Abstract
COVID-19 pandemic and it's consequent biomedical waste is an unprecedented challenge worldwide. Biomedical waste generated during COVID-19 patient isolation, testing and care needs special consideration as it challenges the previous notion that only 15–20% of waste can be considered infectious. With establishment of new home quarantine facility, isolation/quarantine centres the chances of general waste getting contaminated with biomedical waste has increased exponentially. Through this systematic review the authors searched for all possible queries raised by different researchers on COVID19 waste management on Pubmed. A summary of all the different issues unique to COVID19 waste was prepared. Guidelines, rules and recommendation given by national and international agencies published till date were taken into account while trying to answer all the above questions raised by different studies. The key step in COVID19 waste management is segregation of biomedical waste from solid waste. Waste generated from COVID19 patients is like any other infectious waste, therefore creating public awareness about the COVID19 waste hazards and segregation at source is highlighted in all guidelines as a recommendation. These guidelines for management of waste generated during diagnostics and treatment of COVID-19 suspected or confirmed patients, are required to be followed in addition to existing practices under regulation. BMWM in COVID-19 context is a public health concern and is both a legal and social responsibility for all stakeholders.
Keywords: COVID-19, Biomedical waste management, CPCB Guidelines, WHO-WASH, CDC
Covid-19 waste is like any other infectious waste and the guidelines for its management, are required to be followed in addition to existing practices under regulation. BMWM in context of COVID-19 is a public health concern and is both a legal and social responsibility for all stakeholders.
1. Introduction
Health sector and allied services are battling with COVID19 pandemic with the available resources and knowledge. As of third week of March 2021, there are 121,874,133 cases of COVID19 and 2,693,946 had died due to its complications. [ 1 ] While writing this article the total number of cases in India was already around 11,474,605 with more than 3 lakhs active cases. To accommodate the severely ill COVID19 patients, asymptomatic patients were advised for home quarantine and in some cases admitted to temporarily created isolation wards. This massive case number and its consequent healthcare waste is an unprecedented challenge to the existing health services infrastructure. Central Pollution Control Board (CPCB) of India in a report to the National Green Tribunal (NGT) on June 17, 2020, had stated that 101 metric tonsof COVID19 related biomedical waste was generated per day in excess of 609 MT of other biomedical waste (including the waste generated in quarantine homes). Before the pandemic, a hospital generated 500–750 gm of BMW per bed per day. Now the amount of BMW produced have risen to 2.5–4.5 kg. This report recommended segregation of general waste from BMW to reduce the burden on incinerators designed to handle BMW. zz The authors had tried to gather relevant problems arising from the COVID19 waste and put forth the most suitable methods for its mitigation.
2. Material and method
In this literature reviewthe authors had tried to put forward solutions to problems, that might arise from COVID19 waste. Key words like COVID-19 waste, hazards, disposaland management were typed into PubmedCentral (PMC) search bar and all recent relevant studies outlining specific problem rising from COVID19 waste, were included in this study. The PMC database showed 50,000 articles till early fourth week of September of which only biomedical and solid waste related articles were chosen. National Guidelines for COVID19 waste management as per CPCB from March 2020 to July 2020 were included in this review and implementation troubleshoots were also suggested. Recommendation, guidelines and advisory of World Health Organisation (WHO), Centres for Disease Control (CDC), United States Occupational Safety and Health Administration (OSHA), European Union guidelines for COVID19 waste management and infection control practices published from January 2020 to 24 st September 2020 were included in this study. This review also highlights the issues, challenges, troubleshooting of waste management and reviews the national guidelines in the context of the current COVID-19 pandemic.
2.1. Timeline for biomedical waste management rules India
India implemented Biomedical Waste Management (BMWM) rules first in 1998 and then a more comprehensive legislation- BMWM rules, 2016 and their amendments in 2018 and 2019.[3] COVID19 was declared as a pandemic in March 2020 and India had responded with stringent guidelines from CPCB. CPCBbrought out specific guidelines for handling, treatment and disposal of waste generated during treatment, diagnosis, quarantine of COVID-19 patients on March 18, 2020, followed by fourth revision on July 17, 2020 [ 4 ].These guidelines are required to be followed by all stakeholders in addition to existing practices under BMWM Rules, 2016 as amended.
2.2. The unique challenge of the novel Corona virus (SARS CoV2)- COVID19
Knowledge of the virus nature and viability in different environment and on inanimate objects is pertinent for COVID19 waste disposal. COVID19 virus can be transmitted from human to human and also by fomites [ 5 ].SARS CoV19 can remain viable up to 72 h on plastic and metal surfaces whereas no viable virus can be detected after 24 h on cardboard and after 4 h on copper [ 6 ].Human coronavirus can remain infectious on inanimate surfaces for more than 9 days and persistence is reduced at temperature higher than 30 °C [ 7 ].As it has a lipid envelope, it is susceptible to common disinfectants (0.5% hypochlorite, 0.5% hydrogen peroxide, 2%glutaraldehyde), UV radiation, dry heat and moist heat [ 7 ].COVID19 virus can remain suspended in air for more than 3 h and can be a source of further infection [ 7 ]. As per WHO, airborne transmission of the virus can occur in health care settings where specific medical procedures, called aerosol generating procedures, generate very small droplets (≤5 μm) [ 5 ].Some outbreak reports related to indoor crowded spaces have suggested the possibility of aerosol transmission, combined with droplet transmission, for example, during choir practice, in restaurants or in fitness classes [ 5 ].
