Abstract
Background
There is a gap between evidence and practice in the management of cardiovascular (CV) risk. Previous research indicated benefits from community-based, multi-faceted interventions to screen, diagnose, and manage CV risk in people with hypertension.
Methods
The Heart Outcomes Prevention and Evaluation 4 Canada pilot study (HOPE 4) was a quasi-experimental pre–post interventional study, involving one community each in Hamilton, Ontario and Surrey, British Columbia, Canada. Individuals aged ≥50 years with newly diagnosed or poorly controlled hypertension were included. The intervention was comprised of: (i) simplified diagnostic/treatment algorithms implemented by community health workers (firefighters in British Columbia and community health workers in Ontario) guided by decision support and counselling software; (ii) recommendations for evidence-based CV medications and lifestyle modifications; and (iii) support from family/friends to promote healthy behaviours. The intervention was developed as part of the international Heart Outcomes Prevention and Evaluation 4 Canada pilot study trial and adapted to the Canadian context. The primary outcome was the change in Framingham Risk Score 10-year CV disease risk estimate between baseline and 6 months.
Results
Between 2016 and 2017, a total of 193 participants were screened, with 37 enrolled in Surrey, and 19 in Hamilton. Mean age was 69 years (standard deviation 11), with 54% female, 27% diabetic, and 73% with a history of hypertension. An 82% follow-up level had been obtained at 6 months. Compared to baseline, there were significant improvements in the Framingham Risk Score 10-year risk estimate (30.6% vs 24.7%, P < 0.01), and systolic blood pressure (153.1 vs 136.7 mm Hg, P < 0.01). No significant changes in lipids or healthy behaviours were noted.
Conclusions
A comprehensive approach to health care delivery, using a community-based intervention with community health workers, supported by mobile-health technologies, has the potential to significantly reduce cardiovascular risk, but further evaluation is warranted.
Résumé
Contexte
Il existe un écart entre les données probantes et la pratique en matière de prise en charge du risque cardiovasculaire (CV). Les résultats d’études antérieures montrent que des interventions à volets multiples en milieu communautaire visant à dépister, à diagnostiquer et à prendre en charge le risque CV chez les personnes atteintes d’hypertension peuvent être bénéfiques.
Méthodologie
L’étude pilote HOPE4 (Heart Outcomes Prevention and Evaluation 4 Canada) était une étude interventionnelle quasi expérimentale évaluant des patients avant et après certaines interventions, menée au sein de deux communautés canadiennes, l’une située à Hamilton, en Ontario et l’autre à Surrey, en Colombie-Britannique. L’étude réunissait des participants âgés de 50 ans ou plus venant de recevoir un diagnostic d’hypertension ou souffrant d’hypertension mal maîtrisée. Les interventions comprenaient : i) l’utilisation d’algorithmes de diagnostic et de traitement simplifiés par les intervenants en santé du milieu communautaire (pompiers en Colombie-Britannique et agents de santé communautaire en Ontario), à l’aide d’un logiciel d’aide à la décision et de counselling; ii) la formulation de recommandations fondées sur des données probantes concernant la prise de médicaments et l’adoption d’habitudes de vie favorisant la santé CV; et iii) la sollicitation du soutien des membres de la famille et des amis afin de promouvoir l’adoption de comportements favorisant la santé. Ces interventions ont été mises au point dans le cadre de l’étude pilote internationale HOPE4 et adaptées au contexte canadien. Le critère d’évaluation principal était la variation du score de risque de Framingham, qui estime le risque de maladie CV à 10 ans, entre le début et le 6e mois de l’étude.
Résultats
De 2016 à 2017, un nombre total de 193 participants ont été soumis au processus de sélection; 37 patients du centre de Surrey et 19 patients du centre de Hamilton ont été admis à l’étude. L’âge moyen des participants était de 69 ans (écart-type : 11 ans); 54 % d’entre eux étaient des femmes, 27 % étaient atteints de diabète et 73 % avaient des antécédents d’hypertension. Au 6e mois, 82 % des sujets participaient toujours à l’étude. Des améliorations significatives ont été observées comparativement au placebo en ce qui concerne le score de risque de Framingham estimant le risque à 10 ans (30,6 % vs 24,7 %, p < 0,01) et la pression artérielle systolique (153,1 vs 136,7 mmHg, p < 0,01). Aucune variation significative n’a été observée quant à la lipidémie ou aux comportements favorisant la santé.
Conclusions
Une approche exhaustive de la prestation des soins de santé reposant sur des interventions de la part des agents de santé communautaire au moyen de technologies de santé mobiles pourrait aider à réduire significativement le risque CV; une évaluation plus poussée est toutefois nécessaire.
