Abstract
Background
We investigated the association between geographic proximity to hospitals and the administration rate of reperfusion therapy for acute ischemic stroke.
Methods
We identified patients with acute ischemic stroke who visited the hospital within 12 hours of symptom onset from a prospective nationwide multicenter stroke registry. Reperfusion therapy was classified as intravenous thrombolysis (IVT), endovascular therapy (EVT), or combined therapy. The association between the proportion of patients who were treated with reperfusion therapy and the ground transport time was evaluated using a spline regression analysis adjusted for patient-level characteristics. We also estimated the proportion of Korean population that lived within each 30-minute incremental service area from 67 stroke centers accredited by the Korean Stroke Society.
Results
Of 12,172 patients (mean age, 68 ± 13 years; men, 59.7%) who met the eligibility criteria, 96.5% lived within 90 minutes of ground transport time from the admitting hospital. The proportion of patients treated with IVT decreased significantly when stroke patients lived beyond 90 minutes of the transport time (P = 0.006). The proportion treated with EVT also showed a similar trend with the transport time. Based on the residential area, 98.4% of Korean population was accessible to 67 stroke centers within 90 minutes.
Conclusion
The use of reperfusion therapy for acute stroke decreased when patients lived beyond 90 minutes of the ground transport time from the hospital. More than 95% of the South Korean population was accessible to 67 stroke centers within 90 minutes of the ground transport time.
Keywords: Ischemic Stroke, Reperfusion, Thrombolysis, Endovascular Treatment, Utilization
Graphical Abstract
INTRODUCTION
Geographic access to hospitals that offer acute care for patients with trauma or acute myocardial infarction can be crucial because timely treatment can improve outcomes.1,2,3,4 For patients with acute ischemic stroke, access to hospitals that provide reperfusion therapy is important because the reperfusion therapy for acute ischemic stroke is also highly time-sensitive.5,6 Several previous studies have suggested the probability of receiving reperfusion therapies for acute ischemic stroke increased when the patients lived in close geographic proximity to hospitals that provide the therapy, however other studies did not find a significant association between the transport time from home to hospital and the use of reperfusion therapy.7,8,9,10 For example, longer driving time to the treating hospital was significantly associated with longer onset-to-arrival time to the hospitals and lower odds of receiving intravenous thrombolysis (IVT) in a retrospective study of 118,683 acute stroke patients admitted to 1,489 US hospitals.10 For endovascular therapy (EVT) for acute ischemic stroke, the proportion of stroke patients receiving EVT decreased significantly when patients lived beyond a 1-hour ground transport time from hospitals that offer EVT in California during 2009 and 2010.7
Among patients with ST-segment elevation myocardial infarction, a wide regional variation exists in the rate of reperfusion therapy and median time from symptom onset to treatment due to differences in geography, local resource, and organization of regional health system.11 Likewise the association between geographic proximity to a hospital that offers the reperfusion therapy for acute stroke patients and the probability of receiving the therapy can vary depending on population density, geography, and systems of care.12,13 Therefore, each region needs to develop an optimal geospatial modeling of acute care centers to provide maximal population access to such centers.1,14
In this study, we investigated the association between geographic proximity to a hospital that offers reperfusion therapy and the administration rate of the therapy for acute ischemic stroke in South Korea, one of the planet's most densely populated countries with a population density of 529 people per square kilometer in 2018.15
METHODS
Patients
The Clinical Research Collaboration for Stroke in Korea (CRCS-K) is a web-based prospective nationwide multicenter stroke registry.16,17 The registry started enrolling patients in April 2008 and the collection of each patient's home address was permitted until August 2014. From the registry, we identified patients with acute ischemic stroke who were over 18 years old and visited one of the 12 CRCS-K hospitals within 12 hours of symptom onset time. The last known normal time was used when the onset of stroke symptom was unclear. Records were excluded if address information was incorrect or if symptom onset or hospital arrival time was unavailable. We also collected the exact time of intravenous tissue plasminogen activator (tPA) administration and groin-puncture time, and calculated onset-to-door, door-to-needle, and door-to-puncture time. We limited our analyses to the addresses within the same provincial area of the treating hospital because transferring acute stroke patients across provincial line is not considered a usual practice. Reperfusion therapy was classified as either IVT alone, vs. EVT or combined IVT and EVT. For patients who were treated with combined IVT and EVT, we identified patients who had received intravenous tPA at an outside hospital and then transferred to the CRCS-K center for EVT, i.e., drip-and-ship paradigm. For an initial stroke severity measurement, we used the National Institutes of Health Stroke Scale (NIHSS) score. For the subtyping of ischemic stroke, we employed the Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification with minor modification18,19 and classified the subtype as large-artery atherosclerosis (LAA), small-vessel occlusion (SVO), cardioembolism (CE), or undetermined etiology (UDE)/other determined etiology (ODE).
