Abstract
Coronavirus disease 2019 (COVID-19) has become a global pandemic. Previous studies showed that comorbidities in patients with COVID-19 are risk factors for adverse outcomes. This study aimed to clarify the association between nervous system diseases and severity or mortality in patients with COVID-19. We performed a systematic literature search of four electronic databases and included studies reporting the prevalence of nervous system diseases in COVID-19 patients with severe and non-severe disease or among survivors and non-survivors. The included studies were pooled into a meta-analysis to calculate the odds ratio (OR) with 95% confidence intervals (95%CI). We included 69 studies involving 17 879 patients. The nervous system diseases were associated with COVID-19 severity (OR = 3.19, 95%CI: 2.37 to 4.30, P < 0.001) and mortality (OR = 3.75, 95%CI: 2.68 to 5.25, P < 0.001). Specifically, compared with the patients without cerebrovascular disease, patients with cerebrovascular disease infected with COVID-19 had a higher risk of severity (OR = 3.10, 95%CI: 2.21 to 4.36, P < 0.001) and mortality (OR = 3.45, 95% CI: 2.46 to 4.84, P < 0.001). Stroke was associated with severe COVID-19 disease (OR = 1.95, 95%CI: 1.11 to 3.42, P = 0.020). No significant differences were found for the prevalence of epilepsy (OR = 1.00, 95%CI: 0.42 to 2.35, P = 0.994) and dementia (OR = 2.39, 95%CI: 0.55 to 10.48, P = 0.247) between non-severe and severe COVID-19 patients. There was no significant association between stroke (OR = 1.79, 95%CI: 0.76 to 4.23, P = 0.185), epilepsy (OR = 2.08, 95%CI: 0.08 to 50.91, P = 0.654) and COVID-19 mortality. In conclusion, nervous system diseases and cerebrovascular disease were associated with severity and mortality of patients with COVID-19. There might be confounding factors that influence the relationship between nervous system diseases and COVID-19 severity as well as mortality.
Key words: Cerebrovascular disease, COVID-19, meta-analysis, mortality, nervous system disease, severe illness
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. The World Health Organization (WHO) claims that COVID-19 has become a global pandemic on 11 March 2020 [2]. As of 30 October 2020, a total of 44 888 869 confirmed cases were reported globally, of which 1 178 475 cases had resulted in mortality [3].
The previous study showed that comorbidities in patients with COVID-19 are risk factors for adverse outcomes and cerebrovascular disease was associated with severe COVID-19 disease, which needs to be monitored in the intensive care unit (ICU) care [4]. A meta-analysis [5] suggested that cerebrovascular disease was associated with the increased poor composite outcome (RR = 2.04, 95%CI: 1.43 to 2.91, P < 0.001) and another meta-analysis [6] showed similar results. However, the existing meta-analyses only incorporated a small number of samples and most of the studies synthesised came from China. To date, there is still limited evidence regarding the concomitant association between nervous system diseases and COVID-19. Therefore, to address this gap in the literature, it is necessary to conduct a comprehensive meta-analysis. The purpose of this study was to clarify the association between nervous system diseases and severity or mortality in patients with COVID-19.
Methods
To ensure the high quality of our work, we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement to conduct our study [7]. We registered this review protocol in the International Prospective Register of Systematic Reviews (PROSPERO, CRD42020180567).
Eligibility criteria
We included case−control studies and cohort studies that met the following criteria: (1) patients were diagnosed with COVID-19 by a laboratory test or according to the World Health Organization interim guidance [8]; (2) reported data of pre-existing nervous system diseases, such as cerebrovascular disease, stroke and epilepsy between patients with severe and non-severe illness or between non-survivors and survivors; (3) published in English and Chinese.
We excluded studies with the following characteristics: (1) studies with a sample size of fewer than 20 patients; (2) studies did not report data related to nervous system diseases (e.g. cerebrovascular disease, stroke); (3) studies focused on only suspected cases or confirmed cases and suspected cases; (4) without comparisons (e.g. non-survivors vs. survivors); (5) review articles, protocols, guidelines, consensus, comments, abstracts, letters and editorials.
Literature search
We comprehensively identified all potentially relevant articles through a systematic literature search of the electronic databases: PubMed, EMBASE.com, Web of Science and the Cochrane Central Register of Controlled Trials (CENTRAL). The searches were first performed on 8 May 2020 and updated on 10 October 2020. According to the indices of various databases, we used search terms as follows: ‘COVID-19’, ‘coronavirus disease-19’, ‘new coronavirus’, ‘2019-nCoV’, ‘novel corona virus’, ‘novel coronavirus’, ‘nCoV-2019’, ‘novel coronavirus pneumonia’, ‘2019 novel coronavirus’, ‘coronavirus disease 2019’, ‘SARS-CoV-2’, ‘severe acute respiratory syndrome coronavirus 2’, ‘clinical characteristic’, ‘clinical feature’, ‘risk factor’, ‘prognosis’, ‘comorbidit*’, ‘cerebrovascular disease*’, ‘nervous system disease*’, ‘brain’, ‘neurologic*’, ‘stroke’, ‘cerebral infarction’, ‘dementia’ and ‘epilepsy’. The search strategy of PubMed is shown in Appendix Word 1. We manually searched the reference lists of each included paper to identify potentially eligible studies.
Study selection process
Records were managed by EndNote X8 (Thomson Reuters (Scientific) LLC Philadelphia, PA, US) software to exclude duplicates. At first, two authors independently (YG and YMC) screened the titles and abstracts of the records to determine if they met the inclusion criteria. Then, the same two authors retrieved the full text of all potentially eligible studies and assessed the eligibility of each study according to the inclusion criteria. Disagreements were resolved by discussion or by a third reviewer (JHT). When identified multiple studies from the same team or studies with samples from the same settings, we decided which study to include based on the study time frame and detailed data. For studies with overlapping data, we included studies with larger sample sizes.
Data extraction and quality assessment
We used Microsoft Excel 2019 to construct a standard form to extract research data. The data abstracted included: (1) study characteristics (first author, year of publication, journal name, publication language, country of the first author, recruitment time frame, study design, study setting); (2) population characteristics (sex, age, sample size); (3) outcomes of interest (number of nervous system diseases patients, severe cases, non-severe cases, non-survivors, and survivors). The severe disease was defined as patients with acute respiratory distress syndrome (ARDS), needing mechanical ventilation, vital life support or intensive care unit admission [9–12]. We defined nervous system diseases according to the international classification of diseases -11 (ICD-11) [13, 14].
We used the Newcastle−Ottawa quality assessment scale (NOS) to assess the quality of the included studies [15]. Studies with more than 7 stars were regarded as high quality, 5–7 stars were regarded as moderate quality and lower than 5 stars were regarded as low quality. In our study, one reviewer (YG, YMC, ML or ZWS,) evaluated the quality of each study according to the scale and another (MLY and MMN) reviewed it. In the case of incongruity, the third researcher (JHT) was invited to discuss.
