Abstract
Objectives
To determine patterns of mask wearing and other infection prevention behaviours, over two time periods of the COVID-19 pandemic, in cities where mask wearing was not a cultural norm.
Methods
A cross-sectional survey of masks and other preventive behaviours in adults aged ≥18 years was conducted in five cities: Sydney and Melbourne, Australia; London, UK; and Phoenix and New York, USA. Data were analysed according to the epidemiology of COVID-19, mask mandates and a range of predictors of mask wearing.
Results
The most common measures used were avoiding public areas (80.4%), hand hygiene (76.4%), wearing masks (71.8%) and distancing (67.6%). Over 40% of people avoided medical facilities. These measures decreased from March–July 2020. Pandemic fatigue was associated with younger age, low perceived severity of COVID-19 and declining COVID-19 prevalence. Predictors of mask wearing were location (US, UK), mandates, age <50 years, education, having symptoms and knowing someone with COVID-19. Negative experiences with mask wearing and low perceived severity of COVID-19 reduced mask wearing. Most respondents (98%) believed that hand washing and distancing were necessary, and 80% reported no change or stricter adherence to these measures when wearing masks.
Conclusion
Pandemic mitigation measures were widely reported across all cities, but decreased between March and July 2020. Pandemic fatigue was more common in younger people. Cities with mandates had higher rates of mask wearing. Promotion of mask use for older people may be useful. Masks did not result in a reduction of other hygiene measures.
Keywords: Mask use, Pandemic fatigue, COVID-19, Risk mitigation, Health behaviours, Health policy
Introduction
In the absence of a vaccine, non-pharmaceutical measures such as physical distancing, wearing masks and hand hygiene have been key to controlling COVID-19 during the first year of the pandemic (Seale et al., 2020). Whilst Asian countries have a longer history of wearing masks for both infection and pollution, especially after SARS (2003) (Burgess and Horii, 2012, Sin, 2016), the use of masks in the community is not a cultural norm in Western countries (MacIntyre and Chughtai, 2015), and mask wearing was initially discouraged, whilst handwashing was promoted.
As the pandemic unfolded, many countries mandated mask wearing during different stages of the pandemic. In New York City, an executive order was introduced on 15 April 2020 (close to the peak of the first wave) mandating face coverings in public settings where physical distancing was not possible (Government of New York State, 2020). Likewise, Phoenix declared mandatory mask use from 20 June 2020 (before the epidemic peak) (Phoenix City Hall, 2020). In Sydney, masks were not mandated but guidance was updated in June 2020 to recommend mask use when physical distancing was not possible (e.g. on crowded public transport) (New South Wales Department of Health, 2020). London initially had no mask wearing recommendation but a mandate was issued on 24 July 2020 for all public indoor spaces (London City Hall, 2020). In Melbourne, a second wave in July resulted in a mask mandate on 23 July 2020 (Department of Health and Human Services Victoria, 2020a).
There has also been changing guidance over time about community use of face masks from health agencies such as the World Health Organization (WHO) and the Department of Health Australia, the US Centers for Disease Control and Prevention and Public Health England (Australian Government Department of Health, 2020; CDC, 2020; Chan et al., 2020; Government of the United Kingdom, 2020a). Initial reluctance to recommend masks and active advice to not wear masks may have been influenced by global shortages of masks (MacIntyre and Wang, 2020). The WHO also expressed concern that the use of facemasks may give people a false sense of security and lead to reduction of other infection control measures such as hand washing and physical distancing (World Health Organization, 2020).
As the pandemic progressed, evidence accumulated to show that around 40–45% of infections were asymptomatic (Oran and Topol, 2020). This means that infections cannot be readily identified and infected people may be unaware that they are infected, which increases the utility of universal masking. The available evidence on mask use in the community showed a net protective effect of masks (Chu et al., 2020, MacIntyre and Chughtai, 2020).
There may have also been fatigue with social restrictions, mask mandates and other risk-mitigation measures over a long period of the pandemic, yet there are no data to better understand this. It is therefore important to gather evidence about community understanding, experiences and practices around the use of masks and other risk-mitigation measures during the pandemic in settings with different disease incidence and policies. It is also important to understand whether mask use affects other risk-mitigation behaviours. This study aimed to provide insights into mask wearing and other infection prevention behaviours over two time periods of the pandemic in five cities where mask wearing was not a cultural norm.
Methods
Study design
A cross-sectional survey was conducted in five cities from three countries without a culture of mask wearing. These cities were selected to represent a spectrum of low, medium and high incidence of COVID-19, and a range of policies towards community mask use (ranging from a mask mandate to no mandate), with a population of at least 5 million. The cities were classified as low incidence (<1 case per 100,000), medium incidence (1–10 cases per 100,000) and high incidence (>10 cases per 100,000), based on COVID-19 incidence at the start of the survey in July 2020. Adults aged ≥18 years, of any gender, living in the selected cities in 2020 and willing to consent were included in the study, with sampling proportionate to population size.
Recruitment and enrolment
A market research company, Dynata (Dynata, 2020), randomly distributed the survey link by email to a representative sample of their panel members in Sydney, London, Melbourne, Phoenix and New York City. An algorithm using geolocation was used to screen and identify eligibility to take part in the survey. Dynata’s worldwide consumer research panel includes over 60 million people from over 94 countries, including Australia, the United Kingdom (UK) and United States (US), who have been profiled on demographic and health attributes (Dynata, 2020). Panel members undergo a verification process to ensure reliability and accuracy of responses and to avoid duplicate participants. Data provided from panel members undergo regular quality checks, such as participation limits, screening questions, digital fingerprinting, and capturing and removing participants who provide illogical responses or do not spend sufficient time on surveys. No identifying information is provided or collected.