Cardiovascular disease (CVD) affects half of all individuals during their lifetime.1, 2, 3 Multiple modifiable risk factors contribute to its development, with hypertension the most significant.4 Unfortunately, there are significant evidence-practice gaps in detection and management of established CVD and its risk factors everywhere.5,6 For example, despite clear evidence for the benefits of blood pressure (BP) reduction and the availability of low-cost and safe medication,7 most hypertensive individuals are undetected, undertreated, or poorly controlled, with as few as 18% achieving control in high-income countries, as reported in the Population Urban Rural Epidemiologic (PURE) study.8, 9, 10
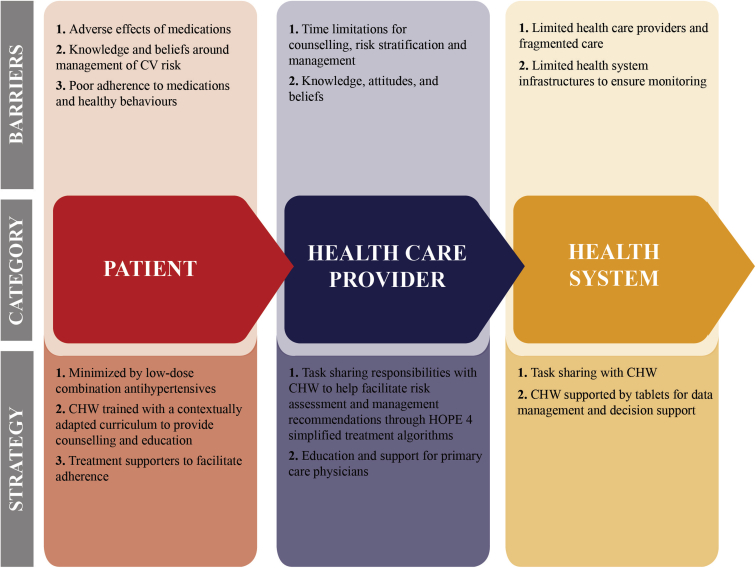
Barriers to CVD prevention occur at the patient, health care provider, and health system levels.11, 12, 13, 14, 15, 16 Unfortunately, people often lack awareness of their condition, and limited access to care can contribute to low treatment rates and poor adherence to medication and recommended lifestyle changes.17 Furthermore, there are few approaches supported by evidence for screening CVD risk, and few systematic efforts to enhance adherence to treatment or to educate patients. Current algorithms to initiate medication are often complex and impractical, and many existing guidelines neglect the role of other CVD risk factors beyond BP.18 Community health workers (CHWs) can address several barriers to CVD risk detection and management. A recent systematic review has highlighted the benefit of task sharing between physicians and CHWs with respect to the screening, diagnosis, and management of hypertension.19 Most published evidence is derived from middle- and low-resource settings; however, community-based CHWs may also have significant impact in low-resource settings within high-income countries.
The primary objective of the Heart Outcomes Prevention and Evaluation 4 (HOPE 4) Canada pilot study was to develop and pilot a community-based, multifaceted intervention package provided by non-physician health workers to improve long-term CVD risk in people with hypertension, by addressing barriers identified in a detailed assessment of the experiences of those with hypertension in each context at the patient, health care provider, and health system levels.
Methods
Study design and community selection
The HOPE 4 Canada pilot study is a community-based, pre–post interventional study involving communities in Hamilton, Ontario (ON) and Surrey, British Columbia (BC), Canada. The city of Surrey, BC has a population of approximately 500,000, of whom 20% live in the lowest quintile of socioeconomic status, and where hypertension has a prevalence of 21.7% (3.4% greater than the provincial average).20,21 The city of Hamilton, ON has a population of approximately 600,000, with 15% of individuals living in poverty.22 The prevalence of hypertension in Hamilton approaches 18%.23
Participant selection
Screening to identify eligible participants involved a combination of household sampling and the use of community outreach centres or events based within public spaces, as appropriate to the community. For this screening, medical clinics (eg, primary care physician offices or hypertension clinics) were purposely avoided. Participants were considered eligible if they were aged ≥50 years with at least ONE of the following criteria: (i) systolic blood pressure (SBP) ≥160 mm Hg was recorded at 1 visit; (ii) SBP 140-159 mm Hg was recorded in 1 visit AND participant reported a medical diagnosis of hypertension or was taking anthypertensive medication; (iii) SBP ≥ 130 mm Hg was recorded in 1 visit AND participant reported a medical diagnosis of diabetes or was taking medication for diabetes; (iv) participants did not meet criteria 1-3, but SBP of 140-159 mm Hg was recorded on 2 separate visits at least 24 hours apart. Blood pressure was measured using 3 separate readings, in which the last 2 were averaged to ensure consistency of recordings, and an automated Omron monitor was used at each visit. All screened participants provided written consent, and all enrolled participants provided full informed written consent. The study was approved by the Hamilton Integrated Research Ethics Board (#13-437) and the Simon Fraser University Research Ethics Board (#H15-01233).
Participants were considered ineligible for this study if they (i) refused to consent; (ii) were concurrently participating in any other study or heart health program that would compromise the protocol of the HOPE 4 Canada pilot study at the time of enrollment; (iii) had a severe comorbid condition with life expectancy <1 year; or (iv) had other medical serious condition(s) or factors likely to interfere with study participation or with their ability to complete the trial.
Intervention
Although the HOPE 4 Canada pilot study has foundations similar to those of the larger HOPE 4 multi-centre, cluster randomized controlled trial (RCT) in Colombia and Malaysia, it has a different design, and a modification of the intervention.24 The development and justification of the HOPE 4 international RCT intervention has been published previously.24 Following screening (Supplemental Appendices S1 and S2), participants in the HOPE 4 Canada pilot study received a tailored multifaceted intervention package designed to address identified barriers at the patient, health care provider, and health system level.25, 26, 27, 28 This package was modified from the HOPE 4 International RCT and entails: (i) detection, treatment, and control of CVD risk factors by CHWs in the community, who use tablet-based simplified management algorithms, decision support, and counseling programs; and (ii) support from a participant-nominated treatment supporter (either a friend or family member; Fig. 1). Details of the 1-week CHW training curriculum, which was developed and piloted in Canada, have been reported previously.29 Following baseline assessment and counseling, participants were seen by CHWs at 4-6 weeks, 10-14 weeks, and the final 6-month follow-up.
