Medication abortion with pharmacist-dispensed mifepristone is effective, with a low prevalence of adverse events, and patients are satisfied with the model of care.
OBJECTIVE:
To estimate effectiveness and acceptability of medication abortion with mifepristone dispensed by pharmacists.
METHODS:
We conducted a prospective cohort study at eight clinical sites and pharmacies in California and Washington State from July 2018 to March 2020. Pharmacists at participating pharmacies underwent a 1-hour training on medication abortion. We approached patients who had already been evaluated, counseled, and consented for medication abortion per standard of care. Patients interested in study participation gave consent, and the clinician electronically sent a prescription to the pharmacy for mifepristone 200 mg orally, followed 24–48 hours later by misoprostol 800 micrograms buccally. Participants were sent web-based surveys about their experience and outcomes on days 2 and 14 after enrollment and had routine follow-up with study sites. We extracted demographic and clinical data, including abortion outcome and adverse events, from medical records. We performed multivariable logistic regression to assess the association of pharmacy experience and other covariates with satisfaction.
RESULTS:
We enrolled 266 participants and obtained clinical outcome information for 262 (98.5%), of whom two reported not taking either medication. Of the 260 participants with abortion outcome information, 252 (96.9%) and 237 (91.2%) completed day 2 and 14 surveys, respectively. Complete medication abortion (primary outcome) occurred for 243 participants (93.5%, 95% CI 89.7–96.1%). Four participants (1.5%, 95% CI 0.4–3.9%) had an adverse event, none of which was serious or related to pharmacist dispensing. In the day 2 survey, 91.3% (95% CI 87.1–94.4%) of participants reported satisfaction with the pharmacy experience. In the day 14 survey, 84.4% (95% CI 79.1–88.8%) reported satisfaction with the medication abortion experience. Those reporting being very satisfied with the pharmacy experience had higher odds of reporting overall satisfaction with medication abortion (adjusted odds ratio 2.96, 95% CI 1.38–6.32).
CONCLUSION:
Pharmacist dispensing of mifepristone for medication abortion is effective and acceptable to patients, with a low prevalence of adverse events.
CLINICAL TRIAL REGISTRATION:
Medication abortion with mifepristone and misoprostol is approved by the U.S. Food and Drug Administration (FDA) for use through 70 days of gestation. Extensive research has documented the safety and effectiveness of medication abortion, as well as high levels of patient satisfaction.1 Since mifepristone's approval in 2000, the FDA has required that the drug only be dispensed in clinics, medical offices, or hospitals, a restriction that is codified in the mifepristone Risk Evaluation and Mitigation Strategy.2 The FDA instituted these restrictions likely because of the limited experience with medication abortion in the United States in 2000. However, there is no evidence that in-person dispensing improves safety, and medications associated with more risks to the patient do not have similar restrictions.3
Twenty years later, such evidence is still lacking, and countries such as Australia and Canada have approved mifepristone without dispensing restrictions.4,5 The mifepristone Risk Evaluation and Mitigation Strategy may be a barrier to access; a national survey of obstetrician–gynecologists found that the number who would provide medication abortion might double if this dispensing restriction were removed.6 The American College of Obstetricians and Gynecologists advocates the removal of the mifepristone Risk Evaluation and Mitigation Strategy.7
Pharmacists dispense medications and controlled substances for all types of indications, including sensitive health issues such as sexually transmitted infections and erectile dysfunction. Currently, 12 states permit pharmacists to prescribe hormonal contraception8; a recent national survey found that 65% of all pharmacists were interested in such prescribing.9
We performed this study under an FDA Investigational New Drug application to document clinical outcomes with and the acceptability of medication abortion when mifepristone is prescribed by clinicians and dispensed by pharmacists. We also sought to identify factors associated with satisfaction with the pharmacist-dispensing model, as well as to explore whether satisfaction with the pharmacy experience was associated with overall satisfaction with medication abortion.
METHODS
We performed a multicenter prospective cohort study of patients undergoing medication abortion who agreed to obtain pharmacist-dispensed mifepristone. The Institutional Review Boards (IRBs) of the University of California San Francisco (UCSF), Kaiser Permanente Northern California, and the University of Washington approved the study, with reliance on the University of California San Francisco IRB granted by the IRBs of the University of California, Davis, and the University of California, San Diego.
From July 2018 through March 2020, we enrolled patients at eight study sites in California and Washington State, each of which was paired with a nearby pharmacy that agreed to dispense mifepristone. Each of the clinical sites provided medication abortion before the study with clinic dispensing of mifepristone; patients obtained other prescribed medications at pharmacies. Six of the eight clinics partnered with an affiliated pharmacy in the same or adjacent building (n=5) or 1.5 miles away (n=1). Two clinics partnered with independent pharmacies, one of which was located in an adjacent building, and the other was located 1.5 miles away. Study investigators trained participating pharmacists on medication abortion and mifepristone dispensing using a standardized 1-hour presentation at the beginning of the study and as needed when new participating pharmacists were hired. At all study pharmacies, leadership permitted pharmacists to participate in the study if interested, including undergoing training, and committed to having coverage during study recruitment times by a pharmacist who could dispense mifepristone. Of note, three chain pharmacies near potential clinic sites declined to participate. Each clinical site principal investigator completed the mifepristone Prescriber Agreement Form.