Panel members who chose to open the survey link were screened for inclusion based on age and location. Participants who met the inclusion criteria were directed to a participant information and consent page, which provided details about the research study, and had to provide consent to proceed with the online survey. Failure to complete the entire survey was considered withdrawal of consent. The survey was launched on 10 July and closed on 27 July 2020. The survey collected data on sociodemographics, risk factors for COVID-19, attitudes towards non-pharmaceutical interventions, adoption of and experiences with mask use, infection control behaviours and attitudes (Appendix Table 1) in people aged ≥18 years in Australia, the UK and the US. It took about 10–15 minutes to complete the survey. Questions on risk-mitigation behaviours and mask wearing were asked about the early period of the pandemic (March–April 2020) and at the time of survey (July 2020). Data were collected using a web-based survey platform, Redcap.
Sample size
The study was powered a priori to identify a 20% difference in the rate of mask use between cities with (New York and Phoenix) and without mask mandates (Sydney, Melbourne and London) with 95% confidence and 80% power. A mask use prevalence of 60% was assumed among cities without mask mandate and 80% among cities with mask mandate (Babalola et al., 2020, Jones, 2020) and a sampling ratio of 0.3, yielding a minimum required sample size of 194. Hence, this study aimed to recruit a total of 2150 participants, from which the samples were selected proportionate to population size, age and gender distribution of the sampled cities (i.e. 200 people from Sydney, 150 from Melbourne, 300 from London, 1200 from New York City and 300 from Phoenix). Post-hoc power analysis was conducted via large sample approximation using G*Power 3.1.9.7 (Faul et al., 2009). In a two-sided test with α = 0.05, the recruited sample size (N = 2343) enabled detection of at least 20% difference in mask use (i.e. odds ratio of 1.2), yielding a power of 94.1%.
Data coding
For sociodemographic and health-related multiple-choice questions, answers were coded as ordinal variables if one option was allowed or separate binary variables for each option if multiple options were allowed. Participants were asked to rank their confidence in the government and their trust in COVID-19 information provided by the government using a Likert scale of 0–4, where 4 represented the highest level of trust or confidence and 0 was none at all. In logistic regression, ratings of 3–4 were coded as 1 (high) and ratings <3 were coded as 0 (low). Pandemic fatigue was coded as present if a participant reported a net decline in number of protective measures in July 2020 compared with March–April 2020. Mask mandate was coded as present for cities with a mandatory mask policy implemented before 27 July 2020 and absent for others. Cities were classified as either experiencing a declining in cases in July 2020 compared with March 2020 (Sydney, London and New York) or not (Melbourne and Phoenix).
Data analysis
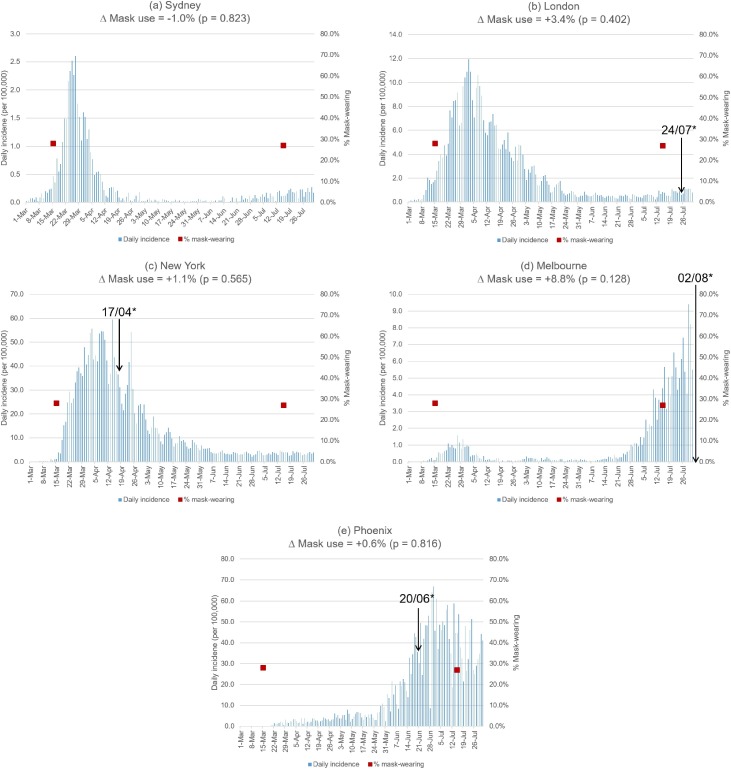
Descriptive statistics were performed for variables relating to mask use, perception and experience of masks, and other infection control behaviours such as hand washing and physical distancing. In order to interpret results according to the epidemiology of COVID-19 at the time of the survey, epidemic curves were plotted based on daily reported COVID-19 cases from respective Departments of Health (Arizona Department of Health Services, 2020, Data.NSW, 2020, Department of Health and Human Services Victoria, 2020b, Government of the United Kingdom, 2020b, New York State Department of Health, 2020). The change in percentage of participants reporting wearing masks between March–April and July 2020, and dates of mask mandate policy from official guidelines (Department of Health and Human Services Victoria, 2020a, Government of New York State, 2020, London City Hall, 2020, New South Wales Department of Health, 2020, Phoenix City Hall, 2020) were compared relative to the epidemic curves.
Statistical analyses were performed to detect significant inter-city differences in health status, mask use, experience of mask shortages, and other health behaviours during the COVID-19 pandemic. The Chi-square test was used for binary variables, one-way ANOVA test for continuous variables, and Kruskal–Wallis H test for ordinal variables. A two-sample proportional test was used to compare percentage mask use between March–April and July 2020 and between age groups. Statistical significance was defined at α-level of 0.05.
Univariate and multivariate logistic regression were used to identify predictors of mask use and pandemic fatigue. All data were cleaned prior to analysis. Analysis was completed using Stata version 14 (Stata Corporation, College Station, TX, USA).