Statistical analysis
We used Stata (13.0; Stata Corporation, College Station, Texas, USA Stata) to perform all meta-analyses. We conducted pairwise meta-analyses to compute the odds ratio (OR) with 95% confidence interval (95%CI) to estimate the association between nervous system diseases and COVID-19 severity or mortality. The meta-analyses used the inverse variance method with the random-effects model to estimate the average effect. We used the I2 statistic and Cochran's Q test to assess statistical heterogeneity. The I2 statistic results were interpreted as <25%, 26–50% and >50%, representing low, moderate and high heterogeneity, respectively [16].
Sensitivity analyses were applied by excluding studies published in Chinese to assess the stability of results. We further performed univariate meta-regression analyses to assess if the OR varied with study sample size. The funnel plot and Egger's test were used to detect publication bias for outcomes with studies no fewer than 10. The statistical level of significance was set at P < 0.05.
Results
Screening results
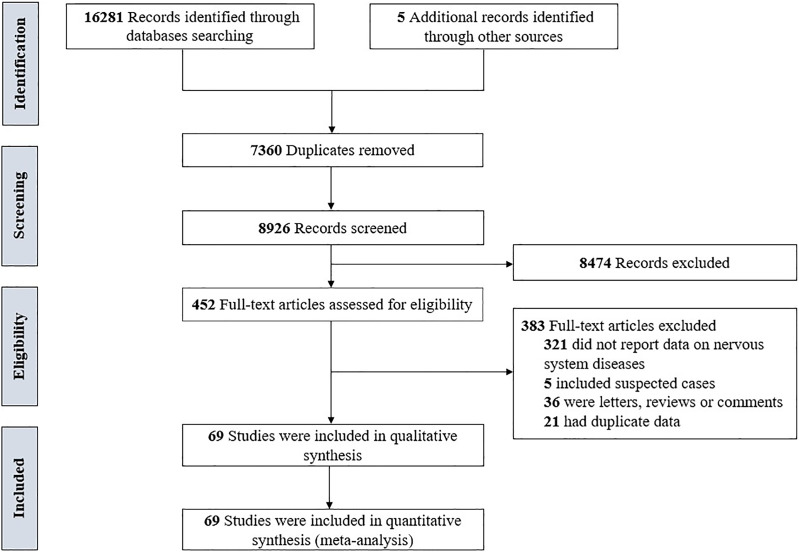
Totally, 16 286 records were identified through the literature search. After removing duplicates, 7360 records were excluded, and after reviewing the titles and abstracts, 8474 records were excluded. Through full-text evaluation of the remaining 452 records, 383 studies were further excluded, we finally included 69 studies [4, 17–84] in our meta-analyses. The flowchart of the screening process is presented in Fig. 1.
Fig. 1.
The flowchart of the screening process.
General characteristics and quality of studies
All included studies were published online in 2020, incorporated patients between 11 December 2019 and 27 June 2020. In all, 68 studies [4, 17–83] were published in English and 1 study [84] published in Chinese. Out of which 54 studies [4, 18–24, 29–31, 34–39, 45–53, 55, 56, 59–84] were from China, 3 studies [17, 32, 54] were from the USA, 3 studies [25, 40, 44] were from Korea, 2 studies [26, 27] were from Italy and the remaining 7 studies [28, 33, 41–43, 57, 58] were from Austria, Iran, Israel, Saudi Arabia, Spain, Turkey, and UK. The sample size per study ranged from 27 to 1590 (total 17 879; 9686 males). Considering methodological quality in items of NOS scale, 23 studies [4, 17, 19, 21, 24, 27–29, 33, 34, 37, 46, 49, 55, 58, 61, 65, 67–69, 73, 75, 76] were rated as high quality (>7 stars) and 46 studies [18, 20, 22, 23, 25, 26, 30–32, 35, 36, 38–45, 47, 48, 50–54, 56, 57, 59, 60, 62–64, 66, 70–72, 74, 77–84] were rated as moderate quality (5−7 stars). The detailed characteristics and quality of the included studies are summarised in Table 1.
Table 1.
Characteristics of included studies
| Study | Year (Online) | Country | Publication language | Recruitment time frame | Sample | Age, yearsa | Sex | NOS | |
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | ||||||||
| Argenziano MG [17] | 2020 | USA | English | 2020.3.1–2020.4.15 | 1000 | 61.7 ± 17.5 | 596 | 404 | 8 |
| Cao JL [18] | 2020 | China | English | 2020.1.3–2020.2.1 | 102 | 54(37–67) | 53 | 49 | 6 |
| Chen T [19] | 2020 | China | English | 2020.1.13–2020.2.12 | 274 | 62(44–70) | 171 | 103 | 8 |
| Chen TL [20] | 2020 | China | English | 2020.1.1–2020.2.10 | 55 | 74(65–91) | 34 | 21 | 6 |
| Chen X [21] | 2020 | China | English | 2020.2.3–2020.2.20 | 73 | 66(59–72.3) | 42 | 31 | 8 |
| Chen XH [22] | 2020 | China | English | 2020.2.1–2020.2.19 | 48 | 64.6 ± 18.1 | 37 | 11 | 7 |
| Cheng AY [23] | 2020 | China | English | 2020.2.8–2020.3.11 | 305 | 65(52–71) | 184 | 121 | 7 |
| Cheng L [24] | 2020 | China | English | 2020.1.3–2020.2.26 | 89 | 59.74 ± 16.42 | 49 | 40 | 8 |
| Chon Y [25] | 2020 | Korea | English | 2020.2.22–2020.4.3 | 281 | 61.5 ± 5.5 | 75 | 206 | 5 |
| Colombi D [26] | 2020 | Italy | English | 2020.2.17–2020.3.10 | 236 | 68(95%CI:66–70) | 177 | 59 | 6 |
| d'Arminio Monforte A [27] | 2020 | Italy | English | 2020.2.24–2020.5.17 | 539 | 66(54–78) | 347 | 192 | 9 |
| Dupley L [28] | 2020 | UK | English | 2020.3.1–2020.4.26 | 64 | 83 ± 9 | 29 | 35 | 8 |
| Feng Y [29] | 2020 | China | English | 2020.1.1–2020.2.15 | 476 | 53(40–64) | 271 | 205 | 8 |
| Fu J [30] | 2020 | China | English | 2020.1.21–2020.3.4 | 35 | 47.94 ± 15 | 13 | 22 | 6 |
| Gao S [31] | 2020 | China | English | 2020.1.23–2020.2.29 | 210 | 71(67–77) | 101 | 109 | 7 |
| Gayam V [32] | 2020 | USA | English | 2020.3.1–2020.4.9 | 408 | 67(56–76) | 231 | 177 | 6 |
| Götzinger F [33] | 2020 | Austria | English | 2020.4.1–2020.4.24 | 582 | 5(0.5–12.0) | 311 | 271 | 9 |
| Guan WJ [34] | 2020 | China | English | 2019.12.11–2020.1.31 | 1590 | 48.9 ± 16.3 | 904 | 686 | 8 |
| Han MF [35] | 2020 | China | English | NR | 154 | 42.4 | 86 | 68 | 7 |
| Hu H [36] | 2020 | China | English | 2020.2.7–2020.3.7 | 105 | 60.82 ± 16.32 | 62 | 43 | 7 |
