Living in a state with a waiting period or a two-visit requirement (or both) to receive abortion care is not associated with increased decision certainty.
OBJECTIVE:
Many U.S. states mandate counseling and a waiting period before abortion, which often necessitates two separate clinic visits. These laws purport to ensure individuals are certain about their abortion decision. We examined whether exposure to these laws is associated with increased decision certainty.
METHODS:
The Google Ads Abortion Access Study is a prospective study of pregnant people considering abortion recruited when searching online using abortion care-related keywords. Eligible participants, who represented all 50 U.S. states, completed baseline and 4-week follow-up surveys. We measured decision certainty using the Decisional Conflict Scale (scores range from 0 to 100; higher scores reflect lower certainty). We used a multivariable linear mixed model to examine the association between living in states with waiting periods, two-visit requirements, or both and changes in decision certainty. We also compared baseline, follow-up, and changes in decision certainty by whether the pregnancy was ongoing or not at follow-up.
RESULTS:
The analytic sample included 750 participants who contributed relevant baseline and follow-up data. At follow-up, 396 participants had an abortion, and 354 had not. There was no significant increase in decision certainty for participants in states with waiting period laws (mean change score −1.0, 95% CI −2.8 to 2.8). In adjusted models, still seeking an abortion at 4-week follow-up was associated with decreased certainty (mean change score 8.05, 95% CI 5.13–10.97). Those still seeking abortion had significantly lower certainty (baseline score 28.8 and follow-up score 32.2) than those who had obtained an abortion (baseline score 21.8 and follow-up score 20.1, P<.01).
CONCLUSION:
Decision certainty is relatively high and stable over time among those who had had an abortion. Living in a state with a waiting period or two-visit requirement is not associated with increased decision certainty.
In the United States, 27 states require that individuals seeking abortion wait 18–72 hours after mandated counseling before having an abortion, and 14 states require that counseling be done in-person, creating a two-visit minimum to obtain care.1 Although the written intent of mandatory waiting periods and two-visit requirements is to aid decision making for those uncertain about their decision, a consequence of these laws is to create obstacles to timely abortion care. These laws presuppose that additional time and information will enable people to consider or reconsider their decision to avoid future regret and emotional distress. For example, in discussions of waiting period legislation in Tennessee in 2019, lawmakers stated that such requirements provide people “time to form ‘mental clarity’” and to be “as certain as possible” about their decision.2,3 However, research consistently demonstrates that decision certainty regarding abortion is high at the time people seek care4 and that the overwhelming majority of people having abortions felt abortion was the right decision for them and did not experience decision regret or have negative emotions arise years later.5
At the same time, studies of mandatory waiting periods and two-visit requirement restrictions have shown that they have negative consequences, including delaying care and increasing costs.6,7 A study of Utah's 72-hour waiting period and two-visit requirement law found it delayed and distressed individuals, but did not change their certainty around their decision to obtain abortion care.8 The few individuals who decided not to proceed with abortion were those who reported being uncertain about their decision at baseline.
A limitation of past research on decision certainty and abortion is its focus on people presenting for abortion care, who may be further along in their decision-making process by the time they are surveyed at abortion facilities. These studies capture the experiences of those able to present to a clinic, and exclude others who may have been considering, but ultimately did not or could not access abortion care. Internet recruitment can better reach this previously excluded population. Additionally, internet recruitment could capture individuals earlier in their care-seeking process (ie, still gathering information and researching options online) to better illustrate the progression of decision certainty, regardless of whether they ultimately decide to obtain an abortion.9
To further explore the relationship between waiting periods and two-visit requirements and decision certainty regarding abortion, we measured changes in decision certainty by policy context. Our analysis sought to test the hypothesis motivating these laws: that individuals seeking abortion care and exposed to mandatory waiting periods and two-visit requirements would be more likely to experience increased decision certainty compared with people unexposed to these requirements.