Clinicians included physicians, physician assistants, and nurse practitioners. Research staff provided study details, including study coverage of clinical costs (see below) to patients only after the clinician had completed all medically necessary requirements for medication abortion. All patients approached for the study had already been fully evaluated for medication abortion medical eligibility according to the FDA-approved mifepristone labeling and local standard of care, signed the mifepristone Patient Agreement Form and any clinic-specific consent form, and received mifepristone use and follow-up instructions. Clinical follow-up options were site-specific and included returning for an in-clinic ultrasonography examination approximately 1–2 weeks later, obtaining serum human chorionic gonadotropin measurements on the day of taking mifepristone and 1–2 weeks later, or performing telephone follow-up 1 week later with a home urine pregnancy test 4 weeks after mifepristone.
Participants were eligible for the study if they spoke English or Spanish, were age 15 years or older (18 years or older at two study sites), had been fully evaluated and consented for medication abortion with a gestational age of 70 days or less confirmed by ultrasonography, and were willing to go to the study pharmacy to obtain mifepristone and to use misoprostol buccally per the FDA-approved mifepristone label. Participants also had to be willing and able to be contacted by email, telephone, or text message to complete survey data collection. Eligible and interested participants provided written study informed consent, including Health Insurance Portability and Accountability Act authorization to allow clinical data abstraction from their medical record.
A clinician then electronically prescribed mifepristone 200 mg and misoprostol 800 micrograms, along with analgesics, antibiotics, antiemetics, or contraceptives, as needed. The prescribing clinician instructed participants to use the mifepristone at an agreed-on time and take the misoprostol buccally 24–48 hours after swallowing the mifepristone, consistent with the FDA-approved labeling.10 Participants went to the pharmacy to obtain the prescribed medications. A trained pharmacist dispensed the mifepristone and other prescribed medications, maintained a study log and provided brief counseling, unless declined by the patient.
On the day after enrollment, the University of California San Francisco study team emailed participants a link to a web-based survey (day 2 survey) in Qualtrics to collect sociodemographic information, including self-described race and ethnicity. Given the evidence of negative health care experiences during pregnancy among people of color due to racism,11 we believed it was important to collect race and ethnicity information to explore associations with satisfaction outcomes. Participants also confirmed whether they obtained the medications at the pharmacy, and if and when they took or planned to take the medications. If they had taken the misoprostol, we asked the route of administration. If a participant obtained the medications and decided not to take them, we asked what they did or planned to do with the medications; if a participant reported they still had the medications, a survey prompt instructed them to return the medications to the pharmacy or the clinic. Participants were asked whether they thought the pregnancy had already been expelled and whether they had had a medical problem that required them to go to a hospital, emergency department, or doctor's office since starting the medication abortion, and, if so, we asked participants to provide details.
In addition, the day 2 survey assessed participant experiences obtaining mifepristone at the pharmacy with multiple choice questions as well as open-response fields for those who reported dissatisfaction to explain their responses. We asked whether the wait time at the pharmacy was “reasonable” or “too long.” All participants were asked, “Did you feel that you got enough information from the pharmacist about how to use the medications?” with response options of “Yes,” “No, I would have liked more information from the pharmacist,” and “No, but I got all the information I needed from the doctor or nurse in clinic.” We asked participants who reported having had a prior medication abortion, “How would you compare your experience of getting the abortion pill this time in the pharmacy compared with last time in the clinic?” with response options of “This time was better,” “Last time was better,” “They were both the same,” or “Not sure.”
Two weeks after enrollment, we sent participants an email link to the day 14 survey, which had similar questions about taking the medications, medical problems for which they sought care, follow-up with the clinic, use of additional misoprostol, and whether they thought the abortion was complete and reasons why they thought it was complete. If a participant reported being unsure whether the abortion was complete, a survey prompt instructed the participant to contact the clinical site and asked permission to follow-up with them again after the visit.
The day 14 survey also included questions about the patient's experience with the overall medication abortion experience and whether they would recommend medication abortion to a friend in a similar situation who decided to have an abortion. We also asked whether they would recommend that the friend “get the abortion pill at the pharmacy like you did.” Finally, we asked, “If you have another medication abortion in the future, how would you feel about the way you get the service?” Responses options were “I would prefer to have medication abortion be available through many primary care providers and providers of women's health care (doctors and nurses) and I would like to pick up my abortion pill at the pharmacy,” “I would prefer to have medication abortion available only in select clinics where the abortion pill can be given to me directly in clinic,” “Either way is fine,” or “Unsure.” The day 14 survey also included open-response questions that allowed participants to elaborate on their responses.
Participants who did not complete the surveys were sent reminders by text, email, or phone, depending on their contact preferences. Those who had not yet completed the day 2 survey received a longer day 14 survey, including the day 2 survey items. The surveys remained open for 1 month.
Six or more weeks after participants enrolled, site investigators abstracted data from patient charts and entered the de-identified data into an electronic REDCap form. Abstracted data included demographics, clinical information from the initial visit, and information about any follow-up visits or contacts with the patient related to the medication abortion, including whether the abortion was complete, additional treatments given, and adverse events. Adverse events were also identified from the patient surveys. Adverse events were captured up to 6 weeks after participants were recruited into the study, and any ongoing adverse events were followed until resolution. Adverse events were defined as serious using the FDA criteria and included death, hospitalization, blood transfusion, and surgery.12,13
Study participants received a $25 electronic gift card for completing each survey. Participants that had to travel from the clinic to the pharmacy also received a small stipend to cover travel expenses. The study covered the cost of mifepristone, misoprostol, and pharmacy dispensing fees, as well as the cost of other medications and clinical care related to the medication abortion provided during the initial and follow-up visits at some sites, depending on whether the site was able to bill for the service in the usual fashion or not.
