Abstract
Background
During COVID-19 pandemic, elective invasive cardiac procedures (ICP) have been frequently cancelled or postponed. Consequences may be more evident in patients with diabetes.
Objectives
The objective was to identify the peculiarities of patients with DM among those in whom ICP were cancelled or postponed due to the COVID-19 pandemic, as well as to identify subgroups in which the influence of DM has higher impact on the clinical outcome.
Methods
We included 2,158 patients in whom an elective ICP was cancelled or postponed during COVID-19 pandemic in 37 hospitals in Spain. Among them, 700 (32.4%) were diabetics. Patients with and without diabetes were compared.
Results
Patients with diabetes were older and had a higher prevalence of other cardiovascular risk factors, previous cardiovascular history and co-morbidities. Diabetics had a higher mortality (3.0% vs. 1.0%; p = 0.001) and cardiovascular mortality (1.9% vs. 0.4%; p = 0.001). Differences were especially important in patients with valvular heart disease (mortality 6.9% vs 1.7% [p < 0.001] and cardiovascular mortality 4.9% vs 0.9% [p = 0.002] in patients with and without diabetes, respectively). In the multivariable analysis, diabetes remained as an independent risk factor both for overall and cardiovascular mortality. No significant interaction was found with other clinical variables.
Conclusion
Among patients in whom an elective invasive cardiac procedure is cancelled or postponed during COVID-19 pandemic, mortality and cardiovascular mortality is higher in patients with diabetes, irrespectively on other clinical conditions. These procedures should not be cancelled in patients with diabetes.
Keywords: Diabetes, Interventional cardiology, COVID-19, Mortality, Waiting list
Introduction
The ongoing COVID-19 pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was declared by the World Health Organization (WHO) in March 2020 [1]. By January 2021, almost 100 million people had suffered the disease, and nearly 2 million have died worldwide. Apart from these direct consequences, health care systems have been severely overwhelmed, negatively impacting on the management of other patients that usually require prompt treatment, especially those with cardiovascular diseases [2–8]. Specifically, invasive cardiac procedures (ICP) have been cancelled or postponed in many centers, and this may have fatal consequences for some patients, as we have recently shown in a multicenter study from Spain [9].
Cardiovascular diseases constitute the main cause of death in patients with diabetes mellitus (DM) [10], and among patients with cardiovascular diseases, those with DM are at an especially high risk of death [11, 12]. Because of that, waiting list in patients pending on cardiovascular procedures that have been postponed due to the pandemic may have especial impact among diabetics [9].
The objective was to identify the peculiarities of patients with DM among those in whom ICP were cancelled or postponed due to the COVID-19 pandemic, as well as to identify subgroups in which the influence of DM has higher impact on the clinical outcome.
Methods
Study population
We have previously published the outcome of patients in whom elective ICP were cancelled or postponed when the state of alarm due to the COVID-19 pandemic was declared in Spain on the 14th of March 2020. In this study, 2,158 patients were included in 37 hospitals [8].
At the time of the publication of that study, DM status was known in 2,110, whereas no information was available for 48 patients. For the present sub-study, doing additional efforts, directly contacting with the patient or obtaining documents from the referral centers, we could obtain DM status for all 2158 patients.
Data collection and follow-up
Data were entered in an electronic database (pInvestiga, Moaña, Pontevedra, Spain). Clinical variables, such as main cardiovascular disease pending on treatment, type of procedure pending to be performed, clinical situation, and cardiovascular risk factors, were collected.
Patients were followed-up until the 30th of April 2020 (45 days) [8]. Patients with DM were compared with those without DM, regarding type of pending procedure, main cardiovascular disease, functional class for heart failure and angina, and other clinical variables. The influence of DM in different patient subgroups was evaluated.
Definitions
Coronary angiography and/or PCI as the type of pending procedure included coronary angiography in patients with previously diagnosed or suspected CAD, and those with previously known CAD pending on PCI (e.g. stage procedures). Coronary angiography to rule out CAD as the underlying cause of left ventricular dysfunction was also included in this category. However, coronary angiography as part of the study of patients pending on any type of surgical intervention was included in a different category, because the main underlying condition was considered to be the disorder pending to be treated (e.g. valvular heart disease) rather than the eventual bystander of coronary artery disease. Other procedures included transcatheter aortic valve implantation (TAVI), percutaneous mitral valve repair, left atrial appendage closure, percutaneous closure of ASD, or treatment of tricuspid regurgitation.
Statistical analysis
Continuous variables are presented as mean ± standard deviation and compared using the Student t-test or appropriate non-parametric tests. Discrete variables are presented as percentages (proportions), and compared with the Chi-square test, using Fisher correction when needed. Statistical analysis was done using the SPSS statistical package (Chicago, Illinois). Associations were considered statistically significant when p < 0.05, although all p values are presented. Univariable and multivariable analysis were conducted in order to identify independent risk factors for mortality, and for secondary endpoints.