METHODS
We used data from the Google Ads Abortion Access Study, a prospective study among people searching online for abortion care from August 2017 to May 2018. Detailed methodology of the study has been described elsewhere.9 In brief, individuals searching with specific keywords in Google, such as “abortion clinic near me,” were shown an ad for the survey in their search results (see https://www.sciencedirect.com/science/article/pii/S2590151619300164#f0010). Recruitment was conducted with a stratified sampling strategy to ensure that we would have baseline and follow-up data from all 50 states and the District of Columbia. The use of Google Ads allowed for the ability to modify ad displays by IP address to target specific states. Our initial goal was to recruit at least 20 participants from every state, but in eight less populated states we recruited fewer than 20 (range 8–19). Those who clicked on the ad were directed to a landing page with more details about the study and its intent so that potential participants could fully provide informed consent and feel they could safely and confidentially share their experiences (see https://www.sciencedirect.com/science/article/pii/S2590151619300164#f0010). Individuals were eligible if they were currently pregnant and considering abortion. Eligible participants provided electronic consent and completed a baseline survey in Qualtrics with questions on sociodemographic characteristics, pregnancy history, gestation of the current pregnancy, and decision certainty. The survey items were nonrandomized and used adaptive questioning. Participants also provided a phone number, email, or both for follow-up. We employed several strategies to reduce fraudulent responses, such as completing the survey more than once or automated responses. First, we added a tag to the survey that prevented it from being presented in search results separate from our ads. Additionally, we did not include in the analysis anyone who arrived to the Qualtrics survey from a source outside of our landing page. Embedded cookies in the survey precluded multiple attempts to take the survey. Lastly, our research team reviewed the IP addresses, phone numbers, and emails of enrolled participants to identify and exclude any duplicate entries.
Four weeks after the baseline survey, each participant received an email or text message invitation with a link to complete the follow-up survey, in which respondents reported their pregnancy status. Decision certainty was again assessed at follow-up. Participants were remunerated with a $50 electronic gift card after completion. The study was approved by the University of California, San Francisco Institutional Review Board (approval No. 16-20627).
Change in decision certainty between baseline and follow-up was our main outcome variable of interest. Decision certainty was assessed using the Decisional Conflict Scale, a 16-item scale that is considered the gold standard for assessing certainty in the context of health care decisions and is validated for use with people seeking abortion.4,10 The Decisional Conflict Scale includes items that span four domains: understanding of the different health care options available; clarity about which risks and benefits matter most; level of support or pressure felt in making a decision; and difficulty in choosing a course of action. The Decisional Conflict Scale items were preceded by the statement “Thinking about this pregnancy and your decision to have an abortion or not have an abortion, please mark your answers to the following questions.” For each item, participants rated their level of agreement on a 5-point scale that ranged from “Strongly Agree” to “Strongly Disagree.” Using scale author guidance,10 we calculated aggregate summary scores by summing individual item responses and scaling such that scores could range from 0 to 100. On this continuous scale, higher scores indicated high levels of conflict with the decision (low decision certainty) and low scores suggested low levels of conflict (high decision certainty). Prior research demonstrates that every point increase on the scale is associated with increasing decision delay or regret and, generally, scores higher than 37.5 are associated with delayed decision making or “feeling unsure.”11 Because we were interested in assessing changes in decision certainty in association with specific laws, we calculated change over time by subtracting baseline Decisional Conflict Scale scores from follow-up Decisional Conflict Scale scores. An increase in decision certainty would therefore be reflected by a lower Decisional Conflict Scale score at follow-up than at baseline and a negative difference between those scores.
The primary independent variable was a three-level indicator of state-level waiting periods and two-visit in-person requirements in the participant's state of residence (Fig. 1).12
Fig. 1. State waiting period and two-visit requirement restrictions for obtaining an abortion, August 2017–May 2018.