2.3. Challenges for bio medical waste management during COVID19
Every day of the COVID19 pandemic brings out a new challenge that needs troubleshooting.
-
•
Waste generated during home quarantine period are also potentially infectious. Their safe disposal needs to be addressed.
-
•
Waste generated in newly formed COVID-19 isolation wards, COVID intensive care unit ICU, quarantine homes and COVID care centres need proper management.
-
•
There is a need of safe burial or cremation of the dead COVID19 patients as this is a matter of safety and sentiment [ 8 ].
-
•
Shedding of the virus in stool, can lead to drinking water contamination if sewage lines fail to operate properly.9 , 10 Sewage overflowing in heavy rainfall and sewage flooding can cause human exposure from aerosolization from sewage water. There is also concern on long term effect on COVID 19 viral shedding in faecal matter in patients as it has environmental implications too [ 11 ].
-
•
During COVID19 pandemic, increased use of biocidal agents, detergents, liquid soaps or simple water used in washing of contaminated material possess a threat to water bodies [ 12 ].
-
•
Environmental problems that may arise from the quantity of COVID-19 waste also need to be addressed [ 13 ].
-
•
PPE is now utilised by general population, patient's attendants visiting hospitals, care centres, office staff in public and private offices, airport staffs and railway officials. These new consumers are either unaware or untrained on the potential hazard of improperly discarded protective gears and etiquettes of PPE.4 , 14 , 15
-
•
COVID 19 testing labs, Vaccine research labs might be handling a huge viral load and any mistake can be catastrophic. [ 16 ].
Real time supervision with proper infrastructure for BMWM along with implementation of existing guidelines are of paramount importance. As per CPCB, in India out of 2.7 lakh health care facilities only 1.1 lakh had complied with the 2016 BMWM and Solid Waste rules. 14 , 15 In the time of pandemic, biomedical waste and solid waste handling and safe disposal are crucial.
Definition of Biomedical waste in COVID-19 context:Biomedical waste in COVID19 context extends to waste generated during treatment, diagnosis, quarantine and home care of COVID19 patients. Solid waste is considered infectious only if it is contaminated by body fluids and secretions of COVID-19 patients (like tissues, masks, gloves etc.), otherwise uncontaminated solid waste is handled as per Solid Waste Management Rules, 2016 [ 15 ].
As COVID19 virus is infectious, adequate measures must be taken while handling the virus in lab setup. For non-propagative lab tests COVID19 is classified under BSL2 (Biosafety Level) and for viral culture assessments, under BSL3.[16]Any patient will shed the virus in respiratory secretion, saliva and aerosol generated during sneezing and coughing that contaminate surfaces, articles of daily use.[5].
2.4. WHO guidance on infection prevention and control and waste management
WHO WASH (Water, Sanitation and Health) has released guidelines for safe handling and management of COVID-19 waste on March 3, 2020 followed by revision on March 24, 2020 and April 23, 2020. The most recent guidelines published on June 29, 2020 include detail of infection control and prevention strategy for COVID-19 patient care and waste management. Any BMWgenerated must be collected in clearly labelled containers and sharp safe boxes. Adequate manpower professionally trained should be assigned for COVID-19 waste management. Onsite treatment should be preferred as much as possible to reduce mishap. When offsite waste treatment is unavoidable care should be taken for its proper disposal. Use of heavy-duty boots, splash proof aprons, goggles, masks and face shields and adherence to hand hygiene after handling waste is recommended for waste handlers. For the cleaning of environment, non-porous, surfaces effectively, at the outset clean the surfaces with water and detergent followed by a disinfectant for COVID-19 (0.1% sodium hypochlorite or 70–90% ethanol). Contact time of a minimum of 1 min is recommended for ethanol, chlorine-based products and hydrogen peroxide ≥0.5%. Thereafter disinfectant residue is rinsed off with clean water. Medical devices and equipment, laundry, food service utensils and medical waste should be managed in accordance with safe routine procedures.17 , 18
2.5. CPCB guidelines, 2020
These guidelines for are required to be followed by stakeholders in addition to existing practices under BMW Management Rules, 2016 as amended [ 4 ].These include colour categories, lab waste disposal, PPE disposal, home care waste disposal, solid waste disposal, liquid waste disposal, duties of stakeholders to troubleshoot the problems faced by health care workers and biomedical waste handlers. The fourth revision of guidelines, July 2020 were issued to provide revised guidance on segregation of general solid waste and biomedical waste from quarantine centres/home-care/healthcare facilities treating COVID-19 patients and to recommend on disposal of PPEs [ 4 ].
-
1.
