Abstract
Introduction
Depression is a major global health problem with a relatively high lifetime prevalence and significant disability. Antidepressants are the most effective medications used for the treatment of depression. Hence, this study is aimed at summarizing the studies on antidepressant use among patients diagnosed with depression.
Method
PubMed, Embase, Web of Science, Scopus, and Google Scholar were searched for literature (2000-2019) using keywords such as depression, drug utilization, antidepressants, prescription, serotonin reuptake inhibitor, serotonin and norepinephrine reuptake inhibitor, tricyclic antidepressants, and atypical antidepressants.
Results
Antidepressant users were mostly females, married people, housewives, lower-income people, employees, and highly educated people, as they were found to be more prone to develop depression than their counterparts. Selective serotonin reuptake inhibitors (SSRIs), such as sertraline, were most commonly prescribed among depressive patients.
Conclusion
Our study suggested that out of five major antidepressant drugs available for the treatment of depression, selective serotonin reuptake inhibitors are preferred over others because of their better side effects and tolerability profile.
1. Introduction
Depression is a common mental disorder and a major cause of functional disability [1, 2]. According to the World Health Organization (WHO), by 2020, it will be the second-highest known cause of worldwide disability [3, 4]. Depression is characterized by a sad mood, pessimistic thought, lowered interest in day-to-day activities, poor concentration, insomnia or increased sleep, significant weight loss or gain, decreased energy, continuous feelings of guilt and worthlessness, decreased libido, and suicidal thoughts occurring for at least two weeks [5, 6]. Depressed patients can be of any gender, age, or background. Due to fear of stigmatization associated with mental disorders, patients lack to seek medical treatment in their early stages [7–9]. To maintain normal human health in patients, drugs play a crucial role. Antidepressant drugs are the most widely used and are most effective in the treatment of depression [10, 11]. For many years, tricyclic antidepressants (TCAs) have been the drug of choice for treating depression in patients [12–14]. Many new antidepressants with better tolerance and broader indications have been discovered because of an increase in the prevalence of depression throughout the world [15]. This results in the gradual replacement of conventional drugs such as TCAs and monoamine oxidase inhibitors (MAOIs) by selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and atypical antidepressants [7, 16, 17]. The most appropriate antidepressants should be selected according to symptoms and patient characteristics, with adequate dose and duration of therapy, to enhance the treatment success rate [18, 19]. However, other factors, such as adverse effect profiles, cost, safety profile, history of prior medication treatment, and patient preference, are important in the initial selection of antidepressants and should be considered by physicians [20, 21]. The optimal use of antidepressants could reduce individual distress, along with the social burden of depression [22]. The aim of the analysis of prescribing patterns is to evaluate the prescription habits of medical practitioners and to suggest necessary modifications if required to make drug therapy rational and cost-effective [6, 16]. The use of antidepressants has increased within the last two decades [23, 24]. As a result of the increased prescription and use of antidepressants, the need for information regarding the actual prescribing practices has become vital to maintain patient safety as well as to ensure that the optimal therapeutic outcome is achieved, especially when the nature of the side effects of these drugs is considered. Hence, this study is aimed at summarizing the studies on antidepressant use among patients diagnosed with depression.
2. Methods
2.1. Search Strategy
Databases such as PubMed, Embase, Web of Science, Scopus, and Google Scholar were searched for studies published between January 2000 and December 2019. The main Medical Subject Heading (MeSH) terms used for literature search within the databases were depression, drug utilization, antidepressants, and prescription. Other keywords used were serotonin reuptake inhibitor, serotonin and norepinephrine reuptake inhibitor, tricyclic antidepressants, and atypical antidepressants. For the second round of search, the keyword “antidepressant” was combined with “drug utilization”, “prescription”, “depression”, “depressive patients”, “systematic reviews”, and “narrative reviews”. The bibliographies of relevant articles were also searched for more studies that were not identified in the original database search. All the abstracts and studies were screened for their relevance and discarded those that did not fit our selection criteria. Only those studies that were identified as potentially relevant to our study title were retrieved and fully reviewed.
