Abstract
Objective
The prevalence of multiple sclerosis (MS)-related fatigue may have changed due to new diagnostic criteria and new disease modifying drugs. We aimed to assess the prevalence of fatigue in a contemporary MS cohort, and to explore associations between fatigue and clinical and demographic factors.
Methods
This is a cross-sectional study of the MS population in three Norwegian counties. Fatigue was assessed with the Fatigue Scale for Motor and Cognitive Functions (FSMC). We also assessed self-reported anxiety, depression and daytime sleepiness.
Results
The response rate was 64% (1599/2512). The mean age of the participants was 52 ± 13 years, median EDSS was 2.5 (IQR 1.5-3.0) and median disease duration from onset was 16 years (IQR 8-25). We found a prevalence of fatigue of 81%. Women had a higher prevalence of fatigue than men (83% vs 78%, p = 0.02). The prevalence increased with age (p < 0.001) and with increasing disease severity (p < 0.001), but in multivariate analyses, only sex and disease severity remained independent determinants of fatigue. Anxiety, depression, and daytime sleepiness were more prevalent in patients with fatigue than in those without fatigue (all p-values < 0.001).
Conclusion
The prevalence of fatigue is high in contemporary patients with MS. Fatigue is associated with female sex and level of disability, as well as with anxiety, depression and excessive daytime sleepiness.
Keywords: Multiple sclerosis, fatigue, prevalence, cohort study
Introduction
The prevalence of multiple sclerosis (MS) in Norway was 203/100 000 in 2012, and the prevalence was 200/100 000 in the Eastern region including Oslo county.1 The estimate for Buskerud county was 214/100.000 in 20142 and 261/100.000 for Telemark county in 2019.3 Fatigue is one of the main causes of impaired quality of life among patients with MS, independent of depression and disability.4 It is one of the major causes of inability to work in patients with MS.5–7 Fatigue can occur at any stage and at any time in the course of the disease. While we have new disease modifying drugs that are efficient at limiting disease progression and neurological deterioration, we do not have effective pharmacological treatment specifically aimed at ameliorating fatigue.8 Physical activity has been shown to reduce the level of fatigue,9 and some studies have shown that cognitive behavioral therapy reduces fatigue, but further studies are needed to determine its long-term effect.10,11
A commonly used definition of fatigue is “a subjective lack of physical and/or mental energy that is perceived by the individual or caregiver to interfere with usual or desired activities” from the 1998 Multiple Sclerosis Council for Clinical Practice Guidelines.12 Another definition is “an overwhelming sense of tiredness, a lack of energy, or feelings of exhaustion, distinct from sadness or weakness, which is perceived by the individual or the caregiver to interfere with usual or desired activity.”13 However, there is currently no universally accepted definition of fatigue. Fatigue is a subjective experience, and it is difficult to measure. Several self-report scales have been developed and different scales are used in different studies without having a “gold standard”. Fatigue often co-exists with other conditions like depression and sleep disturbances, and the differentiation between these are difficult. Several possible mechanisms have been proposed to cause fatigue, which is believed to be multifactorial. This may contribute to the fact that at present, fatigue is a poorly understood and relatively unexplored symptom.
To our knowledge there have been no larger, population-based studies on the prevalence of fatigue in MS for almost 20 years.14 Previous studies have reported a prevalence ranging between 50–90%.14–16
Objectives
Our objectives were to determine the prevalence of fatigue in the current MS population in Norway, and to assess its relation to sex, age, phenotype, disease severity and duration. Our hypothesis was that the prevalence of fatigue in patients with MS is lower than previously reported due to changes in diagnostic criteria,17 possibly resulting in the detection of more benign cases,18 and the introduction of more efficient disease modifying drugs.19
Material and methods
Study design
This is a cross-sectional cohort study of patients with MS in the Norwegian counties Buskerud, Oslo and Telemark (BOT). The study employed self-reported questionnaires combined with a comprehensive registry comprising demographic, clinical, and socioeconomic data. The study was performed in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki)20 and approved by the Regional Ethics Committee (REK 2015/670). All patients provided written informed consent.
Setting
The BOT registry contains information on 3965 patients diagnosed with MS between 1934 and 2017 at the hospitals Vestre Viken Hospital Trust, Telemark Hospital Trust, and Oslo University Hospital (OUS). These hospitals serve a population of 1.17 million people (490 000, 170 000, and 510 000 respectively) in South-East Norway.
Participants
The patients in the BOT database were identified through a search in the electronic patient record system for the ICD-10 diagnosis “G35 multiple sclerosis” in March 2017 and again in January 2018. With the exception of patients whom we knew were incapacitated due to advanced disease, all the patients in the registry who were alive and residing within the three counties as of 2017, were invited to participate in the study. From December 2017 to June 2019, 2512 patients were mailed questionnaires including the Fatigue Scale for Motor and Cognitive Functions (FSMC), the Epworth Sleepiness Scale (ESS) and the Hospital Anxiety and Depression Scale (HADS). During the same period, a small group of three experienced neurologists with a special interest in MS reviewed all the hospital records and collated information on disease onset, diagnosis, disease progression, disease severity and treatment.
The patients who were not invited to participate in the study and the patients who did not respond or responded incompletely on the questionnaires are referred to as non-participants.
