Abstract
Background
Coronavirus disease 2019 (COVID-19) is leading to numerous psychological outcomes, especially emotional distress. Individuals with early life adversity (ELA) may be more susceptible to those psychological stresses during this epidemic.
Aims
To measure the effect of the ELA on acute stress reactions, anxiety and depression during the COVID-19 epidemic, and to examine whether specific trauma types and frequencies of exposure are associated with a more severe acute stress reaction and increased risk of anxiety and depressive symptoms.
Method
This investigation was performed at college students in a comprehensive University of China. The online self-report questionnaire included ELA experiences, exposure to epidemic-related events, acute stress reactions, and anxiety and depression symptoms during the COVID-19 epidemic. Logistic regression and stepwise regression were used to assess the associations and interactions among these variables.
Results
Participants with ELA reported more exposure to epidemic-related events and more severe stress reactions during the epidemics than did those with no ELA. The experience of ELA is associated with acute stress reactions, anxiety and depression in early adulthood. Furthermore, experiencing more ELA during childhood may not only increase the risk of anxiety and depression episode in early adulthood but also lead to more severe acute stress reactions during the epidemic.
Conclusion
Regardless of specific ELA types, ELAs have longer time effects on individual's susceptibility to stress. Under this epidemic, the mental health in young adults with ELA needs more attention.
Keywords: Early life adversity, COVID-19 epidemic, Emotional distress, Anxiety, Depression
1. Introduction
Since the beginning of the 2020, we have been witnessing the coronavirus disease 2019 (COVID-19) spread throughout China and all over the world (Greenberg et al., 2020). With a rapidly increasing number of confirmed cases and deaths, COVID-19 has significantly resulted in various psychological problems in the general population (Xiang et al., 2020), including college students (Liu et al., 2020). The mental health of these young people was affected not only by individuals’ susceptibility to infection and the low predictability of the COVID-19 but also by the dramatically increased social media news surrounding the outbreak. They were concerned about their physical health and families along with experiencing stress and negative emotions, including anxiety, depression and indignation (Li et al., 2020).
Epidemic diseases not only threaten physical health but also affect emotional health (Bao et al., 2020). The experience of early life adversity (ELA) and exposure to traumas are well-documented risk factors for acute stress reactions, depression and anxiety (Wang et al., 2020). During the critical time periods of childhood and adolescence, exposure to traumatic life events increases the risk of psychological distress. The relationship between environmental factors and emotional mental health problems is often characterized as “dose-response” and has long-term effects. Meta-analyses show that ELA is associated with double or more psychological outcomes (Torjesen, 2019; Varese et al., 2012). The chronicity and increased severity of the adversities, in addition to the risks of multiple different types of trauma exposure (Croft et al., 2019) (for example, childhood maltreatment), are often reported in combination with other types of victimization (Radford et al., 2013). These ELAs are thought to elevate sensitivity and responsivity to further stress exposures, and this responsiveness can persist into early adulthood (Epel and Prather, 2018). For example, for those “left behind” children due to their parents migrating to other cities for labor, lacking of parental care, protection and supervision may limit these children's ability to cope with ELA, which in turn leads to more experiences of abuse and neglect (Fellmeth et al., 2018).
In the present study, we investigated the relationship among the frequency and cumulative ELA, anxiety and depression in early adulthood and acute stress reactions during this epidemic. First, we aimed to explore the association of ELA with acute stress reactions, anxiety and depression during the COVID-19 epidemic. Second, we aimed to assess whether this association varies according to ELA type and the frequency of exposure. We hypothesized that the ELA during childhood might have sustained effects for episode of anxiety and depression in early adulthood, and contribute to a higher risk of acute stress reactions during outbreaks.
2. Method
2.1. Participants
Students in a comprehensive universities in Southwest China were invited to participate in the survey on psychological health from February to March 2020, during the outbreak period of COVID-19 in China. A total of 38,962 undergraduate students in the university were invited to participate by completing these questionnaires online. Finally, 14,698 students completed the survey; among them, 1,415 (15.44%) were excluded because they did not complete all the questions about ELA or because their responses showed obvious inconsistencies.