2.2. Study Selection
2.2.1. Inclusion Criteria
Inclusion criteria are the following: (1) literatures of varying methodologies such as observational, cross-sectional, and retrospective studies, survey, and case reports, (2) studies conducted on all patients aged ≥18 years with a primary diagnosis of depression and prescription of at least one antidepressant drug, (3) studies that mainly focused on antidepressant utilization or antidepressant prescription pattern among patients with depression, and (4) full-text articles, published in peer-reviewed journals, in years lying between 2000 and 2019 and available in English language.
2.2.2. Exclusion Criteria
Exclusion criteria are the following: (1) reviews, clinical trials, descriptive studies, pilot studies, editorials, case series, conference abstracts, letters, commentaries, posters, qualitative interviews, and book chapters; (2) studies conducted on patients younger than 18 years with no depression and not prescribed with antidepressants; pregnant or lactating mothers; those with a history of psychotic, bipolar disorder, or drug abuse; and those with cognitive impairment; (3) studies that did not focus on antidepressant utilization or antidepressant prescription pattern among patients with depression; and (4) studies published in non-peer-reviewed journals before 2000 and after 2019 and available in languages other than English.
2.2.3. Study Outcomes
Our study outcomes were the demographic factors and types of antidepressants used among patients with depression.
3. Results
The literature search process is summarized in Figure 1. A total of 51 studies were included in our review; only 13 original articles were reviewed. The studies were conducted in India [25], Bangladesh [26], Malaysia [27], Nigeria [28], Singapore [29], China [30], Italy [31], Saudi Arabia [32], USA [33], Australia [34], Germany [35], Canada [36], and Netherlands [37]. The summarized main findings of the studies are presented as follows (Table 1).
Figure 1.
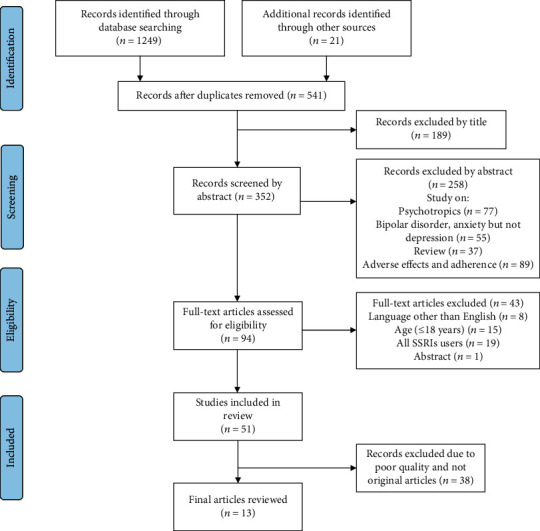
Data screening and extraction.
Table 1.
Study, sample, methods, and major findings of the studies.
| Study | Objective | Methodological review | Major findings |
|---|---|---|---|
| Tejashwini et al. [25], | To evaluate the antidepressant use pattern and associated adverse drug reactions (ADR). | Prospective observational study n = 598 Age: ≥18 years (April 2016 to September 2016) |
Major victims of depression: married, employees, and housewives with secondary education. Antidepressant receivers (majority): males (57.86%) and people aged between 41and 60 years. Commonly prescribed antidepressants: fluoxetine (50.27%), followed by sertraline (40.29%), amitriptyline (25.31%), and escitalopram (3.43%). |
| Islam et al. [26], | To evaluate the antidepressant prescription pattern following WHO prescribing indicators in two teaching hospitals. | Hospital-based descriptive cross-sectional study. n = 300 Age: 18-60 years (June 2015 to June 2016) |
Antidepressant receivers (majority): people aged between 18 and 27 years, married women, housewives, less educated, unemployed, and the lower-income group from a rural area. Commonly prescribed antidepressants: SSRI (sertraline followed by escitalopram, citalopram, and fluoxetine), TCA (amitriptyline followed by imipramine), SNRI (venlafaxine), and atypical group (mirtazapine). |
| Nahas and Sulaiman [27], | To evaluate the antidepressant prescription pattern among depressive men in Malaysia. | Cross-sectional study n = 107 Age: ≥18 years (from May 2015 to ten-month period) |
Mean age: 49.9 years. Commonly prescribed antidepressants: SSRIs (72.9%), followed by TCAs (10.3%), SNRI (8.4%), and MAOIs (2.8%). |
| Kehinde et al. [28], | To evaluate the antidepressant utilization pattern in the tertiary care hospital in Lagos. | Retrospective study n = 683 Age: ≥18 years (January 2013 to December 2014) |
Major victims of depression: people aged between 31 and 45 years, females (67.2%), married (57%), and self-employers (49.7%). Commonly prescribed antidepressants: TCAs (61.3%) and SSRIs (38.7%). Most frequently prescribed: amitriptyline (60.6%) and sertraline (20.2%). |
| Soh et al. [29], | To evaluate the antidepressant prescription pattern in a psychiatric department of a general hospital in Singapore. | Retrospective study n = 206 Age: ≥18 years (January 2013 to December 2013) |
Mean age: 50 years The majority of the patients were females (63.6%), married (70.9%), highly educated (46.1% had tertiary education), and full-time employees (60.2%). Commonly prescribed antidepressants: SSRIs (75.5%), followed by atypical antidepressants (13.5%) and TCAs (8.5%). |
| Chen et al. [30], | To evaluate the prevalence and prescription of antidepressants used in depression in Asia. | Cross-sectional study n = 956 Age: ≥18 years |
