Abstract
Objective
To conduct a scoping review of mobile health (mHealth) application (app) interventions to support needs of adults living with the effects of stroke reported in the literature.
Data Sources
PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Scopus were systematically searched for peer-reviewed publications. Articles were published between January 2007 and September 2020 and met predefined inclusion and exclusion criteria.
Study Selection
Articles included were written in English language, involved adults older than 18 years, and described an mHealth app specifically tested and/or developed as an intervention for someone with stroke to be used remotely and/or independently without constant provider supervision or assistance. Articles were excluded if they focused on acute management of stroke only, focused on primary prevention, were animal studies, were not an app for smartphone or tablet, and did not describe an empirical study.
Data Extraction
Two researchers independently screened titles and abstracts for inclusion. The full-text articles were then reviewed for eligibility by the research team. Data were extracted and verified by a third reviewer.
Data Synthesis
The search yielded 2123 studies and 49 were included for data extraction. The findings reveal that a global surge of studies on mHealth apps for people with stroke have emerged within the past 2 years. Most studies were developed for persons with stroke in the United States and the primary content foci included upper extremity function (31.5%); lower extremity function (5.3%); general exercise, physical activity, and/or functional mobility (23.7%); trunk control (5.3%); medical management and secondary prevention (26.3%); language and speech skills (20.5%); cognitive skills (7.9%); general disability and activities of daily living (5.3%); and home safety (2.6%). Of the included studies, a majority were preliminary in nature, with 36.7% being categorized as pilot or feasibility trials and 24.4% discussing initial design, development, and/or refinement.
Conclusions
Results from this study reveal that the number of apps specifically developed for people with stroke and described in the scientific literature are growing exponentially. The apps have widely varied content to meet the needs of persons with stroke; however, the studies are generally preliminary in nature, focusing on development, usability, and initial pilot testing. This review highlights the need for additional research and development of mHealth apps targeted for adults with stroke. Development should consider the various and complex needs of people living with the effects of chronic stroke, while large-scale trials are needed to build on the existing evidence.
Keywords: Delivery of health care, Rehabilitation, Smartphone, Stroke, Stroke rehabilitation, Telemedicine, Telerehabilitation
List of abbreviations: ADL, activities of daily living; app, application; mHealth, mobile health
Stroke is a chronic health condition, and survivors have persistent unmet needs after hospitalization.1 Poststroke functioning and disability are dynamic, complex, and influenced by impairments and contextual factors.2 People living with the effects of stroke may have challenges managing their day-to-day lives, and oftentimes this burden falls on both the survivors and their families and care partners.3 Furthermore, people living with the effects of stroke are at risk for health-related decline, hospital readmission, and an overall reduction in quality of life.4,5
Adults with stroke describe feeling abandoned and marginalized by health care services and report lacking knowledge and skills to meet their long-term needs.5 In fact, nearly 40% of people with stroke do not receive services needed to support long-term needs.6 Some people with stroke are discharged home immediately after stabilization in the acute hospital, while others receive postacute care services such as inpatient rehabilitation prior to transitioning to life in the community. Nonetheless, it is widely agreed on that services are needed that extend beyond current health care delivery systems to meet population needs.4
Mobile devices, such as smartphones and tablets, are becoming increasingly embedded in peoples’ everyday lives.7 mHealth applications (apps) have the potential to transform health care delivery and may be particularly useful in the effective management of chronic disease and comorbidities. Although they are not without limitations, mHealth apps are becoming increasingly popular. Adults with stroke are frequently downloading and using apps to support everyday life tasks7; however, a residual knowledge gap exists about the role of mHealth apps supporting self-management of health and function among survivors. Therefore, the purpose of this study is to summarize current literature about interventions delivered via mHealth apps for use by persons living with the effects of stroke. Given the wide adoption and popularity of smartphones and tablets, it is anticipated that these findings will guide future research and development to optimize improved long-term health and functional outcomes.
Methods
Design
A scoping review was conducted by systematically searching the literature for eligible studies, extracting relevant data, and qualitatively summarizing the results. Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews was used to guide this current review.8 A review protocol does not exist for this study.
Search strategy and study inclusion
The lead author and research librarian developed a systematic search strategy that was conducted in October 2018 and September 2020. The search was limited to studies written in English language and in adults older than 18 years. It was conducted within PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Scopus and was composed of Medical Subject Headings of the National Library of Medicine and natural language terms. The search terms included stroke, cerebral vascular accident, recovery, rehabilitation, smartphone, mobile applications, mHealth, telerehabilitation, and telemedicine.
The search included articles beginning in 2007, which was when smartphones and apps began to be generally available. All article titles and abstracts were uploaded to Rayyan web and mobile appa for data management. Two authors independently screened titles and abstracts for inclusion and exclusion. A dichotomous “no” or “maybe” scoring system was used for initial article exclusion. When disagreement on article inclusion occurred, a different author would review to make a final decision on inclusion for full-text review. The authors engaged in hand searching, which involved probing reference lists of review articles, included manuscripts, and first author names of included studies in Google Scholar. Articles included were written in English language, involved adults older than 18 years, and described an mHealth app specifically tested and/or developed as an intervention for someone with a stroke to be used remotely and/or independently without constant provider supervision or assistance. Articles were excluded if they (1) focused on acute management of stroke only (eg, alteplase administration), (2) focused on primary prevention, (3) were animal studies, (4) were not an app for smartphone or tablet, or (5) did not describe an empirical study. Review papers were excluded; however, reference lists were reviewed through hand searching.
Data extraction
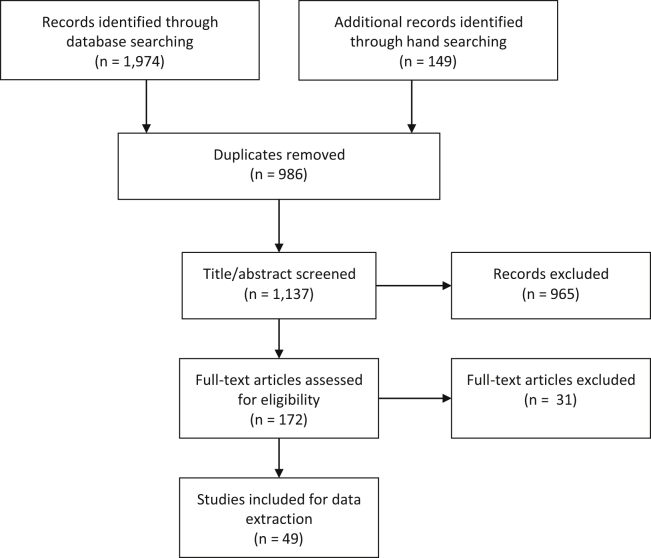
Once all of the publications that met inclusion criteria were identified, the researchers extracted and recorded relevant information that matched the aims of the study (i.e., study design, app name, content, quoted study aims, quoted author conclusions). Content foci categories were coded by the first, second, and third authors. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram (fig 1) illustrates the identification, inclusion, and exclusion of articles leading to the final selection of studies for data extraction.
Fig 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram depicting decision-making progress for study inclusion.
Results
A total of 2123 articles were retrieved from database and hand searching. After removing duplicates and screening for eligibility, 49 articles remained and underwent data extraction. Refer to table 1 for detailed information about included studies.
Table 1.
