Evaluation of a wireless fetal heart rate monitor demonstrates high agreement with heart rate, as assessed by cardiotocography, and is feasible for use at home.
OBJECTIVE:
To evaluate the accuracy, clinical utility, and usability of a wireless fetal and maternal heartbeat monitor to monitor fetal heart rate (FHR).
METHODS:
We conducted a prospective, single-center study of a convenience sample of women aged 18 years or older with a singleton pregnancy of at least 12 weeks of gestation. Fetal heart rate recordings were performed using both the heartbeat monitor and cardiotocography to evaluate accuracy. Clinicians used the heartbeat monitor in the clinic. Women used the device, unassisted, during a clinic visit or at home. Obstetricians assessed the clinical utility of FHR traces. Women rated the heartbeat monitor using the System Usability Scale.
RESULTS:
A total of 81 participants provided 126 recordings. The accuracy of the heartbeat monitor was excellent compared with cardiotocography, with limits of agreement (95%) for mean FHR between −1.6 (CI −2.0 to 1.3) and +1.0 (CI 0.7–1.4) beats per minute (bpm), mean difference −0.3 bpm, intraclass coefficient 0.99. The FHR was detected on all occasions. Clinicians took a median (interquartile range) of 0.5 (0.2–1.2) minutes to detect the FHR, obtaining a continuous trace of longer than 1 minute in 95% (39/41) of occasions. Home users took a median of 0.5 (0.2–2.0) minutes to detect the FHR, obtaining a continuous trace of longer than 1 minute in 92% (24/26) of occasions, with a median total trace time of 4.6 (4.4–4.8) minutes. The traces were deemed clinically useful in 100% (55/55) of clinician and 97% (31/32) of home recordings. The heartbeat monitor ranked in the 96–100th percentile for usability and learnability.
CONCLUSION:
The heartbeat monitor was accurate and easy for clinicians and participants to use. Data recorded at home were equivalent to those obtained using current assessment protocols for low-risk pregnancies, potentially allowing the device to be used in telehealth consultations.
CLINICAL TRIAL REGISTRATION:
Australian New Zealand Clinical Trial Registry, ACTRN12620000739910.
FUNDING SOURCES:
The HeraBEAT devices used in this study were loaned by HeraMED Pty Ltd (HeraMED, Netanya, ISRAEL). The study was supported by PHI Research Group (not-for-profit), which was responsible for Statistician fees and Research Assistants' salaries. Joondalup Health Campus provided infrastructure support, and IT services in-kind to the PHI research group.
In low-risk pregnancies, the fetal heart rate (FHR) is often monitored for 1 minute in a process known as intermittent auscultation.1–3 This is performed using a handheld Doppler, a DeLee-Hillis stethoscope, or a Pinard horn, depending on skills and resources.
As a result of the COVID-19 pandemic, many clinical services have incorporated telehealth consultations into antenatal programs, replacing some face-to-face consultations. However, whereas home monitoring of maternal parameters such as mindfulness, mood disorders, nausea, blood pressure, and weight4–7 is relatively straightforward, it is difficult to obtain clinically useful FHR traces at home.
Home FHR monitors are available, but there have been difficulties with usability, accuracy and reliability, signal noise, differentiation of fetal from maternal heart rate, inadequate recording duration, and cost.8 Handheld Doppler devices, which are used in clinics, require training to operate, cannot differentiate between FHR and maternal heart rate, and cannot store or transmit data. Although there have been attempts to use mobile cardiotocography machines, these machines are costly and not easily transportable. For home monitoring to be practical and clinically useful, FHR monitors need to be as accurate as cardiotocography machines, provide data that clinicians can interpret, be self-administered, and allow secure and reliable data transmission. A home monitor should record a defined trace for at least 1 minute to determine whether the average FHR is within the normal range (110–160 beats per minute [bpm]), evaluate variability and detect accelerations.
HeraBEAT is a medical-grade, low-cost, wireless, self-guided fetal and maternal heartbeat monitor designed for self-administration from 12 weeks of gestation. Our study objectives were to evaluate the accuracy, clinical utility, and operator usability of this monitor for both clinicians and pregnant women and assess whether the data generated were equivalent to those required by intermittent auscultation guidelines.