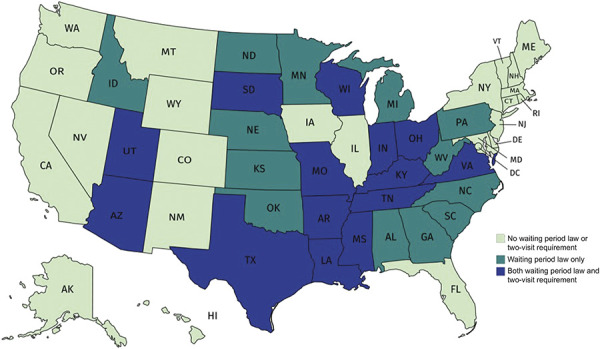
Jovel. Abortion Waiting Periods and Decision Certainty. Obstet Gynecol 2021.
Other variables of interest included gestation of pregnancy at time of recruitment, shared decision making about pregnancy status, and pregnancy status at the 4-week follow-up. Gestation of the current pregnancy was based on the reported last menstrual period, or, if unknown, the estimated number of weeks pregnant. Respondents also reported their level of shared decision making regarding the status of their pregnancy (whether the other person involved in the pregnancy mostly decides, they decide together, or the participant mostly decides). Participants reported their pregnancy statuses at follow-up, which were categorized into three groups: had an abortion, still pregnant and seeking an abortion, and still pregnant and planning to continue the pregnancy. We had a secondary hypothesis that those who were still seeking abortion or planned to continue their pregnancies at follow-up would have had lower decision certainty about abortion at baseline (which would affect their pregnancy status) and that those who had obtained an abortion by follow-up would have had higher decision certainty at baseline, which led to following through on their decision.
We limited the sample to those participants who completed the Decisional Conflict Scale items in both baseline and follow-up surveys. All Decisional Conflict Scale items were programmed to require a response. In addition, to isolate exposure to waiting period and two-visit requirement laws, we excluded participants who reported never having visited or called an abortion facility by the time of the follow-up survey (n=114). Respondents who reported a miscarriage, having already given birth, never having been pregnant, or “other” pregnancy status at follow-up (n=141) were not eligible to complete the follow-up survey, because the Decisional Conflict Scale items were no longer applicable and were excluded from the analysis (Fig. 2).
Fig. 2. Loss to follow-up and reasons for exclusion for final sample. DCS, Decisional Conflict Scale.
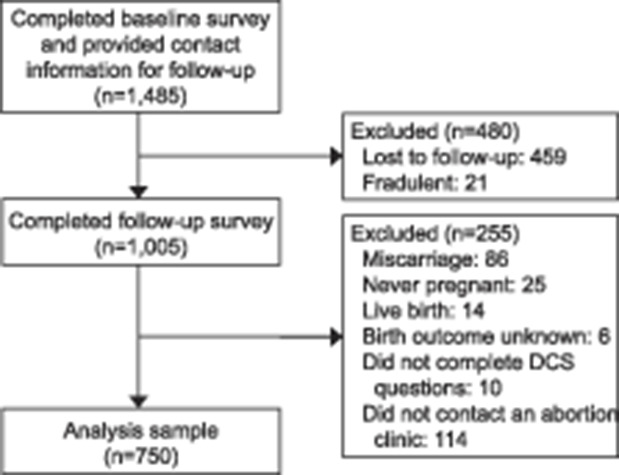
Jovel. Abortion Waiting Periods and Decision Certainty. Obstet Gynecol 2021.
We first described the sociodemographic characteristics of participants by the abortion restrictions in their state of residence, comparing proportions with chi-square tests. We estimated the unadjusted mean baseline, follow-up, and change in Decisional Conflict Scale scores by the three-level state restriction variable, using paired t tests to compare means across groups. We then used a multivariable linear mixed effects model, examining sociodemographic characteristics and other factors hypothesized to contribute to decision certainty at baseline, including baseline Decisional Conflict Scale score. Participants' self-classification of race and ethnicity was included among the sociodemographic factors in the analysis to better capture its possibly unique association with decision certainty, which can reflect community values or shared cultural and historic experiences of abortion care. We used a mixed effects model to account for the nonindependence of the data within states. We ran the adjusted regression model both with and without the final pregnancy status as a covariate to assess whether the association might change after controlling for the participant's decision about their pregnancy.