Included studies on mHealth apps for persons with stroke
| Author | Sample Size (Stroke) | Study Design | Country | App | Primary Content Focus | Reported Study Aim | Reported Author Conclusions |
|---|---|---|---|---|---|---|---|
| Lawson et al9 | N=6 | Mixed methods multiple case study | United States | ARMStrokes | Upper extremity function | To investigate the utility of a mobile app to improve motor control for survivors of stroke by examining changes in motor ability and participation. | Pre- and posttest data from 6 survivors of chronic stroke who used the app in different ways (ie, to measure active and passive motion, to track endurance) demonstrated improvements in accuracy of movements, fatigue, range of motion, and performance of daily activities. Statistically significant changes were not obtained by this pilot study. Further study on the efficacy of this technology is supported. |
| Lawson et al10 | N=10 | Pilot study | United States | ARMStrokes | Upper extremity function | To examine the usability and usefulness of the application. | Based on these pilot study results, the researchers plan to refine the way the phone can be secured to the affected limb, create automated calibration (eliminating the manual calibration process), and create new games and reminders that will help make the app more engaging. Plans also include expanding the application to other diagnostic groups and exploring the telerehabilitation implications. This research is ongoing and will advance to the use of an experimental design to truly determine the effectiveness of the app in improving upper limb recovery and function. |
| Guo et al11 | N=12∗ | Description of development (qualitative) | United States | ARMStrokes | Upper extremity function | To describe the app for use among survivors of stroke and elicit feedback from stakeholders for preliminary evaluation. | Focus groups involving survivors of stroke, caregivers, and therapists have been conducted to evaluate the system, and the feedback is highly positive. |
| Sarfo et al12 | N=20 | Prospective single-arm pre-post study | Ghana | 9zest Stroke App | Exercise/physical activity/functional mobility, upper extremity function, lower extremity function | To preliminarily assess the feasibility of outcomes of mobile technology-assisted physical therapy exercises for survivors of stroke in Ghana. | It is feasible to administer an mHealth delivered physical therapy intervention in SSA with high user satisfaction. Randomized trials to assess the efficacy and cost-effectiveness of this intervention are warranted. |
| Sarfo et al13 | N=60 | Two-arm cluster pilot RCT | Ghana | PINGS | Medical management/secondary prevention | To test the feasibility and preliminary signal of efficacy of an mHealth technology–enabled, nurse-led, multilevel integrated approach to improve blood pressure control among Ghanaian patients with stroke within 1 mo of symptom onset compared with standard of care. | It is feasible to conduct an mHealth-based, nurse-guided blood pressure control intervention among patients with recent stroke in sub-Saharan Africa. We observed a potential signal of efficacy with the intervention, which will need to be tested in a future large definitive study. |
| Sarfo et al14 | N=60 | Two-arm cluster pilot RCT | Ghana | PINGS | Medical management/secondary prevention | To assess whether an mHealth technology-enabled, nurse-guided intervention initiated among patients with stroke within 1 mo of symptom onset is effective in improving their blood pressure control. | This study demonstrated feasibility and signal of improvement in blood pressure control among survivors of stroke in a resource-limited setting via an mHealth intervention. Larger scale studies are warranted. |
| Nichols et al15 | N=16∗ | Qualitative | Ghana | PINGS | Medical management/secondary prevention | To explore postintervention perspectives and gather in-depth insight into the experiences of survivors of stroke and their caregivers after participation in a larger interventional arm of an mHealth blood pressure management study. The study also sought to assess the contextual and organizational facilitators and barriers encountered in the implementation of the intervention within an operational setting. | Four major themes emerged highlighting the ability to self-monitor, the use of technology as an interventional tool, training and support, and postintervention adherence. Overwhelming receptivity toward home blood pressure monitoring and the use of mHealth was noted. Feedback indicated benefits in having access to equipment and that message prompts facilitated adherence. Postintervention adherence declined after study intervention, indicating a need for increased exposure to facilitate long-term behavioral change, although participants conveyed a heightened awareness of the importance of blood pressure monitoring and lifestyle changes needed. |
| Siegel et al16 | N=3 | Case series | United States | PHA app | Medical management/secondary prevention | To examine patients with ischemic stroke who used the PHA app. The authors hypothesized that the PHA would improve postdischarge satisfaction and decrease rehospitalization. | Both patients who used the app were very satisfied with the PHA and their posthospital care coordination. This study had an enrollment rate of about 14% because of various factors, including limited access or use of necessary technology. Although limited by final patient sample size and early termination from funding, this study provides useful information about developing future mobile health apps for patients with acute stroke. |
| Choi et al17 | N=24 | Randomized double-blind controlled trial | South Korea | MoU-Rehab | Upper extremity function | To develop a mobile game-based upper extremity VR program for patients who have experienced stroke and to evaluate the feasibility and effectiveness of the program. | This mobile game-based VR rehabilitation program appears to be feasible and effective for promoting upper limb recovery after ischemic stroke. |
| Choi & Paik18 | N=24 | Quasi-randomized double-blind controlled trial | South Korea | MoU-Rehab | Upper extremity function | This study describes the development of a mobile game-based VR program and its use for patients who have experienced a stroke with upper limb dysfunction. | The findings from the study show that the mobile game-based VR program effectively promotes upper extremity recovery in patients with stroke. In addition, patients completed 2 wk of treatment using the program without adverse effects and were generally satisfied with the program. This mobile game-based VR upper extremity rehabilitation program can substitute for some parts of the conventional therapy that are delivered 1-on-1 by an occupational therapist. |
| Des Roches et al19 | N=46∗ | RCT | United States | Constant Therapy | Language/speech and cognitive skills | To examine the clinical effectiveness of using iPads to deliver personalized therapy to individuals with aphasia, to determine if a structured iPad-based therapy program that includes homework practice results in significant gains in overall communication and how individual severity profiles affect therapy outcomes. | Participants did not differ in the duration of the therapy. and both groups of participants showed improvement over time in the tasks used for therapy. However, experimental participants used the application more often and showed greater changes in accuracy and latency on the tasks than the control participants; experimental participants’ severity level at baseline as measured by standardized tests of language and cognitive skills were a factor in improvement on the tasks. Subgroups of task coimprovement appear to occur between different language tasks, between different cognitive tasks, and across both domains. Finally, experimental participants showed more significant and positive changes because of therapy in their standardized tests than control participants. These results provide preliminary evidence for the usefulness of a tablet-based platform to deliver tailored language and cognitive therapy to individuals with aphasia. |
| Godlove et al20 | N=3686 | Retrospective analysis | United States | Constant Therapy | Language/speech and cognitive skills | To examine if home users of the therapy were compliant in therapy and if this documented practice time was associated with improved outcomes similar to clinic patients who practiced under the guidance of a clinician. | Outcomes of treatment are similar for home users and clinic patients, indicating the potential usability of a home-based treatment program for rehabilitation for poststroke aphasia. |
| Kurland et al21 | N=21 | Before-and-after | United States | Personalized iBooks | Language/speech skills | To determine if a tablet-based home practice program with weekly telepractice support could enable long-term maintenance of recent treatment gains and foster new language gains in poststroke aphasia. |