This study was approved by the research Ethics Committee of the West China Hospital of Sichuan University. All participants provided informed consent and were informed that their participation was voluntary.
2.2. Measurements
2.2.1. General information
All participants were asked for sociodemographic information, including age, sex, ethnicity, whether they were from a one-child family and family income. Birthplace, as defined under China's household registration, was rated on six levels, from rural (countryside) to municipal city. Rural birth was rated at level 1 as the village, and birth in the municipal city was rated at level 6 (Wang et al., 2019).
2.2.2. Exposure of COVID-19-related events
Exposure to the epidemic situation was assessed using a 7-item self-report binary scale (yes/no), which evaluates objective and subjective features of the exposure. Each participant was asked the following: (a) whether they were traveling through the epidemic area; (b) whether family members or close friends were traveling though the epidemic area; (c) whether they had contact with persons who may have been infected; (d) whether they felt that they might be infected; (e) whether they had been infected/quarantined; (f) whether family members or close friends were infected/quarantined; or (g) whether family members or close friends died in this epidemic. The total exposure score was calculated by adding up all scores.
2.2.3. Acute stress reaction
The 17-item Post-Traumatic Stress Disorder Symptom Checklist – Civilian version (PCL-C) was used in this study (Andrykowski et al., 1998). This scale was shown to be a reliable indicator of the severity of posttraumatic stress reactions, as the higher the total scores, the more severe the stress reaction (Yang et al., 2007). In this study, the cut-off points of the total score of 30 and 45 were defined as little/no, moderate and high levels of acute stress reaction, respectively. A total score of 30 or higher was defined as an acute stress reaction of COVID-19 (Vera-Villarroel et al., 2011).
2.2.4. Anxiety status
In the current study, the severity of anxiety status was measured using the 7-item General Anxiety Disorder Assessment (GAD-7) (Plummer et al., 2016), which showed good sensitivity and specificity in a previous study. A total score of 5, 10, and 15 are interpreted as the cut-off points for mild, moderate and severe levels of anxiety, respectively. Scores of 5 or higher were defined as indicating anxiety status.
2.2.5. Depression status
The 9-item Patient Health Questionnaire (PHQ-9) (Kroenke and Spitzer, 2002) was used in this study to measure depressive status in the past two weeks. A total score of 0-4 points indicated minimal depression, 5-9 points indicated mild depression, 10-14 points indicated moderate depression, 15-19 points indicated moderately severe depression and 20-27 points indicated severe depression. We also created a categorical measure using a cut-off of 10 and above for depression based on a meta-analysis of previous studies using the PHQ-9 (Manea et al., 2012).
2.2.6. Early life adversity
Responders were asked if they were left behind, abused, neglected or sexually abused in their childhood or adolescent years using a binary scale (yes = 1, no = 0). The left-behind experience (LBE) was measured if subjects experienced parent-child separation (because parents migrated to other cities due to work) for at least 6 months (Yuan and Wang, 2016). The neglected and abused experiences were assessed with 2 other questions extracted from the Childhood Section of Chinese World Mental Health (WMH) initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview Version 3.1 (WMHCIDI-3.1) (Lee et al., 2011). A four-level rating from 0 to 3 as per the frequency was also recorded, representing “never”, “rarely”, “sometimes” and “often”, respectively.
2.3. Statistical analysis
T-tests or chi-square tests were used to compare the differences in sociodemographic characteristics, potential risk factors, exposure to COVID-19-related events, related behavior, and severity of anxiety, depression and acute stress reactions between the group with ELA and those without ELA as appropriate. Logistic regression (dichotomous variables, adjusted odds ratios (ORs) and 95% CI) with the independent variable recoded into dummies were used to explore the association among different frequency and items of the ELA that the participant experienced and other variables, adjusted by sex, birthplace, low family income and only-child status; a two-tailed alpha level of 0.05 was used. Reference category 1 was defined as participants without ELA. Stepwise multiple regression was performed to assess the contributions of different factors to the severity of depression status.
All analyses were carried out using SPSS 26.0 (SPSS Inc., Chicago, IL, USA), and the figure was drawn by GraphPad Prism 8.0 (GraphPad Software, LLC., San Diego, CA, USA).
