Abstract
Background
We characterised the impact of COVID-19 on the socioeconomic conditions, access to gender affirmation services and mental health outcomes in a sample of global transgender (trans) and non-binary populations.
Methods
Between 16 April 2020 and 3 August 2020, we conducted a cross-sectional survey with a global sample of trans and non-binary people (n=849) through an online social networking app. We conducted structural equational modelling procedures to determine direct, indirect and overall effects between poor mental health (ie, depression and anxiety) and latent variables across socioecological levels: social (ie, reduction in gender affirming services, socioeconomic loss impact) and environmental factors (ie, COVID-19 pandemic environment).
Results
Anxiety (45.82%) and depression (50.88%) in this sample were prevalent and directly linked to COVID-19 pandemic environment. Adjusted for gender identity, age, migrant status, region, education and level of socioeconomic status, our final model showed significant positive associations between relationships of (1) COVID-19 pandemic environment and socioeconomic loss impact (β=0.62, p<0.001), (2) socioeconomic loss impact and reduction in gender affirming services (β=0.24, p<0.05) and (3) reduction in gender affirming services and poor mental health (β=0.19, p<0.05). Moreover, socioeconomic loss impact and reduction in gender affirming services were found to be partial mediators in this model.
Conclusion
The study results supported the importance of bolstering access to gender affirming services and strengthening socioeconomic opportunities and programmatic support to buffer the impact of COVID-19 pandemic environment on poor mental health among trans and non-binary communities globally.
Keywords: COVID-19, mental health & psychiatry, public health
Key questions.
What is already known?
Large-scale public health disasters like the COVID-19 pandemic has been linked with depression and anxiety, and such negative health outcomes are often exacerbated by several socioecological factors.
Current literature on COVID-19 and mental health that exclusively sample transgender (trans) and non-binary populations is severely lacking.
What are the new findings?
In this global sample of trans and non-binary people, positive screenings for anxiety and depression were prevalent, and were directly linked to the impact of COVID-19 pandemic environment.
Moreover, our structural equation model demonstrated and identified factors at the social/community level such as socioeconomic loss impact and reduction in gender affirming services to be important partial mediators on impact of COVID-19 on mental health.
What do the new findings imply?
The findings support the need for strengthening socioeconomic support across societal sectors that are able to facilitate access of trans and non-binary populations to gender affirming services and to address poor mental health outcomes.
These efforts are essential, particularly during a time when environmental and social structures within systems of healthcare and economy across global regions are strained.
Background
The novel COVID-19 pandemic has made a profound and indelible effect on all aspects of life, and has caused immeasurable economic, health and political consequences.1 2 Among these consequences are the detrimental effects of COVID-19 on the mental health of the global population.3 4 The proliferation of research focused on characterising the ramifications of the global pandemic has highlighted the exacerbation of the psychological burden experienced worldwide.3 4 Studies have reported elevated levels of adverse mental health conditions (eg, depression, anxiety, post-traumatic stress disorder and substance use) coupled with a reduction in access to healthcare services (eg, primary healthcare, mental healthcare), all of which have been directly attributable to COVID-19.3–5 Of even greater concern is the potential for the mental health-related effects of COVID-19 to further amplify the health inequities and stressors already experienced by transgender (trans) and non-binary people.6 7 A robust body of research published over the past decade consistently report high prevalence of depression and anxiety among trans people,8–10 and although research focused on the psychological impact of COVID-19 on trans and non-binary people is scant, researchers theorise that trans and non-binary people are disproportionately vulnerable to worsening mental health outcomes.7 11
Large-scale disasters are directly linked to population-level increases in negative health outcomes, including depression and anxiety.12 13 COVID-19 is likely to directly impact several socioecological factors that are linked to poor health outcomes among trans and non-binary people, including community-level (ie, access to gender affirming services) and social-level factors (ie, socioeconomic loss). The prioritisation and expansion of gender affirming services within health policy and health services have historically been met with resistance and are often overlook in myriad parts of the world. Prior to COVID-19, research has documented global health inequities and lack of access to healthcare services and competent providers, be it services specific to primary care, gender affirming services or mental health counselling and therapy services among trans people across low-income, middle-income and high-income countries.14–16 These health inequities stem from a multitude of systematic social and economic marginalisation, violence, stigma and discrimination across societial domains, particularly in healthcare settings.17 Thus, the urgency of COVID-19-related healthcare needs may have deprioritised gender affirming services and further exacerbate already existing social and structural inequities even further.6 11 Reductions in access to gender affirming services have been associated with negative mental health consequences among trans and non-binary people, highlighting one of the many potential unintended consequences of shifting healthcare priorities during the pandemic.18 Additionally, it is widely recognised that socioeconomic factors impact mental health outcomes, including among trans people.17 While we are unaware of any studies describing the association between socioeconomic status and mental health among trans and non-binary people due to COVID-19, the profound economic downturn has increased unemployment, financial insecurity and poverty among the vast majority of the global population, suggesting that worsening mental health outcomes is to follow.1
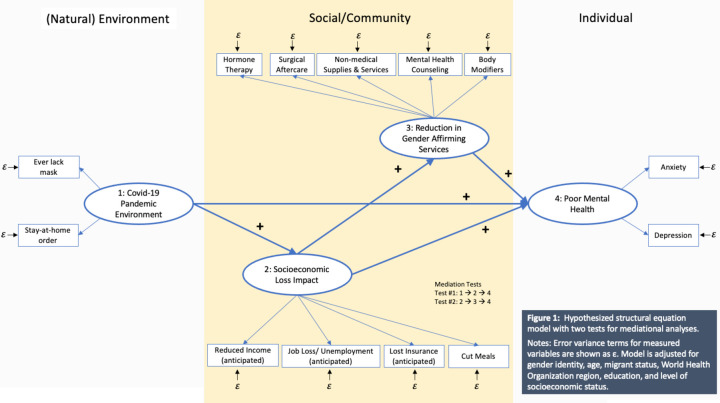
To understand how multilevel factors of mental health exacerbated by COVID-19 are linked among trans and non-binary people, globally, it is essential to examine pathways through which these factors interplay across multiple socioecological levels. Using an exploratory structural equation modelling (SEM) approach, we aim to: (1) test our hypothesised model (figure 1) that mental health outcomes among trans and non-binary people are impacted by social (ie, access to gender affirming services; socioeconomic impact) and environmental factors (ie, COVID-19 pandemic environment) and (2) assess the direct, indirect (ie, mediating) and overall effects of association between the COVID-19 pandemic environment, socioeconomic loss impact, access to gender affirming services on mental health outcomes. Specifically, our hypotheses would be:
Figure 1.