Data sources/measurements
The FSMC is a 20 item scale developed as a measurement of cognitive and motor fatigue. Patients with a subscore of 22 points or higher for either cognitive or motor fatigue, or 43 points or more for the total score, including both subscales, were deemed to have fatigue. The level of fatigue was subdivided into mild, moderate and severe fatigue. A score of 43–52 signifies mild fatigue, 53–62 signifies moderate fatigue, and >63 is severe fatigue. For cognitive fatigue, a subscore of 22–27 indicates mild fatigue, 28–33 moderate fatigue and ≥34 severe fatigue. For motor fatigue, a subscore of 22–26 indicates mild fatigue, 27–31 moderate fatigue and ≥32 severe fatigue.21
Anxiety and depression were assessed by HADS. HADS is a fourteen item scale developed to assess anxiety and depression. Seven of the items relate to anxiety, and seven relate to depression. HADS has been validated in several studies and in different populations.22 A subscore of 8 or more in each subscale indicates anxiety or depression, a sub score of 8-10 is of borderline significance, while a score of 11 or higher denotes clinical depression or anxiety.
Pathological daytime sleepiness was assessed with the ESS. The ESS is a validated, 8-item questionnaire that uses a 4-point Likert scale to quantify the patient's likelihood of falling asleep in 8 sedentary circumstances.23 The ESS score (the sum of 8 item scores, rated 0–3) can range from 0 to 24. The higher the ESS score, the higher that person’s average sleep propensity in daily life (ASP), or their ‘daytime sleepiness’. A total ESS score greater than 10 is indicative of increased sleepiness.
We used validated Norwegian translations of the three questionnaires.24–26
The level of disability was quantified by the Kurtzke Expanded Disability Status Scale (EDSS).27 The assessments were made through review of medical records by three neurologists who are all Neurostatus certified.28 If we did not find an EDSS score but had sufficient information, we calculated Kurtzke Functional Systems Scores retrospectively and determined the EDSS score from these calculations. For the 1454 patient included in the study 8130 EDSS scores were documented, 3846 (47%) were assigned by the clinician assessing the patient, and 4284 (53%) assigned retrospectively. The EDSS scores were categorized as follows; EDSS 0–3.0, 3.5–6.0, 6.5–8.0, and 8.5–9.5.
Statistical methods
Data are presented as means ± standard deviation, median (interquartile range [IQR]), or numbers and percentages depending on distribution. Differences between participants and non-participants, as well as differences between patients with fatigue and patients without fatigue, were assessed using t-tests, Mann-Whitney U-tests or Chi-square tests depending on the distribution of the data. Associations were explored by uni- and multivariate linear regression or by binary logistic regression depending on the distribution of the dependent variables.
For the FSMC questionnaires, missing items were imputed using the mean of the relevant scale (cognitive/motor) if 3 items, at most, were missing; if more than 3 items were missing, the whole questionnaire was classified as a missing value.29 Fatigue was categorized as none, mild, moderate, or severe.
Age was categorized by decades. When testing differences across several categories, we used ANOVA or Chi-square tests depending on the distribution. Post hoc tests were performed if there were over-all differences between categories. The analyses were performed in IBM SPSS statistics version 25.0.
Results
Participants
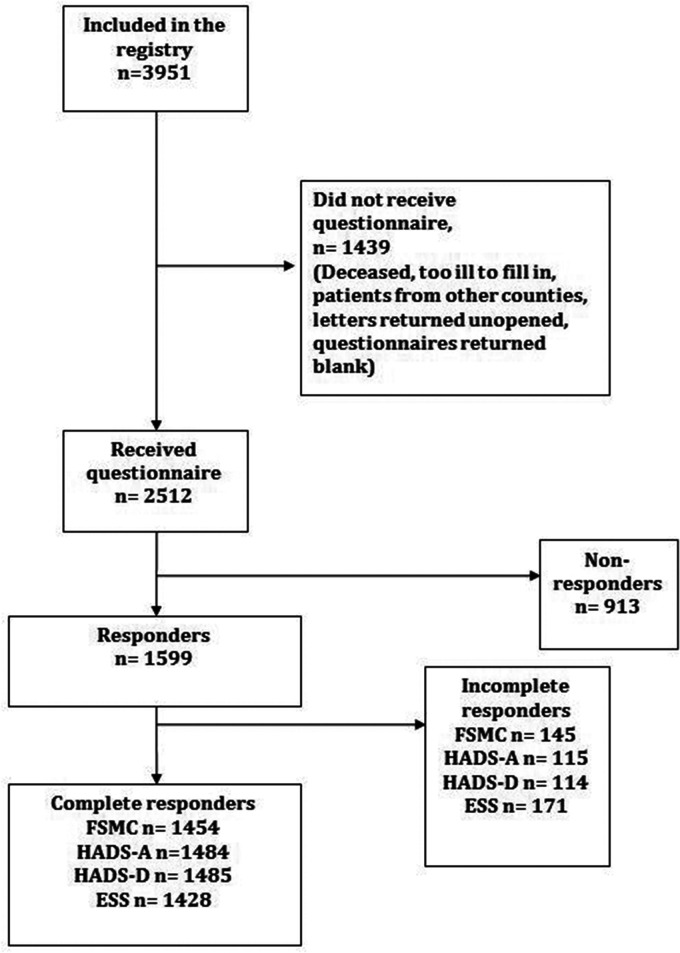
A total of 1599 patients returned the written consent form and questionnaires, 1454 of whom answered ≥17 questions on the FSMC. These patients were included in the results and are referred to as participants (Figure 1).