Unsupervised home practice with weekly video teleconferencing support is effective. This study demonstrates that even individuals with chronic severe aphasia, including those with no prior smart device or even computer experience, can attain independent proficiency to continue practicing and improving their language skills beyond therapy discharge. This could represent a low-cost therapy option for individuals without insurance coverage and/or those for whom mobility is an obstacle to obtaining traditional aphasia therapy. |
| Kurland et al22 | N=8 | RCT | United States | iPractice | Language/speech skills | To investigate the effectiveness of an iPad-based HP program developed primarily by the first and second authors for maintaining and improving recent language treatment gains achieved by 8 survivors of stroke with chronic aphasia. | All participants maintained advances made on words trained during the intensive treatment and additionally were able to learn new words by practicing daily over a 6-mo period. The iPad and other tablet devices have great potential for personalized home practice to maintain and augment traditional aphasia rehabilitation. It appears that motivation to use the technology and adequate training are more important factors than age, aphasia type or severity, or prior experience with computers. |
| Mallet et al23 | N=30 | Survey | Canada | RecoverNow | Language/speech, upper extremity function, and cognitive skills | To gain a better understanding of patient experiences and recovery goals using mobile tablets after expanding to include fine motor and cognitive therapy. | Our results suggest that patients with stroke are interested in mobile tablet-based therapy in acute care. Patients in the acute setting prefer to focus on communication and hand therapies, are willing to begin within days of their stroke, and may require assistance with the tablets. |
| Pugliese et al24 | N=30 | Unblinded single-group prospective cohort | Canada | RecoverNow | Language/speech, upper extremity function, and cognitive skills | The study objective was to demonstrate the feasibility of RecoverNow, a tablet-based stroke recovery platform aimed at delivering speech and cognitive therapy. | Patients with acute stroke are interested in attempting tablet-based stroke rehabilitation and are easily recruited early post stroke. However, tablet-based therapy may be challenging because of patient-, device-, and system-related barriers. Reducing the frequency of common barriers will be essential to keeping patients engaged in tablet-based therapy. |
| Gerber et al25 | N=15∗ | Development and evaluation | Switzerland | BernAphasia App | Language/speech skills | The aim of this project was to develop an adaptive multimodal system that enables patients with aphasia to train at home using language-related tasks autonomously, allows therapists to remotely assign individualized tasks in an easy and time-efficient manner, and tracks the patient’s progress as well as creation of new individual exercises. | Based on the questionnaire scores, the system is well accepted and simple to use for patients and therapists. Furthermore, the new tablet computer–based app and the hierarchical language exercise structure allow patients with different types of aphasia to train with different doses and intensities independently at home. Thus, the novel system has potential for treatment of patients with aphasia as a supplement to face-to-face therapy. |
| Kringle et al26 | N=5 | Sequential descriptive case series | United States | iAdapts | Cognitive skills | To describe lessons learned through adaptation of a complex intervention—strategy training—for delivery via mHealth technology. | Strategy training can be adapted for delivery using mHealth technology, with careful consideration to methods for training participants on new technology and the intervention delivery. Future research should establish the efficacy and effectiveness of integrating mHealth in delivery of interventions that promote engagement in client-selected activities and community participation. |
| Bhattacharjya et al27 | N=4∗ | Usability study | United States | mRehab | Upper extremity function | To assess the usability and consistency of measurement of the mRehab system. | Usability ratings from older adults and individuals with stroke led us to modify the design of the 3-D printed items and improve the clarity of the mRehab app. The modified mRehab system was assessed for consistency of measurement and 6 ADL resulted in CV<10%. This is a commonly used CV goal for consistency. Two ADL ranged between 10% and 15% CV. Only 2 ADL demonstrated high CV. |
| Langan et al28 | N=16 | Single-subject experimental design with multiple baselines | United States | mRehab | Upper extremity function | To examine if people living with chronic stroke can use mRehab in their home to improve upper extremity function | Despite heterogeneity in participants’ use of mRehab, there were improvements in upper limb mobility. Smartphone-based portable technology can support home rehabilitation programs in chronic conditions such as stroke. The ability to record performance data from home rehabilitation offers new insights into the effect of home programs on outcomes. |
| Jang & Jang29 | N=21 | RCT | South Korea | Not reported | Upper extremity function | To investigate the effect of a finger training application program using a tablet PC in patients with chronic hemiparetic stroke. | We found that our application training was effective in terms of the motor function of the affected hand: Manual Muscle Test of the wrist and finger extensors, the Manual Function Test (subtest of manipulative activity), and the Purdue Pegboard Test. |
| Sureshkumar et al30 | N=30 | Mixed methods | India | Care for Stroke | General disability management or ADL | To identify operational issues encountered by study participants in the intervention and to evaluate the feasibility and acceptability of the intervention. | Evaluation indicated that the Care for Stroke intervention was feasible and acceptable in an Indian context. An assessment of effectiveness is now warranted. |
| Paul et al31 | N=23 | Nonrandomized controlled trial | United Kingdom | STARFISH | Exercise/physical activity/functional mobility | To evaluate the potential effectiveness of STARFISH in survivors of stroke. | Use of STARFISH has the potential to improve physical activity and health outcomes in people after stroke and longer term intervention trials are warranted. |
| Groussard et al32 | N=1∗ | Development (qualitative) | Canada | SAMI | General disability management or ADL | To design a mobile cognitive assistant that enhances the autonomy of people living with an acquired brain injury, based on their expressed needs, and to conduct a proof of concept to show that the cognitive assistant meets those needs. | The results demonstrate that the participants were able to participate actively in the conception of SAMI and to use it successfully. People with cognitive impairment showed a slight improvement in their life satisfaction. Because of the small number of participants, these promising results need to be confirmed by a larger-scale study. |
| Seo et al33 | N=48 | Prospective single-center, single-arm, open label clinical trial | South Korea | KUHMS | Medical management/secondary prevention | To test the feasibility of using a smartphone software application for the management of vascular risk factors in patients with stroke. | Many challenges must be overcome before mobile apps can be used for patients with stroke. Nevertheless, the app tested in this study induced a shift in the risk profiles in a favorable direction among the included patients with stroke. |
| Brandenburg et al34 | N=12 | Qualitative | Australia | CommFit | Language/speech skills | The aim of the study was to investigate the barriers and facilitators experienced by people with nonfluent aphasia using CommFit to measure talk time and to determine the ease of use of each step of using the app. |
The results of this study identified barriers to using mobile technology, many of which were not connected to the participants’ stroke-related impairments. It also identified several facilitators that should be capitalized on when using mobile technology with this population. Last, results indicated that the Bluetooth headset was not a highly usable component of the CommFitTM system, especially for older users. This will be addressed in future research on the app. |
| Brandenburg et al35 | N=12∗ | Exploratory | Australia | CommFit | Language/speech skills | To explore the use of talk time, as measured by the CommFit app, as an indicator of participation for people with aphasia. |
This study provides some preliminary data on talk time in people with aphasia, suggesting that talk time is an indicator of participation. |
