Abstract
Background
In Latin America, the prevalence of end-stage kidney disease (ESKD) has risen tremendously during the last decade. Previous studies have suggested that receiving dialysis at high altitude confers mortality benefits; however, this effect has not been demonstrated at >2000 m above sea level (masl) or in developing countries.
Methods
This historical cohort study analyzed medical records from six Peruvian hemodialysis (HD) centers located at altitudes ranging from 44 to 3827 masl. Adult ESKD patients who started maintenance HD between 2000 and 2010 were included. Patients were classified into two strata based on the elevation above sea level of their city of residence: low altitude (<2000 masl) and high altitude (≥2000 masl). Death from any cause was collected from national registries and Cox proportional hazards models were built.
Results
A total of 720 patients were enrolled and 163 (22.6%) resided at high altitude. The low-altitude group was significantly younger, more likely to have diabetes or glomerulonephritis as the cause of ESKD and higher hemoglobin. The all-cause mortality rate was 84.3 per 1000 person-years. In the unadjusted Cox model, no mortality difference was found between the high- and low-altitude groups {hazard ratio [HR] 1.20 [95% confidence interval (CI) 0.89–1.62]}. After multivariable adjustment, receiving HD at high altitude was not significantly associated with higher mortality, but those with diabetes as the cause of ESKD had significantly higher mortality [HR 2.50 (95% CI 1.36–4.59)].
Conclusions
In Peru, patients receiving HD at high altitudes do not have mortality benefits.
Keywords: altitude, anemia, chronic hemodialysis, chronic hypoxia, mortality
INTRODUCTION
Chronic noncommunicable diseases, including chronic kidney disease (CKD), are the leading cause of death in developed countries and impose an enormous cost on countries of Latin America (LA) [1–3]. Data on the CKD burden in LA are scarce; however, some studies have found CKD prevalence to be as high as 8% in Mexico [4], 12% in Chile [5] and 16.8% in Peru [6]. Similarly, the prevalence of end-stage kidney disease (ESKD) patients under renal replacement therapies (RRTs) in LA has substantially increased from 119 patients per million people (pmp) in 1991 to 669 patients pmp in 2013 [7, 8].
In Peru, access to RRTs is not universal, mostly benefiting those with social security (EsSalud) and some with subsidized insurance from the Ministry of Health [6]. In 2010, EsSalud provided RRTs to 9814 patients and the Ministry of Health provided RRTs to 1983 patients in 2014 [9]. These numbers reflect the high prevalence of ESKD requiring RRT in this country, which is similar to developed regions worldwide. Furthermore, they suppose an increasing unmet need that affects a large number of Peruvians.
Peru has 30 million inhabitants and a third of its population lives at altitudes >2000 m. Prior studies have shown that patients who receive dialysis at an altitude >1828 m above sea level (masl) have 15% lower mortality risk in a 5-year follow-up compared with similar patients who receive dialysis at sea level [10]. However, this study was carried out in the USA, with 0.4% of their sample living at >1828 masl and where the highest hemodialysis (HD) center is located at 2299 masl [11]. Thus, little is known about mortality in patients with ESKD living at higher altitudes, especially >2000 masl, where arterial oxygenation saturation starts to decline [12]. Therefore this study was conducted to determine the effect of altitude on mortality in ESKD patients receiving HD in Peru.
MATERIALS AND METHODS
This historical cohort study included patients with ESKD from six HD centers located at different altitudes: Centro Nacional de Salud Renal, EsSalud-Lima, Hospital Nivel IV Victor Lazarte Echegaray, EsSalud-Trujillo (at sea level); Hospital Nivel II Huanuco, EsSalud-Huanuco (at 1894 masl); Hospital Nivel IV Carlos Alberto Seguin Escobedo, EsSalud-Arequipa (at 2335 masl); Hospital Nivel IV Adolfo Guevara Velasco, EsSalud-Cusco (at 3400 masl) and Hospital Nivel III Puno, EsSalud-Puno (at 3827 masl).
All patients who initiated maintenance HD between 2000 and 2010 in these locations and who were >18 years of age were included. Patients who died within 90 days of HD initiation or those who previously received renal transplant or peritoneal dialysis were excluded. The study was approved by the ethics committees from Universidad Peruana Cayetano Heredia and EsSalud. All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethics committees at EsSalud and Cayetano Heredia and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was waived due to the retrospective nature of the study.
Using a standardized form, medical records were reviewed to gather the following information: age, sex, cause of ESKD, date of the first HD session and date of the last follow-up. Death from any cause was the outcome of interest and it was collected from national registries.