Travel distance, ground transport time, and service area
In this study, we classified the patients' residence as metropolitan (city with a population of more than 500,000), urban (city with a population of more than 50,000), or rural region according to the local government act of Korea. After geocoding of the home address and treating hospital for each patient, ground transport time was estimated based on the driving time along the best route from the patient's address to the admitting hospitals using a web-based map service which is optimized for actual traffic condition in Korea (https://map.kakao.com/). For analyses, the travel time was divided into 30-minute increments of ground transport time (i.e., 0–30, 31–60, 61–90, 90–120, and > 120 minutes). To project the findings from CRCS-K hospitals to the national level, we estimated the proportion of the Korean population that lived within each incremental service area from 67 stroke centers accredited by the Korean Stroke Society in 2018 (https://www.stroke.or.kr:4454/hospital/index2.php). To do this, we first obtained the service area from 67 stroke centers using the 30-minute incremental ground transport time threshold. Then, we overlaid these service area maps on the residential areas of 255 administrative districts of South Korea. Finally, we calculated the proportion of the population from each administrative district of South Korea within each service area based on intersection of the service area maps and residential areas. In addition, we repeated the same analysis using the whole territorial area of South Korea including both residential and nonresidential areas. Population data for each administrative district in South Korea were from the Korean National Statistical Office as of December 2019.20 ArcGIS Pro (Version 2.4.0; Esri Inc, Redlands, CA, USA) was used for all geographic analyses.
Statistical analysis
Baseline characteristics of patients were compared using a test for trend across the ordered groups divided into the 30-minute increments of ground transport time. Regression analyses were used to explore the relationship between ground transport time and the proportion of patients that received reperfusion therapies (either IVT alone or EVT). For the non-linear relationship, a restricted cubic spline function with 4 knots defined at the 30 minutes, 60 minutes, 90 minutes, and 120 minutes of ground transport time was used. In the regression analyses, covariates entered the regression models when they had P values less than 0.10 in the univariate analyses. The regression analyses were performed with R software using the “rms” package (version 3.6.0, R Foundation for Statistical Computing, Vienna, Austria). In all analyses, a two-tailed test with P value of less than 0.05 was considered significant.
Ethics statement
This study was approved by the Institutional Review Boards of Jeju National University Hospital (approval No. JEJUNUH 2018-09-003) and all other participating centers with a waiver of informed consent of individual patients because of study subject anonymity and minimal risk to participants.
RESULTS
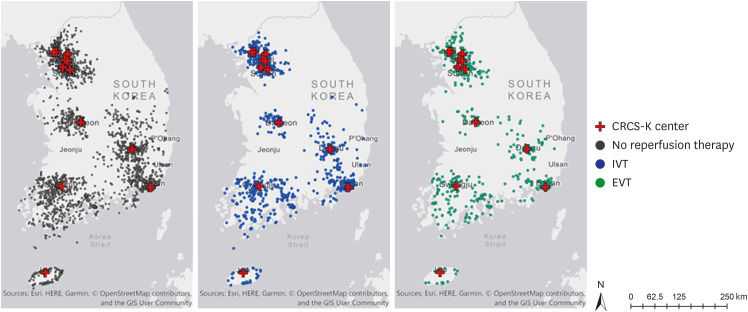
Of 27,122 acute stroke patients who had been admitted to CRCS-K hospitals between April 2008 and August 2014, 12,172 patients met the eligibility criteria (Supplementary Fig. 1). Mean age was 68 ± 13 years, and 59.7% were men. Of 12,172 patients, 2,216 patients (18.2%) were treated with IVT alone and 1238 patients (10.2%) were treated with either EVT alone or combined IVT and EVT. The patients who received reperfusion therapy were more likely to be older, to have atrial fibrillation and higher initial NIHSS score (Supplementary Table 1). In this study, 48.2% of the patients' residence were classified as metropolitan, 41.3% as urban, and 10.5% as rural. The average estimated ground transport time from home to hospital was 23 minutes (interquartile range [IQR], 14–39), and median travel distance was 9.4 km (IQR, 4.5–25.1). In this study, 64.4% of the patients lived within 30 minutes or less to the admitting hospital, 88.7% within 60 minutes or less, 96.5% within 90 minutes or less, and 99.2% with 120 minutes or less. Ground transport times of 30, 60, 90, and 120 minutes corresponded to travel distances of 20.4, 53.5, 86.6, and 119.8 km, respectively. Patients that lived farther from admitting hospitals were more likely to be older, to have atrial fibrillation and CE subtype, and to have a greater initial NIHSS score, but were less likely to have hypertension, diabetes, hyperlipidemia, coronary artery disease and had a lower initial systolic blood pressure (Table 1). The ground transport time did not differ between patients treated with IVT only and patients untreated with reperfusion therapy (rank sum test P = 0.450). However, the ground transport time was slightly but significantly greater for patients treated with EVT compared with patients untreated with reperfusion therapy (24 minutes [14–44] vs. 23 minutes [14–39], rank sum test P = 0.015; Fig. 1 and Supplementary Fig. 2).