Finally, we stratified participants by pregnancy status at follow-up to examine differences in mean baseline, follow-up, and change in Decisional Conflict Scale scores using paired t tests. For any covariates with missing data, a separate “missing” category was created, and all observations were retained for analyses. All analyses were conducted using Stata 15.1.13
RESULTS
As described previously,9 of the 11,552 unique visits to the study site, 1,982 started the survey (17% recruitment rate), 1,485 completed the baseline survey and provided contact information (75% completion rate), and 1,005 completed the follow-up survey (68% follow-up rate). There were no significant differences in baseline decision certainty scores by loss to follow-up. Of the 1,005 participants who completed all baseline and follow-up Decisional Conflict Scale items, 75% reported that they called or visited an abortion clinic, and thus were exposed to the restriction. The resulting final analytic sample was 750 participants (Fig. 2).
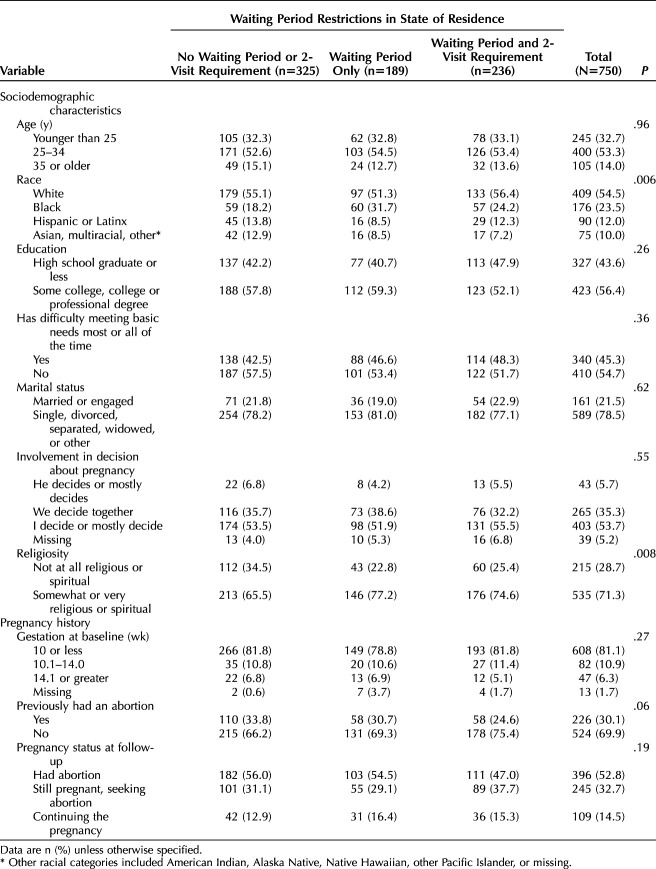
Just more than 43% of participants lived in a state with no waiting period or two-visit requirement restrictions, 25% lived in a state with a waiting period restriction only, and 32% lived in a state with both waiting period and two-visit requirement restrictions (Table 1). The sociodemographic profiles of the participants did not vary significantly by the three levels of state restrictions, except in race and religiosity across groups (Table 1).
Table 1.
Selected Characteristics of the Sample, by State Waiting Period Restrictions
Mean baseline Decisional Conflict Scale scores ranged from 26.2 in the states with no waiting period or two-visit requirements to 25.0 in states with both types of restrictions. At follow-up, mean scores were 26.0 in states with neither requirement, 23.8 in those with waiting periods only, and 24.0 in states with waiting periods and two-visit requirements. That is, in all three categories there was a slight reduction in Decisional Conflict Scale score by follow-up (representing an increase in certainty). We compared the mean scores and 95% CIs among the three state restriction categories with the “no waiting period or 2-visit requirement” category as the reference group. There were no statistically significant differences at baseline, follow-up, or when calculating changes in Decisional Conflict Scale over time (all P>0.10) and significant overlap in CIs (Fig. 3).