ROLE OF THE FUNDING SOURCE
HeraMED Pty Ltd supplied the heartbeat monitors used in the study on loan and supplied media images of the heartbeat monitor system for inclusion in the manuscript. HeraMED did not have a role in protocol design, data acquisition, or analysis. Data remain the property of the named investigators. The authors had access to relevant aggregated study data and other information (such as study protocol-analytic plan and report-validated data table, and clinical study report) required to understand and report research findings. The authors take responsibility for the presentation and publication of the research findings, have been fully involved at all stages of publication and presentation development, and are willing to take public responsibility for all aspects of the work. All individuals included as authors and contributors who made substantial intellectual contributions to the research-data analysis, and publication or presentation development are listed appropriately. The role of the sponsor in the design, execution, analysis, reporting, and funding is fully disclosed. The authors' personal interests, financial or nonfinancial, relating to this research and its publication have been disclosed.
METHODS
Ethical approval was obtained from the Ramsay Health Care Human Research Ethics Committee of Victoria and New South Wales (reference No. 2020-005).
This was a prospective, single-center, clinical study. We recruited participants as a convenience sample in the obstetrics department of a large metropolitan hospital in Western Australia. Women aged 18 years or older with a self-reported singleton pregnancy of at least 12 weeks of gestation were approached to participate in the study. Women who could not read English, who had a skin rash or condition on the abdomen that could be irritated by the ultrasound gel, or who had a pacemaker or other implantable electronic devices were excluded. Women who did not have access to a smartphone or internet connectivity were unable to participate in the home-recording sessions. Enrollment was undertaken by research nurses who explained the study and obtained written informed consent.
The heartbeat monitor is held on the abdomen by the user, weighs 130 g, and is 9 cm in diameter (Fig. 1). It employs ultra-wide beam Doppler technology and integrates a novel optical sensor to directly monitor the maternal heart rate from the abdomen, eliminating FHR–maternal heart rate cross talk. The heartbeat monitor system includes a smartphone-based interface that guides device placement and displays the FHR trace and calculated parameters (average FHR and maternal heart rate using beat-to-beat calculation, duration of FHR trace, duration of search time, and longest continuous FHR segment) on a Bluetooth-connected smartphone. A printable recording of the fetal and maternal heart rates is produced for onsite or remote review (Fig. 2). Clinicians can use a manual method to place the device directly on the appropriate position on the abdomen without voice guidance. The system is compliant with the HIPAA (Health Insurance Portability and Accountability Act) policies on privacy and transmission capabilities. The heartbeat monitor system specifications and safety claims are presented in Appendix 1, available online at http://links.lww.com/AOG/C240.
Fig. 1. Fetal heart rate monitoring system with the device and integrated smartphone interface. Image courtesy of HeraMED Ltd. Used with permission.

Porter. Assessing a Home Fetal Heart Rate Monitor. Obstet Gynecol 2021.
Fig. 2. Data output from the fetal heart rate (FHR) monitoring system. MHR, maternal heart rate.
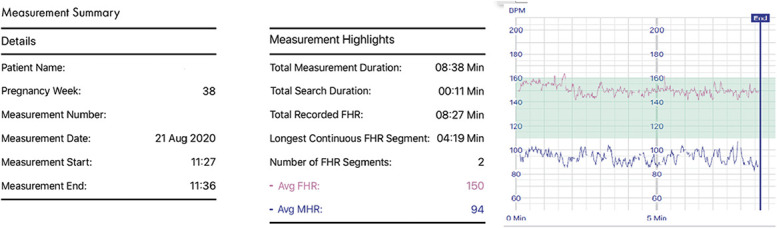
Porter. Assessing a Home Fetal Heart Rate Monitor. Obstet Gynecol 2021.
We collected data on participants' age, gestation, height, weight, body mass index (BMI, calculated as weight in kilograms divided by height in meters squared), gravidity, parity, presence of a structural uterine abnormality, and location of the placenta, as well as data from the heartbeat monitor.