We aimed to recruit a minimum of 300 and up to 350 patients for this study, which we thought was feasible during the study period. With a sample size of 300, if the proportion of patients with a complete abortion is 95%, the 95% CI of that proportion is ±3.1%; with a sample of 350, the interval is ±2.7%.
We examined four outcomes related to clinical experience and satisfaction with the pharmacist-dispensing model. These included two clinical outcomes: 1) effectiveness of medication abortion (primary outcome) and 2) adverse events, as well as two patient satisfaction outcomes that we examined in multivariate mixed-effects logistic regression analyses: 3) satisfaction with the pharmacy experience at day 2 and 4) satisfaction with the overall medication abortion experience at day 14. Effectiveness of medication abortion was defined as the proportion of participants who had a complete abortion with medications alone and did not undergo vacuum aspiration. Given the accuracy of patient self-assessment of abortion completion,14,15 we used self-reported survey data to document abortion outcome if the participant did not have follow-up contact with the clinic. Satisfaction outcomes were based on participants' ratings on a Likert scale. On the day 2 survey, we asked participants “Overall, how satisfied were you with your experience at the pharmacy when you got the abortion pill?” with response options “Very satisfied,” “Somewhat satisfied, “Somewhat dissatisfied,” and “Very dissatisfied.” On the day 14 survey we asked, “Looking back on your experience overall, how satisfied were you with the abortion pill?” with the same response options. We dichotomized responses to the two questions by those who were very satisfied compared with all other responses. We calculated 95% CIs using the binomial method.
We performed multivariable mixed-effects logistic regression analyses to explore associations between participant and pregnancy characteristics and our two patient satisfaction outcomes (satisfaction with pharmacy experience and satisfaction with overall medication abortion experience). We used mixed-effects regression with random intercepts for recruitment site to account for clustering. Independent variables included the following demographic and pregnancy characteristics, selected a priori based on our hypotheses and previous literature16: age, race and ethnicity, highest completed level of education, relationship status, parity, gestational age in days at the initial clinic visit, and prior abortion experience (none, previous medication abortion, or previous procedural abortion only). We also adjusted for whether the participant reported receiving adequate information from the pharmacist about medication abortion and pharmacy wait time (reasonable or too long). We included a dichotomized measure of satisfaction with treatment by pharmacy staff as an independent variable in the analysis of satisfaction with the pharmacy experience outcome. To assess whether the pharmacy experience contributed to overall satisfaction with the medication abortion experience, we also included satisfaction with the pharmacy experience as an independent variable to model this outcome.
To account for missing covariate data, we conducted multiple imputation then deletion methods, using chained equations.17 We excluded participants with missing outcome data after performing multiple imputation. All demographic variables and pharmacy experience responses were collected from patient surveys except gestational age at the clinic visit, which came from clinical charts. Missing survey data for age, race and ethnicity, and parity were obtained from patients' clinical chart data when available.
We conducted all analyses using Stata 15 and reported significance at P<.05. Open-ended survey responses were sorted by relevance to study intervention and organized under unifying themes.
RESULTS
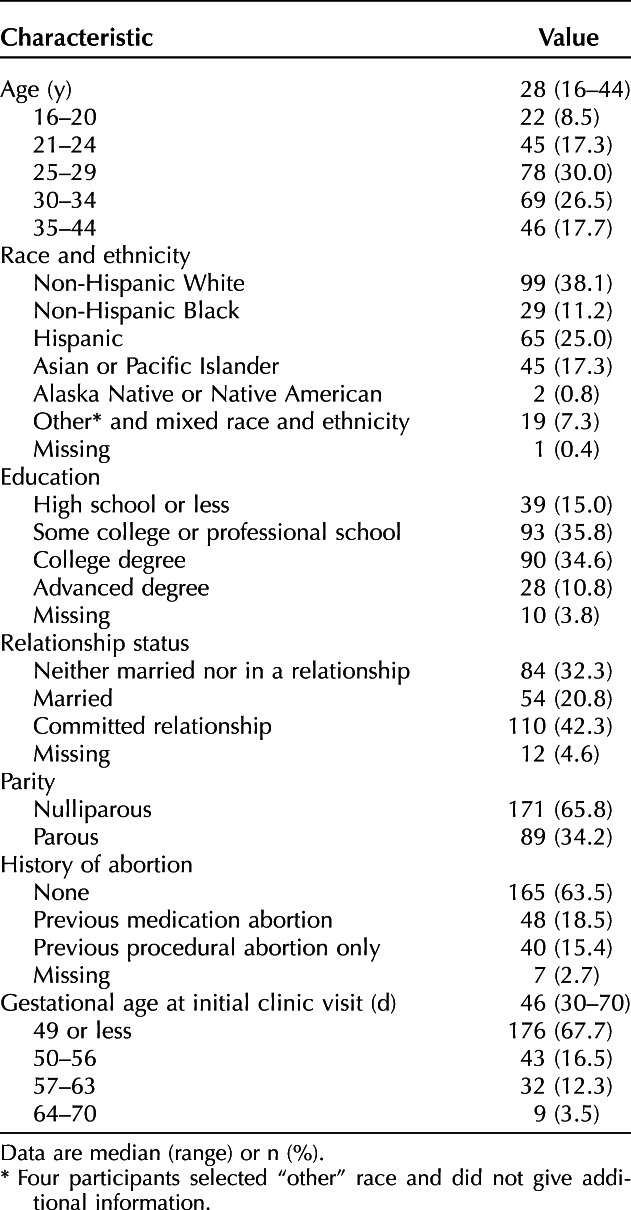
Study recruitment began in July 2018 and was halted before reaching our desired sample size in March 2020 owing to the coronavirus disease 2019 (COVID-19) pandemic, which limited the ability to have research staff in clinical facilities and lengthen patient visits for the purposes of research consent. Research staff assessed 499 patients for eligibility, of whom 233 were ineligible (n=163) or declined to participate (n=70) (Fig. 1). We enrolled 266 participants, all of whom received the study medications from the pharmacy. The median number of participants recruited at the eight sites was 27 (range 8–74). Medication abortion and study outcome information was available for 262 participants (98.5%); the other four were lost to follow-up. In addition, one participant opted not to have a medication abortion and returned the medications to the study site, and one reported flushing the medications down the toilet after having a spontaneous pregnancy loss. The characteristics of the 260 participants (97.7%) who took the medications and have abortion outcome data are presented in Table 1. The median gestational age was 46 days at the time of initial clinic visit. Two hundred forty-six participants (94.6%) reported the date they took mifepristone; all had a gestational age of 70 days or less on that date.