Table 1. Characteristics of patients by estimated ground transport time.
| Characteristics | 0–30 min (n = 7,837) | 31–60 min (n = 2,958) | 61–90 min (n = 949) | 91–120 min (n = 335) | > 120 min (n = 93) | P value | ||
|---|---|---|---|---|---|---|---|---|
| Demographic characteristics | ||||||||
| Age, yr | 67 ± 13 | 67 ± 12 | 69 ± 12 | 69 ± 11 | 71 ± 11 | < 0.001 | ||
| Male sex | 4,657 (59.4) | 1,815 (61.4) | 556 (58.6) | 193 (57.6) | 48 (51.6) | 0.600 | ||
| Medical history | ||||||||
| Hypertension | 5,257 (67.1) | 1,912 (64.6) | 605 (63.8) | 214 (63.9) | 55 (59.1) | 0.001 | ||
| Diabetes mellitus | 2,367 (30.2) | 826 (27.9) | 259 (27.3) | 90 (26.9) | 16 (17.2) | < 0.001 | ||
| Atrial fibrillation | 2,159 (27.5) | 820 (27.7) | 297 (31.3) | 121 (36.1) | 39 (41.9) | < 0.001 | ||
| Hyperlipidemia | 2,417 (30.8) | 921 (31.1) | 251 (26.4) | 65 (19.4) | 19 (20.4) | < 0.001 | ||
| Current smoking | 1,991 (25.4) | 804 (27.2) | 225 (23.7) | 80 (23.9) | 10 (10.8) | 0.144 | ||
| History of stroke | 1,721 (22.0) | 612 (20.7) | 196 (20.7) | 70 (20.9) | 22 (23.7) | 0.272 | ||
| History of CAD | 810 (10.3) | 299 (10.1) | 82 (8.6) | 20 (6.0) | 9 (9.7) | 0.015 | ||
| Medication history | ||||||||
| Antiplatelet agents | 2,357 (30.1) | 865 (29.2) | 243 (25.6) | 79 (23.6) | 19 (20.4) | < 0.001 | ||
| Oral anticoagulants | 476 (6.1) | 170 (5.7) | 55 (5.8) | 16 (4.8) | 7 (7.5) | 0.485 | ||
| Statin | 1,271 (16.2) | 440 (14.9) | 124 (13.1) | 34 (10.1) | 10 (10.8) | < 0.001 | ||
| Clinical characteristics | ||||||||
| Onset-to-arrival time (IQR), min | 176 (65–389) | 216 (107–405) | 251 (154–402) | 270 (182–416) | 298 (221–479) | 0.001 | ||
| Initial NIHSS score | 4 (2–11) | 5 (2–13) | 6 (2–14) | 8 (3–14) | 9 (4–15) | < 0.001 | ||
| TOAST classification | 0.038 | |||||||
| LAA | 2,503 (31.9) | 946 (32.0) | 302 (31.8) | 104 (31.0) | 21 (22.6) | |||
| CE | 2,291 (29.2) | 882 (29.8) | 314 (33.1) | 125 (37.3) | 41 (44.1) | |||
| SVO | 1,183 (15.1) | 438 (14.8) | 105 (11.1) | 26 (7.8) | 7 (7.5) | |||
| UDE or ODE | 1,860 (23.7) | 692 (23.4) | 228 (24.0) | 80 (23.9) | 24 (25.8) | |||
| Laboratory values | ||||||||
| Systolic blood pressure, mmHg | 148 ± 28 | 147 ± 27 | 144 ± 25 | 140 ± 24 | 140 ± 24 | < 0.001 | ||
| Diastolic blood pressure, mmHg | 86 ± 17 | 86 ± 16 | 86 ± 15 | 84 ± 14 | 86 ± 14 | 0.682 | ||
| Fasting glucose, mg/dL | 124 ± 51 | 123 ± 48 | 123 ± 46 | 129 ± 48 | 133 ± 59 | 0.012 | ||
| LDL cholesterol, mg/dL | 108 ± 36 | 108 ± 36 | 110 ± 37 | 110 ± 37 | 112 ± 32 | 0.018 | ||
| Hemoglobin, g/dL | 14 ± 2 | 14 ± 2 | 13 ± 2 | 13 ± 2 | 13 ± 2 | < 0.001 | ||
| Platelet counts, 103/μL | 231 ± 75 | 225 ± 71 | 224 ± 73 | 225 ± 78 | 204 ± 56 | < 0.001 | ||
| BUN, mg/dl | 17 ± 9 | 17 ± 9 | 17 ± 9 | 17 ± 8 | 20 ± 14 | 0.812 | ||
| Residential and travel information | ||||||||
| Residence | < 0.001 | |||||||
| Metropolitan | 4,933 (62.9) | 853 (28.8) | 75 (7.9) | 10 (3.0) | - | |||
| Urban | 2,839 (36.2) | 1,565 (52.9) | 457 (48.2) | 154 (46.0) | 14 (15.1) | |||
| Rural | 65 (0.8) | 540 (18.3) | 417 (43.9) | 171 (51.0) | 79 (84.9) | |||
| Transport time (IQR), min | 17 (11–23) | 41 (35–50) | 71 (66–78) | 101 (95–107) | 136 (124–146) | < 0.001 | ||
| Travel distance (IQR), km | 6 (3–9) | 27 (18–39) | 71 (57–85) | 115 (98–123) | 145 (137–156) | < 0.001 | ||
| Thrombolytic therapy | 0.008 | |||||||
| None | 5,645 (72.0) | 2,140 (72.3) | 645 (68.0) | 219 (65.4) | 69 (74.2) | |||
| IVT alone | 1,432 (18.3) | 507 (17.1) | 186 (19.6) | 74 (22.1) | 17 (18.3) | |||
| EVT or combined therapy | 760 (9.7) | 311 (10.5) | 118 (12.4) | 42 (12.5) | 7 (7.5) | |||
Data are presented as number (%) or mean ± standard deviation.