Fig. 3. Change in Decisional Conflict Scale (DCS) score by pregnancy status at 4-week follow-up, by three-level state abortion restriction category. None of the differences among the three categories of states were statistically significant.
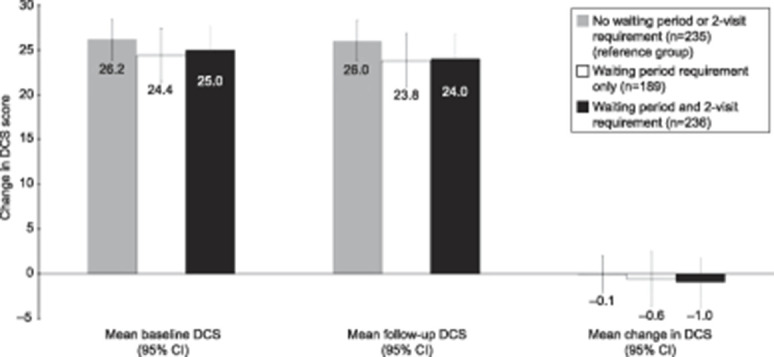
Jovel. Abortion Waiting Periods and Decision Certainty. Obstet Gynecol 2021.
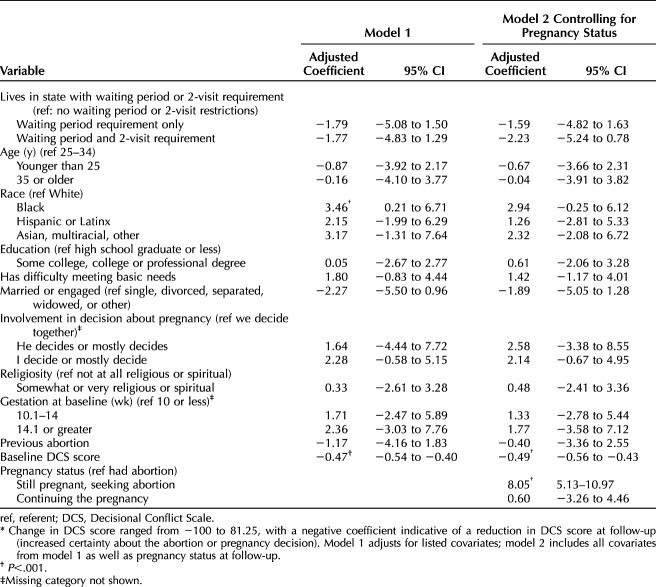
In the adjusted linear regression models, there were no statistically significant associations between state restrictions and changes in decision certainty. We did not observe statistically significant increases in decision certainty between baseline and follow-up in states with either waiting periods only or waiting periods and two-visit requirements (Table 2, model 1). This lack of significance persisted even when pregnancy status at follow-up was included in the model (Table 2, model 2).
Table 2.
Mixed-Effects Multivariable Linear Regression Examining Changes in Decisional Conflict Scale Score Associated With State Waiting Period Restrictions (N=750)*
However, several covariates in the linear regression models were associated with a significant change in Decisional Conflict Scale scores over time. In the first model, identifying as Black was associated with decreased certainty (adjusted mean change score 3.5, 95% CI 0.2–6.7), and participants with higher Decisional Conflict Scale scores (lower certainty) at baseline had increased certainty over time (adjusted mean change score: −0.5, 95% CI −0.6 to −0.4). In the model with pregnancy status at follow-up (model 2), those who reported that they were still seeking an abortion at follow-up were more likely to report higher Decisional Conflict Scale scores (decreased certainty) (adjusted mean change score 8.1, 95% CI 5.1–11.0) than those who had had an abortion by follow-up.