Hypothesised structural equation model with two proposed tests for mediation analyses. Error variance terms for measured variables are shown as ε. Model is adjusted for gender identity, age, migrant status, WHO region, education and level of socioeconomic status.
Socioeconomic loss impact mediates the relationship between COVID-19 environment and poor mental health.
Reduction in gender affirming services mediates the relationship between socioeconomic loss and poor mental health.
Methods
Study design and sample
We used the STrengthening the Reporting of OBservational Studies in Epidemiology guidelines for reporting cross-sectional studies, as displayed in table 1.
Table 1.
Reporting checklist for a cross-sectional study design using STrengthening the Reporting of OBservational studies in Epidemiology statement
| Item no. | Recommendation | Page no. | |
| Title and abstract | (a) Indicate the study’s design with a commonly used term in the title or the abstract. | 1–3 | |
| (b) Provide in the abstract an informative and balanced summary of what was done and what was found. | 3–34 | ||
| Introduction | |||
| Background/Rationale | 2 | Explain the scientific background and rationale for the investigation being reported. | 5 |
| Objectives | 3 | State specific objectives, including any prespecified hypotheses. | 5 |
| Methods | |||
| Study design | 4 | Present key elements of study design early in the paper. | 5–6 |
| Setting | 5 | Describe the setting, locations and relevant dates, including periods of recruitment, exposure, follow-up and data collection. | 5–6 |
| Participants | (a) Cohort study—give the eligibility criteria, and the sources and methods of selection of participants. Describe methods of follow-up. Case-control study—give the eligibility criteria, and the sources and methods of case ascertainment and control selection. Give the rationale for the choice of cases and controls. Cross-sectional study—give the eligibility criteria, and the sources and methods of selection of participants. | 5–6 | |
| (b) Cohort study—for matched studies, give matching criteria and number of exposed and unexposed. Case-control study—for matched studies, give matching criteria and the number of controls per case. | 5–6 | ||
| Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders and effect modifiers. Give diagnostic criteria, if applicable. | 6–7 |
| Data sources/measurement | 8 | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group. | 6–7 |
| Bias | 9 | Describe any efforts to address potential sources of bias. | 6–7 |
| Study size | 10 | Explain how the study size was arrived at. | 6–7 |
| Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. if applicable. Describe which groupings were chosen and why. | 6–7 |
| Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding. | 7 |
| (b) Describe any methods used to examine subgroups and interactions. | 7 | ||
| (c) Explain how missing data were addressed. | 7 | ||
| (d) Cohort study—if applicable, explain how loss to follow-up was addressed. Case-control study—if applicable, explain how matching of cases and controls was addressed. Cross-sectional study—if applicable, describe analytical methods taking account of sampling strategy. | 7 | ||
| (e) Describe any sensitivity analyses. | 7 | ||
| Results | |||
| Participants | 13 | (a) Report number of individuals at each stage of study—eg, numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up and analysed. | 7–8 |
| (b) Give reasons for non-participation at each stage. | n/a | ||
| (c) Consider use of a flow diagram. | n/a | ||
| Descriptive data | 14 | (a) Give characteristics of study participants (eg, demographic, clinical, social) and information on exposures and potential confounders. | 7–8 |
| (b) Indicate number of participants with missing data for each variable of interest. | 12 | ||
| (c) Cohort study—summarise follow-up time (eg, average and total amount). | n/a | ||
| Outcome data | 15 | Cohort study—report number of outcome events or summary measures over time. | n/a |
| Case-control study—report numbers in each exposure category, or summary measures of exposure. | 7–8 | ||
| Cross-sectional study—report number of outcome events or summary measures. | 7–8 | ||
| Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (eg, 95% CI). Make clear which confounders were adjusted for and why they were included. | 7–8 |
| (b) Report category boundaries when continuous variables were categorised. | 7–8 | ||
| (c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period. | n/a | ||
| Other analyses | 17 | Report other analyses done—eg, analyses of subgroups and interactions, and sensitivity analyses. | n/a |
| Discussion | |||
| Key results | 18 | Summarise key results with reference to study objectives. | 8–9 |
| Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias. | 9 |
| Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies and other relevant evidence. | 8–9 |
| Generalisability | 21 | Discuss the generalisability (external validity) of the study results. | 9–10 |
| Other information | |||
| Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based. | 10 |
Data for this study came from the Global COVID-19 Disparities Survey, an online cross-sectional study that surveyed members of Hornet and its social networking apps about the impact of COVID-19 pandemic on their personal and social experiences and well-being. Detailed study design and procedures are discussed elsewhere.19 The study was conducted between 16 April and 3 August 2020 and survey eligibility included participants who: (1) reported to be at least 18 years old and (2) provided an electronic written consent.
Procedures
Survey invitations were sent to active members’ inbox. We operationalised active members as members who have been using their apps in the last year. App members interested in the study were screened for eligibility. Following electronic informed consent, eligible app members answered the survey using their own device (eg, smartphones or tablet computers).