| Kizony et al36 | N=20∗ | Feasibility trial | Israel | Apps for dexterity (Dexteria, Scribble Kid, Peg Light, Tap-It!, bowling game) | Upper extremity function | To assess the feasibility of using tablet apps to increase dexterity and to characterize the user’s experience and performance with different apps. | Performance of tablet app-based hand activities was affected by impaired hand dexterity in older participants without a disability and in participants with stroke. Tablet apps may potentially provide a way to facilitate self-training of repetitive, task-oriented, isolated finger and hand dexterity after stroke. |
| Grau-Pellicer et al37 | N=41 | Pilot randomized unblended trial | Spain | Fitlab Training and Fitlab Test | Exercise/physical activity/functional mobility | To investigate the effectiveness of an mHealth app in improving levels of physical activity. | The results suggest that mHealth technology provides a novel way to promote adherence to home exercise programs post stroke. However, frequent support and guidance of caregiver is required to ensure the use of mobile devices. |
| Garcia et al38 | N=8 | Describe design/development and pilot single-blind randomized trial | Philippines | Theraphasia | Language/speech skills | To design and develop a speech therapy game application, as an additional neurorehabilitation modality for patients with aphasia and to assess its applicability as an adjunct to the traditional neuromuscular rehabilitation through a pilot study. | The comparison of before and after treatment revealed an improvement in all of the QAB subtests: level of consciousness, connected speech, word comprehension, sentence comprehension, picture naming, repetition, reading aloud, and motor speech. This suggests the development of this speech therapy game and the preliminary findings from the pilot study may be an effective neurorehabilitation instrument for therapy of patients with aphasia. |
| Requena et al39 | N=159 | 2-Arm open-label nonrandomized trial | Spain | FARMALARM | Medical management/secondary prevention and exercise/physical activity/functional mobility | To validate the use of FARMALARM, an app for smartphones, in vascular risk factor control as a tool for secondary prevention of stroke. | In patients with stroke discharged home, the use of mobile apps to monitor medication compliance and increase stroke awareness is feasible and seems to improve the control of vascular risk factors. |
| Kang et al40 | N=63 | Single-blind (assessor) RCT | Taiwan | SHEMA | Medical management/secondary prevention | To develop a stroke health education mobile app and examine its effectiveness on improvement of knowledge of stroke risk factors and health-related quality of life. | Both the SHEMA intervention and traditional stroke health education can improve patients’ knowledge of stroke risk factors, but the SHEMA was not superior to traditional stroke health education. |
| Vloothius et al41 | N=7∗ | Qualitative | Netherlands | CARE4STROKE | Exercise/physical activity/functional mobility | To explore how people living with stroke and caregivers managed exercises together. | Different role dynamics are at play in caregiver-mediated exercises, and it is important to be aware of possible effects on the strain of patient or caregiver. These caregiver-mediated exercises were found to enhance individualization of the treatment plan and preparation for discharge home. |
| Vloothius et al42 | N=66∗ | Observer-blinded multicenter RCT | Netherlands | CARE4STROKE | Exercise/physical activity/functional mobility | Hypothesized that CARE4STROKE program would lead to improved self-reported mobility, reduced length of stay without increasing caregiver burden, and improved psychosocial function and mobility-related functional outcomes (eg, balance, lower limb function). | This proof of concept trial did not find significant effects on both primary outcomes mobility and LOS as well as the secondary functional outcomes. Treatment contrast in terms of total exercise time may have been insufficient to achieve these effects. However, caregiver-mediated exercises showed a favorable effect on secondary outcome measures of mood for both patient and caregiver. |
| Hughes et al43 | N=6∗ | Usability study | Ethiopia | outREACH | Upper extremity function and medical management/secondary prevention | To conduct usability testing of the current outREACH telerehabilitation system and to determine the acceptance of the mobile app and its features in Ethiopian rehabilitation clinicians, patients with stroke, and patient caregivers. | Overall, the results of usability testing were promising, and all participants rated the app as easy to use and a useful tool to supplement in-clinic rehabilitation of poststroke upper limb dysfunction. The majority of respondents could successfully navigate through the system modules, found the aesthetics to be visually appealing, and expressed a strong desire to use the system. This innovative care strategy has the potential to change how stroke rehabilitation is delivered in countries such as Ethiopia where a large proportion of the population lives in rural areas and experience a deficit of experienced health professionals. |
| Hughes et al44 | N=11 | Usability study (mixed methods) | United States | outREACH | Upper extremity function and medical management/secondary prevention | To conduct (1) usability testing of a medium fidelity prototype and (2) semistructured interviews to solicit responses about app usefulness, features, and acceptance. | Two main usability issues in round 1 were identified with the scheduler module and the similarities between the Home screen and the My Care Plan screen. After applying modifications for the second iteration, there was a significant increase in the average usability score (43%-88%) and a reduction in both the number of errors and the time taken to complete each task. The results of the present study will be integrated into the development, integration, and evaluation of the outREACH system that supports stroke telerehabilitation in underserved populations. |
| Ballard et al45 | N=5 | Feasibility trial | Australia | The Word Trainer | Language/speech skills | To evaluate an iPad-based speech therapy app that uses ASR software to provide feedback on speech accuracy to determine the ASR’s accuracy against human judgment and whether participants’ speech improved with this ASR-based feedback. | For these participants with apraxia of speech plus aphasia due to stroke, satisfactory gains were made in word production accuracy with an app-based therapy program providing ASR-based feedback on accuracy. Findings support further testing of this ASR-based approach as a supplement to clinician-run sessions to assist clients with similar profiles in achieving higher amount and intensity of practice as well as empowering them to manage their own therapy program. |
| Costa et al46 | N=55 | Observational with repeated measures | Brazil | Google Fit, Health, STEPZ, Pacer, and Fitbit Ultra | Exercise/physical activity/functional mobility | To (1) determine validity of mHealth devices, (2) determine test-retest reliability of mHealth devices, and (3) compare whether the number of steps in individuals with chronic stroke is affected by where the device is positioned. | mHealth devices (Pacer [iPhone], Fitbit Ultra, Google Fit, and Pacer [Android]) are valid and reliable for step counting in survivors of chronic stroke. Body location (paretic or nonparetic side) does not affect validity or reliability of the step count metric. |
| Simpson et al47 | N=10 | Single-group pre-post feasibility trial | Australia | Not reported | Exercise/physical activity/functional mobility | To (1) investigate feasibility of delivering a 4-wk remotely prescribed functional exercise program using a tablet, app, and sensory system and (2) provide an estimate of the effect of the intervention outcomes. | It was feasible and safe to prescribe and monitor exercises using an app and sensor-based system. A definitive trial will determine whether such technology could facilitate greater exercise participation after stroke. |
| Kamal et al48 | N=155∗ | Randomized controlled, outcome assessor-blinded, parallel group single-center superiority trial | Pakistan | Movies4Stroke | Medical management/secondary prevention | To evaluate the effectiveness and safety of locally designed 5-min movies. | The Movies4Stroke trial failed to achieve its primary specified outcome. However, secondary outcomes that directly related to survival skills of survivors of stroke demonstrated the effectiveness of the video-based intervention on improving stroke-related mortality and survival without disability. |
