Abstract
Introduction
The presence of conditions, such as cardiovascular or chronic lung diseases, was reported to be associated with more severe cases of COVID-19. It is, however, so far unclear how patients with a history of pulmonary embolism (PE) perceive their individual COVID-19 risk. Moreover, their worries and preventive behaviors and their associations with risk perception are unknown.
Materials and methods
A postal survey was conducted in April 2020, including participants with previous PE from the German “Lungenembolie Augsburg” (LEA) cohort study. The questionnaire contained items on COVID-19 knowledge, risk perception (infection likelihood, susceptibility, dangerousness), information sources and satisfaction with information, individual assignment to a high risk group due to pre-existing conditions, worries, infection likelihood, and implementation of preventive behaviors.
Results
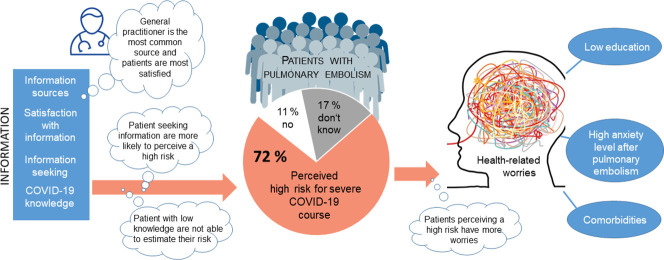
From the 185 respondents, 71.7% assigned themselves to a high risk group in terms of developing a severe case of COVID-19. The likelihood of being infected was rated as verylow/low by 82.3% and the susceptability by 37.8%. A considerable percentage of patients expected a very high/high infection risk in a hospital (48.3%) or at a doctor's practice (37.9%). Major sources of information were the patients' general practitioners (48.9%) and the internet (31.5%). Assignment to a high risk group (β = 1.04) and uncertainty in terms of assignment (β = 1.26) were significantly (p = 0.01) associated with a higher level of health-related worries.
Conclusions
Most patients with previous PE feel that they belong to a high risk group in terms of severe illness from COVID-19. Support in coping with their individual COVID-19 risk is warranted.
Keywords: COVID-19, Pulmonary embolism, Risk perception, Anxiety
Graphical abstract
1. Introduction
Early in the course of the coronavirus disease 19 (COVID-19) pandemic [1], clinicians and researchers tried to identify groups with high risk of severe disease and/or high case fatality. The risk of severe illness and mortality increases with advancing age and male gender [[2], [3], [4]]. In addition, comorbid conditions such as cardiovascular disease, hypertension, diabetes mellitus, chronic pulmonary disease, and cancer are associated with worse outcomes [2,5]. So far, previous pulmonary embolism (PE) was not found to bear an additional risk for severe COVID-19 courses. However, it was shown that acute PE is one of the most common complications of COVID-19 [6,7].
People who experienced a PE prior to the COVID-19 pandemic may identify themselves as being at a higher risk for a severe COVID-19 illness in case of an infection for several reasons. First, they are likely to be at a higher age or to have arterial hypertension, diabetes mellitus or cancer; conditions which are known risk factors for PE [8]. Cardiac diseases in particular, including hypertension and ischemic heart diseases, were reported to be prevalent in 24 to 73% of patients with PE depending on the age group [9]. However, the COVID-19 risk perception of patients with PE has not been investigated so far. In addition, perception of a higher individual risk of severe disease may also affect health-related worries and performance of preventive behaviors. Finally, risk perception may be influenced by the information sources used by patients with PE. Additionally, it is unknown whether patients with PE are satisfied with the information they have retrieved in order to assess their risk associated with COVID-19.
The overall objective of this study was to get a comprehensive picture of the COVID-19 risk perceptions, worries and preventive behaviors and their associations in patients with previous PE. Specific aims of this study were to determine how many patients with PE perceive themselves as persons with a higher risk for severe COVID-19 illness, what the characteristics of these persons are and which information sources they used to gather information on this issue. Furthermore, the question of whether the perception of being at a higher risk for a worse outcome is associated with different levels of worries or different preventive behaviors should be answered.
2. Material and methods
Ethical approval for the “Lungenembolie Augsburg” (LEA) cohort study was obtained from the ethics committee of the Ludwig-Maximilians University Munich (No. 17-378) in August 2017.
2.1. Study design and data collection
An observational, cross-sectional study was performed with participants of the LEA cohort study. A detailed description of the study design and the assessments is provided by Meisinger et al. [10]. From the 355 participants of the LEA study, 10 have refused storage of address data, 2 have completely declined study participation, 80 refused participation in follow-up surveys, and 22 have died. The remaining 231 patients were sent a questionnaire by mail on April 29th 2020 and 167 patients returned the questionnaire by May 20th 2020. Non-respondents (n = 64) received a postal reminder. Of these, 18 completed the questionnaire, resulting in 185 respondents in total.
The maximum COVID-19 7-day incidence rate for the city of Augsburg in spring 2020 was 36 positively tested cases per 100.000 inhabitants on March 30th [11]. Thus, it was comparable with the COVID-19 incidence in the total German population, but even lower than in surrounding cities and regions in Bavaria [12]. The 7-day incidence rate decreased to 3/100.000 inhabitants on May 1st and constantly decreased until June 1st. From March 20th to May 3rd 2020, people in the study area lived in a lockdown situation, which included not leaving their home without cause, minimizing physical contacts and keeping distance to other persons. Restaurants were closed and only shops that provide essential goods were open. Use of public transportation was only allowed wearing a face mask. Outdoor physical activity and sports were only allowed if performed alone, with household members or with one person who is not a member of one's own household. From May 4th to June 14th restrictions were reduced step by step.
In order to improve comparability to similar studies, the questionnaire included a number of items from the COVID-19 Snapshot Monitoring [13,14]. These items and scales have been adapted for the use in COVID-19 studies [15] and were modified for the use in patients with PE in the present study, if necessary. Although information on the psychometric properties of the original items and scales is mostly available [[16], [17], [18], [19]], it is so far lacking for the modified version.