Results
Type of pending procedure
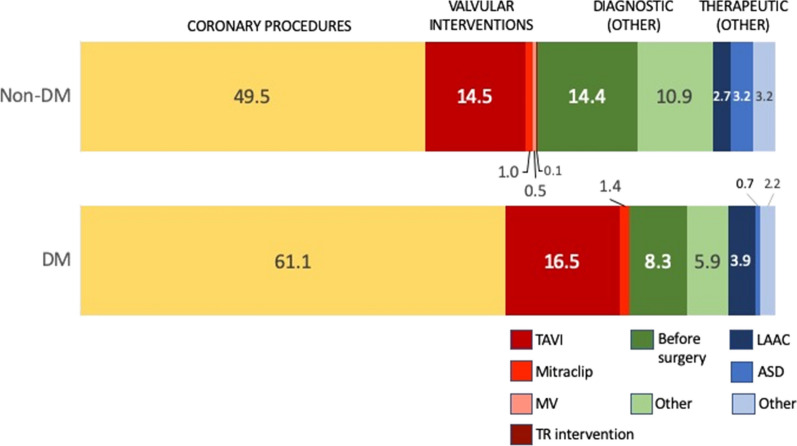
Out of the 2,158 patients, 700 (32.4%) were DM. Figure 1 shows the type of pending procedure in patients with and without DM. Coronary diagnostic and/or therapeutic intervention was the most frequent pending procedure for both groups of patients, but it was more frequent in DM than in non-DM (61.5% vs. 49.5%, respectively; p < 0.001). The second type of procedure was percutaneous valvular intervention, that accounted for 17.9% and 16.2% for DM and non-DM, respectively (p = 0.300). Other diagnostic procedure was pending in 14.2% and 25.2% of DM and non-DM patients, respectively (p < 0.001). Other therapeutic procedure was pending in 6.7% and 9.1% in patients with and without DM, respectively (p = 0.060).
Fig. 1.
Type of pending procedures in patiens with and without DM
Comparison of patients with and without DM
Table 1 shows the differences among patients with and without DM in relation with clinical characteristics. Patients with DM were older, and had a higher prevalence of hypertension, hypercholesterolemia, chronic renal failure, peripheral artery disease, and previously diagnosed coronary artery disease including previous infarction, and previous myocardial revascularization. Left ventricular dysfunction was more frequently present in patients with DM. Functional class for heart failure (NYHA) was similar for patients with and without DM, but functional class for angina (CCS) was worse in patients with DM.
Table 1.
Clinical characteristics of patients with and without DM
| DM | |||
|---|---|---|---|
| Yes (n = 700) | No (n = 1458) | P value | |
| Age | 72.3 ± 10.0 | 69.2 ± 12.7 | < 0.001 |
| Age ≥ 80 (%) | 24.9 | 21.4 | 0.078 |
| Female gender (%) | 34.9 | 39.9 | 0.066 |
| Hypertension (%) | 82.9 | 59.8 | < 0.001 |
| Hypercholesterolemia (%) | 71.0 | 47.9 | < 0.001 |
| Smoking (%) | 30.8 | 29.3 | 0.483 |
| Chronic renal failure (%) | 13.2 | 7.5 | < 0.001 |
| Peripheral artery disease (%) | 14.2 | 9.0 | < 0.001 |
| Previous CAD (%) | 41.7 | 27.4 | < 0.001 |
| Previous infarction (%) | 17.9 | 11.4 | < 0.001 |
| Previous PCI (%) | 23.6 | 15.5 | < 0.001 |
| Previous CABG (%) | 6.7 | 3.4 | 0.001 |
| Previous valve replacement (%) | 3.5 | 4.9 | 0.144 |
| Left ventricular dysfunction (%) | 27.1 | 21.4 | 0.033 |
| NYHA > II (%) | 20.1 | 19.0 | 0.282 |
| CCS > II (%) | 10.0 | 8.4 | 0.001 |
| Main cardiovascular condition (%) | |||
| Ischemic heart disease | 57.6 | 47.0 | < 0.001 |
| Valvular heart disease | 29.2 | 36.9 | |
| Other | 13.3 | 16.2 | |
CAD coronary artery disease, PCI Percutaneous coronary intervention, CABG Coronary artery bypass grafting, NYHA New York Heart Association, CCS Cardiology Canadian Society
Among the 2,158 patients, 559 had previously documented coronary artery disease. Patients with DM had higher frequency of multi-vessel disease (72.9% vs. 56.7% in non-DM, p < 0.001). Left main disease was also more frequent in patients with DM, but differences were not statistically significant (13.9% vs. 9.8% in non-DM, p = 0.133).