Figure 1.
Heart Outcomes Prevention and Evaluation 4 (HOPE 4) Canada pilot study intervention strategies to address barriers to cardiovascular (CV) disease risk reduction. CHW, community health worker.
Although the HOPE 4 international cluster RCT used a strategy similar to the one implemented in Canada, it is essential to note that each intervention package was adapted following an assessment of the local context. For example, in Canada, the HOPE 4 pilot study focused on identifying high-risk individuals within the community and connecting them to existing services and programs. CHWs were responsible for identifying participants with new or poorly controlled hypertension and then recommending an evidence-based management strategy of antihypertensive medications and a statin, to both participants and their primary care physician (Supplemental Appendix S3).30 Furthermore, the CHWs provided counselling regarding health lifestyle behaviours, including diet, exercise, medication adherence, and smoking cessation.24 Given that access to medications for CVD risk reduction was considered to be less of a barrier, compared to the accessibility in low- and middle-income countries, particularly for those aged ≥ 65 years (where public drug funding through PharmaCare, and BC and Ontario Drug Benefit is available), medications were not provided as part of the intervention in this Canadian pilot study.
To promote sustainability of the program, and consistency with the core element of the intervention, adaptation to local context and existing infrastructure was used when possible. In Surrey, the HOPE 4 Canada pilot study utilized the existing Surrey Fire Service’s community fire check safety program, which involved household screening for hazards in vulnerable households and neighborhoods. By leveraging this existing program and the enthusiastic support of the Surrey Fire Chief (L. Garis), community-based firefighters were trained to implement the intervention package as non-physician health workers. In Hamilton, the Urban Core Community Health Centre was the central hub within a low-resource setting. Individuals without any formal health care training but who were associated with the Community Health Centre were recruited as CHWs in Hamilton.
Outcomes
The primary outcome was the mean difference in the Framingham Risk Score (FRS) change from baseline to 6 months, presented as the FRS 10-year risk estimate. Given the potential for detection bias during the study follow-up, the development of a new diagnosis of diabetes after the initial screening assessment did not factor into the FRS calculations at 6 months. The validated FRS was chosen as the primary outcome because it includes multiple CVD risk factors (ie, blood pressure, smoking, cholesterol) targeted by the intervention.31
Secondary outcomes included the change from baseline to 6 months in: (i) SBP; (ii) proportion of participants with well-controlled SBP (ie, ≤140 mm Hg); (iii) low-density lipoprotein (LDL), high-density lipoprotein, total cholesterol, triglycerides, and glucose; (iv) smoking status; (v) physical activity; and (vi) proportion of participants receiving 2 or more antihypertensives and a statin.
Analysis
Continuous variables are reported as mean and standard deviation. Categorical variables are reported as number and percentage of participants corresponding to each category. Baseline and 6-month data were compared using the paired t-test for continuous measures, and McNemar's test for categorical measures. As the sample size of this study was small, and participants were recruited opportunistically from household and community settings, P-values reported in this article need to be interpreted with caution. All analyses were conducted using SAS version 9.2
Results
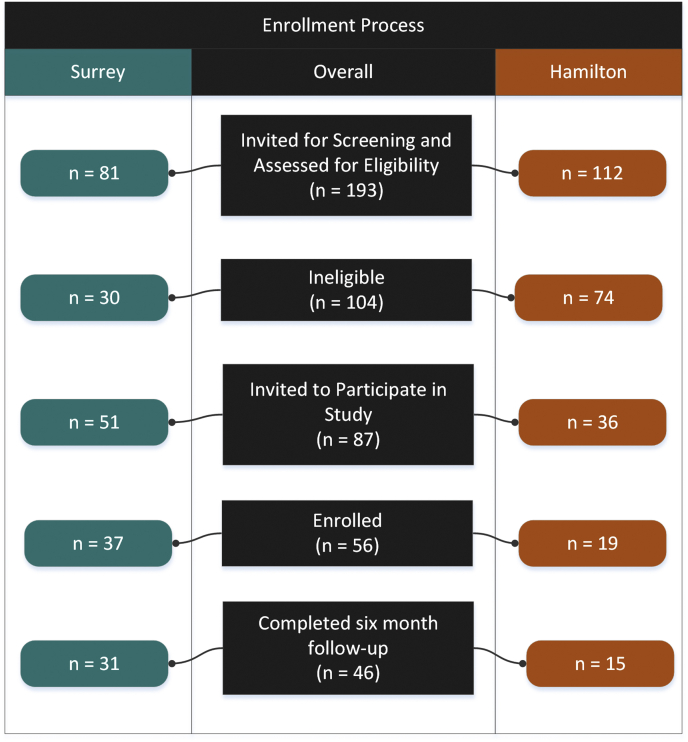
Between January 2016 and November 2017, a total of 193 participants were screened for participation. Of these, 104 were ineligible, and 87 were invited to participate. A total of 56 participants provided informed consent (37 in Surrey, and 19 in Hamilton; Fig. 2). Table 1 outlines the baseline characteristics of the study participants. The mean age was 69 years (standard deviation 11), with 54% female, 27% diabetic, 73% with a history of hypertension, 7% with prior myocardial infarction, and 9% with a prior stroke (Table 1). Follow-up was obtained at 6 months in 82% of participants (n = 46). There were no significant differences in baseline characteristics between those lost to follow-up and those completing follow-up at 6 months.