Patients were classified into two strata based on the elevation above sea level of their city of residence: low altitude (<2000 masl) and high altitude (≥2000 masl). A sensitivity analysis using a lower altitude cutoff (1828 masl) was performed. Medians and frequencies of patient characteristics were calculated by elevation group. Pearson chi-squared and Wilcoxon rank-sum tests were used for univariate analyses of baseline characteristics. Cox proportional hazards models assessed the time from first HD to death from any cause, stratifying for each year and following patients for up to 5 years after first dialysis. Observations were censored by the end of the data collection (January 1, 2012) and censure criteria were applied as following: loss to follow-up, survival after 5 years of first HD, transference to another HD center outside the city, renal transplantation or migration to peritoneal dialysis during follow-up. Patients living at low altitude served as a reference category for all analyses.
Cox proportional hazards models were employed to look at the unadjusted and adjusted associations with mortality; the latter included altitude, age, sex and cause of ESKD as well as interactions of cause of ESKD with altitude. A subgroup analysis looked at the association between hemoglobin and mortality. P-values <0.05 were considered statistically significant. All analyses were carried out using SAS/STAT software, version 9.4 (SAS Institute, Cary, NC, USA) on a Windows 7 platform.
RESULTS
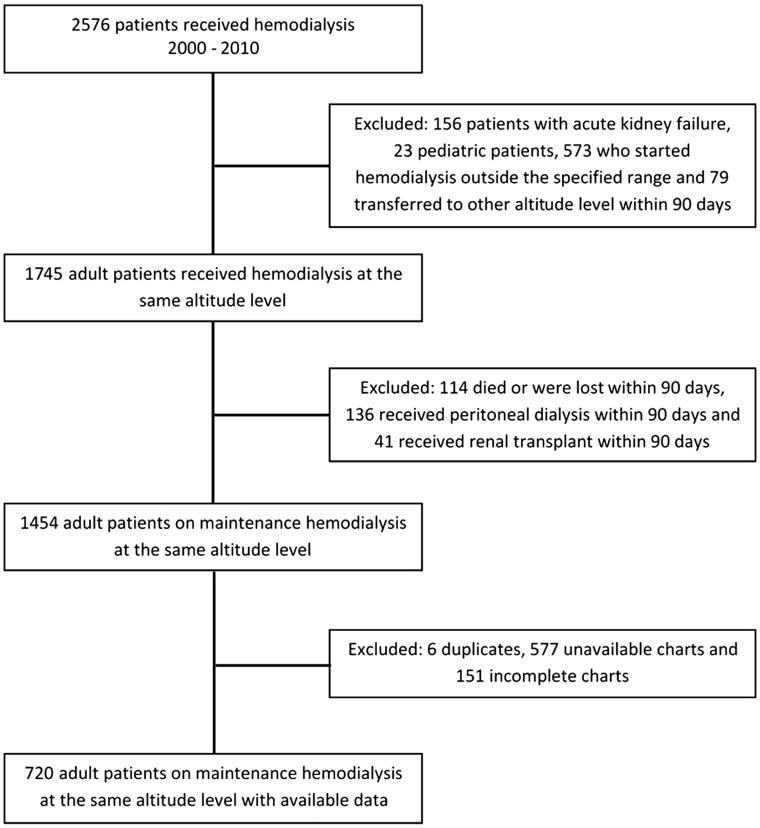
Of 2576 patients who started HD between 2000 and 2010 at the six HD centers, 720 (39.6%) met inclusion criteria (Figure 1). In Trujillo, Lima and Huanuco, 77.4, 81.8 and 84.5% of incident HD patients were enrolled, respectively; whereas in Puno, Cusco and Arequipa, these proportions fell to 34.7, 33.3 and 4.8%, respectively (Figure 2). A total of 557 (77.4%) patients were in the low-altitude group (72 from Trujillo, 436 from Lima and 49 from Huanuco) and 163 (22.6%) were in the high-altitude group (37 from Arequipa, 116 from Cusco and 10 from Puno). Baseline characteristics are shown in Table 1, stratified by elevation group. Patients in the low-altitude group were significantly younger, more likely to have diabetes or glomerulonephritis as the cause of ESKD and had higher hemoglobin.
FIGURE 1.
Patient inclusion flowchart.
FIGURE 2.