Influence of DM on clinical outcomes
During the 45-day follow-up period, 36 patients died (1.7%), most of them due to cardiovascular causes (n = 19, 59.4%). Patients with DM had a higher rate of both overall mortality (3.0% vs. 1.0% in non-DM, p = 0.001) and cardiovascular mortality (1.9% vs. 0.4% in non-DM, p = 0.001), whereas differences in non-cardiovascular mortality were not statistically different (1.1% vs. 0.6% in DM and non-DM, respectively; p = 0.196).
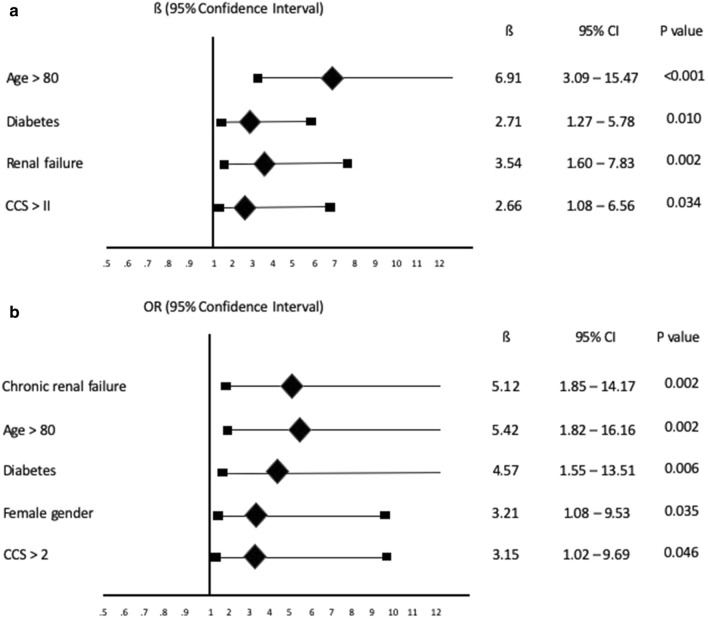
In the multivariable analysis, DM remained as an independent risk factor both for overall and cardiovascular mortality (Fig. 2).
Fig. 2.
Independent risk factors for mortality (a) and cardiovascular mortality (b)
The proportion of patients that underwent an urgent procedure due to clinical instabilization was also significantly higher in patients with DM (10.4% vs. 7.3% in non-DM; p = 0.015).
During the study period, 17 patients with DM (2.4%) and 21 without DM (1.4%) had a diagnosis of COVID-19 by protein-chain reaction test for SARS-CoV-2 (p = 0.157). Out of these patients, 11 (29.7%) died. Among patients with COVID-19 disease, 16 were diabetics, and 21 non diabetics, mortality being higher in diabetics (6/16; 37.5%) than in non diabetics (5/21; 23.8%), but difference was not statistically significant (p = 0.475).
Mortality in patients with and without DM among different subgroups
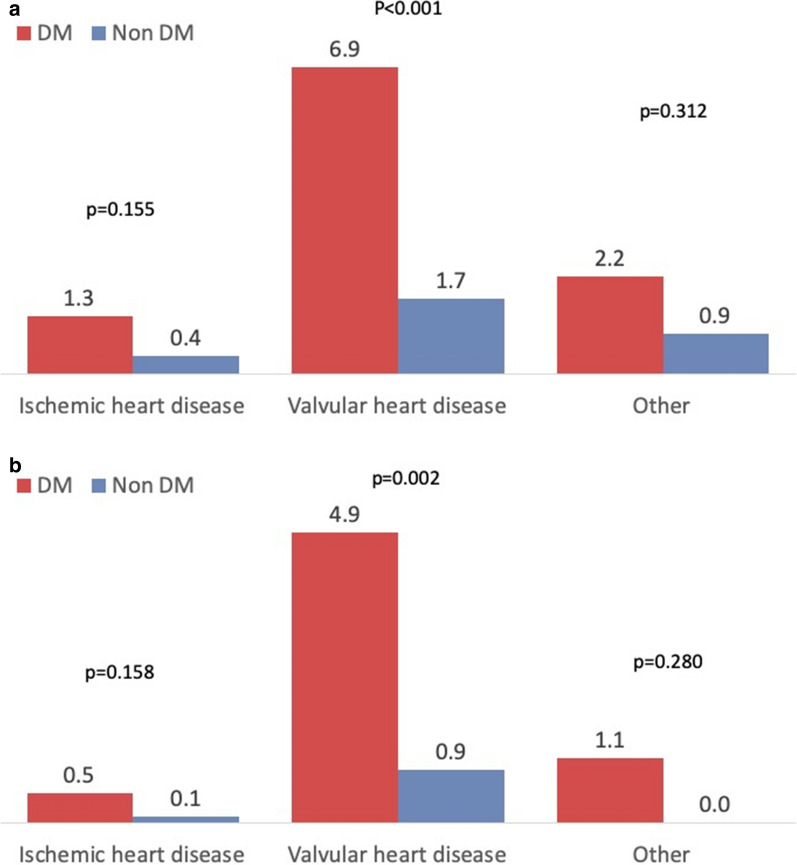
Mortality and cardiovascular mortality were higher in patients with DM regardless the main cardiovascular disease, although differences were statistically significant only for those patients with valvular heart disease (Fig. 3a and b).