Figure 2.
Participant recruitment in Surrey, British Columbia, and Hamilton, Ontario, Canada.
Table 1.
Baseline characteristics of the study participants
| Characteristic | Overall | Surrey | Hamilton |
|---|---|---|---|
| Number of subjects | 56 | 37 | 19 |
| Age, y (mean, SD) | 69.3 (10.5) | 73.6 (8.38) | 61.0 (9.25) |
| Women | 30 (53.6) | 19 (51.4) | 11 (57.9) |
| Education | |||
| None/primary/unknown | 7 (12.5) | 2 (5.4) | 5 (26.3) |
| Secondary/high school | 24 (42.9) | 18 (48.6) | 6 (31.6) |
| Trade/college/university | 25 (44.6) | 17 (45.9) | 8 (42.1) |
| Past medical history (self-reported) | |||
| Current smoker | 8 (14.3) | 3 (8.1) | 5 (26.3) |
| Among women | 1 (3.3) | 0 (0.0) | 1 (9.1) |
| Among men | 7 (26.9) | 3 (16.7) | 4 (50.0) |
| Diabetes | 15 (26.8) | 7 (18.9) | 8 (42.1) |
| History of hypertension | 41 (73.2) | 27 (73.0) | 14 (73.7) |
| Atrial fibrillation | 7 (12.5) | 6 (16.2) | 1(5.3) |
| Stroke | 5 (8.9) | 3 (8.1) | 2 (10.5) |
| Myocardial infarction | 4 (7.1) | 1 (2.7) | 3 (15.8) |
| Angina | 5 (8.9) | 4 (10.8) | 1 (5.3) |
| Congestive heart failure | 1 (1.8) | 1 (2.7) | 0 |
| Liver disease | 1 (1.8) | 0 | 1 (5.3) |
| Kidney disease | 2 (3.6) | 2 (5.4) | 0 |
Values are n (%), unless otherwise indicated.
SD, standard deviation.
Compared to baseline, there was a significant improvement in the FRS 10-year risk estimate (30.6% vs 24.7%, P < 0.01), SBP (153.1 vs 136.7 mm Hg, P < 0.01), and proportion of participants with controlled SBP (5.6% vs 56.5%, P < 0.01). No significant changes in lipids, smoking status, or physical activity were noted. There was a significant increase in use of 2 or more antihypertensive medications (54.5% vs 68.6%, P = 0.01) and statins (40.7% vs 52.2%, P = 0.01) at 6 months compared to baseline (Table 2).
Table 2.
Change in outcomes between baseline and 6 months in Canadian cohort of HOPE 4
| Outcome | Baseline (n = 56) | 6 months (n = 46) | P∗ |
|---|---|---|---|
| FRS 10-year risk estimate, mean (SD) | 30.6 (18.1) | 24.7 (17.0) | < 0 .01 |
| Current smoker† | 8 (14.8) | 5 (10.9) | — |
| Physically active | 25 (46.3) | 28 (60.9) | 0.11 |
| Use of BP-lowering medications | 37 (68.5) | 35 (76.1) | 0.10 |
| Use of one BP-lowering medication | 17 (45.9) | 11 (31.4) | 0.01 |
| Use of ≥ 2 BP-lowering medications | 20 (54.5) | 24 (68.6) | 0.01 |
| SBP, mm Hg, mean (SD) | 153.1 (12.1) | 136.7 (15.7) | < 0.01 |
| Controlled SBP, < 140 mm Hg | 3 (5.6) | 26 (56.5) | < 0.01 |
| Use of statins | 22 (40.7) | 24 (52.2) | 0.01 |
| Total cholesterol, mmol/L, mean (SD) | 4.8 (1.3) | 4.7 (1.1) | 0.10 |
| LDL, mmol/L, mean (SD) | 2.7 (1.1) | 2.7 (0.9) | 0.15 |
| HDL, (mmol/L), mean (SD) | 1.4 (0.5) | 1.4 (0.5) | 0.15 |
| Triglyceride, mmol/L, mean (SD) | 1.6 (0.7) | 1.6 (0.7) | 0.20 |
Values are n (%), unless otherwise indicated.
BP, blood pressure; FRS, Framingham risk score; HDL, high-density lipoprotein; HOPE, Heart Outcomes Prevention and Evaluation Canada pilot study; LDL. low-density lipoprotein; SBP, systolic blood pressure; SD, standard deviation.
Based on paired subjects only, who had both baseline and 6 months using paired t-test for continuous measures and McNemar's test for categorical measures.
There is no change in smoking status among 46 participants who had both baseline and 6-month follow-up measures. As a result, P is not estimable for this exposure.
Discussion
This pilot study suggests that a contextually appropriate, community-based, multifaceted intervention package provided by CHWs can reduce CVD risk within a high-income country, primarily through improvements in blood pressure level.