All participants used the heartbeat monitor in the self-guided mode, which uses the inbuilt position guidance system. The device is activated, coated with ultrasound gel and placed below the umbilicus, directed by the smartphone interface, to a position-dependent on pregnancy gestation. The device continues to self-direct positioning using audio instructions until two distinct heart rates (FHR and maternal heart rate) are detected. Clinicians performed recordings in the antenatal clinic, where simultaneous monitoring using the heartbeat monitor and an Avalon FM20 or Avalon FM30 cardiotocography machine was undertaken to establish accuracy.
A research nurse showed participants how to use the heartbeat monitor during a 5-minute training session and asked them to record data in the clinic and at home (self-monitoring). Participants were required to use the monitor unassisted to detect and record data for longer than 1 minute. They were then asked to rate the heartbeat monitor for usability and learnability. Home recordings were done between 1 and 21 days after clinic recordings.
We assessed the accuracy of the heartbeat monitor compared with cardiotocography by calculating paired FHR measurements taken at 15-second intervals for five sequential measures. Differences in FHR (bpm) between the paired measurements were analyzed for the mean of each person’s five measurements. The agreement between the heartbeat monitor and cardiotocography was established using Bland Altman plots and 95% limits of agreement. Reliability was established using intraclass correlation coefficients using a two-way mixed-effects model. The measurement comparison was deemed accurate if the 95% limits of agreement were within 8 bpm. This target was selected in keeping with other accuracy studies9,10 of FHR monitors as a clinically acceptable range in which important features, such as fetal bradycardias, accelerations, and decelerations, can be recognized.
From the recordings done by clinicians and from home recordings, we looked at the following outcome measures: 1) detection of FHR (different from maternal heart rate), 2) number of continuous recordings longer than 1 minute, 3) total FHR recording time, 4) time taken to detect FHR, and 5) average FHR. We performed subgroup analyses to evaluate the relationship between BMI, gestation, obstetric history, and placental position on outcome measures for all participants and for the subgroup of women who were beyond 28 weeks of gestation (in which cardiotocography monitoring is typically performed). The relationship with clinical features was assessed using nonparametric tests owing to the skewed distributions (Kruskal-Wallis and Mann-Whitney U). When participants used the heartbeat monitor in the clinic, the recordings were truncated at 1 minute, and total trace times were not reported.
To examine clinical utility, obstetricians reviewed all recordings of longer than 1 minute to determine whether 1) the FHR was in the normal range, 2) separate FHRs and maternal heart rates were detected, and 3) FHR variability or accelerations were detectable during the duration of trace available. Because all recordings were shorter than required to establish a traditional baseline FHR (10 minutes), an average FHR (automatically calculated by the heartbeat monitor) was used. The recordings from home were also assessed by obstetricians for quality of data after electronic transmission.
To assess the usability and learnability of the heartbeat monitor, we used the international medical standard System Usability Scale.11 The System Usability Scale is a 10-statement survey that evaluates the learnability, reliability, and usability of products. It has been shown to have high reliability (alpha of .91) over a wide range of interface types.12 When evaluating the results, System Usability Scale raw scores are reported as means and 95% CIs, and converted to a percentile rank (0–100) with a corresponding letter grade (A+ to F), as per the System Usability Scale scoring system template (Appendix 2, available online at http://links.lww.com/AOG/C240). Comparisons between clinic and home monitoring were performed using a paired t test. We used the positive version of the System Usability Scale and included an additional adjective rating scale, a single Likert scale question that demonstrates high correlation with overall System Usability Scale scores13 (Appendix 3, available online at http://links.lww.com/AOG/C240). When reporting the adjectival rating scale, the median and interquartile range were provided given the skewed distribution. Participants completed System Usability Scale questionnaires after using the heartbeat monitor.
All data were analyzed using Stata 14.1.