Fig. 3.
Mortality (a) and cardiovascular mortality (b) rates in patients with and without DM accordingly to the main cardiovascular disease
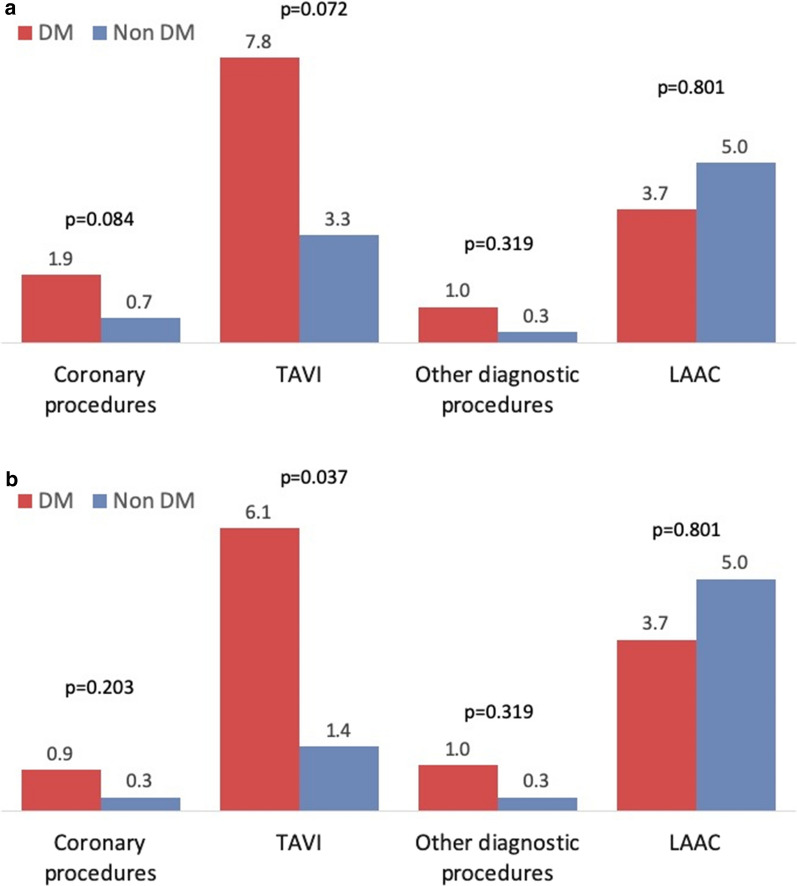
Figure 4 shows the mortality and cardiovascular mortality rates in patients with and without DM in the most frequent types of pending procedures. Mortality and cardiovascular mortality rates were higher in patients pending on coronary diagnostic or therapeutic procedures, TAVI, and other diagnostic procedures, but differences reached statistical significance only for cardiovascular mortality in patients pending on TAVI. In patients pending on LAAC, mortality was higher in non-DM but differences were not statistically different.
Fig. 4.
Mortality (a) and cardiovascular mortality (b) in patients with and without DM accordingly to the type of pending procedure
Tables 2 and 3 show the overall and cardiovascular mortality in patients with and without DM in different patient subgroups accordingly to clinical characteristics. No significant interaction was found between DM and other clinical variables (Table 4).
Table 2.
Mortality in patients with and without DM in different patients subgroups
| Factor present | ||||||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| DM | Non-DM | P value | DM | Non-DM | P value | |
| Age > 80 (%) | 7.5 | 3.8 | 0.071 | 1.5 | 0.3 | 0.006 |
| Female gender (%) | 5.0 | 1.2 | 0.001 | 2.0 | 0.9 | 0.098 |
| Hypertension (%) | 3.3 | 1.1 | 0.003 | 0.0 | 0.7 | 0.362 |
| Hypercholesterolemia (%) | 3.3 | 1.2 | 0.012 | 1.5 | 0.7 | 0.378 |
| Smoking (%) | 1.0 | 0.2 | 0.262 | 3.4 | 1.2 | 0.004 |
| Chronic renal failure (%) | 9.9 | 2.8 | 0.036 | 2.0 | 0.9 | 0.044 |
| Peripheral artery disease (%) | 3.1 | 3.1 | 1.000 | 3.0 | 0.8 | < 0.001 |
| Previous CAD (%) | 2.4 | 1.8 | 0.537 | 3.0 | 0.7 | 0.001 |
| Previous infarction (%) | 2.4 | 0.6 | 0.314 | 3.1 | 1.1 | 0.002 |
| Previous PCI (%) | 2.4 | 0.4 | 0.165 | 3.2 | 1.1 | 0.003 |
| Previous CABG (%) | 0.0 | 6.3 | 0.242 | 3.2 | 0.9 | < 0.001 |
| Previous valve replacement (%) | 4.3 | 1.5 | 0.444 | 2.6 | 0.8 | 0.002 |
| Left ventricular dysfunction (%) | 1.6 | 0.7 | 0.370 | 3.2 | 1.0 | 0.001 |
| NYHA > 2 (%) | 7.1 | 2.5 | 0.061 | 2.1 | 0.7 | 0.014 |
| CCS > 2 (%) | 4.8 | 3.9 | 1.000 | 2.7 | 0.7 | 0.001 |
PC Percutaneous coronary intervention. CABG Coronary artery bypass grafting, NYHA New York Heart Association, CCS Cardiology Canadian Society
Table 3.