IQR = interquartile range, NIHSS = National Institutes of Health Stroke Scale, LAA = large artery atherosclerosis, CE = cardioembolism, SVO = small-vessel occlusion, UDE = undetermined etiology, ODE = other determined etiology, LDL = low-density lipoprotein, BUN = blood urea nitrogen, IVT = intravenous thrombolysis, EVT = endovascular therapy.
Fig. 1. Patient distribution by reperfusion therapy.
CRCS-K = The Clinical Research Collaboration for Stroke in Korea, IVT = intravenous thrombolysis, EVT = endovascular therapy.
Exact treatment time was available in 1,669 patients (83.4%) treated with IVT alone. The median door-to-needle time was 40 minutes (30–53) and the median onset-to-needle time was 124 minutes (88–170). As expected, the onset-to-needle time was positively correlated with ground transport time (Pearson coefficient 0.201, P < 0.001) since it took more time to arrive at the hospital. However, the door-to-needle was inversely associated with ground transport time (Pearson coefficient −0.108, P < 0.001). Regarding EVT, exact treatment time for patients treated with EVT was available for 1,077 patients (87.0%). The median door-to-puncture time was 107 minutes (85–135) and the median onset-to-puncture time was 240 minutes (170–340). The onset-to-puncture time was positively correlated with ground transport time (Pearson coefficient 0.192, P < 0.001). Like the door-to-needle time in IVT, the door-to-puncture showed a negative association with ground transport time in patients treated with EVT (Pearson coefficient −0.089, P < 0.001) (Supplementary Fig. 3).
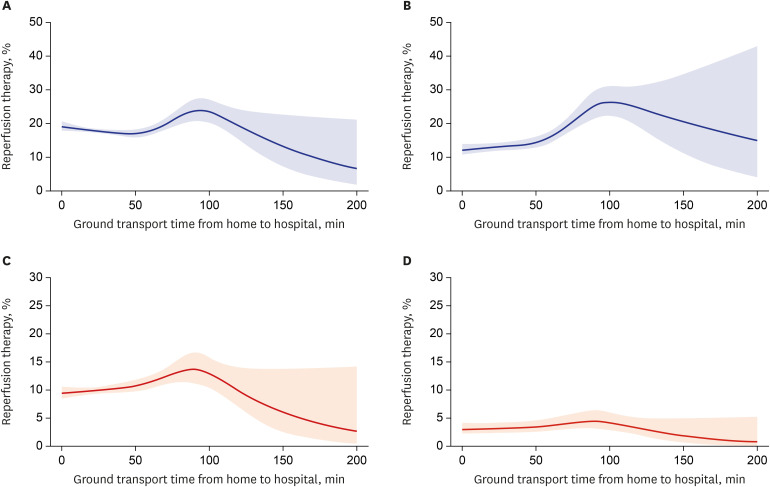
The proportion of patients treated with IVT ranged from 17.1% to 22.1% among the groups with 30-minute increments of ground transport time, and proportion of EVT ranged from 7.5% to 12.4% (Supplementary Fig. 4). In the restricted cubic spline analyses, the proportion of patients treated with IVT decreased significantly when the patients lived beyond a 90-minute ground transport time from the hospital (unadjusted P = 0.003; adjusted P = 0.006). The proportion of stroke patients treated with EVT showed a similar trend with estimated ground transport time in the restricted cubic spline analyses, but it did not reach statistical significance in both unadjusted and adjusted analyses (unadjusted P = 0.086; adjusted P = 0.105) (Fig. 2).
Fig. 2. Estimated proportion of the patients received reperfusion therapy by ground transport time.