Waste generated in COVID-19 isolation centres: To reduce the COVID19 contaminated waste it is advised to discard BMW contaminated with COVID-19 patients body fluids and secretions into COVID-19 waste labelled foot operated colour coded bins [Table .1 ].General solid waste should be collected separately as per SWM Rules, 2016 [ 4 ].The wet (compostable bags) and dry solid waste bags need to be tied securely in leak-proof bags, sprayed with hypochlorite solution and hand over to authorized waste collector of ULBs on daily basis, without opening them. Masks, tissues and toiletries used by COVID-19 patient can be contaminated with respiratory secretion, hence they need to be discarded into yellow colour bags [ 4 ].
COVID19 waste managementchallenges faced by isolation/quarantine centres:Training in BMWM in COVID-19 context has to be practiced with social distancing norms (small groups in halls or on-line training, or onsite training in small groups). All HCWs, individuals, groups working in hospital like doctors, nurses, technicians, sanitation workers and staff who use PPE, should be included. BMWM needs to be practiced with social distancing norms, hand hygiene, PPE, respiratory etiquettes. CPCB mobile application (App.) mandates the COVID-19 BMW colour category wise to be submitted daily to state pollution control board (SPCB). The various categories of BMW as mentioned in BMWM rules 2016 and CPCB guidelines, 2020 as amended is depicted in Table 1.
-
2.
Waste generated during Home Quarantine or Home-Care facilities: Covid-19 patients clinically assigned to as very mild/pre-symptomatic/asymptomatic can be home isolated [ 19 ]. As mentioned in SW rules 2016, general waste classified into bio-degradable, non-biodegradable and domestic hazardous waste [ 15 ]. Biodegradable waste and non-bio-degradable waste should be discarded into designated colour coded bags and collected by municipal solid waste collector of municipality or ULBs. General solid waste should comprise of general waste used by suspected quarantined persons and COVID-19 patient at homecare or home quarantine. Only the used masks, gloves and tissues or swabs contaminated with blood/body fluids of COVID-19 patients, including used syringes, medicines, etc., if any generated should be treated as biomedical waste [ 4 ].Masks worn by COVID-19 patients should be disposed in yellow biohazard bag to picked by dedicated waste handler from ULB [ 4 ]. In case the ULB has not started such facilities then the mask can be disinfected by 1% hypochlorite before discarding [ 20 ].Furthermore, it is advised to store used gloves and mask from COVID 19 negative households in paper bags for a minimum of 72 h and disposing them as general non-bio-degradable waste after mutilation [ 4 ].
-
3.
Sewage treatment facilities:Uptill now no proven case of COVID19 was linked to wastewater or sewage aerosol has been reported. Previously many studies had reported that aerosol generated in sewer lines can act as a potential source of coronavirus infection.9,10 Health care facilities with effluent treatment plants need to follow all guidelines for disinfection prior to discharge into general sewage lines. Persons working in effluent treatment plants and wastewater treatment facilities should be equipped with PPE, gloves, masks and goggles [ 4 ].Training the workers on standard precaution, respiratory etiquette, hand hygiene, etc can reduce the risk of any accidental exposure. The reuse of waste water should be avoided during pandemic [ 4 ].
-
4.
Safe disposal of personal protective equipment:To reduce volume of PPE and to prevent scarcity,it's reuse has been advised with proper precaution [21]. N95 masks can be reused for 3–4 times by the same person if stored in paper bags and kept out of reach of other people [ 22 ]. Visors and goggles are made of hard plastic hence can be disinfected by immersing in 1% sodium hypochlorite or 70% alcohol for 10 min [ 21 ]. Gloves, surgical masks should not be reused and should be discarded in proper colour coded bags after mutilation to prevent pilferage. Masks, shoe cover and head cover made of mixed material with 30–40% polyethylene plastic fibre should be discarded into yellow bags/bins for incineration. But latex gloves, full plastic PPE, splash-proof apron, plastic coverall, Hazmat suites, visors (face shields) and nitrile gloves need to be discarded into red bags for sterilisation by chemical method, microwaving or autoclaving before being recycled as plastic encapsulated bricks or plastic for road making. At Material Recovery Facilities (MRFs), discarded PPEs containing plastic should be shredded and sent to SPCB authorized plastic waste recyclers, or may be converted into refuse derived fuel (RDF) for co-processing or energy recovery (Waste to Energy Plants or for road making). When these facilities are unavailable the end product from treated PPE, gloves and other plastic materials can be sent to sanitary landfill sites [ 20 ].
-
5.
