Abstract
The COVID-19 pandemic has brought unprecedented challenges to the medical workforce. This has put them at increased risk of burnout at a time when levels are already worryingly high in the profession, with recent studies consistently showing that around half of doctors meet the validated criteria for burnout.
Objectives
To understand the wider factors influencing and impacting upon hospital doctors’ well-being during the COVID-19 pandemic in England.
Design
Cross-sectional survey and mixed quantitative–qualitative analysis.
Setting
Acute National Health Service (NHS) Foundation Trust in England.
Participants
An online survey was circulated in early June 2020 to all 449 doctors employed by the Trust. 242 doctors completed the survey (54% response rate).
Primary outcome measures
Questions assessed occupational details, self-reported changes in physical and mental health, satisfaction with working hours and patterns, availability of personal protective equipment (PPE), medication and facilities, communication and sought to identify areas seen as having a significant effect on doctors’ well-being.
Results
96% of respondents requiring PPE were able to access it. Nearly half of the respondents felt that their mental health had deteriorated since the start of the pandemic. Over a third stated that their physical health had also declined. Issues identified as having a negative impact on doctors included increased workload, redeployment, loss of autonomy, personal issues affecting family members, anxiety around recovery plans, inadequate access to changing and storage facilities and to rest areas that allow for social distancing. Doctors appreciated access to ‘calm rooms’ that were made available for staff, access to clinical psychology support, free drinks and free car parking on site.
Conclusion
The emerging themes are suggestive of increased burnout risk among doctors during the COVID-19 pandemic and encompass factors well beyond shortage of PPE. Small organisational initiatives and the implementation of changes suggested by survey respondents can have a positive impact on doctors’ well-being.
Keywords: mental health, COVID-19, occupational & industrial medicine
Strengths and limitations of this study.
This study provides a comprehensive qualitative narrative of doctors’ well-being during the COVID-19 pandemic.
The topic of doctors’ well-being urgently needs further addressing during the ongoing and evolving pandemic.
The response rate of the survey was good at 54% and appropriately represented doctors from all grades and specialties.
The survey was conducted at a single Acute NHS Foundation Trust in the UK, limiting its external validity and generalisability.
The cross-sectional design does not consistently allow causality to be inferred from any quantitative associations observed.
Introduction
Levels of burnout—characterised by emotional exhaustion, reduced personal accomplishment and depersonalisation due to stressors in the workplace1—were already worryingly high among doctors prior to COVID-19, with studies reporting rates of 30%–80%.2–12 Burnout levels were previously assessed at a local Acute NHS Foundation Trust using the validated Maslach Burnout Inventory,1 where 49% of the senior doctors and 67% of the junior doctors met the criteria for burnout (unpublished data). Recently, the importance of doctors’ well-being has been increasingly recognised by official bodies in the UK including the General Medical Council,13 the British Medical Association (BMA)14–17 among others.18–21 Burnout affects the individual doctor, risking mental and physical ill-health,22 reduces the quality of patient care23 and leads to maladaptive coping strategies that impair relationships with both patients and colleagues.24 There is growing evidence that organisational strategies that improve the working environment have significantly greater impact on the well-being of physicians than strategies targeting the individual and their resilience alone.3 25 26
Almost a year into the COVID-19 pandemic, the unprecedented impact on healthcare services has become clear across the globe. The increased demand on services, restructuring of resources, cessation of elective activity, requirement for personal protective equipment (PPE), command and control structure and risk of infection of staff have all challenged doctors’ well-being.21 27 Reports from countries severely affected early in the pandemic suggested that 15%–90% of doctors were at risk of burnout.28–33 Recognising the additional impact of COVID-19 on already high burnout rates, the BMA has launched national surveys assessing doctors’ mental well-being.34 However, none of these studies has included the assessment of qualitative data to lend doctors a voice to express concerns beyond those listed in the templates of their questionnaires.
Therefore, a decision was made during the first wave in May 2020 within the same Acute NHS Foundation Trust in which the aforementioned burnout questionnaire was distributed to conduct a further survey, this time to assess for the impact of COVID-19 on the medical workforce. The aim was to identify factors that were modifiable within a reasonable time frame, while the more obvious shortages of PPE and patient beds have attracted much media coverage, to our knowledge, there has not yet been any in-depth analysis of the wider factors influencing doctors’ well-being, which could be more significant en masse, and in the longer term.
Objectives
The key objective was to capture a snapshot of doctors’ experience of working through the first phase of the pandemic using a survey and thematic analysis. We sought to understand which factors have caused most concern to doctors working in an Acute NHS Foundation Trust. We aimed to evaluate the impact of interventions which this Trust had already put in place to support doctors’ well-being and to determine which further interventions could be beneficial.
Method
All doctors employed at the Acute NHS Trust were sent an email from a database held by the Human Resources Department to the employees’ work email addresses. This email contained information describing the study and an encrypted link to an anonymised online questionnaire for completion during the period of 4–19 June 2020. Participants were reassured that the responses would be anonymous and not identifiable when used for audit and research purposes. Informed consent was implied on return of the survey. The study was approved by the Trust’s Research Operational Committee.
Patient and public involvement
The focus of this study was on doctors in secondary care without direct patient or public involvement. However, the survey also assessed issues affecting doctors as individuals outside of the working environment; this included the impact of contracting COVID-19, therefore, becoming patients themselves and the wider impact on friends and family.
Study questionnaire
The cross-sectional survey was created using the SurveyMonkey platform. The format mostly consisted of nominal, multiple-choice questions, followed by a free-text ‘other’ option, with the exception of two exclusively free-text questions (see online supplemental file 1 for the complete layout of survey). By using the free-text questions, we allowed the respondents the opportunity to give their wider narrative on isues of importance that may not have been captured by the specific questions and may have been overlooked by larger scale studies.
bmjopen-2021-050223supp001.pdf (89KB, pdf)
The topics of the questions were chosen based on several sources: first, findings published by other official bodies invested in doctors’ well-being in the early stages of the pandemic, including the Royal College of Anaesthetists35 and the BMA34; second, wellbeing-related work previously undertaken internally at the Trust and finally, common discussion topics sampled from informal sources including social media, mainstream media and topics frequently discussed among staff members. These topics included PPE; availability of medications; redeployment; working hours and patterns; staff facilities and testing. Response biases were minimised by the broad spectrum of input to the survey sought prior to distribution, including the Trust’s Human Resource department, Communication team, Estates and Facilities, Better Working Lives Group (BWLG) and Junior Doctor Forum. Prior to wider circulation, a draft survey was distributed to several representative clinicians for review.
Analysis
Quantitative data were collected as part of the survey to accompany our qualitative analysis in presentations to our trust members and management structures. Simple quantitative data analysis of survey results and demographics was performed using Microsoft Excel. Qualitative data were initially analysed manually by the senior author and then grouped together through thematic analysis, based broadly on the worklife themes identified by Leiter and Maslach36 and COVID-19-specific themes frequently featuring in the free-text answers. A consensus meeting was held where all authors reviewed the free-text responses and agreed their attribution across seven themes. Detailed statistical group analysis was not performed as the numbers of responses were too low to allow meaningful comparison between groups and most of the data were nominal.
Results
Demographics of survey respondents
In total, 242 out of 449 doctors completed the survey, a response rate of 54%.
Of the 242 respondents, 123 were consultants (50.1%) and 119 were doctors of other grades (49.9%), including associate specialists (3.3%), trust grade and locally employed doctors (5%), specialty registrars (6.6%), core trainees in years 1–3 (16.6%), foundation year 2 doctors (13.7%), foundation year 1 doctors (7%), interim foundation doctors (3.7%) and general practice trainees (2.1%). Respondents represented different specialties and areas of work, with about a third reporting to usually work in a medical specialty (32.6%), surgery (17.8%), anaesthetics and intensive treatment unit (ITU) (14.9%), radiology (7.4%), acute assessment unit (7%), obstetrics and gynaecology (5.8%), the emergency department (5%), paediatrics (5%), laboratory services (3.7%) and general practice (0.8%). The demographics are summarised in figures 1 and 2.
Figure 1.
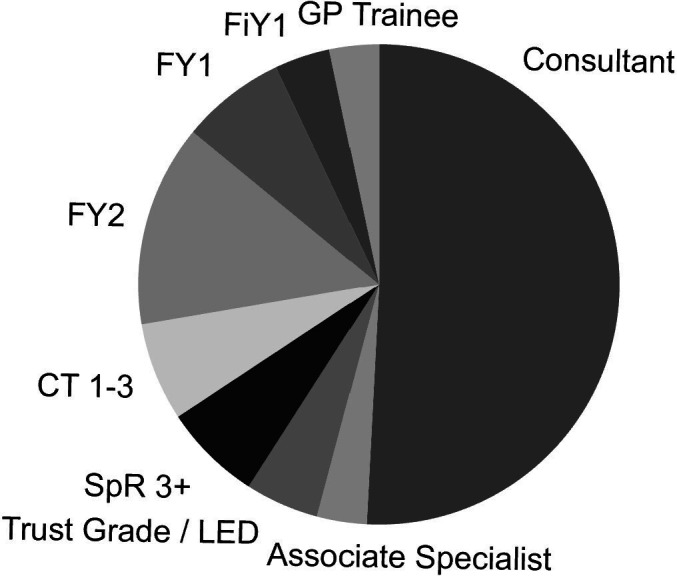
Demographics by grade of doctors responding to our survey and across the Trust at which the survey was undertaken (N=242). GP, general practice; LED, Locally Employed Doctor.
Figure 2.
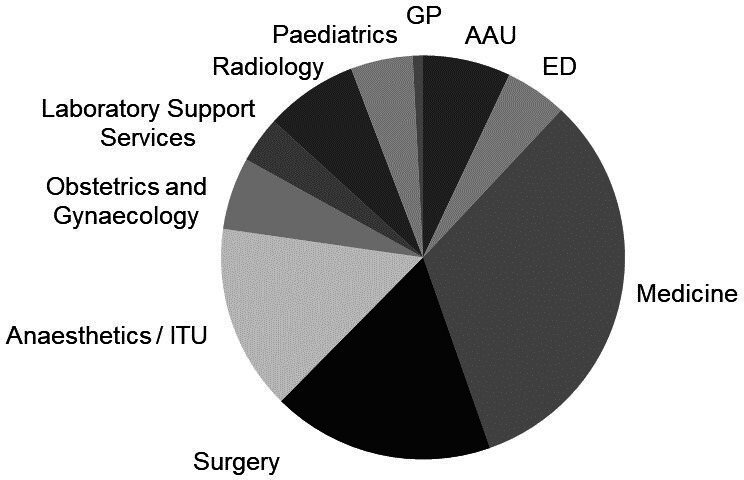
Demographics by specialty of doctors responding to our survey and across the Trust at which the survey was undertaken (N=242). AAU, acute assessment unit; ED, Emergency Department; GP, general practice; ITU, anaesthetics/intensive treatment unit.
Impact on mental and physical health
Almost half of all respondents reported a decline in their mental health (47.1%). One doctor wrote: ‘Dealing with the impact of COVID-19 on my mental health has been tough. The prolonged uncertainty is ongoing, with the added stress of not being able to see friends or family and not being able to turn to my usual things to de-stress. I struggle to sleep, and on my days off, it can be difficult to forget about work’.
Over a third of respondents felt their physical health had deteriorated during the pandemic (34.3%). There were differences across specialities in our Trust; doctors in all specialities with the exception of Acute medicine saw a greater decline in mental health compared with physical health (figure 3). The greatest source of concern were colleagues and the environment not supporting social distancing and the individual’s personal situation, which is mentioned above (figure 4).
Figure 3.
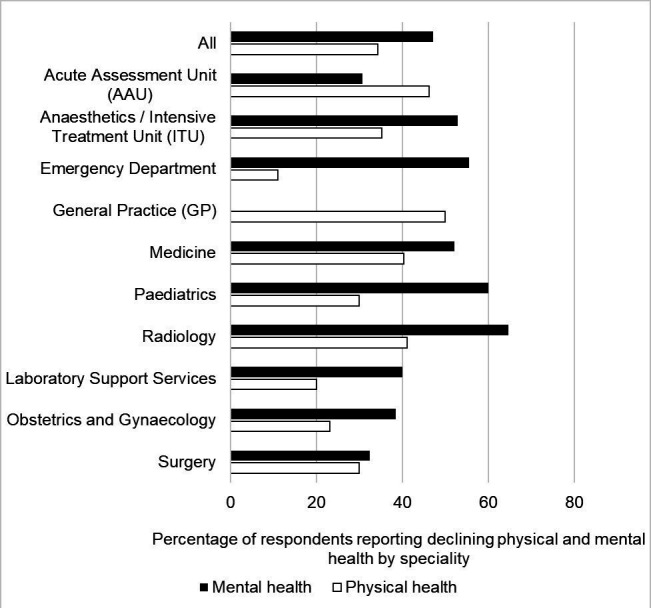
Self-reported decline in physical and mental health among respondents; specialties are listed here by alphabetical order (N=210; the question was not made compulsory in the survey). AAU, acute assessment unit; GP, general practice; ITU, anaesthetics/intensive treatment unit.
Figure 4.
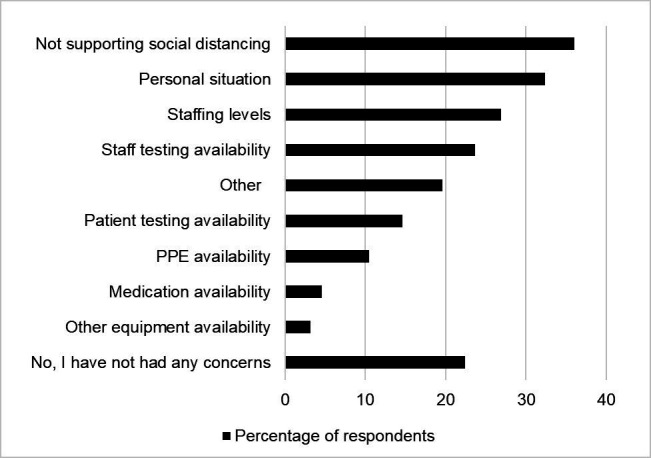
Causes of anxieties and stress, as identified by the nominal (quantitative) question: ‘Within the past 2 weeks, have any of the following caused you additional worry or anxiety?’ (N=219; the question was not made compulsory in the survey). PPE, personal protective equipment.
Further significant causes of distress appeared to be staffing levels; the availability of staff testing; theatre flow and working environment; annual leave (the ability to book leave and having to cover absence of colleagues); effect on patient care (missed cancer diagnoses, delays in treatment, theatre waiting lists); recovery phase and the return to ‘normal activity’; lack of guidance or leadership; tiredness, stress and fatigue; feeling undervalued; relations between different specialities and staff group and increased vulnerability of Black, Asian and minority ethnic (BAME) staff. ‘We need proper, practical on the floor support for BAME staff, particularly those who are the top of the high-risk profile’.
Thematic analysis
Seven worklife themes were identified (figure 5): the lack of things, workload volume/parity/working patterns, culture, communication, control/autonomy, reward/recognition and personal issues.
Figure 5.
Manual qualitative analysis of the free-text answers to the survey led to the identification of seven major themes, many of which overlap with the factors relevant to burnout as identified by Leiter and Maslach (see text).
The lack of things
There were 26 free-text answers falling under the theme of ‘lack of’ and, interestingly, these mostly related to the physical environment. The most frequently raised issue was lack of space to allow for social distancing and the general lack of adherence to social distancing rules. This is in line with the quantitative data, which showed that only half of all respondents felt that they had sufficient access to rest areas that allowed for social distancing (55.3%), to changing facilities with sufficient room to allow for social distancing (45.2%) and to adequate secure facilities for storage of personal items (55.6%). Other issues identified included the lack of scrubs, of hand gel, of COVID-19 staff testing and of cleaning of doors and communal areas, such as coffee rooms and the staff canteen.
Medication and PPE availability seemed to be less of a concern in our Trust at the time the survey was undertaken. The majority of respondents (96.0%) reported having access to the necessary PPE required for their role. 16% of respondents had felt pressured into seeing a patient with suspected or confirmed COVID-19 without adequate PPE. When asked who, or what, made them feel pressured into doing so, respondents attributed this to the urgency of the situation or patient’s condition; external pressure from senior and junior colleagues; internal pressure from self and pressure from multiple sources including ward managers, nursing colleagues, senior management, ‘specific ward guidelines’, ‘poor national and local guidance’ and ‘COVID-positive patients on non-COVID wards’. Of the respondents who stated that medication availability was a concern, only one respondent said a drug had actually been unavailable for them to prescribe. None of the respondents felt medication shortage had resulted in a negative impact on the quality or effectiveness of the treatment they were able to offer a patient.
Workload volume, parity and working patterns
The majority of respondents (90%) had seen changes in their rota or working pattern. In general, this meant more working hours: 56.2% of all doctors responding to the survey reported working more hours regularly than previously and 49.3% reported not always being able to take adequate breaks during working hours. Almost half of all respondents reported having to take time off work for a reason that was directly related to the pandemic (44.0%), most commonly due to a suspected or confirmed diagnosis of COVID-19 in themselves (28.7%) or due to a household member being affected (14.4%). Other reasons for taking time off were stress or anxiety directly related to the pandemic (4.2%), self-isolation (shielding) due to underlying medical conditions (1.4%) and childcare commitments (1.4%). Furthermore, about a third of all respondents had been redeployed or moved into a different area of practice, away from their usual place of work (31.5%). Many of those who had been redeployed felt they had not received adequate induction (40%), although the survey did not specify or ask further what would constitute adequate induction training.
There were 19 free-text answers under the theme of workload. Unsurprisingly, increased workload volume was a frequently raised issue, but there was also an emphasis on parity of workload, with some respondents noting certain specialities were shouldering more of the COVID-19 workload than others.‘Our department has been under significant pressure over the last 10 weeks. However, it is apparent that not all staff or departments are under the same pressures or workloads’. The burden of increased out of hours work was also highlighted, with schedules described as unhealthy, emotionally draining and adversely affecting sleep. 'One needs to ensure well-being rotas and not just compliant rotas. Going from days to nights to days is unhealthy and causes sleep disturbance’. Concerns were also raised about the potential impact of the recovery phase. ‘What caused early distress was the urgency to reconfigure at the beginning—a time full of adrenaline and anxiety about what was to come. Then, the exhaustion of working all hours and not being able to sleep. Now, the burnout makes it hard to keep going and have the energy to plan for the recovery… A rollercoaster with no end in sight’.
Culture
There were 16 comments relating to culture. Areas highlighted included the need to: engage and motivate teams, encourage staff to contribute, acknowledge and appreciate the efforts staff have gone to through the pandemic and treat staff with empathy and kindness in the workplace. ‘We need more of a listening and compassionate culture. We are all professionals and everyone’s voice counts'. ‘We need a change in workplace culture where all team members are engaged in the decisions about their working life, are encouraged to contribute to policy developments and feel consulted and valued for their contribution’.
Communication
Half of all respondents (49%) felt that they had received just the right amount of information and communication regarding the COVID-19 situation from the Trust. Junior doctors were more likely to respond that there was not enough information; however, consultants were more likely to respond that there was too much information. In terms of resources predominantly used by doctors in our Trust to access the most up-to-date information about the pandemic, both electronic forms and in-person communication such as small group and online meetings and teaching were valued.
There were 15 comments within the theme of communication. Many of these related to the need to communicate not just the decision, but the rationale underpinning it, more clearly. It was felt that the command and control structure had restricted bottom-up communication and suggestions for change. Several respondents pointed out that information provided by the Trust on the COVID-19 pandemic was often conflicting: ‘too much information, not enough communication, too many opinions'; 'the responsibility to assimilate all this conflicting advice is the source of stress’. Several doctors also expressed an interest in easier access to the Trust’s own COVID-19 statistics. Finally, respondents highlighted the need for clearer communication about changes in responsibilities and the need to share plans for the recovery phase.
Control and autonomy
There were 11 comments relating to control and autonomy. The command and control structure adopted by NHS Trusts during the pandemic followed national guidance in the UK.37 However, several respondents disliked the associated loss of autonomy, stating that it negatively affected the ability to work in a collaborative manner. Some doctors also felt that working patterns were forced on them without consultation, and as a result felt marginalised. ‘I have found the command and control structure the worst thing for my wellbeing and for the ability of teams to work in a professional manner’. ‘Less pressure to work outside of one’s comfort zone, and more understanding that everyone’s personal circumstances are different [would be appreciated]’.
Reward and recognition
There were 10 comments relating to reward and recognition. Access to free food and drinks, the introduction of calm rooms and free car parking and the expansion of psychological support services were widely recognised as helping doctors feel recognised and acknowledged as well as boosting morale. For example: ‘Free coffee and car parking makes me feel that my contribution is actually respected’. Some specialities, in particular, acute physicians, felt that their contribution had not been appropriately recognised in the same manner as those working in ITU. ‘A proper acknowledgement of the work that Medicine is doing would be appreciated. Physicians have felt marginalised, living in the shadow of ITU colleagues, whereas the workload has been greatest for us’. Those on part-time contracts also felt that the disproportionate increase in their workload had not been recognised.
Personal
The personal impact of COVID-19 was highlighted by 10 respondents. Issues raised included a negative effect on relationships with family and friends, sleep quality and work–life balance. Comments also mentioned the increased vulnerability of BAME staff as a cause of personal concern: ‘The anxieties involved with being a BAME healthcare worker; even though one passes the risk assessment doesn’t make you immune to the virus’.
Discussion
Our cross-sectional survey aimed to identify the factors affecting the well-being of doctors in an Acute NHS Foundation Trust 3 months into the pandemic, to evaluate the impact of measures the Trust had put in place to support doctors and to highlight further steps that could be taken to support doctors in the workplace. The themes that emerged were broadly consistent with previously identified drivers for burnout in doctors,36 38 with an associated impact on mental health.39 Unsurprisingly, increased workload volume was a dominant theme, but the results also highlighted areas more easily amenable to intervention, for example, through improving culture and communication and appropriately recognising doctor’s contributions. Not all was negative; highlighting the positives was equally important to inform further planning. The introduction of free drinks, car parking, calm rooms, the availability of free food out of hours and the expansion of psychological services were widely appreciated by doctors.
The self-reported negative impact of the COVID-19 pandemic on both the mental and physical health of survey respondents was significant, with nearly half (47.1%) reporting a deterioration in mental health, while a third (34.3%) reported a deterioration in physical health since the start of the pandemic. This was a self-reported outcome rather than measured on a validated scale. Nevertheless, in a workforce with burnout levels prior to COVID-19 of over 50%,3 5 this is a real concern. Left unchecked, the increased levels of stress will undoubtedly result in higher levels of burnout. Data from early studies affirmed a high risk of burnout among doctors during the COVID-19 pandemic, with studies reporting burnout rates of 15%–90%.28–31 40 41 A rapid review and meta-analysis of 12 studies performed in China and one study in Singapore suggested that the prevalence of anxiety, depression and insomnia among healthcare workers (including both doctors and nurses) during the COVID-19 pandemic was 23%, 23% and 39%, respectively.42 Similar or worse results have been reported for doctors in Europe40 43 and the USA.31 The contributors to any perceived deterioration in mental health are generally acknowledged to be complex and multifactorial. The themes that our current study identified included changed working patterns, staffing levels, the personal situation in the face of illness and death, lack of ability to socially distance, availability of staff testing for COVID-19 and dissatisfaction with the command and control structure and discrepancies in information.
Of particular note, the command and control structure and its top-down hierarchy imposed nationally in the UK on every NHS Trust at the beginning of the pandemic44 45 were perceived by many respondents as having a negative impact on a sense of autonomy and value. While such a structure may aid rapid decision-making, it risks a loss of empathy and compassion—both crucial prerequisites for maintaining a healthy working environment in the longer term. Therefore, it could have significant negative impact on the well-being of those who are at the receiving end—mirroring the views expressed by others previously.27 46 Moving forward, a more collaborative approach is likely to have a more positive impact on the sense of control, autonomy and engagement that are key to the well-being of healthcare workers.10 38
While the limited availability of PPE had caused major concern across NHS hospitals early on in the pandemic,34 47 48 PPE shortage was not one of the principal concerns among doctors at the time of this survey in June 2020. Rather, other deficits in the working environment were highlighted as more significant to this Trust’s doctors at this point, most notably the lack of access to adequate changing facilities, secure lockers, scrubs and the lack of both office space and adequate rest areas to facilitate adherence to social distance guidelines. Social distancing has been identified as a cause of concern not only for individuals in general49 but also specifically for clinicians.50 Locally, the Space Utilisation Group of the Acute Trust is now addressing the issue of lack of space for adequate social distancing.
This leads us to three important take-home messages. First, we predict that concerns about shortage of facilities including rest spaces may be affecting many hospitals across the globe which were not built for the purpose of coping with a pandemic in the first place. This should be taken into consideration when planning for further waves. Second, given that the Acute Trust in question was less severely affected by the lack of PPE and also by the COVID-19 caseload than many other NHS hospitals—with a total of 254 COVID-19-positive patients being admitted to the Trust over the period of 4 months as of 13 July 202051—we are concerned that the survey results might represent doctors’ well-being and burnout at the better end of a spectrum: doctors are at extremely high risk of burnout during the COVID-19 pandemic. Third, we hope to instigate further interest in well-being research and initiatives during the pandemic and beyond. Research has consistently shown that structural and organisational interventions are more effective in improving physician burnout than those targeting individuals, although the combination of the two is the most effective.3 23 26 One way to ensure and facilitate well-being work at a local level is through a dedicated position of responsibility or working group. For instance, in the Trust in question, a Better Working Lives Group (BWLG) had been set up in the past year to address the issues of doctors’ well-being and burnout. Therefore, uniquely, a previous questionnaire on doctors’ well-being was available to provide information on local levels of burnout prior to COVID-19 to inform the creation of this current survey. The good response rates to both surveys suggest that doctors are invested in their well-being. The BWLG further ensured the expansion of clinician-led psychological support services available to all doctors at the Trust and was involved in the introduction of the calm rooms. These initiatives were explicitly mentioned by doctors responding to our survey with gratitude, but more importantly, they are also supported by evidence in well-being research more widely.15 16 18 52
This study had several strengths and weaknesses. First, as a cross-sectional study at a single Acute NHS Foundation Trust in England conducted during a dynamic healthcare crisis causing uncertainties across the globe, we acknowledge that the generalisability of our findings is limited. We hope to instigate more interest in further well-being research instead by communicating our local findings. Second, cross-sectional surveys provide a snapshot of responses at a single time point and allow no causality to be inferred, especially in the presence of the risk of any recall biases. However, attempts at minimising recall and response biases were made as explained in the method section. Any discussion of potential causality was made based on free-text answers which often explicitly mentioned a self-reported cause for distress rather than through combination of individual nominal questions in the survey. Third, the focus on qualitative data has inherent drawbacks, as issues that are highlighted may apply to a small subset of doctors or even single individuals. At the same time, the qualitative analysis of our study of a sample size of 242 is the main and unique strength of this study, as manual analyses of open-ended, free-text questions becomes too laborious with a larger sample size than here, and their interpretation is difficult when pooling too many different contexts.
Going forward, we hope to see a combination of large-scale, powered studies on well-being in healthcare such as the BMA well-being survey,34 longitudinal studies using validated burnout tools and focused mixed qualitative-quantitative or purely qualitative studies on well-being, of which some are already underway.53 Future work should also particularly consider the well-being and burnout rates of nurses and other healthcare professionals who are also at high risk of burnout41 and of healthcare professionals who have been identified as vulnerable to COVID-19 or at higher risk of burnout and mental ill-health, such as BAME,54 female31 and nonbinary professionals. It will be essential to keep the well-being of healthcare workers high on the agenda and involve them in local decision-making to prevent burnout and deleterious effects on the well-being not only of the individual doctor but also the nation: doctors’ well-being is still too often a missing quality indicator in healthcare55 and it is absolutely essential not to return to status quo, or worse, after the pandemic.56
Conclusion
While a shortage of PPE, frequent confrontation with deaths and personal losses do constitute important causes of distress among doctors during the COVID-19 pandemic, there are numerous other less obvious but crucial factors underpinning doctors’ well-being and stress levels during such a sudden, rapid change in the health service. On the one hand, this is alarming, as burnout rates were high among the profession prior to the pandemic. On the other hand, it is also helpful to dissect these factors, as many of the issues raised can be tackled and addressed—often through small but impactful organisational changes, as we have shown here. Our findings may be generalisable to an extent to other NHS Trusts in the UK, but more importantly, we hope to instigate further interest in doctors’ well-being research, both during the COVID-19 pandemic and beyond.
Original protocol
See supplemental files for a copy of the survey (online supplemental file 1).
Supplementary Material
Footnotes
Contributors: All authors met at least one of the criteria recommended by the ICMJE and have agreed on the final version of the manuscript. LJC, CJS, LCJ and PDM were involved in conceiving and designing the original protocol. LJC conducted the quantitative analysis of the results, YRI and PDM conducted qualitative analyses. YRI wrote the first draft in the manuscript. LJC, CJS, LCJ and PDM contributed to subsequent drafts.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: LJC, YRI, CJS, LCJ and PDM were employed by the Trust at the time the survey was undertaken and declare no further competing interests.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No data are available. No additional data available.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Maslach C, Jackson SE, Leiter MP. The Maslach burnout inventory manual. Maslach Burn Invent 1996:191–217. [Google Scholar]
- 2.West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 2016;388:2272–81. 10.1016/S0140-6736(16)31279-X [DOI] [PubMed] [Google Scholar]
- 3.Wiederhold BK, Cipresso P, Pizzioli D, et al. Intervention for physician burnout: a systematic review. Open Med 2018;13:253–63. 10.1515/med-2018-0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lim R, Aarsen KV, Gray S, et al. Emergency medicine physician burnout and wellness in Canada before COVID19: a national survey. CJEM 2020;22:603–7. 10.1017/cem.2020.431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Imo UO. Burnout and psychiatric morbidity among doctors in the UK: a systematic literature review of prevalence and associated factors. BJPsych Bull 2017;41:197–204. 10.1192/pb.bp.116.054247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuerer HM, Eberlein TJ, Pollock RE, et al. Career satisfaction, practice patterns and burnout among surgical oncologists: report on the quality of life of members of the Society of surgical oncology. Ann Surg Oncol 2007;14:3043–53. 10.1245/s10434-007-9579-1 [DOI] [PubMed] [Google Scholar]
- 7.Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg 2009;250:463–71. 10.1097/SLA.0b013e3181ac4dfd [DOI] [PubMed] [Google Scholar]
- 8.Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general us working population between 2011 and 2014. Mayo Clin Proc 2015;90:1600–13. 10.1016/j.mayocp.2015.08.023 [DOI] [PubMed] [Google Scholar]
- 9.Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med 2014;89:443–51. 10.1097/ACM.0000000000000134 [DOI] [PubMed] [Google Scholar]
- 10.Khan A, Teoh KR, Islam S, et al. Psychosocial work characteristics, burnout, psychological morbidity symptoms and early retirement intentions: a cross-sectional study of NHS consultants in the UK. BMJ Open 2018;8:e018720:1–11. 10.1136/bmjopen-2017-018720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bourne T, Shah H, Falconieri N, et al. Burnout, well-being and defensive medical practice among obstetricians and gynaecologists in the UK: cross-sectional survey study. BMJ Open 2019;9:e030968:1–11. 10.1136/bmjopen-2019-030968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McKinley N, McCain RS, Convie L, et al. Resilience, burnout and coping mechanisms in UK doctors: a cross-sectional study. BMJ Open 2020;10:e031765. 10.1136/bmjopen-2019-031765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.General Medical Council . Caring for doctors, caring for patients: an independent review chaired by Professor Michael West and Dame Denise Coia, 2019. [Google Scholar]
- 14.British Medical Association, National Health Service Employers . Good rostering guide, 2018. [Google Scholar]
- 15.British Medical Association . Caring for the mental health of the medical workforce, 2019. [Google Scholar]
- 16.British Medical Association . Supporting health and wellbeing at work, 2020. [Google Scholar]
- 17.British Medical Association . Fatigue and facilities charter, 2019. [Google Scholar]
- 18.Rimmer A. Provide doctors with rest spaces and on-call rooms, says mental health review. BMJ 2019;364:l848. 10.1136/bmj.l848 [DOI] [PubMed] [Google Scholar]
- 19.Society of Occupational Medicine . What could make a difference to the mental health of UK doctors? 2018. [Google Scholar]
- 20.Health Education England. NHS Staff and Learners’ Wellbeing Commission . NHS staff and learners wellbeing review, 2020. [Google Scholar]
- 21.Unadkat S, Farquhar M. Doctors’ wellbeing: self-care during the covid-19 pandemic. BMJ 2020;368:m1150:1–2. 10.1136/bmj.m1150 [DOI] [PubMed] [Google Scholar]
- 22.Medisauskaite A, Kamau C. Does occupational distress raise the risk of alcohol use, binge-eating, ill health and sleep problems among medical doctors? A UK cross-sectional study. BMJ Open 2019;9:e027362. 10.1136/bmjopen-2018-027362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med 2017;177:195–205. 10.1001/jamainternmed.2016.7674 [DOI] [PubMed] [Google Scholar]
- 24.McManus IC, Keeling A, Paice E. Stress, burnout and doctors' attitudes to work are determined by personality and learning style: a twelve year longitudinal study of UK medical graduates. BMC Med 2004;2:29. 10.1186/1741-7015-2-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA 2011;306:952–60. 10.1001/jama.2011.1247 [DOI] [PubMed] [Google Scholar]
- 26.Shanafelt TD, Noseworthy JH, Leadership E. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc 2017;92:129–46. 10.1016/j.mayocp.2016.10.004 [DOI] [PubMed] [Google Scholar]
- 27.Seedat A, Tissingh E, Johnson O. Is ‘Gold Command’ the right way to manage the NHS’s response to covid? Health Serv J 2020. [Google Scholar]