(A) IVT, unadjusted analysis (P = 0.003); (B) IVT, adjusted analysis (P = 0.006); adjusted for age, hypertension, diabetes, atrial fibrillation, stroke history, coronary artery disease, use of an antiplatelet agent, oral anticoagulants or statins before the index stroke, diastolic blood pressure, fasting blood glucose, low-density lipoprotein cholesterol, platelet count, onset-to-arrival time, initial NIHSS score, and TOAST classification. (C) EVT, unadjusted analysis (P = 0.090); (D) EVT, adjusted analysis (P = 0.100); adjusted for age, sex, hypertension, diabetes, atrial fibrillation, hyperlipidemia, smoking, coronary artery disease, use of an antiplatelet agent or oral anticoagulants before the index stroke, systolic blood pressure, hemoglobin, platelet count, blood urea nitrogen, onset-to-arrival time, initial NIHSS score, and TOAST classification.
IVT = intravenous thrombolysis, EVT = endovascular therapy, NIHSS = National Institutes of Health Stroke Scale, TOAST = Trial of Org 10172 in Acute Stroke Treatment.
Of 779 patients who had been treated with combined IVT-EVT, we could identify exact referral pattern in 439 patients (56.4%). Among 439 patients, 69 patients (15.7%) were treated by drip- and-ship paradigm. The use of drip-and-ship paradigm increased significantly with greater ground transport time (P < 0.001) (Supplementary Table 2).
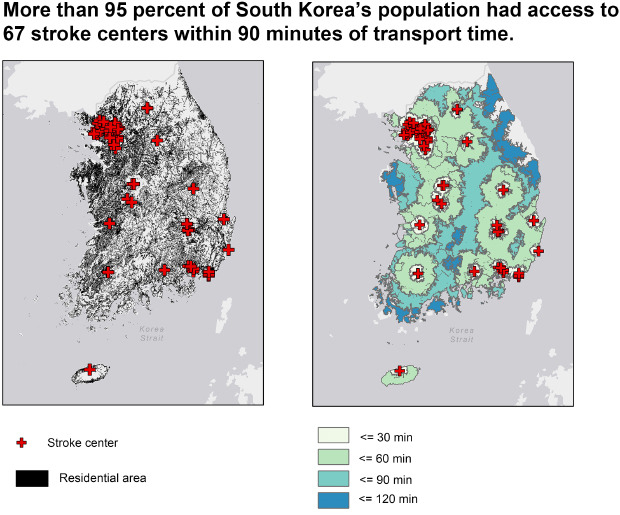
For national coverage from the 67 stroke centers, only 9.3% of the total land area of South Korea was reachable within 30 minutes while 75.0% of the land was accessible within 90 minutes. In contrast, 73.0% of the residential area was reachable within 30 minutes of the ground transport time, and 98.4% of the area was accessible within 90 minutes (Fig. 3 and Table 2).
Fig. 3. Left map shows the residential areas (black) of Korea (A). The service area map on the right shows service areas accessible from the 67 stroke centers accredited by the Korean Stroke Society within each ground transport time threshold (B).
Table 2. Proportion of stroke patients from CRCS-K hospitals and the estimated proportion of Korean population from 67 accredited stroke centers by each ground transport time threshold.
| Hospital | Target population or region | ≤ 30 min | ≤ 60 min | ≤ 90 min | ≤ 120 min |
|---|---|---|---|---|---|
| From 12 CRCS-K centers | CRCS-K population | 64.4% | 88.7% | 96.5% | 99.2% |
| From 67 accredited stroke centers | Total land area of Korea | 11.0% | 54.8% | 82.6% | 92.9% |
| From 67 accredited stroke centers | Residential area of Korea | 73.0% | 93.2% | 98.4% | 99.6% |
CRCS-K = The Clinical Research Collaboration for Stroke in Korea.
DISCUSSION
In this nationwide analysis, we found that more than 95% of patients with acute ischemic stroke who visited one of the 12 CRCS-K hospitals within 12 hours of symptom onset had less than 90 minutes of ground transport time. The proportion of patients treated with IVT decreased significantly when patients had more than 90 minutes of the ground transport time from the hospital. The proportion of stroke patients treated with EVT also showed a similar trend with the transport time. From a national viewpoint, more than 98% of the residential area was accessible within 90 minutes of ground transport time from 67 accredited stroke centers in South Korea.
Geographic access to hospitals offering reperfusion therapy can be crucial to successful reperfusion therapy because the time spent on symptom recognition to decision to medical seeking and the transport time from the scene to the hospital are important contributors to prehospital delays. Living close to treating hospitals was associated with a significantly higher chance of receiving thrombolytic therapy in a study conducted in St. Louis in the US.8 Interestingly, the increased use of thrombolytic therapy was not explained by earlier arrival time in that study, which indicates the presence of other factors such as the use of ambulance transport and health-seeking behavior. Other previous research that used claims data from more than 100,000 Japanese stroke patients did not find an association between driving time and administration of tissue plasminogen activator.9 Instead, they found a significant association between the use of ambulance and the use of thrombolytic therapy regardless of driving time and population density of the area. However, a recent large study enrolling 118,683 patients from the Get With The Guidelines-Stroke Registry (GWTG-Stroke) in the US found a significant association between a longer driving time to hospital and longer onset to arrival time and lower odds of IVT.10 In our study, the proportion of patients treated with IVT decreased significantly when patients had more than 90 minutes of the ground transport time from the hospital. Our findings suggest that the distance to the hospital will not be a major barrier to the use of IVT in South Korea as more than 98% of the South Korean population lives within 90 min from 67 accredited stroke centers in this study.