RESULTS
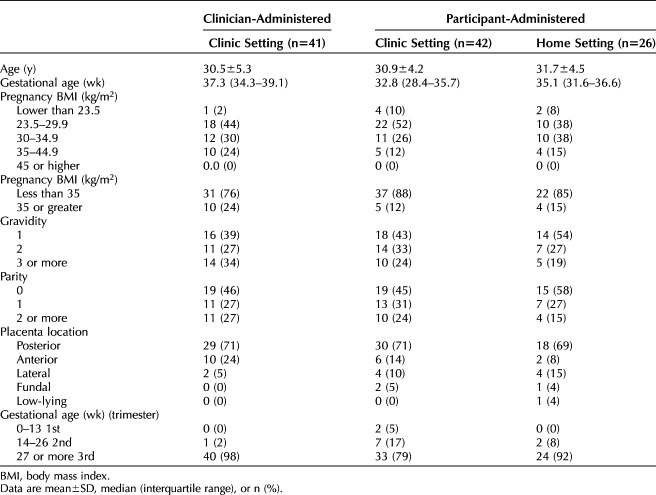
Between July and September 2020, we enrolled 81 women into the study with a total of 126 recordings available for analysis (Fig. 3 and Table 1). No adverse events were reported. The gestational age of pregnancies ranged from 12 weeks to 40 weeks. The FHR was detected on 100% of occasions by clinicians and participants (81 women, 126 recordings) who used the device.
Fig. 3. Participant involvement in the study. *Two participants were included in both the clinician and participant recording arms. †All participants who self-recorded at home were a subset of participants who self-recorded in the clinic.
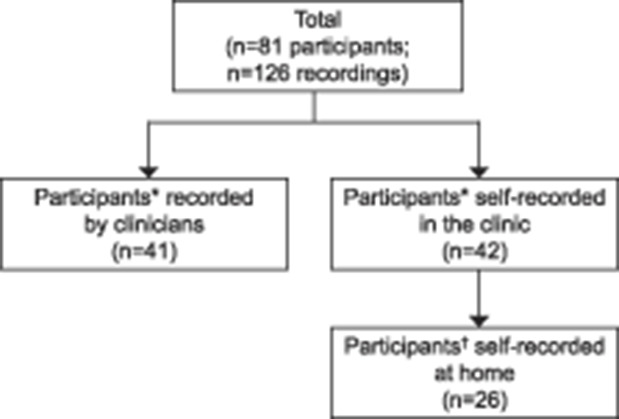
Porter. Assessing a Home Fetal Heart Rate Monitor. Obstet Gynecol 2021.
Table 1.
Demographic and Clinical Features
We compared the accuracy of the heartbeat monitor with cardiotocography using simultaneous heartbeat monitor and cardiotocography recordings from 41 women. Using only the first recording provided by each participant produced 41 recordings, totaling 214 time-paired data points, across a FHR range 120–166 bpm. Of the 214 paired measurements, the difference in FHR was 2 bpm or less in 205 (95.8%) and between 2 and 5 bpm in nine (4.2%).
When the difference between the means of the five time points for each device (n=41) was compared, the 95% limits of agreement were 1.6 (CI −2.0 to 1.3) and +1.0 (CI 0.7–1.4), with a mean difference of −0.3 bpm (Fig. 4). The intraclass coefficient was 0.99. There was no association between placental position, BMI or gestational age and difference in FHR between devices.
Fig. 4. Bland-Altman plot showing comparable accuracy between the fetal heartbeat monitor and the cardiotocograph. The difference in mean fetal heart rates over five time points (n=41).

Porter. Assessing a Home Fetal Heart Rate Monitor. Obstet Gynecol 2021.
Eleven of the 41 participants were recorded twice, giving 52 recordings and 260 time-paired data points for comparison. When all individual time-paired data points were evaluated, the 95% limits of agreement between measurement devices were −3 bpm and 2.4 bpm, with a mean difference of −0.3 bpm (Appendix 4, available online at http://links.lww.com/AOG/C240). The intraclass correlation coefficient was 0.99. Characteristics of participants with a difference of more than 2 bpm between heartbeat monitor and cardiotocography at any given time point are shown in Appendix 5, available online at http://links.lww.com/AOG/C240.
