dissection; or vasospasm.6 Despite the possibility of this complication in patients with acute stroke, data regarding its incidence and clinical consequences have not yet been reported in literature, to our knowledge.
Thus, this study aimed to investigate the incidence and clinical outcomes of arterial reocclusion in patients with acute stroke undergoing emergent angioplasty with or without stent placement following stent-retriever embolectomy. Additionally, we sought to determine the risk factors associated with acute reocclusion in these patients.
Materials and Methods
Patients
Between January 2011 and February 2014, 240 patients with acute ischemic stroke were treated with mechanical embolectomy at our comprehensive regional stroke center. Of these, 50 (20.8%) consecutive patients with underlying ICAS as a cause of acute large-vessel occlusion underwent emergent intracranial angioplasty with or without stent placement subsequent to mechanical embolectomy. Forty-six of these patients underwent follow-up head CTA after endovascular therapy, as per our institutional protocol for acute stroke management. The remaining 4 patients could not undergo CTA during hospitalization due to their poor health status. Thus, 46 patients were finally enrolled in this retrospective study, and their clinical and radiologic data were analyzed. The institutional ethics committee approved this retrospective analysis and waived informed consent due to the retrospective study design.
On admission, a stroke neurologist performed an assessment by using the NIHSS. Before the initiation of endovascular treatment, all patients underwent nonenhanced cranial CT and multimodal MR imaging. The inclusion criteria for endovascular therapy were as follows: presentation within 6 and 8 hours of stroke onset for anterior and posterior circulation stroke, respectively; a baseline NIHSS score of ≥4; no evidence of intracranial hemorrhage on cranial CT or MR imaging; evidence of major arterial occlusion on MR angiography; a target mismatch pattern on multimodal MR imaging based on visual estimation (time-to-peak map of perfusion imaging showing a lesion volume ≥30% larger than that detected with DWI) for an anterior circulation stroke; an infarct volume of less than one-third of the MCA territory for anterior circulation stroke, as determined by DWI or nonenhanced CT; an absence of bilateral diffuse pontine ischemia on DWI for posterior circulation stroke; and a premorbid mRS score of ≤3.
Endovascular Therapy
All endovascular therapy was performed by a single interventional neuroradiologist with 12 years of experience in neurovascular intervention. For each patient, written informed consent for endovascular therapy was obtained from a family member. Both cerebral angiography and endovascular therapy were performed with the patient under conscious sedation. In case of agitation, an intravenous bolus of midazolam was administered and repeated if necessary. When pretreatment diagnostic angiography showed an arterial occlusion, stent-retriever embolectomy with the Solitaire stent (Covidien, Irvine, California) was performed as the first-line endovascular treatment. When stent-retriever embolectomy was unsuccessful, other mechanical approaches were performed, including manual aspiration embolectomy by using a Penumbra aspiration catheter (Penumbra, Alameda, California). The details of the techniques used for mechanical embolectomy have been described previously.7,8
If severe (>70%) underlying ICAS of the target artery was seen on the initial diagnostic angiography or on follow-up angiography after mechanical embolectomy, intracranial angioplasty with or without stent placement was performed. The severity of arterial stenosis was graded according to the Warfarin-Aspirin Symptomatic Intracranial Disease criteria.9 For underlying ICAS seen after the initial mechanical embolectomy, ICAS was determined if the stenotic lesion remained unchanged 3–5 minutes after intra-arterial injection of a vasodilator through the guide catheter. The devices and techniques used for intracranial angioplasty and stent placement have been described in detail elsewhere.4
Neither heparin nor glycoprotein IIb/IIIa inhibitor was administered either intravenously or intra-arterially during the endovascular procedure. All patients underwent nonenhanced CT immediately after endovascular therapy. If no intracranial hemorrhage was detected on this scan, aspirin and clopidogrel (Plavix) were administered orally via the nasogastric tube after the procedure. Dual antiplatelet therapy was then continued for at least 3 months after the procedure.