COVID19 testing labs, other testing laboratory and Vaccine research labs: COVID19 testing labs, sample collection centres and research laboratories needs to follow stringent guidelines for waste disposal. Used articles like vacutainers, viral transport media, pipettes tips, Eppendorf tubes and nasopharyngeal swabs must be pre-treated by sterilisation by autoclaving or microwaving or hydroclaving or chemical disinfection and thereafter disposed in red colour category. Foot operated colour coded bins should be lined with double bags. Maintenance of record of the volume and number of bags is the responsibility of the site in-charge [ 4 ].Pre-treatment of all lab waste must be done before handing over to waste collectors [ 3 ].Autoclaves run at 121 °C 15 psi pressure for a minimum time of30 min can sterilize cultures, stocks, sharp, blood and body fluid contaminated material and all other lab waste like plastic vials, pipette tips, and Eppendorf tubes. Waste-treatment autoclaves (pre-vacuum autoclaves) must have treatment option to treat the air released to prevent infective aerosol escaping into the environment [ 23 ]. Each autoclave run should be monitored by Bowie-Dick test, thermochromic monitoring (each run) or biological monitoring bacteria Geobacillus stearothermophilus spores (once a week). Autoclavable plastic bags or containers should be used as normal plastic bags or containers are not permeable to steam. Discard jars used to hold pipette tips, Eppendorf's tube or small tubes should be autoclavable. They should contain chemical disinfectant of appropriate dilution (1% sodium hypochlorite). Sharps should be discarded in puncture proof transparent plastic containers. Other testing lab waste can be disposed as per BMWM rules, 2016 into colour coded bags and bins. It is the legal duty of the generator to segregate waste into proper colour coded container as part of vicarious responsibility under the rules. Waste should be properly labelled, and waste disposal guidelines should be displayed at the site in easily understandable pictures/posters. Schedule for cleaning or autoclaving of all equipment should be included in the Standard Operating Procedure (SOP) and should be based on the labs daily load of waste generation. All personnel working in the lab must have knowledge of SOP and biomedical waste management. Spill kit for infectious material should be available at easily accessible places. All gauze/paper material used in absorption of spill and non-plastic PPE (mask, non-plastic/linen gown, shoe cover, cap) should be discarded into a yellow bag provided in the spill kit. If plastic PPE used then it must be discarded into red bags. Vaccination or immunization waste needs to be managed by Guidelines on management of BMW under Universal Immunization Programme, Guidance document by MoHFW; CPCB, 8 Feb 2021.
-
6.
Liquid waste disposal: As per mandate of BMWM, rules 2016, all hospital and bedded health care facilitiesneed to install effluent treatment plant (ETP) onsite [ 3 ].Non-compliance by institutes or individuals is a punishable (fine/jail)offence. WHO classifies hospital wastewater into black water (sewage), grey water (sullage from washing, rinsing, lab processes, laundary) and storm water (from rainfall) [ 24 ].Hospital wastewater can contain drugs, disinfectants, chemicals, etc. COVID19 is a respiratory virus but can possibly contaminate all wastewater sources while patients spit, rinse mouth, bathe, urinate and defecate. If this wastewater is released into the surrounding it can pollute the environment and can be a potential source of infection. Liquid lab waste consists of blood, body fluids, sputum, vomit, urine, and viral transport media used for transporting viral samples. Pre-treatment of liquid lab waste can be done byacid-base neutralization, filtration and sedimentation, or autoclaving [ 24 ].In hospitals with ETP chemical wastewater should be collected with separate drainage system leading to ETP [ 3 ].It is advised not to reuse the treated wastewater for flushing purposes during COVID-19 pandemic [ 4 ].
-
7.
Waste handlers, waste handling facilities: In house COVID-19 waste transport should be done in closed trolleys with easy manoeuvrable wheels and labelled with COVID-19 waste. These trolleys should be disinfected regularly. All biomedical waste bags should be double-layered, non-chlorinated, leakproof, labelled COVID-19 waste and barcoded and then handed over to CBWTF. All areas involved in COVID19 case management should be provided and serviced only with COVID19 WASTE labelled bins, bags and containers [ 4 ]. Waste handlers should be equipped with PPE as mentioned earlier. All waste handlers to be trained with infection prevention measures such as hand hygiene, respiratory etiquettes, social distancing, use of appropriate PPE, etc. via videos and demonstration in local language at regular interval. Designated nodal officer for BMWM of the facility should carry out these trainings [ 4 ].
-
8.
Treatment of biomedical waste: At the CBWTF level, waste collected in yellow bags should be incinerated. Waste collected in red bags are recycled after following sterilisation by chemical sterilisation/microwaving/autoclaving/hydroclaving. Blue plastic boxes containing metal and glass to be sterilised by autoclaving/chemical sterilisation [3].Finally, all the material produced by autoclaving/microwaving/hydroclaving/chemical disinfection should be shredded and handed over to authorised recyclers and thereafter, finally given at material recovery facility. Ash produced by incineration should be used in landfill.3,4
-
9.
Monitoring system:Stringent record keeping of waste created, bags tagged with barcodes and GPS and regular visit to monitor compliance at all levels internally by internal BMWM auditors and also externally by SPCB are all necessary steps to monitor compliance. It is the responsibility of the authority creating newer facilities for COVID19 isolation and quarantine to create the channel of communication to establish smooth biomedical waste collection by the licensed CBWTF or install in house equipment for biomedical waste treatment. They should appoint a nodal officer designated for biomedical waste management [4]. CPCB has created an app ‘COVID19BWM’ for daily updates on COVID19 waste management and follow-up [ 4 ].
-
10.COVID-19 WASTE management duties of different governing bodies [ 4 ].