The HOPE 4 Canada pilot study combined multiple strategies to achieve these results. First, we have demonstrated that with proper training and oversight, individuals with minimal to no experience in health promotion can learn to use a tablet-based decision support system to effectively identify, educate, and counsel participants about their CVD risk. Second, the HOPE 4 Canada pilot study intervention was informed by an extensive barrier-to-care analysis.25, 26, 27, 28 Third, our study used a community-based intervention in which participants were recruited from their homes or community-outreach events. This approach was intended to help overcome the traditionally low detection of hypertension in community settings. Fourth, the HOPE 4 Canada intervention involved task sharing among CHWs and physicians, as recommended by the World Health Organization.32,33 This strategy addresses health system barriers relating to both physician shortages and the time limitations of health care providers for education and counseling. Fifth, this study overcame medication-related barriers to the community management of CVD risk. The HOPE 4 strategy included recommendations to primary care providers (via participants) that support the rapid and simplified initiation of combinations of low doses of antihypertensive agents, an approach endorsed by several guidelines.34, 35, 36, 37 Statins were recommended to all patients, as the evidence supports their use in individuals with hypertension, regardless of lipid concentrations.38, 39, 40, 41, 42 Finally, the HOPE 4 intervention actively encouraged the involvement of participants’ families and/or friends as treatment supporters of the management of their CVD risk. This strategy has been shown to be effective at improving medication adherence and even mortality in other chronic conditions.43 Adaptation of this health system intervention package to a high-income country shows promise per the results of this pilot study.
The growing global burden of poorly managed hypertension and CVD strongly indicates the need for a markedly different approach to controlling CVD risk. Task sharing with non-physician health workers has been demonstrated to be effective in low- and middle-income countries. A recent systematic review of task sharing with non-physician health workers for the management of BP reported reductions in SBP by a mean of 4.8 mm Hg (95% confidence interval 3.6-6.1).19 Although the majority of non-physician health workers in this review were nurses (30 of 63), 30% were CHWs, similar to those in the HOPE 4 Canada pilot study. The recently published international HOPE 4 international RCT demonstrated that a comprehensive model of care led by CHWs substantially improved BP control and CVD risk.44 This open, community-based, cluster RCT involved 1371 individuals with new or poorly controlled hypertension, from 30 communities in Colombia and Malaysia. There was an absolute 11.5 mm Hg greater reduction in SBP, and a 0.4 mmol/L greater reduction in LDL with the intervention group (both P < 0.0001). Change in blood pressure control status (<140 mm Hg) was 69% in the intervention group vs 30% in the control group (P < 0.0001). The HOPE 4 international RCT achieved a much greater reduction in hypertension than that observed in the systematic review, suggesting that our protocol is particularly effective. The World Health Organization’s Heart Failure Etiology and Analysis Research Team (HEART) technical package employs a similar training curriculum for non-physician health workers and supports task sharing as a means for community-based CVD risk management.29 In further support of the HOPE 4 approach, the PolyIran RCT demonstrated that an intervention comprised of community screening with CHWs and the use of a single polypill (combination antihypertensives with a statin) resulted in significant reductions in cardiovascular events as compared to usual care.45
Our current Canadian pilot study expands on these data to explore the feasibility of the intervention package, including task sharing, in a high-income country. Three RCTs also support components of the HOPE 4 health system interventions in high-income countries. Muñoz et al. demonstrated the benefits of a polypill (combination antihypertensives with a statin) to reduce SBP and LDL, compared to usual care in a high-income country, in a lower-income population.46A paramedic-led, community-based health promotion program significantly lowered the number of ambulance calls, increased the number of quality-adjusted life years and ability to perform usual activities, and lowered SBP, among older adults living in subsidized housing within a high-income country.47 Finally, a cluster RCT in a high-income country, involving volunteer-run cardiovascular risk assessment and education sessions held in community-based pharmacies, demonstrated a significant reduction in cardiovascular morbidity.48 Although health care systems differ among countries with different income levels, there are substantial gaps in all countries that the components of the HOPE 4 intervention can help address.
Limitations
Although the HOPE 4 Canada pilot study demonstrated a significant reduction in the FRS 10-year risk estimate and improved BP control, this was a small pre–post pilot study, focusing primarily on the feasibility of implementing the intervention package within 2 communities in a high-income country. Furthermore, there were no changes in LDL or health behaviours. There was no control group, and our results could be influenced by regression to the mean.
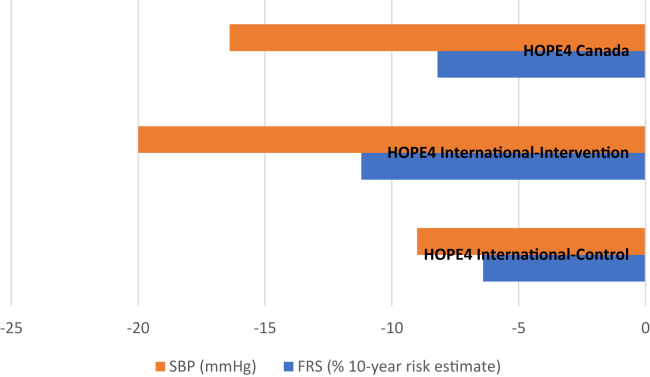
However, our results in the HOPE 4 Canada pilot study were similar to the differences observed in the international HOPE 4 RCT, which was well-powered, had a randomized control group, and demonstrated a similar level of benefit with a similar intervention.44 The absolute reductions in FRS and SBP in this Canadian cohort fall between the reductions noted in the intervention and control groups of the international HOPE 4 study (Fig. 3). This comparison highlights the power of community screening and increased participant awareness of personal CVD risk. This knowledge likely drove the observed improvements in both the Canadian cohort and the control group in the international HOPE 4 study.