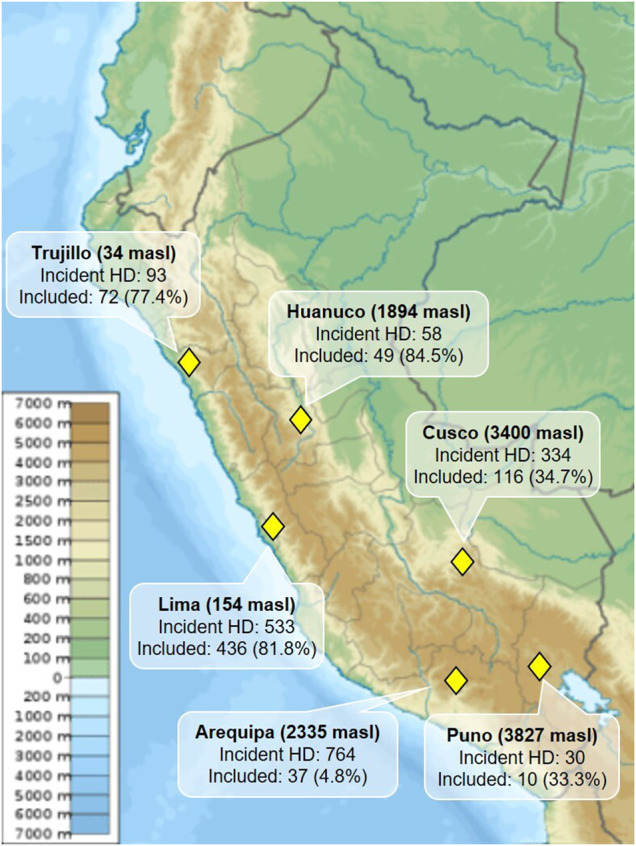
Map of Peru displaying the location and name of the participating cities according to altitude level as well as the number of incident HD patients and number of patients included in our study. Map source: Wikimedia Commons.
Table 1.
Baseline characteristics by elevation group
| Variable | Low altitude (n = 557) | High altitude (n = 163) | P-value |
|---|---|---|---|
| Age (years), median (range)a | 51.8 (18.1–94.4) | 56.8 (18.2–98.3) | <0.001 |
| Sex, n (%)b,c | |||
| Men | 297 (61.2) | 104 (63.8) | 0.559 |
| Women | 188 (38.8) | 59 (36.2) | |
| Cause of ESKD, n (%)b | |||
| Hypertension | 172 (30.9) | 52 (31.9) | <0.001 |
| Diabetes | 119 (21.4) | 24 (14.7) | |
| Glomerulonephritis | 86 (15.4) | 12 (7.4) | |
| Other | 88 (15.8) | 21 (12.9) | |
| Undetermined | 13 (2.3) | 10 (6.1) | |
| Mixed | 2 (0.4) | 12 (7.4) | |
| Not filed | 77 (13.8) | 32 (19.6) | |
| Hemoglobin (g/dL), median (range)a,d | 9.0 (4.0–16.4) | 8.3 (3.6–18.7) | 0.009 |
| Follow-up (years), median (range) | 3.9 (0.3–5.0) | 2.4 (0.2–5.0) | < 0.001 |
Wilcoxon rank-sum test.
Chi-squared test.
Information available in 648 records.
Baseline hemoglobin was determined in 54% of the patients: 309 patients in the low-altitude group and 86 patients in the high-altitude group.
Over a median follow-up of 3.6 years, there were 260 (36.1%) deaths (overall mortality rate 84.3 per 1000 person-years). In the low-altitude group, 207 (37.2%) patients died, while in the high-altitude group, 53 (32.5%) died. In an unadjusted Cox proportional hazards model, the high-altitude group had a trend toward higher mortality, although it was not statistically significant {hazard ratio [HR] 1.20 [95% confidence interval (CI) 0.89–1.62], P = 0.243} (Figure 3). In the sensitivity analysis using a lower altitude cutoff of 1828 masl, the high-altitude group had significantly higher mortality [HR 1.42 (95% CI 1.07–1.90), P = 0.016] (Supplementary data). In the univariate subgroup analysis, increased hemoglobin was not significantly associated with lower mortality [HR 0.95 (95% CI 0.87–1.04), P = 0.274].
FIGURE 3.