-
a)Duties of CBWTF: Adequate training and protective gear should be provided to the sanitation worker. Over 50-year-old sanitation workers should only work in processing non-COVID waste. Strict record of all COVID-19 waste collected and processed must be kept. All COVID-19 waste must be processed or treated on the very same day it gets collected. Vehicles, trolleys, and storage areas must be sanitized daily with 1% sodium hypochlorite. Daily report should be updated unto the COVID-19 tracking app.
-
b)Duties of SPCBs: It is the duty of SPCB to facilitate the operation of care homes, quarantine centres by reducing hassle for certification. Communication between all isolation camps/quarantine homes and CBWTF must be established and monitored. Violations by any of the participants are dealt under BMWM rules 2016 as amended.
-
c)Duties of ULBs: ULBs are responsible for awareness, safe collection and transport of all waste from waste generating facility to CBWTF. They must create different teams for doorstep collection of BMW which will prevent any mixing of COVID19 waste with nonCOVID19 waste. Sanitation workers must be provided with adequate training and protective gear.
-
a)
Table 1.
Colour Categories of BMW as per BMWM rules, 2016, amendments 2018,2019 and CPCB guidelines 2020.
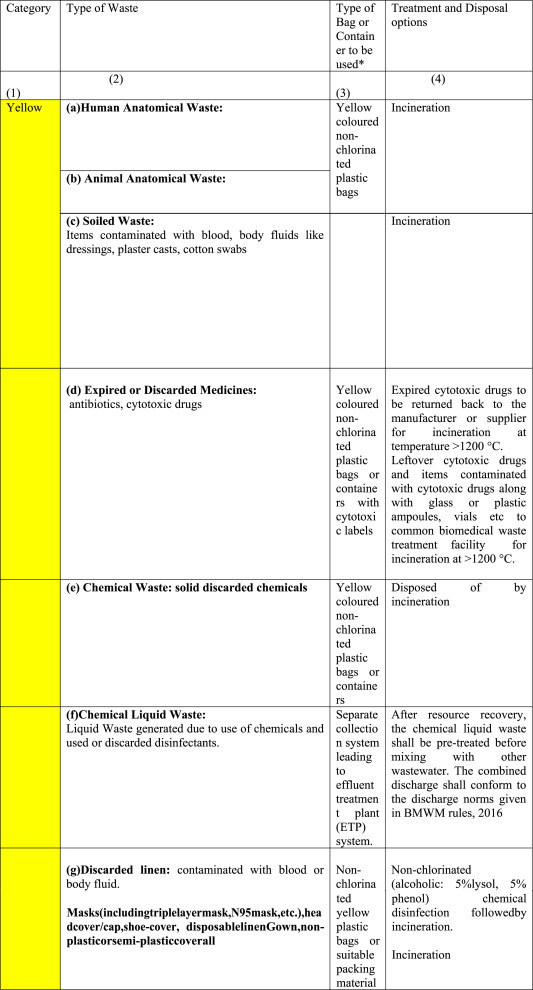
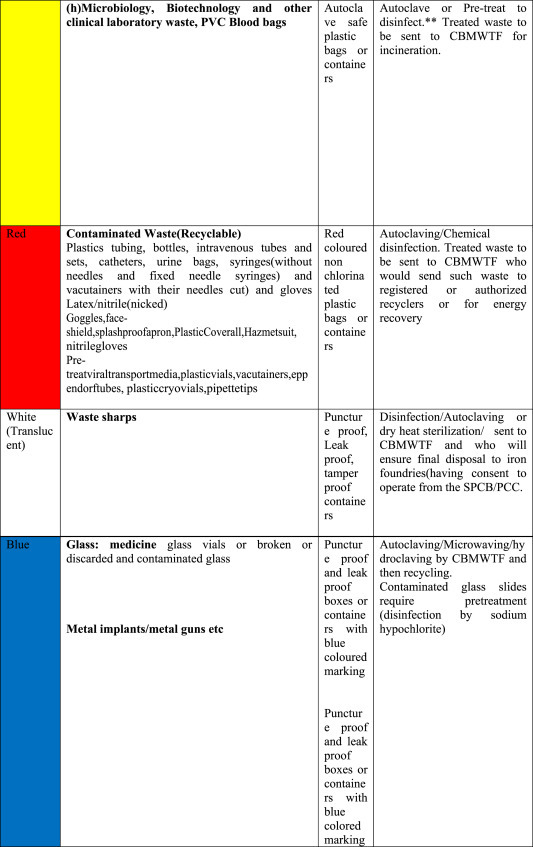
∗Barcode label will have to be made available on every bag or container as per CPCB guidelines.
∗∗For disinfection of BMWM articles freshly prepared 1–2% Sodium hypochlorite is recommended.
∗∗∗1% Sodium hypochlorite is 1:100 dilution (525–615 ppm of available chlorine).
∗∗∗∗Hospital supply of sodium hypochlorite is 10% or 4% (please see label and manufacturers instructions).
∗∗∗∗∗All lab waste: patient's samples, blood bags, toxins, live and attenuated vaccines, cultures (liq/solid), devices used to transfer cultures need pretreatment by autoclaving/microwaving/hydroclaving etc-then their respective category plastic (red)/glass (blue).