Cardiovascular mortality in patients with and without DM in different patients subgroups
| Factor present | ||||||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| DM | Non-DM | P value | DM | Non-DM | P value | |
| Age > 80 (%) | 4.6 | 1.9 | 0.093 | 1.0 | 0.0 | 0.003 |
| Female gender (%) | 4.1 | 0.5 | 0.001 | 0.7 | 0.3 | 0.409 |
| Hypertension (%) | 2.3 | 0.5 | 0.002 | 0.0 | 0.2 | 1.000 |
| Hypercholesterolemia (%) | 2.0 | 0.6 | 0.023 | 1.5 | 0.1 | 0.032 |
| Smoking (%) | 0.5 | 0.0 | 0.335 | 2.3 | 0.5 | 0.002 |
| Chronic renal failure (%) | 7.7 | 1.9 | 0.083 | 1.0 | 0.3 | 0.079 |
| Peripheral artery disease (%) | 0.0 | 0.0 | 1.000 | 2.2 | 0.5 | < 0.001 |
| Previous CAD (%) | 1.4 | 0.5 | 0.244 | 2.3 | 0.4 | 0.002 |
| Previous infarction (%) | 0.8 | 0.6 | 1.000 | 2.1 | 0.4 | < 0.001 |
| Previous PCI (%) | 1.8 | 0.4 | 0.312 | 1.9 | 0.4 | 0.004 |
| Previous CABG (%) | 0.0 | 2.1 | 1.000 | 2.0 | 0.4 | < 0.001 |
| Previous valve replacement (%) | 4.3 | 0.0 | 0.253 | 1.7 | 0.4 | 0.002 |
| Left ventricular dysfunction (%) | 1.1 | 0.7 | 0.635 | 2.2 | 0.4 | 0.001 |
| NYHA > 2 (%) | 5.1 | 1.2 | 0.049 | 1.6 | 0.2 | 0.004 |
| CCS > 2 (%) | 3.2 | 2.9 | 1.000 | 1.8 | 0.2 | < 0.001 |
PCI Percutaneous coronary intervention, CABG Coronary artery bypass grafting, NYHA New York Heart Association, CCS Cardiology Canadian Society
Table 4.
Interaction between different variables and the effect of diabetes on mortality and cardiovascular mortality
| P for interaction | ||
|---|---|---|
| Mortality | Cardiovascular mortality | |
| Age > 80 (%) | 0.192 | 0.990 |
| Female gender (%) | 0.353 | 0176 |
| Hypertension (%) | 0.996 | 0.996 |
| Hypercholesterolemia (%) | 0.774 | 0.375 |
| Smoking (%) | 0.799 | 0.994 |
| Chronic renal failure (%) | 0.499 | 0.790 |
| Peripheral artery disease (%) | 0.128 | 1.000 |
| Previous CAD (%) | 0.102 | 0.478 |
| Previous infarction (%) | 0.774 | 0.361 |
| Previous PCI (%) | 0.550 | 0.950 |
| Previous CABG (%) | ||
| Previous valve replacement (%) | 0.976 | 0.997 |
| Left ventricular dysfunction (%) | ||
| NYHA > 2 (%) | 0.953 | 0.561 |
| CCS > 2 (%) | 0.212 | 0.066 |
Discussion
Among patients in whom an elective cardiac invasive procedure was cancelled or postponed, those with DM had a significantly higher mortality, mainly due to a higher cardiovascular mortality. Overall mortality was 3 times higher and cardiovascular mortality 4.75 times higher in DM in comparison with patients without DM.
Patients with DM had a worse clinical profile, including more advanced age, and higher prevalence of additional cardiovascular risk factors, previous cardiovascular diseases, and some co-morbidities, such as renal failure. However, DM was an independent predictor both for mortality and cardiovascular mortality, indicating that DM per se is a risk factor in this special population. The main practical implication of these findings is that elective invasive cardiac procedures should be prioritized in patients with DM. That is, during COVID-19 pandemic, invasive cardiac procedures should not be postponed in patients with DM. Even, this may be applicable not only during COVID-19 pandemic in particular [7], but also in other situations in which health care system cannot adequately attend all patients pending on invasive procedures, and in waiting list management of interventional cardiology in general.