Mean age: 45.2 years Antidepressant receivers (majority): females Commonly prescribed antidepressants: sertraline (19.6%), escitalopram (18.6%), and mirtazapine (16.1%). |
| Trifirò et al. [31], | To evaluate the antidepressant prescription pattern in Italian primary care. | A prospective, observational cohort study n = 1,377 Age: ≥18 years (1 January 2007 to 1 June 2008) |
Mean age: 52 years Antidepressant receivers (majority): 45-64 years age group, where most of them were females (71.5%), homemakers (31.1%), married or cohabiting (60.4%), highly educated (44.2%), and current or former smokers and alcohol consumers and obese (53.5%). Frequently prescribed antidepressants: SSRIs (paroxetine 25.9% and escitalopram 18.4%), SNRIs (venlafaxine 11.6% and duloxetine 5.6%) (80.2%), and TCA (2%). |
| Alhulwah et al. [32], | To evaluate the long-time users of antidepressants at Riyadh Military Hospital. | Cross-sectional study n = 120 Age: ≥18 years (July 2009 to September 2010) |
Mean age: 42 years Antidepressant receivers (majority): females (57.5%) and 35-50 years age group (46%) Commonly prescribed antidepressants: SSRI (61.7%), atypical antidepressant (14.2%), and TCA (11.7%), respectively. |
| Prukkanone et al., [33] | To evaluate the antidepressant prescription pattern in the hospice program. | Retrospective cohort study n = 17 Age: ≥18 years (June 2007 and December 2008) |
Most users were female. Commonly prescribed antidepressants: SSRIs (prescribed in 9 out of 10 patients). |
| Shiroma et al. [34], | To measure adherence and determine the antidepressant prescription pattern in patients with major depression. | Retrospective study, n = 1,058 Age: ≥18 years (patient treated between August 2005 and September 2008) |
Average age: 46 years Antidepressant receivers (majority): females (64%) and 15-86 years age group Commonly prescribed antidepressants: fluoxetine (in two-thirds of patients), TCAs, and other SSRIs. |
| Bauer et al. [35], | To evaluate the recent antidepressant prescription pattern in European countries. | Prospective, observational study n = 3,468 Age: ≥18 years (May 2004 to September 2005) |
Mean age: 46.8 years Antidepressant receivers (majority): females (68.2%), married, less educated, unemployed, paid workers, and smokers. Commonly prescribed antidepressants: SSRIs (63.3%), followed by TCAs (26.5%) and SNRIs (13.6%). |
| Beck et al. [36], | To evaluate the antidepressant utilization in relation to sociodemographic variables, in Canada. | Cross-sectional survey n = 2,145 Age: ≥18 years (May-December 2002) |
The majority of antidepressant users were age group (25-64 years), females, married, lowest-income group, and people with higher education. |
| Meijer et al. [37], | To evaluate the prescribing pattern in patients using new antidepressants. | Observational cohort study n = 1,251 Age: ≥18 years (1995-1997) |
Median age: 41 years Female: 64.1% Commonly prescribed antidepressants: sertraline (52.7%), paroxetine (31.2%), fluoxetine (9.2%), and fluvoxamine (7%). |
4. Discussion
We identified thirteen studies through this review, and the majority of the patients were in the economically productive age group of 40-50 years [25–30, 32–37]. Conversely, the findings of a study from Italy showed that the mean age of the patients receiving antidepressant prescriptions was more than 50 years [31]. Our review showed that the majority of the patients receiving antidepressants for the treatment of their depression were females [26, 28–41]. This could be due to hormones that are associated with the regulation of the menstruation cycle and pregnancy affecting mood in females. These alterations in hormonal regulation cause dysregulation of the stress response, which makes them more sensitive to depression and often shows magnified neuroendocrine responses to even low levels of stress [28, 38, 39, 42]. Women play multiple roles in family and society, such as homemakers, spouses, mothers, professionals, and caregivers. These multiple responsibilities may be the source of increased stress that might have led to depression in them [43, 44]. In many societies, until today women are not given equal respect, they are considered less powerful with low status, they cannot make a choice, and they are sexually abused, which all results in the development of depression in them [5, 42]. In contrast, a study from our neighboring country, India, depicted more depressive males than females, which could be due to more stress at work, a monotonous lifestyle with no entertainment, low income, and economic burden of family [25]. Evidence suggests that depression is associated with various psychological factors, such as loneliness, lack of family care and affection, poor family support, insufficient time with