Abstract
Background
High levels of visceral adipose tissue (VAT) are associated with abdominal obesity and increased risk of metabolic deterioration. Recent studies showed that intensive physical exercise results in the reduction of subcutaneous and visceral fat.
Aims
This study investigates the effect of supramaximal muscle contractions induced by a HIFEM procedure for abdominal VAT changes.
Methods
Computed tomography (CT) scans of 22 subjects (47.3 ± 8.4 years, BMI of 23.5 ± 3.5 kg/m2) who received 8 HIFEM treatments of the abdomen (2‐3 days apart) were retrospectively evaluated for the changes in VAT. The CT scans were obtained at baseline and 1 month after the last treatment. The transverse slices at umbilical, infraumbilical, and supraumbilical levels were used to determine the cross‐sectional area (CSA) of VAT through a semi‐automated segmentation method.
Results
Analysis of the CSA revealed a significant (P = .004) and uniform reduction of the abdominal VAT area by 14.3% (−16.7 cm2) from 110.6 ± 69.0 cm2 to 93.9 ± 54.6 cm2. In general, a higher relative improvement was seen infraumbilically (17.1%), followed by supraumbilical (15.5%) and umbilical (10.7%) levels. The reduction of VAT was strongly correlated to the reduction of subcutaneous fat (r(17) = 0.66; P = .002). A decrease in VAT volume contributed to the overall aesthetic enhancement visible on digital photographs.
Conclusions
The outcomes indicate that HIFEM technology has a positive effect on VAT. However, further studies are necessary to validate these outcomes and to clarify the exact mechanism of a VAT reduction. Based on our results, the HIFEM procedure may be a beneficial treatment option for patients with high VAT deposits.
Keywords: computed tomography, electromagnetic fields, subcutaneous fat, visceral fat
1. INTRODUCTION
Unlike the subcutaneous adipose tissue (SAT), which is located superficially under the skin, visceral adipose tissue (VAT) accumulates predominantly intra‐abdominally in the vicinity of internal organs. Besides the differences in distribution inside the human body, the visceral fat and subcutaneous fat also differ functionally. It has been described that VAT is metabolically more active, more sensitive to lipolysis, and more insulin resistant when compared to SAT. 1 Visceral fat is also considered to behave as an endocrine and paracrine organ since it affects several metabolic processes by releasing various cytokines and bioactive markers, which may influence body weight, lipid metabolism, inflammation, and pathogenesis of diabetes mellitus. 2
Given the essential regulatory functions of VAT, the maintenance of healthy body weight should not be underestimated. Excessive accumulation of VAT in the abdominal area, referred to as central or abdominal obesity, is closely linked to various health disorders. These include elevated blood pressure, cardiovascular disease, type 2 diabetes, or cancer. 1 , 3 , 4 , 5 As shown by computed tomography (CT), patients who exceed a VAT cross‐sectional area of 100 cm2 at the umbilical level are suggested to be at increased risk of metabolic deterioration while exceeding 160‐200 cm2 implies high risk. 6 , 7 , 8 , 9 Such high VAT values are frequently associated with the unpleasant aesthetic appearance of so‐called “pot or beer belly,” which progresses in advanced age, especially in men. 10
Controlled physical exercise programs may lead to favorable changes in body composition achieved by the overall reduction of fat tissue. 11 , 12 A dose‐response relationship between training volume and fat reduction may be suggested, as Irving et al showed that the intensity of performed exercise determines the improvement rate. This means that better outcomes are seen when patients are subjected to a high‐intensity endurance training. 12 It has been found that such reduction is not selective to the SAT only, but it also involves changes in VAT since the decrease of subcutaneous and visceral fat after the exercise is correlated. 2
HIFEM procedure that is based on the principles of electromagnetic induction was found to be an effective body shaping modality for multiple body parts. 13 , 14 , 15 HIFEM selectively and noninvasively stimulates the striated muscle tissue by utilizing supramaximal contractions performed with higher tension than those achieved during regular exercise. Besides the muscle enlargement due to the muscle fiber hypertrophy and hyperplasia, 16 various imaging techniques including CT, 17 MRI, 14 and diagnostic ultrasound 18 documented SAT‐reducing effect of HIFEM when applied to the abdomen. Although it could be assumed that a reduction of VAT may have accompanied SAT changes, none of the previous studies focused on assessing abdominal VAT after the HIFEM treatments.
This study aims to investigate whether the HIFEM‐induced supramaximal contractions effectively promote changes in the volume of visceral fat when applied to the abdomen.
2. MATERIALS AND METHODS
2.1. The original study set up
This is a retrospective evaluation of CT scans, initially collected for measurement of abdominal fat and muscle tissue after HIFEM procedure in previously published single‐center study. 17 This evaluation did not involve any treatment intervention or collection of any additional patient data.
The original study included participants aged 21‐65 years and excluded subjects that reported a weight change of five lbs or more in the preceding month, pregnancy, implanted electronic devices and metal implants, heart disorders, or any medical condition which may contradict application of the electromagnetic field. The study conformed to ethical principles for medical research involving humans (Declaration of Helsinki).
Based on the specified inclusion criteria, 22 subjects (three men, 19 women) with an average BMI of 23.5 ± 3.5 kg/m2 and 47.3 ± 8.5 years were recruited. After signing the informed consent, they underwent eight abdominal HIFEM procedures in supine position with the EMSCULPT device (BTL Industries Inc.) spaced 2‐3 days apart. The device utilizes a circular coil embedded in the applicator that generates time‐varying magnetic field achieving magnetic flux densities of 1.8 Tesla. The applicator was positioned over the umbilicus and secured by a Velcro belt. During each 30‐minute session, the intensity of the HIFEM field was gradually increased to 100% to induce intense muscle contractions. Posttreatments, the subjects were instructed to avoid major diet and lifestyle changes and all of them successfully completed a 1‐month follow‐up visit.
CT imaging (General Electric VCT 64 slice Lightspeed CT scanner) was performed before the first treatment and at the 1‐month follow‐up. The scanned area was delineated by T2 and S1 vertebrae to capture the whole treated volume of the abdomen. Throughout the study, visual appearance, waist circumference (measured by anthropometric tape at the upper edge of the umbilicus), and safety of subjects were monitored.
2.2. Visceral fat assessment
To investigate changes in subject's VAT, original transverse (axial) CT scans in DICOM format were subjected to additional analysis. By using a semiautomated segmentation (InVesalius 3.1.1 software), the cross‐sectional area (CSA) of visceral fat inside the abdominal cavity was identified at the three levels including umbilical (L3‐L4 vertebrae), infraumbilical (L4‐L5 vertebrae) and supraumbilical (L2‐L3 vertebrae). A simple thresholding method was used to automatically label the voxels of densities between −200 and −50 Hounsfield units indicating adipose tissue. Automatic segmentation using this threshold was then followed by manual checking of the abdominal cavity boundary separating VAT from the SAT. Only the area occupied by VAT was considered for evaluation, and area of subcutaneous tissue was excluded. The final CSA referring to VAT was calculated for each level separately.
The 1‐month results were compared with baseline and mean difference in VAT area was tested for statistical significance by paired t test (α = 0.05). Pearson's r correlation coefficient was calculated to determine any possible relationship between VAT and previously measured variables.
3. RESULTS
The average baseline BMI of 23.5 ± 3.5 kg/m2 remained unchanged since it was equal to 23.4 ± 3.4 kg/m2 at the follow‐up. The waist circumference decreased on average by 3.9 ± 3.1 cm from 81.1 cm at baseline to 77.2 cm after the last treatment.
CT scans of all enrolled subjects were found eligible for evaluation. HIFEM procedure was safe since the posttreatment scans did not show any signs of abdominal trauma. Out of 22 treated subjects, 18 (82%) showed a measurable decrease in VAT at 1‐month follow‐up, and 15 subjects (68%) exceeded the reduction of VAT by 10%. On the other hand, two subjects did not show any improvement (change up to ±1%), and the remaining two subjects showed an increase in VAT when compared to baseline. All non‐responding subjects were females with average age (44.3 years) and BMI (22.4) that not significantly differ from study group values, nevertheless their average CSA was held below the 100 cm2, indicating healthy VAT levels. Although they did not show any plausible changes in visceral fat, they still achieved an average reduction of 16% in SAT. In general, the average posttreatment decrease of VAT in the study group was statistically significant while there was no significant difference among the umbilical, supraumbilical, and infraumbilical levels individually (see Table 1).
TABLE 1.
The average CSA (mean ± standard deviation) of visceral fat in the abdominal cavity at the predefined levels measured at baseline and 1‐mo follow‐up
| Measured level | Supraumbilical (L2‐L3) | Umbilicus (L3‐L4) | Infraumbilical (L4‐L5) | Average |
|---|---|---|---|---|
| Baseline CSA (cm2) | 107.0 ± 77.8 | 124.3 ± 72.0 | 100.5 ± 59.6 | 110.6 ± 69.0 |
| 1 mo CSA (cm2) | 90.5 ± 63.6 | 108.0 ± 57.0 | 83.3 ± 47.8 | 93.9 ± 54.6 |
| Difference in cm2 (P‐value) | 16.5 (<.01) | 16.3 (<.05) | 17.2 (<.01) | 16.7 (<.01) |
The average reduction of the VAT cross‐sectional area was 14.3% (16.7 cm2; P = .004). Male subjects (N = 3) showed greater values of visceral CSA and greater average improvement rate (19.9%) when compared with females (13.5%), however, due to their limited numbers, this tendency could not be statistically verified although the difference in VAT improvement between the sexes was 42.3 cm2. As shown in Table 1, the greatest amount of VAT was observed at the L3‐L4 level. Therefore, although the absolute differences of CSA were similar in all the three examined regions, the relative improvement rate slightly differed. The greatest VAT reduction was seen infraumbilically (17.1%; P = .002), followed by supraumbilical (15.5%; P = .003) and umbilical (10.7%; P = .02) level.
When conjoined with recently published data, 17 it was found that improvement in VAT is considerably related to improvement in SAT. After removing two outliers from the VAT data set (patients with an increase of visceral CSA), this mutual relationship showed a significant, positive, and strong correlation with r(17) = 0.66 at the significance level of P = .002. In addition, subjects with well‐developed musculature inclined to lower baseline values of visceral CSA (r(20) = 0.48; P = .03) and subjects with greater muscle increase tend to have slightly better improvement rate.
The individual CT results can be seen on Figures 1 and 2. The significant decrease of visceral volume is clearly noticeable as the segmented CSA at the 1 month (green) occupies much lesser area than baseline (blue). With decreased SAT thickness, enlargement and toning of abdominal muscles, the subjects’ body image has been substantially improved. The overall improvement of body contour achieved by the aforementioned changes was documented by the digital photographs which complemented the CT analysis (see Figures 1 and 2).
FIGURE 1.
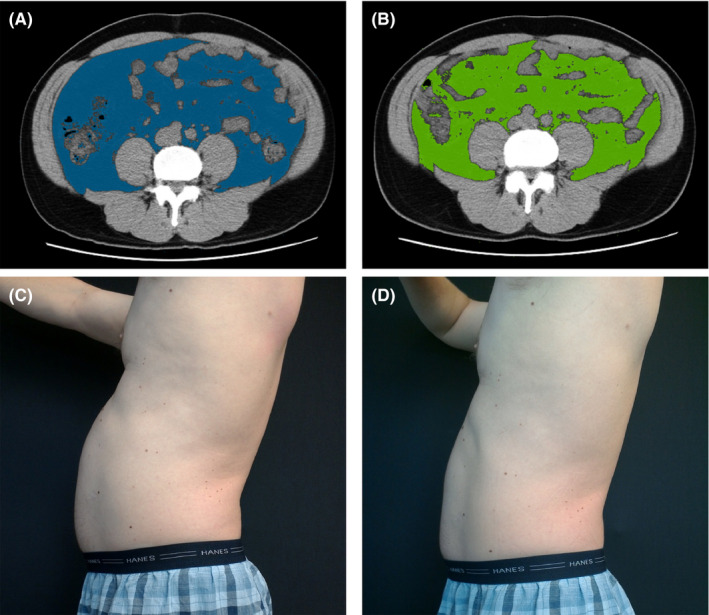
Male subject with high visceral fat ratio, 48 years old. Upper row—Infraumbilical VAT area before (A) and 1 month posttreatments (B); average VAT reduction of 19.9%, average SAT reduction of 18.2%. Bottom row—digital photographs showing improvement of the abdominal body contour from baseline (C) to 1 month (D); circumference reduction of 5 cm
FIGURE 2.
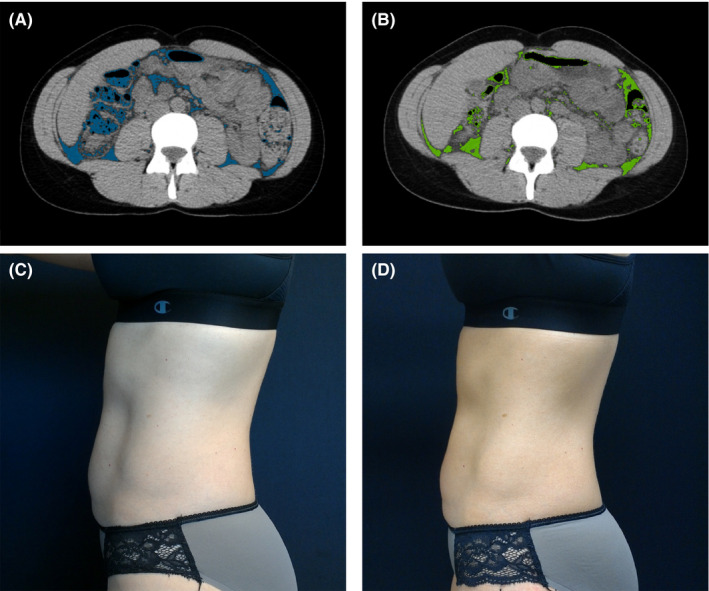
Female subject with low visceral fat ratio, 37 years old. Upper row—umbilical VAT area before (A) and 1 month posttreatments (B); average VAT reduction of 39.0%, SAT reduction of 26.0%. Bottom row—digital photographs showing improvement of the abdominal body contour from baseline (C) to 1 month (D); circumference reduction of 2 cm
4. DISCUSSION
The main outcome of this study is the documentation of the VAT reduction after a set of HIFEM abdominal treatments. HIFEM safely and effectively induced desirable aesthetic improvement of body contour through a significant decrease of both subcutaneous 17 and visceral fat.
Body contouring depends on the individual body composition including the distribution of VAT inside the abdominal cavity. As seen in this study, the individuals with better‐developed musculature were more likely to have a lesser portion of VAT at baseline which may limit the magnitude of its reduction. However, the subjects with sedentary lifestyle and noticeable “pot belly” showed greater potential for a change in VAT (see Figures 1 and 2) and SAT correspondingly. Either way, regardless of the degree of improvement, this study documented that HIFEM‐induced VAT reduction presumably contributes to the improvement of overall aesthetic appearance.
Previous studies found that HIFEM affects the SAT through intensive lipolysis, the breakdown of lipids to free fatty acids (FFA) stored inside the fat cells. 19 Validity of this mechanism in regards to VAT reduction after HIFEM is not clear yet. However, considering that VAT is more susceptible to lipolysis, it is most likely that VAT and SAT respond similarly when the muscle is exposed to supramaximal contractions. Also, the VAT has a greater capacity to generate FFAs, 5 which may explain its significant reduction when energy expenditure is elevated during and postexercise, and the muscle mass increase elevates the metabolic rate.
Our results correspond to general findings in the literature, since we found demonstrable difference in VAT deposits between men and women, 20 positive correlation between VAT and SAT reduction, 2 and between rectus abdominis fitness and low VAT values. 21 Also, the shift of group average CSA toward values below the threshold of 100 cm2 indicates a decreased risk of visceral obesity. 9 Nevertheless, the results mentioned above represent only preliminary findings of the cause‐effect relationship between HIFEM and VAT. They do not concern the examination of the hypothesized beneficial effect of lowered VAT levels on human health. Interestingly, two patients showed an increase of visceral fat at 1 month, which may be attributed to the imbalance in food intake and energy expenditure, 22 possibly followed by a compensatory increase in VAT due to the significant SAT reduction, bolstered by a lack of physical activity. 23 Also, there is increasing evidence that body fat distribution is controlled by genetic factors which may explain the outliers observed in our study; however, the polygenic background of visceral obesity has not been fully identified and outlined yet to infer decisive conclusions. 24 Future studies should, therefore, aim for more in‐depth assessment to determine any changes of metabolic parameters or proposed compensatory fat redistribution.
One of the strengths of this study is the use of CT imaging, which is considered to be a highly reliable modality for adipose tissue evaluation and has been already used by numerous authors to determine the amount of abdominal VAT. 4 , 25 , 26 In addition, VAT has shown to be uniformly distributed in the measured L2‐L5 range, 25 which only further contributes to the reliability of our results. Nevertheless, the study has some limitations. The greatest drawback is a relatively limited sample size with unbalanced numbers of male and female subjects that do not allow unbiased comparisons. Also, the study group mainly consisted of patients with BMI of 20‐26 kg/m2 thus validity of results in higher range BMI subjects should be ascertained. Lastly, the exact mechanism of VAT reduction with possible health‐related benefits and longevity of the results has not yet been examined. In the future, more research is needed for an enhanced explanation of documented results.
5. CONCLUSIONS
To our knowledge, this is the first study that documents the effect of HIFEM procedure on the visceral fat. In conclusion, the results of this study revealed a significant VAT‐reducing effect induced by HIFEM resulting in the improved aesthetic appearance of the abdomen. Further research is needed to determine whether patients may also benefit from this technology to maintain the healthy VAT levels which may possibly diminish a risk of metabolic deterioration.
CONFLICT OF INTEREST
David E. Kent MD and Brian M. Kinney MD are medical advisors for BTL Industries (Boston, MA). The authors received no financial support for the research, authorship and publication of this article.
ACKNOWLEDGMENTS
None.
Kent DE, Kinney BM. The effect of high‐intensity focused electromagnetic procedure on visceral adipose tissue: Retrospective assessment of computed tomography scans. J Cosmet Dermatol. 2021;20:757–762. 10.1111/jocd.13952
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Wajchenberg BL. Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev. 2000;21(6):697‐738. [DOI] [PubMed] [Google Scholar]
- 2. Merlotti C, Ceriani V, Morabito A, Pontiroli AE. Subcutaneous fat loss is greater than visceral fat loss with diet and exercise, weight‐loss promoting drugs and bariatric surgery: a critical review and meta‐analysis. Int J Obes. 2017;41(5):672‐682. [DOI] [PubMed] [Google Scholar]
- 3. Nicklas BJ, Penninx BWJH, Cesari M, et al. Association of visceral adipose tissue with incident myocardial infarction in older men and women: the Health, Aging and Body Composition Study. Am J Epidemiol. 2004;160(8):741‐749. [DOI] [PubMed] [Google Scholar]
- 4. Sottier D, Petit J‐M, Guiu S, et al. Quantification of the visceral and subcutaneous fat by computed tomography: interobserver correlation of a single slice technique. Diagn Interv Imaging. 2013;94(9):879‐884. [DOI] [PubMed] [Google Scholar]
- 5. Liu F, Flatt S, Nichols J, et al. Factors associated with visceral fat loss in response to a multifaceted weight loss intervention. J Obes Weight Loss Ther. 2017;7(4):346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kim Y‐A, Cho YJ. The association between visceral fat, subcutaneous fat and serum 25‐hydroxyvitamin D3 levels. Obes Med. 2019;13:29‐33. [Google Scholar]
- 7. Pickhardt PJ, Jee Y, O’Connor SD, del Rio AM. Visceral adiposity and hepatic steatosis at abdominal CT: association with the metabolic syndrome. AJR Am J Roentgenol. 2012;198(5):1100‐1107. [DOI] [PubMed] [Google Scholar]
- 8. Nicklas BJ, Penninx BWJH, Ryan AS, Berman DM, Lynch NA, Dennis KE. Visceral adipose tissue cutoffs associated with metabolic risk factors for coronary heart disease in women. Diabetes Care. 2003;26(5):1413‐1420. [DOI] [PubMed] [Google Scholar]
- 9. Freedland ES. Role of a critical visceral adipose tissue threshold (CVATT) in metabolic syndrome: implications for controlling dietary carbohydrates: a review. Nutr Metab. 2004;1:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Joy AM, Panchu P, Bahuleyan B, Vijayan V, Jojy J. Age and sex variation in the distribution of visceral fat among healthy doctors. Int J Res Med Sci. 2018;7(1):186. [Google Scholar]
- 11. Zhang H, Tong TK, Qiu W, et al. Comparable effects of high‐intensity interval training and prolonged continuous exercise training on abdominal visceral fat reduction in obese young women. J Diabetes Res. 2017;2017:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Irving BA, Davis CK, Brock DW, et al. Effect of exercise training intensity on abdominal visceral fat and body composition. Med Sci Sports Exerc. 2008;40(11):1863‐1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jacob C, Kinney B, Busso M, et al. High intensity focused electro‐magnetic technology (HIFEM) for non‐invasive buttock lifting and toning of gluteal muscles: a multi‐center efficacy and safety study. J Drugs Dermatol JDD. 2018;17(11):1229‐1232. [PubMed] [Google Scholar]
- 14. Kinney BM, Lozanova P. High intensity focused electromagnetic therapy evaluated by magnetic resonance imaging: safety and efficacy study of a dual tissue effect based non‐invasive abdominal body shaping: MRI evaluation of electromagnetic therapy. Lasers Surg Med. 2019;51(1):40‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Katz B. MRI assessment of arm and calf muscle toning with high‐intensity focused electromagnetic technology: case study. J Drugs Dermatol. 2020;19(5):408‐410. [PubMed] [Google Scholar]
- 16. Duncan D, Dinev I. Noninvasive induction of muscle fiber hypertrophy and hyperplasia: effects of high‐intensity focused electromagnetic field evaluated in an in‐vivo porcine model: a pilot study. Aesthet Surg J. 2020;40(5):568‐574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kent DE, Jacob CI. Simultaneous changes in abdominal adipose and muscle tissues following treatments by high‐intensity focused electromagnetic (HIFEM) technology‐based device: computed tomography evaluation. J Drugs Dermatol JDD. 2019;18(11):1098‐1102. [PubMed] [Google Scholar]
- 18. Katz B, Bard R, Goldfarb R, Shiloh A, Kenolova D. Ultrasound assessment of subcutaneous abdominal fat thickness after treatments with a high‐intensity focused electromagnetic field device: a multicenter study. Dermatol Surg. 2019;45(12):1542‐1548. [DOI] [PubMed] [Google Scholar]
- 19. Halaas Y, Bernardy J. Mechanism of nonthermal induction of apoptosis by high‐intensity focused electromagnetic procedure: Biochemical investigation in a porcine model. J Cosmet Dermatol. 2020;19(3):605‐611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Onat A, Avci GS, Barlan MM, Uyarel H, Uzunlar B, Sansoy V. Measures of abdominal obesity assessed for visceral adiposity and relation to coronary risk. Int J Obes Relat Metab Disord J Int Assoc Study Obes. 2004;28(8):1018‐1025. [DOI] [PubMed] [Google Scholar]
- 21. Ramírez‐Vélez R, Correa‐Rodríguez M, Izquierdo M, Schmidt‐RioValle J, González‐Jiménez E. Muscle fitness to visceral fat ratio, metabolic syndrome and ideal cardiovascular health metrics. Nutrients. 2018;11(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ozato N, Saito S, Yamaguchi T, et al. Association between nutrients and visceral fat in healthy Japanese adults: a 2‐year longitudinal study brief title: micronutrients associated with visceral fat accumulation. Nutrients. 2019;11(11):2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Benatti F, Solis M, Artioli G, et al. Liposuction induces a compensatory increase of visceral fat which is effectively counteracted by physical activity: a randomized trial. J Clin Endocrinol Metab. 2012;97(7):2388‐2395. [DOI] [PubMed] [Google Scholar]
- 24. Schleinitz D, Böttcher Y, Blüher M, Kovacs P. The genetics of fat distribution. Diabetologia. 2014;57(7):1276‐1286. [DOI] [PubMed] [Google Scholar]
- 25. Lee SJ, Liu J, Yao J, Kanarek A, Summers RM, Pickhardt PJ. Fully automated segmentation and quantification of visceral and subcutaneous fat at abdominal CT: application to a longitudinal adult screening cohort. Br J Radiol. 2018;91(1089):20170968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ryckman EM, Summers RM, Liu J, del Rio AM, Pickhardt PJ. Visceral fat quantification in asymptomatic adults using abdominal CT: is it predictive of future cardiac events? Abdom Imaging. 2015;40(1):222‐226. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