The questionnaire contained 10 single items. Among these, two items inquired about the presence of a COVID-19 infection among the respondents (1 item) and within their social environment (1 item). Items on self-assessed COVID-19 knowledge (1 item) and risk perception (infection likelihood, susceptibility, severity) (3 items) with numeric response options (1 = low to 7 = high) were used [19]. In addition, the certainty of an individual risk for a severe disease course in case of infection (1 items), and satisfaction with information (1 item) were requested. Furthermore, the indiviual assignment to a high risk group due to pre-existing conditions (1 item, yes/no/don't know) and the information sources used (1 item, 10 response options) were requested.
Fears and worries were adressed with 15 items on a 7-point numeric scale (1 = low to 7 = high). Furthermore, the implementation of preventive behaviors was assessed using 19 items and patients were requested to report the likelihood of being infected in 18 situations (7-point numeric scale; 1 = low to 7 = high).
Finally, information on sociodemographic characteristics, medical history and symptoms of depression and anxiety (Hospital Anxiety and Depression Scale, HADS) was obtained from the baseline assessment within the LEA study, which was performed during the initial hospitalization for PE.
2.2. Statistical analysis
The frequency of response categories and/or mean, standard deviation, median and interquartile range were presented. For items rated on a 7-point numeric scale, responses were collapsed for several analyses and presented as “very low/low” (scores 1–3), “medium” (score 4), and “high/very high” (scores 5–7).
This classification was also used when analyzing the association between different levels of COVID-19 knowledge, infection likelihood, susceptibility, dangerousness and certainty of dangerousness rating and patient chararcteristics such as gender, age group, and presence of concomitant diseases using CHI square test or Fisher's exact test, if appropriate.
In order to summarize single items which intend to measure overarching constructs such as “worries”, factor analysis (Principal component analysis with Varimax rotation) was conducted on the corresponding 15 items. The number of retained factors was determined according to the Scree test. Factor analysis resulted in a 2-factor solution with one factor “health-related worries” (7 items) and another factor “general worries” (8 items).
Statistical testing of differences between groups of PE patients in terms of multiple items on worries and preventive behaviors was based on an exploratory approach and therefore no adjustments of type I error were made.
Multinomial logistic regression analysis was used to determine variables associated with the assignment to a high-risk group for a worse COVID-19 outcome (yes/no/don't know). Independent variables were gender, age, school education, COVID-19 knowledge, information about COVID-19 high-risk groups, and presence of comorbidities.
A multivariable linear regression model was calculated in order to identify variables significantly associated with health-related worries. Age, gender, educational and family status, pre-existing comorbidities, time since last PE, self-rated COVID-19 knowledge, infection risk, and suceptability, assignment to high-risk group, presence of COVID-19 cases in the social environment, and baseline symptoms of anxiety were included as independent variables in the regression model. A backward elimination process was used in order to get a parsimonious model. Age and gender were forced to stay in the model, while variables with the highest p-values were removed step by step.
The level of significance was set to 0.05. Statistical analyses were performed with SAS version 9.4.
3. Results
From 231 patients who received the questionnaire, 185 persons (80%) completed it. Sample characteristics are detailed in Table 1 .
Table 1.
Sample characteristics.
| Median | 25%/75% quantile | |
|---|---|---|
| Age (n = 184) | 65.0 | 54/73 |
| Time between last PE event and survey (years) (n = 165) | 0.9 | 0.47/1.99 |
| n | % | |
|---|---|---|
| Gender (n = 185) | ||
| Male | 99 | 53.5 |
| Female | 86 | 46.5 |
| Marital status (n = 181) | ||
| Married | 119 | 65.8 |
| Divorced | 14 | 7.6 |
| Single | 26 | 14.4 |
| Widowed | 22 | 12.2 |
| School education (n = 181) | ||
| “Hauptschule” (9 years) | 67 | 37.0 |
| “Mittlere Reife” (10 years) | 59 | 32.6 |
| “Fachhochschulreife” (11 years) | 16 | 8.8 |
| “Abitur” (high school diploma) (12 years) | 34 | 18.8 |
| None | 1 | 0.6 |
| Others | 4 | 2.2 |
| Living with partner (n = 178) | 52 | 29.2 |
| Number of persons in household (n = 181) | ||
| 1 | 46 | 25.4 |
| 2 | 89 | 49.2 |
| 3–5 | 46 | 25.4 |
| COVID-19 infection (n = 184) | ||
| No | 156 | 84.8 |
| Don't know | 28 | 15.2 |
| COVID-19 infection in personal environment (n = 185) | ||
| No affected persons | 152 | 82.2 |
| Untested suspected cases | 4 | 2.2 |
| Confirmed cases | 8 | 4.3 |
| Recovered persons | 6 | 3.2 |
| Cases of death | 3 | 1.6 |
| Don't know | 15 | 8.1 |
| Disease history | ||
| Recurrent PE (n = 181) | 16 | 8.8 |
| Asthma bronchiale (n = 179) | 24 | 13.4 |
| Autoimmune disease (n = 179) | 18 | 10.1 |
| COPD (n = 178) | 15 | 8.4 |
| Depression (n = 180) | 19 | 10.6 |
| Diabetes mellitus (n = 179) | 18 | 10.1 |
| Chronic heart failure (n = 179) | 10 | 5.6 |
| Systemic hypertension (n = 180) | 91 | 50.6 |
| Cancer (previous 12 months) (n = 179) | 17 | 9.5 |
| Chronic renal disease (n = 178) | 11 | 6.2 |
| Pneumonia (n = 177) | 40 | 22.6 |
| Deep vein thrombosis (n = 177) | 34 | 18.9 |
| Duration hospitalization (n = 171) | ||
| No hospitalization | 17 | 9.9 |
| ≤7 days | 45 | 26.3 |
| 8–14 days | 71 | 41.6 |
| ≥15 days | 38 | 22.2 |
| Intensive care (n = 171) | ||
| No | 99 | 57.9 |
| ≤2 days | 53 | 31.0 |
| 3–7 days | 9 | 5.3 |
| ≥8 days | 10 | 5.8 |
| Simplified PESI score at admission (n = 152) | ||
| Low risk (score = 0) | 78 | 51.3 |
| High risk (score > 0) | 74 | 48.7 |
PE = pulmonary embolism, COPD = chronic obstructive pulmonary disease.