Results
A total of 2343 people from the greater metropolitan areas of each city were surveyed: 200 from Sydney, 148 from Melbourne, 291 from London, 1204 from New York City and 500 from Phoenix. Trust in state or local government was higher than trust in national government (Table 1 ), and trust in government was generally higher in Australia than the UK or US (Appendix Table 4). The mean age was 50.8 ± 17.8. Participants were younger in Sydney (45.3 ± 15.8), London (45.2 ± 15.6) and Melbourne (46.7 ± 17.9). More than half of the participants (n = 1,288, 55.0%) had at least one comorbidity (Appendix Table 2). Mask use between March and July 2020 relative to the epidemic curve in each city is shown in Figure 1 . The average incidence per 100,000 population between March–April 2020 was 0.33 for Melbourne, 0.61 for Sydney, 1.79 for Phoenix, 5.10 for London and 25.98 for New York.
Table 1.
Reported mask use, experience with COVID-19 and beliefs about health/mask use.
| Mask use patterns and behaviours | (N = 2343) | |
|---|---|---|
| Mask use for any reason | 1700 | (72.6%) |
| Mask use during COVID-19 pandemic | 1683 | (71.8%) |
| Adherence to government guideline on masks | ||
| Always followed guidelines | 1561 | (66.6%) |
| Sometimes followed guidelines | 422 | (18.0%) |
| Wore mask even before guidelines | 184 | (7.9%) |
| Did not follow guidelines | 176 | (7.5%) |
| Prior experience with masks | (N = 1700) | |
|---|---|---|
| Other reasons for past use of masks | ||
| Cleaning or dusting | 306 | (18.0%) |
| Work requirement | 216 | (12.7%) |
| Building/home repairs | 200 | (11.8%) |
| Bushfire or wildfire smoke | 82 | (4.8%) |
| Any negative issues faced while wearing masks | 382 | (22.5%) |
| Feeling embarrassed | 141 | (8.3%) |
| Being stared at | 93 | (5.5%) |
| Receiving negative comments | 88 | (5.2%) |
| Receiving racist comments | 56 | (3.3%) |
| Being mistaken as being infected | 51 | (3.0%) |
| Being laughed at | 40 | (2.4%) |
| Change in other risk reduction measures during the pandemic | (N = 1683) | |
|---|---|---|
| No change | 991 | (58.9%) |
| More strict on other behaviours | 335 | (19.9%) |
| Less strict on hand washing only | 155 | (9.2%) |
| Less strict on physical distancing only | 138 | (8.2%) |
| Less strict on both hand-washing and physical distancing | 60 | (3.6%) |
| Experience with COVID-19 | (N = 2343) | |
|---|---|---|
| Experiencing chest infection, cold or flu-like illness in March–June 2020 | 293 | (12.5%) |
| Tested for COVID-19 | 609 | (26.0%) |
| Tested because of contact with a case, without falling sick | 149 | (6.4%) |
| Tested after falling sick | 147 | (6.3%) |
| Tested for other reasons | 313 | (13.4%) |
| Diagnosed with COVID-19 | 123 | (5.2%) |
| Knowing a family member, friend or colleague who was diagnosed with COVID-19 | 874 | (37.3%) |
| Risk and efficacy perception | (N = 2343) | |
|---|---|---|
| Health self-rating (1–100) | 66.6 ± 20.2 | |
| Perceived severity of COVID-19 (1–100) | 62.0 ± 25.2 | |
| Perceived risk of contracting COVID-19 (1–100) | 54.8 ± 23.5 | |
| Perceived effectiveness of masks (1–100) | ||
| N95/P2 masks | 66.5 ± 21.5 | |
| Surgical masks | 60.8 ± 21.9 | |
| Cloth masks | 54.1 ± 22.5 | |
| Perception of other preventive behaviours while wearing masks | ||
| Need to wash hands | 1647 | (97.9%) |
| Need to maintain 1.5-m distance from others | 1641 | (97.5%) |
| Confidence in national government (Likert 0–4) | 2 | (1–3) |
| Confidence in state/local government (Likert 0–4) | 3 | (2–3) |
| Trust in COVID-19 information from national government (Likert 0–4) | 2 | (1–3) |
| Trust in COVID-19 information from state/local government (Likert 0–4) | 2 | (2–3) |
*Statistically significant at α = 0.05.
Note: (a) Percentages may not add up to 100% in some questions because participants could choose more than one options.
(b) Mean ± SD were reported for sliding scale (1–100; 1 = minimum and 100 = maximum) questions. Median (IQR range) were reported for Likert scale (0–4) questions.
Figure 1.
Daily COVID-19 incidence (per 100,000) and temporal change in population reported wearing masks (%), by city.
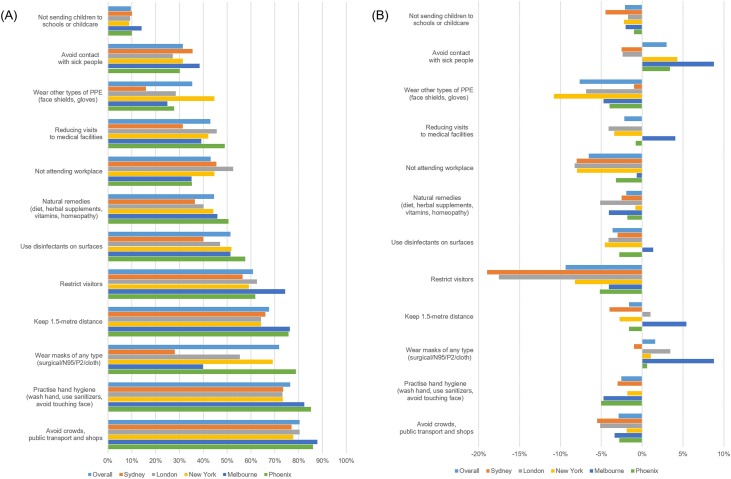
Pandemic fatigue
Participants reported adopting a wide range of measures in March–April 2020 (early stages of the pandemic) and later (July 2020) to reduce the risk of COVID-19 (Figure 2 ). The most common measures early in the pandemic were: avoiding crowded areas, public transport and physical shops (80.4%), practicing hand hygiene (washing hands, using hand sanitizers, not touching face) (76.4%), wearing masks (71.8%), physical distancing (67.6%), restricting visitors (60.9%), reducing visits to medical facilities (42.9%) and avoiding contact with sick people (31.5%). There was a consistent decrease reported in almost all risk-mitigation behaviours between March–April 2020 and July across the cities (Figure 2). However, mask use increased in all cities except Sydney, where it decreased. Melbourne, which was in the midst of a second wave at the time of the survey, had an increase in wearing masks, avoiding contact with sick individuals and medical facilities, and physical distancing.