3. Results
After quality control, a total of 7,747 (84.56%) participants were included; the mean age of the sample was 20.74 (1.15) years, 49.05% were girls, and 10.78% were ethnic minorities. Of these, 4,295 (55.44%) reported childhood life adversities, 4 (0.05%) reported a history of COVID-19 infection, and 15 (0.19%) reported family member deaths because of COVID-19. The comparison of individuals with ELA and those with no ELA are shown in Table 1 . Females reported more ELA experiences (χ2 = 13.465, p < 0.001), anxiety (t = 6.577, p < 0.001), depression (t = 7.488, p < 0.001) and acute stress reactions (t = 6.585, p < 0.001) than males did. Compared with those without ELA, participants with ELA were more likely to have rural births (χ2 = 152.418, p < 0.001), to not be only children (χ2 = 72.698, p < 0.001), and to come from a family with lower income (χ2 = 39.278, p < 0.001). The exposure to COVID-19-related events seems more severe in students with ELA (t = 5.821, p < 0.001).
Table 1.
The comparison of the demographics and risk factors of the participants with ELA and no ELA.
| With no ELA3452 (44.56%) | With ELA4295 (55.44%) | t/χ2 | p | |
|---|---|---|---|---|
| Mean (SD) / N (%) | Mean (SD) / N (%) | |||
| Age, year | 20.72(1.15) | 20.76(1.14) | 1.709 | 0.087 |
| Sex | ||||
| Boys | 1839(53.27) | 2108(49.08) | 13.465 | <0.001 |
| Girls | 1613(46.73) | 2187(50.92) | ||
| Minority | 349(10.11) | 486(11.31) | 7.971 | 0.436 |
| Birth in rural | 1024(29.66) | 1860(43.31) | 152.418 | <0.001 |
| Only-child | 2222(64.37) | 2353(54.78) | 72.698 | <0.001 |
| Low family income | 316(9.15) | 591(13.76) | 39.278 | <0.001 |
| Exposure of COVID-19 related events | 0.74(1.25) | 0.92(1.44) | 5.821 | <0.001 |
Table 2 shows that the severity of acute stress reactions and anxiety and depression status in early adulthood was higher in the group with ELA than in the group without ELA.
Table 2.
The comparison of the severity of acute stress, anxiety and depression of the participants with ELA and no ELA.
| With no ELAN (%) | With ELAN (%) | χ2 | p | |
|---|---|---|---|---|
| Acute stress reaction (PCL-C) | 10.153 | 0.006 | ||
| Little / no | 3212(93.05) | 3912(91.08) | ||
| Moderate | 202(5.85) | 327(7.61) | ||
| High | 38(1.10) | 56(1.30) | ||
| Anxiety (GAD-7) | 12.246 | 0.007 | ||
| Little / no | 3137(90.87) | 3800(88.47) | ||
| Mild | 237(6.86) | 383(8.91) | ||
| Moderate | 65(1.88) | 93(2.16) | ||
| Severe | 13(0.38) | 19(0.44) | ||
| Depression (PHQ-9) | 26.236 | <0.001 | ||
| Little / no | 2960(85.74) | 3509(81.70) | ||
| Mild | 364(10.54) | 560(13.04) | ||
| Moderate | 87(2.52) | 153(3.56) | ||
| Moderately severe | 27(0.78) | 58(1.35) | ||
| Severe | 14(0.40) | 15(0.35) |
Table 3 shows that the risks of anxiety, depression and acute stress reactions increased with the increasing frequency of being neglected and abused. Compared to those without sexual abuse experience, those who had experienced sexual abuse may have a greater risk of anxiety (AOR = 1.387, 95% CI = 1.202-1.600, p < 0.001) and depression (AOR = 1.958, 95% CI = 1.371-2.796, p < 0.001) in early adulthood and more than double the risk of acute stress reactions (AOR = 2.728, 95% CI = 1.473-5.050, p = 0.001) during this outbreak. Compared to those without left behind experience, the participants who were left behind during childhood shows higher risks of anxiety and depression.
Table 3.