Fig. 1. Medication abortion study flow of patients who received mifepristone from pharmacists. PI, principal investigator.
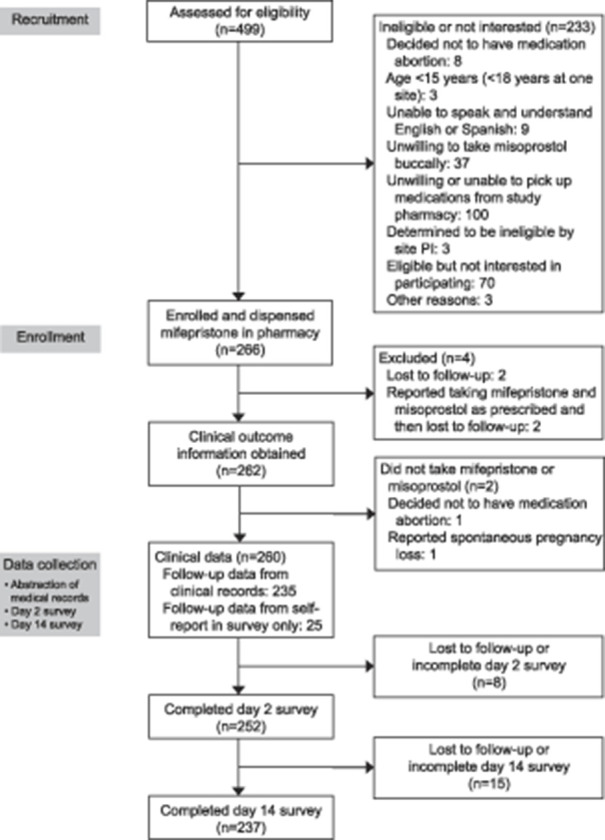
Grossman. Pharmacist Dispensing of Mifepristone. Obstet Gynecol 2021.
Table 1.
Characteristics of Study Participants Having Medication Abortion and Receiving Mifepristone at a Pharmacy (n=260)
We obtained abortion outcomes for most participants (n=235, 90.4%) based on completed clinical follow-up, with the remainder based on survey responses. Follow-up assessments are detailed in online Appendix 1, available online at http://links.lww.com/AOG/C227. Complete abortion occurred for 243 participants (93.5%, 95% CI 89.7–96.1%) with medication alone. Twenty-seven participants received a second dose of misoprostol, including 18 who ultimately had a complete abortion. Seventeen participants were diagnosed with incomplete abortion based on symptoms and ultrasonography findings, all of whom underwent vacuum aspiration. No participant had an ongoing pregnancy. Outcomes by gestational age are presented in Appendix 2, available online at http://links.lww.com/AOG/C227.
Four participants (1.5%, 95% CI 0.4–3.9%) had an adverse event possibly related to the abortion. Three participants went to an emergency department: one received intravenous fluids for dehydration, one reported heavy bleeding and was treated with pain medication, and one was diagnosed with pelvic inflammatory disease after an aspiration for incomplete abortion. None were hospitalized. In addition, one participant reported at a follow-up visit that she had transient pain and swelling in her cheeks after taking the misoprostol buccally, which had resolved and was thought to be a possible allergic reaction. After review by the site principal investigators, no adverse event was thought to be related to pharmacist dispensing. No participant reported a serious adverse event, and none were identified in chart abstraction.
For survey data, we excluded 8 of 260 (3.1%) participants missing pharmacy satisfaction data and 23 of 260 (8.8%) participants missing overall medication abortion satisfaction data. Participants completed the day 2 survey a median of 2 days after enrollment (interquartile range 1–4 days) and completed the day 14 survey a median of 16 days after enrollment (interquartile range 14–21 days). Table 2 shows participants' satisfaction as reported in the day 2 survey (n=252). Among survey respondents, 91.3% (95% CI 87.1–94.4%) reported being very (68.7%) or somewhat (22.6%) satisfied with their experience at the pharmacy, and 96.8% (95% CI 93.8–98.6%) reported being very (79.8%) or somewhat (17.1%) satisfied with their treatment by pharmacy staff. Four-fifths (79.4%) of participants said the wait time in the pharmacy was reasonable.