| Chae et al49 | N=23 | Prospective comparative trial | South Korea | HBR | Upper extremity function | To (1) develop an HBR to recognize and record type and frequency of rehabilitation exercises using a smartwatch and smartphone app and (2) evaluate the efficacy of the HBR system. | This study found that a home care system using a commercial smartwatch and machine learning model can facilitate participation in home training and improve the functional score of the Wolf Motor Function Test and shoulder range of motion of flexion and internal rotation in the treatment of patients with chronic stroke. This strategy can possibly be a cost-effective tool for the home care treatment of survivors of stroke in the future. |
| LaPiana et al50 | N=5 | Acceptability case study | United States | Not reported | Upper extremity function | To assess the acceptability of a smartphone-based augmented reality game as a means of delivering stroke rehabilitation for patients with upper limb motor function loss. | Based on the questionnaire scores, the patients with upper limb motor deficits after stroke who participated in our case study found our augmented reality game motivating, comfortable, engaging, and tolerable. Improvements in augmented reality technology motivated by this case study may one day allow patients to work with improved versions of this therapy independently in their own home. We therefore anticipate that smartphone-based augmented reality gaming systems may eventually provide useful postdischarge self-treatment as a supplement to professional therapy for patients with upper limb deficiencies from stroke. |
| Chung et al51 | N=56 | Randomized, controlled, assessor-blinded clinical trial | China | Not reported | Exercise/physical activity/functional mobility, upper extremity function, lower extremity function, trunk control | To compare the effectiveness of mobile video-guided home exercise program and standard paper-based home exercise program. | The use of mobile video-guided home exercise program was superior to standard paper-based home exercise program in exercise adherence and self-efficacy for exercise scale mobility gain but not basic ADL gain for patients recovering from stroke. |
| Ifejika et al52 | N=36 | Phase 1 pilot prospective RCT with open blinded endpoint study | United States | Swipe out Stroke | Medical management/secondary prevention | To determine the feasibility and preliminary treatment effects of a smartphone-based weight loss intervention vs food journals to monitor dietary patterns in minority patients with stroke. | In a population of obese minority survivors of stroke, the use of a smartphone did not lead to a significant difference in weight change compared with keeping a food journal. The presence of baseline depression (19/36, 53%) was a confounding variable, which improved with app engagement. Future studies that include treatment of poststroke depression may positively influence intervention efficacy. |
| Shin et al53 | N=24 | Single-blind RCT | South Korea | SPVFTCT system | Trunk control | To investigate the role of SPVFTCT for improvement of trunk control and spatiotemporal gait parameter in patients with stroke. | The results of this study indicate that the SPVFTCT system is effective in improving the trunk control ability and spatiotemporal gait parameters of patients with chronic stroke. The advantage of this SPVFTCT system is that it can be easily used in combination with a smartphone to build a visual feedback training environment to help trunk control and gait of patients with stroke. Furthermore, additional visual feedback trunk control training may reduce the treatment time needed to improve the trunk control and gait ability of patients with stroke. Further studies including larger sample sizes and equal total training times between the SPVFTCT and control group are required to generalize the effects of the SPVFTCT system. |
| Kim et al54 | N=99 | 12-wk single-arm intervention | South Korea | SmartAftercare | Medical management/secondary prevention and exercise/physical activity/functional mobility | To evaluate the effects of a smartphone-based mHealth system on health behaviors and risk factor control. | Awareness of stroke, depression, and blood pressure was enhanced when using the smartphone-based mHealth system. Emerging mHealth techniques have potential as new nonpharmacologic secondary prevention methods because of their ubiquitous access, near real-time responsiveness, and comparatively lower cost. |
| Zhang et al55 | N=16∗ | Describe development, usability study, home-based clinical trial | United States | RehabPhone | Upper extremity function | To describe design and development and test usability and conduct a trial for smartphone based assessment and clinical assessment of adherence and clinical efficacy. | Results indicate that users with stroke with RehabPhone demonstrate a high adherence and clinical efficacy in a self-managed home-based rehabilitation course. |
| Zhang et al56 | N=167 | Cohort study | China | Medical management/secondary prevention | To evaluate WeChat-based service for ischemic stroke secondary prevention and examine efficacy, feasibility, and acceptability. | Use of WeChat self-monitoring showed a trend of increasing medication compliance and decreasing ischemic endpoint event rate compared with traditional monitoring. However, there were ceiling effects in the outcomes, and a relatively small sample size was used. Male participants displayed better adherence to WeChat self-monitoring. The community-based population displayed good adherence when using WeChat self-monitoring. | |
| Rogerson et al57 | N=20 | Mixed methods | United Kingdom | Howz | Home safety | To assess the feasibility and acceptability of the Howz smart home system for survivors of stroke. | The Howz system was feasible and acceptable for survivors of stroke. It gave users and their families an enhanced sense of security and peace of mind that help would be at hand if needed. |
Abbreviations: ASR, automatic speech recognition; CV, coefficient of variation; HBR, home-based rehabilitation; HP, home program; KUHMS, Korea University Health Monitoring System; LOS, length of stay; PC, personal computer; PHA, personal health assistant; QAB, Quick Aphasia Battery; RCT, randomized controlled trial; SAMI, Services Assistance Mobile and Intelligent; SHEMA, Stroke Health Education Mobile App; SPVFTCT, smartphone-based visual feedback trunk control training; SSA, sub-Saharan Africa; 3-D, 3-dimensional; VR, virtual reality
Population of persons with stroke are among a larger pool of participants also involved in the study but not reported in this table. Note. Author report is directly pulled or direct quotation from the identified study when available.
Overall, the literature described 38 mobile apps, which involved a variety of aims and objectives ranging from describing development to trials examining effectiveness. A majority of the apps examined elements such as usability; operational issues; descriptions of use for continued development and refinement; and pilot, feasibility, proof of concept, and initial study to examine preliminary outcomes such as signals of improvement or efficacy. Eighteen studies (36.7%) were categorized as pilot, feasibility, or proof-of-concept trials.9,10,12, 13, 14,17,24,30,33,36, 37, 38,42,45,47,52,56,57 In general, the studies had relatively small sample sizes, where 23 studies (46.9%) had ≤20 participants,9, 10, 11, 12,15,16,22,25, 26, 27, 28,32,34, 35, 36,38,41,43, 44, 45,47,50,57 22 studies (44.9%) had between 21 and 100 participants,13,14,17, 18, 19, 20, 21,23,24,29,30,31,33,40,42,46,49,51, 52, 53, 54 and 4 studies (8.2%) had >100 participants (see table 1).20,39,48,56
Content foci
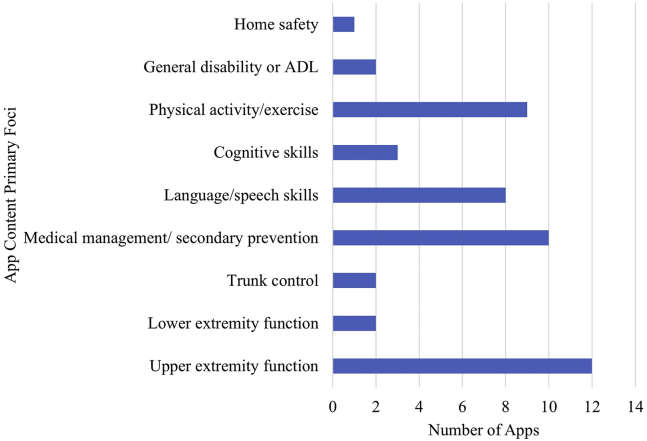
The 49 articles described 38 apps with content that varied in focus. The apps focused on upper extremity function (n=12; 31.5%)9, 12,17,18,23,24,27, 28, 29,36,43,44,49,50,51,55; lower extremity function (n=2; 5.3%)12,51; general exercise, physical activity, and/or functional mobility (n=9; 23.7%)12,31,37,39,41,42,46,47,51,54; trunk control (n=2; 5.3%)51,53; medical management and secondary prevention (n=10; 26.3%)13, 14, 15, 16,33,39,40,43,44,48,51,52,54,56; language and speech skills (n=8; 20.5%)19, 20, 21, 22, 23, 24, 25,34,35,38,45; cognitive skills (n=3; 7.9%)23,24,26; general disability and activities of daily living (ADL) (n=2; 5.3%)30,32; and home safety (n=1; 2.6%) (fig 2).57
Fig 2.
App content primary foci.
Global perspective
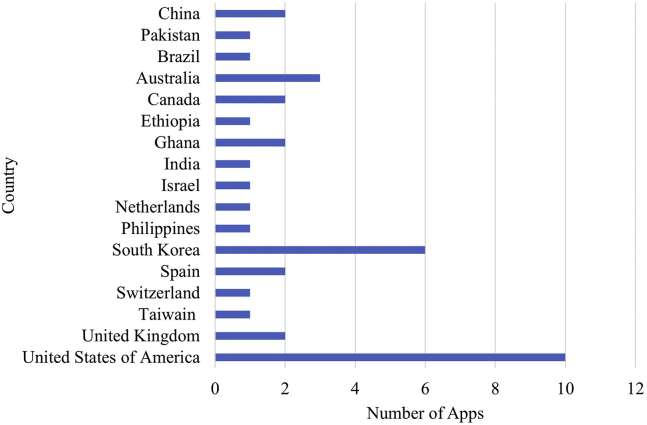
The included studies represented various countries throughout the world. The primary author’s location or described target population contributed to data in this section. Of the identified apps in the literature, 17 countries were identified. The United States had the highest frequency, which included 10 total apps.9, 10, 11,16,19, 20, 21, 22,26, 27, 28,44,50,52,55 Refer to fig 3 for a depiction of representation by country for each app identified in the literature.