The risks of different frequency of the ELA for acute stress, anxiety and depression under this epidemic.
| Acute stress reaction | Anxiety | Depression | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N(%) | B(SE) | AOR† (95% CI) | p | N(%) | B(SE) | AOR† (95% CI) | p | N(%) | B(SE) | AOR† (95% CI) | p | |
| Neglected | ||||||||||||
| Never | 349(7.24) | 1 | 447(9.27) | 1 | 711(9.18) | 1 | ||||||
| Rarely | 83(8.54) | 0.20(0.13) | 1.220(0.949-1.567) | 0.121 | 112(11.52) | 0.27(0.11) | 1.307(1.048-1.630) | 0.017 | 180(2.32) | 0.29(0.09) | 1.342(1.119-1.609) | 0.001 |
| Sometimes | 58(11.96) | 0.56(0.15) | 1.751(1.302-2.355) | <0.001 | 75(15.46) | 0.59(0.13) | 1.809(1.387-2.360) | <0.001 | 120(1.55) | 0.64(0.11) | 1.911(1.530-2.387) | <0.001 |
| Often | 53(5.67) | 0.82(0.14) | 2.277(1.749-2.964) | <0.001 | 70(7.49) | 0.91(0.12) | 2.485(1.962-3.147) | <0.001 | 110(1.42) | 0.90(0.10) | 2.455(2.001-3.013) | <0.001 |
| Abused | ||||||||||||
| Never | 396(1.81) | 1 | 528(9.94) | 1 | 840(10.84) | 1 | ||||||
| Rarely | 92(10.00) | 0.38(0.12) | 1.456(1.144-1.852) | 0.002 | 112(11.52) | 0.29(0.11) | 1.341(1.077-1.670) | 0.009 | 185(2.39) | 0.36(0.92) | 1.428(1.193-1.709) | <0.001 |
| Sometimes | 43(12.68) | 0.64(0.17) | 1.902(1.356-2.667) | <0.001 | 56(16.52) | 0.66(0.16) | 1.930(1.425-2.612) | <0.001 | 86(1.11) | 0.67(0.13) | 1.954(1.510-2.530) | <0.001 |
| Often | 14(10.29) | 0.40(0.29) | 1.495(0.850-2.630) | 0.162 | 19(13.97) | 0.46(0.25) | 1.588(0.968-2.607) | 0.067 | 22(0.28) | 0.13(0.09) | 2.739(1.545-4.854) | 0.001 |
| Left behind | ||||||||||||
| Never | 472(7.78) | 1 | 604(9.96) | 1 | 973(12.55) | 1 | ||||||
| Ever | 151(8.97) | 0.18(0.10) | 1.195(0.9797-1.459) | 0.080 | 206(12.24) | 0.26(0.09) | 1.303(1.094-1.553) | 0.003 | 305(3.94) | 0.39(0.08) | 1.165(1.005-1.350) | 0.043 |
| Sexual abused | ||||||||||||
| Never | 605(7.94) | 1 | 785(10.30) | 1 | 1243(16.04) | 1 | ||||||
| Ever | 18(14.17) | 1.00(0.31) | 2.728(1.473-5.050) | 0.001 | 25(19.68) | 1.04(0.29) | 2.824(1.612-4.948) | <0.001 | 35(0.48) | 1.42(0.25) | 4.133(2.525-6.765) | <0.001 |
†. Adjusted for sex, birthplace, low family income and only-child.
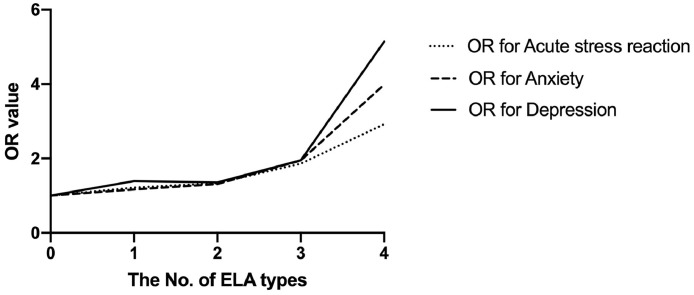
Fig. 1 shows that the risks of anxiety, depression and acute stress reactions increased with an increasing items of ELA, by logistic regression analysis. For individuals with 4 ELAs during their childhood, the risk of acute stress reactions reached 2.924 (95% CI = 1.824-10.375, p = 0.009).