We performed multiple best-practice procedures to increase data quality of our web-based survey study.20 21 This included deduplication of responses by (a) flagging IP addresses that were not unique and (b) cross-matching any identical responses to 20 random variables. We did not find any deduplicated responses based on these procedures. We then removed participants who were indicated to: (a) have incomplete survey responses of 89% or below (n=271), (b) completed the survey before the minimum piloted time of 7 min (n=47), (c) provided illogical responses for sequential questions (n=3) and those with incomplete data with respect to our latent outcome variable (n=115).
Measures
Demographic (control) variables
We asked about participants’ demographic characteristics regarding their gender (categorised into non-binary/trans feminine/trans masculine), age (18–29/30–39/40–49/50+ years old), education attained (less than college/some college or more), WHO region (Europe/South-East Asia/Americas/Eastern Mediterranean/Western Pacific/Africa) and immigrant status (yes/no/not sure). Participants reported their socioeconomic income background as low, middle and upper socioeconomic level.
Natural environmental-level variable
COVID-19 pandemic environment as a latent variable was operationalised via two indicators relevant to the pandemic: (a) ever lack mask and (b) stay-at-home order. Specifically, we asked participants about whether they have ever lacked access to masks during the pandemic (yes/no), and whether they are in a location that ever issued ‘stay-at-home’ confinement orders (yes/no).
Social-level/community-level variables
We operationalised the latent variable socioeconomic loss impact using four indicators: (a) anticipated reduced income, (b) anticipated job loss/unemployment, (c) anticipated insurance loss, and (d) cut meals.
To assess the socioeconomic loss impact, we asked participants the following questions and dichotomise responses, respectively: (a) How much are you expecting your income to reduce because of the COVID-19 crisis? (yes=1% or more vs no=0%); (b) Do you expect to lose your job or be unemployed because of the COVID-19 crisis? (yes vs no/unsure); (c) Do you expect to lose your health insurance coverage because of the COVID-19 crisis? (yes=definitely yes/probably yes vs no=might or might not/probably not/definitely not); (d) Since the COVID-19 crisis began, have you had to cut the size of your meals or skip meals because there was not enough money for food? (yes vs no/unsure).
We operationalised the latent variable reduction in gender affirmation services via a series of items that asked whether the COVID-19 pandemic limited their access to the following gender affirming services: hormone therapy and/or medications (yes/no); surgical aftercare materials (eg, vaginal dilators) (yes/no); cosmetic supplies and services (eg, makeup, wigs and hair removal) (yes/no); mental health counselling (eg, therapy services) (yes/no) and body modifiers (eg, binders and packing materials) (yes/no).
Individual-level variable (outcome)
Poor mental health as a latent outcome variable was operationalised via screening positive for (a) depression and (b) anxiety. We used the 4-item Patient Health Questionnaire (PHQ-4), which screens for symptoms of depression and anxiety.22 This questionnaire asked participants about their mental health over the past 2 weeks regarding how often they have been bothered by the following problems: (1) feeling nervous, anxious or on edge, (2) not being able to stop or control worrying, (3) feeling down, depressed or hopeless and (4) little interest or pleasure in doing things. Responses were in a 4-point Likert response options from 0=not at all, 1=several days, 2=more than half the days to 3=nearly every day. A total score of ≥3 for the first two questions suggests positive for anxiety, and a total score of ≥3 for the last two questions suggests positive for depression. Responses were scored accordingly (M=1.47, SD=1.06, Cronbach’s α=0.85 for anxiety; M=1.39, SD=1.09, Cronbach’s α=0.83 for depression). The PHQ-4 is a validated questionnaire,23 and has been used by other researchers in the context of COVID-19 pandemic.24 25
Analysis plan
Analyses were restricted to 849 participants with complete data on our latent outcome variable of poor mental health (ie, depression and anxiety). Descriptive and bivariate analyses (ie, χ2 test or t-test) were conducted to examine relationships between the outcome of interest and independent variables (table 2). We then conducted sensitivity analyses to determine internal reliability of our scored variables (table 3). All Cronbach’s alphas have acceptable reliability (all α>0.80, range=0.83–0.85).
Table 2.
Sample characteristics by mental health outcomes (n=849)
| Total sample N (%) or M (SD) | Anxiety | Depression | |||||
| Screened positive N (%) or M (SD) |
Screened negative N (%) or M (SD) |
χ2 or t-test | Screened positive N (%) or M (SD) |
Screened negative N (%) or M (SD) |
χ2 or t-test | ||
| Total | 849 (100.00%) | 389 (45.82%) | 460 (54.18%) | 432 (50.88%) | 417 (49.12%) | ||
| Demographic (control) variables | |||||||
| Gender | |||||||
| Non-binary | 583 (68.67) | 248 (63.75) | 335 (72.83) | 0.017* | 276 (63.89) | 307 (73.62) | 0.004** |
| Trans feminine | 233 (27.44) | 124 (31.88) | 109 (23.70) | 140 (32.41) | 93 (22.30) | ||
| Trans masculine | 33 (3.89) | 17 (4.37) | 16 (3.48) | 16 (3.70) | 17 (4.08) | ||
| Age (years) | |||||||
| 18–29 | 437 (51.47) | 213 (54.76) | 224 (48.70) | <0.001*** | 243 (56.25) | 194 (46.54) | <0.001*** |
| 30–39 | 249 (29.33) | 129 (33.16) | 120 (26.09) | 137 (31.71) | 112 (26.86) | ||
| 20–49 | 112 (13.19) | 39 (10.03) | 73 (15.87) | 42 (9.72) | 70 (16.79) | ||
| 50+ | 51 (6.01) | 8 (2.06) | 43 (9.35) | 10 (2.31) | 41 (9.83) | ||
| Education attained | |||||||
| Less than college | 177 (20.97) | 95 (24.48) | 82 (17.98) | 0.021* | 112 (25.99) | 65 (15.74) | <0.001*** |
| Some college or more | 667 (79.03) | 293 (75.52) | 374 (82.02) | 319 (74.01) | 348 (84.26) | ||
| Socioeconomic level status | |||||||
| Lower | 127 (14.99) | 79 (20.31) | 48 (10.48) | <0.001*** | 87 (20.19) | 40 (9.62) | <0.001*** |
| Middle | 683 (80.64) | 293 (75.32) | 390 (85.15) | 323 (74.94) | 360 (86.54) | ||
| Upper | 37 (4.37) | 17 (4.37) | 20 (4.37) | 21 (4.87) | 16 (3.85) | ||
| WHO region | |||||||
| Europe | 382 (46.30) | 189 (49.74) | 193 (43.37) | <0.001*** | 224 (53.21) | 158 (39.11) | <0.001*** |
| South-East Asia | 215 (26.06) | 64 (16.84) | 151 (33.93) | 64 (15.20) | 151 (37.38) | ||
| Americas | 81 (9.82) | 48 (12.63) | 33 (7.42) | 46 (10.93) | 35 (8.66) | ||
| Eastern Mediterranean | 76 (9.21) | 47 (12.37) | 29 (6.52) | 48 (11.40) | 28 (6.93) | ||
| Western Pacific | 40 (4.85) | 16 (4.21) | 24 (5.39) | 21 (4.99) | 19 (4.70) | ||
| Africa | 31 (3.76) | 16 (4.21) | 15 (3.37) | 18 (4.28) | 13 (3.22) | ||
| Immigrant status | |||||||
| Yes | 103 (12.32) | 53 (13.84) | 50 (11.04) | 0.352 | 62 (14.62) | 41 (9.95) | 0.075 |
| No | 662 (79.19) | 295 (77.02) | 367 (81.02) | 323 (76.18) | 339 (82.28) | ||
| Unsure | 71 (8.49) | 35 (9.14) | 36 (7.95) | 39 (9.20) | 32 (7.77) | ||
| Natural environmental-level variable | |||||||
| COVID-19 pandemic environment | |||||||
| Ever lack masked | |||||||
| Yes | 112 (13.22) | 69 (17.74) | 43 (9.39) | <0.001*** | 76 (17.59) | 36 (8.67) | <0.001*** |
| No | 735 (86.78) | 320 (82.26) | 415 (90.16) | 356 (82.41) | 379 (91.33) | ||
| In a stay-at-home order | |||||||
| Yes | 651 (76.86) | 299 (77.06) | 352 (76.69) | 0.898 | 326 (75.64) | 325 (78.12) | 0.391 |
| No | 196 (23.14) | 89 (22.94) | 107 (23.31) | 105 (24.36) | 91 (21.88) | ||
| Social/Community-level variables | |||||||
| Socioeconomic loss impact | |||||||
| Reduced income (anticipated) | |||||||
| Yes | 607 (72.87) | 278 (72.77) | 329 (72.95) | 0.955 | 315 (74.12) | 292 (71.57) | 0.408 |
| No | 226 (27.13) | 104 (27.23) | 122 (27.05) | 110 (25.88) | 116 (28.43) | ||
| Job loss/Unemployment (anticipated) | |||||||
| Yes | 132 (15.64) | 86 (22.11) | 46 (10.11) | <0.001*** | 87 (20.19) | 45 (10.90) | <0.001*** |
| No | 712 (84.36) | 303 (77.89) | 409 (89.89) | 344 (79.81) | 368 (89.10) | ||
| Insurance loss (anticipated) | |||||||
| Yes | 99 (16.39) | 57 (21.27) | 42 (12.50) | 0.004** | 63 (20.59) | 36 (12.08) | <0.005** |
| No | 505 (83.61) | 211 (78.73) | 294 (87.50) | 243 (79.41) | 262 (87.92) | ||
| Cutting meals | |||||||
| Yes | 299 (37.52) | 189 (51.50) | 110 (25.58) | <0.001*** | 201 (49.63) | 98 (25.00) | <0.001*** |
| No | 498 (62.48) | 178 (48.50) | 320 (74.42) | 204 (50.37) | 294 (75.00) | ||
| Reduction in gender affirmation services | |||||||
| Hormone therapy† (n=346) | |||||||
| Yes | 115 (33.24) | 70 (45.75) | 45 (23.32) | <0.001*** | 78 (46.99) | 37 (20.56) | <0.001*** |
| No | 231 (66.76) | 83 (54.25) | 148 (76.68) | 88 (53.01) | 143 (79.44) | ||
| Surgical aftercare† (n=318) | |||||||
| Yes | 99 (31.13) | 53 (39.55) | 46 (25.00) | 0.006** | 59 (40.97) | 40 (22.99) | 0.001** |
| No | 219 (68.87) | 81 (60.45) | 138 (75.00) | 85 (59.03) | 134 (77.01) | ||
| Cosmetic supplies and services† (n=459) | |||||||
| Yes | 168 (36.60) | 93 (46.27) | 75 (29.07) | <0.001*** | 102 (45.54) | 66 (28.09) | <0.001*** |
| No | 291 (63.40) | 108 (53.73) | 183 (70.93) | 122 (54.46) | 169 (71.91) | ||
| Mental health counselling† (n=407) | |||||||
| Yes | 168 (41.28) | 96 (52.46) | 72 (32.14) | <0.001*** | 102 (51.26) | 66 (31.73) | <0.001*** |
| No | 239 (58.72) | 87 (47.54) | 152 (67.86) | 97 (48.74) | 142 (68.27) | ||
| Body modifiers† (n=402) | |||||||
| Yes | 134 (33.33) | 75 (42.86) | 59 (25.99) | <0.001*** | 85 (44.50) | 49 (23.22) | <0.001*** |
| No | 268 (66.67) | 100 (57.14) | 168 (74.01) | 106 (55.50) | 162 (76.78) | ||
Column percentages are reported. Sample sizes stratified by variables may not add up to total sample size due to missingness.
*P<0.05, **p<0.01, ***p<0.001.
†Applicable to participants who received gender affirmation services prior to COVID-19 pandemic.
Trans, transgender.
Table 3.
Descriptive statistics and reliabilities of scored variables (n=849)
| Poor mental health | M | SD | Range | Reliability* |
| Anxiety | 1.47 | 1.06 | 0–3 | 0.85 |
| Depression | 1.39 | 1.09 | 0–3 | 0.83 |
M=mean.
*Cronbach’s α.
We tested our hypothesised model by conducting structural equation modelling using maximum likelihood estimation procedures. To maximise accuracy of our estimates based on the modest sample size of our data, we used a non-parametric bootstrapping procedure with 100 iterations, which resampled and increased our confidence in statistical interpretation and inference. We controlled for age, gender identity, immigrant status, WHO region, education and socioeconomic status in our model. We used the following cut-off points to assess overall fitness of our SEM model: (a) χ2 badness-of-fit index value at p>0.05, (b) root mean square error approximation (RMSEA) value at <0.08, (c) non-normed fit index or Tucker-Lewis Index (TLI) value at >0.90, (d) comparative fit index (CFI) value at >0.90 and (e) standardised root mean square residual value at <0.08.26 All analyses were performed using StataSE V.16.1.27 Statistical significance was set at two-sided, p=0.05.
Results
Sample description
A total of 849 trans and non-binary identified participants were included in the analyses. Sample characteristics are displayed in table 1. Overall, 68.67% were non-binary, 27.44% were trans feminine and 3.89% were trans masculine. Most participants were between ages 18 and 29 (51.47%), had attained some college or more education (79.03%), reported coming from middle socioeconomic level status (80.64%), were currently residing in the European region (46.30%) and were non-immigrants (79.19%). More than three-fourths (76.86%) were located in an area with an issued stay-at-home order, and more than one-tenths (13.22%) reported ever lacking a mask. Particularly due to the COVID-19 pandemic, 72.87% of the participants reported anticipating reduced income, 15.64% job loss or unemployment and 16.39% insurance loss. Moreover, more than one-third (37.52%) reported cutting meals since COVID-19 pandemic began. A number of participants reported using gender affirming services such as hormone therapy (n=346), surgical aftercare (n=318), cosmetic supplies and services (n=459), mental health counselling (n=407) and body modifiers (n=402). Among those who were receiving gender affirming services prior to when COVID-19 pandemic began, more than one-third reported a reduction in hormone therapy (33.24%), surgical aftercare (31.13%), cosmetic supplies and services (36.60%), mental health counselling (41.28%) and body modifiers (33.33%). A total of 45.82% screened positive for anxiety and 50.88% for depression.
Bivariate analysis
Bivariate test results are displayed in table 2. With exception to immigration status, living in a location with stay-at-home order, and anticipated reduced income, all examined independent variables were associated with screening positive for depression and anxiety (all p values<0.05).
Compared with screening negative for anxiety and depression, a significantly greater proportion of those screening positive reported being trans feminine, aged 18–29 years and 30–39 years, having attained less than a college-level education, were from lower socioeconomic level and currently resided in the European, American or Eastern Mediterranean region. Moreover, screening positive was also significantly associated with participants who reported to ever lack access to a mask, anticipated job loss or unemployment, anticipated insurance loss and had cut meals. Among trans and non-binary participants who were receiving gender affirming services prior to COVID-19 pandemic, screening positive was also significantly associated with a reduction of all of the examined gender affirming services.
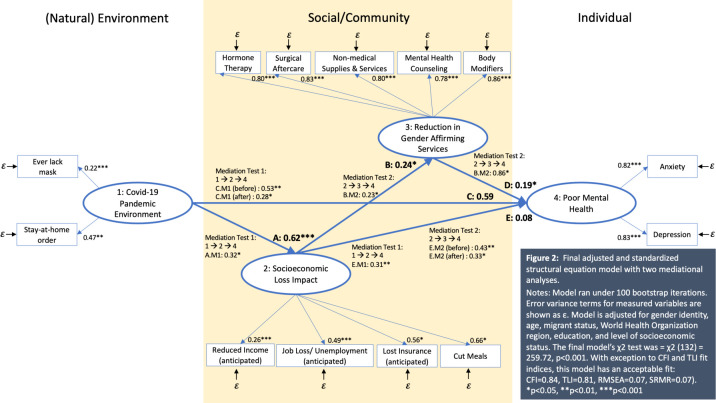
Final adjusted and standardised structural equation model
Our final adjusted and standardised SEM model is displayed in figure 2, adjusted for all demographic variables. The final model’s χ2 test was=χ2(132)=259.72, p<0.001. With exception to CFI and TLI fit indices, our overall adjusted and standardised model had an acceptable fit, with values of CFI=0.84, TLI=0.81, RMSEA=0.07 and SRMSR=0.07.
Figure 2.
Final adjusted and standardised structural equation model with two mediational analyses. Model ran under 100 bootstrap iterations. Error variance terms for measured variables are shown as ε. Model is adjusted for gender identity, age, migrant status, WHO region, education and level of socioeconomic status. The final model’s χ2 test was=χ2(132)=259.72, p<0.001. With exception to comparative fit index (CFI) and TLI fit indices, this model has an acceptable fit: CFI=0.84, TLI=0.81, root mean square error approximation=0.07, standardised root mean square residual=0.07). *P<0.05, **p<0.01, ***p<0.001.
Overall effects
Significant positive associations were found between relationships of (1) COVID-19 pandemic environment and socioeconomic loss impact (A: β=0.62, p<0.001), (2) between socioeconomic loss impact and reduction in gender affirming services (B: β=0.24, p<0.05) and (3) reduction in gender affirming services and poor mental health (D: β=0.19, p<0.05).
Positive associations were found between COVID-19 pandemic environment and poor mental health (C: β=0.59, p=0.28), as well as socioeconomic loss impact and poor mental health (E: β=0.08, p=0.87), however, these relationships were not significant.
Direct and indirect (mediating) effects
Partial mediations were observed in our two hypothesised mediational tests. The results of the mediational analyses are as follows:
Hypothesis 1
Socioeconomic loss impact partially mediated the relationship between COVID-19 pandemic environment and poor mental health, given that the direct effect between COVID-19 pandemic environment and poor mental health continued to be significant after socioeconomic loss impact was added in the model (C.M1 (before mediation): β=0.53, p<0.01 vs C.M1. (after mediation): β=0.28, p<0.05). The indirect positive effect between COVID-19 pandemic environment and socioeconomic loss impact (A.M1: β=0.32, p<0.05), as well as between socioeconomic loss impact and poor mental health (E.M1: β=0.31, p<0.01) remained statistically significant and provided further support for partial mediation.
Hypothesis 2
Reduction in gender affirming services partially mediated the relationship between socioeconomic loss impact and poor mental health, given that the direct effect between socioeconomic loss impact and poor mental health continued to be significant after reduction in gender affirming services was added in the model (E.M2: β=0.43, p<0.01 (before mediation) vs E.M2: β=0.33, p<0.05). The indirect positive effect between socioeconomic loss impact and reduction in gender affirming services (B.M2: β=0.23, p<0.05), as well as between reduction in gender affirming services and poor mental health (E.M2: β=0.86, p<0.05) remained statistically significant and provided further support for partial mediation.
Discussion
To our knowledge, this study provides one of the first exploratory model studies that map the impact of COVID-19 pandemic environment on trans and non-binary people’s mental health across the globe by linking together mediators across the socioecological levels. The sample was recruited across multiple geographical regions, providing a global insight into trans and non-binary’s mental health well-being in the early emergence of COVID-19 public health crisis. Screening positive for anxiety (45.82%) and depression (50.88%) in this sample was prevalent and were directly linked to COVID-19 pandemic environment. In addition, the results identified socioeconomic loss and reduction in gender affirmation services to be important mediators of this relationship. These findings corroborate with other studies that have sampled the general population and linked negative mental health outcomes to COVID-19 pandemic environment,24 28 underscoring the importance of addressing and exploring pathways and factors that can be leveraged across the socioecological levels to help alleviate and improve mental health outcomes among these important populations.
The findings of this study support our hypotheses. First, the results highlight the partial mediating impact of socioeconomic loss between COVID-19 pandemic environment and poor mental health—supporting previous research delineating the role of natural environmental large-scale disasters to increase negative health outcomes among already marginalised communities.12 13 We further add that the high negative mental health outcomes observed in this study is partially explained by socioeconomic-related stressors introduced by COVID-19 that impend stresses related to basic needs such as anticipated loss of income, jobs, insurance and food shortages. Minority stress may offer a possible explanation to these relationships, which posits that distal stressors (ie, low socioeconomic conditions) lead to chronic high levels of mental health distresses among marginalised communities.29 For instance, depression and anxiety due to stress associated with anticipating loss of income, jobs and insurance may be more pronounced for trans and non-binary individuals given their previous negative interactions with employers and insurers such as stigma and discrimination.8 17 A robust body of research published over the past decade consistently report prevalent work-related and insurance-related stigma and discrimination among these populations, specifically because of their gender identities.8 17 As such, COVID-19 could likely present a situation in which trans and non-binary people may be positioned to re-experience work-related and insurance-related distresses, particularly those who are anticipating job and insurance loss. While the extent in which the minority stress framework has been applied to socioecological models and studied in the context of natural environmental large-scale disasters like COVID-19 pandemic are lacking in the literature, it offers a possible contextual framework that links increase in screening positive for depression and anxiety as a result of anticipations of socioeconomic loss due to COVID-19 among already disenfranchised groups,30 including trans and non-binary communities. Future research should explore this postulation, as well as factors that can further explain and/or buffer against such mental distresses due to socioeconomic loss for trans and non-binary individuals.
Among those who reported using gender affirming services in this sample, more than one-third reported a reduction in hormone therapy (33.24%), surgical aftercare (31.13%), cosmetic supplies and services (36.60%), mental health counselling (41.28%) and body modifiers (33.33%). We found that the reduction in gender affirming services partially explained the relationship between socioeconomic loss and poor mental health outcomes. This result aligns with previous disparate research that individually linked gender affirming services and socioeconomic conditions with mental health outcomes among trans and non-binary populations.9 10 17 18 Our study expands this research by linking socioeconomic loss with reduced access to gender affirming services. As access to gender affirming services is related to cost of services and coverage in insurance, ensuring that gender affirming services remain affordable, flexible and covered during COVID-19 pandemic will be important in mollifying mental health outcomes. However, as insurers’ policies around gender affirming services may change, it is crucial for insurers to clearly communicate these changes in a timely manner to ensure that such services are not delayed and/or interrupted, particularly among those who may need to rely on out-of-network services as they move in response to the pandemic. Moreover, as healthcare systems in some parts of the world are facing reformation as a result of COVID-19 pandemic,31 32 it is crucial to recognise gender affirming services, including gender-related mental health services, as a legitimate part of healthcare coverage among trans and non-binary populations.
Finally, it is worth noting the other indicators associated with poor mental health outcomes. A significantly greater portion of participants in this sample screened positive for depression and anxiety who were trans feminine, young adults (between ages 18–29 and 30–39 years old), from lower socioeconomic levels, less than college educated and from regions of Europe, the Americas and Eastern Mediterranean. These results suggest that there are distinct mental health disparities across sociodemographic strata and regions among trans and non-binary populations globally. Given that trans and non-binary populations are a non-monolithic group,33 there is a need to explore how these results may differ by subgroups globally. Understanding the different pathways and factors related to mental health that may be shared and/or unique across strata and regions will be important in informing and tailoring interventions at a national and local level. For instance, given the partial mediation results of this study, understanding other socioecological indicators such as the kinds of healthcare systems (ie, single-payer vs universal healthcare), different health insurance plans (eg, health maintenance organisations, preferred provider organisations, exclusive provider organisations, point-of-service), various operationalisations of government-sponsored COVID-19 financial relief programmes, levels of government-issued COVID-19 mandates (ie, strict to non-strict quarantine, enforcement of physical distancing, stay-at-home mandates, etc) and living with unsupportive immediate families,34 could contribute to the social level and environmental level that impact mental health of trans and non-binary populations. Other social and structural factors describing the structural political climates across nations in regard to their acceptance, recognition and protection of trans and non-binary populations in social settings, may also play a role in how trans and non-binary populations experience depression and anxiety.
Moreover, while the linkages between socioeconomic loss and gender affirming services due to COVID-19 were predictive of this sample’s mental health outcomes, it is also crucial for researchers, programme designers and policymakers to address other basic social and structural needs such as food and housing of trans communities during a global crisis. Programmes that provide and/or supplement these basic needs could also be strengthened by partnerships with mental health services. Thus, the results of this study point to the need for innovative mental health responses in the context of COVID-19 to be tightly interwoven with other programmatic services, policies and research interventions that address social and structural conditions impacting those who are struggling to cope.35 Bolstering telemedicine and other remote services could provide an accessible channel for effectively reaching and supporting trans and non-binary populations to help mitigate the negative effects of the pandemic.36
Limitations
The results of this study should be viewed in light of its limitations. First, a cross-sectional survey cannot determine causation between our independent and outcome variables, imploring the need for longitudinal inquiry for future research and to strengthen the results of the mediational analyses. Second, the measures assessed across socioecological levels were assessed based on individual perspectives and experiences. As such, these analyses could be further bolstered by having data that do not rely on self-reported variables (eg, economic data, surveillance, clinic data, health insurance datasets and so on). Third, due to the sample being recruited via a convenience sample, the results of this study are not generalisable nor representative of all trans and non-binary populations globally, particularly those who do not use these specific apps, have access to the web, or possess a smartphone or a tablet computer. Moreover, our sample had most respondents hailing from Europe and Southeast Asia regions, and as such our findings on mental health outcomes may be more indicative and reflective of those from these regions. Similarly, while we were able to reach a number of non-binary and trans feminine individuals, trans masculine respondents in this study were under-represented and therefore results cannot be generalised to the entire trans populations. Lastly, as the variables of interest were collected in a self-reported manner, it is possible that stigmatising topics such as mental health could be under-reported in this study, particularly in parts of the world in which mental health may not be part of social and cultural norms and healthcare systems.
Conclusion
This study revealed the importance of leveraging and designing multilevel interventions and programming that aim to address factors across socioecological levels (eg, socioeconomic loss, reduction in gender affirming services) to improve mental health exacerbated by COVID-19 pandemic for trans and non-binary populations. The results of this study support the importance of bolstering access to gender affirming services as well as strengthening socioeconomic opportunities and support to buffer the impact of COVID-19 pandemic environment on mental health among these important communities. This includes finding innovative ways in which mental health programmes and services can be tightly interwoven into a myriad of programmatic services, policies and research interventions that address social and structural conditions among trans and non-binary populations in need of mental healthcare.35 The findings also corroborate existing intersecting literature that link gender affirmation with mental health, which delineates that supportive environmental and social structures that affirm gender can help improve mental health outcomes among trans and non-binary populations. We expanded this research by contextualising the need for strengthening socioeconomic support across societal sectors that are able to facilitate trans and non-binary populations’ access to gender affirming services and address poor mental health outcomes, particularly during a time when environmental and social structures within systems of healthcare and economy across global regions are strained.
Acknowledgments
The authors would like to thank the participants of this study.
Footnotes
Handling editor: Seye Abimbola
Twitter: @BrotherAdamson
Contributors: All authors contributed to the conceptualisation and editing of this article. BJ and SWB curated and prepared the data. AJR analysed the dataset. AJR and HJ wrote the manuscript. All authors were involved in data interpretation and reviewed the manuscript.
Funding: AJR and HJ were supported by the National Institute of Allergy and Infectious Diseases (grant T32AI102623). BAJ was supported by the National Institute of Mental Health (grant F31MH121128). SWB was supported by the National Institute of Mental Health (grant K01MH114715).