CTA Image Acquisition and Analysis
CTA was performed on a dual-source CT scanner (Somatom Definition Flash; Siemens, Erlangen, Germany) with the following parameters: collimation, 128 × 0.6 mm; tube voltage, 120 kV; tube current, 250 mA; gantry rotation, 0.28 seconds; pitch factor, 0.6; FOV, 180 mm; and matrix, 512 × 512. All patients were administered 100 mL of nonionic contrast agent with 350 mg of iodine per milliliter (iohexol, Omnipaque 350; GE Healthcare, Piscataway, New Jersey), which was injected into the antecubital vein at a rate of 4 mL/s. Scanning was triggered by the bolus-tracking technique with the ROI positioned in the aortic arch and the trigger threshold set at 25 HU. CTA source images were then reconstructed with a section width of 0.75 mm for further evaluation. The source images were transferred to the workstation and processed with the use of a commercial software package (syngo.CT Dynamic Angio; Siemens). Thick, maximum-intensity-projection images (section thickness, 30 mm; increments, 5 mm) were reconstructed in axial, coronal, sagittal, and oblique coronal planes to evaluate the intracranial arteries.
Maximum-intensity-projection and source images of all patients were reviewed by 2 neuroradiologists and were evaluated for the presence or absence of occlusion or stenosis of ≥50% at the site of previous angioplasty or stent placement. Decisions were made by consensus between the 2 investigators. Arterial occlusion was defined as a hypoattenuation within the arterial segment with discrete discontinuation of the arterial contrast column between the proximal and distal points of the hypoattenuated lesion.
Outcome Measures
We recorded the clinical and radiologic data from the medical records of the patients. The “start of endovascular therapy” was defined as the moment the needle punctured the common femoral artery. “Symptomatic intracranial hemorrhage” was defined as any intracranial hemorrhage that caused neurologic deterioration, which was a ≥4-point increase in the NIHSS score or a 1-point deterioration in the level of consciousness.
Revascularization status was assessed by using the final angiogram according to the modified TICI scale,10 with “successful revascularization” defined as a modified TICI grade of 2b or 3. “Arterial perforation” was defined by evidence of frank angiographic contrast extravasation on serial angiograms. “Arterial dissection” was defined as an identifiable, intimal flap on the final angiogram. The angiographic findings were characterized as either “optimal” (<50% residual stenosis) or “suboptimal” (≥50% residual stenosis) on the final angiogram.11,12 Angiographic images were evaluated by 2 neuroradiologists in consensus.
Neurologic evaluation was performed by a stroke neurologist immediately and 24 hours after treatment, before discharge, 3 months after treatment, and when there were any changes in clinical symptoms. Clinical outcome was assessed by a stroke neurologist by using the mRS score during an outpatient visit 3 months after treatment. If patients were unable to attend the outpatient clinic, assessment was made via telephone interviews. A good clinical outcome was defined as an mRS score of ≤2 or equal to the premorbid mRS score.
Statistical Analysis
Continuous variables are presented as medians and interquartile ranges (IQRs). Discrete variables are presented as counts and percentages. First, patients were divided into 2 groups for comparison, according to the presence or absence of acute reocclusion on head CTA. The baseline characteristics and clinical outcomes of the 2 groups were compared. Second, the relationship between each clinical and radiologic characteristic and the 3-month outcome was determined. The χ2 or Fisher exact test was used for comparing categoric and binary data, and the Mann-Whitney U test was used for comparing continuous data. Third, a logistic regression analysis was performed to identify independent predictors of good clinical outcome. The variables tested in the logistic regression models were those with P < .05 in the univariate analysis, age, and successful revascularization. All statistical analyses were performed with SPSS software (Version 21.0; IBM, Armonk, New York). A P value < .05 was significant.
Results
Data from 46 patients were analyzed. Baseline patient characteristics are shown in Table 1. Of the 46 patients treated with emergent angioplasty with or without stent placement for acute stroke, 26 had ICAS in the MCA; 12, in the basilar artery; and 8, in the intracranial internal carotid artery. Follow-up CTA was performed within 48 hours of endovascular therapy in 45 patients (97.8%). The remaining patient underwent CTA 120 hours after endovascular therapy.