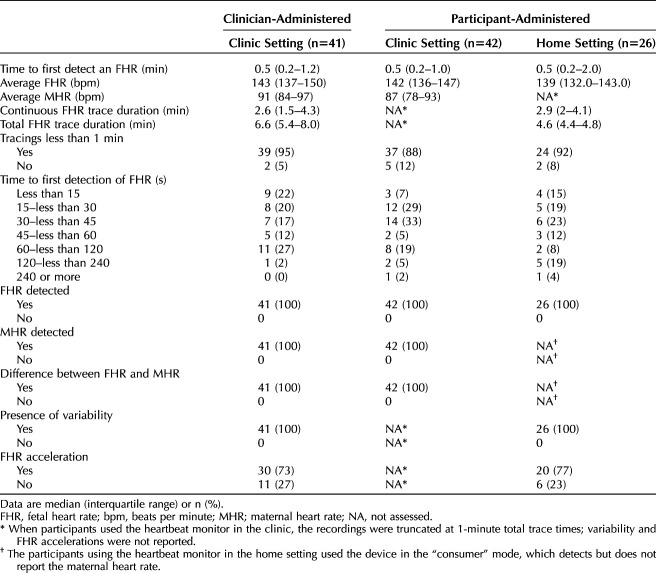
The median time taken to detect an FHR was 0.5 minutes when the device was used by clinicians (41 occasions), with all FHRs detected in less than 2 minutes, 0.5 minutes when self-recordings were done in the clinic (42 occasions), with 98% of FHRs detected in less than 2 minutes, and 0.5 minutes when self-recordings were done at home (26 occasions), with 96% of FHRs detected in less than 2 minutes (Table 2).
Table 2.
Fetal Heart Rate Metric Data
A continuous FHR trace of longer than 1 minute was recorded on 95% of occasions by clinicians, 88% of occasions by participants in the clinic, and on 92% of occasions by participants at home. The median total duration of the FHR trace obtained was 6.6 minutes for clinicians and 4.6 minutes for home users.
To assess for clinical utility, obstetricians evaluated 84 heartbeat monitor traces, comprising 52 recordings from clinicians and 32 home users. The FHR was detected on 100% of occasions, and the traces were deemed to have clinical utility in 52 of 52 (100%) of clinician-obtained recordings and 31out of 32 (97%) of home recordings. One home-recorded trace was of insufficient duration to allow for evaluation of variability. Fetal heart rate accelerations were identified in 73% of clinician recordings and 77% of home recordings. All home recordings were successfully transmitted to the clinical team with no data corruption.
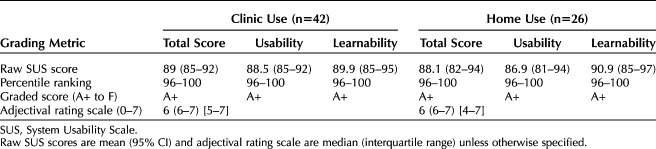
Participants who used the heartbeat monitor in the clinic and at home rated the usability and learnability of the heartbeat monitor using the System Usability Scale. The mean total usability, reliability, and learnability scores ranked in the 96th–100th percentile (Table 3). There were no differences in System Usability Scale scores between clinic and home monitoring (P=.90, paired t test). The adjectival rating scale, scored on a Likert scale of 1–7, gave a median score of 6 for both in-clinic and home use.
Table 3.
System Usability Scale Results for Clinic and Home Use
There was no association between pregnancy variables including BMI, gestation, placental position or recording site, and the time taken to detect an FHR, trace duration, or clinical utility of the heartbeat monitor trace for the whole population and for pregnancies beyond 28 weeks of gestation (Appendix 6, available online at http://links.lww.com/AOG/C240). There were no differences when participants at less than 28 weeks of gestation were excluded from the analysis. Two participants at 12 weeks of gestation (two of two) successfully located the FHR and recorded continuous traces of longer than 1 minute.