Fig. 1.
The risks of different No. of the ELA types for acute stress reaction, anxiety and depression.
To identify factors that contribute to the severity of depression status, we used stepwise multiple regression with the independent variables as follows: anxiety, acute stress reactions, exposure to COVID-19-related events, sex and ELA. These variables explained 70.8% of the variance in this depression model (Table 4 ). The strongest predictor of the severity of the depression status was anxiety, accounting for 66.5% of the variance. The second-strongest predictor was acute stress reactions (accounting for 4.0% of the variance), followed by exposure to COVID-19-related events, sex and ELA (each accounting for 1.0% of the variance).
Table 4.
Stepwise multiple regression showing the contribution of different factors to severity of depression symptoms.
| Independent Variable | Step 0: correlation | Step 1: Adjusted R2=0.665 | Step 2: Delta R2=0.040 | Step 3: Delta R2=0.001 | Step 4: Delta R2=0.001 | Step 5: Delta R2=0.001 | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| r | Beta † | Partial correlation | Beta † | Partial correlation | Beta † | Partial correlation | Beta † | Partial correlation | Beta † | Partial correlation | |
| Anxiety (GAD-7) | 0.816*** | 0.816*** | 0.816*** | 0.601*** | 0.603*** | 0.600*** | 0.602*** | 0.599*** | 0.602*** | 0.599*** | 0.602*** |
| Acute stress reaction (PCL-C) | 0.733*** | 0.347*** | 0.294*** | 0.347*** | 0.291*** | 0.342*** | 0.290*** | 0.341*** | 0.289*** | 0.340*** | |
| Exposure of COVID-19 related events | 0.183*** | 0.076*** | 0.039*** | 0.022*** | 0.039*** | 0.022*** | 0.037*** | 0.020*** | 0.037*** | ||
| Sex | 0.085*** | 0.042*** | 0.033** | 0.033** | 0.018** | 0.033** | 0.019** | 0.035** | |||
| ELA | 0.060*** | 0.043*** | 0.034** | 0.017** | 0.032** | 0.018** | 0.033** | ||||
†. Beta = standardized regression coefficient; *** p<0.001; **p<0.01
4. Discussion
In the current study, we investigated the association among ELA in early childhood, acute stress reactions, anxiety and depression in college students during the outbreak of COVID-19. The severity and chronicity of ELA may increase the risks of acute stress reactions and anxiety and depression status. We also observed that ELA, anxiety and acute stress reactions may predict more severe depression status during this outbreak.
Compared with participants without ELAs, the ELA group reported more exposure to COVID-19-related events. Worse anxiety and depression status and acute stress reactions were observed in the group with ELA than in the group without ELA, which is consistent with the findings of previous studies (Young et al., 1997). A previous study suggested that ELA increased sensitivity and vulnerability when affected individuals faced stress, and people may show a more negative attitude toward the epidemic situation (Maccari et al., 2014). Although online psychological consulting services were provided for those in need (Dong and Bouey, 2020; Zhai and Du, 2020), the effects still showed significant differences between the two groups.
Childhood and adolescence are sensitive time periods for mental health problems (Maggioni et al., 2020). Studies in animals show that living with overloaded stress may affect the maturity and development of the brain. Compared with other age groups, children and adolescents show increased hypothalamic-pituitary-adrenal activation and anxiety after stress (Lupien et al., 2009; Romeo et al., 2006). In present study, we found that exposure to all types of the ELA is correlated with anxiety and depression, and the long-lasting effects of exposure to multiple types of ELA or recurring ELA increase the risks for anxiety and depression, which is in line with previous studies (Roth et al., 2009). It has been suggested that ELA may play an important role in the underlying mechanisms of stress, depression and anxiety (Rao et al., 2010). The connection is largely dependent on the severity and chronicity of the exposure. Moreover, a more severe acute stress reaction may lead to more severe psychological outcomes, such as posttraumatic stress disorder and major depression, which needs further exploration.