Table 1:
Baseline characteristics of the study population
| All Patients (N = 46) | Patients with Acute Reocclusion (n = 6) | Patients without Acute Reocclusion (n = 40) | P Value | |
|---|---|---|---|---|
| Age (yr) (IQR) | 66 (57.75–74.75) | 63 (57.5–72.5) | 66 (57.5–76.25) | NS |
| Male sex (No.) (%) | 28 (60.9) | 3 (50) | 25 (62.5) | NS |
| Risk factors (No.) (%) | ||||
| Hypertension | 29 (63) | 4 (66.7) | 25 (62.5) | NS |
| Diabetes mellitus | 20 (43.6) | 2 (33.3) | 18 (45) | NS |
| Dyslipidemia | 26 (56.5) | 4 (66.7) | 22 (55) | NS |
| Smoking | 10 (21.7) | 2 (33.3) | 8 (20) | NS |
| Atrial fibrillation | 4 (8.7) | 0 (0) | 4 (10) | NS |
| Previous CAD | 1 (2.2) | 0 (0) | 1 (2.5) | NS |
| Congestive heart failure | 1 (2.2) | 0 (0) | 1 (2.5) | NS |
| History of stroke or TIA | 8 (17.4) | 4 (66.7) | 4 (10) | .005 |
| Occlusion site (No.) (%) | ||||
| Middle cerebral artery | 26 (56.5) | 5 (83.3) | 21 (52.5) | NS |
| Internal carotid artery | 8 (17.4) | 0 (0) | 8 (20) | NS |
| Basilar artery | 12 (26.1) | 1 (16.7) | 11 (27.5) | NS |
| Baseline NIHSS score (IQR) | 12 (8–14) | 9.5 (6.5–14.5) | 10 (9–14) | NS |
| Intravenous thrombolysis (No.) (%) | 18 (39.1) | 4 (66.7) | 14 (35) | NS |
| Intra-arterial thrombolysis (No.) (%) | 7 (15.2) | 1 (16.7) | 6 (15) | NS |
| Time to procedure (min) (IQR) | 270 (207.75–362) | 277.5 (233.75–330.00) | 252.5 (187.5–360) | NS |
| Procedural time (min) (IQR) | 36 (25–46.75) | 33 (22.75–47.25) | 37 (25.75–48.75) | NS |
| Time to revascularization (min) (IQR) | 319.5 (231.75–401.5) | 305 (264.75–385.75) | 301 (217.5–407) | NS |
| Postprocedural residual stenosis (%) (IQR) | 25 (19.5–35.0) | 56 (42.3–71.3) | 25 (19–33) | 0.009 |
| Postprocedural antiplatelet therapy (No.) (%) | 41 (89.1) | 6 (100) | 35 (87.5) | NS |
Note:—CAD indicates coronary artery disease; NS, not significant.
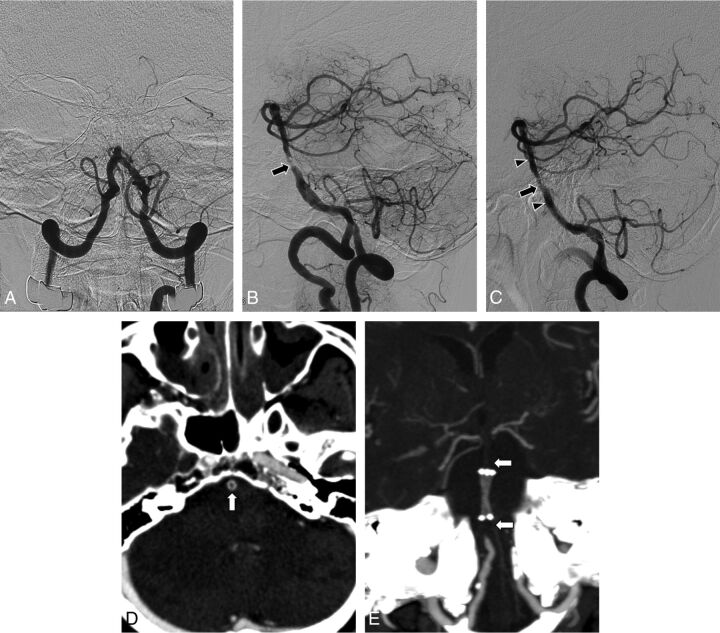
Follow-up CTA showed reocclusion at the site of angioplasty or stent placement in 6 patients (13%), with reocclusion occurring in the MCA in 5 patients and in the basilar artery in 1 patient (Fig 1). A history of previous stroke or TIA was more frequent in patients with reocclusion (66.7% versus 10%, P = .005) than in those without it. Postprocedural residual stenosis was significantly greater in patients with acute reocclusion (56% versus 25%, P = .009). No significant intergroup differences were noted in terms of patient age, sex, history of other risk factors, occlusion sites, use of intravenous or intra-arterial thrombolysis, time to procedure, duration of the procedure, time to revascularization, and baseline NIHSS score. Severe stenosis (≥50%) at the site of angioplasty or stent placement was not observed in the remaining 40 patients.