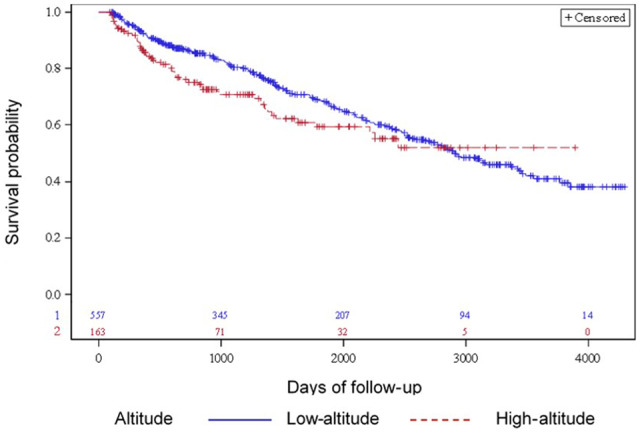
Survival plot displays the estimated survival time for patients at low and high altitude, with the number of subjects at risk at 0, 1000, 2000, 3000 and 4000 days. Patients at high altitude have a nonsignificant trend toward lower survival in unadjusted analysis.
An adjusted Cox model (Table 2) with altitude, age, sex and cause of ESKD was fit and demonstrated that the high-altitude group had higher mortality, but this association did not reach statistical significance [HR 1.16 (95% CI 0.85–1.58), P = 0.360]. Similarly, women had a nonsignificant trend toward higher mortality [HR 1.30 (95% CI 1.00–1.69), P = 0.050]. Additionally, for each year of increase in age, the hazard of death increased by 4% [HR 1.04 (95% CI 1.03–1.05), P < 0.001] over both altitudes. A second adjusted Cox model (Table 3) with altitude, age, sex and interaction of cause of ESKD and altitude level was fit and showed that patients with diabetes as the cause of ESKD in the high-altitude group experience significantly higher mortality [HR 2.50 (95% CI 1.36–4.59), P = 0.003]. There is also a suggestion that this is true for hypertension as cause of ESKD.
Table 2.
Adjusted mortality HRs in Peruvian patients receiving HD
| Variable | HR (95% CI) | P-value |
|---|---|---|
| High versus low altitude | 1.16 (0.85–1.58) | 0.360 |
| Age (1-year increase) | 1.04 (1.03–1.05) | <0.001 |
| Sex (women versus men) | 1.30 (1.00–1.69) | 0.050 |
| Cause of ESKD | 1.01 (0.98–1.10) | 0.693 |
| Diabetes versus othera | 1.20 (0.86–1.69) | 0.290 |
| Hypertension versus otherb | 1.23 (0.91–1.66) | 0.186 |
When compared with causes of ESKD other than hypertension.
When compared with causes of ESKD other than diabetes.
Table 3.
Adjusted mortality HRs, with altitude by cause of ESKD interaction, in Peruvian patients receiving HD
| Variable | HR (95% CI) | P-value |
|---|---|---|
| Age (1-year increase) | 1.04 (1.03–1.05) | <0.001 |
| Sex (women versus men) | 1.26 (0.96–1.63) | 0.091 |
| Interaction of altitude and sex | 0.83 (0.44–1.58) | 0.571 |
| Interaction of altitude and cause of ESKD | 0.014 | |
| High versus low altitude for diabetes | 2.50 (1.36–4.59) | 0.003 |
| High versus low altitude for hypertension | 1.15 (0.71–1.89) | 0.567 |
DISCUSSION
This is the first study, to our knowledge, that has examined the association between altitude and mortality in patients receiving HD in the Andes. This is important not only due to the altitude levels seen in these cities, but also because this is an ethnic group that is very different from others living at high altitude. In fact, Andeans have lived at high altitude for >11 000 years, developing circulatory, respiratory and hematological adaptations; however, when compared with Tibetan populations, the former have higher hemoglobin concentrations, lower resting ventilation, higher oxygen saturation and an absence of genetic adaptation [13, 14].
Our sample was composed of middle-aged subjects, a population relatively younger than that of other studies involving maintenance HD [10]. Interestingly, those who started HD at high altitude were significantly older than their low-altitude counterparts. This is in agreement with prior evidence showing that slower CKD progression may be present at high altitude [15, 16]. However, other factors such as lower survival in older patients living at low altitude due to significant comorbidities or increased availability of healthcare resources with planned HD initiation in these settings need to be considered.