- 28.Dimitriu MCT, Pantea-Stoian A, Smaranda AC, et al. Burnout syndrome in Romanian medical residents in time of the COVID-19 pandemic. Med Hypotheses 2020;144:109972. 10.1016/j.mehy.2020.109972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cao J, Wei J, Zhu H, et al. A study of basic needs and psychological wellbeing of medical workers in the fever clinic of a tertiary General Hospital in Beijing during the COVID-19 outbreak. Psychother Psychosom 2020;89:252–4. 10.1159/000507453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu Y, Wang J, Luo C, et al. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manage 2020;60:e60–5. 10.1016/j.jpainsymman.2020.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kannampallil TG, Goss CW, Evanoff BA, et al. Exposure to COVID-19 patients increases physician trainee stress and burnout. PLoS One 2020;15:e0237301. 10.1371/journal.pone.0237301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.De Sio S, Buomprisco G, La Torre G, et al. The impact of COVID-19 on doctors' well-being: results of a web survey during the lockdown in Italy. Eur Rev Med Pharmacol Sci 2020;24:7869–79. 10.26355/eurrev_202007_22292 [DOI] [PubMed] [Google Scholar]
- 33.Jha S, Shah S, Calderon MD. The effect of COVID-19 on interventional pain management practices: a physician burnout survey. Pain Physician 2020:271–82. [PubMed] [Google Scholar]
- 34.British Medical Association . COVID-19: analysing the impact of coronavirus on doctors, 2020. [Google Scholar]
- 35.Royal College of Anaesthetists . View from the frontline of anaesthesia during COVID-19, April 2020 survey results, 2020. [Google Scholar]
- 36.Leiter MP, Maslach C. Six areas of worklife: a model of the organizational context of burnout. J Health Hum Serv Adm 1999;21:472–89. [PubMed] [Google Scholar]
- 37.NHS England, NHS Operations, National EPRR Team . Concept of operations for the management of mass casualties, 2017. [Google Scholar]
- 38.West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med 2018;283:516–29. 10.1111/joim.12752 [DOI] [PubMed] [Google Scholar]
- 39.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med 2020;383:510–2. 10.1056/NEJMp2008017 [DOI] [PubMed] [Google Scholar]
- 40.Azoulay E, De Waele J, Ferrer R, et al. Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care 2020;10:110. 10.1186/s13613-020-00722-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zerbini G, Ebigbo A, Reicherts P. Psychosocial burden of healthcare professionals in times of COVID-19 - a survey conducted at the University Hospital Augsburg. Ger Med Sci 2020;18. 10.3205/000281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pappa S, Ntella V, Giannakas T, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 2020;88:901–7. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Giusti EM, Pedroli E, D'Aniello GE, et al. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front Psychol 2020;11:1684. 10.3389/fpsyg.2020.01684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.NHS England . Incident response plan (national), 2017. Available: https://www.england.nhs.uk/wp-content/uploads/2017/07/NHS-england-incident-response-plan-v3-0.pdf
- 45.Watts G, Wilkinson E. What the NHS is learning from the British army in the covid-19 crisis. BMJ 2020;369:m2055. 10.1136/bmj.m2055 [DOI] [PubMed] [Google Scholar]
- 46.Horton R. Offline: COVID-19 and the NHS-"a national scandal". Lancet 2020;395:1022. 10.1016/S0140-6736(20)30727-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Locke T. COVID-19 Medscape UK PPE Poll: 7 in 10 lack supplies. Medscape 2020. [Google Scholar]
- 48.Iacobucci G. Covid-19: Doctors still at "considerable risk" from lack of PPE, BMA warns. BMJ 2020;368:m1316. 10.1136/bmj.m1316 [DOI] [PubMed] [Google Scholar]
- 49.Venkatesh A, Edirappuli S. Social distancing in covid-19: what are the mental health implications? BMJ 2020;369:m1379. 10.1136/bmj.m1379 [DOI] [PubMed] [Google Scholar]
- 50.Bansal P, Bingemann TA, Greenhawt M, et al. Clinician wellness during the COVID-19 pandemic: extraordinary times and unusual challenges for the Allergist/Immunologist. J Allergy Clin Immunol Pract 2020;8:1781–90. 10.1016/j.jaip.2020.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.West Suffolk Hospital NHS Foundation Trust . COVID-19 patient numbers - weekly update, 2020. [Google Scholar]
- 52.Walsh G, Hayes B, Freeney Y, et al. Doctor, how can we help you? qualitative interview study to identify key interventions to target burnout in hospital doctors. BMJ Open 2019;9:e030209. 10.1136/bmjopen-2019-030209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fuchs A, Abegglen S, Berger-Estilita J, et al. Distress and resilience of healthcare professionals during the COVID-19 pandemic (DARVID): study protocol for a mixed-methods research project. BMJ Open 2020;10:e039832. 10.1136/bmjopen-2020-039832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rimmer A. Covid-19: disproportionate impact on ethnic minority healthcare workers will be explored by government. BMJ 2020;369:m1562. 10.1136/bmj.m1562 [DOI] [PubMed] [Google Scholar]
- 55.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet 2009;374:1714–21. 10.1016/S0140-6736(09)61424-0 [DOI] [PubMed] [Google Scholar]
- 56.Hartzband P, Groopman J. Physician burnout, interrupted. N Engl J Med 2020;382:2485–7. 10.1056/NEJMp2003149 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-050223supp001.pdf (89KB, pdf)