Figure 3.
Comparison of absolute reductions in systolic blood pressure (SBP) and Framingham Risk Score (FRS) 10-year risk estimate between the intervention and control groups of the international Heart Outcomes Prevention and Evaluation 4 (HOPE 4) study and the HOPE 4 Canada pilot study.
The HOPE 4 Canada pilot study had plans to expand to multiple communities within BC using the firefighter model. Due to changing municipal needs, fire services are re-examining their emergency responder roles and expanding their community engagement.49 With the decline in traditional firefighting work, owing to improved safety practices and building technologies, fire services have the potential to address a variety of health and safety issues, including CVD risk reduction. Furthermore, established door-to-door firefighter community outreach programs offer opportunistic screening for CVD risk. Unfortunately, due to the opioid crisis in Western Canada, and related competing priorities, the fire services could not continue their focus on CVD risk reduction in Surrey, BC.50 Task sharing with firefighters as CHWs was demonstrated to be feasible, but sustainability of this model in a high-income setting proved to be the primary challenge facing the HOPE 4 Canada pilot study. Firefighters, paramedics, community pharmacists, and trained volunteers all offer promise in community-based CVD risk reduction, but there is a need to further evaluate their potential roles within existing health care prevention models to ensure sustainability and optimal impact.19,47,48
Conclusions
Improvements in individual CVD risk factors from baseline to 6-month follow-up in this health system strategy pilot study were each modest. However, collectively, the impact led to a significant reduction in the FRS 10-year risk estimate, which translates into a 20% reduction in CVD risk. These results are consistent with those of the larger HOPE 4 international cluster RCT, suggesting that the HOPE 4 model of community-based intervention involving CHWs may be applicable to high-income countries. A comprehensive approach to healthcare delivery using a community-based intervention with CHWs, and supported by mobile-health technologies, has the potential to significantly reduce CVD risk in high-income countries, but further evaluation is warranted.
Acknowledgements
The authors acknowledge the important contributions of the late Denise Brooks, formerly Executive Director, Urban Core Community Health Centre, Hamilton, Ontario, Canada.
Funding Sources
This work was supported by (i) the Canadian Institutes of Health Research (CIHR), Grand Challenges Canada (GCC), as part of the Global Alliance for Chronic Disease program (GACD; CIHR grant numbers: 120389 and 133733; GCC grant numbers: 0069-04 and 0070-04); (ii) CIHR’s Strategy for Patient Oriented Research (SPOR), through the Ontario SPOR Support Unit, as well as the Ontario Ministry of Health and Long-Term Care; (iii) an unrestricted grant from Boehringer Ingelheim; (iv) the Department of Management of Non-Communicable Diseases, World Health Organization; and (v) the Population Health Research Institute.
No official support or endorsement of this article by the GACD hypertension program, the World Health Organization, or federal, provincial, or regional governments of participating countries is intended or should be inferred.
Disclosures
J.D.S., T.M., P.L., H.M., S.I., and S.Y. from the Population Health Research Institute, report that their institution received grants from the Canadian Institutes of Health Research, the Ontario Ministry of Health and Long-Term Care, Boehringer Ingelheim, and from the Department of Management of Non-Communicable Disease, World Health Organization, Geneva Switzerland, for the conduct of the study. M.M., from the London School of Hygiene and Tropical Medicine, reports that that institution received a grant from the Canadian Institutes of Health Research. The other authors have no conflicts of interest to disclose.
Footnotes
Ethics Statement: All screened participants provided written consent, and all enrolled participants provided full informed written consent. The study was approved by the Hamilton Integrated Research Ethics Board (#13-437) and the Simon Fraser University Research Ethics Board (#H15-01233).
See page 273 for disclosure information.
To access the supplementary material accompanying this article, visit CJC Open at https://www.cjcopen.ca/ and at https://doi.org/10.1016/j.cjco.2020.10.006.