| Hu L [37] | 2020 | China | English | 2020.1.8–2020.2.20 | 323 | 61(23–91) | 166 | 157 | 8 |
| Huang HF [38] | 2020 | China | English | 2020.1.13–2020.3.10 | 64 | 47.8 ± 18.5 | 37 | 27 | 6 |
| Huang Q [39] | 2020 | China | English | 2020.1.17–2020.2.10 | 54 | 41(31–51) | 28 | 26 | 7 |
| Hwang JM [40] | 2020 | Korea | English | 2020.2.1–2020.3.25 | 103 | 67.62 ± 15.32 | 52 | 51 | 6 |
| Itelman E [41] | 2020 | Israel | English | 2020.2–2020.4.10 | 162 | 52 ± 20 | 105 | 57 | 6 |
| Javanian M [42] | 2020 | Iran | English | 2020.2.25–2020.3.12 | 100 | 60.12 ± 13.87 | 51 | 49 | 6 |
| Kutluhan MA [43] | 2020 | Turkey | English | 2020.3.11–2020.5.10 | 96 | 58 ± 18.5 | 57 | 39 | 7 |
| Lee JY [44] | 2020 | Korea | English | 2020.2.21–2020.4.2 | 694 | 52.1 ± 18.29 | 212 | 482 | 7 |
| Lei SQ [45] | 2020 | China | English | 2020.1.2–2020.2.5 | 34 | 55(43–63) | 14 | 20 | 7 |
| Li M [46] | 2020 | China | English | 2019.12.26–2020.2.25 | 245 | 54(37–64) | 118 | 127 | 8 |
| Li Q [47] | 2020 | China | English | 2020.1.20–2020.2.29 | 325 | 51(36–64) | 167 | 158 | 7 |
| Li T [48] | 2020 | China | English | 2020.2.1–2020.3.31 | 312 | 69.2 ± 7.3 | 187 | 125 | 6 |
| Liu Q [49] | 2020 | China | English | 2020.1.23–2020.2.29 | 84 | 51(37–59) | 45 | 39 | 8 |
| Liu SQ [50] | 2020 | China | English | 2020.1.10–2020.3.15 | 625 | 44.44 ± 17.19 | 329 | 296 | 7 |
| Lu L [51] | 2020 | China | English | 2020.1.18–2020.2.18 | 304 | 44(33–59.25) | 182 | 122 | 7 |
| Luo XM [52] | 2020 | China | English | 2020.1.30–2020.2.20 | 298 | 57(40–69) | 150 | 148 | 7 |
| Lyu PJ [53] | 2020 | China | English | 2020.1.15–2020.2.14 | 51 | 54 ± 17 | 29 | 22 | 7 |
| Maeda T [54] | 2020 | USA | English | 2020.3.13–2020.3.31 | 224 | 63 ± 17 | 127 | 97 | 7 |
| Pan L [55] | 2020 | China | English | 2020.1.18–2020.2.28 | 103 | 52.91 ± 15.98 | 55 | 48 | 9 |
| Qin C [56] | 2020 | China | English | 2020.1.10–2020.2.12 | 452 | 58(47–67) | 235 | 217 | 7 |
| Romero-Sánchez CM [57] | 2020 | Spain | English | 2020.3.1–2020.4.1 | 841 | 66.42 ± 14.96 | 473 | 368 | 6 |
| Shabrawishi M [58] | 2020 | Saudi Arabia | English | 2020.3.12–2020.3.31 | 150 | 46.1 ± 15.3 | 90 | 60 | 8 |
| Wang CZ [59] | 2020 | China | English | 2020.1.23–2020.2.13 | 45 | 39(16–62) | 23 | 22 | 6 |
| Wang D [60] | 2020 | China | English | 2020.1.15–2020.2.28 | 143 | 58(39–67) | 73 | 70 | 6 |
| Wang DW(a) [4] | 2020 | China | English | 2020.1.1–2020.1.28 | 138 | 56(42–68) | 75 | 63 | 8 |
| Wang DW(b) [61] | 2020 | China | English | −2020.2.10 | 107 | 51(36–65) | 57 | 50 | 8 |
| Wang F [62] | 2020 | China | English | 2020.1–2020.3 | 108 | Survivors 70.9 ± 10.6/non-survivors 71.1±10.1 | 72 | 36 | 7 |
| Wang L [63] | 2020 | China | English | 2020.1.1–2020.2.6 | 339 | 69(65–76) | 168 | 171 | 5 |
| Wang LW [64] | 2020 | China | English | 2020.1.14–2020.2.13 | 116 | 54(38–69) | 67 | 49 | 6 |
| Wang WL [65] | 2020 | China | English | 2020.2.10–2020.3.27 | 123 | 68(56.5–78) | 60 | 63 | 8 |
| Wang YF [66] | 2020 | China | English | 2020.1-2020.2.10 | 110 | NR | 48 | 62 | 7 |
| Wang YP [67] | 2020 | China | English | 2020.1.20–2020.2.10 | 275 | 49(34–62) | 128 | 147 | 8 |
| Wei YP [68] | 2020 | China | English | 2020.1.27–2020.3.11 | 276 | 51(41–58) | 155 | 121 | 9 |
| Wu GY [69] | 2020 | China | English | 2019.12.23–2020.2.13 | 299 | 50(35.5–63) | 137 | 162 | 8 |
| Wu J [70] | 2020 | China | English | 2020.1.20–2020.2.20 | 280 | 43.12 ± 19 | 151 | 129 | 7 |
| Wu SR [71] | 2020 | China | English | 2020.1.27–2020.2.26 | 270 | 62(50–69) | 139 | 131 | 6 |
| Xie JF [72] | 2020 | China | English | 2020.1.1–2020.2.29 | 733 | 65(56–73) | 477 | 256 | 7 |
| Yan XQ [73] | 2020 | China | English | 2020.1.21–2020.6.27 | 218 | 42.9(32–52.3) | 122 | 96 | 9 |
| Yan YL [74] | 2020 | China | English | 2020.1.10–2020.2.24 | 193 | 64(49–73) | 114 | 79 | 7 |
| Yang QX [75] | 2020 | China | English | 2020.1.28–2020.2.12 | 136 | 56(44–64) | 66 | 70 | 8 |
| Yang XB [76] | 2020 | China | English | 2019.12.24–2020.1.26 | 52 | 59.7 ± 13.3 | 35 | 17 | 8 |
| Yuan ML [77] | 2020 | China | English | 2020.1.1–2020.1.25 | 27 | 60(47–69) | 12 | 15 | 6 |
| Zhang GQ [78] | 2020 | China | English | 2020.1.2–2020.2.10 | 221 | 55(39–66.5) | 108 | 113 | 7 |
| Zhang HM [79] | 2020 | China | English | 2020.1.28–2020.2.24 | 88 | 55(22–89) | 45 | 43 | 7 |
| Zhang JJ [80] | 2020 | China | English | 2020.1.16–2020.2.3 | 140 | 57(25–87) | 71 | 69 | 7 |
| Zhang L [81] | 2020 | China | English | 2020.1.20–2020.2.29 | 409 | 65(56–71) | 234 | 175 | 6 |
| Zhao Y [82] | 2020 | China | English | 2020.1.13- 2020.3.4 | 539 | 58(43–69) | 255 | 284 | 6 |
| Zheng F [83] | 2020 | China | English | 2020.1.17–2020.2.7 | 161 | 45(33.5–57) | 80 | 81 | 6 |
| Zou WB [84] | 2020 | China | Chinese | 2020.2.1–2020.2.29 | 63 | Severe 52 ± 16/non-severe 43±16 | 32 | 31 | 6 |
Age data presented as median (IQR) or mean ± s.d.. NR, not reported.