Figure 1.
Patient selection.
Legend: Flow chart depicting patient selection
Patient characteristics are detailed in Table 1. 70% of the participants were female. The mean age was 52 ± 13 years, 60% were ≥50 years. For 70% of the participants, MS symptom onset was more than 10 years before the survey, the median disease duration from onset was 16 years (IQR 8–25). For 48% of the participants, more than 10 years had elapsed since the time of diagnosis. The median EDSS was 2,5 (IQR 1.5–3.0). 83% had a relapsing-remitting MS, 9% had progressive MS and 9% were classified as unknown due to a lack of clear information on phenotype at onset.
Table 1.
Patient characteristics.
| All patients (n = 1454) | Fatigue (n = 1183) | No fatigue (n = 271) | p-value | |
|---|---|---|---|---|
| Sex, female - no (%) | 1012 (70) | 840 (71) | 172 (64) | 0.02 |
| Age – years | 52.1 ± 13.2 | 52.7 ± 13.1 | 48.6 ± 12.9 | <0.001 |
| Years from onset, median (IQR) | 16 (8–26) | 17 (8–26) | 13 (7–21) | 0.001 |
| Years from diagnosis,median (IQR) | 10 (5–18) | 10 (5–18) | 9 (4–16) | 0.01 |
| Relapsing MS No (%) | 1250 (86) | 1004 (85) | 246 (91) | 0.01 |
| EDSS, median (IQR)*DMT, No (%) | 2.5 (1.5–5.0) 857 (59) | 3.0 (2.0–5.5) 686 (58) | 2.0(1.0–3.0) 171 (63) | <0.001 0.13 |
*An EDSS score was available in 1343 patients at the time of the survey. DMT = Disease Modifying Treatment, EDSS = Expanded Disability Status Scale, IQR = inter quartile range, MS = multiple sclerosis
The participants were slightly younger and had shorter disease duration than the non-participants (Supplementary Table 1).
Prevalence of fatigue
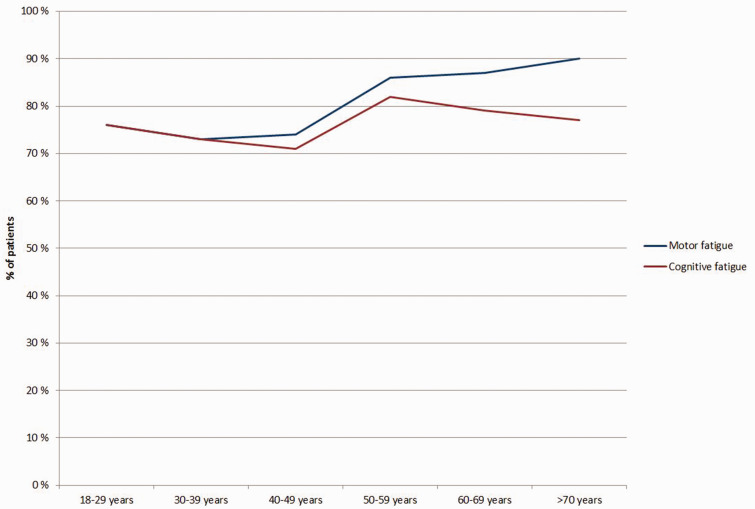
Based on total fatigue score, 1182 patients (81%) had fatigue. Among these, 15% had mild fatigue, 19% had moderate fatigue and 67% had severe fatigue. 1119 patients (77%) had cognitive fatigue and 1188 patients (82%) had motor fatigue. Patients younger than 40 years had equal levels of cognitive and motor fatigue, the patients older than 40 had more motor fatigue than cognitive fatigue (Figure 2).
Figure 2.
Motor and cognitive fatigue by age.
Legend: The prevalence of motor fatigue (blue graph) and cognitive fatigue (red graph) stratified by age.
Sex
Fatigue was more prevalent in females than in males (83% vs 78%, p = 0.02). The association remained after adjusting for age, EDSS and depression/anxiety (p < 0.001).
Age
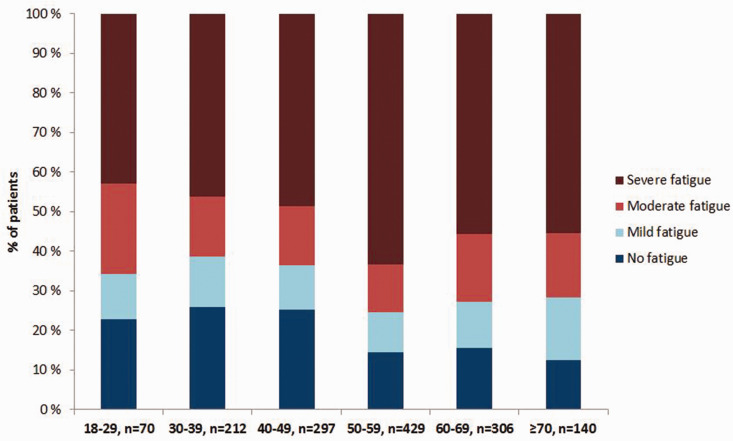
The prevalence of fatigue increased with age (Figure 3) and was significantly higher in patients aged ≥50 compared with those aged <50 (86% vs 75%, p < 0.001). The association between fatigue and age was no longer significant after adjusting for sex, EDSS and anxiety/depression.