3.1. Risk perception
3.1.1. COVID-19 knowledge, infection likelihood, susceptability, dangerousness and certainty of dangerousness rating
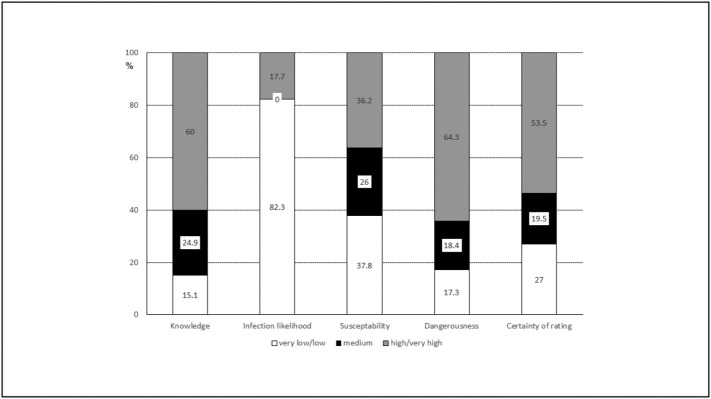
The ratings regarding COVID-19 knowledge, infection likelihood, susceptability, dangerousness and the certainty of the dangerousness assessment are shown in Fig. 1 .
Fig. 1.
Proportion of patients rating their COVID-19 knowledge, infection likelihood, susceptability, dangerousness, and certainty of dangerousness rating as “very low/low” (scores 1–3), “medium” (score 4), or “very high/high” (scores 5–7).
Stratification by gender, age group and number of comorbid conditions showed no significant differences between the groups in terms of COVID-19 knowledge (see Online resource 1) and dangerousness (see Online resource 4). Regarding infection likelihood, subgroup analysis revealed a trend that the proportion of patients who believed that they had a higher infection likelihood was higher in the >65 years age groups compared with the younger patients (p = 0.09). Significant differences by gender or the number of comorbid conditions were not found (see Online resource 2). For the rating of susceptability, subgroup analysis revealed a trend that women reported a higher susceptibility (43.0% very high/high) than men (30.3% very high/high) (p = 0.07) (see Online resource 3). In addition, patients without comorbid conditions were significantly more certain about their rating of dangerousness (19.4% very low/low) (p = 0.01) compared with patients with one and patients with at least two comorbid conditions (31.4% very low/low) (see Online resource 5).
3.1.2. Sources of infection
Coughing or sneezing of other persons was rated as the most likely source of infection (mean score 5.29) and public transportation (mean score 4.48) as the second most likely infection source. Sports or outside activities (mean score 2.12) and contact with children (mean score 2.25) were regarded as minor infection sources (see Online resource 6). Importantly, 48.3% of the patients considered their likelihood of being infected in a hospital as high/very high (scores 5–7), while 37.9% gave the same rating to the likelihood of infection in an outpatient setting.
3.1.3. Assignment to high-risk group and sources of information
Overall, 132 patients (71.7%) assigned themselves to a “high-risk group” with the potential for severe COVID-19 illness due to pre-existing conditions such as pulmonary embolism (see Table 2 ). Age, gender, school education and presence of comorbidities were not significantly related to the assignment to a high risk group in a multinomial regression analysis (see Table 3 ). Patients with a higher self-rating of COVID-19 knowledge had a 0.59-fold odds (95% confidence interval (CI) 0.35–0.98; p = 0.04) of not knowing whether they may belong to a high-risk group compared with patients with less knowledge. Moreover, patients who sought information about COVID-19 high risk groups had a nine-fold higher odds (Odds ratio 9.15, 95% CI 2.38–35.23, p = 0.001) to believe that they are at a higher risk for a more severe case of COVID-19 compared with those who didn't seek information.
Table 2.
Risk perception and information sources.
| n | % | |
|---|---|---|
| Assignment to a “high-risk group” due to pre-existing conditions such as pulmonary embolism | 184 | |
| Yes | 132 | 71.7 |
| No | 21 | 11.4 |
| Don't know | 31 | 16.9 |
| Infomation seeking to know whether one belongs to a “high risk group” | 183 | |
| Yes | 92 | 50.3 |
| No | 91 | 49.7 |
| If yes, source of information | ||
| General practitioner | 45 | 48.9 |
| Medical specialist | 21 | 22.8 |
| Family, friends or colleagues | 35 | 38.0 |
| Internet (e.g. social media, online news, search machines) | 29 | 31.5 |
| Print periodicals | 12 | 13.0 |
| Websites of health authorities | 19 | 20.7 |
| Websites of health services providers (e.g. pharmacies, health insurance companies) | 13 | 14.1 |
| Television and radio | 49 | 53.3 |
| Daily or weekly newspapers | 37 | 40.2 |
| Other sources | 3 | 3.3 |
Table 3.