Although several recent clinical trials have extended the treatment time window for EVT using various perfusion imaging studies, the time interval between stroke onset and reperfusion therapy is still the most important factor affecting eligibility and outcomes for reperfusion therapy in most patients with acute ischemic stroke.21,22,23 For the association between the use of EVT and distance from the hospital, there is not much evidence from the previous literature despite the prehospital delay due to greater transport time could be also crucial to the timely performance of this life-saving therapy for acute ischemic stroke due to large vessel occlusion. In our previous study conducted in California, 94% of the stroke patients lived within a 2-hour ground transport time to the hospital offering the treatment. However, those who lived within 1-hour ground transport time had a significantly increased chance of receiving EVT compared with those who lived beyond 1-hour ground transport time (0.9% vs. 0.2%, P < 0.001).7 In this study, the proportion of stroke patients treated with EVT also decreased when the patients lived beyond a 90-minute ground transport time, however the association did not reach statistical significance. This finding is possibly due to selective referral of the patients who were candidates for EVT from other hospitals although we could not verify this due to lack of information on referral patterns. As with IVT, the ground transport time will not be an important obstacle to receive EVT in South Korea because more than 98% of the population lives within 90 min from 67 stroke centers where most of the EVT procedures would take place.
In addition to personal factors such as health-seeking behavior, or recognition of stroke symptoms, various systemic factors can be associated with thrombolysis administration rates in acute ischemic stroke. Studies have found that urban location, centralized acute stroke care system, use of ambulance, neurologist staffing, and use of acute stroke protocol had a significant impact on the increased use of thrombolysis.24 According to the recent report on the national averages for acute stroke care in Korea during 2013–2014, median arrival time to the hospital was 6 h and only 50% of patients with ischemic stroke used ambulance.25 Overall, IVT was used in 10.7% and EVT in 3.6% of patients with acute ischemic stroke. IVT seems to have been used more frequently than other countries although the drip-and-ship paradigm was used only in 1%. However, significant regional disparities in the rates of reperfusion therapy were found and substantial number of acute stroke patients were treated with reperfusion therapy at low-volume hospitals.25,26 In another research conducted with Korean national stroke audit data, only one-third of patients who were EVT candidates were initially taken to EVT-capable hospitals and initial routing to EVT-capable hospitals was associated with more than two-folds increased chance of receiving EVT compared with initial routing to primary stroke hospital.27 Since South Korea has a universal national health insurance system with a high population density, it is advantageous for treating acute stroke. Therefore, there are a lot of opportunities to improve the rates of reperfusion therapy for stroke patients by enhancing collaboration between stroke centers and emergency medical system, and redefining roles of comprehensive and primary stroke centers with special care for rural residence.
As of 2018, 81.4% of the Korean population live in the urban area according to the world bank data.28 Of 12,172 patients treated at 12 CRCS-K hospitals, 1,272 patients (10.5%) lived in rural region. Therefore, the rural population was underrepresented in our study population and the actual proportion of the stroke patients who received IVT or EVT could be lower in rural regions compared with the urban area. In this study, drip-and-ship paradigm was used in only 15.7% of patients treated with combined IVT-EVT and the use of the paradigm significantly correlated with increased ground transport time. This finding is consistent with our previous work that also reported infrequent use of the paradigm (13.2%) among 1843 patients treated with intravenous tPA at the CRCS-K hospitals.29 From a national perspective, the drip-and-ship paradigm was used in only 1.0% of acute stroke patients and only one-third of EVT candidates were initially routed to EVT-capable hospitals.25,27 Additionally, interhospital transfer of patients initially routed to primary stroke hospitals to EVT-capable hospital occurred in only 17.4% in Korea. Because the stroke patients who live in the rural region would be the most probable patients who need more than 90 min of ground transportation time to stroke centers, placing EVT-capable hospitals in strategic locations readily accessible to the rural population should be considered in planning nationwide coverage for stroke systems of care. The nationwide stroke systems of care should ensure effective interhospital transfer of patients for further treatment and monitoring whenever it is needed and direct routing of patients suspected of large vessel occlusion to EVT-capable hospitals.
This study has several limitations. First, we used the data from 2008 to 2014 when the collection of patients' home addresses was permitted. Therefore, the current study may not reflect the exact nature of the EVT population because the use of a stentriever or aspiration catheter was not as common during most of this period. Second, we do not have information on referrals and use of ambulance which could be associated with the increased use of reperfusion therapy. Referral bias might play an important role in the estimating the proportion of EVT among the patients who lived farther from the admitting hospital. Third, various personal and systemic factors could affect the rate of reperfusion therapy and many of them were not measured in our registry. Fourth, we do not have exact information for the annual volume of IVT or EVT at 67 stroke centers, and therefore we could not estimate the accessibility of the Korean population for high-volume centers separately. Lastly, we also do not have exact information on the place where the patient had suffered the stroke that led to the current admission. Patients could have developed stroke symptoms at other places and therefore the estimation of the ground transport time between the patients' residence and the admitting hospital serves only as a proxy for geographic access to treating hospitals.