Fig 1.
Brain images obtained in a patient with acute stroke. A, Anteroposterior view of a vertebral angiogram shows arterial occlusion at the proximal portion of the basilar artery. B, Lateral projection of the vertebral angiogram obtained after stent-retriever embolectomy reveals severe underlying stenosis (arrow) at the site of arterial occlusion. There were no retrieved thrombi with the Solitaire stent. C, Lateral projection of vertebral angiography performed after intracranial stent placement shows suboptimal angioplasty, with residual stenosis of 60% (arrow). Arrowheads indicate the proximal and distal ends of the stent. D, Axial source image of CTA shows hypoattenuation (arrow) within the stented segment of the basilar artery. E, Maximum-intensity-projection image of the follow-up CTA 2 days after the procedure shows a discontinuation of the contrast column both proximal and distal to the stent (arrows).
Thirty-two patients underwent both intracranial angioplasty and stent placement, while 14 patients underwent only angioplasty. Acute reocclusion was more frequent among patients treated with intracranial angioplasty alone than among those treated with intracranial stent placement in addition to angioplasty (23.5% versus 6.9%); however, this difference was not statistically significant (P = .174). Of the 46 patients, 41 received antiplatelet medication after completion of endovascular therapy; 5 patients did not receive this therapy because they showed evidence of intracranial hemorrhage in the postprocedural CT scan. However, none of these 5 patients exhibited acute reocclusion on follow-up CTA.
Of 6 patients with reocclusion, 4 patients had an ASPECTS of 8, 1 had an ASPECTS of 7, and 1 had a posterior circulation ASPECTS of 5 on pretreatment DWI. The NIHSS score gradually increased by 2–5 points during the first 24 hours after endovascular therapy in all 6 patients with reocclusion. At the time of discharge, the NIHSS score was unchanged in 3 patients, decreased in 2 patients (by 2 and 4 points, respectively), and slightly increased in 1 patient (by 3 points) compared with the score on day 1.
The clinical outcomes of patients with or without acute reocclusion are shown in Table 2. Overall, successful revascularization (modified TICI grade 2b or 3) was achieved in 95.7% (44/46) of patients. There was no significant difference between the 2 groups in terms of the rate of successful revascularization. A suboptimal result (≥50% residual stenosis at the site of angioplasty or stent placement) was observed on the final angiograms in 7 patients (15.2%). Furthermore, acute reocclusion was more frequent among patients with a suboptimal result than among those without (71.4% [5/7] versus 2.6% [1/39], P < .001). The relative risk for acute reocclusion in patients with a suboptimal result was 27.857 (95% CI, 3.806–203.911). Overall, a good clinical outcome was achieved in 60.9% (28/46) of patients. A good outcome was less frequent in patients with acute reocclusion than in those without it (16.7% versus 67.5%, P = .028); the relative risk of a poor outcome in patients with acute reocclusion was 2.564 (95% CI, 1.447–4.544).
Table 2:
Comparison of clinical outcomes between patients with and without acute reocclusion
| All Patients (N = 46) | Patients with Acute Reocclusion (n = 6) | Patients without Acute Reocclusion (n = 40) | P Value | |
|---|---|---|---|---|
| m-TICI grade 2b or 3 (No.) (%) | 44 (95.7) | 5 (83.3) | 39 (97.5) | NS |
| Suboptimal result (No.) (%) | 7 (15.2) | 5 (83.3) | 2 (5) | <.001 |
| mRS 0–2 (No.) (%) | 28 (60.9) | 1 (16.7) | 27 (67.5) | .028 |
| Symptomatic hemorrhage (No.) (%) | 2 (4.3) | 0 (0) | 2 (5) | NS |
| Mortality (No.) (%) | 3 (6.5) | 0 (0) | 3 (7.5) | NS |
Note:—m-TICI indicates modified TICI; NS, not significant.