Figure 3.
Fatigue severity by age.
Legend: The severity of fatigue stratified by patient age. The prevalence of severe fatigue peaked in patients aged 50–59.
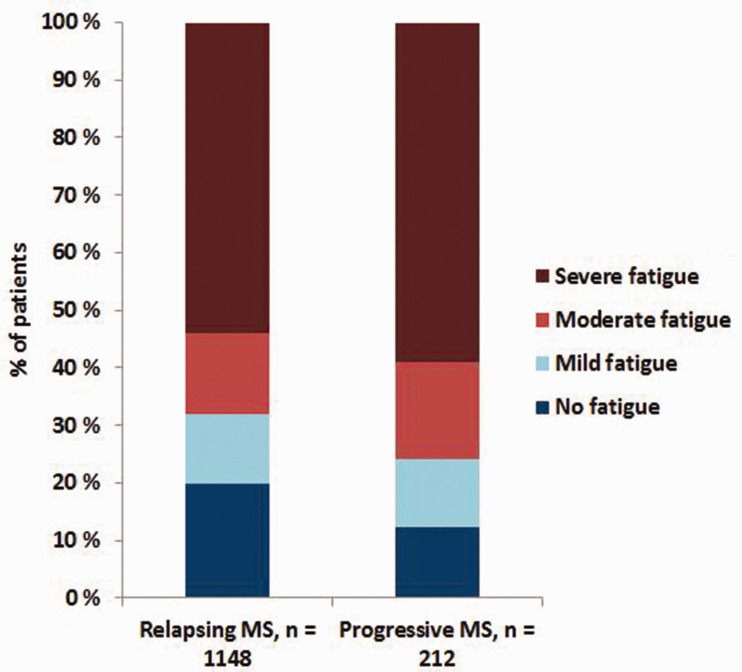
MS phenotype
The prevalence of fatigue was higher in patients with progressive MS (88% compared to 80% in the RR-MS group; p = 0.03) (Figure 4). The mean age of the patients with progressive disease at the time of the survey was 63 ± 10 years, whereas the mean age in the patients with relapsing disease was 50 ± 13 years (p < 0.001). The median EDSS was higher in patients with progressive disease at onset than in patients with relapsing disease at onset (p < 0.001). When adjusting for age and EDSS, the association between phenotype and fatigue was no longer significant (p = 0.81).
Figure 4.
Fatigue in relapsing vs progressive multiple sclerosis.
Legend: Bar chart depicting the severity of fatigue in relapsing versus progressive multiple sclerosis
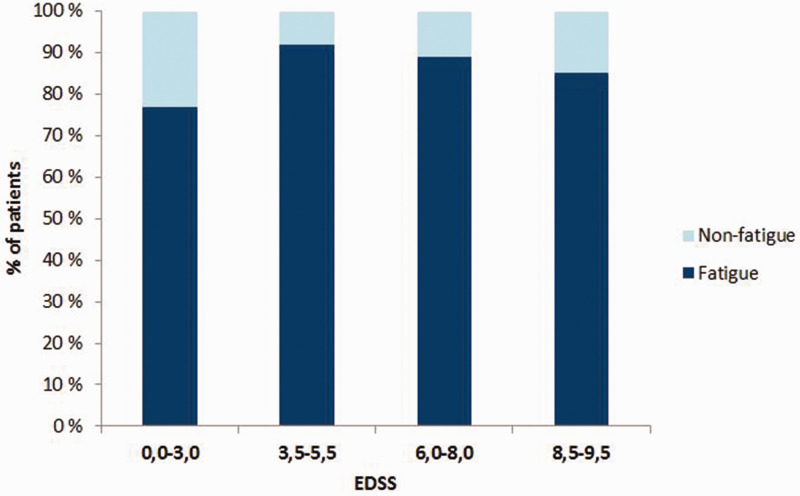
Disease severity
The median EDSS close to the time of the survey was 1.5 in patients younger than 40 years and thereafter increased gradually with age to 6.0 in the patients >70 years of age. The patients with fatigue had a higher EDSS than the patients without fatigue (EDSS 3.0 (IQR 2-2.5) compared to EDSS 2.0 (IQR 1-3) respectively). The rate of severe fatigue was highest in patients with EDSS between 3.5 and 5.5 (Table 2, Figure 5). Severe fatigue was significantly more prevalent in the group with EDSS above 3.0 (66% compared to 48% in the group with EDSS 0.0-3.0, p < 0.001).
Table 2.
Disease severity.
| EDSS 0.0–3.0, n = 799 | EDSS 3.5–5.5, n = 247 | EDSS 6.0–8.0, n = 264 | EDSS 8.5–9.5, n = 33 | |
|---|---|---|---|---|
| Age, mean (SD) | 48 ± 12 | 57 ± 11 | 63 ± 9 | 62 ± 8 |
| Sex, female - % | 76 | 61 | 63 | 64 |
| Fatigue - % | 77 | 92 | 89 | 85 |
| Severe fatigue - % | 48 | 71 | 62 | 64 |
EDSS = Expanded Disability Status Scale; SD = standard deviation
Figure 5.
Fatigue stratified by neurologic disability.