Association between nervous system diseases and the severity and mortality of COVID-19
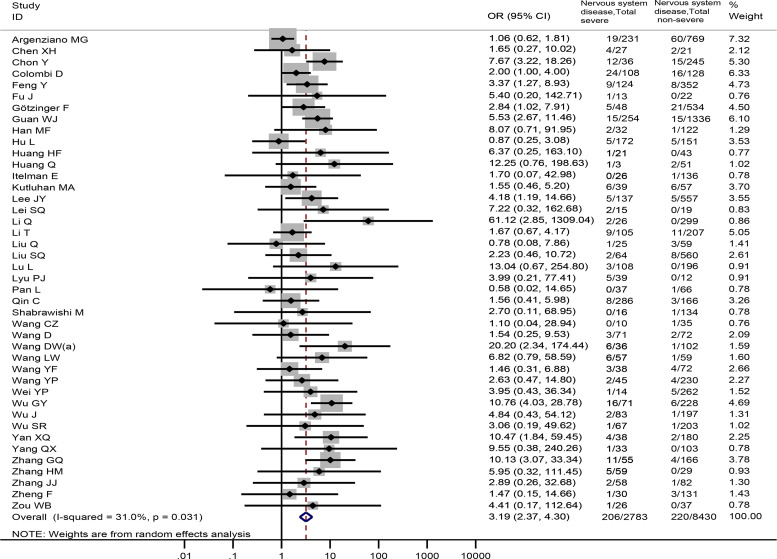
In all, 42 studies [4, 17, 22, 25, 26, 29, 30, 33–35, 37–39, 41, 43–45, 47–51, 53, 55, 56, 58–60, 64, 66–71, 73, 75, 78–80, 83, 84] totaling 11 213 patients reported prevalence of nervous system diseases among COVID-19 patients with the severe and non-severe disease. The meta-analysis demonstrated that nervous system diseases were associated with COVID-19 severity (OR = 3.19, 95%CI: 2.37 to 4.30, P < 0.001; I2 = 31.0%) (Fig. 2). We observed a significant association (OR = 3.19, 95%CI: 2.36 to 4.32, P < 0.001) between nervous system diseases and COVID-19 severity after excluding a Chinese study [84] (Appendix Fig. 1).
Fig. 2.
Association between nervous system diseases and the severity of COVID-19.
Overall, 23 studies [18–21, 23, 24, 27, 31, 32, 34, 36, 42, 46, 52, 61–63, 72, 74, 76, 77, 81, 82], involving 6900 patients provided nervous system diseases data between non-survivors and survivors. The result revealed that nervous system diseases were associated with a significantly enhanced risk of death (OR = 3.75, 95%CI: 2.68 to 5.25, P < 0.001; I2 = 35.6%) (Fig. 3).
Fig. 3.
Association between nervous system diseases and the mortality of COVID-19.
Association between cerebrovascular disease and the severity and mortality of COVID-19
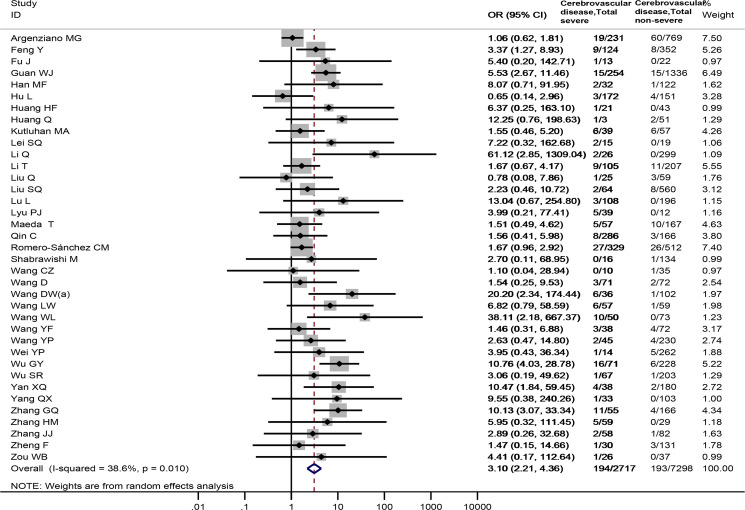
Thirty-seven studies [4, 17, 29, 30, 34, 35, 37–39, 43, 45, 47–51, 53, 54, 56–60, 64–69, 71, 73, 75, 78–80, 83, 84], totaling 10 015 samples, reported the prevalence of cerebrovascular disease between severe and non-severe COVID-19 patients. Cerebrovascular disease was observed to be associated with a significantly enhanced risk of severe COVID-19 disease (OR = 3.10, 95%CI: 2.21 to 4.36, P < 0.001; I2 = 38.6%), Fig. 4. Sensitivity analysis by excluding a Chinese study [84] showed similar results (OR = 3.10, 95%CI: 2.19 to 4.39), Appendix Fig. 2.
Fig. 4.
Association between cerebrovascular disease and the severity of COVID-19.
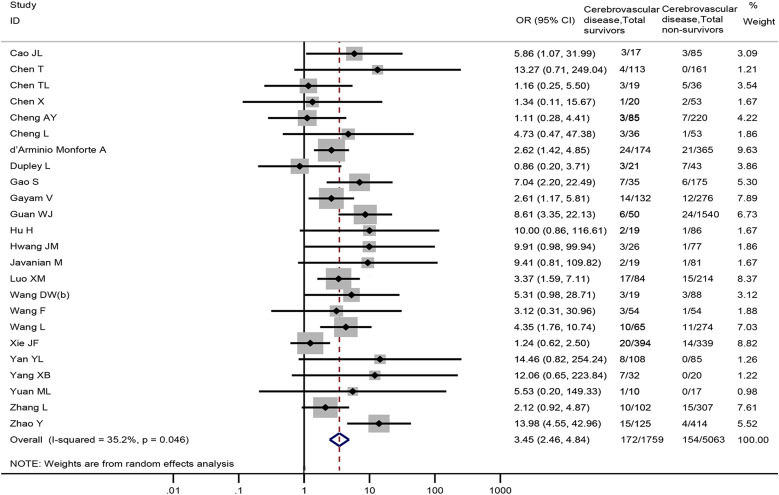
Twenty-four studies [18–21, 23, 24, 27, 28, 31, 32, 34, 36, 40, 42, 52, 61–63, 72, 74, 76, 77, 81, 82], including 6822 patients, reported cerebrovascular disease data between non-survivors and survivors. The meta-analysis demonstrated that cerebrovascular disease was associated with death in COVID-19 patients (OR = 3.45, 95% CI: 2.46 to 4.84, P < 0.001; I2 = 35.2%) (Fig. 5).
Fig. 5.
Association between cerebrovascular disease and the mortality of COVID-19.