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: All study procedures received approval by the Johns Hopkins School of Public Health Institutional Review Board. Due to the secondary analysis nature of this de-identified dataset, this study does not qualify as human subjects research and was determined that the protocol qualified for Exempt status under Category 4. All enrolled participants provided electronic written informed consent.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on request. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020;7:547–60. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jo W, Chang D. Political consequences of COVID-19 and media framing in South Korea. Front Public Health 2020;8:425. 10.3389/fpubh.2020.00425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Staples L, Nielssen O, Kayrouz R, et al. Rapid report 2: Symptoms of anxiety and depression during the first 12 weeks of the Coronavirus (COVID-19) pandemic in Australia. Internet Interv 2020;22:100351. 10.1016/j.invent.2020.100351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ren Z, Zhou Y, Liu Y. The psychological burden experienced by Chinese citizens during the COVID-19 outbreak: prevalence and determinants. BMC Public Health 2020;20:1617. 10.1186/s12889-020-09723-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Lancet Infectious Diseases . The intersection of COVID-19 and mental health. Lancet Infect Dis 2020;20:1217. 10.1016/S1473-3099(20)30797-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts SA, Williams CR, Grimstad FW. Considerations for providing pediatric Gender-Affirmative care during the COVID-19 pandemic. J Adolesc Health 2020;67:635–7. 10.1016/j.jadohealth.2020.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gibb JK, DuBois LZ, Williams S, et al. Sexual and gender minority health vulnerabilities during the COVID-19 health crisis. Am J Hum Biol 2020;32:e23499. 10.1002/ajhb.23499 [DOI] [PubMed] [Google Scholar]
- 8.Bazargan M, Galvan F. Perceived discrimination and depression among low-income Latina male-to-female transgender women. BMC Public Health 2012;12:663. 10.1186/1471-2458-12-663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rimes KA, Goodship N, Ussher G, et al. Non-binary and binary transgender youth: comparison of mental health, self-harm, suicidality, substance use and victimization experiences. Int J Transgend 2019;20:230–40. 10.1080/15532739.2017.1370627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reisner SL, Hughto JMW. Comparing the health of non-binary and binary transgender adults in a statewide non-probability sample. PLoS One 2019;14:e0221583. 10.1371/journal.pone.0221583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Y, Pan B, Liu Y, et al. Health care and mental health challenges for transgender individuals during the COVID-19 pandemic. Lancet Diabetes Endocrinol 2020;8:564–5. 10.1016/S2213-8587(20)30182-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldmann E, Galea S. Mental health consequences of disasters. Annu Rev Public Health 2014;35:169–83. 10.1146/annurev-publhealth-032013-182435 [DOI] [PubMed] [Google Scholar]
- 13.Gaillard JC, Gorman-Murray A, Fordham M. Sexual and gender minorities in disaster. Gender, Place & Culture 2017;24:18–26. 10.1080/0966369X.2016.1263438 [DOI] [Google Scholar]
- 14.Reisner SL, Poteat T, Keatley J, et al. Global health burden and needs of transgender populations: a review. Lancet 2016;388:412–36. 10.1016/S0140-6736(16)00684-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scheim A, Kacholia V, Logie C, et al. Health of transgender men in low-income and middle-income countries: a scoping review. BMJ Glob Health 2020;5:e003471. 10.1136/bmjgh-2020-003471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thomas R, Pega F, Khosla R, et al. Ensuring an inclusive global health agenda for transgender people. Bull World Health Organ 2017;95:154–6. 10.2471/BLT.16.183913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: a critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med 2015;147:222–31. 10.1016/j.socscimed.2015.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bränström R, Pachankis JE. Reduction in mental health treatment utilization among transgender individuals after Gender-Affirming surgeries: a total population study. Am J Psychiatry 2020;177:727–34. 10.1176/appi.ajp.2019.19010080 [DOI] [PubMed] [Google Scholar]
- 19.Santos G-M, Ackerman B, Rao A, et al. Economic, mental health, HIV prevention and HIV treatment impacts of COVID-19 and the COVID-19 response on a global sample of Cisgender gay men and other men who have sex with men. AIDS Behav 2021;25:311–21. 10.1007/s10461-020-02969-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Selm M, Jankowski NW. Conducting online surveys. Quality and Quantity 2006;40:435–56. 10.1007/s11135-005-8081-8 [DOI] [Google Scholar]
- 21.King DB, O'Rourke N, DeLongis A. Social media recruitment and online data collection: A beginner’s guide and best practices for accessing low-prevalence and hard-to-reach populations. Canadian Psychology/Psychologie canadienne 2014;55:240–9. 10.1037/a0038087 [DOI] [Google Scholar]
- 22.Kroenke K, Spitzer RL, Williams JBW, et al. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 2009;50:613–21. 10.1176/appi.psy.50.6.613 [DOI] [PubMed] [Google Scholar]
- 23.Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: validation and standardization of the patient health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord 2010;122:86–95. 10.1016/j.jad.2009.06.019 [DOI] [PubMed] [Google Scholar]
- 24.Czeisler Mark É, Lane RI, Petrosky E, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1049. 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bendau A, Petzold MB, Pyrkosch L. Associations between COVID-19 related media consumption and symptoms of anxiety, depression and COVID-19 related fear in the general population in Germany. Eur Arch Psychiatry Clin Neurosci 2020:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kline RB. Principles and practice of structural equation modeling. Guilford publications, 2015. [Google Scholar]
- 27.StataCorp . StataSE 16.1 [computer software. TX: StataCorp College Station, 2019. [Google Scholar]
- 28.Ettman CK, Abdalla SM, Cohen GH, et al. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open 2020;3:e2019686. 10.1001/jamanetworkopen.2020.19686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the minority stress model. Prof Psychol 2012;43:460–7. 10.1037/a0029597 [DOI] [Google Scholar]
- 30.McGarrity LA. Socioeconomic status as context for minority stress and health disparities among lesbian, gay, and bisexual individuals. Psychol Sex Orientat Gend Divers 2014;1:383–97. 10.1037/sgd0000067 [DOI] [Google Scholar]
- 31.Blumenthal D, Fowler EJ, Abrams M, et al. Covid-19 - Implications for the Health Care System. N Engl J Med 2020;383:1483–8. 10.1056/NEJMsb2021088 [DOI] [PubMed] [Google Scholar]
- 32.Cutler D. How will COVID-19 affect the health care economy? JAMA 2020;323:2237–8. 10.1001/jama.2020.7308 [DOI] [PubMed] [Google Scholar]
- 33.Operario D, Nemoto T. On being transnational and transgender: human rights and public health considerations. American Public Health Association, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gonzales G, Loret de Mola E, Gavulic KA, et al. Mental health needs among lesbian, gay, bisexual, and transgender college students during the COVID-19 pandemic. J Adolesc Health 2020;67:645–8. 10.1016/j.jadohealth.2020.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cénat JM, Dalexis RD, Kokou-Kpolou CK, et al. Social inequalities and collateral damages of the COVID-19 pandemic: when basic needs challenge mental health care. Int J Public Health 2020;65:717–8. 10.1007/s00038-020-01426-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gava G, Seracchioli R, Meriggiola MC. Telemedicine for endocrinological care of transgender subjects during COVID-19 pandemic. Evid Based Ment Health 2020;23:e1-e. 10.1136/ebmental-2020-300201 [DOI] [PMC free article] [PubMed] [Google Scholar]