No significant interaction was found between DM and other clinical variables. This simplifies the indication of not cancelling ICP in patients with DM, because mortality and cardiovascular mortality was higher in patients with DM irrespectively on other clinical characteristics.
The worse outcome in patients with DM may have several reasons. First, DM is associated with an impaired systolic and diastolic left ventricular function in patients without significant coronary artery disease [13], and this could have a negative impact on the outcome of patients with heart failure or valvular heart disease. Second, DM patients have a procoagulant state [14] that may increase the risk of thromboembolic events in patients pending on structural interventions. Third, the response to anti-thrombotic agents is impaired in patients with DM [15], and this could have an impact on the risk of ischemic events in patients pending on coronary interventions. Fourth, coronary artery disease is more frequent and more severe in patients with DM and severe valvular disease [16], and this could have a negative prognostic impact on clinical outcome. Finally, DM predisposes to infections [18], that constitute an important cause of non-cardiovascular death in elderly cardiovascular patients [19, 20].
DM had a negative impact on mortality in all type of pending ICP. DM is associated with more severe coronary stenosis [17], and is a very well known risk factor for mortality in patients with CAD [11, 12].
Among patients with aortic stenosis, those with DM have a higher mortality rate [21]. This may be partly explained by the higher frequency of some co-morbidities (e.g. renal insufficiency) and CAD [16], but DM also might have a direct effect on prognosis of these patients. Among patients with aortic stenosis, those with DM have a more impaired myocardial function and more severe hypertrophy [22]. In patients with aortic valve sclerosis, insulin resistance is a powerful independent predictor of subclinical left ventricular dysfunction regardless of concomitant visceral obesity and left ventricular hypertrophy [23]. Additionally, DM impairs coronary microvascular function in asymptomatic patients with severe aortic and non-obstructed coronary arteries [24]. Besides these potential explanations, cardiac mortality rate was unexpectedly high in DM patients awaiting a valvular procedure during a relatively short follow-up (45 days), and this novel finding warrants further research.
Other procedures apart from coronary and valvular interventions had also higher mortality in patients with DM. DM is a risk factor for mortality in patients on atrial fibrillation [25], and thus it is not surprising that among patients pending on LAAC, mortality was higher in diabetics.
Study limitations
This study has several limitations. First, the main goal of this study was to evaluate the short-term consequences of delaying or postponing invasive cardiac procedures. Because of that, clinical follow-up was restricted to only 45 days. Second, metabolic control, treatment of diabetes and type of diabetes were not collected, and therefore the potential influence of these factors could not be evaluated. Finally, some patients underwent an emergent procedure due to clinical instabilization. As this occurred more frequently in patients with DM, the influence of DM on mortality in our population even may have been underestimated.
Conclusion
Among patients in whom an elective invasive cardiac procedure is cancelled or postponed, those with DM have an especial worse clinical outcome, with higher mortality and cardiovascular mortality rates at short-term, irrespective on other clinical conditions. Elective invasive cardiac procedures should be prioritized in patients with diabetes.
Acknowledgements
Not applicable.
Abbreviations
- ASD
Atrial Septal Defect
- CABG
Coronary Artery Bypass Grafting
- CAD
Coronary Artery Disease
- CCS
Canadian Cardiac Society
- COVID-19
COronaVIrus Disease 2019
- DM
Diabetes
- ICP
Invasive Cardiac Procedures
- LAAC
Left Atrial Appendage Closure
- NYHA
New York Heart Association
- PCI
Percutaneous Coronary Intervention
- SARS-CoV-2
Severe Acute Respiratory Syndrome CoronaVirus 2
- TAVI
Transcatheter aortic valve implantation
Authors' contributions
all authors have approved the submitted versión of the manuscript, and have agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.Each author contribution is detailed below: Substantial contributions to the conception: RM, JAD, JAB, APP, FS, AGB, VRQ, FJI, BGB, MV, Design of the work: RM, JLD, RT, IAS, RR, SO, ICG, JM, SMBP,.Acquisition, analysis, and interpretation of data: RM, PS, JAC, PP, JJM, AF, EP. Drafted the work or substantively revised it: RM, JMTH, JFD, BV, DMS, FA, EB, EP, JRRA, FL, JRR, EN, EAB, RL. All authors read and approved the final manuscript.
Funding
Funding for data collection and analysis: Association of Interventional Cardiology of the Spanish Society of Cardiology (ACI-SEC). No funding was used for interpretation of data or manuscript writing.