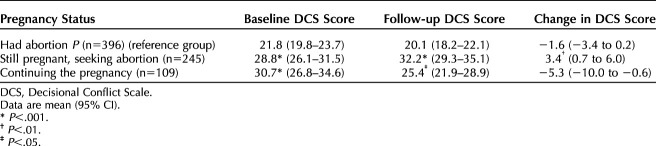
When participants were stratified by pregnancy status at follow-up, those who had had an abortion had the highest decision certainty across the three groups at both time points (baseline 21.8, 95% CI 19.8–23.7; follow-up 20.1, 95% CI 18.2–22.1), and this group had the smallest absolute mean change in scores (change −1.6, 95% CI −3.4 to 0.2) (Table 3). Those who were continuing their pregnancy at follow-up had significantly lower decision certainty at baseline than those who ultimately had an abortion, evidenced by their higher Decisional Conflict Scale scores. However, this group also had a decrease in Decisional Conflict Scale scores over time (change −5.3, 95% CI -10.0 to −0.6), reflecting an overall increase in decision certainty between baseline and follow-up. Participants still seeking an abortion had the lowest decision certainty of the three groups at follow-up. They also had a significantly greater increase in Decisional Conflict Scale scores between baseline and follow-up than those who had had an abortion, indicating a decrease in certainty over time (change 3.4, 95% CI 0.7–6.0).
Table 3.
Mean Baseline, 4-Week Follow-up, and Change in Decisional Conflict Scale Scores, by Pregnancy Status
DISCUSSION
In this analysis, we find that living in a state with a waiting period, two-visit requirement, or both is not associated with an increase in decision certainty, when compared with those living in states with no such restrictions. These results suggest that these state restrictions by themselves likely did not have their intended effect of increasing decision certainty in a population of individuals considering abortion.
Overall, in this sample of people searching for abortion information online, those who had obtained abortions by follow-up had the most stable levels of decision certainty over time, which is consistent with previous literature.4 High decision certainty at follow-up was particularly evident in groups that had made a decision—either to have an abortion or to continue the pregnancy. The only group that had a reduction in decision certainty over time was the still seeking abortion group. This result possibly reflects delayed decision making as a result of lower decision certainty at baseline or other barriers to obtaining care that have put them in a situation 4 weeks later at follow-up in which they have even less certainty that they will be able to obtain an abortion.14
Very few factors were associated with changes in decision certainty. Before controlling for pregnancy status at follow-up, just one demographic factor—being of Black race—was significantly associated with reduced decision certainty over time in the adjusted model. This association could be a proxy for other associated factors not fully explored in this analysis, such as unique community values, a long history of reproductive injustice, ongoing medical racism, targeted anti-abortion messaging of “Black genocide,” as well as a possible compound effect of these factors interacting with additional barriers (eg, economic, access, support) that are disproportionately concentrated in Black communities.15–18
Moreover, having a higher baseline Decisional Conflict Scale score was associated with an increase in certainty over time. Those who already had high certainty (low Decisional Conflict Scale score) would not have had as much room for a decrease in scores. Therefore, the key factors associated with changes in decision certainty in this sample are race, how someone feels about the decision at baseline, and likely other unmeasured factors, rather than living in a state with waiting period or two-visit requirements.
Although waiting period and two-visit requirement restrictions assume that all individuals would benefit from mandated time to reconsider their abortion decision, mean Decisional Conflict Scale scores were generally low across all groups in this analysis. This suggests that even among those considering, but not yet seeking abortion, certainty is relatively high and supports prior research conclusions that the majority of those presenting for abortion care are certain of their decision.19–22 Considering that these restrictions do not have their intended effect as most individuals are sure about their decision, it is important to note that this study did not capture possible harms of the restrictions such as the detrimental effects on emotional and logistical experience. For instance, these restrictions can make the process of obtaining abortion care more inflexible by increasing the time-sensitive nature of the process and requiring up-front investment of arranging travel, childcare, or time off of work. These constraints may make individuals feel pressured to pursue an abortion once they have started the process and put them at risk of developing negative emotions or perceptions of their care.