Arterial perforation of a thalamoperforating artery by microguidewire occurred in 1 patient. Arterial dissection was not observed in the postprocedural angiograms of any patients. Overall, 2 patients (4.3%) without acute reocclusion had symptomatic hemorrhage, while 3 patients (6.5%) without acute reocclusion died before the 3-month follow-up. However, none of the patients with acute reocclusion showed symptomatic hemorrhage or 3-month mortality. There was no significant difference between the 2 groups in the rate of symptomatic hemorrhage and mortality.
In a univariate analysis, the following variables were identified as predictors of a good outcome at 3 months: acute reocclusion, history of stroke or TIA, and procedural time. A good outcome occurred less frequently among patients with a history of previous stroke or TIA than among those without (12.5% [1/8] versus 71.1% [27/38], P = .004). The median procedural time was shorter in patients with a good outcome than in those with a poor outcome (35 minutes [IQR, 25–42 minutes] versus 44 minutes [IQR, 32.75–62 minutes], P = .019). When acute reocclusion, history of previous stroke or TIA, procedural time, each year of age, and successful revascularization were selected for the logistic regression analysis, independent predictors of good outcome were a history of previous stroke or TIA (OR, 0.055; 95% CI, 0.004–0.821; P = .035) and procedural time (per 1-minute decrease; OR, 1.046; 95% CI, 1.000–1.093; P = .048).
Discussion
The main findings of this study are summarized as follows: 1) acute reocclusion of arteries treated with emergent angioplasty with or without stent placement was fairly common in this study population, at a rate of 13%; 2) suboptimal angioplasty with or without stent placement was significantly associated with acute reocclusion; and 3) acute reocclusion was significantly associated with a poor outcome at 3-month follow-up.
Few studies have been published thus far on the incidence of acute reocclusion after intracranial angioplasty in acute stroke. Consistent with our study, Lee et al2 reported that early reocclusion occurred within 48 hours in 16.7% (2/12) of patients with acute MCA occlusion after intracranial stent placement for the treatment of underlying ICAS. Additionally, Guo et al13 reported that acute reocclusion occurred in 9.1% (1/11) of patients within 1 day of intracranial stent placement. Moreover, Bang et al14 reported that in-stent thrombosis occurred within 1 week in 18.8% (6/32) of their patients who underwent intracranial stent placement for acute ischemic stroke. However, the latter 2 studies differ from our study and that of Lee et al in that stent placement was attempted to recanalize the embolic occlusions and not to treat the underlying ICAS. Furthermore, those studies did not provide data on specific stroke etiology or postprocedural antiplatelet medication for the treated patients.
In our study, suboptimal angioplasty (≥50% residual stenosis) seemed to be a main predisposing factor for acute reocclusion. Suboptimal angioplasty was associated with a 28-fold increase in the rate of acute reocclusion in the present study. A suboptimal result may cause insufficient blood flow through the angioplasty-treated or stented arterial segment, thereby accelerating platelet aggregation. Sufficient blood flow at the site of angioplasty, with or without stent placement, prevents acute thrombus formation.15 Thus, our findings strongly suggest that neurointerventionists should pay particular attention to achieving optimal patency of the target artery during emergent intracranial angioplasty or stent placement for the treatment of underlying ICAS in patients with acute stroke.
A systematic review has shown that the frequency of reocclusion after stent placement is lower than after angioplasty alone in patients undergoing acute coronary interventions.16 Similarly, intracranial stent placement has been shown to be more effective than angioplasty alone in postoperative residual stenosis or late restenosis in cases of subacute-to-chronic symptomatic ICAS.12,17 Stent placement has been associated with a lower incidence of acute reocclusion than angioplasty alone, by eliminating vascular recoil and dissection and allowing increased vessel diameter.15 In our study, we also noted a trend toward a lower incidence of acute reocclusion among patients treated with stent placement than among those treated with angioplasty alone (6.9% versus 23.5%); however, this difference was not statistically significant, probably due to the small sample size.