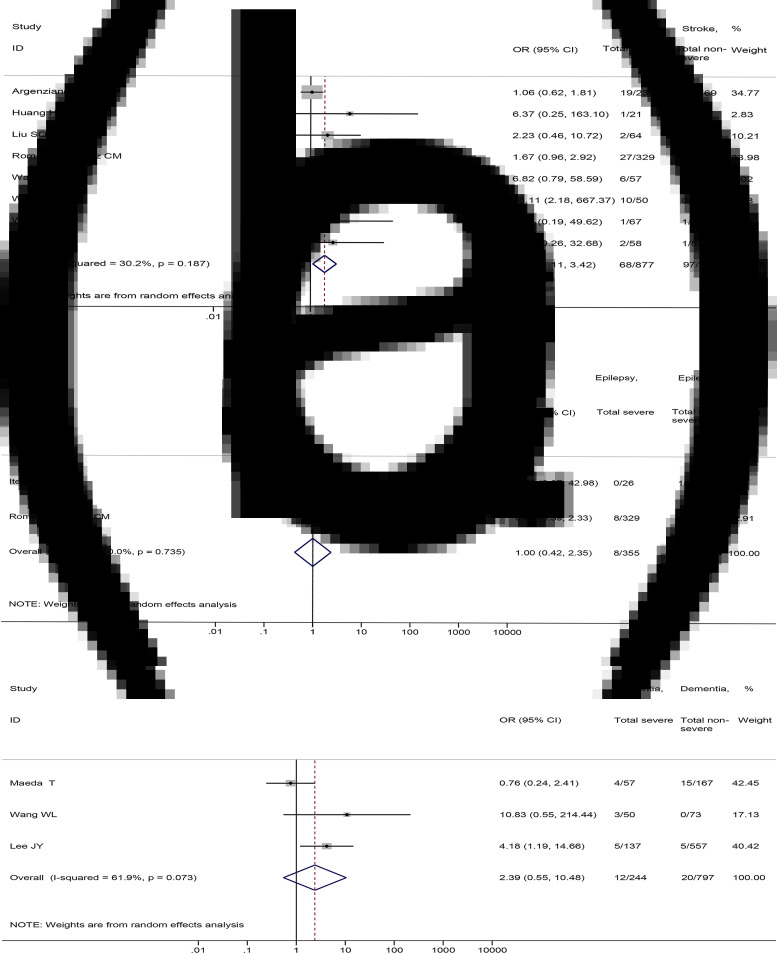
Association between stroke, epilepsy, dementia and the severity and mortality of COVID-19
As for specific nervous system diseases, our meta-analysis showed that stroke was associated with severe COVID-19 disease (8 studies [17, 38, 50, 57, 64, 65, 71, 80], 3178 patients; OR = 1.95, 95%CI: 1.11 to 3.42, P = 0.020; I2 = 30.2%) (Fig. 6A). There were no significant differences in the prevalence of epilepsy (2 studies [41, 57], 1003 patients; OR = 1.00, 95%CI: 0.42 to 2.35, P = 0.994; I2 = 0.0%) and dementia (3 studies [44, 54, 65], 1041 patients; OR = 2.39, 95%CI: 0.55 to 10.48, P = 0.247; I2 = 61.9%) between severe and non-severe patients (Fig. 6B and C).
Fig. 6.
Association between (a) stroke, (b) epilepsy, (c) dementia and the severity of COVID-19.
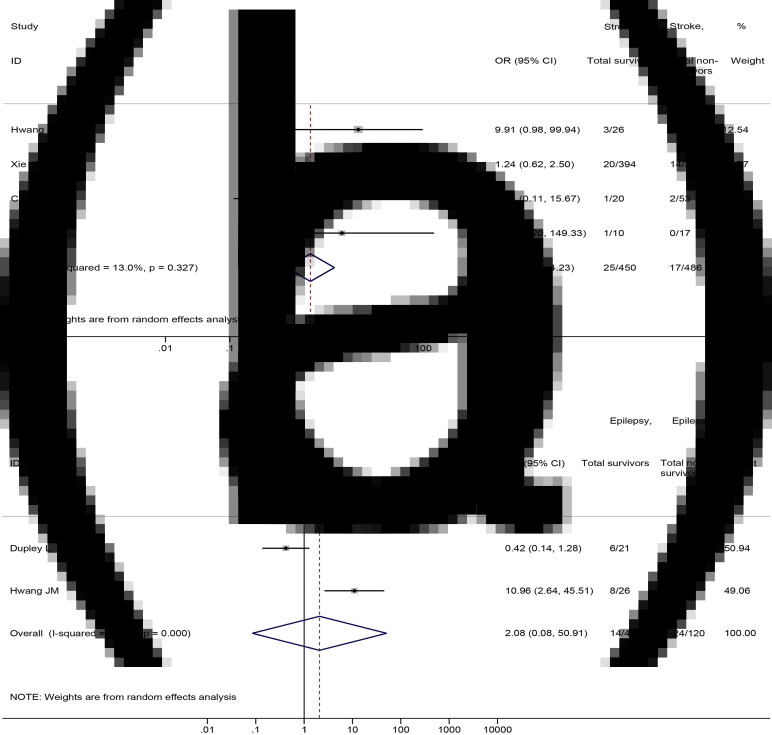
No significant differences were found in the prevalence of stroke (4 studies [21, 40, 72, 77], 936 patients; OR = 1.79, 95%CI: 0.76 to 4.23, P = 0.185; I2 = 13.0%) and epilepsy (2 studies [28, 40], 167 patients; OR = 2.08, 95%CI: 0.08 to 50.91, P = 0.654; I2 = 92.0%) between non-survival and survival patients (Fig. 7).
Fig. 7.
Association between (a) stroke and (b) epilepsy and the mortality of COVID-19.
Meta-regression analyses
Univariate meta-regression analyses revealed that the sample size of individual study was not the source of heterogeneity or the factor affecting the association between nervous system diseases and COVID-19 severity or mortality (Appendix Figs 3 and 4) and the association between cerebrovascular disease and COVID-19 severity or mortality (Appendix Figs. 5 and 6).
Publication bias
The funnel plot and Egger's test revealed that there was no statistically significant publication bias of nervous system diseases associated with severity (P = 0.090) (Appendix Fig. 7) and mortality of COVID-19 (P = 0.061) (Appendix Fig. 8). We found that there was a possibility of publication bias for the association between cerebrovascular disease and COVID-19 severity (P = 0.011) (Appendix Fig. 9). There was no statistically significant publication bias for the association between cerebrovascular disease and COVID-19 mortality (P = 0.100) (Appendix Fig. 10).
Discussion
Principal findings
This study included 69 studies and systematically assessed the association between nervous system diseases and the severity and mortality of patients with COVID-19. Specifically, we also conducted meta-analyses to explore the association between cerebrovascular disease and severity or mortality of patients with COVID-19, as well as the association between stroke, epilepsy, dementia and COVID-19 severity and mortality. Our meta-analyses revealed that nervous system diseases were associated with severity and mortality of patients with COVID-19. Cerebrovascular disease was associated with severity and mortality of patients with COVID-19. Severe COVID-19 patients were more likely to have a stroke compared with non-severe patients. There were no significant associations between epilepsy and dementia and COVID-19 severity or mortality. Sensitivity analyses suggested that the results did not change substantially after excluding studies published in Chinese.