In conclusion, more than 95% of the patients with acute ischemic stroke who visited the hospitals within 12 hours of symptom onset lived within 90 minutes of ground transport time from the hospital in this nationwide study. The use of reperfusion therapy decreased when the patients lived beyond 90 minutes of transport time from the hospital. From a national perspective, more than 98% of the South Korean population was accessible to 67 stroke centers within 90 minutes of the ground transport time.
Footnotes
Funding: This work was supported by a research grant from Jeju National University Hospital in 2017.
Disclosure: Dr. Jay Chol Choi is a site investigator of multicenter clinical trials or clinical studies sponsored by Boehringer Ingelheim, AstraZeneca, Jeil pharmaceutical company, and ChongKeunDang Corp. He also received lecture compensation from BMS Korea, Samjin pharmaceutical company Ltd, Bayer Korea, and Dakeda Korea Ltd (modest), but he made no influence on this work in relation with the company or its products. All other authors have no potential conflicts of interest.
- Conceptualization: Choi JC, Kim AS, Bae HJ.
- Data curation: Kim JG, Kang CH, Kang JH, Lee SJ, Park JM, Park TH, Choi YJ, Lee KB, Lee J, Kim DE, Cha JK, Kim JT, Lee BC.
- Formal analysis: Choi JC, Kim JS.
- Writing - original draft: Choi JC, Kim JS.
- Writing - review & editing: Kim JG, Kang CH, Kang JH, Lee SJ, Park JM, Park TH, Choi YJ, Lee KB, Lee J, Kim DE, Cha JK, Kim JT, Lee BC, Kim AS, Bae HJ.
SUPPLEMENTARY MATERIALS
Characteristics of the patients by reperfusion therapy
Use of drip-and-ship paradigm among 439 patients treated with combined intravenous thrombolysis and endovascular therapy by ground transport time
Flow diagram showing the enrollment of the patients.
Violin plot showing the distribution of ground transport time by reperfusion therapy.
Correlations between the treatment time and ground transport time in patients treated with intravenous thrombolysis or endovascular therapy.
Proportion of patients receiving reperfusion therapy by ground transport time.
References
- 1.Jansen JO, Morrison JJ, Wang H, He S, Lawrenson R, Hutchison JD, et al. Access to specialist care: optimizing the geographic configuration of trauma systems. J Trauma Acute Care Surg. 2015;79(5):756–765. doi: 10.1097/TA.0000000000000827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Di Domenicantonio R, Cappai G, Sciattella P, Belleudi V, Di Martino M, Agabiti N, et al. The tradeoff between travel time from home to hospital and door to balloon time in determining mortality among STEMI patients undergoing PCI. PLoS One. 2016;11(6):e0158336. doi: 10.1371/journal.pone.0158336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109(10):1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 4.Harmsen AM, Giannakopoulos GF, Moerbeek PR, Jansma EP, Bonjer HJ, Bloemers FW. The influence of prehospital time on trauma patients outcome: a systematic review. Injury. 2015;46(4):602–609. doi: 10.1016/j.injury.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 5.Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016;316(12):1279–1288. doi: 10.1001/jama.2016.13647. [DOI] [PubMed] [Google Scholar]
- 6.Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384(9958):1929–1935. doi: 10.1016/S0140-6736(14)60584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi JC, Hsia RY, Kim AS. Regional availability of mechanical embolectomy for acute ischemic stroke in California, 2009 to 2010. Stroke. 2015;46(3):762–768. doi: 10.1161/STROKEAHA.114.007735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Acharya AB, Nyirenda JC, Higgs GB, Bloomfield MS, Cruz-Flores S, Connor LT, et al. Distance from home to hospital and thrombolytic utilization for acute ischemic stroke. J Stroke Cerebrovasc Dis. 2011;20(4):295–301. doi: 10.1016/j.jstrokecerebrovasdis.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 9.Kunisawa S, Morishima T, Ukawa N, Ikai H, Otsubo T, Ishikawa KB, et al. Association of geographical factors with administration of tissue plasminogen activator for acute ischemic stroke. J Am Heart Assoc. 2013;2(5):e000336. doi: 10.1161/JAHA.113.000336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ader J, Wu J, Fonarow GC, Smith EE, Shah S, Xian Y, et al. Hospital distance, socioeconomic status, and timely treatment of ischemic stroke. Neurology. 2019;93(8):e747–57. doi: 10.1212/WNL.0000000000007963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosselló X, Huo Y, Pocock S, Van de Werf F, Chin CT, Danchin N, et al. Global geographical variations in ST-segment elevation myocardial infarction management and post-discharge mortality. Int J Cardiol. 2017;245:27–34. doi: 10.1016/j.ijcard.2017.07.039. [DOI] [PubMed] [Google Scholar]
- 12.Schwamm LH, Pancioli A, Acker JE, 3rd, Goldstein LB, Zorowitz RD, Shephard TJ, et al. Recommendations for the establishment of stroke systems of care: recommendations from the American Stroke Association's Task Force on the Development of Stroke Systems. Stroke. 2005;36(3):690–703. doi: 10.1161/01.STR.0000158165.42884.4F. [DOI] [PubMed] [Google Scholar]
- 13.Muñoz Venturelli P, Robinson T, Lavados PM, Olavarría VV, Arima H, Billot L, et al. Regional variation in acute stroke care organisation. J Neurol Sci. 2016;371:126–130. doi: 10.1016/j.jns.2016.10.026. [DOI] [PubMed] [Google Scholar]
- 14.Mullen MT, Branas CC, Kasner SE, Wolff C, Williams JC, Albright KC, et al. Optimization modeling to maximize population access to comprehensive stroke centers. Neurology. 2015;84(12):1196–1205. doi: 10.1212/WNL.0000000000001390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The World Bank Data. Population density. [Updated 2020]. [Accessed March 27, 2020]. https://data.worldbank.org/indicator/EN.POP.DNST.