Figure 2.
Frequency of COVID-19 risk-control measures in March–April 2020 early in the pandemic (A) and percentage changes of these measures by July 2020 (B).
Behaviours and experiences with masks
Table 1 shows that 1683 participants (71.8%) reported wearing a mask of any type during the COVID-19 pandemic. Prevalence of wearing masks was significantly lower in Sydney (45.5%) and Melbourne (51.4%), and higher in London (70.8%), Phoenix (75.6%) and New York (77.4%) (p < 0.001). Overall, mask use among participants ≥50 years old was significantly lower than that of people aged <50 years (p = 0.0150), but the difference was not significant in New York (p = 0.0945), Phoenix (p = 0.0955) and Melbourne (p = 0.2667) (Appendix Table 3). Compared with the overall prevalence (55.3%), cloth mask use was higher in Phoenix (75.4%) and much lower in Sydney (16.8%) (Appendix Table 4). Table 1 also shows that most participants did not report any negative issues while wearing masks (n = 1318, 77.5%). Reported problems included receiving negative or racist remarks (n = 144, 8.5%), embarrassment (n = 141, 8.3%), being stared or laughed at (n = 133, 7.8%), or being mistaken for being sick (n = 51, 3.0%). Almost all participants believed that when wearing a mask, they also needed to wash their hands (n = 1647, 97.9%) and adhere to physical distancing (n = 1,641, 97.5%); more than half (n = 991, 58.9%) reported no change in other risk reduction measures when wearing a mask, 20% (n = 335) reported stricter adherence to these measures and 21.0% (n = 353) reported less adherence to one or more measure.
Experience with COVID-19
Table 1 shows that in the period of March–June 2020, 12.5% participants (n = 293) reported symptoms of a chest infection or cold or flu-like illnesses. Approximately a quarter of participants (n = 609, 26.0%) reported being tested for COVID-19, most commonly because they had symptoms (6.3%) or they were contacts of a confirmed case (6.4%). A total of 123 participants tested positive for COVID-19, representing a positive rate of 20.2% (5.2% of total population). Melbourne had a higher proportion of the population who were tested (n = 67, 45.3%) but a significantly lower proportion of positive tests (n = 1, 0.7%). More than one-third of participants (n = 874, 37.3%) had a family member, work colleague or friend who had confirmed COVID-19. The proportion was lowest in Sydney and Melbourne, and highest in New York.
Perception of COVID-19
The mean perceived severity of COVID-19 was lowest in London (57.2 ± 25.2) and highest in Melbourne (63.9 ± 25.1). The mean perceived risk of getting COVID-19 was lowest in Phoenix (52.2 ± 23.8) and highest in New York (56.4 ± 23.6). The mean perceived effectiveness rating for N95/P2, surgical and cloth masks was higher in New York and Phoenix than other cities. Results for comparison between cities are presented in Appendix Table 4.
Predictors of mask wearing
On univariate regression analysis (Table 2 ) respondents in the UK and US were more likely to wear masks during the COVID-19 pandemic compared with those in Australia (p < 0.001). There was a significant relationship between mask use and age (p = 0.014) and having negative issues while wearing masks (p < 0.001), but not gender (p = 0.953). A mask mandate was associated with mask use (p < 0.001) but was excluded from multivariable regression due to collinearity with country of residence. After adjusting for effects of other covariates, multivariable analysis showed that experiencing negative issues (p < 0.001) and low perceived severity of COVID-19 (p = 0.033) remained significantly associated with lower mask use. Factors associated with higher mask use were: age <50 years (p < 0.001); tertiary education (p = 0.001); wearing a mask before the pandemic (p < 0.001); knowing a family member, friend or colleague who was diagnosed with COVID-19 (p = 0.001); having a chest infection, cold or flu-like symptoms in March–June 2020 (p = 0.002); and self-reported adherence to local mask guidelines (p = 0.006) (Table 2).
Table 2.
Predictors of mask use during the COVID-19 pandemic.
