To the Editor: A myriad of potential dermatologic manifestations of COVID-19, caused by SARS-CoV-2, has been reported.1, 2, 3, 4, 5 However, some of these previous reports had considerable limitations, including the lack of laboratory-confirmed COVID-19 diagnosis, suboptimal study designs, or the absence of case controls.
Here, we report the results of a prospective and controlled cohort study with a 4-week follow-up period in which we investigated potential skin findings in 102 hospitalized SARS-CoV-2–positive patients and 41 age- and sex-matched SARS-CoV-2–negative controls with acute, nonprimary infectious diseases of the skin. In the control group, the most common infections were viral respiratory infections (26.8%), bacterial pneumonia (24.4%), and urinary tract infections (14.6%).
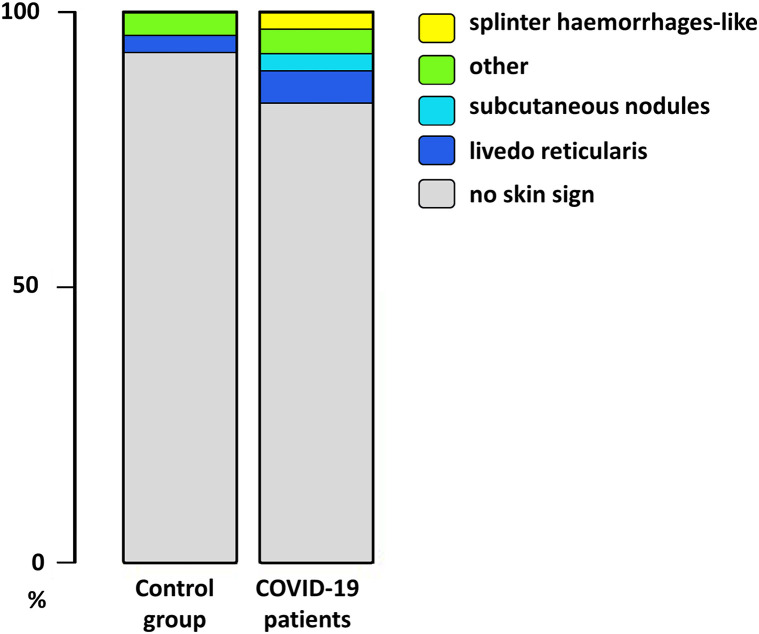
We observed newly occurring skin symptoms, concomitant with the infection in 17 (16.6%) COVID-19 patients. Three major groups of cutaneous manifestations were discerned: livedo reticularis (n = 6, 5.8%), splinter hemorrhage-like lesions (n = 4, 3.9%), and subcutaneous nodules (n = 2 ,2%) (Fig 1 ). Five patients had various other skin symptoms (rashes containing macules and papules, papular exanthema, burning sensation of the oral cavity, and vitiligo). In the control group, 5 patients (n = 5, 12.2%) had an onset of skin symptoms, including livedo reticularis in 1 patient. Four patients had other skin manifestations (petechial enanthem, nail hemorrhage, as well as rashes containing macules and papules). In each group, 1 rash containing macules and papules was considered as drug-induced, whereas no other apparent cause was found in the rest of the patients. Statistical analyses did not reveal significant differences between COVID-19 patients and control group in terms of the occurrence of skin symptoms (Fisher's exact test; P value = .6130) (Fig 1).
Fig 1.
An overview of cutaneous manifestations in COVID-19 patients and the control group. Skin symptoms were examined in patients who tested positive (n = 102) and negative for SARS-CoV-2 (n = 41). We grouped the skin symptoms into 4 groups: livedo reticularis, splinter hemorrhage-like lesions, subcutaneous nodules, and others. We compared the number of cases in the COVID-19 patients and control group using the Fisher's exact test.