Legend: The prevalence of fatigue stratified by neurologic disability quantified by the Expanded Disability Status Scale (EDSS)
Geography
The prevalence of fatigue was slightly higher in Buskerud and Telemark than in Oslo (86% and 85% versus 75% respectively, p < 0.001). The mean age of the participants from Buskerud was 54 ± 13 years, from Telemark 53 ± 13 years, and from Oslo 50 ± 14 years. However, when adjusting for age there was still a significant difference between Oslo and the other two counties.
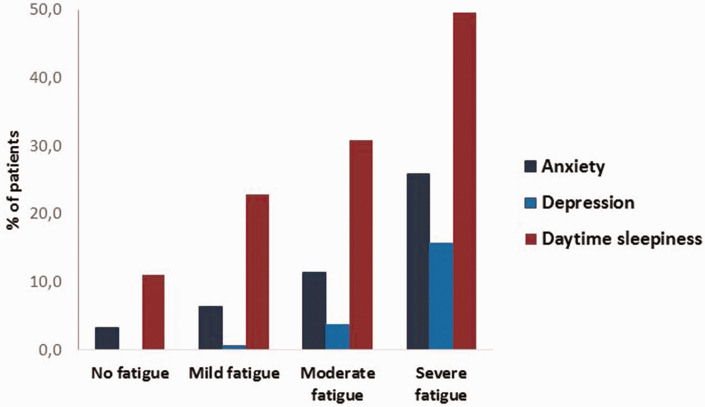
Anxiety, depression and excessive daytime sleepiness
Anxiety, depression, and daytime sleepiness were more prevalent in patients with fatigue than in those without fatigue (20% versus 3.3%; 11% versus 0%; and 42% versus 11%, respectively; all p-values < 0.001). The mean HADS-anxiety score was 6.1 ± 4.3, the HADS-depression score was 4.7 ± 3.7 and the mean ESS score was 8.15 ± 4.7. The association between the degree of fatigue and anxiety, depression, and daytime sleepiness is illustrated in Figure 6.
Figure 6.
Fatigue severity in relation to anxiety, depression and excessive daytime sleepiness.
Legend: The prevalence of anxiety, depression and excessive daytime sleepiness in patients related to the level of fatigue severity
Determinants of fatigue
Age, sex, MS phenotype, and MS disease severity were all associated with fatigue on univariate analyses. In multivariate analyses, however, only sex, disease severity and anxiety/depression remained independent determinants of fatigue. We observed the same pattern when we assessed fatigue score as a continuous parameter (Table 3).
Table 3.
Associations with fatigue score.
|
Univariate |
Multivariate |
|||
|---|---|---|---|---|
| β | p-value | Β | p-value | |
| Age | 0.115 | <0.001 | 0.029 | 0.25 |
| Sex | 0.083 | 0.002 | 0.08 | <0.001 |
| EDSS | 0.256 | <0.001 | 0.243 | <0.001 |
| Depression/ | 0.568 | <0.001 | 0.557 | <0.001 |
| Anxiety | ||||
EDSS = Expanded Disability Status Scale; SD = standard deviation
Discussion
We found that the prevalence of fatigue is high in contemporary patients with MS despite the advances that have been made in diagnostics and treatments over the past 20 years. We expected the prevalence to be lower compared to previous studies because the course of MS seem to be milder, at least during the last decade, partly due to improvements in diagnostics and treatment.18,30 Fatigue is more prevalent in women, and increases with the level of neurological disability. The rate of concomitant anxiety, depression and daytime sleepiness increased with increasing levels of fatigue.
Previous studies have found a prevalence of MS-related fatigue of between 50 and 90%.14–16,31 This quite substantial variation might be explained by differences in how study subjects are selected, the size of the study population, and in the methods used to assess fatigue. Rooney et al. (2018) found a prevalence of fatigue of 69%, using the fatigue severity scale (FSS ≥5) to measure fatigue severity and the Modified Fatigue Impact Scale (MFIS) to measure fatigue impact .They also found that both fatigue severity and impact were associated with higher levels of disability and greater depression and anxiety. The mean age of the study population was 46 ± 11.5 years.15 In 2008 Hadjimichael and colleagues found a prevalence of severe fatigue of 74% as assessed by the FSS questionnaire (FSS ≥36) in in a study population with a mean age of 48 ± 10.7 In 2003, Lerdal et al assessed the MS population of Oslo, based on the Oslo City MS registry. They found a prevalence of fatigue at 60% (n = 368). Fatigue was determined by the FSS questionnaire (FSS >5). The mean age of the subjects was 48 ± 10 years. A recent study from Eizaguirre and colleagues found a prevalence of fatigue of 52% when using the FSS questionnaire with a cut-off score of 4 (FSS ≥4). The mean age of the study population was 40 ± 10.5 years (range 18-60), the mean EDSS score was 2.43 ± 1.87 and the disease duration 10 ± 7 years.32 In a study validating the Finnish version of FSS from 2017 Rosti-Otajärvi and colleagues found a prevalence of fatigue of 65% (FSS ≥4). The mean age of the study population was 54 ± 11.4 years and the mean patient assessed EDSS score 4.0 ± 2.5.33
A population based cross-sectional study from Lausanne in Switzerland evaluated the prevalence of fatigue in a middle-aged normal population between 2014 and 2017. They included 2848 participants (53% women, age range 45–86 years) and found a prevalence of fatigue of 21.9% (95% CI 20.4% to 23.4%) as assessed by the FSS.34
Given the high proportion of patients with fatigue in our study, and the lack of a clear definition of fatigue, it is appropriate to ask if the tools we employed overdiagnosed fatigue. However, the FSMC questionnaire is highly sensitive and specific in detecting fatigued MS patients.21 In a validation study by Penner et al, both subscales significantly differentiated between patients and controls (p < 0.01), and the internal consistency (Cronbach’s alpha a > 0.91) as well as test–retest reliability (r > 0.80) were high. The scale scored high on both sensitivity and specificity in differentiating patients with MS from healthy controls,21 and was also found to have excellent convergent correlation with the Fatigue Severity Scale (FSS). The FSMC questionnaire was validated in a Danish cohort in 2017 with similar results.35
The mean age of the participants in our study was slightly higher than in the studies we have mentioned above for comparison. We now diagnose more MS patients, both earlier in the disease course and at an older age.30 The prevalence of fatigue was high in all age groups, but slightly higher in the older. This might contribute to the higher prevalence of fatigue in our study. Disease severity as assessed by EDSS increased with increasing age, and the rate of fatigue increases with increasing disease severity. We do not provide pharmacological treatment for fatigue at our hospitals, so the distribution of fatigue was not influenced by such treatment.