2.6. Safe disposal of dead bodies of unknown/suspected/confirmed cases of COVID19 patients
Incineration of the dead bodies is not mandatory in COVID19 patients [ 25 ].To date no evidence of patients exposed to confirmed COVID19 patient's dead body, has been reported. Risk of infection from dead bodies might be low but safe handling is advised. Dead bodies should be packed in a body bag whose exterior is sanitized with 1% hypochlorite. PPE, gloves, masks, gowns and goggles to be used during handling of dead bodies [ 26 ].Burial possess no additional threat to environment. Ash produced after cremation can be collected by the families as it possesses no additional threat. Morgue, vehicles used for transportation should be sanitized with 1% hypochlorite [ 17 , 26 ] .
PPEs doffed by HCWs accompanying diseased body of COVID-19 patient to crematorium should be treated as BMW and disposed as per provisions under BMWM Rules, 2016. Crematoriums may opt for disposal of such PPEs: in yellow-bag and handed over to authorized waste picker engaged by of ULBs or HCWs to take-back the PPEs after collecting it in red and yellow bags/bins provided in the hospital ambulance or to doff the PPEs at the mortuary of concerned hospital [ 4 ].
2.7. International guidelines for COVID-19 waste management (Table 2)
Table 2.
Comparison of country or state or organization specific international guidelines with CPCB guidelines, 2020 as amended.
| Country/organisation | Covid-19 waste category and management | References |
|---|---|---|
| WHO | All COVID-19 waste should be collected in designated COVID-19 waste containers and preferably treated onsite. When on-site treatment, option is not available offsite transport can be done under strict supervision. Hand hygiene is must after handling COVID-19 waste [27]. | 17 |
| US (OSHA) | OSHA guidelines state that COVID19 waste possess no extra threat and should be handled as any biomedical waste. SARS CoV-2 contaminated general municipality waste also should be treated as non-contaminated general waste. PPE, gloves, masks must be worn all time while handling COVID-19 waste. [43] | 28 |
| EU | Masks worn by COVID-19 confirmed orsuspected cases should be collected separately from the care takers and family members in paper bags. These bags can be handed over to the professional COVID-19 waste handling facilities through designated COVID-19 waste collectors. [44] | 29 |
| Italy | Italian authorities divided waste into T1 and T2. Waste collected from homes with COVID-19 patients is classified as T1 and is considered infectious. Waste from all other homes without any COVID-19 patient, are under T2 category. T1 waste should be collected in double layered and requires no at source separation. No elderly person should be employed in handling of T1 waste. T2 waste can be collected and treated as per normal municipality waste. [ | 30 |
| Centre for Disease Control (CDC) | Waste generated during COVID-19 patient management is no different than waste generated by any other patient treatment. They are not considered category A waste should be treated as regulated medical waste (RMW). | 27 |
| Texas Commission on Environmental Quality (TCEQ)[31] | As per CDC guidelines TCEQ had categorised COVID-19 waste as RMW. With all safety precaution COVID-19 waste should be treated as RMW and hand hygiene to be performed after handling. | 31 |
| California Department of Public Health (CDPH)[32] | Medical Waste Management Program (MWMP) had categorised COVID-19 waste as RMW (as per CDC). No extra steps required for COVID-19 waste handling. | 32 |
| CPCB (India) | A double-layered bag (2 bags) should be used for the collection of waste from COVID-19 isolation wards to ensure adequate strength and no leaks. Prior to handling over to Common Bio-medical Waste Treatment Facility (CBWTF), Collect and store biomedical waste separately. There should be a separate record of waste generated from COVID-19 isolation wards. The waste collection bags, bins, trolleys should be marked as ‘COVID-19 waste’. The labeling is to ensure the priority treatment and disposal immediately upon receipt at CBWTF. Only laboratory waste is to be pretreated on site, rest waste is treated at CBWTF level. | 4 |
Guidelines implemented worldwide for COVID-19 waste management like WHO, CDC, OSHA CPCB recommend that COVID-19 waste poses no extra threat than any other biomedical waste and advise to handle it as any other infectious waste (Table 2). Briefly, the following guidelines are discussed:
CDC:As per Centre for Disease Control waste from COVID 19 patients is not a A category infectious waste so BMW from potential or known COVID-19 virus contamination should be managed like any other regulated medical waste (RMW) with assurance of safe work practices and PPE utilization to prevent waste worker from waste stream exposure [27].
United States- OSHA (Occupational Safety and Health Administration) and other state guidelines mentioned COVID-19 waste posing no extra threat than any other biomedical waste and advised to handle as other BMW. COVID19 contaminated solid/general waste should be processed as any other solid waste. Strict maintenance of safe engineering practices, wearing of personal protection gear is also advised while handling waste [28].
Europe: COVID-19 patients staying at home were advised to keep a paper bag in the same room to discard used masks. Care takers and family members must keep separate paper bag to discard masks worn by them. These bags can then be handed over to waste collectors. All waste bags must be double layered to reduce any leaking to the environment [ 29 ].