Table 2.
Acceptability and Satisfaction at Day 2 Survey Among Women Having Medication Abortion and Receiving Mifepristone at a Pharmacy (n=252)
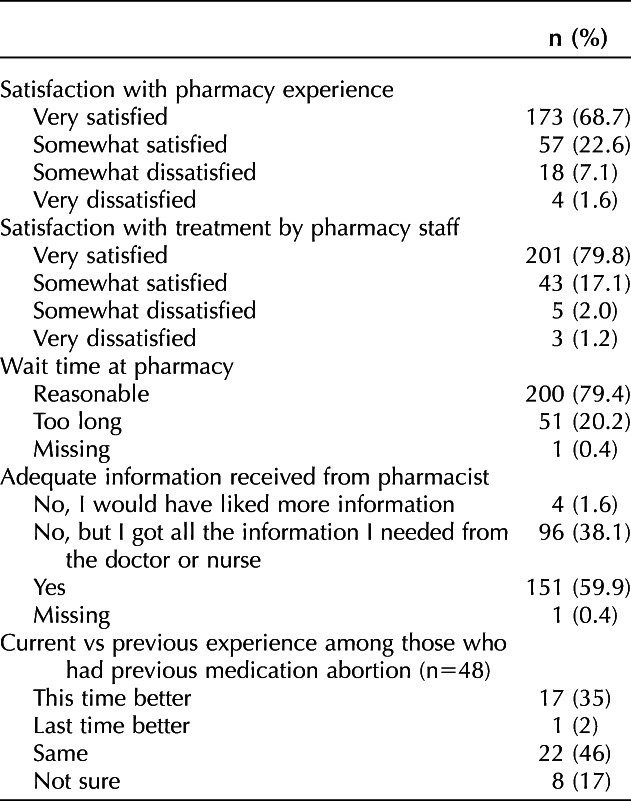
Participants who were less than very satisfied with the pharmacy experience (n=76) or treatment by pharmacy staff (n=42) gave open-ended responses describing their dissatisfaction. Common themes cited included complaints about long wait times (n=38), confusion on the part of pharmacists or staff regarding dispensing (n=27), perceived negative pharmacist attitudes (n=10), inadequate pharmacist knowledge about the medications (n=8), initially not receiving all prescribed medications (n=8), and privacy not adequately maintained (n=4), among others. Some participants pointed to more than one factor that contributed to their dissatisfaction.
In the day 2 survey, most participants reported they received adequate information from the pharmacist (59.9%) or reported they did not receive enough information from the pharmacist but received all the information they needed from the clinician they had seen previously (38.1%). Only four participants (1.6%) reported that they would have liked more information about how to use the medications from the pharmacist.
Among the 48 participants who reported a prior medication abortion, most said the current experience was the same (n=22, 46%) or better (n=17, 35%) as receiving the medications in the clinic. Eight (17%) were unsure and one (2%) reported the experience as worse. In an open-response field, participants wrote they appreciated the ability to schedule when they would take the medications, which improved convenience and allowed them to have more control over when the abortion would take place. Although some participants saw this model of care as allowing more privacy and social support, a few thought the model was less private and felt less supported by the pharmacy staff compared with the clinic staff.
Table 3 shows measures of satisfaction collected from the 237 (91.2%) women who completed the day 14 survey. Overall, 84.4% (95% CI 79.1–88.8%) reported being very (65.4%) or somewhat (19.0%) satisfied with their medication abortion experience. The majority said they would recommend medication abortion (67.9%) and pharmacist dispensing (74.3%) to a friend in a similar situation. When asked how they would prefer to obtain medication abortion in the future, if needed, the majority (62.0%) said they would prefer to have medication abortion available through prescriptions from primary care clinics with medications dispensed in pharmacies. Only 5.5% said they would prefer to have the service only available in select clinics where the medications are dispensed directly to patients in clinic. About one quarter (28.7%) said either way was fine, and 3.0% were unsure.
Table 3.
Acceptability and Satisfaction at Day 14 Survey Among Women Having Medication Abortion and Receiving Mifepristone at a Pharmacy (n=237)
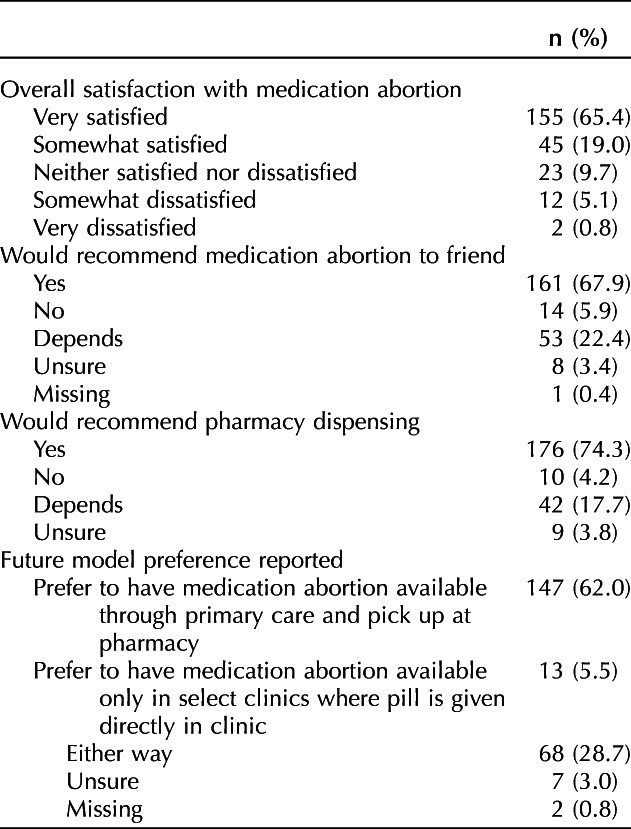
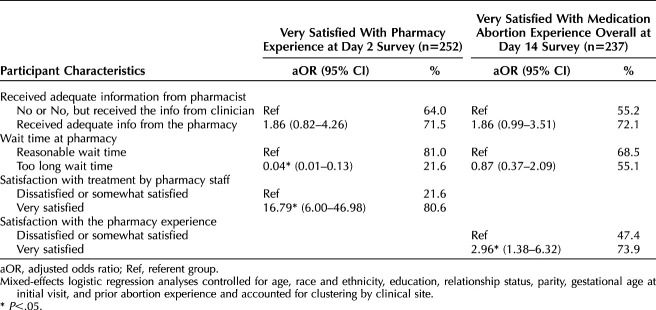
Table 4 shows the results of multivariable mixed-effects logistic regression analyses exploring factors associated with patient satisfaction with the pharmacy and medication abortion experience. Those reporting excessively long wait times had lower odds of satisfaction with pharmacy dispensing (adjusted odds ratio [aOR] 0.04, 95% CI 0.01–0.13), and those who reported being very satisfied with the treatment by pharmacy staff had higher odds of satisfaction with pharmacy dispensing (aOR 16.79, 95% CI 6.00–46.98). Those who reported that they were very satisfied with the pharmacy experience had higher odds of being very satisfied with their medication abortion overall compared with those who were somewhat satisfied or dissatisfied with the pharmacy experience (aOR 2.96, 95% CI 1.38–6.32).
Table 4.
Multivariable Adjusted Odds Ratios for Reporting Satisfaction With the Pharmacy Experience and Overall Abortion Experience Among Women Having Medication Abortion and Receiving Mifepristone at a Pharmacy
DISCUSSION
In this study, medication abortion provision with pharmacist dispensing of mifepristone was effective and acceptable to patients. Among participants with follow-up data, 93% had a complete abortion, and none had an ongoing pregnancy. These outcome proportions are similar to those reported in the literature when the medications are dispensed by a clinician.18,19 Few patients (1.5%) had adverse events, and none were related to pharmacist dispensing.
We also found that the vast majority of patients were satisfied with the model of care, and overall satisfaction was similar to other studies of medication abortion with clinician-dispensed mifepristone, which have found that 87–88% were satisfied with the method.19,20 Satisfaction with the pharmacy and treatment by pharmacy staff, reported on the day 2 survey, were somewhat higher than overall satisfaction with medication abortion reported later. This is not surprising given that overall method satisfaction is correlated with symptoms and outcomes of the medication abortion,21 which might not yet have been apparent by the day 2 survey. The vast majority reported they received adequate information—either from the clinician or pharmacist—and more than 90% indicated their support for pharmacist dispensing of mifepristone in the future.
Although satisfaction with this model was high, the open-ended responses point to areas for improvement that could be addressed through additional training of pharmacists and pharmacy staff. The finding that elements of the pharmacy experience, such as wait time and treatment by the pharmacy staff, were associated with satisfaction with the pharmacy experience, which in turn was associated with overall abortion satisfaction, is similar to research on other pharmacy services.22
It is a reassuring finding that one-third of participants who had had a prior medication abortion reported that the current experience of getting the medications at the pharmacy was better. The open-ended responses suggest that patients appreciated the convenience of being able to schedule when to take the medications. Since the FDA approved updated labeling for mifepristone in 2016, patients are no longer required to take the pill in the facility after it is dispensed,10 although some state laws still require this. It is also notable that two participants did not proceed with the medication abortion after completing their clinic visit and filling the prescription. Other studies that allow patients to take the mifepristone at home after receiving it in the clinic or that mail the medications patients have also reported that a very small number of patients choose not to proceed with the abortion.23,24
One concern that has been raised with allowing clinicians to issue prescriptions for mifepristone is that some pharmacists may refuse to fill the prescription, limiting the feasibility of this model.25 In our study, the participating pharmacies were required to have a pharmacist on duty during clinic hours who had been trained in the study protocol and was willing to dispense mifepristone. As a result, all participants were able to fill their prescriptions when they went to the pharmacy. We also collected survey and interview data with the pharmacists at the study pharmacies to evaluate their perceptions of the model, which will be reported separately. Although we did not have challenges with individual pharmacists refusing to dispense mifepristone, we did have difficulty obtaining study approval at chain pharmacies. If the dispensing requirement for mifepristone is eliminated, some pharmacies may refuse to stock the medication, as has been reported for ulipristal acetate emergency contraception,26 highlighting a potential role for mail-order pharmacies once the Risk Evaluation and Mitigation Strategy is removed.
This study has several strengths, including low loss to follow-up and standardized pharmacist training. It also has several limitations. We had to stop recruitment early because of the COVID-19 pandemic, reaching 89% of our planned minimum sample size. However, the effect of the reduced sample size on the precision of our estimates was small. The sample size is similar to the only other published report on providing medication abortion in the United States without in-clinic dispensing (n=190 with abortion outcome data).24 In addition, our findings may have limited generalizability given that no chain pharmacy participated; patient experiences at chain pharmacies theoretically may be different. Finally, satisfaction with the pharmacy experience may increase over an extended time as pharmacy staff become more accustomed to dispensing mifepristone.
This study, together with another report of a direct-to-patient telemedicine service in which patients received the medications by mail,24 demonstrate that medication abortion may be offered with a high level of effectiveness and satisfaction and low prevalence of adverse events without requiring mifepristone to be dispensed in the clinic or medical office. These data further support eliminating the dispensing requirement for mifepristone and allowing pharmacies to dispense the medication.
Authors' Data Sharing Statement
Will individual participant data be available (including data dictionaries)? No.
What data in particular will be shared? No data beyond what is presented in the manuscript will be shared.
What other documents will be available? Study protocol and data collection forms will be available.
When will data be available (start and end dates)? Study documents will be available from the date of publication for a period of 5 years.
By what access criteria will data be shared (including with whom, for what types of analyses, and by what mechanism)? Individuals interested in obtaining study documents should email the corresponding author.
Footnotes
Financial Disclosure: Dr. Grossman has served as a consultant to Planned Parenthood Federation of America and the Center for Reproductive Rights. Dr. Creinin and Dr. Meckstroth are consultants for Danco, Inc., the manufacturer of Mifeprex (mifepristone 200 mg). Dr. Rafie is a consultant for GenBioPro, the manufacturer of generic mifepristone. The other authors did not report any potential conflicts of interest.
Presented in part as an oral abstract at the Society of Family Planning’s Annual Meeting, October 19–21, 2019, Los Angeles, California.
Funded by a grant from Fidelity Charitable.
The authors thank the research staff who assisted with data collection, as well as the pharmacists at the study sites and patients who volunteered to be study participants. The findings and conclusions in this article are those of the authors and do not necessarily reflect the views of Planned Parenthood Federation of America, Inc., or Kaiser Permanente Northern California.
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/C228.
Contributor Information
C. Finley Baba, Email: Finley.Baba@ucsf.edu.
Shelly Kaller, Email: Shelly.Kaller@ucsf.edu.
M. Antonia Biggs, Email: Antonia.Biggs@ucsf.edu.
Sarah Raifman, Email: Sarah.Raifman@ucsf.edu.
Tanvi Gurazada, Email: Tanvi.Gurazada@ucsf.edu.
Sally Rafie, Email: sally@birthcontrolpharmacist.com.
Sarah Averbach, Email: saverbach@health.ucsd.edu.
Karen R. Meckstroth, Email: karen.meckstroth@ucsf.edu.
Elizabeth A. Micks, Email: emicks@uw.edu.
Erin Berry, Email: Erin.Berry@ppgnhi.org.
Tina R. Raine-Bennett, Email: Tina.R.Raine-Bennett@kp.org.
Mitchell D. Creinin, Email: mdcreinin@ucdavis.edu.
REFERENCES
- 1.Medication abortion up to 70 days of gestation. ACOG Practice Bulletin No. 225. American College of Obstetricians and Gynecologists. Obstet Gynecol 2020;136:e31–47. doi: 10.1097/AOG.0000000000004082 [DOI] [PubMed] [Google Scholar]
- 2.U.S. Food and Drug Administration. Risk evaluation and mitigation strategy (REMS) single shared system for mifepristone 200MG. Accessed August 23, 2020. https://www.accessdata.fda.gov/drugsatfda_docs/rems/Mifepristone_2019_04_11_REMS_Document.pdf
- 3.Mifeprex REMS Study Group, Raymond EG, Blanchard K, Blumenthal P, Cleland K, Foster AM, et al. Sixteen years of overregulation: time to unburden Mifeprex. N Engl J Med 2017;376:790–4. doi: 10.1056/NEJMsb1612526 [DOI] [PubMed] [Google Scholar]
- 4.Grossman D, Goldstone P. Mifepristone by prescription: a dream in the United States but reality in Australia. Contraception 2015;92:186–9. doi: 10.1016/j.contraception.2015.06.014 [DOI] [PubMed] [Google Scholar]
- 5.Government of Canada. MIFEGYMISO (mifepristone and misoprostol tablets) - Canadian distribution and administration program. Accessed August 23, 2020. https://healthycanadians.gc.ca/recall-alert-rappel-avis/hc-sc/2017/63330a-eng.php [Google Scholar]