Substantial mortality rates were found across both altitude groups and a nonsignificant trend toward higher mortality was observed in those living at high altitude in the adjusted analysis. Our results differ from prior findings [10, 17, 18] that showed up to 18% mortality reduction in dialysis patients receiving HD at increased altitudes. Notably, these studies were conducted mainly in Caucasian populations at altitudes not significantly >2000 masl. Our results could potentially be explained by a myriad of factors, including not only the magnitude of altitude level, but also genetic and adaptation variances from our specific patient population, comorbid conditions, healthcare-associated factors and social disparities. Erythropoietin use may also differ in different Peruvian centers, as noted by lower hemoglobin levels in the high-altitude group, which may make them prone to the deleterious effects of anemia in an already hypoxic environment.
Additionally, our study raises concern for a potential sex disparity in Peruvian patients receiving HD across altitude levels, since women had a nonsignificant increase in the hazard of death of 30%. A similar observation has been documented in Caucasian and Asian populations receiving HD and potential reasons include longer waiting times to HD initiation, greater loss of residual renal function, lower urea clearance adjusted for urea volume (Kt/Vurea) and shorter HD sessions [19].
Moreover, we found higher mortality among those subjects with diabetes receiving HD at high altitude. Regarding the previously described independent association between higher altitude, worsening hypoxemia and increased cardiometabolic risk factors [20], it is possible that this higher mortality may be strongly influenced by cardiovascular disease. Future studies are needed to explore this association, accounting for potential confounders.
Our study was performed in patients who had social security to ensure access to healthcare and guideline uniformity. However, we could not account for specific differences in the way healthcare is delivered in each center, their staffing needs or medication availability. Furthermore, Andeans’ lifestyle and stress levels may be different than their coastal peers, impacting mortality outcomes. Indirect data that support the existence of regional differences include the gross domestic product per capita [in Lima, Arequipa and Trujillo (US$1631–3073) is higher than in Cusco, Puno and Huanuco (US$681–1228)] [21], life expectancy [in Lima, Arequipa and Trujillo (74.1–78.4 years) is higher than in Huanuco, Puno and Cusco (64.3–68.5 years)] [22], human development index (higher in Lima and Arequipa; intermediate in Trujillo; and lower in Huanuco, Cusco and Puno) [23], number of university hospitals offering nephrology training (nine in Lima, two in Arequipa, one in Cusco and none in Trujillo, Huanuco or Puno) [24] and the proportion of Quechua ethnicity [higher in Cusco, Puno and Huanuco (43.1–74.7%) than in Arequipa, Lima and Trujillo (2.9–31.3%)] [25].
This study has several limitations. Our high-altitude group size was comparatively small and clustering of altitude levels was performed. The percentage of incident HD patients that were enrolled in Arequipa was <10%, mostly due to missing charts (71%), while in Cusco this proportion was <35% due to the high incidence of acute kidney injury (26%). The differences observed in our results could be due to uncontrolled patient characteristics or environmental factors correlated with altitude rather than an independent effect of altitude. Moreover, comorbid conditions, medication use (including erythropoietin analogs), nutritional status, dialysis efficiency (Kt/V) and residual renal function were variably reported in paper charts and many times missing, therefore mortality could not be adjusted for them in the Cox proportional models.
In conclusion, Peruvian patients receiving HD at high altitudes do not have mortality benefits.
SUPPLEMENTARY DATA
Supplementary data are available at ckj online.
Supplementary Material
ACKNOWLEDGEMENTS
Special thanks to the International Society of Nephrology, who supported this research through the Global Outreach and Prevention Program. We also recognize the support from the following nephrologists: Myriam Fiestas, José Taypicahuana, José Figueroa, Raúl Hinojosa, Jhony Paredes Silva and Nancy García.
FUNDING
This study was supported by a grant from International Society of Nephrology, Global Outreach Research and Prevention Program.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest. The results presented in this article have not been published previously in whole or part, except in abstract format.