Italy: Waste was categorised into T1 (Municipal waste generated by households with COVID-19 positive people in isolation or people in mandatory quarantine) and T2 (Municipal waste generated by households without COVID-19 positive people in isolation or people in mandatory quarantine). T1 waste is considered as infectious waste and has to be picked up by specific agencies dealing this type of waste [30].
3. Conclusion
Recent revisions and review in national and international guidelines were specific for COVID19 waste management include the new isolation facilities, laboratories, camps, and care homes [ [4], [27], [28], [29], [30], [31], [32] ]. Stringent compliance to the established rules, guidelines and identification of newer support areas are warranted, that can help in reducing the burden and in preventing potential outbreak. Just as for COVID19 management “Identify Isolate and Treat” the same goes for COVID19 waste identify the generator, isolate i.e., manage separately in covid19 waste designated bins, trolleys, and finally treat the waste adequately. The essential principle of BMWM rules in COVID-19 context remain essentially the same based on WHO core principles and with focus on non-burn technologies for BMWM using the best available practices and best available techniques. COVID 19 waste is an important public health concern, therefore it is a legal and a social responsibility of all stakeholders. Furthermore, without active stakeholders including citizens participation and cooperation, intermixing of biomedical waste with solid waste can endanger the occupational safety of HCWs, society and environment.
Source(s) of support
No outside support was taken for writing this article.
Conflicting interest (if present, give more details)
Authors declare no conflict of interest.
References
- 1.WHO Coronavirus disease (COVID-19) weekly epidemiological update and weekly operational update. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports Published on September 21. (Accessed September 24, 2020)
- 2.Compliance Status Report by CPCB in OA 72 of 2020 (In Re Scientific Disposal of Bio-Medical Waste Arising Out of COVID-19 Treatment- Compliance of BMW Rules. 2016. https://greentribunal.gov.in/sites/default/files/news_updates/Complaince/statusreport%20.pdf Published on July 18, 2020. Available at. (Accessed on September 15,2020) [Google Scholar]
- 3.MOEF & FF: BMWM Rules Gazette of India, extraordinary, Part II. Section. 2016;3(i):1–37. http://www.egazette.nic.in/WriteReadData/2016/168832.pdf Published on March 28,2016. Available at: (Accessed June 20, 2020) [Google Scholar]
- 4.MOEF& FF: Central Pollution Control Board. (Revision 4) Guidelines for Handling, Treatment and Disposal of Waste Generated during Treatment/Diagnosis/ Quarantine of COVID-19 Patients. Published on July 17, 2020. Available at:https://cpcb.nic.in/uploads/Projects/Bio-Medical-Waste/BMW-GUIDELINES-COVID_1.pdf(Accessed July 18, 2020).
- 5.WHO & FF . 2020. Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions.https://www.who.int/publications/i/item/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations Published on July 9. (Accessed July 11, 2020) [Google Scholar]
- 6.van Doremalen N., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382(16):P1564–P1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.01.022. https://www.sciencedirect.com/science/article/pii/S0195670120300463 Available at. (Accessed on June 13, 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yaacoub S., Schünemann H.J., Khabsa J., et al. Safe management of bodies of deceased persons with suspected or confirmed COVID-19: a rapid systematic review. BMJ Global Health. 2020;5 doi: 10.1136/bmjgh-2020-002650. https://gh.bmj.com/content/bmjgh/5/5/e002650.full.pdf Available at. (Accessed on June 18, 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tang A., Tong Z.D., Wang H.L., Dai Y.X., Li K.F., Liu J.N., Wen-jie Wu W., Yuan C., Yu M., Li P., Yan J.B. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg. Infect. Dis. 2020;26(6):P1341–P1343. doi: 10.3201/eid2606.200301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lodder W., de Roda Husman A.M. SARS-CoV-2 in wastewater: potential health risk, but also data source. The lancet. Gastroenterol. Hepatol. 2020;5(6):P533–P534. doi: 10.1016/S2468-1253(20)30087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quilliam R.S., Weidmann M., Moresco V., Purshouse H., O'Hara Z., OliverCOVID-19 D.M. The environmental implications of shedding SARS-CoV-2 in human faeces. Environ. Int. 2020;140:105790. doi: 10.1016/j.envint.2020.105790. (Accessed June 13, 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nghiem Long, Morgan Branwen, Donner Erica, Short Michael. 2020. The COVID-19 Pandemic: Considerations for the Waste and Wastewater Services Sector. Case Studies in Chemical and Environmental Engineering.https://www.sciencedirect.com/science/article/pii/S2666016420300049?via%3Dihub Available at. (Accessed on 28 June 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saadat S., Rawtani D., Hussain C.M. vol. 728. 2020. https://www.researchgate.net/publication/340863634_Environmental_perspective_of_COVID-19 (Environmental Perspective of COVID-19 Sci. TotalEnviron.). Article 138870. Available at. (Accessed June 11, 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.NGT National Green Tribunal Order regarding COVID-19 waste management dated 24/04/2020. https://cpcb.nic.in/uploads/Projects/Bio-Medical-Waste/NGT_Order_covid_28.04.2020.pdf Published on Available at. (Accessed on June 23,2020)