| Predictor | N (%) | OR (95% CI) | p-value | Adjusted OR (95% CI) | Adjusted p-value |
|---|---|---|---|---|---|
| Country | |||||
| Australia (reference) | 348 (14.9) | 1.00 | – | 1.00 | – |
| UK | 291 (12.4) | 2.63 (1.89–3.65) | <0.001* | 2.69 (1.80–4.03) | <0.001* |
| US | 1,704 (72.7) | 3.60 (2.84–4.47) | <0.001* | 2.24 (1.63–3.07) | <0.001* |
| Age <50 years | 1,052 (44.9) | 1.25 (1.05–1.50) | 0.014* | 1.77 (1.38–2.26) | <0.001* |
| Male | 1,118 (47.7) | 1.00 (0.84–1.20) | 0.953 | 0.95 (0.76–1.18) | 0.637 |
| Tertiary education | 1,803 (77.0) | 1.59 (1.30–1.95) | <0.001* | 1.55 (1.20–1.99) | 0.001* |
| Ex/current smoker | 953 (40.7) | 1.20 (1.00–1.44) | 0.056 | 1.23 (0.98–1.55) | 0.070 |
| ≥1 comorbidities | 1,288 (55.0) | 1.25 (1.04–1.49) | 0.017* | 1.26 (0.99–1.60) | 0.055 |
| Past wearing of a mask for non-COVID-19 purposes | 709 (30.3) | 3.13 (2.48–3.96) | <0.001* | 1.69 (1.29–2.21) | <0.001* |
| Having negative experience while wearing mask | 1,025 (43.8) | 0.12 (0.10–0.15) | <0.001* | 0.12 (0.10–0.16) | <0.001* |
| Knowing a COVID-19 case (family/friend/colleague) | 874 (37.3) | 1.97 (1.61–2.40) | <0.001* | 1.50 (1.18–1.91) | 0.001* |
| Diagnosed with COVID-19 | 486 (20.7) | 2.54 (1.51–4.28) | <0.001* | 1.64 (0.89–3.03) | 0.110 |
| Having COVID-19–like symptoms in March–June 2020 | 293 (12.5) | 2.11 (1.53–2.91) | <0.001* | 1.83 (1.25–2.68) | 0.002* |
| Adherence to mask-wearing guideline | 1,983 (84.6) | 1.95 (1.54–2.46) | <0.001* | 1.50 (1.12–2.00) | 0.006* |
| Perceived own health status < averagea | 1,043 (44.5) | 0.77 (0.64–0.92) | 0.004* | 0.87 (0.69–1.08) | 0.210 |
| Perceived self-risk of getting COVID-19 < averagea | 1,338 (57.1) | 0.59 (0.49–0.71) | <0.001* | 0.83 (0.64–1.07) | 0.142 |
| Perceived COVID-19 severity < averagea | 1,110 (47.4) | 0.62 (0.52–0.74) | <0.001* | 0.77 (0.60–0.98) | 0.033* |
| Perceived effectiveness of surgical masks < averagea | 1,154 (49.3) | 0.57 (0.48–0.68) | <0.001* | 0.85 (0.63–1.14) | 0.277 |
| Perceived effectiveness of N95/P2 masks < averagea | 1,064 (45.4) | 0.56 (0.47–0.68) | <0.001* | 0.90 (0.68–1.19) | 0.457 |
| Perceived effectiveness of cloth masks < averagea | 1,321 (56.4) | 0.65 (0.54–0.79) | <0.001* | 1.24 (0.94–1.65) | 0.133 |
| Confidence in national government ≥3b | 978 (41.7) | 0.91 (0.75–1.09) | 0.284 | 1.02 (0.76–1.38) | 0.889 |
| Confidence in state/local government ≥3b | 1,257 (53.7) | 1.33 (1.11–1.60) | 0.002* | 1.14 (0.84–1.55) | 0.411 |
| Trust in COVID-19 information from national government ≥3b | 814 (34.7) | 0.98 (0.81–1.18) | 0.794 | 0.97 (0.69–1.37) | 0.875 |
| Trust in COVID-19 information from state/local government ≥3b | 1,111 (47.4) | 1.36 (1.13–1.63) | 0.001* | 1.06 (0.76–1.48) | 0.729 |
Note: The overall multivariate model is statistically significant (LR χ2(24) = 677.26, p < 0.001). Area under ROC curve (C = 0.8149) indicates good discriminatory power of the model. The mean variance inflation factor in multivariate model is 1.46.
Statistically Significant at α = 0.05
Average refers to the population mean of each variable (refer to Table 1). Variables were coded as “1” if their values were larger than the population mean and coded as “0” if smaller than the population mean
On a scale of 0–4, where 4 represents highest level of trust/confidence.
Predictor of pandemic fatigue
Multivariable regression (Table 3 ) showed that younger age (<50 years) (p = 0.002) and low perceived severity of COVID-19 (p = 0.01) were associated with pandemic fatigue. People living in cities that experienced declining COVID-19 incidence between March 2020 and July 2020 (p = 0.002) were also more likely to show pandemic fatigue.
Table 3.
Predictors of pandemic fatigue during the COVID-19 pandemic.