- 16.Kim BJ, Han MK, Park TH, Park SS, Lee KB, Lee BC, et al. Current status of acute stroke management in Korea: a report on a multicenter, comprehensive acute stroke registry. Int J Stroke. 2014;9(4):514–518. doi: 10.1111/ijs.12199. [DOI] [PubMed] [Google Scholar]
- 17.Kim BJ, Park JM, Kang K, Lee SJ, Ko Y, Kim JG, et al. Case characteristics, hyperacute treatment, and outcome information from the clinical research center for stroke-fifth division registry in South Korea. J Stroke. 2015;17(1):38–53. doi: 10.5853/jos.2015.17.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adams HP, Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 19.Ko Y, Lee S, Chung JW, Han MK, Park JM, Kang K, et al. MRI-based algorithm for acute ischemic stroke subtype classification. J Stroke. 2014;16(3):161–172. doi: 10.5853/jos.2014.16.3.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Korean Statistical Information Service. Population of the administrative district. [Updated 2019]. [Accessed March 1, 2020]. http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B040A3.
- 21.Ma H, Campbell BC, Parsons MW, Churilov L, Levi CR, Hsu C, et al. Thrombolysis guided by perfusion imaging up to 9 hours after onset of stroke. N Engl J Med. 2019;380(19):1795–1803. doi: 10.1056/NEJMoa1813046. [DOI] [PubMed] [Google Scholar]
- 22.Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708–718. doi: 10.1056/NEJMoa1713973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378(1):11–21. doi: 10.1056/NEJMoa1706442. [DOI] [PubMed] [Google Scholar]
- 24.Paul CL, Ryan A, Rose S, Attia JR, Kerr E, Koller C, et al. How can we improve stroke thrombolysis rates? A review of health system factors and approaches associated with thrombolysis administration rates in acute stroke care. Implement Sci. 2016;11(1):51. doi: 10.1186/s13012-016-0414-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim JY, Lee KJ, Kang J, Kim BJ, Kim SE, Oh H, et al. Acute stroke care in Korea in 2013–2014: National averages and disparities. J Korean Med Sci. 2020;35(20):e167. doi: 10.3346/jkms.2020.35.e167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seo KD, Suh SH. Endovascular treatment in acute ischemic stroke: a nationwide survey in Korea. Neurointervention. 2018;13(2):84–89. doi: 10.5469/neuroint.2018.01053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kang J, Kim SE, Park HK, Cho YJ, Kim JY, Lee KJ, et al. Routing to endovascular treatment of ischemic stroke in Korea: recognition of need for process improvement. J Korean Med Sci. 2020;35(41):e347. doi: 10.3346/jkms.2020.35.e347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The World Bank Data. Urban population. [Updated 2020]. [Accessed December 14, 2020]. https://data.worldbank.org/indicator/SP.URB.TOTL.IN.ZS?locations=KR.
- 29.Park MS, Lee JS, Park TH, Cho YJ, Hong KS, Park JM, et al. Characteristics of the drip-and-ship paradigm for patients with acute ischemic stroke in South Korea. J Stroke Cerebrovasc Dis. 2016;25(11):2678–2687. doi: 10.1016/j.jstrokecerebrovasdis.2016.07.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Characteristics of the patients by reperfusion therapy
Use of drip-and-ship paradigm among 439 patients treated with combined intravenous thrombolysis and endovascular therapy by ground transport time
Flow diagram showing the enrollment of the patients.
Violin plot showing the distribution of ground transport time by reperfusion therapy.
Correlations between the treatment time and ground transport time in patients treated with intravenous thrombolysis or endovascular therapy.
Proportion of patients receiving reperfusion therapy by ground transport time.