There are several limitations to this study. One is that we assessed decision certainty at only two points in the decision-making process. Levels of decision certainty may have fluctuated between or after these time points, and decision certainty for those pregnant and still seeking abortion at follow-up may ultimately change once a final outcome is reached. Additionally, participants who were lost to follow-up may also have different trends in decision certainty which we could not capture. Lastly, we did not measure which course of action (abortion or continuing the pregnancy) participants were most considering at baseline, and thus we cannot ascertain whether their decision certainty corresponded to having an abortion or not having an abortion. However, because the introduction to the Decisional Conflict Scale specifically asked about their abortion decision, it is likely they were describing their decision certainty regarding abortion. In any case, abortion and continuation of pregnancy are the only two possible choices, and so high conflict about one necessarily suggests high conflict about the other.
This study had several strengths. The study was designed to recruit and follow individuals living in all 50 states and the District of Columbia with and without restrictions that mandate waiting periods and two-visit requirements as they made their abortion decisions. It measured decision certainty earlier in the decision-making process in a population not well captured with other methodologies, including those who were considering abortion, but ultimately did not proceed to or were unable to access abortion care. Additionally, this study measured decision certainty at two different time points to describe change over time. We were able to compare trends in decision certainty and found no significant increase in decision certainty regarding abortion associated with living in a state with these restrictions. Rather, our study results reflect previous findings that people who ultimately obtain abortion care already have high levels of decision certainty even before seeking care, which changed very little between baseline and follow-up.
Ultimately, these restrictive laws are not associated with an increase in decision certainty. An evidence-informed approach to abortion care would therefore assume that most people are certain about their desired pregnancy outcome when they present for care and provide all pregnant people with the full range of options available to them for their pregnancy, referrals to care as requested, and decision support as needed. Restrictions that impose additional visits and waiting periods on a time-sensitive procedure assuming that all people are uncertain do not appear to be based on pregnant people's true decision-making process.
Footnotes
This research was supported by a Resource Allocation Program Award from the UCSF National Center of Excellence in Women's Health, Advancing New Standards in Reproductive Health core support, and The Susan Thompson Buffett Foundation (Upadhyay). Alice Cartwright was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health under award number P2C HD050924. Lauren Ralph was supported by NICHD, Office of Research on Women's Health, Building Interdisciplinary Research Careers in Women's Health grant No. 2K12 HD052163.
Financial Disclosure The authors did not report any potential conflicts of interest.
Presented at the National Abortion Federation’s annual meeting, April 21-24, 2018, Seattle, Washington; and at the North American Forum on Family Planning, October 19-21, 2019, Los Angeles, California.
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews are available at http://links.lww.com/AOG/C234.
Contributor Information
Iris Jovel, Email: iris.jovel@ucsf.edu.
Alice F. Cartwright, Email: alice.cartwright@unc.edu.
Lauren Ralph, Email: lauren.ralph@ucsf.edu.
REFERENCES
- 1.Kaiser Family Foundation. Mandatory waiting periods for women seeking abortions. Accessed September 1, 2020. https://www.kff.org/womens-health-policy/state-indicator/mandatory-waiting-periods
- 2.Wadhwani A. Tennessean. Tennessee's 48-hour abortion waiting period has its day in court. Accessed September 1, 2020. https://www.tennessean.com/story/news/2019/09/23/abortion-law-tennessee-waiting-period-planned-parenthood/2385126001
- 3.Loller T. Witnesses clash in Tennessee abortion wait period trial. Accessed September 1, 2020. https://abcnews.go.com/Health/wireStory/witnesses-clash-tennessee-abortion-wait-period-trial-65863500
- 4.Ralph LJ, Foster DG, Kimport K, Turok D, Roberts SC. Measuring decisional certainty among women seeking abortion. Contraception 2017;95:269–78. doi: 10.1016/j.contraception.2016.09.008 [DOI] [PubMed] [Google Scholar]
- 5.Rocca CH, Kimport K, Roberts SC, Gould H, Neuhaus J, Foster DG. Decision rightness and emotional responses to abortion in the United States: a longitudinal study. PLoS One 2015;10:e0128832. doi: 10.1371/j.pone.0128832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karasek D, Roberts SC, Weitz TA. Abortion patients' experience and perceptions of waiting periods: survey evidence before Arizona's two-visit 24-hour mandatory waiting period law. Womens Health Issues 2016;26:60–6. doi: 10.1016/j.whi.2015.10.004 [DOI] [PubMed] [Google Scholar]
- 7.Morse JE, Charm S, Bryant A, Ramesh S, Krashin J, Stuart GS. The impact of a 72-hour waiting period on women's access to abortion care at a hospital-based clinic in North Carolina. North Carolina Med J 2018;79:205–9. doi: 10.18043/ncm.79.4.205 [DOI] [PubMed] [Google Scholar]
- 8.Roberts SCM, Belusa E, Turok DK, Combellick S, Ralph L. Do 72-hour waiting periods and two-visit requirements for abortion affect women's certainty? A prospective cohort study. Women's Health Issues 2017;27:400–6. doi: 10.1016/j.whi.2017.02.009 [DOI] [PubMed] [Google Scholar]
- 9.Upadhyay UD, Jovel IJ, McCuaig KD, Cartwright AF. Using Google Ads to recruit and retain a cohort considering abortion in the United States. Contracept X 2020;2:100017. doi: 10.1016/j.conx.2019.100017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Connor AM. Validation of a decisional conflict scale. Med Decis Making 1995;15:25–30. doi: 10.1177/0272989X9501500105 [DOI] [PubMed] [Google Scholar]
- 11.O'Connor A. User manual-decisional conflict scale. Ottawa Hospital Research Institute; 1993. [Google Scholar]
- 12.Counseling and waiting periods for abortion. Guttmacher Institute; 2020. [Google Scholar]
- 13.StataCorp. Stata statistical software: release 15. StataCorp LLC; 2017. [Google Scholar]
- 14.Upadhyay UD, McCook AA, Bennett AH, Cartwright AF, Roberts SCM. State abortion policies and Medicaid coverage for abortion are associated with pregnancy outcomes among individuals seeking abortion recruited using Google Ads: a national cohort study. Soc Sci Med 2021 Feb 6 [Epub ahead of print]. doi: 10.1016/j.socscimed.2021.113747 [DOI] [PubMed] [Google Scholar]
- 15.Roberts DE. Killing the Black body: race, reproduction, and the meaning of liberty. Vintage Books; 1999. [Google Scholar]
- 16.Davis DA. Trump, race, and reproduction in the afterlife of slavery. Cult Anthropol 2019;34:26–33. doi: 10.14506/ca34.1.05 [DOI] [Google Scholar]
- 17.Luna Z. “Black children are an endangered species”: examining racial framing in social movements. Sociological Focus 2018;51:238–51. doi: 10.1080/00380237.2018.1412233 [DOI] [Google Scholar]
- 18.Harris LH, Wolfe T. Stratified reproduction, family planning care and the double edge of history. Curr Opin Obstet Gynecol 2014;26:539–44. doi: 10.1097/GCO.0000000000000121 [DOI] [PubMed] [Google Scholar]
- 19.Kumar U, Baraitser P, Morton S, Massil H. Decision making and referral prior to abortion: a qualitative study of women's experiences. J Fam Plann Reprod Health Care 2004;30:51–4. doi: 10.1783/147118904322702009 [DOI] [PubMed] [Google Scholar]
- 20.Gatter M Kimport K Foster DG Weitz TA, Upadhyay UD. Relationship between ultrasound viewing and proceeding to abortion. Obstet Gynecol 2014;123:81–7. doi: 10.1097/AOG.0000000000000053 [DOI] [PubMed] [Google Scholar]
- 21.Cameron ST, Glasier A. Identifying women in need of further discussion about the decision to have an abortion and eventual outcome. Contraception 2013;88:128–32. doi: 10.1016/j.contraception.2012.10.032 [DOI] [PubMed] [Google Scholar]
- 22.Foster DG, Gould H, Taylor J, Weitz TA. Attitudes and decision making among women seeking abortions at one U.S. clinic. Perspect Sex Reprod Health 2012;44:117–124. doi: 10.1363/4411712 [DOI] [PubMed] [Google Scholar]