| Predictor | N (%) | OR (95% CI) | p-value | Adjusted OR (95% CI) | Adjusted p-value |
|---|---|---|---|---|---|
| Cities with declining COVID-19 incidence in July 2020 | 1,695 (72.3) | 1.31 (1.07–1.60) | 0.008* | 1.40 (1.13–1.72) | 0.002* |
| Age <50 years | 1,052 (44.9) | 0.77 (0.64–0.91) | 0.001* | 1.39 (1.13–1.71) | 0.002* |
| Male | 1,118 (47.7) | 0.89 (0.74–1.06) | 0.180 | 0.90 (0.75–1.08) | 0.249 |
| Working/studying | 1,320 (56.3) | 1.14 (0.96–1.36) | 0.142 | 1.06 (0.87–1.29) | 0.576 |
| Tertiary education | 1,803 (77.0) | 0.91 (0.74–1.12) | 0.376 | 0.98 (0.79–1.21) | 0.837 |
| Ex/current smoker | 953 (40.7) | 1.01 (0.84–1.20) | 0.954 | 1.07 (0.89–1.29) | 0.493 |
| ≥1 comorbidities | 1,288 (55.0) | 0.93 (0.78–1.10) | 0.391 | 1.14 (0.94–1.39) | 0.188 |
| Perceived own health status < averagea | 1,043 (44.5) | 1.00 (0.84–0.84) | 0.974 | 1.00 (0.83–1.21) | 0.995 |
| Perceived COVID-19 severity < averagea | 1,338 (57.1) | 0.71 (0.60–0.85) | <0.001* | 1.31 (1.07–1.60) | 0.010* |
| Perceived self-risk of getting COVID-19 < averagea | 1,110 (47.4) | 0.77 (0.65–0.92) | 0.004* | 1.18 (0.95–1.45) | 0.129 |
| Diagnosed with COVID-19 | 486 (20.7) | 0.86 (0.58–1.29) | 0.468 | 0.86 (0.55–1.34) | 0.503 |
| Knowing a COVID-19 case (family/friend/colleague) | 874 (37.3) | 0.86 (0.72–1.03) | 0.106 | 0.88 (0.73–1.07) | 0.191 |
| Having COVID-19–like symptoms in Mar–Jun 2020 | 293 (12.5) | 0.91 (0.70–1.19) | 0.498 | 0.90 (0.67–1.22) | 0.495 |
| Adherence to mask-wearing guidelines | 1,983 (84.6) | 1.23 (0.96–1.57) | 0.107 | 1.34 (1.04–1.74) | 0.025* |
| Perceived effectiveness of surgical masks < averagea | 1,154 (49.3) | 0.96 (0.81–1.15) | 0.689 | 0.85 (0.66–1.09) | 0.191 |
| Perceived effectiveness of N95/P2 masks < averagea | 1,064 (45.4) | 0.82 (0.69–0.98) | 0.027* | 1.17 (0.93–1.47) | 0.178 |
| Perceived effectiveness of cloth masks < averagea | 1,321 (56.4) | 0.93 (0.78–1.11) | 0.417 | 0.96 (0.76–1.21) | 0.747 |
| Confidence in national government ≥3b | 978 (41.7) | 1.12 (0.94–1.33) | 0.214 | 1.13 (0.89–1.44) | 0.317 |
| Confidence in state/local government ≥3b | 1,257 (53.7) | 0.94 (0.79–1.12) | 0.483 | 0.98 (0.76–1.27) | 0.902 |
| Trust in COVID-19 information from national government ≥3b | 814 (34.7) | 1.01 (0.84–1.21) | 0.903 | 1.05 (0.80–1.38) | 0.714 |
| Trust in COVID-19 information from state/local government ≥3b | 1,111 (47.4) | 0.85 (0.72–1.02) | 0.075 | 0.81 (0.62–1.05) | 0.116 |
Note: The overall multivariate model is statistically significant (LR χ2(22) = 59.13, p < 0.001). Area under ROC curve (C = 0.5976) indicates moderate discriminatory power of the model. The mean variance inflation factor in multivariate model is 1.42.
Statistically significant at α = 0.05.
Average refers to the population mean of each variable (refer to Table 1). Variables coded as “1” if their values were larger than the population mean and coded as “0” if smaller than the population mean.
On a scale of 0–4, where 4 represents highest level of trust/confidence.
Discussion
Mask mandates had a strong effect on mask use and masks did not reduce compliance with other control measures. A range of social distancing and hygiene measures was used, with hand hygiene being the most common and more prevalent than physical distancing or mask use. This may reflect the strong focus on hand hygiene in early pandemic messaging. This study confirmed that >40% of people avoided medical facilities and healthcare during the pandemic, which is cause for concern. Pandemic fatigue was seen in all cities except Melbourne, which was experiencing a resurgence of COVID-19 during the survey period. Phoenix was also experiencing a resurgence at the time but participants reported reduced preventive measures by July. Younger age and male gender predicted pandemic fatigue, pointing to these being key groups for health promotion messaging in protracted epidemics. Some studies suggest that males may be less compliant with mask guidance due to perceived association with a lack of 'masculinity' (Seale et al., 2020) but the current study did not find any difference in mask use by gender.
The surveyed cities represented a wide spectrum of disease incidence and varied community mask policies. Age restriction was stricter in London (compulsory for all aged ≥3 years), Phoenix and New York (≥2 years) than Melbourne (≥12 years). Fines were more severe in Melbourne (A$250), London (£200) and Phoenix (US$250) than New York ($50 for non-compliance on public transit) (Bowling, 2020; Department of Health and Human Services Victoria, 2020a; London City Hall, 2020; Office, 2020). In three cities (New York, Phoenix and Melbourne), mask mandates occurred close to the epidemic peak. In London, masks were mandated about three months after the epidemic peak, after substantial advocacy (Greenhalgh et al., 2020). Only Sydney had no mask mandate (New South Wales Department of Health, 2020), and also had the lowest incidence of COVID-19 and the lowest rate of mask use. Except for Melbourne, all cities with mask mandates reported mask usage in excess of 70%, with the highest rates in New York and Phoenix. These findings are consistent with a global survey on knowledge, attitudes and practices (KAP) for COVID-19 prevention measures (Johns Hopkins Bloomberg School of Public Health, 2020), in which individuals in Australia reported lower prevalence of mask use (47%) than those in the UK (66%) and US (87%) in July 2020.
These data show that mask wearing decreased after the age of 50 years, with a significant difference by age in Australia and the UK but not in the US. This is of concern, given that older people are at highest risk for serious complications and death (Leung, 2020) and barriers among older people should be investigated. In contrast, higher mask usage has been reported among older people in Asian countries (Lee et al., 2020, Seale et al., 2020). The current study found that negative issues experienced while wearing masks reduced the likelihood of people wearing them. Early in the pandemic, people of Asian ethnicity reported racism and harassment, while others reported being suspected of criminal intent while wearing masks (Zine, 2020). The negative connotations of disease and identity concealment associated with masks in Western countries prior to the COVID-19 pandemic may have been further catalysed by rising geopolitical tension (Ma and Zhan, 2020) and early public health messages that actively discouraged mask use (Wang et al., 2020). Mandating mask wearing may eliminate this stigma by making it a mainstream behaviour (Betsch et al., 2020, Feng et al., 2020). The current findings were consistent with a recent report, which showed higher levels of trust in the government among Australians (54%) than those in UK (41%) or US (34%) (Evans et al., 2020); however, trust was not a significant predictor of mask wearing.