DISCUSSION
The results of this study show that the heartbeat monitor is accurate and easy to use in the hospital and at home. The FHR data obtained at home are equivalent to those required in the clinic using current intermittent auscultation protocols for low-risk pregnancies. The 95% limits of agreement between mean FHR from the heartbeat monitor and cardiotocography were well within the predefined acceptability limit of 8 bpm. Agreement was maintained across the FHR range (120–166 bpm), and was not affected by BMI, parity or placental position. The FHR was detected quickly on all occasions by clinicians and pregnant women. Fetal heart rate traces met the defined clinical utility criteria in all clinician-performed recordings and in 97% of participant-administered recordings. The heartbeat monitor ranked between the 96–100 percentiles for usability, reliability, and user satisfaction.
Based on these results, the heartbeat monitor could facilitate the evolution of antenatal care models to incorporate telehealth consultations and remote self-monitoring. For clinicians, the monitor may be used as an alternative to handheld Doppler devices for intermittent auscultation in antepartum care.
During the COVID-19 pandemic, the Royal Australian and New Zealand College of Obstetrics and Gynaecology recommended reducing face-to-face visits, limiting consultations to less than 15 minutes, and using telehealth consultations.14 For telehealth programs to be effective, there must be robust surveillance of maternal and fetal biomarkers.15 The accuracy and usability of the heartbeat monitor, as well as its ability to store and transmit data, positions it strongly as a device that can be used in these programs.
Intermittent auscultation is routinely performed to monitor FHR despite its uncertain predictive value.1–3,16 Regular FHR monitoring is associated with improved maternal wellbeing, satisfaction, and engagement.18 Detection of an FHR in the healthy range is the first aim of intermittent auscultation, but recognition of variability is dependent on clinical experience and accelerations are only noted if they occur within the 1-minute window. This short period of monitoring is not stored for review. The heartbeat monitor has advantages over handheld Doppler devices, including cost, ability to distinguish maternal and fetal heart rates, ease of use for self-administration, data storage, and transmission capabilities.
Globally, up to 2 million fetuses die during labor each year.19 The International Federation of Gynecology and Obstetrics recommends intermittent auscultation during antenatal care and labor when there is no access to cardiotocography machines.20 In resource-limited settings, the heartbeat monitor would allow inexperienced operators to accurately record, store, and transmit FHR data. Intermittent auscultation is recommended for intrapartum monitoring in low-risk pregnancies, including home births.21 Further research is required to determine whether the heartbeat monitor remains accurate during contractions.
Our study has several limitations. Based on requirements for intermittent auscultation in antenatal settings, we focused on recording FHR for at least 1 minute. Our study times exceeded this but are not equivalent to nonstress test examinations. A 10- to 20-minute cardiotocography recording is recommended to assess baseline FHR, variations, accelerations, and decelerations in high-risk pregnancies and labor.21 Our traces were too short to exclude decelerations and were not collected during contractions. We used an automatically generated average FHR based on beat-to-beat measurements and assessed variability and accelerations from that baseline. Despite the short duration, accelerations were evident in 77% of home recordings.
A strength of the study was the ability to compare accuracy with gold-standard cardiotocography data. Additionally, we enrolled a diverse study population in terms of gestation (12–40 weeks), BMI, placental positions, and obstetric history. There were no adverse effects from higher BMIs or anterior placentas, conditions that could theoretically interfere with ultrasound detection of FHR. We selected a robust learnability and usability rating system which is widely used to evaluate medical devices.
We have shown that women can use the heartbeat monitor at home to perform accurate detection of FHR. Replicating the findings in more patients would be valuable. The device addresses a critical hurdle for telehealth consultations and may offer confidence in the transition towards this new model of service.
Authors' Data Sharing Statement
Will individual participant data be available (including data dictionaries)? Individual, de-identified participant data may be shared by the corresponding author, providing appropriate reciprocal ethical approval has been sort for use of the data.
What data in particular will be shared? Available data will include individual FHR metrics, SUS scores and accuracy measurements.
What other documents will be available? The study protocol is available.
When will data be available (start and end dates)? Data will be available after manuscript publication for a period of 24 months.
By what access criteria will data be shared (including with whom, for what types of analyses, and by what mechanism)? Data will be shared for reanalysis to confirm results. All use of data must comply with HREC requirements and Good Clinical Practice.