- 15.MOEF & CC: Solid Waste Management Rules . 2016. The Gazette of India: Extraordinary. Part II, 3(ii; pp. 8–12.http://www.egazette.nic.in/WriteReadData/2016/169079.pdf Published on April 8, 2016. Available at: (Accessed June 20, 2020) [Google Scholar]
- 16.WHO Laboratory biosafety guidance related to the novel coronavirus (2019-nCoV) Interim guidance. https://www.who.int/docs/default-source/coronaviruse/laboratory-biosafety-novel-coronavirus-version-1-1.pdf?sfvrsn=912a9847_2 Published on February 12, 2020. Available at. (Accessed September 18, 2020)
- 17.WHO . 2020. Infection Prevention and Control during Health Care when Coronavirus Disease (COVID-19) Is Suspected or Confirmed.https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-2020.4 (June):1–13. Published on June 29, 2020). Available at. (Accessed July 12, 2020) [Google Scholar]
- 18.WHO Water, sanitation, hygiene, and waste management (WASH) for the COVID-19 virus: interim guidance. https://www.who.int/publications/i/item/water-sanitation-hygiene-and-waste-management-for-the-covid-19-virus-interim-guidance Published on April 23, 2020. Available at. (Accessed September 15, 2020)
- 19.Government of India, Ministry of Health & Family Welfare Revised guidelines for Home Isolation of very mild/pre-symptomatic/asymptomatic COVID-19 cases. https://www.mohfw.gov.in/pdf/RevisedHomeIsolationGuidelines.pdf Published on July 2, 2020. Available at. (Accessed on June 20, 2020)
- 20.MOHFW Guidelines on use of masks by public. https://www.mohfw.gov.in/pdf/Useofmaskbypublic.pdf Published on March 11, 2020. Available at. (Accessed September 20, 2020)
- 21.MOHFW India Advisory on re-processing and re-use of eye-protection – Goggles. https://www.mohfw.gov.in/pdf/Advisoryonreprocessingandreuseofeyeprotectiongoggles.pdf Published on May 27, 2020. Available at. (Accessed June 28, 2020)
- 22.The National Institute for Occupational Safety and Health Niosh Recommended guidance for extended use and limited reuse of N95 filtering facepiece respirators in healthcare settings. https://www.cdc.gov/niosh/topics/hcwcontrols/recommendedguidanceextuse.html available at. (Accessed June 28, 2020)
- 23.Capoor M.R., Bhowmik K.T. Current perspectives on biomedical waste management: rules, conventions and treatment technologies. Indian J. Med. Microbiol. 2017;35:157–164. doi: 10.4103/ijmm.IJMM_17_138. [DOI] [PubMed] [Google Scholar]
- 24.Chartier Y., Emmanuel J., Pieper U., Prüss A., Rushbrook P., Stringer R., Townend W., Wilburn S., Zghondi R. second ed. WHO); 2014. Safe Management of Wastes from Health-Care Activities. [Google Scholar]
- 25.Who Infection prevention and control for the safe management of a dead body in the context of COVID-19: interim guidance. 2020. https://www.who.int/publications/i/item/infection-prevention-and-control-for-the-safe-management-of-a-dead-body-in-the-context-of-covid-19-interim-guidance Published on September 4. (Accessed on September 20, 2020)
- 26.MOHFW India Guidelines on dead body management. https://www.mohfw.gov.in/pdf/1584423700568_COVID19GuidelinesonDeadbodymanagement.pdf Published on March 15, 2020. Available at. (Accessed on June 21, 2020)
- 27.CDC Coronavirus disease 2019 (COVID19) waste management. https://www.cdc.gov/coronavirus/2019-ncov/hcp/faq.html#Waste-Management Published on August 4, 2020. Available at. (Accessed June 30, 2020)
- 28.OSHA and the U.S. Department of Health and Human Services (HHS) guidelines on COVID-19 control and prevention. https://www.osha.gov/SLTC/covid-19/controlprevention.html#solidwaste Available at. (Accessed June 22, 2020)
- 29.European guidelines on Waste management in the context of the coronavirus crisis. https://ec.europa.eu/info/files/wastemanagement-contextcoronavirus-crisis_en Available at. (Accessed June 22, 2020)
- 30.Italian guidelines on classification of waste. https://www.snpambiente.it/2020/03/24/emergenza-covid-19-indicazionisnpasulla-gestione-deirifiuti Available at. (Accessed June 22, 2020)
- 31.TECQ Disposal of coronavirus (COVID-19) contaminated waste. https://www.tceq.texas.gov/downloads/response/covid-19/coronavirus-disposal-contaminated-waste-2020-07-01.pdf Published on July 1, 2020. Available at. (Accessed June 15, 2020)
- 32.CDPH COVID-19 medical waste management. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/MedicalWasteManagementInterimGuidelines.aspx Published on March 16, 2020. Available at. (Accessed on June 20, 2020)