Patients with progressive disease at onset had more fatigue, but when adjusted for age and EDSS there was no significant difference in the rate of fatigue between patients with progressive MS and patients with relapsing MS. Earlier reports have shown inconsistent results regarding the association between disease subtype and fatigue. Kroencke et al found an association between fatigue and depression and the level of disability, but not with phenotype.36
We found a significant association between fatigue and anxiety/depression. For motor fatigue the association was stronger for depression, for cognitive fatigue the association was strong both for anxiety and depression. There is a large degree of symptom overlap between these conditions. Whether fatigue precedes depression and anxiety, or the causality is the other way around, remains to be determined.
We found a lower rate of fatigue in Oslo, the capital of Norway, than in Buskerud and Telemark counties. This might be due to the fact that Oslo has a different population composition, with a higher proportion of young people coming to Oslo to study and work.
Our hypothesis was that the prevalence of fatigue would be lower than reported in previous studies. The persistently high prevalence may be due to the fact that we have an older MS population. Previous studies have measured fatigue with the FSS, which focuses on motor fatigue. We used the FSMC, which captures both cognitive and motor fatigue. In a younger population, where employment rates presumably are higher, cognitive fatigue may be of greater importance.
Strengths and limitations
The BOT-registry comprises nearly all patients with MS within a defined geographical area, and the cohort is well characterized. The over-all response rate was 63%. However, the participants in this study differed somewhat from the non-participants in that they were slightly younger, had shorter disease duration and a slightly lower median EDSS score at onset. The questionnaires were sent and returned by postal mail. The motivation to participate may have been associated with the degree of fatigue. On the other hand, a high degree of fatigue may have prevented patients from partaking in the survey. We hypothesized that the prevalence of fatigue would be lower than previously reported, partly due to the introduction of more potent disease modifying drugs. However, an analysis of the complex interaction between disease modifying treatment and fatigue is beyond the scope of this manuscript. We plan to investigate this issue further.
This is a cross-sectional study that incorporates retrospective data. This complicates the assessment of the temporal relationship between events. The associations we have uncovered therefore do not imply causal relationships.
Conclusion
The prevalence of fatigue is high in contemporary patients with MS. MS fatigue is associated with female sex, and with the level of disability as assessed by EDSS. It is also associated with anxiety, depression and excessive daytime sleepiness.
Supplemental Material
Supplemental material, sj-jpg-1-mso-10.1177_2055217321999826 for High prevalence of fatigue in contemporary patients with multiple sclerosis by Line Broch, Cecilia Smith Simonsen, Heidi Øyen Flemmen, Pål Berg-Hansen, Åshild Skardhamar, Heidi Ormstad and Elisabeth Gulowsen Celius in Multiple Sclerosis Journal – Experimental, Translational and Clinical
Supplemental material, sj-jpg-2-mso-10.1177_2055217321999826 for High prevalence of fatigue in contemporary patients with multiple sclerosis by Line Broch, Cecilia Smith Simonsen, Heidi Øyen Flemmen, Pål Berg-Hansen, Åshild Skardhamar, Heidi Ormstad and Elisabeth Gulowsen Celius in Multiple Sclerosis Journal – Experimental, Translational and Clinical
Supplemental material, sj-jpg-3-mso-10.1177_2055217321999826 for High prevalence of fatigue in contemporary patients with multiple sclerosis by Line Broch, Cecilia Smith Simonsen, Heidi Øyen Flemmen, Pål Berg-Hansen, Åshild Skardhamar, Heidi Ormstad and Elisabeth Gulowsen Celius in Multiple Sclerosis Journal – Experimental, Translational and Clinical
Supplemental material, sj-pdf-4-mso-10.1177_2055217321999826 for High prevalence of fatigue in contemporary patients with multiple sclerosis by Line Broch, Cecilia Smith Simonsen, Heidi Øyen Flemmen, Pål Berg-Hansen, Åshild Skardhamar, Heidi Ormstad and Elisabeth Gulowsen Celius in Multiple Sclerosis Journal – Experimental, Translational and Clinical
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: LB has received an unrestricted research grant from Sanofi and advisory board honoraria from Merck. CSS has received unrestricted research grants from Sanofi and Novartis, and advisory board and/or speaker honoraria from Sanofi, Merck and Biogen. HØF has received unrestricted research grants from Biogen and Novartis, and advisory board and/or speaker honoraria Sanofi, Merck and Biogen. PBH has received an unrestricted research grant from Novartis and funding for travel or speaker's fees from Novartis, UCB, Biogen, Teva and Sanofi. EGC has received unrestricted research grants from Novartis and Sanofi, and advisory board and/or speaker honoraria from Biogen, Merck, Roche, Novartis, Sanofi and Teva.