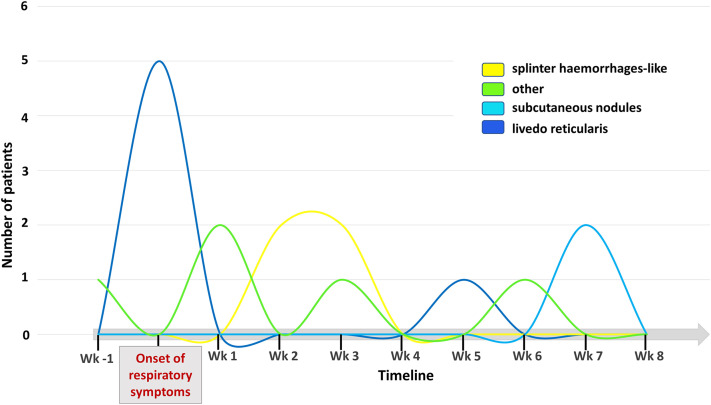
Livedo reticularis occurred within the first week and splinter hemorrhage-like lesions occurred within the third week after disease onset (Fig 2 ). Asymptomatic subcutaneous nodules without systemic symptoms occurred in 2 patients 7 weeks after the occurrence of respiratory symptoms (Fig 2). Both patients suffered from a severe course of the disease, including intensive care unit admission. Subcutaneous drug application as a possible cause was excluded. The histopathologic workup result was consistent with reactive septal panniculitis, and both patients were negative for SARS-CoV-2, as determined using a quantitative polymerase chain reaction test. Five months after study inclusion, the patients reported spontaneous partial regression of the nodules.
Fig 2.
Appearance of cutaneous manifestation over time. Timeline of newly manifested skin symptoms in COVID-19 patients depicted as the number of patients with the respective skin symptom over 8 weeks measured from the onset of respiratory symptoms.
The relatively small sample size must be considered as a limitation of our study. Therefore, we might have missed less frequent cutaneous manifestations and could not achieve statistical significance regarding the present skin findings.
Although we observed skin symptoms in 16.6% of the patients, including signs of vasculopathy during the early course of the disease and subcutaneous nodules as a possible late manifestation, no statistically significant difference was detected when the COVID-19 patients were compared with the control group of patients with other acute infectious diseases. Therefore, our study suggests that skin manifestations in COVID-19 patients are less specific compared with those previously assumed and cannot be considered as reliable diagnostic tools. Physicians confronted with skin lesions in patients with confirmed or suspected COVID-19 need to carefully evaluate possible differential diagnoses before attributing the symptoms to COVID-19. Larger and well-planned controlled studies are required to further elucidate skin manifestations in COVID-19 patients.
Conflicts of interest
None disclosed.
Footnotes
Drs Unterluggauer and Pospischil contributed equally to this article.
Funding source: This work was supported by funds of the Department of Dermatology, Medical University of Vienna, Austria, and the MED-CALL from the Faculty of Medicine, Johannes Kepler University Linz, Austria.
IRB approval status: Approved (#1392/2020).
References
- 1.Bouaziz J.D., Duong T., Jachiet M., et al. Vascular skin symptoms in COVID-19: a French observational study. J Eur Acad Dermatol Venereol. 2020;34(9):e451–e452. doi: 10.1111/jdv.16544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fernandez-Nieto D., Jimenez-Cauhe J., Suarez-Valle A., et al. Characterization of acute acral skin lesions in nonhospitalized patients: a case series of 132 patients during the COVID-19 outbreak. J Am Acad Dermatol. 2020;83(1):e61–e63. doi: 10.1016/j.jaad.2020.04.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freeman E.E., McMahon D.E., Lipoff J.B., et al. The spectrum of COVID-19-associated dermatologic manifestations: an international registry of 716 patients from 31 countries. J Am Acad Dermatol. 2020;83(4):P1118–P1129. doi: 10.1016/j.jaad.2020.06.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galvan Casas C., Catala A., Carretero Hernandez G., et al. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020;183(1):71–77. doi: 10.1111/bjd.19163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34(5):e212–e213. doi: 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]