Availability of data and materials
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Since this work was done during acute phase of COVID-19 pandemic, involving aspects related with the pandemic, ethics committee aproval was not required.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report - 78. Geneva: WHO; 2020. World Health Organization. Coronavirus disease . (COVID-19) Situation Report - 78. Geneva: WHO; 2019. p. 2020. [Google Scholar]
- 2.Rodríguez-Leor O, Cid-Álvarez B, Ojeda S, Martín-Moreiras J, Rumoroso JR, López-Palop R, et al. On behalf of all the participants of the ACI-SEC Infarction Code Registry Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. Interv Cardiol. 2020;2:82–89. [Google Scholar]
- 3.Romaguera R, Cruz-González I, Jurado-Román A, Ojeda S, Fernández-Cisnal A, Jorge-Pérez P, et al. Considerations on the invasive management of ischemic and structural heart disease during the COVID-19 coronavirus outbreak. Consensus statement of the Interventional Cardiology Association and the Ischemic Heart Disease and Acute Cardiac Care Association of the Spanish Society of Cardiology. REC Interv Cardiol. 2020;2:106–111. [Google Scholar]
- 4.Rodríguez-Leor O, Cid-Álvarez B, de Prado A, Rossello X, Ojeda S, Serrador A, López-Palop R, Martín-Moreiras J, et al. Impact of COVID-19 on ST-segment elevation myocardial infarction care The Spanish experience. Rev Esp Cardiol. 2020;73:994–1002. doi: 10.1016/j.recesp.2020.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chieffo A, Stefanini GG, Price S, Barbato E, Tarantini G, Karam N, Moreno R, Buchanan GL, Gilard M, Halvorsen S, Huber K, James S, Neumann FJ, Möllmann H, Roffi M, Tavazzi G, Mauri Ferré J, Windecker S, Dudek D, Baumbach A. EAPCI Position Statement on Invasive Management of Acute Coronary Syndromes during the COVID-19 pandemic. Eur Heart J. 2020;41:1839–1851. doi: 10.1093/eurheartj/ehaa381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Luca G, Verdoia M, Cercek M, Jensen LO, Vavlukis M, Calmac L, Johnson T, Ferrer GR, Ganyukov V, Wojakowski W, et al. Impact of COVID-19 pandemic on mechanical reperfusion for patients with STEMI. J Am Coll Cardiol. 2020;76:2321–2330. doi: 10.1016/j.jacc.2020.09.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chieffo A, Tarantini G, Naber CK, Barbato E, Roffi M, Stefanini GG, Buchanan GL, Buszman P, Moreno R, Zawiślak B, Cayla G, Danenberg H, Da Silveira JAB, Nef H, James SK, Mauri Ferre J, Voskuil M, Witt N, Windecker S, Baumbach A, Dudek D. Performing elective cardiac invasive procedures during the COVID-19 outbreak: a position statement from the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Eur Heart J. 2020;41:1839–1851. doi: 10.1093/eurheartj/ehaa381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moreno R, Ojeda S, Romaguera R, Jimenez-Quevedo P, Cruz-González I. Transcatheter aortic valve replacement during COVID-19 pandemic Recommendations from the Association of Interventional Cardiology of the Spanish Society of Cardiology (ACI-SEC). REC: Interv Cardiol 2020;2:230–231.
- 9.Moreno R, Díez JL, Diarte JA, Macaya F, et al Consequences of canceling elective invasive cardiac procedures during Covid-19 outbreak. Catheter Cardiovasc Interv. 2020.Doi: 10.1002/ccd.29433(Epub ahead of print). [DOI] [PubMed]
- 10.Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17:83. doi: 10.1186/s12933-018-0728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Malmberg K, Yusuf S, Gerstein HC, Brown J, Zhao F, Hunt D, Piegas L, Calvin J, Keltai M, Budaj A. Impact of diabetes on long-term prognosis in patients with unstable angina and non-Q-wave myocardial infarction: results of the OASIS (Organization to Assess Strategies for Ischemic Syndromes) Registry. Circulation. 2000;102:1014–1019. doi: 10.1161/01.CIR.102.9.1014. [DOI] [PubMed] [Google Scholar]
- 12.Moreno R, de Sa E, Lopez-Sendon JL, Ortega A, Fernández MJ, Fernandez-Bobadilla J, et al. Prognosis of medically stabilized unstable angina pectoris with a negative exercise test. Am J Cardiol. 1998;82:662–5. doi: 10.1016/S0002-9149(98)00411-1. [DOI] [PubMed] [Google Scholar]