Footnotes
The study was supported by PHI Research Group (not-for-profit), which was responsible for the study design, data collection and Research Assistants' salaries. Joondalup Health Campus provided infrastructure support, and IT services in-kind to the PHI Research Group. The HeraBEAT devices used in this study were loaned by HeraMED Pty Ltd (HeraMED, Netanya, Israel). PHI Research Group paid Ms. Natasha Wenner to provide copyediting and style advice on the final manuscript before submission. Natasha Bear and Jennie Carson received consultancy fees from the PHI Research Group for the provision of statistical analysis for this study.
Financial Disclosure This study was an investigator-funded study of the PHI Research Group, which employs Joanna Brisbane, Brooke Schneider, and Jennifer Choveaux. Desiree Silva and Jennifer Choveaux are shareholders and option holders of HeraMED Pty Ltd. Paul Porter has an interest in a company that holds shares and options of HeraMED Pty Ltd. The other authors did not report any potential conflicts of interest.
Before submission to Obstetrics & Gynecology, this article was posted to a preprint server at: http://dx.doi.org/10.1101/2020.11.18.20190959
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/C241.
Contributor Information
Fleur Muirhead, Email: fleur-muirhead@live.com.au.
Joanna Brisbane, Email: brisbanej@ramsayhealth.com.au.
Brooke Schneider, Email: brooke@cablewise.com.au.
Jennifer Choveaux, Email: ChoveauxJ@ramsayhealth.com.au.
Natasha Bear, Email: natasha@bearstats.com.au.
Jennie Carson, Email: jennie.carson@gmail.com.
Kym Jones, Email: joneskym@ramsayhealth.com.au.
Desiree Silva, Email: desirees@westnet.com.au.
Cliff Neppe, Email: NeppeC@ramsayhealth.com.au.
Figure.
No available caption
REFERENCES
- 1.Women and Newborn Health Service. Clinical practice guideline—abdominal examination. Accessed September 30, 2020. https://kemh.health.wa.gov.au/∼/media/Files/Hospitals/WNHS/For%20health%20professionals/Clinical%20guidelines/OG/WNHS.OG.AbdominalExamination.pdf [Google Scholar]
- 2.Murray H. Antenatal foetal heart monitoring. Best Pract Res Clin Obstet Gynaecol 2017;38:2–11. doi: 10.1016/j.bpobgyn.2016.10.008 [DOI] [PubMed] [Google Scholar]
- 3.Haws RA, Yakoob MY, Soomro T, Menezes EV, Darmstadt GL, Bhutta ZA. Reducing stillbirths: screening and monitoring during pregnancy and labour. BMC Pregnancy Childbirth 2009;9(suppl 1):S5. doi: 10.1186/1471-2393-9-S1-S5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marko KI, Krapf JM, Meltzer AC, Oh J, Ganju N, Martinez AG, et al. Testing the feasibility of remote patient monitoring in prenatal care using a mobile app and connected devices: a prospective observational trial. JMIR Res Protoc 2016;5:e200. doi: 10.2196/resprot.6167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Overdijkink SB, Velu AV, Rosman AN, van Beukering MD, Kok M, Steegers-Theunissen RP. The usability and effectiveness of mobile health technology-based lifestyle and medical intervention apps supporting health care during pregnancy: systematic review. JMIR Mhealth Uhealth 2018;6:e109. doi: 10.2196/mhealth.8834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Runkle J, Sugg M, Boase D, Galvin SL, Coulson CC. Use of wearable sensors for pregnancy health and environmental monitoring: descriptive findings from the perspective of patients and providers. Digit Health 2019;5:2055207619828220. doi: 10.1177/2055207619828220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van den Heuvel JF, Groenhof TK, Veerbeek JH, van Solinge WW, Lely AT, Franx A, et al. eHealth as the next-generation perinatal care: an overview of the literature. J Med Internet Res 2018;20:e202. doi: 10.2196/jmir.9262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Houze de l'Aulnoit A, Boudet S, Genin M, Gautier PF, Schiro J, Houze de l'Aulnoit D, et al. Development of a smart mobile data module for fetal monitoring in E-healthcare. J Med Syst 2018;42:83. doi: 10.1007/s10916-018-0938-1 [DOI] [PubMed] [Google Scholar]