Multinomial logistic regression model with dependent variable “assignment to high risk group” (yes/no/don't know).
| Variable | High risk group | Odds ratio | 95% confidence interval | p-Value |
|---|---|---|---|---|
| Gender (female) | Yes | 1.00 | 0.34–2.97 | 1.00 |
| Don't know | 2.85 | 0.81–10.12 | 0.10 | |
| Age [years] | Yes | 1.02 | 0.99–1.06 | 0.27 |
| Don't know | 1.02 | 0.98–1.07 | 0.28 | |
| School education (>9 years) | Yes | 0.71 | 0.21–2.42 | 0.58 |
| Don't know | 0.47 | 0.12–1.92 | 0.30 | |
| COVID-19 knowledgea | Yes | 0.83 | 0.54–1.30 | 0.42 |
| Don't know | 0.59 | 0.35–0.98 | 0.04 | |
| Information about COVID-19 high risk groups (yes) | Yes | 9.15 | 2.38–35.23 | 0.001 |
| Don't know | 1.82 | 0.37–8.86 | 0.46 | |
| Comorbidities (yes) | Yes | 2.59 | 0.85–7.92 | 0.09 |
| Don't know | 0.75 | 0.20–2.79 | 0.66 |
Numeric scale ranging from 1 (low) to 7 (high).
About one half (50.3%) of the patients reported that they were seeking information to be able to assess whether they may belong to a “high-risk group”. Most common information sources were television and radio (53.3%) and the patients' general practitioner (48.9%) (see Table 2). Overall, of the patients who sought information, 55 (63.2%) reported that they were very satisfied or satisfied with the provided information, 21 (24.1%) were moderately satisfied, and 11 (12.6%) were unsatisfied or very unsatisfied. Level of satisfaction was highest in patients who gathered information from their general practitioners (mean score 5.65) and lowest in patients who used the internet as information source (mean score 4.64) (see Table 4 ). Patients who named their general practitioner as information source were significantly (p = 0.03) more satisfied (mean score 5.56) with the provided information than patients who did not consult their doctor (mean score 4.85). In contrast, patients who gathered information from the internet were significantly (p = 0.01) less satisfied (mean score 4.64) with the provided information compared with patients who did not (mean score 5.46) (see Table 4). The number of information sources used did not correlate with the level of satisfaction (r = −0.10, p = 0.37).
Table 4.
Satisfaction with information sources by used sources. Numeric rating scale: 1 = very unsatisfied to 7 = very satisfied.
| Used |
Not used |
p-Value | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| General practitioner | 5.56 | 1.47 | 4.86 | 1.53 | 0.03 |
| Medical specialist | 5.38 | 1.40 | 5.15 | 1.58 | 0.66 |
| Family, friends or colleagues | 5.06 | 1.48 | 5.29 | 1.57 | 0.41 |
| Internet (e.g. social media, online news, search machines) | 4.64 | 1.31 | 5.48 | 1.57 | 0.01 |
| Print periodicals | 5.18 | 1.54 | 5.21 | 1.54 | 0.93 |
| Websites of health authorities | 5.06 | 1.59 | 5.25 | 1.55 | 0.67 |
| Websites of health services providers (e.g. pharmacies, health insurance companies) | 5.38 | 1.33 | 5.18 | 1.57 | 0.78 |
| Television and radio | 5.40 | 1.56 | 5.02 | 1.50 | 0.21 |
| Daily or weekly newspapers | 5.38 | 1.26 | 5.09 | 1.69 | 0.59 |
SD = standard deviation.
3.2. Worries
About one half of the patients expressed a high level of worry regarding the potential of severe illness in case of a COVID-19 infection (52.7%), the possibility to die from COVID-19 due to their PE (47.8%) or to loose a loved one (46.7%) (see Table 5 ). Furthermore, 47.5% of the patients were afraid that a recurrent PE event may be diagnosed with delay due to the current COVID-19 situation. Patients who believed that they belong to a high-risk group reported significantly higher levels of worry in almost all questions addressing health and health care issues (Items number 1–7, Table 5) than patients who did not assign themselves to a high-risk group.
Table 5.
Worries due to the current COVID-19 situation.
| Item |
n | Total sample |
Total sample |
Risk group yes |
Risk group don't know |
Risk group no |
p-Value | |
|---|---|---|---|---|---|---|---|---|
| Due to the current corona situation, how much worried are you that … | n (%) much/very much | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| 1 | .. you may have a severe disease course in case of a COVID-19 infection | 184 | 97 (52.7) | 4.46 (1.78) | 3.81 (1.40) | 3.81 (1.40) | 2.57 (1.67) | <0.0001 |
| 2 | … a recurrent pulmonary embolism may be diagnosed with delay | 183 | 87 (47.5) | 4.19 (1.91) | 3.71 (1.62) | 3.71 (1.62) | 3.15 (1.98) | 0.004 |
| 3 | … you may not receive good treatment for pulmonary embolism due to overload of hospitals | 184 | 65 (35.3) | 3.65 (1.93) | 3.81 (1.96) | 3.81 (1.96) | 2.95 (2.01) | 0.16 |
| 4 | … you may die from a COVID-19 infection due to your pulmonary embolism | 184 | 88 (47.8) | 4.23 (2.04) | 4.03 (1.80) | 4.03 (1.80) | 2.38 (1.80) | <0.0001 |
| 5 | … necessary medication for the treatment of your pulmonary embolism is not available | 184 | 46 (25.0) | 3.11 (1.92) | 3.23 (1.80) | 3.23 (1.80) | 2.10 (1.61) | 0.02 |
| 6 | … you may lose a beloved person | 184 | 86 (46.7) | 4.37 (2.00) | 4.65 (1.66) | 4.65 (1.66) | 2.86 (2.29) | 0.003 |
| 7 | … the health care system is overload | 184 | 69 (37.5) | 3.99 (1.80) | 4.48 (1.48) | 4.48 (1.48) | 3.19 (2.16) | 0.03 |
| 8 | … smaller companies declare bankruptcy | 183 | 110 (60.1) | 4.90 (1.85) | 5.16 (1.81) | 5.16 (1.81) | 4.62 (2.07) | 0.60 |
| 9 | … an economic recession may occur | 184 | 124 (67.4) | 5.09 (1.72) | 5.61 (1.48) | 5.61 (1.48) | 4.86 (1.96) | 0.17 |
| 10 | … access to food may be restricted | 184 | 15 (8.2) | 2.38 (1.49) | 2.64 (1.54) | 2.64 (1.54) | 1.86 (1.39) | 0.06 |
| 11 | … power breakdowns my occur | 185 | 12 (6.5) | 2.10 (1.36) | 2.65 (1.64) | 2.65 (1.64) | 1.71 (1.19) | 0.04 |
| 12 | … the society will become more egoistic | 182 | 59 (32.4) | 3.70 (1.76) | 3.93 (1.87) | 3.93 (1.87) | 3.52 (1.83) | 0.70 |
| 13 | … you may lose your job (if applicable) | 103 | 15 (14.6) | 2.32 (1.89) | 2.69 (1.70) | 2.69 (1.70) | 2.58 (1.98) | 0.21 |
| 14 | … the gap between the poor and the rich may widen | 184 | 105 (56.0) | 4.53 (1.75) | 4.90 (1.66) | 4.90 (1.66) | 4.29 (2.26) | 0.53 |
| 15 | … you will experience financial difficulties due to loss of income (e.g. related with short time work) | 144 | 18 (12.5) | 2.35 (1.82) | 2.86 (2.10) | 2.86 (2.10) | 3.18 (2.16) | 0.02 |
Means refer to the numeric rating scale 1 = not at all to 7 = very much.