Comparison with other studies
A previous meta-analysis, including three studies with a total sample size of 1299, demonstrated that a significant relationship between patients with severe COVID-19 and cerebrovascular disease (OR = 3.89, 95% CI: 1.64 to 9.22, P = 0.002) [85]. Another meta-analysis, including seven studies involving 2585 patients, showed that cerebrovascular disease was significantly associated with severe COVID-19 disease (RR = 1.88, 95% CI: 1.00 to 3.51, P = 0.05) and five studies involving 936 patients revealed that cerebrovascular disease was associated with COVID-19 mortality (RR = 2.38, 95%CI: 1.92 to 2.96, P < 0.001) [5]. Compared with these two studies, our study reached similar conclusions. However, it has distinct advantages and our results are more comprehensive. Our study meta-analysed 37 studies involving a total of 10 015 COVID-19 patients between cerebrovascular disease and COVID-19 severity, at the same time, 24 studies with a total sample size of 6822 between cerebrovascular disease and COVID-19 mortality. Therefore, our meta-analysis has the advantage of expanding the sample size and including more research studies. To the best of our knowledge, the two previous meta-analyses that included studies completely came from China. In this study, we included 15 studies from the USA, Korea, Italy, UK, Austria, Iran, Israel, Saudi Arabia, Spain and Turkey, which expanded our research scope. Another difference between our study and previous meta-analyses is that we also analysed the relationship between detailed nervous system diseases including stroke, epilepsy, dementia and the severity and mortality of patients with COVID-19. Furthermore, we also performed sensitivity analyses and meta-regression analyses and investigated the publication bias, and these analyses indicated that results of our study were stable. Therefore, the results of our study are more systematic and comprehensive.
Implications for research and practice
Previous studies have reported that SARS and Middle East respiratory syndrome (MERS) patients with nervous system diseases are at a higher risk of poor outcomes [86, 87]. Our study revealed that nervous system diseases were associated with severity and mortality of patients with COVID-19. Previous studies have shown that SARS-CoV-1 can invade the nerves and cause direct central nervous system infection [88, 89], which may also be one of the pathogenic pathways of SARS-CoV-2. Furthermore, the SARS-CoV-2 virus may enter the cerebral circulation, and the interaction between the viral spike proteins and the ACE2 receptors expressed in the brain capillary endothelium may destroy the blood−brain barrier [90, 91]. SARS-CoV-2 can infect cardiomyocytes through ACE2 receptors and cause vascular damage and inflammation, making thrombus easy to form and increasing the risk of stroke [92, 93]. COVID-19 could also cause viral encephalitis and haemorrhagic necrosis in the mesial temporal lobes and thalamus [93]. These may be the potential mechanisms for the poor prognosis of COVID-19 patients with nervous system diseases. However, the exact mechanism of increased severity of COVID-19 in patients with nervous system diseases remains unclear, which requires further research to clarify.
Our meta-analyses found that cerebrovascular disease was associated with severity and mortality of patients with COVID-19. These findings highlight the need for neurologists to be vigilant to the high risk of serious illness and death associated with COVID-19 infection in patients with nervous system diseases. A systematic review showed that an increasing number of reports of COVID-19 patients with neurological disorders have added emergent experimental models with neuro-invasion, which is a reasonable concern because SARS-CoV-2 is a new neuropathogen [94]. However, at present, there is a lack of treatment strategies for COVID-19 patients with nervous system diseases. Therefore, protecting patients with nervous system diseases from COVID-19 is a problem worthy of our attention. To the best of our knowledge, there is currently no recommendation regarding the treatment strategies for nervous system diseases patients with COVID-19. The results of our meta-analysis also provide the latest references for the development of new guidelines. There is an urgent need for high-quality evidence-based guidelines to clarify the protective measures for patients with nervous system diseases, as well as care and treatment strategies for nervous system disease patients with COVID-19.
Strengths and limitations
Despite comprehensive analyses, our meta-analysis has many limitations. First, we found that some patients of included studies were still hospitalised at the end of the study and no studies reported the specific time period of nervous system diseases. Second, since we included cohort studies and case−control studies, there might be confounding factors that influence the relationship between nervous system diseases and COVID-19 severity as well as mortality. Third, there was much variation in eligibility for SARS-CoV-2 testing between studies or over time within studies. Fourth, we conducted meta-regression analysis and sensitivity analysis to explore the sources of heterogeneity, but the selected factors were not the sources of heterogeneity and the results of some meta-analyses may be affected by the high heterogeneity. Finally, the total number of patients with nervous system diseases included in analyses is relatively small even in this comprehensive literature review, resulting in some wide confidence intervals. As described above, these limitations showed that caution is required before drawing any firm conclusions in the absence of high-quality, comprehensive evidence.
Conclusions
Nervous system diseases were associated with severity and mortality of patients with COVID-19. Among them, cerebrovascular disease was associated with a high risk of severity and mortality of patients with COVID-19. However, due to the limitations of this study, more high-quality, large sample, multicentre trials are needed to provide robust evidence to support clinical practice.
Acknowledgements
The authors thank all investigators and supporters involved in this study.
Author contributions
YG, YMC and JHT planned and designed the study. YG, YMC, ML, MMN, MLY and ZWS participated in the literature search and data collection. YG, YMC and ML analysed the data. YG and YMC drafted the paper. YG, YMC and JHT revised the paper. All authors read and approved the final paper.
Financial support
This study was funded by the Emergency Research Project of Key Laboratory of Evidence-based Medicine and Knowledge Translation of Gansu Province (grant no. GSEBMKT-2020YJ01).
Role of the Funding Source
The funders had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the paper; and decision to submit the paper for publication.
Ethical standards
Not applicable.
Consent for publication
Not applicable.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0950268821000376.
click here to view supplementary material
Conflict of interest
The authors declare that they have no competing interests.
Data
All datasets generated for this study are included in the manuscript.
References
- 1.Xu XW, et al. (2020) Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ (Clinical Research ed) 368, m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Director-General's opening remarks at the media briefing on COVID-19: 11 March 2020. Published 11 March 2020. Available at https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-themedia-briefing-on-covid-19---11-march-2020.
- 3.World Health Organization. Coronavirus disease (COVID-2019) situation reports. Available at https://www.who.int/publications/m/item/weekly-operational-update---30-october-2020.
- 4.Wang D et al. (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323, 1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pranata R et al. (2020) Impact of cerebrovascular and cardiovascular diseases on mortality and severity of COVID-19 − systematic review, meta-analysis, and meta-regression. Journal of Stroke and Cerebrovascular Diseases: The Official Journal of National Stroke Association 29, 104949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu J et al. (2020) The association of cerebrovascular disease with adverse outcomes in COVID-19 patients: a meta-analysis based on adjusted effect estimates. Journal of Stroke and Cerebrovascular Diseases: The Official Journal of National Stroke Association 29, 105283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liberati A et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical Research ed) 339, b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: Interim guidance V 1.2. 13 March 2020. Available at https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected. Accessed October 20, 2020.