- 9.Mhajna M, Schwartz N, Levit-Rosen L, Warsof S, Lipschuetz M, Jakobs M, et al. Wireless, remote solution for home fetal and maternal heart rate monitoring. Am J Obstet Gynecol MFM 2020;2:100101. doi: 10.1016/j.ajogmf.2020.100101 [DOI] [PubMed] [Google Scholar]
- 10.Cohen WR, Ommani S, Hassan S, Mirza FG, Solomon M, Brown R, et al. Accuracy and reliability of fetal heart rate monitoring using maternal abdominal surface electrodes. Acta Obstet Gynecol Scand 2012;91:1306–13. doi: 10.1111/j.1600-0412.2012.01533 [DOI] [PubMed] [Google Scholar]
- 11.Sauro J. A practical guide to the system usability scale: background, benchmarks, and best practices. Measuring Usability LLC; 2011. [Google Scholar]
- 12.Lewis J. The system usability scale: past, present and future. Int J Human-Computer Interaction 2018;34:577–90. doi: 10.1080/10447318.2018.1455307 [DOI] [Google Scholar]
- 13.Bangor A, Kortum P, Miller J. Determining what individual SUS scores mean: adding an adjective rating scale. J Usability Stud 2009;4:114–23. [Google Scholar]
- 14.Royal Australian and New Zealand College of Obstetrics and Gynaecology. COVID-19 hub: info for pregnant women. Accessed September 20, 2020. https://ranzcog.edu.au/statements-guidelines/covid-19-statement/information-for-pregnant-women [Google Scholar]
- 15.de Mooij MJM, Hodny RL, O'Neil DA, Gardner MR, Beaver M, Brown AT, et al. OB nest: reimagining low-risk prenatal care. Mayo Clin Proc 2018;93:458–66. doi: 10.1016/j.mayocp.2018.01.022 [DOI] [PubMed] [Google Scholar]
- 16.Henderson J, Roberts T, Sikorski J, Wilson J, Clement S. An economic evaluation comparing two schedules of antenatal visits. J Health Serv Res Policy 2000;5:69–75. doi: 10.1177/135581960000500203 [DOI] [PubMed] [Google Scholar]
- 17.Royal Australian and New Zealand College of Obstetrics and Gynaecology. Routine antenatal assessment in the absence of pregnancy complications. Accessed September 27, 2020. https://ranzcog.edu.au/RANZCOG_SITE/media/RANZCOG-MEDIA/Women%27s%20Health/Statement%20and%20guidelines/Clinical-Obstetrics/Routine-antenatal-assessment-in-the-absence-of-pregnancy-complications-(C-Obs-3b)_2.pdf?ext=.pdf [Google Scholar]
- 18.Rivenes Lafontan S, Sundby J, Ersdal HL, Abeid M, Kidanto HL, Mbekenga CK. I was relieved to know that my baby was safe: women's attitudes and perceptions on using a new electronic fetal heart rate monitor during labor in Tanzania. Int J Environ Res Public Health 2018;15:302. doi: 10.3390/ijerph15020302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grivell RM, Alfirevic Z, Gyte GM, Devane D. Antenatal cardiotocography for fetal assessment. The Cochrane Database of Systematic Reviews 2015, Issue 9. Art. No.: CD007863. doi: 10.1002/14651858.CD007863.pub4 [DOI] [PMC free article] [PubMed]
- 20.Lewis D, Downe S. FIGO intrapartum fetal monitoring expert consensus panel. FIGO consensus guidelines on intrapartum fetal monitoring: intermittent auscultation. Int J Gynaecol Obste 2015;131:9–12. doi: 10.1016/j.ijgo.2015.06.019 [DOI] [PubMed] [Google Scholar]
- 21.Umana OD, Siccardi MA. Prenatal non-stress test. Accessed February 19, 2021. https://www.ncbi.nlm.nih.gov/books/NBK537123/