Fears that an economic recession may occur or smaller companies will declare bankruptcy were pronounced by 67.4% and 60.1%, respectively, of the patients and constitute the most common general/societal worries (see Table 5). Significant differences between high-risk group patients,patients who did not believe that they belong to a high-risk group and those who were uncertain were only found in two items on power breakdowns (p = 0.04) and financial difficulties (p = 0.02).
In a multivariable linear regression model (R2 = 0.27, adjusted R2 = 0.21), higher school education was significantly (p = 0.02) associated with a lower level of health-related worries, whereas the presence of comorbidities (p = 0.002) and a higher anxiety score (Hospital Anxiety and Depression Scale) after the PE event (p = 0.02) were independently related with a higher level of health-related worries (see Table 6 ). Perceived infection risk was also significantly (p = 0.04) associated with higher levels of worries. Patients who assigned themselves to a high-risk group (p = 0.01) as well as patients who were unsure whether they may belong to a high risk group (p = 0.01) showed significantly higher levels of worries compared with those who did not believe that they are at a high risk.
Table 6.
Multivariable linear regression model with dependent variable “health-related worries”.
| Variable | Reference | Parameter estimate | Standard error | p-Value |
|---|---|---|---|---|
| Gender (female) | Male | 0.19 | 0.24 | 0.43 |
| Age [years] | −0.01 | 0.01 | 0.25 | |
| Living with partner (yes) | No | −0.46 | 0.27 | 0.08 |
| School education (>9 years) | ≤9 years | −0.61 | 0.26 | 0.02 |
| COVID-19 infection riska | 0.18 | 0.09 | 0.04 | |
| COVID-19 risk group (yes) | No | 1.04 | 0.37 | 0.01 |
| COVID-19 risk group (don't know) | No | 1.26 | 0.44 | 0.01 |
| Comorbidities (yes) | No | 0.82 | 0.25 | 0.002 |
| HADS anxiety score | 0.06 | 0.03 | 0.02 |
SD = standard deviation.
Numeric scale ranging from 1 (low) to 7 (high).
3.3. Preventive behaviors
A number of preventive behaviors was performed by over 90% of the patients always or often in the week before the survey (see Table 7 ). Some behaviors seemed to be less frequently performed by patients who did not assign themselves to a high risk group compared with the high risk group and those who were unsure. Significant differences, however, were only found in terms of staying at home if ill (e.g. when having a cold) (p = 0.02) and keeping a distance of 1.5 m to other persons in the public (p = 0.04).
Table 7.
Preventive behaviors in the past week. Number and percentage of patients who took the measures always or often.
| n | Total sample | Risk group yes | Risk group don't know | Risk group no | p-Valuea | |
|---|---|---|---|---|---|---|
| Eyes, nose and mouth not touched with unwashed hands | 176 | 93 (52.8) | 64 (50.4) | 17 (56.7) | 12 (63.2) | 0.53 |
| Use of disinfectants | 181 | 99 (54.7) | 77 (58.8) | 15 (50.0) | 7 (35.0) | 0.12 |
| Stayed at home if ill (e.g. when having a cold) | 112 | 90 (80.4) | 70 (86.4) | 12 (70.6) | 8 (57.1) | 0.02 |
| Mouth covered when coughing | 169 | 161 (95.3) | 120 (96.8) | 26 (92.9) | 15 (88.2) | 0.11 |
| Close contact with infected persons avoided | 82 | 72 (87.8) | 53 (88.3) | 10 (83.3) | 9 (90.0) | 0.86 |
| Wearing a nose-mouth mask | 174 | 135 (77.6) | 101 (80.2) | 21 (72.4) | 13 (68.4) | 0.40 |
| Washing hands 20 s | 178 | 164 (92.1) | 122 (93.9) | 28 (93.3) | 14 (77.8) | 0.06 |
| Avoiding hand shakes | 176 | 174 (98.9) | 128 (100.0) | 29 (96.7) | 17 (94.4) | 0.07 |
| Keeping a distance of 1.5 m to other persons in the public | 177 | 174 (98.3) | 127 (99.2) | 30 (100.0) | 17 (89.5) | 0.04 |
| Self-quarantine without having symptoms (if a contact with an infected persons was possible) | 56 | 35 (62.5) | 27 (71.1) | 2 (28.6) | 6 (54.6) | 0.10 |
| Self-quarantine when having symptoms | 30 | 12 (40.0) | 10 (55.6) | 0 (0.0) | 10 (33.3) | 0.05 |
| Avoidance of public places | 171 | 148 (86.6) | 112 (89.6) | 24 (82.8) | 12 (70.6) | 0.07 |
| No participation at private parties | 138 | 119 (86.2) | 87 (83.7) | 19 (90.5) | 13 (100.0) | 0.31 |
| Moving in the public only with one other person or members of the own household | 169 | 132 (78.1) | 96 (78.7) | 21 (72.4) | 15 (83.3) | 0.65 |
| Taken only necessary actions outside (e.g. purchases and doctors consultations) | 178 | 158 (88.8) | 113 (88.3) | 26 (83.9) | 19 (100.0) | 0.20 |
| Being careful when opening letters | 162 | 43 (26.5) | 32 (26.9) | 9 (33.3) | 2 (12.5) | 0.32 |
| Intake of dietary supplements | 155 | 20 (12.9) | 13 (11.4) | 4 (16.7) | 3 (17.7) | 0.52 |
| No private meetings with persons from other households | 157 | 77 (49.0) | 59 (51.8) | 11 (39.3) | 7 (46.7) | 0.49 |
Chi2 test or Fisher's exact test if appropriate.