Fig 3.
Number of included apps published representing various countries.
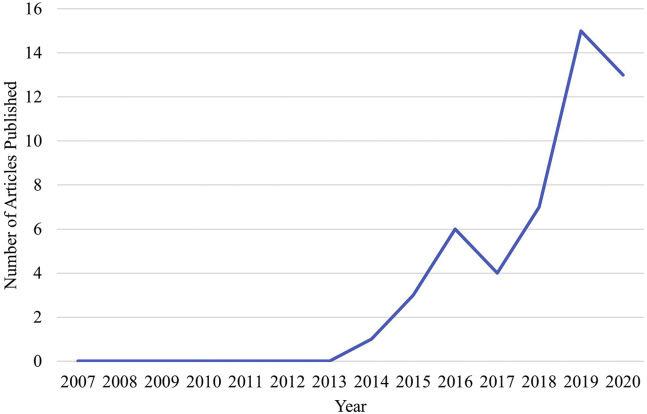
Temporal trends
In recent years mHealth apps for people living with the effects of stroke have gained significant traction. The earliest study included in this review was from 2014.22 This number has grown substantially, with 15 of the included studies14,15,20,23, 24, 25, 26, 27,37, 38, 39, 40,42,43,45 being published in 2019 and 14 studies28,41,46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57 between January and September of 2020. Refer to fig 4 for a visual depiction of articles included by year.
Fig 4.
Number of included articles published by year (2007-2019).
Discussion
This scoping review identified 49 articles describing 38 mHealth apps for use by individuals after stroke. Our study revealed (1) the studies were generally describing development and refinement, pilot/feasibility trials, and included small sample sizes; (2) the studies and apps covered a range of foci but seemed to neglect to focus on psychosocial and other important problems areas after stroke such as anxiety, depression, fatigue, and sleep; (3) the number of published articles on mHealth apps for persons living with the effects of stroke is increasing each year; and (4) although apps are being created across the globe, most published research articles are authored or carried out in the United States.
Most literature supporting mHealth apps present only emergent evidence, lower-power designs such as pilot and feasibility studies, and case series,58 which is consistent with the findings of this study. The vast majority of included articles discuss design and development, are pilot/feasibility studies, and examine outcomes such as usability and acceptability. Most of the articles concluded that additional trials with larger sample sizes are warranted. As more people continue to survive after acute stroke,59 systems must be in place to support long-term needs.
Long-term needs are diverse after stroke, and we discovered a variety of content foci to support these needs. People with stroke must engage in the day-to-day management of living with a chronic condition, and mHealth apps may be particularly useful in supporting this. For instance, some people may be seeking mHealth apps to continue working toward progress in cognitive function, while others may be more focused on learning approaches for recurrent stroke prevention. Of the identified apps, 79.6% focused on either upper extremity function, language/speech skills, medical management/secondary prevention, or exercise/physical activity/functional mobility. Although this finding is generally positive, several content areas need further study. We found that 20.4% of the studies focused on either lower extremity function, trunk control, cognitive function, disability/ADL, and home safety. Furthermore, people living with the effects of stroke have a vast range of needs beyond the content foci identified in this study. For instance, poststroke depression and fatigue are major problem areas that influence health and function. Although we did not identify any apps targeting these topics, it is possible that apps are available for general users or conditions other than stroke.
Interestingly, the increasing rate of stroke among adults younger than 55 years and the rising number of years lived with poststroke disability are pressing the need for alternatives to hospital and institutionalized care.58 Use of devices to manage various aspects of health care after stroke is gaining traction and popularity to increase long-term self-management of stroke and to help offset reduced accessibility to skilled care. Leveraging mobile technologies has great potential for supporting the long-term needs of people with stroke. With smartphone ownership increasing globally,60 mHealth apps can provide innovative solutions that are scalable to reach populations with limited access to services after stroke despite geographic location.
The global demand for mHealth apps to support outcomes in persons with stroke is high. Our study discovered a wide representation of countries and populations testing apps for people with stroke to meet health and rehabilitation demands, although most of the research on mHealth apps for persons with stroke is being conducted in the United States. Currently, the severe acute respiratory syndrome coronavirus 2 pandemic is having an effect on health care and service delivery globally. We expect to see a greater surge of mHealth apps to support long-term needs of people living with the effects of stroke to emerge in the near future.
In addition to this scoping review emphasizing the need for additional large-scale trials, it is essential that studies continue to use iterative approaches to design and development. Several of the studies we reviewed described co-design and participatory design approaches to improve overall acceptance of the targeted end user. Engaging people living with the effects of stroke at multiple time points throughout the developmental process is an essential consideration for developing products that are valued and used.
Study limitations
Despite a comprehensive search strategy, this study is not without limitations. The primary limitation of this review is that some published articles may have been missed that met inclusion criteria because they did not emerge in the databases we selected. This study also only included studies that examined mHealth apps as an independent intervention or as an adjunct to traditional therapy with minimal involvement from a health care provider. This decision was guided by our inquiry of how mHealth can support individuals living with disability as a result of stroke but limited the articles included in this study. We also did not include non-English articles, which may have limited the diversity of articles included in our search; however, our search did capture articles from 13 different countries.
Conclusions
The purpose of this study was to systematically identify the literature on mHealth app interventions to support the self-management of adults living with the effects of stroke. The results of this study suggest that there is growing global interest in mHealth apps for this population but that many gaps persist. Although the literature discovered with the search strategy primarily consisted of development, pilot, and feasibility studies, it is promising that most of the articles describe next steps to examine efficacy with larger sample sizes. Continued research and development are critical in this area to best meet the needs of the growing population who are surviving and living with the long-term effects of stroke. Future studies should also involve longitudinal designs to examine long-term engagement and mHealth app effect on health and functional outcomes.
Supplier
-
a.
Rayyan; Qatar Computing Research Institute.