Angioplasty with or without stent placement may lead to mechanical disruption of atherosclerotic plaques or endothelial injury that triggers platelet activation, adhesion, and aggregation, which are key features of arterial thrombosis and reocclusion. Therefore, adequate antiplatelet therapy is generally recommended to prevent acute thrombosis and reocclusion in cases of scheduled intracranial angioplasty or stent placement. Although optimal doses of antiplatelet therapy for periprocedural support during endovascular stroke therapy have not yet been established, loading doses of aspirin (300–650 mg) and clopidogrel (600 mg) are generally recommended, followed by daily doses of aspirin (100–300 mg) and clopidogrel (75 mg) for 1–3 months.18 Most interesting, the administration of periprocedural antiplatelet therapy did not appear to be associated with acute reocclusion in our study. There was no acute reocclusion in the 5 patients who did not receive postprocedural antiplatelet therapy in our study. All patients with acute reocclusion received loading doses of aspirin and clopidogrel after the procedure. Therefore, further studies are necessary to determine the exact role of periprocedural antiplatelet therapy in patients undergoing emergency angioplasty with or without stent placement for the management of acute ischemic stroke in patients with ICAS.
There have been no studies to date on the clinical consequences of acute reocclusion after emergency angioplasty with or without stent placement in patients with acute stroke due to ICAS. In our study, a good outcome was considerably less frequent among patients with acute reocclusion than among those without it (16.7% versus 67.5%, P = .028); in fact, acute reocclusion was associated with a 2.6-fold increase in poor outcome at the 3-month follow-up. Similar results have been reported in a study on the immediate reocclusion of recanalized arteries during intra-arterial thrombolysis for embolic occlusion. Janjua et al19 showed that a favorable outcome was less frequently achieved in patients with immediate arterial reocclusion after various endovascular treatments than in those without it (6% versus 37%, P = .01). The odds ratio of a poor outcome in patients with arterial reocclusion was 3.9 in their analysis.19
The limitations of our study include its small sample size and retrospective design. While most patients (97.8%) underwent head CTA 2 days after endovascular therapy, 1 patient underwent the procedure 5 days after the operation. In addition, platelet function testing was not routinely performed. Thus, individualizing antiplatelet therapy was not possible; this situation may have influenced the incidence of acute reocclusion in this study. However, the impact of clopidogrel resistance on the effectiveness of endovascular therapy for acute ischemic stroke remains largely unstudied. Furthermore, routine platelet-function testing is not currently recommended in cases of acute coronary intervention.18,20
Conclusions
Our findings indicate that acute reocclusion of treated vessels with or without stent placement after emergent angioplasty is common in patients with acute stroke due to ICAS and that this complication is associated with a poor outcome. Acute reocclusion in such cases appears to be associated with suboptimal angioplasty or stent placement. In light of these results, neurointerventionists should make every effort to achieve optimal results in restoring the patency of the affected artery during emergent angioplasty in cases of acute stroke due to ICAS.
ABBREVIATIONS:
- ICAS
intracranial atherosclerotic stenosis
- IQR
interquartile range
References
- 1. Gorelick PB, Wong KS, Bae HJ, et al. Large artery intracranial occlusive disease: a large worldwide burden but a relatively neglected frontier. Stroke 2008;39:2396–99 10.1161/STROKEAHA.107.505776 [DOI] [PubMed] [Google Scholar]
- 2. Lee HK, Kwak HS, Chung GH, et al. Balloon-expandable stent placement in patients with immediate reocclusion after initial successful thrombolysis of acute middle cerebral arterial obstruction. Interv Neuroradiol 2012;18:80–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kang DH, Kim YW, Hwang YH, et al. Instant reocclusion following mechanical thrombectomy of in situ thromboocclusion and the role of low-dose intra-arterial tirofiban. Cerebrovasc Dis 2014;37:350–55 10.1159/000362435 [DOI] [PubMed] [Google Scholar]
- 4. Yoon W, Kim SK, Park MS, et al. Endovascular treatment and the outcomes of atherosclerotic intracranial stenosis in patients with hyperacute stroke. Neurosurgery 2015;76:680–86; discussion 686 10.1227/NEU.0000000000000694 [DOI] [PubMed] [Google Scholar]
- 5. Behme D, Weber W, Mpotsaris A. Acute basilar artery occlusion with underlying high-grade basilar artery stenosis: multimodal endovascular therapy in a series of seven patients. Clin Neuroradiol 2015;25:267–74 10.1007/s00062-014-0303-9 [DOI] [PubMed] [Google Scholar]
- 6. Qureshi AI, Siddiqui AM, Kim SH, et al. Reocclusion of recanalized arteries during intra-arterial thrombolysis for acute ischemic stroke. AJNR Am J Neuroradiol 2004;25:322–28 [PMC free article] [PubMed] [Google Scholar]
- 7. Yoon W, Jung MY, Jung SH, et al. Subarachnoid hemorrhage in a multimodal approach heavily weighted toward mechanical thrombectomy with Solitaire stent in acute stroke. Stroke 2013;44:414–19 10.1161/STROKEAHA.112.675546 [DOI] [PubMed] [Google Scholar]
- 8. Kim SK, Yoon W, Moon SM, et al. Outcomes of manual aspiration thrombectomy for acute ischemic stroke refractory to stent-based thrombectomy. J Neurointerv Surg 2015;7:473–77 10.1136/neurintsurg-2014-011203 [DOI] [PubMed] [Google Scholar]
- 9. Samuels OB, Joseph GJ, Lynn MJ, et al. A standardized method for measuring intracranial arterial stenosis. AJNR Am J Neuroradiol 2000;21:643–46 [PMC free article] [PubMed] [Google Scholar]
- 10. Zaidat OO, Yoo AJ, Khatri P, et al. ; Cerebral Angiographic Revascularization Grading (CARG) Collaborators, STIR Revascularization working group, STIR Thrombolysis in Cerebral Infarction (TICI) Task Force. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke 2013;44:2650–63 10.1161/STROKEAHA.113.001972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yoon W, Seo JJ, Cho KH, et al. Symptomatic middle cerebral artery stenosis treated with intracranial angioplasty: experience in 32 patients. Radiology 2005;237:620–26 10.1148/radiol.2372041620 [DOI] [PubMed] [Google Scholar]
- 12. Siddiq F, Memon MZ, Vazquez G, et al. Comparison between primary angioplasty and stent placement for symptomatic intracranial atherosclerotic disease: meta-analysis of case series. Neurosurgery 2009;65:1024–33; discussion 1033–34 10.1227/01.NEU.0000360138.54474.52 [DOI] [PubMed] [Google Scholar]
- 13. Guo XB, Song LJ, Guan S. Emergent angioplasty and stent placement recanalization without thrombolysis in acute middle cerebral artery occlusions. J Stroke Cerebrovasc Dis 2013;22:694–99 10.1016/j.jstrokecerebrovasdis.2011.10.010 [DOI] [PubMed] [Google Scholar]
- 14. Bang JS, Oh CW, Jung C, et al. Intracranial stent placement for recanalization of acute cerebrovascular occlusion in 32 patients. AJNR Am J Neuroradiol 2010;31:1222–25 10.3174/ajnr.A2055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brekenfeld C, Tinguely P, Schroth G, et al. Percutaneous transluminal angioplasty and stent placement in acute vessel occlusion: evaluation of new methods for interventional stroke treatment. AJNR Am J Neuroradiol 2009;30:1165–72 10.3174/ajnr.A1541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wilson SH, Bell MR, Rihal CS, et al. Infarct artery reocclusion after primary angioplasty, stent placement, and thrombolytic therapy for acute myocardial infarction. Am Heart J 2001;141:704–10 10.1067/mhj.2001.114971 [DOI] [PubMed] [Google Scholar]
- 17. Siddiq F, Vazquez G, Memon MZ, et al. Comparison of primary angioplasty with stent placement for treating symptomatic intracranial atherosclerotic diseases: a multicenter study. Stroke 2008;39:2505–10 10.1161/STROKEAHA.108.515361 [DOI] [PubMed] [Google Scholar]
- 18. Nahab F, Kass-Hout T, Shaltoni HM. Periprocedural antithrombotic strategies in acute ischemic stroke interventional therapy. Neurology 2012;79(13 suppl 1):S174–81 10.1212/WNL.0b013e31826959af [DOI] [PubMed] [Google Scholar]
- 19. Janjua N, Alkawi A, Suri MF, et al. Impact of arterial reocclusion and distal fragmentation during thrombolysis among patients with acute ischemic stroke. AJNR Am J Neuroradiol 2008;29:253–58 10.3174/ajnr.A0825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yousuf O, Bhatt DL. The evolution of antiplatelet therapy in cardiovascular disease. Nat Rev Cardiol 2011;8:547–59 10.1038/nrcardio.2011.96 [DOI] [PubMed] [Google Scholar]