children, high use of emotional coping, low level of spirituality, stressful incidents, poor health, and dependency [25, 38]. Sedentary lifestyle, lack of physical exercise, lack of hobby, irregular dietary habits, smoking, and taking alcoholic beverages or substance abuse are also interconnected with depression [25, 30, 35]. Continuous arguments, stressful daily routines, unsupportive spouses, continuous discouragement, lack of family time or husbands or wives going to other countries for employment, and ignorance from family members may be the reason for more married, housewives, and lower-income people being vulnerable to depression [25, 26, 28, 29, 31, 35, 36, 45]. One study showed that a spouse's weekly working hours are greatly associated with the partner's risk of developing depression and suicidal thoughts [46]. This means that long working hours not only affect individuals' own mental health but also affect their spouses [46]. Unsatisfactory job, lower income, high level of physical activity, time pressure, lack of encouragement, promotion, and job security are associated with lowering self-esteem and hence could be the reason for taking antidepressants by a high number of employees involved in paid works [25, 29, 35]. Similarly, being concerned about more profit or suffering a continuous loss in business may also lead to depression in people involved in self-employed business [28]. Our review showed that education is another source of depression in many people. People with a higher education background becomes the victim of depression when they do not get a job equivalent to their qualification. On the other hand, in the job they got involved, they have to work as instructed with unsatisfactory payment and no opportunity to implement their knowledge and skills due to which they feel lack of challenges in their work along with lack of intellectual growth in them [25, 29, 31, 36]. However, other studies have displayed less educated people as victims of depression [26, 35]. These people work as machine operators, laborers, farmers, and unskilled manual workers, where there is more physical and psychological-related stress along with less respect from other employees.
The prescribing pattern of antidepressants for patients with depression varies across different countries. This could be due to differences in availability and antidepressant prices as well as variations in recommendations in each country's national guidelines [28, 36]. Medical treatment of depression not only improves the mental health of patients but also increases their physical and social performance, making them optimistic and encouraged towards life [32]. Our review revealed that SSRIs are the dominant antidepressants prescribed over TCAs, SNRIs, and other atypical antidepressants for the treatment of depression [25–27, 29–37]. The preference of psychiatrists for SSRI prescription over other antidepressants could be because of the advantages they offer to the patients. Antidepressants other than SSRIs nonselectively inhibit the reuptake of norepinephrine, dopamine, and serotonin into presynaptic vesicles and affect adrenergic, cholinergic, postsynaptic serotonin, and histaminic receptors in the brain, which are unrelated to depression, leading to intolerable adverse effects [47]. SSRIs do not cause life-threatening adverse effects, such as overdose-related cardiotoxicity and CNS toxicity, as they do not show receptor antagonism [48]. Additionally, they can be administered once daily, require less dose titration than TCAs, are safer, and show fewer side effects compared to other antidepressants [26, 31, 33–37, 49]. Hence, it could be safer and effective for many patients. In contrast, a study showed TCAs as the most commonly prescribed antidepressants despite SSRIs being more advantageous [28]. This could be due to the affordability and easy availability of TCAs over SSRIs. In developing countries, the affordability of drugs plays an important role in the continuation of treatment because many low-income families cannot afford expensive medicines. The majority of the population has to rely on government insurance policies to obtain drugs for their treatment. Many people buy their prescribed antidepressants from the government hospital as they are available at cheaper prices than in retail pharmacies. Such regional differences along with cultural differences and country economy also create huge differences in the prescription of antidepressants [50, 51]. Our review showed that sertraline was the most frequently prescribed SSRI, followed by others such as escitalopram, fluoxetine, paroxetine, and fluvoxamine. Amitriptyline was commonly prescribed among TCAs, venlafaxine and duloxetine among SNRIs, and mirtazapine and bupropion among atypical antidepressants.