4. Discussion
This study showed that persons with a history of PE rated their likelihood of being infected with COVID-19 as low overall, their susceptibility as higher and the dangerousness in case of being infected as high. These findings can be compared with the results from the COSMO study derived from a sample of the German population [20]. The mean scores for COVID-19 knowledge (scaled 1 = no knowledge to 7 = very much knowledge) were 4.80 ± 1.31 for the patients with PE and 4.95 for the German population sample [20]. The ratings of infection likelihood and susceptibility were also overall similar, whereas the ratings of dangerousness showed larger differences. From the patients with PE, 64% rated the dangerousness as high/very high compared with 34% from the total German population sample (all age groups, survey date: 05/05/2020). Even when considering the older groups aged 50–64 years with 43% high/very high ratings and 65–74 years with 57% high/very high ratings, a difference with our study participants can be noticed [20]. The patients' perception that PE has a negative impact on their pulmonary health may have contributed to these differences. Moreover, patients with PE may be aware of other comorbidities which were communicated in the media as additional risk factors for a more severe case of COVID-19. However, our study also showed that the high rating of dangerousness was based on a high level of uncertainty among the patients. This uncertainty may be driven by a lack of comprehensive or consistent information. For instance, “chronic lung diseases (e.g. COPD)” in general are reported of being associated with severe COVID-19 courses [21]. However, patients with PE may be unsure whether PE belongs to this group of diseases. The estimation of individual risks requires a comprehensive consideration of a number of individual factors. This might be better provided by a physician, e.g. the general practitioner, than by the patients themselves on the basis of general information from internet sources. Indeed, this hypothesis was supported by the study's findings that the patient's general practitoner was a main source of information and that patients who collected information on their risk from the general practitioner were more satisfied with the provided information than patients who relied on internet sources. The present study also indicates that many patients were worried about a high infection risk for COVID-19 in the hospital or at a physicians' practice. These worries may have negative effects on health care utilization, especially in the case of a recurrent PE event. A reduction of hospital admissions during the COVID-19 lockdown has already been reported for diseases such as acute coronary syndrome [22,23] and chronic obstructive pulmonary disease [24]. Whether patients with PE were also reluctant to seek help for upcoming PE events remains open.
Prior research has demonstrated that a considerable proportion of people suffer from worry and anxiety symptoms during the COVID-19 pandemic [25,26]. In the present study, patients with PE who experienced higher levels of anxiety during their PE event were more likely to worry about the COVID-19 situation and specifically about their own infection risk and disease consequences. This finding is similar to the results from Jungmann et al. [27] who found that the trait health anxiety was positively associated with COVID-19 anxiety. The finding that patients with PE with lower school education experience higher levels of health-related worries than patients with higher education indicates the need to offer appropriate information to these patients [25,27]. Jungmann et al. [27] already demonstrated that information may buffer the negative effects of anxiety during the COVID-19 pandemic. The same applies to patients with comorbidities which may be associated with a higher risk for severe COVID-19, for patients who are unsure whether they belong to a risk group or patients who believe that they have a higher risk for severe COVID-19.
As previous studies have shown, risk perception is an important predictor of preventive behavior [16]. People are more likely to comply with preventive behaviors if they perceive themselves as susceptible and if this illness is deemed to have severe consequences [16]. Thus, it was hypothesized that in the present study, patients with PE who assigned themselves to a high risk group may differ from those who perceived themselves as being at a lower risk in terms of performance of preventive behaviors. This hypothesis, however, was only partially supported by the study data. Maybe the fact that most important preventive measures were taken by more than 90% and small sample sizes in the risk groups have hampered the detection of differences. Besides the comparison within the groups of patients with PE, results of patients with PE can also be compared with responses of the general population from the COSMO study [20]. Indeed, the preventive measures which showed borderline significant differences between the PE patient risk groups, also differed between the total sample of patients with PE and people from the general population. For instance, “Avoidance of public places” was perfomed by 87% of the patients with PE and 73% of the general population sample. Differences can also be observed regarding “Washing hands 20 s” (92% vs. 86%), “Avoiding hand shakes” (99% vs. 93%), and “Keeping a distance of 1.5 m to other persons in the public” (98% vs. 89%).
Overall, the results of the present study offer some starting points for improving the health of patients with PE during the COVID-19 pandemic. Since most patients with PE perceive a higher risk for a negative outcome in case of COVID-19, but seem to be uncertain about their appraisal, they may benefit from support regarding the estimation of their individual risk. Firstly, this may include concise communication of potential COVID-19 risks specifically for patients with PE. Health authorities, health insurance companies and associations for pulmonology and cardiology may offer such information online. Secondly, since individual risk assessment is complex and people may be overwhelmed with this task, specifically if they have a low educational level or further comorbidities, further support may be needed. An individual risk estimation based on scientific evidence and a persons' individual background, living conditions, medical history and current health status should be offered by the patients' attending physicians, either their general practitioners or PE specialists. A realistic risk perception can positively influence patients' lives. The known relation between risk perception and worry has been confirmed in the present study. A provision of appropriate information facilitating a realistic risk perception may subsequently reduce worries. A reduction of worries enhances the quality of life of patients with PE during the pandemic. As shown in previous studies, high levels of fear are associated with ineffective or unfavorable preventive behavior [[28], [29], [30]]. Consequently, the reduction of worries may also reduce COVID-19 incidence among patients with PE.