Footnotes
Disclosures: none
References
- 1.Ullberg T., Zia E., Petersson J., Norrving B. Doctor’s follow-up after stroke in the south of Sweden: an observational study from the Swedish stroke register (Riksstroke) Eur Stroke J. 2016;1:114–121. doi: 10.1177/2396987316650597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . World Health Organization; Geneva, Switzerland: 2001. International classification of functioning, disability, and health: ICF. [Google Scholar]
- 3.Burns S.P., Lutz B.J., Magwood G.S. Timing it right': needs of African American adults with stroke and their caregivers across the care continuum. Ethn Health. 2019:1–15. doi: 10.1080/13557858.2019.1693512. [DOI] [PubMed] [Google Scholar]
- 4.Burns S.P., Schwartz J.K., Scott S.L. Interdisciplinary approaches to facilitate return to driving and return to work in mild stroke: a position paper. Arch Phys Med Rehabil. 2018;99:2378–2388. doi: 10.1016/j.apmr.2018.01.032. [DOI] [PubMed] [Google Scholar]
- 5.Pindus D.M., Mullis R., Lim L. Stroke survivors' and informal caregivers' experiences of primary care and community healthcare services–a systematic review and meta-ethnography. PLoS One. 2018;13:1–23. doi: 10.1371/journal.pone.0192533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prvu Bettger J., McCoy L., Smith E.E., Fonarow G.C., Schwamm L.H., Peterson E.D. Contemporary trends and predictors of postacute service use and routine discharge home after stroke. J Am Heart Assoc. 2015;4 doi: 10.1161/JAHA.114.001038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burns S., Perea J. Popular mHealth apps for adults living with stroke: review and content analysis. Arch Phys Med Rehabil. 2018;99 [Google Scholar]
- 8.Tricco A.C., Lillie E., Zarin W. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 9.Lawson S., Tang Z., Feng J. Supporting stroke motor recovery through a mobile application: a pilot study. Am J Occup Ther. 2017;71:1–5. doi: 10.5014/ajot.2017.025023. [DOI] [PubMed] [Google Scholar]
- 10.Lawson S., Guo J., Smith T., Tang Z., Feng J. In: RESNA’s 2016 annual conference; Arlington, VA; 2016 Feb 12. Preliminary evaluation of a mobile app for everyday stroke rehabilitation; pp. 1–6. [Google Scholar]
- 11.Guo J, Smith T, Messing D, Tang Z, Lawson S, Feng JH. ARMStrokes: a mobile app for everyday stroke rehabilitation. In: Proceedings of the 17th International ACM SIGACCESS Conference on Computers & Accessibility, Libson, Portugal. 2015 Oct 26. p 429-430.
- 12.Sarfo F.S., Adusei N., Ampofo M., Kpeme F.K., Ovbiagele B. Pilot trial of a tele-rehab intervention to improve outcomes after stroke in Ghana: a feasibility and user satisfaction study. J Neurol Sci. 2018;387:94–97. doi: 10.1016/j.jns.2018.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarfo F., Treiber F., Gebregziabher M. PINGS (phone-based intervention under nurse guidance after stroke) interim results of a pilot randomized controlled trial. Stroke. 2018;49:236–239. doi: 10.1161/STROKEAHA.117.019591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sarfo F., Treiber F., Gebregziabher M. Phone-based intervention for blood pressure control among Ghanaian stroke survivors: a pilot randomized controlled trial. Int J Stroke. 2019;14:630–638. doi: 10.1177/1747493018816423. [DOI] [PubMed] [Google Scholar]
- 15.Nichols M., Sarfo F.S., Singh A. Assessing mobile health capacity and task shifting strategies to improve hypertension among Ghanaian stroke survivors. Am J Med Sci. 2017;354:573–580. doi: 10.1016/j.amjms.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Siegel J., Edwards E., Mooney L. A feasibility pilot using a mobile personal health assistant (PHA) app to assist stroke patient and caregiver communication after hospital discharge. Mhealth. 2016;2:31. doi: 10.21037/mhealth.2016.08.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Choi Y.H., Ku J., Lim H., Kim Y.H., Paik N.J. Mobile game-based virtual reality rehabilitation program for upper limb dysfunction after ischemic stroke. Restor Neurol Neurosci. 2016;34:455–463. doi: 10.3233/RNN-150626. [DOI] [PubMed] [Google Scholar]
- 18.Choi Y.H., Paik N.J. Mobile game-based virtual reality program for upper extremity stroke rehabilitation. J Vis Exp. 2018;133 doi: 10.3791/56241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Des Roches C.A., Balachandran I., Ascenso E.M., Tripodis Y., Kiran S. Effectiveness of an impairment-based individualized rehabilitation program using an iPad-based software platform. Front Hum Neurosci. 2015;8 doi: 10.3389/fnhum.2014.01015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Godlove J., Anantha V., Advani M., Des Roches C.A., Kiran S. Comparison of therapy practice at home and in the clinic: a retrospective analysis of the Constant Therapy platform data set. Front Neurol. 2019;10:e140. doi: 10.3389/fneur.2019.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kurland J., Liu A., Stokes P. Effects of a tablet-based home practice program with telepractice on treatment outcomes in chronic aphasia. J Speech Lang Hear Res. 2018;61:1140–1156. doi: 10.1044/2018_JSLHR-L-17-0277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kurland J., Wilkins A., Stokes P. iPractice: piloting the effectiveness of a tablet-based home practice program in aphasia treatment. Semin Speech Lang. 2014;35:51–64. doi: 10.1055/s-0033-1362991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mallet K., Shamloul R., Pugliese M. RecoverNow: a patient perspective on the delivery of mobile tablet-based stroke rehabilitation in the acute care setting. International J Stroke. 2019;14:174–179. doi: 10.1177/1747493018790031. [DOI] [PubMed] [Google Scholar]
- 24.Pugliese M., Ramsay T., Shamloul R. RecoverNow: a mobile tablet-based therapy platform for early stroke rehabilitation. PloS One. 2019;14 doi: 10.1371/journal.pone.0210725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gerber S.M., Schütz N., Uslu A.S. Therapist-guided tablet-based telerehabilitation for patients with aphasia: proof-of-concept and usability study. JMIR Rehabil Assist Technol. 2019;6:e13163. doi: 10.2196/13163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kringle E.A., Setiawan I.M., Golias K., Parmanto B., Skidmore E.R. Feasibility of an iterative rehabilitation intervention for stroke delivered remotely using mobile health technology. Disabil Rehabil Assist Technol. 2020;15:908–916. doi: 10.1080/17483107.2019.1629113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bhattacharjya S., Stafford M.C., Cavuoto L.A. Harnessing smartphone technology and three dimensional printing to create a mobile rehabilitation system, mRehab: assessment of usability and consistency in measurement. J Neuroeng Rehabil. 2019;16:e127. doi: 10.1186/s12984-019-0592-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Langan J., Bhattacharjya S., Subryan H. In-home rehabilitation using a smartphone app coupled with 3D printed functional objects: single-subject design study. JMIR Mhealth Uhealth. 2020;8 doi: 10.2196/19582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jang S.H., Jang W.H. The effect of a finger training application using a tablet PC in chronic hemiparetic stroke patients. Somatosens Mot Res. 2016;33:124–129. doi: 10.1080/08990220.2016.1197117. [DOI] [PubMed] [Google Scholar]
- 30.Sureshkumar K., Murthy G.V., Natarajan S., Naveen C., Goenka S., Kuper H. Evaluation of the feasibility and acceptability of the ‘Care for Stroke’ intervention in India, a smartphone-enabled, carer-supported, educational intervention for management of disability following stroke. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2015-009243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paul L., Wyke S., Brewster S. Increasing physical activity in stroke survivors using STARFISH, an interactive mobile phone application: a pilot study. Top Stroke Rehabil. 2016;23:170–177. doi: 10.1080/10749357.2015.1122266. [DOI] [PubMed] [Google Scholar]