4.1. Limitation and Strength of the Study
There are certain limitations to our study. Literature published in languages other than English was excluded, which might be associated with language bias. The data used were observational, cross-sectional, retrospective, survey, and case reports only. This does not provide direct insight into the changing trends of prescribing behaviors of physicians over time in patients and may reflect a bias. Likewise, based on clinical setting and physician variables, prescription pattern varies. This study does not provide information on such variables and clinical appropriateness of antidepressants used. However, systematic search strategy and review of types of studies included which are of about two decades are the strength of this study. Additionally, a number of characteristics associated with antidepressant prescription such as age, gender, education, marital state, socioeconomic status, and all other sociodemographic factors are identified. Hence, the findings of this study are expected to have a good impact on the education of psychopharmacology.
5. Conclusion
Our study revealed that the majority of antidepressant users were aged between 40 and 50 years, females, married, housewives, lower income, and highly educated people. SSRIs were found to be highly prescribed over TCAs, SNRIs, MAOIs, and atypical antidepressants. Among the prescribed SSRIs, sertraline was the dominant SSRI. The result of this study suggests the further need for high-quality studies, which may consider the use of data sources like clinical files and patient self-reports, and also includes reports on whether antidepressants were prescribed to treat physical or mental symptoms.
Acknowledgments
We acknowledge all the authors of the retrieved original articles and surveys.
Data Availability
The raw data used to support the findings of this study are made available from the corresponding author upon reasonable request.
Disclosure
We would like to pledge that the aforementioned manuscript has been published as a preprint with doi: https://10.21203/rs.3.rs-65197/v1.
Conflicts of Interest
The authors declare that they have no competing interests.
References
- 1.Ferrari A. J., Charlson F. J., Norman R. E., et al. The epidemiological modelling of major depressive disorder: application for the Global Burden of Disease Study 2010. PLoS One. 2013;8(7, article e69637) doi: 10.1371/journal.pone.0069637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferrari A. J., Charlson F. J., Norman R. E., et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Medicine. 2013;10(11, article e1001547) doi: 10.1371/journal.pmed.1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Depression WH. Other common mental disorders: global health estimates. Geneva: World Health Organization; 2017. [Google Scholar]
- 4.Banerjee I., Sathian B., Chakraborty P. K., et al. Pharmacotherapy of bipolar affective disorder: a hospital based study from sub Himalayan Valley of Nepal. Journal of clinical and diagnostic research: JCDR. 2014;8(6):HC22–HC27. doi: 10.7860/JCDR/2014/8661.4524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shrestha Manandhar J., Shrestha R., Basnet N., Silwal P., Shrestha H., Risal A. Study of adherence pattern of antidepressants in patients with depression. Kathmandu University Medical Journal. 2017;57(1):3–9. [PubMed] [Google Scholar]
- 6.Hussain A., Sekkizhar M., Kumar M. A., Niramala P. An observational study on drug utilization pattern and pharmacovigilance of antidepressant drugs. Journal of Medical Science and Clinical Research. 2018;6(10):540–552. doi: 10.18535/jmscr/v6i10.91. [DOI] [Google Scholar]
- 7.Huang C. H., Chen C. M., Hsu K. Y., Wang L. J., Chen S. Y., Lee C. F. The prescription pattern and analyses of antidepressants under the National Health Insurance Policy in Taiwan. Taiwanese Journal of Psychiatry. 2011;25(2):76–85. [Google Scholar]