REFERENCES
- 1. Barreto SM, Miranda JJ, Figueroa JP. et al. Epidemiology in Latin America and the Caribbean: current situation and challenges. Int J Epidemiol 2012; 41: 557–571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mathers CD, Boerma T, Ma Fat D.. Global and regional causes of death. Br Med Bull 2009; 92: 7–32 [DOI] [PubMed] [Google Scholar]
- 3. Cusumano AM, Gonzalez Bedat MC.. Chronic kidney disease in Latin America: time to improve screening and detection. Clin J Am Soc Nephrol 2008; 3: 594–600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Amato D, Alvarez-Aguilar C, Castaneda-Limones R. et al. Prevalence of chronic kidney disease in an urban Mexican population. Kidney Int Suppl 2005; 68: S11–S17 [DOI] [PubMed] [Google Scholar]
- 5. Zuniga SMC, Muller OH, Flores OM. [ Prevalence of chronic kidney disease in subjects consulting in urban primary care clinics]. Rev Med Chil 2011; 139: 1176–1184 [PubMed] [Google Scholar]
- 6. Francis ER, Kuo CC, Bernabe-Ortiz A. et al. Burden of chronic kidney disease in resource-limited settings from Peru: a population-based study. BMC Nephrol 2015; 16: 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rosa-Diez G, Gonzalez-Bedat M, Pecoits-Filho R. et al. Renal replacement therapy in Latin American end-stage renal disease. Clin Kidney J 2014; 7: 431–436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cusumano AM, Rosa-Diez GJ, Gonzalez-Bedat MC.. Latin American dialysis and transplant registry: experience and contributions to end-stage renal disease epidemiology. World J Nephrol 2016; 5: 389–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Herrera-Anazco P, Benites-Zapata VA, Huarcaya-Cotaquispe L-YI. et al. Chronic kidney disease in Peru: a challenge for a country with an emerging economy. J Bras Nefrol 2015; 37: 507–508 [DOI] [PubMed] [Google Scholar]
- 10. Winkelmayer WC, Liu J, Brookhart MA.. Altitude and all-cause mortality in incident dialysis patients. JAMA 2009; 301: 508–512 [DOI] [PubMed] [Google Scholar]
- 11.Centers for Medicare & Medicaid Services. Dialysis Facilities in the U.S. https://data.medicare.gov/Dialysis-Facility-Compare/Dialysis-Facilities-in-the-U-S-/kwkm-uxp2 (23 February 2020, date last accessed)
- 12. Rojas-Camayo J, Mejia CR, Callacondo D. et al. Reference values for oxygen saturation from sea level to the highest human habitation in the Andes in acclimatised persons. Thorax 2018; 73: 776–778 [DOI] [PubMed] [Google Scholar]
- 13. Bigham AW, Wilson MJ, Julian CG. et al. Andean and Tibetan patterns of adaptation to high altitude. Am J Hum Biol 2013; 25: 190–197 [DOI] [PubMed] [Google Scholar]
- 14. Beall CM. Two routes to functional adaptation: Tibetan and Andean high-altitude natives. Proc Natl Acad Sci USA 2007; 104: 8655–8660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Luks AM, Johnson RJ, Swenson ER.. Chronic kidney disease at high altitude. J Am Soc Nephrol 2008; 19: 2262–2271 [DOI] [PubMed] [Google Scholar]
- 16. Ghahramani N, Ahmed F, Al-Laham A. et al. The epidemiological association of altitude with chronic kidney disease: evidence of protective effect. Nephrology (Carlton) 2011; 16: 219–224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sibbel S, Maroni BJ, Brunelli SM.. The effect of altitude on erythropoiesis-stimulating agent dose, hemoglobin level, and mortality in hemodialysis patients. J Nephrol 2017; 30: 821–829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shapiro BB, Streja E, Rhee CM. et al. Revisiting the association between altitude and mortality in dialysis patients. Hemodial Int 2014; 18: 374–383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vongsanim S, Davenport A.. The effect of gender on survival for hemodialysis patients: Why don’t women live longer than men? Semin Dial 2019; 32: 438–443 [DOI] [PubMed] [Google Scholar]
- 20. Miele CH, Schwartz AR, Gilman RH. et al. Increased cardiometabolic risk and worsening hypoxemia at high altitude. High Alt Med Biol 2016; 17: 93–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Instituto Nacional de Estadística e Informática. Producto Bruto Interno por Departamentos. Lima, Peru: Instituto Nacional de Estadística e Informática, 2019
- 22.Instituto Nacional de Estadística e Informática. Proyecciones Departamentales de la Población 1995–2015. Evolución de la Esperanza de Vida al Nacer. Lima, Peru: Instituto Nacional de Estadística e Informática, 2015
- 23.Instituto Nacional de Estadística e Informática. Genero, Equidad y Disparidades. Desarrollo Humano y Genero en la Década de Los Noventa. Lima, Peru: Instituto Nacional de Estadística e Informática, 2000
- 24. Consejo Nacional de Residentado Médico Ley N 30453. http://www.conareme.org.pe/web/proceso-de-admision-2010.php (23 February 2020, date last accessed)
- 25.Instituto Nacional de Estadística e Informática. Censo Nacional 2017 XII de Población, VII de Vivienda y III de Comunidades Indígenas. Lima, Peru: Instituto Nacional de Estadística e Informática, 2018
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.