This study was not without limitations. The method of recruitment from an online panel and non-response from panelists may have potentially introduced response bias (Baker et al., 2010). However, Dynata panels have over 60 million people and are widely used in research. In addition, the survey was only administered online and in English. As a result, non-English speakers or people with limited access to the Internet may have been excluded and may have been different to their English-speaking or Internet-using counterparts. Although mask use was surveyed by ethnicity, it was not incorporated into the multivariable regression model because of the complexity associated with multiple-response questions. Ethnicity is an important factor influencing mask adoption because of its link to culture, socioeconomic status and family/community norms (Sim et al., 2014). This survey only provided a cross-sectional description of mask use, which relied on recall for reporting behaviours in the early pandemic period and may have introduced recall bias.
Conclusion
The COVID-19 pandemic has seen a rise in mask use in cities with no previous mask culture, as well as adoption of a wide range of other preventive behaviours, with hand hygiene being the most common. Mask use was widespread in the studied cities, especially where mandates were issued, but usage was lower in older adults. This age effect was not seen in the US and may reflect cultural differences. Masks did not result in a net change in other risk-mitigation behaviours such as hand washing and distancing. The reduction of risk-mitigation behaviours between March and July 2020 may have reflected changing epidemiology of the local pandemic and a corresponding change in risk perception. Both Melbourne and Phoenix were experiencing a resurgence during the survey but only Melbourne showed an increase in most risk-mitigation behaviours. The reduction in these behaviours in all other cities may have reflected pandemic fatigue, which was more common in young people and males.
Funding
The study was funded by the Medical Research Future Fund by the Australian Government [Grant number APP1201320]. The funding organisation had no role in the design of the study; the collection, analysis, and interpretation of the data; nor the decision to approve publication of the finished manuscript.
Ethics approval
The study was approved by the Human Research Ethics Committee of the University of New South Wales (project number HC200460) and conformed to the principles embodied in the Declaration of Helsinki.
Conflict of interest
CRM reports being on the advisory board for development of masks at Ascend Technologies, and having consulted for the development of masks at Detmold and Atmos, outside the submitted work. AAC reports testing of filtration of masks by 3 M for his Ph.D. more than 10 years ago. 3M products were not used in his research. He also has worked with CleanSpace Technology on research on fit testing of respirators (no funding was involved). PYYN, MT, BG, KS and HS declare no conflicts of interest.
Acknowledgements
The authors would like to acknowledge the support of the staff at the Biosecurity Program (The Kirby Institute) who assisted with the administration of the survey.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijid.2021.03.056.
Appendix A. Supplementary data
The following are Supplementary data to this article:
Age-gender distribution of participants, by city.
References
- Arizona Department of Health Services . 2020. Data dashboard.https://www.azdhs.gov/preparedness/epidemiology-disease-control/infectious-disease-epidemiology/covid-19/dashboards/index.php [Google Scholar]
- Australian Government Department of Health . 2020. Masks.https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/how-to-protect-yourself-and-others-from-coronavirus-covid-19/masks [Google Scholar]
- Babalola S., Krenn S., Rimal R., Serlemitsos E., Shaivitz M., Shattuck D. Johns Hopkins Center for Communication Programs, Massachusetts Institute of Technology, Global Outbreak Alert and Response Network, Facebook Data for Good; 2020. KAP COVID dashboard – exploring knowledge, attitudes and practices for COVID-19 prevention.https://ccp.jhu.edu/kap-covid/ [Google Scholar]
- Baker R., Groves R.M., Krosnick J. Research synthesis: AAPOR report on online panels. Public Opin Q. 2010;74:711–781. doi: 10.1093/poq/nfq048. [DOI] [Google Scholar]
- Betsch C., Korn L., Sprengholz P., Felgendreff L., Eitze S., Schmid P. Social and behavioral consequences of mask policies during the COVID-19 pandemic. Proc Natl Acad Sci U S A. 2020;117:21851–21853. doi: 10.1073/pnas.2011674117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling J. AZ Cent; 2020. Phoenix will require mask or other face covering starting Saturday.https://www.azcentral.com/story/news/local/phoenix/2020/06/19/phoenix-require-mask-other-face-covering-starting-saturday/3219102001/ [Google Scholar]
- Burgess A., Horii M. Risk, ritual and health responsibilisation: Japan’s ‘safety blanket’ of surgical face mask-wearing. Sociol Health Illn. 2012;34:1184–1198. doi: 10.1111/j.1467-9566.2012.01466.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2020. Use masks to help slow spread.https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html [Google Scholar]
- Chan A.L., Leung C., Lam T., Cheng K. To wear or not to wear: WHO’s confusing guidance on masks in the covid-19 pandemic. BMJ Opin. 2020 https://blogs.bmj.com/bmj/2020/03/11/whos-confusing-guidance-masks-covid-19-epidemic/ (Accessed 18 October 2020) [Google Scholar]
- Chu D.K., Akl E.A., Duda S., Solo K., Yaacoub S., Schünemann H.J. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Data.NSW . 2020. NSW COVID-19 cases data.https://data.nsw.gov.au/nsw-covid-19-data/cases [Google Scholar]
- Department of Health and Human Services Victoria . 2020. Face coverings: whole of Victoria.https://www.dhhs.vic.gov.au/face-coverings-covid-19 [Google Scholar]