Previous studies suggested that stress, anxiety and depression are strongly correlated with overlapping clinical features, and are associated genetic and susceptibility factors (Brady and Kendall, 1992). In this study, the strongest predictor of depression was the severity of anxiety, and then followed by acute stress. One of the most widely supported psychopathology models is the biological model of stress, which suggests a significant overlap of the dopaminergic and glutaminergic systems(Grace, 2016). Increasing studies have suggested that posttraumatic cognitive and perceptual biases might be associated with dopaminergic and glutaminergic dysfunction, which in turn results in more mental health problems (da Silva Ferreira et al., 2014; van der Gaag et al., 2013). However, the deep interactions among these factors and the potential targets for intervention require further evidence.
Consistent with a previous study (Meiser-Stedman et al., 2012), we found that ELA, anxiety, depressive symptoms and stress reactions are more common in females than in males (Li et al., 2014). It may be due to that less attention is paid to females in remote areas of China, and insufficient concern and love may lead to excessive tension in later life (Dorrington et al., 2019). More attention should be paid to those with ELA, especially in females, during this outbreak.
5. Limitations
There are some limitations in present study. We only included the participants who provided complete information of their ELA experience in the final analysis which have selective bias for sampling. However, we compared demographic data between the included and excluded participants and did not find statistical significance between them (Table 5 ). In addition, our study in college students may not be generalized in other population.
Table 5.
The comparison of participants included and excluded.
| Included participants 7747 (84.56%) | Excluded participants 1415 (15.44%) | t/χ2 | p | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Exposure of COVID-19 related events | 0.84(1.37) | 0.76(1.26) | 1.962 | 0.050 |
| Related behavior under the epidemic | ||||
| Times of wash hands, per day | 2.00(0.86) | 2.00(0.86) | 0.015 | 0.988 |
| Time of browse information about the outbreak, min/day | 64.45(114.12) | 72.24(147.61) | 1.884 | 0.060 |
| Acute stress reaction (PCL-C) | 20.61(6.17) | 20.82(6.17) | 1.189 | 0.235 |
| Anxiety (GAD-7) | 1.23(2.67) | 1.31(2.54) | 3.934 | 0.344 |
6. Conclusion
In this study we found that ELA is highly associated with emotional distress during the epidemic of COVID-19. The sustained effect of the severity and chronicity of ELA increases the risk of acute stress reactions and anxiety and depressive status. Further studies on underlying mechanism and intervention is needed.
Funding Sources
This work was partly supported by the National Natural Science Foundation of China (81630030 and 81920108018); Special Foundation for Brain Research from Science and Technology Program of Guangdong (2018B030334001); Key R & D projects of Science and Technology Department of Sichuan Province (2019YFS0535, 2019YFS0039); 1.3.5 Project for disciplines of excellence, West China Hospital of Sichuan University (ZY2016103, ZY2016203 and ZYGD20004).
Ethical statement
The study was conducted following the principles of the Declaration of Helsinki.
CRediT authorship contribution statement
Xiaojing Li: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing - original draft, Writing - review & editing. Qiuyue Lv: Data curation, Formal analysis, Investigation, Validation, Writing - review & editing. Wanjie Tang: Data curation, Formal analysis, Investigation, Validation, Writing - review & editing. Wei Deng: Data curation, Formal analysis, Investigation, Validation, Writing - review & editing. Liansheng Zhao: Data curation, Formal analysis, Investigation, Validation, Writing - review & editing. Yajing Meng: Data curation, Formal analysis, Investigation, Validation, Writing - review & editing. Wanjun Guo: Data curation, Formal analysis, Investigation, Validation, Writing - review & editing. Tao Li: Conceptualization, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing - review & editing.
Declaration of Competing Interest
The authors have no conflicts of interest to disclose.
Acknowledgments
The authors would like to acknowledge the efforts of the research team and the kindness of the participants for their participation.