Supplementary Material
References
- 1.Statistics Canada Ten leading causes of death by selected age groups, by sex, Canada—all ages. https://www150.statcan.gc.ca/n1/pub/84-215-x/2012001/tbl/t001-eng.htm Available at:
- 2.World Health Organization (WHO) World Health Organization; Geneva: 2011. Global Status Report on Non-Communicable Diseases 2010. [Google Scholar]
- 3.Lloyd-Jones D.M., Leip E.P., Larson M.G. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 4.Roth G.A., Johnson C., Abajobir A. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70:1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yusuf S., Islam S., Chow C.K. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. 2011;378:1231–1243. doi: 10.1016/S0140-6736(11)61215-4. [DOI] [PubMed] [Google Scholar]
- 6.Chow E., Iqbal A., Bernjak A., Ajjan R., Heller S.R. Effect of hypoglycaemia on thrombosis and inflammation in patients with type 2 diabetes. Lancet. 2014;383:35. [Google Scholar]
- 7.Neal B., MacMahon S., Chapman N. Blood pressure lowering treatment trialists collaboration. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Lancet. 2000;356:1955–1964. doi: 10.1016/s0140-6736(00)03307-9. [DOI] [PubMed] [Google Scholar]
- 8.Clara K., Chow K.K.T., Rangarajan S. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–968. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 9.Kearney P.M., Whelton M., Reynolds K., Whelton P.K., He J. Worldwide prevalence of hypertension: a systematic review. J Hypertens. 2004;22:11–19. doi: 10.1097/00004872-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Lee D.S., Chiu M., Manuel D.G. Trends in risk factors for cardiovascular disease in Canada: temporal, socio-demographic and geographic factors. CMAJ. 2009;181:55–66. doi: 10.1503/cmaj.081629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Austin P.C., Tu J.V., Ko D.T., Alter D.A. Use of evidence-based therapies after discharge among elderly patients with acute myocardial infarction. CMAJ. 2008;179:895–900. doi: 10.1503/cmaj.071481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eagle K.A., Nallamothu B.K., Mehta R.H. Trends in acute reperfusion therapy for ST-segment elevation myocardial infarction from 1999 to 2006: we are getting better but we have got a long way to go. Eur Heart J. 2008;29:609–617. doi: 10.1093/eurheartj/ehn069. [DOI] [PubMed] [Google Scholar]
- 13.Ong K.L., Cheung B.M., Wong L.Y. Prevalence, treatment, and control of diagnosed diabetes in the U.S. National Health and Nutrition Examination Survey 1999–2004. Ann Epidemiol. 2008;18:222–229. doi: 10.1016/j.annepidem.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 14.Hobbs F.D., Jukema J.W., Da Silva P.M., McCormack T., Catapano A.L. Barriers to cardiovascular disease risk scoring and primary prevention in Europe. QJM. 2010;103:727–739. doi: 10.1093/qjmed/hcq122. [DOI] [PubMed] [Google Scholar]
- 15.Huffman M.D., van Geertruyden P.H. Does low pre-test probability of coronary artery disease reflect overuse of stress testing? JACC Cardiovasc Imaging. 2011;4:1143–1144. doi: 10.1016/j.jcmg.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Nieuwlaat R., Schwalm J.D., Khatib R., Yusuf S. Why are we failing to implement effective therapies in cardiovascular disease. Eur Heart J. 2013;34:1262–1269. doi: 10.1093/eurheartj/ehs481. [DOI] [PubMed] [Google Scholar]
- 17.Bagnall A.J., Yan A.T., Yan R.T. Optimal medical therapy for non-ST-segment–elevation acute coronary syndromes: exploring why physicians do not prescribe evidence-based treatment and why patients discontinue medications after discharge. Circ Cardiovasc Qual Outcomes. 2010;3:530. doi: 10.1161/CIRCOUTCOMES.109.919415. [DOI] [PubMed] [Google Scholar]
- 18.McAlister F.A., Campbell N.R.C., Zarnke K., Levine M., Graham I.D. The management of hypertension in Canada: a review of current guidelines, their shortcomings and implications for the future. CMAJ. 2001;164:517–522. [PMC free article] [PubMed] [Google Scholar]
- 19.Anand T.N., Joseph L.M., Geetha A.V., Prabhakaran D., Jeemon P. Task sharing with non-physician health-care workers for management of blood pressure in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Glob Health. 2019;7:e761–e771. doi: 10.1016/S2214-109X(19)30077-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Statistics Canada Census Profile, 2016 Census. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm?Lang = E&Geo1 = CSD&Code1 = 5915004&Geo2 = PR&Code2 = 59&SearchText = Surrey&SearchType = Begins&SearchPR = 01&B1 = All&GeoLevel = PR&GeoCode = 5915004&TABID = 1&type = 0 Available at:
- 21.Chronic diseases registries, BC Minitry of Health 2001-2015. http://communityhealth.phsa.ca/HealthProfiles/HealthReportHealthStatusAndChronicDisease/Abbotsford#ChronicDiseaseHeader Available at:
- 22.Social Planning and Research Council of Hamilton Hamilton’s Social Landscape Bulletin: Poverty Among Hamilton’s Taxfilers. http://www.sprc.hamilton.on.ca/wp-content/uploads/2017/04/SPRC-HSL-Bulletin-14-Poverty-of-taxfilers-April-2017.pdf Available at:
- 23.Hamilton Niagara Haldimand Brant LHIN Profile of Chronic Conditions in the Hamilton Niagara Haldimand Brant LHIN. http://www.hnhblhin.on.ca/∼/media/sites/hnhb/ uploadedfiles/Public_Community/CDPM/HNHB%20LHIN%20Chronic%20Conditions%20Profile%20Oct%205,%202008(1).pdf Available at:
- 24.Schwalm J.R., McCready T., Lamelas P. Rationale and design of a cluster randomized trial of a multifaceted intervention in people with hypertension: The Heart Outcomes Prevention and Evaluation 4 (HOPE 4) Study. Am Heart J. 2018;203:57–66. doi: 10.1016/j.ahj.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 25.Maimaris W., Paty J., Perel P. The influence of health systems on hypertension awareness, treatment, and control: a systematic literature review. PLoS Med. 2013;10 doi: 10.1371/journal.pmed.1001490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khatib R., Schwalm J.D., Yusuf S. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta-analysis of qualitative and quantitative studies. PLoS One. 2014;9 doi: 10.1371/journal.pone.0084238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Legido-Quigley H., Lopez P.A.C., Balabanova D. Patients’ knowledge, attitudes, behaviour and health care experiences on the prevention, detection, management and control of hypertension in Colombia: a qualitative study. PLoS One. 2015;10 doi: 10.1371/journal.pone.0122112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Risso-Gill I., Balabanova D., Majid F. Understanding the modifiable health systems barriers to hypertension management in Malaysia: a multi-method health systems appraisal approach. BMC Health Serv Res. 2015;15:254. doi: 10.1186/s12913-015-0916-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khan M., Lamelas P., Musa H. Development, testing, and implementation of a training curriculum for nonphysician health workers to reduce cardiovascular disease. Glob Heart. 2018;13:92–100. doi: 10.1016/j.gheart.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yusuf S., Phil D., Lonn E. Blood pressure and cholesterol lowering in persons without cardiovascular disease. N Engl J Med. 2016;374:2032–2043. doi: 10.1056/NEJMoa1600177. [DOI] [PubMed] [Google Scholar]
- 31.D’Agostino R.B., Sr., Vasan R.S., Pencina M.J. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 32.Abegunde D.O., Shengelia B., Luyten A. Can non-physician health-care workers assess and manage cardiovascular risk in primary care? Bull World Health Organ. 2007;85:432–440. doi: 10.2471/BLT.06.032177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization (WHO) WHO; Geneva: 2002. WHO CVD-risk management package for low- and medium-resource settings. [Google Scholar]
- 34.López-Jaramillo P., Barbosa E., Molina D.I. Latin American consensus on management of hypertension in the patient with diabetes and the metabolic syndrome. J Hypertens. 2019;37:1126–1147. doi: 10.1097/HJH.0000000000002072. [DOI] [PubMed] [Google Scholar]
- 35.Mancia G., De Baker G., Dominiczak A. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2007;28:1462–1536. doi: 10.1093/eurheartj/ehm236. [DOI] [PubMed] [Google Scholar]
- 36.Chobanian A.V., Bakris G.L., Black H.R. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. J Hypertens. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 37.Malaysian Society of Hypertension . 5th ed. Malaysian Society of Hypertension; Malaysia: 2018. Working Group on Hypertension. Clinical Practice Guidelines—Management of Hypertension. [Google Scholar]
- 38.Sever P.S., Dahlöf B., Poulter N.R. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial—Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet. 2003;361:1149–1158. doi: 10.1016/S0140-6736(03)12948-0. [DOI] [PubMed] [Google Scholar]
- 39.Yusuf S., Lonn E., Pais P. Blood-pressure and cholesterol lowering in persons without cardiovascular disease. N Engl J Med. 2016;374:2032–2043. doi: 10.1056/NEJMoa1600177. [DOI] [PubMed] [Google Scholar]
- 40.Lonn E.M., Bosch J., Lopez-Jaramillo P. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374:2009–2020. doi: 10.1056/NEJMoa1600175. [DOI] [PubMed] [Google Scholar]
- 41.Yusuf S., Bosch J., Dagenais G. Cholesterol lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374:2021–2031. doi: 10.1056/NEJMoa1600176. [DOI] [PubMed] [Google Scholar]
- 42.Grundy S.M., Stone N.J., Bailey A.L. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. Circulation. 2019;139:e1082–e1143. doi: 10.1161/CIR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nachega J.B., Chaisson R.E., Goliath R. Randomized controlled trial of trained patient-nominated treatment supporters providing partial directly observed antiretroviral therapy. AIDS. 2010;24:1273–1280. doi: 10.1097/QAD.0b013e328339e20e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schwalm J.D., McCready T., Lopez-Jaramillo P. A community-based comprehensive intervention to reduce cardiovascuar risk in hypertension (HOPE 4): a cluster-randomised controlled trial. Lancet. 2019;394:1231–1242. doi: 10.1016/S0140-6736(19)31949-X. [DOI] [PubMed] [Google Scholar]
- 45.Roshandel G., Khoshnia M., Poustchi H. Effectiveness of Polypill for primary and secondary prevention of cardiovascular diseases: a pragmatic cluster randomized controlled trial. Lancet. 2019;394:672–683. doi: 10.1016/S0140-6736(19)31791-X. [DOI] [PubMed] [Google Scholar]
- 46.Muñoz D., Uzoije P., Reynolds C. Polypill for cardiovascular disease prevention in an underserved population. Engl J Med. 2019;381:1114–1123. doi: 10.1056/NEJMoa1815359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Agarwal G., Angeles R., Pirrie M. Evaluation of a community paramedicine health promotion and lifestyle risk assessment program for older adults who live in social housing: a cluster randomized trial. CMAJ. 2018;190:638–647. doi: 10.1503/cmaj.170740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kaczorowski J., Chambers L.W., Dolovich L. Improving cardiovascular health at population level: 39 community cluster randomised trial of Cardiovascular Health Awareness Program (CHAP) BMJ. 2011;342:442. doi: 10.1136/bmj.d442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Garis L., Schwalm J.D. Doing more: expanding the role of the fire service to create healthier and safer communities. Simcoe: Canadian Firefighter. 2018;41:10–12. [Google Scholar]
- 50.Fischer B., Vojtila L., Rehm J. The ‘fentanyl epidemic’ in Canada—some cautionary observations focusing on opioid-related mortality. Prev Med. 2017;107:109–113. doi: 10.1016/j.ypmed.2017.11.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.