To our knowledge, this is the first study which investigated COVID-19 risk perceptions, worries and preventive behaviors in patients with previous PE. It is based on data collected in the framework of a cohort study of all consecutive cases of PE in a defined study area with defined inclusion criteria. Study limitations include the small sample size in the stratified analyses. Although the response rate of 80% was high, a selection bias cannot be ruled out. Moreover, although the applied questionnaire was based on items from validated scales, it was not possible to determine its psychometric properties for the use in the present study. Finally, the study was performed in a defined region in Germany and it is unknown whether the findings are generalizable to people from other regions or countries with different COVID-19 incidence, mortality and hospitalization rates.
5. Conclusions
In conclusion, the present study showed that persons with a history of PE often perceive themselves as being at a high risk for severe COVID-19 illness, but many of them are unsure about this appraisal. Information seeking and COVID-19 knowledge plays a major role for the individual risk assessment. A realistic estimation of one's own risk is essential because it is significantly related with health-related fears and worries. Thus, patients with PE may need support in order get a realistic view of their health situation and the risks related to COVID-19. Firstly, support may consist of online, evidence-based information on COVID-19 risks for patients with PE and secondly, of an individual risk estimation offered by the patients' attending physicians, either their general practitioners or PE specialists.
The following are the supplementary data related to this article.
Self-rated COVID-19 knowledge levels “very low/low” (scores 1–3), “medium” (score 4), or “very high/high” (scores 5–7) stratified by sex, age group and presence of comorbid conditions.
Self-rated COVID-19 infection likelihood levels “very low/low” (scores 1–3), “medium” (score 4), or “very high/high” (scores 5–7) stratified by sex, age group and presence of comorbid conditions.
Self-rated COVID-19 susceptability levels “very low/low” (scores 1–3), “medium” (score 4), or “very high/high” (scores 5–7) stratified by sex, age group and presence of comorbid conditions.
Self-rated COVID-19 dangerousness levels “very low/low” (scores 1–3), “medium” (score 4), or “very high/high” (scores 5–7) stratified by sex, age group and presence of comorbid conditions.
COVID-19 certainty of dangerousness rating “very low/low” (scores 1–3), “medium” (score 4), or “very high/high” (scores 5–7) stratified by sex, age group and presence of comorbid conditions.
Assessment of infectionlikelihoodin different situations. Meanscores (1 = extremely unlikely, 7 = extremely likely).
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thank all members of the Chair of Epidemiology and the Department of Cardiology, Respiratory Medicine and Intensive Care at the University Hospital Augsburg who are involved in the conduct of the LEA study, especially Sabine Haberl, Yvonne Bodenstein, Dorothea Küster and Marion Kötzner.
References
- 1.Who director-general's opening remarks at the media briefing on covid-19 - 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020; Date accessed 01.07.2020.
- 2.Guzik T.J., Mohiddin S.A., Dimarco A., Patel V., Savvatis K., Marelli-Berg F.M., Madhur M.S., Tomaszewski M., Maffia P., D’Acquisto F., Nicklin S.A., Marian A.J., Nosalski R., Murray E.C., Guzik B., Berry C., Touyz R.M., Kreutz R., Wang D.W., Bhella D., Sagliocco O., Crea F., Thomson E.C., McInnes I.B. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc. Res. 2020;116:1666–1687. doi: 10.1093/cvr/cvaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 4.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Emami A., Javanmardi F., Pirbonyeh N., Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emerg Med. 2020;8 [PMC free article] [PubMed] [Google Scholar]
- 6.Tal S., Spectre G., Kornowski R., Perl L. Venous thromboembolism complicated with COVID-19: what do we know so far? Acta Haematol. 2020;143:417–424. doi: 10.1159/000508233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roncon L, Zuin M, Barco S, Valerio L, Zuliani G, Zonzin P, Konstantinides SV. Incidence of acute pulmonary embolism in COVID-19 patients: systematic review and meta-analysis. Eur J Intern Med 2020:S0953-6205(20)30349-6. doi: 10.1016/j.ejim.2020.09.006. [DOI] [PMC free article] [PubMed]
- 8.Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, Huisman MV, Humbert M, Jennings CS, Jiménez D, Kucher N, Lang IM, Lankeit M, Lorusso R, Mazzolai L, Meneveau N, Ní Áinle F, Prandoni P, Pruszczyk P, Righini M, Torbicki A, Van Belle E, Zamorano JL; ESC Scientific Document Group. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J 2019. pii: ehz405. doi: 10.1093/eurheartj/ehz405. [DOI]
- 9.Andersson T., Söderberg S. Incidence of acute pulmonary embolism, related comorbidities and survival; analysis of a Swedish national cohort. BMC Cardiovasc. Disord. 2017;17:155. doi: 10.1186/s12872-017-0587-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meisinger C., Linseisen J., Kirchberger I., von Scheidt W., Berghaus T.M. Long-term outcomes in patients with acute pulmonary embolism after in-hospital treatment: study protocol of the prospective Lungenembolie Augsburg Studie (LEA study) BMJ Open. 2019;9 doi: 10.1136/bmjopen-2019-031411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.City of Augsburg. Coronavirus number of cases. https://www.augsburg.de/umwelt-soziales/gesundheit/coronavirus/fallzahlen. Date accessed 16/02/2021.
- 12.Robert Koch Institut. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-03-30-de.pdf?__blob=publicationFile. Date accessed 16/02/2021.