References
- Andrykowski M.A., Cordova M.J., Studts J.L., Miller T.W. Posttraumatic stress disorder after treatment for breast cancer: Prevalence of diagnosis and use of the PTSD Checklist–Civilian Version (PCL–C) as a screening instrument. J. Consult. Clin. Psychol. 1998;66:586–590. doi: 10.1037//0022-006x.66.3.586. [DOI] [PubMed] [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet (London, England) 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady E.U., Kendall P.C. Comorbidity of anxiety and depression in children and adolescents. Psychol. Bull. 1992;111:244. doi: 10.1037/0033-2909.111.2.244. [DOI] [PubMed] [Google Scholar]
- Croft J., Heron J., Teufel C., Cannon M., Wolke D., Thompson A., Houtepen L., Zammit S. Association of trauma type, age of exposure, and frequency in childhood and adolescence with psychotic experiences in early adulthood. JAMA Psychiatry. 2019;76:79–86. doi: 10.1001/jamapsychiatry.2018.3155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silva Ferreira G.C., Crippa J.A., de Lima Osório F. Facial emotion processing and recognition among maltreated children: a systematic literature review. Front. Psychol. 2014;5:1460. doi: 10.3389/fpsyg.2014.01460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong, L., Bouey, J., 2020. Public mental health crisis during COVID-19 pandemic, China. Emerg Infect Dis. 26. [DOI] [PMC free article] [PubMed]
- Dorrington S., Zavos H., Ball H., McGuffin P., Sumathipala A., Siribaddana S., Rijsdijk F., Hatch S.L., Hotopf M. Family functioning, trauma exposure and PTSD: a cross sectional study. J. Affect. Disord. 2019;245:645–652. doi: 10.1016/j.jad.2018.11.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epel E.S., Prather A.A. Stress, telomeres, and psychopathology: toward a deeper understanding of a triad of early aging. Annu. Rev. Clin. Psychol. 2018;14:371–397. doi: 10.1146/annurev-clinpsy-032816-045054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fellmeth G., Rose-Clarke K., Zhao C., Busert L.K., Zheng Y., Massazza A., Sonmez H., Eder B., Blewitt A., Lertgrai W., Orcutt M., Ricci K., Mohamed-Ahmed O., Burns R., Knipe D., Hargreaves S., Hesketh T., Opondo C., Devakumar D. Health impacts of parental migration on left-behind children and adolescents: a systematic review and meta-analysis. Lancet North Am. Ed. 2018;392:2567–2582. doi: 10.1016/S0140-6736(18)32558-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace A.A. Dysregulation of the dopamine system in the pathophysiology of schizophrenia and depression. Nat. Rev. Neurosci. 2016;17:524. doi: 10.1038/nrn.2016.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L. The PHQ-9: a new depression diagnostic and severity measure. Psychiatric Ann. 2002;32:509–515. [Google Scholar]
- Lee S., Guo W., Tsang A., He Y., Huang Y., Zhang M., Liu Z., Shen Y., Kessler R. The prevalence of family childhood adversities and their association with first onset of DSM-IV disorders in metropolitan China. Psychol. Med. 2011;41:85–96. doi: 10.1017/S0033291710000450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S., Wang Y., Xue J., Zhao N., Zhu T. The Impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. Int. J. Environ. Res. Public Health. 2020:17. doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Guo W., Kang Y., Li N., Wang Y., Tan Z., Liu C., Luo Y., Feng J. The influence of lack of parental accompaniment, physical abuse and neglect in childhood on the psychological distress in college entrant students. Chin. J. Nerv. Ment. Dis. 2014;40:590–595. [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y.T., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupien S.J., McEwen B.S., Gunnar M.R., Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat. Rev. Neurosci. 2009;10:434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- Maccari S., Krugers H., Morley-Fletcher S., Szyf M., Brunton P. The consequences of early-life adversity: neurobiological, behavioural and epigenetic adaptations. J. Neuroendocrinol. 2014;26:707–723. doi: 10.1111/jne.12175. [DOI] [PubMed] [Google Scholar]