ORCID iDs: Line Broch https://orcid.org/0000-0002-9317-4901
Cecilia Smith Simonsen https://orcid.org/0000-0002-9408-7199
Elisabeth Gulowsen Celius https://orcid.org/0000-0002-9127-6488
Supplemental material: Supplemental material for this article is available online.
References
- 1.Berg-Hansen P, Moen SM, Harbo HF, et al. High prevalence and no latitude gradient of multiple sclerosis in Norway. Mult Scler 2014; 20: 1780–1782. [DOI] [PubMed] [Google Scholar]
- 2.Simonsen CS, Edland A, Berg-Hansen P, et al. High prevalence and increasing incidence of multiple sclerosis in the norwegian county of Buskerud. Acta Neurol Scand 2017; 135: 412–418. [DOI] [PubMed] [Google Scholar]
- 3.Flemmen H, Simonsen CS, Berg-Hansen P, et al. Prevalence of multiple sclerosis in rural and urban districts in Telemark county, Norway. Mult Scler Relat Disord 2020; 45: 102352. [DOI] [PubMed] [Google Scholar]
- 4.Krupp LB, Alvarez LA, LaRocca NG, et al. Fatigue in multiple sclerosis. Arch Neurol 1988; 45: 435–437. [DOI] [PubMed] [Google Scholar]
- 5.Smith MM, Arnett PA. Factors related to employment status changes in individuals with multiple sclerosis. Mult Scler 2005; 11: 602–609. [DOI] [PubMed] [Google Scholar]
- 6.Marrie RA, Cutter G, Tyry T, et al. Validation of the NARCOMS registry: fatigue assessment. Mult Scler 2005; 11: 583–584. [DOI] [PubMed] [Google Scholar]
- 7.Hadjimichael O, Vollmer T, Oleen-Burkey M; North American Research Committee on Multiple Sclerosis. Fatigue characteristics in multiple sclerosis: the North American research committee on multiple sclerosis (NARCOMS) survey. Health Qual Life Outcomes 2008; 6: 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nourbakhsh B, Revirajan N, Morris B, et al. Safety and efficacy of amantadine, modafinil, and methylphenidate for fatigue in multiple sclerosis: a randomised, placebo-controlled, crossover, double-blind trial. Lancet Neurol 2021; 20: 38–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asano M, Finlayson ML. Meta-analysis of three different types of fatigue management interventions for people with multiple sclerosis: exercise, education, and medication. Mult Scler Int 2014; 2014: 798285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van den Akker LE, Beckerman H, Collette EH, et al.; TREFAMS-ACE Study Group. Cognitive behavioral therapy positively affects fatigue in patients with multiple sclerosis: results of a randomized controlled trial. Mult Scler 2017; 23: 1542–1553. [DOI] [PubMed] [Google Scholar]
- 11.Phyo AZZ, Demaneuf T, De LA, et al. The efficacy of psychological interventions for managing fatigue in people with multiple sclerosis: a systematic review and meta-analysis. Front Neurol 2018; 9: 149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.MS Council for Clinical Practice Guidelines. Fatigue and multiple sclerosis: evidence-based management strategies for fatigue in multiple sclerosis. Washington, DC: Paralyzed Veterans of America, 1998.