- 9.Liu M et al. (2020) The association between severe or dead COVID-19 and autoimmune diseases: a systematic review and meta-analysis. The Journal of Infection 81, e93–e95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gao Y et al. (2020) Association between tuberculosis and COVID-19 severity and mortality: a rapid systematic review and meta-analysis. Journal of Medical Virology. doi: 10.1002/jmv.26311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Henry BM et al. (2020) Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clinical Chemistry and Laboratory Medicine 58, 1021–1028. [DOI] [PubMed] [Google Scholar]
- 12.Gao Y et al. (2020) Impacts of immunosuppression and immunodeficiency on COVID-19: a systematic review and meta-analysis. The Journal of Infection 81, e93–e95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shakir R et al. (2016) Revising the ICD: stroke is a brain disease. Lancet (London, England) 388, 2475–2476. [DOI] [PubMed] [Google Scholar]
- 14.The Lancet (2019) ICD-11. Lancet (London, England) 393, 2275. [DOI] [PubMed] [Google Scholar]
- 15.Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. European Journal of Epidemiology 25, 603–605. [DOI] [PubMed] [Google Scholar]
- 16.Higgins JP et al. (2003) Measuring inconsistency in meta-analyses. BMJ (Clinical Research ed) 327, 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Argenziano MG et al. (2020) Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ (Clinical Research ed) 369, m1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cao J et al. (2020) Clinical features and short-term outcomes of 102 patients with corona virus disease 2019 in Wuhan, China. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America 71, 748–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen T et al. (2020) Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ (Clinical Research ed) 368, m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen T et al. (2020) Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China (2019): a single-centered, retrospective study. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences 75, 1788–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen X et al. (2020) Laboratory abnormalities and risk factors associated with in-hospital death in patients with severe COVID-19. Journal of Clinical Laboratory Analysis 34, e23467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen X et al. (2020) Detectable serum SARS-CoV-2 viral load (RNAaemia) is closely correlated with drastically elevated interleukin 6 (IL-6) level in critically ill COVID-19 patients. Clinical Infectious Diseases : An Official Publication of the Infectious Diseases Society of America 71, 1937–1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cheng A et al. (2020) Diagnostic performance of initial blood urea nitrogen combined with D-dimer levels for predicting in-hospital mortality in COVID-19 patients. International Journal of Antimicrobial Agents 56, 106110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheng L et al. (2020) Prognostic value of serum amyloid A in patients with COVID-19. Infection 48, 715–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chon Y et al. (2020) Adverse initial CT findings associated with poor prognosis of coronavirus disease. Journal of Korean Medical Science 35, e316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Colombi D et al. (2020) Well-aerated lung on admitting chest CT to predict adverse outcome in COVID-19 pneumonia. Radiology 296, e86–e96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.d'Arminio Monforte A et al. (2020) The importance of patients’ case-mix for the correct interpretation of the hospital fatality rate in COVID-19 disease. International Journal of Infectious Diseases: IJID: Official Publication of the International Society for Infectious Diseases 100, 67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dupley L, Oputa TJ and Bourne JT (2021) 30-day Mortality for fractured neck of femur patients with concurrent COVID-19 infection. European Journal of Orthopaedic Surgery & Traumatology: Orthopedie Traumatologie 31, 341–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feng Y et al. (2020) COVID-19 with different severity: a multicenter study of clinical features. American Journal of Respiratory and Critical Care Medicine 201, 1380–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fu J et al. (2020) The value of serum amyloid A for predicting the severity and recovery of COVID-19. Experimental and Therapeutic Medicine 20, 3571–3577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gao S et al. (2020) Risk factors influencing the prognosis of elderly patients infected with COVID-19: a clinical retrospective study in Wuhan. China. Aging (Albany NY) 12, 12504–12516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gayam V et al. (2020) Clinical characteristics and predictors of mortality in African-Americans with COVID-19 from an inner-city community teaching hospital in New York. Journal of Medical Virology 93, 812–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Götzinger F et al. (2020) COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. The Lancet Child & Adolescent Health 4, 653–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guan WJ et al. (2020) Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. The European Respiratory Journal 55, 2000547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Han MF et al. (2020) Assessing SARS-CoV-2 RNA levels and lymphocyte/T cell counts in COVID-19 patients revealed initial immune status as a major determinant of disease severity. Medical Microbiology and Immunology 209, 657–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hu H, Yao N and Qiu Y (2020) Comparing rapid scoring systems in mortality prediction of critically ill patients with novel coronavirus disease. Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine 27, 461–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hu L et al. (2020) Risk factors associated with clinical outcomes in 323 COVID-19 hospitalized patients in Wuhan, China. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America 71, 2089–2098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang H et al. (2020) Predictors of coronavirus disease 2019 severity: a retrospective study of 64 cases. Japanese Journal of Infectious Diseases 74, 54–60. [DOI] [PubMed] [Google Scholar]
- 39.Huang Q et al. (2020) Clinical characteristics and drug therapies in patients with the common-type coronavirus disease 2019 in Hunan, China. International Journal of Clinical Pharmacy 42, 837–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hwang JM et al. (2020) Neurological diseases as mortality predictive factors for patients with COVID-19: a retrospective cohort study. Neurological Sciences : Official Journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology 41, 2317–2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Itelman E et al. (2020) Clinical characterization of 162 COVID-19 patients in Israel: preliminary report from a large tertiary center. The Israel Medical Association Journal: IMAJ 22, 271–274. [PubMed] [Google Scholar]
- 42.Javanian M et al. (2020) Clinical and laboratory findings from patients with COVID-19 pneumonia in Babol North of Iran: a retrospective cohort study. Romanian Journal of Internal Medicine = Revue roumaine de medecine interne 58, 161–167. [DOI] [PubMed] [Google Scholar]
- 43.Kutluhan MA et al. (2020) Assessment of clinical features and renal functions in coronavirus disease-19: a retrospective analysis of 96 patients. International Journal of Clinical Practice 74, e13636. [DOI] [PubMed] [Google Scholar]
- 44.Lee JY et al. (2020) Epidemiological and clinical characteristics of coronavirus disease 2019 in Daegu, South Korea. International Journal of Infectious Diseases: IJID: Official Publication of the International Society for Infectious Diseases 98, 462–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lei S et al. (2020) Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine 21, 100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li M et al. (2020) Analysis of the risk factors for mortality in adult COVID-19 patients in Wuhan: a multicenter study. Frontiers in Medicine 7, 545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li Q et al. (2020) Clinical characteristics of SARS-CoV-2 infections involving 325 hospitalized patients outside Wuhan. Research Square, 1–15. doi: 10.21203/rs.3.rs-18699/v1. [DOI] [Google Scholar]
- 48.Li T et al. (2020) Clinical characteristics of 312 hospitalized older patients with COVID-19 in Wuhan, China. Archives of Gerontology and Geriatrics 91, 104185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu Q et al. (2020) Associations between serum amyloid A, interleukin-6, and COVID-19: a cross-sectional study. Journal of Clinical Laboratory Analysis 34, e23527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu S et al. (2020) Clinical characteristics and risk factors of patients with severe COVID-19 in Jiangsu province, China: a retrospective multicentre cohort study. BMC Infectious Diseases 20, 584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lu L et al. (2020) New-onset acute symptomatic seizure and risk factors in Corona virus disease 2019: a retrospective multicenter study. Epilepsia 61, e49–e53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Luo X et al. (2020) Prognostic value of C-reactive protein in patients with COVID-19. Clinical Infectious Diseases: an Official Publication of the Infectious Diseases Society of America 71, 2174–2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lyu PJ et al. (2020) The performance of chest CT in evaluating the clinical severity of COVID-19 pneumonia: identifying critical cases based on CT characteristics. Investigative Radiology 55, 412–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Maeda T et al. (2021) The association of interleukin-6 value, interleukin inhibitors, and outcomes of patients with COVID-19 in New York city. Journal of Medical Virology 93, 463–471. [DOI] [PubMed] [Google Scholar]