- Maggioni E., Squarcina L., Dusi N., Diwadkar V.A., Brambilla P. Twin MRI studies on genetic and environmental determinants of brain morphology and function in the early lifespan. Neurosci. Biobehav. Rev. 2020;109:139–149. doi: 10.1016/j.neubiorev.2020.01.003. [DOI] [PubMed] [Google Scholar]
- Manea L., Gilbody S., McMillan D. Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): a meta-analysis. CMAJ. 2012;184:E191–E196. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meiser-Stedman R., Dalgleish T., Yule W., Smith P. Intrusive memories and depression following recent non-traumatic negative life events in adolescents. J. Affect. Disord. 2012;137:70–78. doi: 10.1016/j.jad.2011.12.020. [DOI] [PubMed] [Google Scholar]
- Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- Radford L., Corral S., Bradley C., Fisher H.L. The prevalence and impact of child maltreatment and other types of victimization in the UK: findings from a population survey of caregivers, children and young people and young adults. Child. Abuse Negl. 2013;37:801–813. doi: 10.1016/j.chiabu.2013.02.004. [DOI] [PubMed] [Google Scholar]
- Rao U., Chen L.A., Bidesi A.S., Shad M.U., Thomas M.A., Hammen C.L. Hippocampal changes associated with early-life adversity and vulnerability to depression. Biol. Psychiatry. 2010;67:357–364. doi: 10.1016/j.biopsych.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romeo R.D., Bellani R., Karatsoreos I.N., Chhua N., Vernov M., Conrad C.D., McEwen B.S. Stress history and pubertal development interact to shape hypothalamic-pituitary-adrenal axis plasticity. Endocrinology. 2006;147:1664–1674. doi: 10.1210/en.2005-1432. [DOI] [PubMed] [Google Scholar]
- Roth T.L., Lubin F.D., Funk A.J., Sweatt J.D. Lasting epigenetic influence of early-life adversity on the BDNF gene. Biol. Psychiatry. 2009;65:760–769. doi: 10.1016/j.biopsych.2008.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torjesen I. Childhood trauma doubles risk of mental health conditions. BMJ. 2019;364:l854. doi: 10.1136/bmj.l854. [DOI] [PubMed] [Google Scholar]
- van der Gaag M., Schütz C., ten Napel A., Landa Y., Delespaul P., Bak M., Tschacher W., De Hert M. Development of the Davos assessment of cognitive biases scale (DACOBS) Schizophr. Res. 2013;144:63–71. doi: 10.1016/j.schres.2012.12.010. [DOI] [PubMed] [Google Scholar]
- Varese F., Smeets F., Drukker M., Lieverse R., Lataster T., Viechtbauer W., Read J., van Os J., Bentall R.P. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr. Bull. 2012;38:661–671. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vera-Villarroel P., Zych I., Celis-Atenas K., Cordova-Rubio N., Buela-Casal G. Chilean validation of the posttraumatic stress disorder checklist-civilian version (PCL-C) after the earthquake on February 27, 2010. Psychol. Rep. 2011;109:47–58. doi: 10.2466/02.13.15.17.PR0.109.4.47-58. [DOI] [PubMed] [Google Scholar]
- Wang C., Wang Q., Li X., Zhang Y., Wei W., Deng W., Guo W., He L., Tang W., Chen T., Li T. Rural birth/upbringing and childhood adversities are associated with psychotic experiences in university students in China. Schizophr. Res. 2019;209:105–112. doi: 10.1016/j.schres.2019.05.009. [DOI] [PubMed] [Google Scholar]
- Wang Y., Xu J., Lu Y. Associations among trauma exposure, post-traumatic stress disorder, and depression symptoms in adolescent survivors of the 2013 Lushan earthquake. J. Affect Disord. 2020;264:407–413. doi: 10.1016/j.jad.2019.11.067. [DOI] [PubMed] [Google Scholar]
- Xiang Y.-T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X., Yang H., Li Q. The research on the reliability and validity of PCL-C and influence factors. China J. Health Psychol. 2007;15:6–9. [Google Scholar]
- Young E.A., Abelson J.L., Curtis G.C., Nesse R.M. Childhood adversity and vulnerability to mood and anxiety disorders. Depress. Anxiety. 1997;5:66–72. [PubMed] [Google Scholar]
- Yuan P., Wang L. China boom leaves children behind. Nature. 2016;529 doi: 10.1038/529025a. 25-25. [DOI] [PubMed] [Google Scholar]
- Zhai Y., Du X. Mental health care for international Chinese students affected by the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e22. doi: 10.1016/S2215-0366(20)30089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]