- 13.Krupp LB, Serafin DJ, Christodoulou C. Multiple sclerosis-associated fatigue. Expert Rev Neurother 2010; 10: 1437–1447. [DOI] [PubMed] [Google Scholar]
- 14.Lerdal A, Celius EG, Moum T. Fatigue and its association with sociodemographic variables among multiple sclerosis patients. Mult Scler 2003; 9: 509–514. [DOI] [PubMed] [Google Scholar]
- 15.Rooney S, Wood L, Moffat F, et al. Prevalence of fatigue and its association with clinical features in progressive and non-progressive forms of multiple sclerosis. Mult Scler Relat Disord 2019; 28: 276–282. [DOI] [PubMed] [Google Scholar]
- 16.Kister I, Bacon TE, Chamot E, et al. Natural history of multiple sclerosis symptoms. Int J MS Care 2013; 15: 146–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thompson AJ, Banwell BL, Barkhof F, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 2018; 17: 162–173. [DOI] [PubMed]
- 18.Sorensen PS, Sellebjerg F, Hartung HP, et al. The apparently milder course of multiple sclerosis: changes in the diagnostic criteria, therapy and natural history. Brain 2020; 143: 2637–2652. [DOI] [PubMed] [Google Scholar]
- 19.Filippi M, Bar-Or A, Piehl F, et al. Multiple sclerosis. Nat Rev Dis Primers 2018; 4: 43. [DOI] [PubMed] [Google Scholar]
- 20.Association WM. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013; 310: 2191–2194. [DOI] [PubMed] [Google Scholar]
- 21.Penner IK, Raselli C, Stocklin M, et al. The fatigue scale for motor and cognitive functions (FSMC): validation of a new instrument to assess multiple sclerosis-related fatigue. Mult Scler 2009; 15: 1509–1517. [DOI] [PubMed] [Google Scholar]
- 22.Bjelland I, Dahl AA, Haug TT, et al. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res 2002; 52: 69–77. [DOI] [PubMed] [Google Scholar]
- 23.Popp RF, Fierlbeck AK, Knuttel H, et al. Daytime sleepiness versus fatigue in patients with multiple sclerosis: a systematic review on the Epworth sleepiness scale as an assessment tool. Sleep Med Rev 2017; 32: 95–108. [DOI] [PubMed] [Google Scholar]
- 24.Beiske KK, Kjelsberg FN, Ruud EA, et al. Reliability and validity of a Norwegian version of the Epworth sleepiness scale. Sleep Breath 2009; 13: 65–72. [DOI] [PubMed] [Google Scholar]
- 25.Svenningsson A, Falk E, Celius EG, et al. Natalizumab treatment reduces fatigue in multiple sclerosis. Results from the TYNERGY trial; a study in the real life setting. PLoS One 2013; 8: e58643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leiknes K, Dalsbø TK, Siqveland J. Psychometric assessment of the Norwegian version of the hospital anxiety and depression scale (HADS). Oslo: Institute of Public Health, Health DoP, 2016. [Google Scholar]
- 27.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 1983; 33: 1444–1452. [DOI] [PubMed] [Google Scholar]
- 28.D'Souza M, Yaldizli Ö, John R, et al. Neurostatus e-scoring improves consistency of expanded disability status scale assessments: a proof of concept study. Mult Scler 2017; 23: 597–603. [DOI] [PubMed] [Google Scholar]
- 29.von Bismarck O, Dankowski T, Ambrosius B, et al. Treatment choices and neuropsychological symptoms of a large cohort of early MS. Neurol Neuroimmunol Neuroinflamm 2018; 5: e446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Simonsen CS, Flemmen H, Broch L, et al. The course of multiple sclerosis rewritten: a Norwegian population-based study on disease demographics and progression. J Neurol. 2020 Oct 22. doi: 10.1007/s00415-020-10279-7. Online ahead of print.URL:https://pubmed.ncbi.nlm.nih.gov/33090270/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Penner IK, Paul F. Fatigue as a symptom or comorbidity of neurological diseases. Nat Rev Neurol 2017; 13: 662–675. [DOI] [PubMed] [Google Scholar]
- 32.Eizaguirre MB, Ciufia N, Roman MS, et al. Perceived fatigue in multiple sclerosis: the importance of highlighting its impact on quality of life, social network and cognition. Clin Neurol Neurosurg 2020; 199: 106265. [DOI] [PubMed] [Google Scholar]
- 33.Rosti-Otajärvi E, Hämäläinen P, Wiksten A, et al. Validity and reliability of the fatigue severity scale in Finnish multiple sclerosis patients. Brain Behav 2017; 7: e00743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Galland-Decker C, Marques-Vidal P, Vollenweider P. Prevalence and factors associated with fatigue in the Lausanne middle-aged population: a population-based, cross-sectional survey. BMJ Open 2019; 9: e027070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oervik MS, Sejbaek T, Penner IK, et al. Validation of the fatigue scale for motor and cognitive functions in a Danish multiple sclerosis cohort. Mult Scler Relat Disord 2017; 17: 130–134. [DOI] [PubMed] [Google Scholar]
- 36.Kroencke DC, Lynch SG, Denney DR. Fatigue in multiple sclerosis: relationship to depression, disability, and disease pattern. Mult Scler 2000; 6: 131–136. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-jpg-1-mso-10.1177_2055217321999826 for High prevalence of fatigue in contemporary patients with multiple sclerosis by Line Broch, Cecilia Smith Simonsen, Heidi Øyen Flemmen, Pål Berg-Hansen, Åshild Skardhamar, Heidi Ormstad and Elisabeth Gulowsen Celius in Multiple Sclerosis Journal – Experimental, Translational and Clinical
Supplemental material, sj-jpg-2-mso-10.1177_2055217321999826 for High prevalence of fatigue in contemporary patients with multiple sclerosis by Line Broch, Cecilia Smith Simonsen, Heidi Øyen Flemmen, Pål Berg-Hansen, Åshild Skardhamar, Heidi Ormstad and Elisabeth Gulowsen Celius in Multiple Sclerosis Journal – Experimental, Translational and Clinical
Supplemental material, sj-jpg-3-mso-10.1177_2055217321999826 for High prevalence of fatigue in contemporary patients with multiple sclerosis by Line Broch, Cecilia Smith Simonsen, Heidi Øyen Flemmen, Pål Berg-Hansen, Åshild Skardhamar, Heidi Ormstad and Elisabeth Gulowsen Celius in Multiple Sclerosis Journal – Experimental, Translational and Clinical
Supplemental material, sj-pdf-4-mso-10.1177_2055217321999826 for High prevalence of fatigue in contemporary patients with multiple sclerosis by Line Broch, Cecilia Smith Simonsen, Heidi Øyen Flemmen, Pål Berg-Hansen, Åshild Skardhamar, Heidi Ormstad and Elisabeth Gulowsen Celius in Multiple Sclerosis Journal – Experimental, Translational and Clinical