- 55.Pan L et al. (2020) Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. The American Journal of Gastroenterology 115, 766–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Qin C et al. (2020) Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America 71, 762–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Romero-Sánchez CM et al. (2020) Neurologic manifestations in hospitalized patients with COVID-19: the ALBACOVID registry. Neurology 95, e1060–e1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shabrawishi M et al. (2020) Clinical, radiological and therapeutic characteristics of patients with COVID-19 in Saudi Arabia. PloS One 15, e0237130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang CZ et al. (2020) Preliminary study to identify severe from moderate cases of COVID-19 using combined hematology parameters. Annals of Translational Medicine 8, 593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang D et al. (2020) Correlation analysis between disease severity and clinical and biochemical characteristics of 143 cases of COVID-19 in Wuhan, China: a descriptive study. BMC Infectious Diseases 20, 519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wang D et al. (2020) Clinical course and outcome of 107 patients infected with the novel coronavirus, SARS-CoV-2, discharged from two hospitals in Wuhan, China. Critical Care (London, England) 24, 188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang F et al. (2020) Establishing a model for predicting the outcome of COVID-19 based on combination of laboratory tests. Travel Medicine and Infectious Disease 36, 101782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang L et al. (2020) Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. The Journal of Infection 80, 639–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang L et al. (2020) Coronavirus disease 19 infection does not result in acute kidney injury: an analysis of 116 hospitalized patients from Wuhan, China. American Journal of Nephrology 51, 343–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang W et al. (2020) Clinical features and potential risk factors for discerning the critical cases and predicting the outcome of patients with COVID-19. Journal of Clinical Laboratory Analysis 34, e23547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang Y et al. (2020) Clinical characteristics of patients with severe pneumonia caused by the SARS-CoV-2 in Wuhan, China. Respiration; International Review of Thoracic Diseases 99, 649–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang Y et al. (2020) Clinical characteristics of patients infected with the novel 2019 coronavirus (SARS-Cov-2) in Guangzhou, China. Open Forum Infectious Diseases 7, ofaa187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wei Y et al. (2020) Clinical characteristics of 276 hospitalized patients with coronavirus disease 2019 in Zengdu District, Hubei Province: a single-center descriptive study. BMC Infectious Diseases 20, 549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wu G et al. (2020) Development of a clinical decision support system for severity risk prediction and triage of COVID-19 patients at hospital admission: an international multicentre study. The European Respiratory Journal 56, 2001104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wu J et al. (2020) Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). Journal of Internal Medicine 288, 128–138. [DOI] [PubMed] [Google Scholar]
- 71.Wu S et al. (2020) Identification and validation of a novel clinical signature to predict the prognosis in confirmed COVID-19 patients. Clinical Infectious Diseases : An Official Publication of the Infectious Diseases Society of America 71, 3154–3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Xie JF et al. (2020) Clinical characteristics and outcomes of critically ill patients with novel coronavirus infectious disease (COVID-19) in China: a retrospective multicenter study. Intensive Care Medicine 46, 1863–1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yan X et al. (2020) Clinical characteristics and prognosis of 218 patients with COVID-19: a retrospective study based on clinical classification. Frontiers in Medicine 7, 485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yan Y et al. (2020) Clinical characteristics and outcomes of patients with severe Covid-19 with diabetes. BMJ Open Diabetes Research & Care 8, e001343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yang Q et al. (2020) Analysis of the clinical characteristics, drug treatments and prognoses of 136 patients with coronavirus disease 2019. Journal of Clinical Pharmacy and Therapeutics 45, 609–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yang X et al. (2020) Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. The Lancet Respiratory Medicine 8, 475–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yuan M et al. (2020) Association of radiologic findings with mortality of patients infected with 2019 novel coronavirus in Wuhan, China. PloS One 15, e0230548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang G et al. (2020) Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. Journal of Clinical Virology : The Official Publication of the Pan American Society for Clinical Virology 127, 104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhang H et al. (2020) Clinical and hematological characteristics of 88 patients with COVID-19. International Journal of Laboratory Hematology 42, 780–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhang JJ et al. (2020) Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 75, 1730–1741. [DOI] [PubMed] [Google Scholar]
- 81.Zhang L et al. (2020) Diarrhea and altered inflammatory cytokine pattern in severe coronavirus disease 2019: impact on disease course and in-hospital mortality. Journal of Gastroenterology and Hepatology. doi: 10.1111/jgh.15166. [DOI] [PubMed] [Google Scholar]
- 82.Zhao Y et al. (2020) Abnormal immunity of non-survivors with COVID-19: predictors for mortality. Infectious Diseases of Poverty 9, 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zheng F et al. (2020) Clinical characteristics of 161 cases of corona virus disease 2019 (COVID-19) in Changsha. European Review for Medical and Pharmacological Sciences 24, 3404–3410. [DOI] [PubMed] [Google Scholar]
- 84.Zou W et al. (2020) [Comparison of recovery phase CT features between mild/moderate and severe/critical coronavirus disease 2019 patients]. Zhongguo yi xue ke xue yuan xue bao Acta Academiae Medicinae Sinicae 42, 370–375. [DOI] [PubMed] [Google Scholar]
- 85.Wang B et al. (2020) Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging 12, 6049–6057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chen CY et al. (2005) Clinical features and outcomes of severe acute respiratory syndrome and predictive factors for acute respiratory distress syndrome. Journal of the Chinese Medical Association: JCMA 68, 4–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lee SY, Khang YH and Lim HK (2019) Impact of the 2015 Middle East respiratory syndrome outbreak on emergency care utilization and mortality in South Korea. Yonsei Medical Journal 60, 796–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gu J et al. (2005) Multiple organ infection and the pathogenesis of SARS. The Journal of Experimental Medicine 202, 415–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Xu J et al. (2005) Detection of severe acute respiratory syndrome coronavirus in the brain: potential role of the chemokine mig in pathogenesis. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America 41, 1089–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Patel U et al. (2021) Pre-existing cerebrovascular disease and poor outcomes of COVID-19 hospitalized patients: a meta-analysis. Journal of Neurology 268, 240–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Baig AM et al. (2020) Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chemical Neuroscience 11, 995–998. [DOI] [PubMed] [Google Scholar]
- 92.Hamming I et al. (2004) Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. The Journal of Pathology 203, 631–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lee KW et al. (2020) Stroke and novel coronavirus infection in humans: a systematic review and meta-analysis. Frontiers in Neurology 11, 579070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Montalvan V, et al. (2020) Neurological manifestations of COVID-19 and other coronavirus infections: a systematic review. Clinical Neurology and Neurosurgery 194, 105921. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0950268821000376.
click here to view supplementary material
Data Availability Statement
All datasets generated for this study are included in the manuscript.