- 13.Andersson C, Gislason GH, Weeke P, Hoffmann S, Hansen PR, Torp-Pedersen C, Søgaard P. Diabetes is associated with impaired myocardial performance in patients without significant coronary artery disease. Cardiovasc Diabetol. 2010;9:3. doi: 10.1186/1475-2840-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jax TW, Peters AJ, Plehn G, Schoebel FC. Hemostatic risk factors in patients with coronary artery disease and type 2 diabetes - a two year follow-up of 243 patients. Cardiovasc Diabetol. 2009;8:48. doi: 10.1186/1475-2840-8-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Angiolillo DJ, Bernardo E, Sabaté M, Jimenez-Quevedo P, Costa MA, Palazuelos J, Hernández-Antolin R, Moreno R, Escaned J, Alfonso F, Bañuelos C, Guzman LA, Bass TA, Macaya C, Fernandez-Ortiz A. Impact of platelet reactivity on cardiovascular outcomes in patients with type 2 diabetes mellitus and coronary artery disease. J Am Coll Cardiol. 2007;50:1541–1547. doi: 10.1016/j.jacc.2007.05.049. [DOI] [PubMed] [Google Scholar]
- 16.Lappé JM, Grodin JL, Wu Y, Bott-Silverman C, Cho L. Prevalence and prediction of obstructive coronary artery disease in patients referred for valvular heart surgery. Am J Cardiol. 2015;116:280–285. doi: 10.1016/j.amjcard.2015.03.063. [DOI] [PubMed] [Google Scholar]
- 17.Chu ZG, Yang ZG, Dong ZH, Zhu ZY, Peng LQ, Shao H, He C, Deng W, Tang SS, Chen J. Characteristics of coronary artery disease in symptomatic type 2 diabetic patients: evaluation with CT angiography. Cardiovasc Diabetol. 2010;9:74. doi: 10.1186/1475-2840-9-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moutschen MP, Scheen AJ, Lefebvre PJ. Impaired immune responses in diabetes mellitus: analysis of the factors and mechanisms involved Relevance to the increased susceptibility of diabetic patients to specific infections. Diabete Metab. 1992;18:187–201. [PubMed] [Google Scholar]
- 19.Moreno R, Calvo L, Salinas P, Dobarro D, Santiago JV, Sanchez A, Galeote G, Riera L, Moreno-Gomez I, Mesa J, Plaza I, Lopez-Sendon J. Causes of peri-operative mortality after transcatheter aortic valve implantation: a pooled analysis of 12 studies and 1223 patients. J Invasive Cardiol. 2011;23:180–184. [PubMed] [Google Scholar]
- 20.Aschauer S, Zotter-Tufaro C, Duca F, Kammerlander A, Dalos D, Mascherbauer J, Bonderman D. Modes of death in patients with heart failure and preserved ejection fraction. Int J Cardiol. 2017;228:422–426. doi: 10.1016/j.ijcard.2016.11.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lancellotti P, Magne J, Dulgheru R, Clavel MA, Donal E, Vannan MA, Chambers J, Rosenhek R, Habib G, Lloyd G, Nistri S, Garbi M, Marchetta S, Fattouch K, Coisne A, Montaigne D, Modine T, Davin L, Gach O, Radermecker M, Liu S, Gillam L, Rossi A, Galli E, Ilardi F, Tastet L, Capoulade R, Zilberszac R, Vollema EM, Delgado V, Cosyns B, Lafitte S, Bernard A, Pierard LA, Bax JJ, Pibarot P, Oury C. Outcomes of Patients With Asymptomatic Aortic Stenosis Followed Up in Heart Valve Clinics. JAMA Cardiol. 2018;3:1060–1068. doi: 10.1001/jamacardio.2018.3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pagé A, Dumesnil JG, Clavel MA, Chan KL, Teo KK, Tam JW, Mathieu P, Després JP, Pibarot P; ASTRONOMER Investigators. Metabolic syndrome is associated with more pronounced impairment of left ventricle geometry and function in patients with calcific aortic stenosis: a substudy of the ASTRONOMER (Aortic Stenosis Progression Observation Measuring Effects of Rosuvastatin). J Am Coll Cardiol. 2010;55:1867–74. [DOI] [PubMed]
- 23.Utsunomiya H, Yamamoto H, Kunita E, Hidaka T, Kihara Y. Insulin resistance and subclinical abnormalities of global and regional left ventricular function in patients with aortic valve sclerosis. Cardiovasc Diabetol. 2014;13:86. doi: 10.1186/1475-2840-13-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Julius BK, Spillmann M, Vassalli G, Villari B, Eberli FR, Hess OM. Angina pectoris in patients with aortic stenosis and normal coronary arteries. Mech Pathophysiol Concepts Circ. 1997;95:892–898. doi: 10.1161/01.cir.95.4.892. [DOI] [PubMed] [Google Scholar]
- 25.Bassand JP, Virdone S, Goldhaber SZ, Camm AJ, Fitzmaurice DA, Fox KAA, Goto S, Haas S, Hacke W, Kayani G, Mantovani LG, Misselwitz F, Pieper KS, Turpie AGG, van Eickels M, Verheugt FWA, Kakkar AK. Early risks of death, stroke/systemic embolism, and major bleeding in patients with newly diagnosed atrial fibrillation. Circulation. 2019;139:787–798. doi: 10.1161/CIRCULATIONAHA.118.035012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.