- Department of Health and Human Services Victoria . 2020. Victorian coronavirus (COVID-19) data.https://www.dhhs.vic.gov.au/victorian-coronavirus-covid-19-data [Google Scholar]
- Dynata . 2020. COVID-19 insights.https://www.dynata.com/covid-19-insights/ [Google Scholar]
- Evans M., Valgardsson V., Jennings W., Stoker G. 2020. Political trust and democracy in times of coronavirus: is Australia still the lucky country? [Google Scholar]
- Faul F., Erdfelder E., Buchner A., Lang A.-G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- Feng S., Shen C., Xia N., Song W., Fan M., Cowling B.J. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. 2020;8:434–436. doi: 10.1016/S2213-2600(20)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of New York State . 2020. No. 202.17: continuing temporary suspension and modification of laws relating to the disaster emergency.https://www.governor.ny.gov/news/no-20217-continuing-temporary-suspension-and-modification-laws-relating-disaster-emergency [Google Scholar]
- Government of the United Kingdom . 2020. Face coverings: when to wear one, exemptions, and how to make your own.https://www.gov.uk/government/publications/face-coverings-when-to-wear-one-and-how-to-make-your-own/face-coverings-when-to-wear-one-and-how-to-make-your-own [Google Scholar]
- Government of the United Kingdom . 2020. Coronavirus (COVID-19) in the UK.https://coronavirus.data.gov.uk/ [Google Scholar]
- Greenhalgh T., Schmid M.B., Czypionka T., Bassler D., Gruer L. Face masks for the public during the covid-19 crisis. BMJ. 2020;369 doi: 10.1136/bmj.m1435. [DOI] [PubMed] [Google Scholar]
- Johns Hopkins Bloomberg School of Public Health . 2020. KAP COVID: exploring knowledge, attitudes and practices for COVID-19 prevention.https://ccp.jhu.edu/kap-covid/ [Google Scholar]
- Jones Sarah P. 2020. Imperial College London Big Data Analytical Unit and YouGov Plc. COVID-19 Behaviour Tracker.https://ichpanalytics.imperialcollegehealthpartners.com/#/site/BDAU/views/YouGovICLCOVID-19BehaviourTracker/4Allbehaviorsovertime?:iid=1 [Google Scholar]
- Lee L.Y.K., Lam E.P.W., Chan C.K., Chan S.Y., Chiu M.K., Chong W.H. Practice and technique of using face mask amongst adults in the community: a cross-sectional descriptive study. BMC Public Health. 2020;20:948. doi: 10.1186/s12889-020-09087-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung C. Risk factors for predicting mortality in elderly patients with COVID-19: a review of clinical data in China. Mech Ageing Dev. 2020;188 doi: 10.1016/j.mad.2020.111255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- London City Hall . 2020. Face covering guidance.https://www.london.gov.uk/coronavirus/face-covering-guidance [Google Scholar]
- Ma Y., Zhan N. To mask or not to mask amid the COVID-19 pandemic: how Chinese students in America experience and cope with stigma. Chin Sociol Rev. 2020:1–26. doi: 10.1080/21620555.2020.1833712. [DOI] [Google Scholar]
- MacIntyre C.R., Chughtai A.A. A rapid systematic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, healthcare workers and sick patients. Int J Nurs Stud. 2020;108 doi: 10.1016/j.ijnurstu.2020.103629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacIntyre C.R., Chughtai A.A. Facemasks for the prevention of infection in healthcare and community settings. BMJ. 2015;350 doi: 10.1136/bmj.h694. [DOI] [PubMed] [Google Scholar]
- MacIntyre C.R., Wang Q. Physical distancing, face masks, and eye protection for prevention of COVID-19. Lancet. 2020;395:1950–1951. doi: 10.1016/S0140-6736(20)31183-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New South Wales Department of Health . 2020. Face masks.https://www.nsw.gov.au/covid-19/face-masks [Google Scholar]
- New York State Department of Health . 2020. Workbook: NYS-COVID19-Tracker.https://covid19tracker.health.ny.gov [Google Scholar]
- Office TG of NYS . 2020. Governor Cuomo issues executive order directing MTA to develop plan to bolster mask compliance on public transit system.https://www.governor.ny.gov/news/governor-cuomo-issues-executive-order-directing-mta-develop-plan-bolster-mask-compliance-public [Google Scholar]
- Oran D.P., Topol E.J. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med. 2020;173:362–367. doi: 10.7326/M20-3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phoenix City Hall . 2020. Phoenix requires face coverings; frequently asked questions.https://www.phoenix.gov/newsroom/em-and-hs/1353 [Google Scholar]
- Seale H., Dyer C.E.F., Abdi I., Rahman K.M., Sun Y., Qureshi M.O. Improving the impact of non-pharmaceutical interventions during COVID-19: examining the factors that influence engagement and the impact on individuals. BMC Infect Dis. 2020;20:607. doi: 10.1186/s12879-020-05340-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim S.W., Moey K.S.P., Tan N.C. The use of facemasks to prevent respiratory infection: a literature review in the context of the Health Belief Model. Singapore Med J. 2014;55:160–167. doi: 10.11622/smedj.2014037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin M.S.Y. Masking fears: SARS and the politics of public health in China. Crit Public Health. 2016;26(January (1)):88–98. doi: 10.1080/09581596.2014.923815. [DOI] [Google Scholar]
- Zine J. Unmasking the racial politics of the coronavirus pandemic. The Conversation. 2020 https://theconversation.com/unmasking-the-racial-politics-of-the-coronavirus-pandemic-139011 (Accessed 3 November 2020) [Google Scholar]
- Wang J., Pan L., Tang S., Ji J.S., Shi X. Mask use during COVID-19: a risk adjusted strategy. Environ Pollut. 2020;266 doi: 10.1016/j.envpol.2020.115099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. Advice on the use of masks in the community, during home care and in healthcare settings in the context of the novel coronavirus (COVID-19) outbreak, 5 June 2020.https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Age-gender distribution of participants, by city.