- 13.WHO Regional Office For Europe. COVID-19 Snapshot MOnitoring (COSMO Standard): monitoring knowledge, risk perceptions, preventive behaviors, and public trust in the current coronavirus outbreak - WHO standard protocol. PsychArchives, 2020. doi:10.23668/PSYCHARCHIVES.2782.
- 14.Betsch C., Wieler L., Bosnjak M., Ramharter M., Stollorz V., Omer S., Korn L., Sprengholz P., Felgendreff L., Eitze S., Schmid P. Germany COVID-19 Snapshot MOnitoring (COSMO Germany): monitoring knowledge, risk perceptions, preventive behaviors, and public trust in the current coronavirus outbreak in Germany. PsychArchives. 2020 doi: 10.23668/psycharchives.2776. [DOI] [Google Scholar]
- 15.World Health Organization. Monitoring knowledge, risk perceptions, preventive behaviours and trust to inform pandemic outbreak response. https://www.euro.who.int/__data/assets/pdf_file/0007/436705/COVID-19-survey-tool-and-guidance.pdf. Date accessed 20/02/2021.
- 16.Brewer N.T., Chapman G.B., Gibbons F.X., Gerrard M., McCaul K.D., Weinstein N.D. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26(2):136. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- 17.Steel Fisher G.K. Public response to the 2009 influenza A H1N1 pandemic: a polling study in five countries. Lancet Infect. Dis. 2012;12:845–850. doi: 10.1016/S1473-3099(12)70206-2. [DOI] [PubMed] [Google Scholar]
- 18.McCarthy-Larzelere M., Diefenbach G.J., Williamson D.A., Netemeyer R.G., Bentz B.G., Manguno-Mire G.M. Psychometric properties and factor structure of the Worry Domains Questionnaire. Assessment. 2001;8(2):177–191. doi: 10.1177/107319110100800206. [DOI] [PubMed] [Google Scholar]
- 19.Krawczyk A., Stephenson E., Perez S., Lau E., Rosberger Z. Deconstructing human papillomavirus (HPV) knowledge: objective and perceived knowledge in males’ intentions to receive the HPV vaccine. Am. J. Health Educ. 2013;44(1):26–31. [Google Scholar]
- 20.Betsch C, Korn L, Felgendreff L, Eitze S, Schmid P, Sprengholz P, Wieler L, Schmich P, Stollorz V, Ramharter M, Bosnjak M, Omer SB, Thaiss H, De Bock F, Von Rüden U, Crockett M, Krauth C, Brockmann D, Schlosser F. German COVID-19 snapshot monitoring (COSMO) - Welle 9 (28.04.2020). PsychArchives 2020. doi:10.23668/PSYCHARCHIVES.2890.
- 21.Robert-Koch Institut. SARS-CoV-2 Steckbrief zur Coronavirus-Krankheit-2019 (COVID-19). https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Steckbrief.htm. Date accessed 07.10.2020.
- 22.De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L, Iannaccone M, Galvani M, Ugo F, Barbero U, Infantino V, Olivotti L, Mennuni M, Gili S, Infusino F, Vercellino M, Zucchetti O, Casella G, Giammaria M, Boccuzzi G, Tolomeo P, Doronzo B, Senatore G, Grosso Marra W, Rognoni A, Trabattoni D, Franchin L, Borin A, Bruno F, Galluzzo A, Gambino A, Nicolino A, Truffa Giachet A, Sardella G, Fedele F, Monticone S, Montefusco A, Omedè P, Pennone M, Patti G, Mancone M, De Ferrari GM. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med 2020. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed]
- 23.Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J 2020; 41 (19):1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed]
- 24.Berghaus T.M., Karschnia P., Haberl S., Schwaiblmair M. Disproportionate decline in admissions for exacerbated COPD during the COVID-19 pandemic. Respir. Med. 2020 Aug;14:106120. doi: 10.1016/j.rmed.2020.106120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jungmann S.M., Witthöft M. Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: which factors are related to coronavirus anxiety? J Anxiety Disord. 2020;73:102239. doi: 10.1016/j.janxdis.2020.102239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gaygisiz U., Gaygisiz E., Ozkan T., Lajunen T. Individual differences in behavioral reactions to H1N1 during a later stage of the epidemic. Journal of Infection and Public Health. 2012;5:9–21. doi: 10.1016/j.jiph.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 29.Liao Q., Cowling B.J., Lam W.W., Ng D.M., Fielding R. Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 pandemic in Hong Kong: ten cross-sectional surveys. BMC Infect. Dis. 2014;14:169. doi: 10.1186/1471-2334-14-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peng E.Y., Lee M.B., Tsai S.T., Yang C.C., Morisky D.E., Tsai L.T., Weng Y.L., Lyu S.Y. Population-based post-crisis psychological distress: an example from the SARS outbreak in Taiwan. J. Formos. Med. Assoc. 2010;109:524–532. doi: 10.1016/S0929-6646(10)60087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Self-rated COVID-19 knowledge levels “very low/low” (scores 1–3), “medium” (score 4), or “very high/high” (scores 5–7) stratified by sex, age group and presence of comorbid conditions.
Self-rated COVID-19 infection likelihood levels “very low/low” (scores 1–3), “medium” (score 4), or “very high/high” (scores 5–7) stratified by sex, age group and presence of comorbid conditions.
Self-rated COVID-19 susceptability levels “very low/low” (scores 1–3), “medium” (score 4), or “very high/high” (scores 5–7) stratified by sex, age group and presence of comorbid conditions.
Self-rated COVID-19 dangerousness levels “very low/low” (scores 1–3), “medium” (score 4), or “very high/high” (scores 5–7) stratified by sex, age group and presence of comorbid conditions.
COVID-19 certainty of dangerousness rating “very low/low” (scores 1–3), “medium” (score 4), or “very high/high” (scores 5–7) stratified by sex, age group and presence of comorbid conditions.
Assessment of infectionlikelihoodin different situations. Meanscores (1 = extremely unlikely, 7 = extremely likely).