- 6.Grossman D, Grindlay K, Altshuler AL, Schulkin J. Induced abortion provision among a national sample of obstetrician–gynecologists. Obstet Gynecol 2019;133:477–83. doi: 10.1097/AOG.0000000000003110 [DOI] [PubMed] [Google Scholar]
- 7.American College of Obstetricians and Gynecologists. Improving access to mifepristone for reproductive health indications. Accessed August 23, 2020. https://www.acog.org/en/Clinical Information/Policy and Position Statements/Position Statements/2018/Improving Access to Mifepristone for Reproductive Health Indications [Google Scholar]
- 8.Birth Control Pharmacist. Policies: pharmacist prescribing of hormonal contraception. Accessed September 13, 2020. https://birthcontrolpharmacist.com/policies/
- 9.Rafie S, Cieri-Hutcherson NE, Frame TR, Griffin B, Harris JB, Horlen C, et al. Pharmacists' perspectives on prescribing and expanding access to hormonal contraception in pharmacies in the United States. J Pharm Pract 2019 Aug 7. [Epub ahead of print]. doi: 10.1177/0897190019867601 [DOI] [PubMed] [Google Scholar]
- 10.U.S. Food and Drug Administration. Mifeprex (mifepristone) tablets label. Accessed August 23, 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/020687s020lbl.pdf [Google Scholar]
- 11.Altman MR, McLemore MR, Oseguera T, Lyndon A, Franck LS. Listening to women: recommendations from women of color to improve experiences in pregnancy and birth care. J Midwifery Womens Health 2020;65:466–73. doi: 10.1111/jmwh.13102 [DOI] [PubMed] [Google Scholar]
- 12.U.S. Food and Drug Administration. What is a serious adverse event? Accessed September 12, 2020. https://www.fda.gov/safety/reporting-serious-problems-fda/what-serious-adverse-event
- 13.Upadhyay UD, Desai S, Zlidar V, Weitz TA, Grossman D, Anderson P, et al. Incidence of emergency department visits and complications after abortion. Obstet Gynecol 2015;125:175–83. doi: 10.1097/AOG.0000000000000603 [DOI] [PubMed] [Google Scholar]
- 14.Perriera LK, Reeves MF, Chen BA, Hohmann HL, Hayes J, Creinin MD. Feasibility of telephone follow-up after medical abortion. Contraception 2010;81:143–9. doi: 10.1016/j.contraception.2009.08.008 [DOI] [PubMed] [Google Scholar]
- 15.Chen MJ, Rounds KM, Creinin MD, Cansino C, Hou MY. Comparing office and telephone follow-up after medical abortion. Contraception 2016;94:122–6. doi: 10.1016/j.contraception.2016.04.007 [DOI] [PubMed] [Google Scholar]
- 16.Grossman D, Grindlay K, Buchacker T, Lane K, Blanchard K. Effectiveness and acceptability of medical abortion provided through telemedicine. Obstet Gynecol 2011;118:296–303. doi: 10.1097/AOG.0b013e318224d110 [DOI] [PubMed] [Google Scholar]
- 17.von Hippel PT. Regression with missing Ys: an improved strategy for analyzing multiply imputed data. Sociological Methodol 2007;37:83–117. doi: 10.1111/j.1467-9531.2007.00180.x [Google Scholar]
- 18.Chen MJ, Creinin MD. Mifepristone with buccal misoprostol for medical abortion: a systematic review. Obstet Gynecol 2015;126:12–21. doi: 10.1097/AOG.0000000000000897 [DOI] [PubMed] [Google Scholar]
- 19.Winikoff B, Dzuba IG, Chong E, Goldberg AB, Lichtenberg ES, Ball C, et al. Extending outpatient medical abortion services through 70 days of gestational age. Obstet Gynecol 2012;120:1070–6. doi: 10.1097/aog.0b013e31826c315f [DOI] [PubMed] [Google Scholar]
- 20.Winikoff B, Ellertson C, Elul B, Sivin I. For the mifepristone clinical trials group. Acceptability and feasibility of early pregnancy termination by mifepristone-misoprostol: results of a large multicenter trial in the United States. Arch Fam Med 1998;7:360–6. doi: 10.1001/archfami.7.4.360 [DOI] [PubMed] [Google Scholar]
- 21.Teal SB, Dempsey-Fanning A, Westhoff C. Predictors of acceptability of medication abortion. Contraception 2007;75:224–9. doi: 10.1016/j.contraception.2006.10.008 [DOI] [PubMed] [Google Scholar]
- 22.Patel PM, Vaidya V, Osundina F, Comoe DA. Determining patient preferences of community pharmacy attributes: a systematic review. J Am Pharm Assoc 2020;60:397–404. doi: 10.1016/j.japh.2019.10.008 [DOI] [PubMed] [Google Scholar]
- 23.Chong E, Frye LJ, Castle J, Dean G, Kuehl L, Winikoff B. A prospective, non-randomized study of home use of mifepristone for medical abortion in the U.S. Contraception 2015;92:215–9. doi: 10.1016/j.contraception.2015.06.026 [DOI] [PubMed] [Google Scholar]
- 24.Raymond E, Chong E, Winikoff B, Patais I, Mary M, Lotarevich T, et al. TelAbortion: evaluation of a direct to patient telemedicine abortion service in the United States. Contraception 2019;100:173–7. doi: 10.1016/j.contraception.2019.05.013 [DOI] [PubMed] [Google Scholar]
- 25.Raifman S, Orlando M, Rafie S, Grossman D. Medication abortion: potential for improved patient access through pharmacies. J Am Pharm Assoc (2003) 2018;58:377–81. doi: 10.1016/j.japh.2018.04.011 [DOI] [PubMed] [Google Scholar]
- 26.Shigesato M, Elia J, Tschann M, Bullock H, Hurwitz E, Wu YY, et al. Pharmacy access to ulipristal acetate in major cities throughout the United States. Contraception 2018;97:264–9. doi: 10.1016/j.contraception.2017.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]