- 8.Kanter J. W., Rusch L. C., Brondino M. J. Depression self-stigma. Journal of Nervous & Mental Disease. 2008;196(9):663–670. doi: 10.1097/NMD.0b013e318183f8af. [DOI] [PubMed] [Google Scholar]
- 9.Hsu L. K. G., Wan Y. M., Chang H., Summergrad P., Tsang B. Y. P., Chen H. Stigma of depression is more severe in Chinese Americans than Caucasian Americans. Psychiatry. 2008;71(3):210–218. doi: 10.1521/psyc.2008.71.3.210. [DOI] [PubMed] [Google Scholar]
- 10.van Servellen G., Heise B. A., Ellis R. Factors associated with antidepressant medication adherence and adherence-enhancement programmes: a systematic literature review. Mental Health in Family Medicine. 2011;8(4):255–271. [PMC free article] [PubMed] [Google Scholar]
- 11.Akincigil A., Bowblis J. R., Levin C., Walkup J. T., Jan S., Crystal S. Adherence to antidepressant treatment among privately insured patients diagnosed with depression. Medical Care. 2007;45(4):363–369. doi: 10.1097/01.mlr.0000254574.23418.f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bae K. Y., Kim S. W., Kim J. M., et al. Antidepressant prescribing patterns in Korea: results from the clinical research center for depression study. Psychiatry investigation. 2011;8(3):234–244. doi: 10.4306/pi.2011.8.3.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lawrenson R. A., Tyrer F., Newson R. B., Farmer R. D. The treatment of depression in UK general practice: selective serotonin reuptake inhibitors and tricyclic antidepressants compared. Journal of Affective Disorders. 2000;59(2):149–157. doi: 10.1016/S0165-0327(99)00147-0. [DOI] [PubMed] [Google Scholar]
- 14.Anderson I. M., Ferrier I. N., Baldwin R. C., et al. Evidence-based guidelines for treating depressive disorders with antidepressants: a revision of the 2000 British Association for Psychopharmacology guidelines. Journal of Psychopharmacology. 2008;22(4):343–396. doi: 10.1177/0269881107088441. [DOI] [PubMed] [Google Scholar]
- 15.Liu Y. M., Yang Y. H., Hsieh C. R. Financial incentives and physicians' prescription decisions on the choice between brand-name and generic drugs: Evidence from Taiwan. Journal of health economics. 2009;28(2):341–349. doi: 10.1016/j.jhealeco.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 16.Milea D., Verpillat P., Guelfucci F., Toumi M., Lamure M. Prescription patterns of antidepressants: findings from a US claims database. Current medical research and opinion. 2010;26(6):1343–1353. doi: 10.1185/03007991003772096. [DOI] [PubMed] [Google Scholar]
- 17.Ghosh S., Roychaudhury S. Prescribing pattern of antidepressant drugs in a tertiary care hospital of eastern India. Journal of Chemical and Pharmaceutical Research. 2014;6(6):2593–2597. [Google Scholar]
- 18.American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder (revision) The American Journal of Psychiatry. 2000;157(Supplement 4):1–45. [PubMed] [Google Scholar]
- 19.Lagerberg T., Molero Y., D’Onofrio B. M., et al. Antidepressant prescription patterns and CNS polypharmacy with antidepressants among children, adolescents, and young adults: a population-based study in Sweden. European Child & Adolescent Psychiatry. 2019;28(8):1137–1145. doi: 10.1007/s00787-018-01269-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gelenberg A. J., Freeman M. P., Markowitz J. C., et al. American Psychiatric Association practice guidelines for the treatment of patients with major depressive disorder. The American Journal of Psychiatry. 2010;167(Supplement 10):9–118. [Google Scholar]
- 21.Qaseem A., Snow V., Denberg T. D., Forciea M. A., Owens D. K. Using second-generation antidepressants to treat depressive disorders: a clinical practice guideline from the American College of Physicians. Annals of Internal Medicine. 2008;149(10):725–733. doi: 10.7326/0003-4819-149-10-200811180-00007. [DOI] [PubMed] [Google Scholar]
- 22.Kim J. M., Stewart R., Kim S. W., et al. Interactions between life stressors and susceptibility genes (5-HTTLPR and BDNF) on depression in Korean elders. Biological Psychiatry. 2007;62(5):423–428. doi: 10.1016/j.biopsych.2006.11.020. [DOI] [PubMed] [Google Scholar]
- 23.Abbing-Karahagopian V., Huerta C., Souverein P. C., et al. Antidepressant prescribing in five European countries: application of common definitions to assess the prevalence, clinical observations, and methodological implications. European journal of clinical pharmacology. 2014;70(7):849–857. doi: 10.1007/s00228-014-1676-z. [DOI] [PubMed] [Google Scholar]
- 24.Exeter D., Robinson E., Wheeler A. Antidepressant dispensing trends in New Zealand between 2004 and 2007. Australian and new Zealand Journal of psychiatry. 2009;43(12):1131–1140. doi: 10.3109/00048670903279879. [DOI] [PubMed] [Google Scholar]
- 25.Tejashwini K., Bhushan A., Suma S., Katte R. Drug utilization pattern and adverse drug reactions in patients on antidepressants. National Journal of Physiology, Pharmacy and Pharmacology. 2019;9(1):1–11. doi: 10.5455/njppp.2019.9.103222910102018. [DOI] [Google Scholar]
- 26.Islam B., Shahriar I., Jannat T. Prescribing pattern of antidepressant drugs in two teaching hospitals in Bangladesh. Mediscope. 2019;6(2):53–58. doi: 10.3329/mediscope.v6i2.43153. [DOI] [Google Scholar]
- 27.Nahas A. R. F., Sulaiman S. A. S. Prescribing patterns of antidepressants among depressive men in Malaysia: a survey. Journal of Young Pharmacists. 2018;10(1):98–101. doi: 10.5530/jyp.2018.10.22. [DOI] [Google Scholar]
- 28.Kehinde O. A., Anyika E. N., Abah I. Drug utilization patterns of antidepressants in federal neuro-psychiatric hospital Lagos, Nigeria. Journal of Hospital Administration. 2017;6(5):p. 12. doi: 10.5430/jha.v6n5p12. [DOI] [Google Scholar]
- 29.Soh T. H., Lim L., Chan H. N., Chan Y. H. Antidepressant prescribing patterns for depressive and anxiety disorders in a Singapore hospital. Open Journal of Psychiatry. 2015;5(2):144–152. doi: 10.4236/ojpsych.2015.52016. [DOI] [Google Scholar]
- 30.Chen C., Si T.-M., Xiang Y.-T., et al. Prevalence and prescription of antidepressants in depression with somatic comorbidity in Asia: the research on East Asian psychotropic prescription patterns study. Chinese medical journal. 2015;128(7):853–858. doi: 10.4103/0366-6999.154272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trifirò G., Tillati S., Spina E., et al. A nationwide prospective study on prescribing pattern of antidepressant drugs in Italian primary care. European journal of clinical pharmacology. 2013;69(2):227–236. doi: 10.1007/s00228-012-1319-1. [DOI] [PubMed] [Google Scholar]
- 32.Alhulwah L. M., Alhathloul A. M., Alblowi A. S., Alyahya K. M. Long term antidepressants prescribing in the Psychiatry Department at Riyadh Military Hospital. Cross-sectional study. Saudi Medical Journal. 2011;32(10):1051–1054. [PubMed] [Google Scholar]
- 33.Prukkanone B., Vos T., Burgess P., Chaiyakunapruk N., Bertram M. Adherence to antidepressant therapy for major depressive patients in a psychiatric hospital in Thailand. BMC Psychiatry. 2010;10(1) doi: 10.1186/1471-244X-10-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shiroma P. R., Geda Y. E., Mohan A., Richardson J. Antidepressant prescription pattern in a hospice program. American Journal of Hospice and Palliative Medicine®. 2011;28(3):193–197. doi: 10.1177/1049909110385539. [DOI] [PubMed] [Google Scholar]
- 35.Bauer M., Monz B. U., Montejo A. L., et al. Prescribing patterns of antidepressants in Europe: results from the Factors Influencing Depression Endpoints Research (FINDER) study. European Psychiatry. 2008;23(1):66–73. doi: 10.1016/j.eurpsy.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 36.Beck C. A., Patten S. B., Williams J. V. A., et al. Antidepressant utilization in Canada. Social psychiatry and psychiatric epidemiology. 2005;40(10):799–807. doi: 10.1007/s00127-005-0968-0. [DOI] [PubMed] [Google Scholar]
- 37.Meijer W. E. E., Heerdink E. R., Pepplinkhuizen L. P., van Eijk J. T. M., Leufkens H. G. M. Prescribing patterns in patients using new antidepressants. British journal of clinical pharmacology. 2001;51(2):181–183. doi: 10.1111/j.1365-2125.2001.01329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kendler K. S., Kuhn J., Prescott C. A. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. The American Journal of Psychiatry. 2004;161(4):631–636. doi: 10.1176/appi.ajp.161.4.631. [DOI] [PubMed] [Google Scholar]
- 39.Piparva K. G., Singh A. P., Trivedi H. R., Parmar D. M., Gajera M. V. Drug utilization study of psychotropic drugs in outdoor patients in a teaching hospital. Indian journal of psychological medicine. 2011;33(1):54–58. doi: 10.4103/0253-7176.85396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lamichhane D. C., Giri B. R., Pathak O. K., Panta O. B., Shankar P. R. Morbidity profile and prescribing patterns among outpatients in a teaching hospital in Western Nepal. McGill journal of medicine: MJM : an international forum for the advancement of medical sciences by students. 2006;9(2):126–133. [PMC free article] [PubMed] [Google Scholar]
- 41.Avasthi A., Grover S., Aggarwal M. Research on antidepressants in India. Indian journal of psychiatry. 2010;52(7) Supplement 1:p. 341. doi: 10.4103/0019-5545.69263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nolen-Hoeksema S. Gender differences in depression. Current Directions in Psychological Science. 2016;10(5):173–176. [Google Scholar]
- 43.Jerg-Bretzke L., Limbrecht K. Where have they gone? A discussion on the balancing act of female doctors between work and family. GMS Zeitschrift für medizinische Ausbildung. 2012;29(2):p. Doc19. doi: 10.3205/zma000789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Banerjee S., Varma R. P. Factors affecting non-adherence among patients diagnosed with unipolar depression in a psychiatric department of a tertiary hospital in Kolkata, India. Depression research and treatment. 2013;2013:12. doi: 10.1155/2013/809542.809542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dutta S., Kaul V., Beg M. A., Singh N. K., Dutta S., Bawa S. A comparative drug utilization study of depression patients between tertiary care teaching hospital and private practitioners of Dehradun City, Uttarakhand. Journal of Drug Delivery and Therapeutics. 2015;5:45–49. [Google Scholar]
- 46.Yoon J. H., Kang M. Y. The crossover effect of spouses’ long working hours on depressive symptoms and suicidal ideation. Industrial Health. 2016;54(5):410–420. doi: 10.2486/indhealth.2015-0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ferguson J. M. SSRI antidepressant medications: adverse effects and tolerability. Primary care companion to the Journal of clinical psychiatry. 2001;3(1):22–27. doi: 10.4088/PCC.v03n0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hiemke C., Härtter S. Pharmacokinetics of selective serotonin reuptake inhibitors. Pharmacology & therapeutics. 2000;85(1):11–28. doi: 10.1016/S0163-7258(99)00048-0. [DOI] [PubMed] [Google Scholar]
- 49.Bauer M., Whybrow P. C., Angst J., Versiani M., Möller H. J. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders, part 1: acute and continuation treatment of major depressive disorder. The World Journal of Biological Psychiatry. 2009;3(1):5–43. doi: 10.3109/15622970209150599. [DOI] [PubMed] [Google Scholar]
- 50.Mamdani M., Wilby K. International variation in drug utilization: Antidepressant utilization in North America, Greece, and Ireland. Journal of Health Specialties. 2013;1(2):78–83. doi: 10.4103/1658-600x.114689. [DOI] [Google Scholar]
- 51.Zito J. M., Safer D. J., de Jong-van den Berg L. T. W., et al. A three-country comparison of psychotropic medication prevalence in youth. Child and Adolescent Psychiatry and Mental Health. 2008;2(1):p. 26. doi: 10.1186/1753-2000-2-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data used to support the findings of this study are made available from the corresponding author upon reasonable request.