- 32.Groussard P.Y., Pigot H., Giroux S. From conception to evaluation of mobile services for people with head injury: a participatory design perspective. Neuropsychol Rehabil. 2018;28:667–688. doi: 10.1080/09602011.2015.1117499. [DOI] [PubMed] [Google Scholar]
- 33.Seo W.K., Kang J., Jeon M. Feasibility of using a mobile application for the monitoring and management of stroke-associated risk factors. J Clin Neurol. 2015;11:142–148. doi: 10.3988/jcn.2015.11.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brandenburg C., Worrall L., Copland D., Rodriguez A.D. Barriers and facilitators to using the CommFit™ smart phone app to measure talk time for people with aphasia. Aphasiology. 2017;31:901–927. [Google Scholar]
- 35.Brandenburg C., Worrall L., Copland D., Rodriguez A. An exploratory investigation of the daily talk time of people with non-fluent aphasia and non-aphasic peers. Int J Speech Lang Pathol. 2017;19:418–429. doi: 10.1080/17549507.2016.1209558. [DOI] [PubMed] [Google Scholar]
- 36.Kizony R., Zeilig G., Dudkiewicz I., Schejter-Margalit T., Rand D. Tablet apps and dexterity: comparison between 3 age groups and proof of concept for stroke rehabilitation. J Neurol Phys Ther. 2016;40:31–39. doi: 10.1097/NPT.0000000000000110. [DOI] [PubMed] [Google Scholar]
- 37.Grau-Pellicer M., Lalanza J.F., Jovell-Fernández E., Capdevila L. Impact of mHealth technology on adherence to healthy PA after stroke: a randomized study. Top Stroke Rehabil. 2020;27:354–368. doi: 10.1080/10749357.2019.1691816. [DOI] [PubMed] [Google Scholar]
- 38.Garcia M.B. A speech therapy game application for aphasia patient neurorehabilitation–a pilot study of an mHealth app. Int J Simul Syst Sci Technol. 2019;20(5):1–9. [Google Scholar]
- 39.Requena M., Montiel E., Baladas M. FARMALARM: application for mobile devices improves risk factor control after stroke. Stroke. 2019;50:1819–1824. doi: 10.1161/STROKEAHA.118.024355. [DOI] [PubMed] [Google Scholar]
- 40.Kang Y.N., Shen H.N., Lin C.Y. Does a mobile app improve patients’ knowledge of stroke risk factors and health-related quality of life in patients with stroke? A randomized controlled trial. BMC Med Inform Decis Mak. 2019;19:1–9. doi: 10.1186/s12911-019-1000-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vloothuis J., de Bruin J., Mulder M., Nijland R., Kwakkel G., van Wegen E.E. Description of the CARE4STROKE programme: a caregiver-mediated exercises intervention with e-health support for stroke patients. Physiother Res Int. 2018;23:e1719. doi: 10.1002/pri.1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vloothuis J.D., Mulder M., Nijland R.H. Caregiver-mediated exercises with e-health support for early supported discharge after stroke (CARE4STROKE): a randomized controlled trial. PLoS One. 2019;14:e193. doi: 10.1371/journal.pone.0214241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hughes C, Mariscal T, Baye M, et al. Development of an upper extremity stroke rehabilitation mHealth application for sub-Saharan Africa: a usability study. In: 2019 IST-Africa Week Conference (IST-Africa), Nairobi, Kenya; July 2019. p 1-8.
- 44.Hughes CM, Hintze A, Padilla A, et al. Development of a mHealth system for post-stroke upper limb rehabilitation in medically underserved populations: an iterative usability study. In: 2018 IEEE Global Humanitarian Technology Conference (GHTC). San Jose, CA; January 2019. p. 1-8.
- 45.Ballard K.J., Etter N.M., Shen S., Monroe P., Tien Tan C. Feasibility of automatic speech recognition for providing feedback during tablet-based treatment for apraxia of speech plus aphasia. Am J Speech Lang Pathol. 2019;28:818–834. doi: 10.1044/2018_AJSLP-MSC18-18-0109. [DOI] [PubMed] [Google Scholar]
- 46.Costa P.H.V., De Jesus T.P.D., Winstein C., Torriani-Pasin C., Polese J.C. An investigation into the validity and reliability of mHealth devices for counting steps in chronic stroke survivors. Clin Rehabil. 2019;34:394–403. doi: 10.1177/0269215519895796. [DOI] [PubMed] [Google Scholar]
- 47.Simpson D.B., Bird M., English C. Connecting patients and therapists remotely using technology is feasible and facilitates exercise adherence after stroke. Top Stroke Rehabil. 2020;27:93–102. doi: 10.1080/10749357.2019.1690779. [DOI] [PubMed] [Google Scholar]
- 48.Kamal A., Khoja A., Usmani B. Effect of 5-minute movies shown via a mobile phone app on risk factors and mortality after stroke in a low- to middle-income country: randomized controlled trial for the stroke caregiver dyad education intervention (Movies4Stroke) JMIR Mhealth Uhealth. 2020;8:e12113. doi: 10.2196/12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chae S.H., Kim Y., Lee K., Park H. Development and clinical evaluation of a web-based upper limb home rehabilitation system using a smartwatch and machine learning model for chronic stroke survivors: prospective comparative study. JMIR Mhealth Uhealth. 2020;8 doi: 10.2196/17216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.LaPiana N., Duong A., Lee A. Acceptability of a mobile phone-based augmented reality game for rehabilitation of patients with upper limb deficits from stroke: case study. JMIR Rehabil Assist Technol. 2020;7 doi: 10.2196/17822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chung B.P.H., Chiang W.K.H., Lau H. Pilot study on comparisons between the effectiveness of mobile video-guided and paper-based home exercise programs on improving exercise adherence, self-efficacy for exercise and functional outcomes of patients with stroke with 3-month follow-up: a single-blind randomized controlled trial. Hong Kong Physiother J. 2020;40:63–73. doi: 10.1142/S1013702520500079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ifejika N.L., Bhadane M., Cai C.C., Noser E.A., Grotta J.C., Savitz S.I. Use of a smartphone-based mobile app for weight management in obese minority stroke survivors: pilot randomized controlled trial with open blinded end point. JMIR Mhealth Uhealth. 2020;8 doi: 10.2196/17816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shin D. Smartphone-based visual feedback trunk control training for gait ability in stroke patients: a single-blind randomized controlled trial. Technol Health Care. 2020;28:45–55. doi: 10.3233/THC-191647. [DOI] [PubMed] [Google Scholar]
- 54.Kim D.Y., Kwon H., Nam K., Lee Y., Kwon H., Chung Y.S. Remote management of poststroke patients with a smartphone-based management system integrated in clinical care: prospective, nonrandomized, interventional study. J Med Internet Res. 2020;22 doi: 10.2196/15377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhang H, Guo G, Comstock E, et al. RehabPhone: a software-defined tool using 3D printing and smartphones for personalized home-based rehabilitation. Proceedings of the 18th International Conference on Mobile Systems, Applications, and Services (MobiSys '20). Toronto ON, Canad; June 15-19, 2020. p 434-447.
- 56.Zhang Y., Fan D., Ji H., Qiao S., Li X. Treatment adherence and secondary prevention of ischemic stroke among discharged patients using mobile phone- and WeChat-based improvement services: cohort study. JMIR Mhealth Uhealth. 2020;8 doi: 10.2196/16496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rogerson L., Burr J., Tyson S. The feasibility and acceptability of smart home technology using the Howz system for people with stroke. Disabil Rehabil Assist Technol. 2020;15:148–152. doi: 10.1080/17483107.2018.1541103. [DOI] [PubMed] [Google Scholar]
- 58.Matthew-Maich N., Harris L., Ploeg J. Designing, implementing, and evaluating mobile health technologies for managing chronic conditions in older adults: a scoping review. JMIR Mhealth Uhealth. 2016;4:e29. doi: 10.2196/mhealth.5127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yu A.Y.X., Kapral M.K. More people are surviving after acute stroke. BMJ. 2019;(365):l2150. [Google Scholar]
- 60.Silver L., Johnson C. Majorities in sub-Saharan Africa own mobile phones, but smartphone adoption is modest. https://www.pewresearch.org/global/2018/10/09/majorities-in-sub-saharan-africa-own-mobile-phones-but-smartphone-adoption-is-modest/ Available at: