Abstract
Introduction
A physically active lifestyle during pregnancy improves maternal and offspring health but can be difficult to follow. In Denmark, less than 40% of pregnant women meet physical activity (PA) recommendations. The FitMum study aims to explore strategies to increase PA during pregnancy among women with low PA and assess the health effects of PA. This paper presents the FitMum protocol, which evaluates the effects of structured supervised exercise training or motivational counselling supported by health technology during pregnancy on PA level and health of mother and offspring.
Methods and analysis
A single-site three-arm randomised controlled trial that aims to recruit 220 healthy, pregnant women with gestational age (GA) no later than week 15 and whose PA level does not exceed one hour/week. Participants are randomised to one of three groups: structured supervised exercise training consisting of three weekly exercise sessions, motivational counselling supported by health technology or a control group receiving standard care. The interventions take place from randomisation until delivery. The primary outcome is min/week of moderate-to-vigorous intensity PA (MVPA) as determined by a commercial activity tracker, collected from randomisation until GA of 28 weeks and 0-6 days, and the secondary outcome is gestational weight gain (GWG). Additional outcomes are complementary measures of PA; clinical and psychological health parameters in participant, partner and offspring; analyses of blood, placenta and breastmilk samples; process evaluation of interventions; and personal understandings of PA.
Ethics and dissemination
The study is approved by the Danish National Committee on Health Research Ethics (# H-18011067) and the Danish Data Protection Agency (# P-2019-512). Findings will be disseminated via peer-reviewed publications, at conferences, and to health professionals via science theatre performances.
Trial registration number
Protocol version
This paper was written per the study protocol version 8 dated 28 August 2019.
Keywords: obstetrics, sports medicine, public health, clinical physiology
Strengths and limitations of this study.
The efficacy of structured supervised exercise training and motivational counselling supported by health technology to improve physical activity and reduce weight gain of pregnant women is directly compared in a randomised controlled trial.
The trial involves complex interventions and is held in one site only, so generalisability and fidelity might be a concern. Yet, as one of the additional outcomes, a process evaluation is conducted alongside the trial to explore how the interventions are carried out and adapted.
The study is comprehensive and multidisciplinary in its design. Many different methodologies are used, and mother, partner and offspring are studied.
Activity trackers can increase physical activity level and are feasible tools in everyday life, but commercial activity trackers have limited validity for the quantification of physical activity.
Physical activity is extensively measured using three different methods: commercial activity trackers, gold standard doubly labelled water and the validated Pregnancy Physical Activity Questionnaire.
Introduction
Although the health effects of PA are widely acknowledged, the means of how to best implement and maintain PA in everyday life are lacking.1 Pregnancy can be regarded as a window of opportunity to implement good habits of PA as pregnant women are in regular contact with health professionals and are likely motivated to adopt healthy behaviours, as illustrated by reduced alcohol consumption and smoking cessation.2–4 However, pregnancy can be seen as an opportunity to be exempt from fitness demands and bodily ideals and can be experienced as a troublesome time due to fatigue and discomfort.5 6 Moreover, pregnancy is a relatively short period of time in regards to forming new habits6 and that may affect the motivations and challenges in being physically active. Furthermore, differences in work status, social relations and family situations, as well as varying material and structural conditions, may contribute to the implementation of PA.7
Insufficient PA is a global problem8 that occurs also during pregnancy.8–12 It is a significant public health issue, as increasing evidence suggests that lifestyle during pregnancy influences health in the mother and her offspring.4 13 Regular PA during pregnancy promotes clinical and metabolic health in both mother and offspring and reduces the number of complications during pregnancy and delivery.14–19 PA reduces GWG,20–26 the risk of gestational diabetes mellitus,27–32 the intensity of low back pain33 and the risk of caesarean delivery22 29 34–37 and improves maternal body composition.38 Additionally, a physically active pregnancy improves the health of the offspring by normalising birth weight,22 reducing the risk of preterm delivery39 40 and improving neonatal body composition41 42 as well as placental function,43 44 which results in optimised intrauterine growth conditions.
The Danish Health Authorities recommend that healthy pregnant women are physically active for at least 30 min/day at moderate intensity,45 but only 38% of Danish pregnant women achieve this recommended level.46 Several barriers to PA during pregnancy are addressed in the literature,47 including anxiety about overdoing exercise, low motivation to adopt an active lifestyle during pregnancy, changing energy levels throughout the pregnancy and lack of time to be physically active.48 The latest recommendations on lifestyle interventions during pregnancy support individualised advice on how to increase the PA level rather than a generic approach,6 as pregnant women prefer personalised information.49 Consequently, policymakers, healthcare professionals and pregnant women advocate for evidence-based guidance on how to implement PA in everyday life during pregnancy safely and effectively, with approaches that meet the needs, preferences and choices of the pregnant woman.
During the past decades, many PA intervention studies in pregnant women have been conducted on overweight and obese populations23 24 26 28 50–57 as well as in healthy normal-weight pregnant women.20 21 32 33 58–61 Still, none of these studies have focused primarily on investigating the effect of the exercise interventions on actual PA level in pregnant women nor have they used novel objective methods to measure actual PA levels. Structured, supervised exercise training and motivational counselling have been applied separately in pregnant women,20 21 23 24 26 28 32 33 50–55 58–63 but the relative efficacy of these interventions has not been compared; this hampers the evidence-based implementation of effective exercise programmes into everyday life.
Objective
This paper describes the protocol of the FitMum study, which is a randomised controlled trial (RCT). The FitMum RCT aims to evaluate the effects of structured supervised exercise training (EXE) and motivational counselling supported by health technology (MOT) compared with standard care (CON) on PA level and GWG during pregnancy. Additional aims of the study are to investigate the effects of EXE and MOT on clinical and metabolic health parameters in both mother and offspring. We will also explore how the FitMum exercise programmes are carried out and adopted by conducting a process evaluation. In addition, we explore the personal attribution of meaning to the experiences and practices of PA among participants. Furthermore, we investigate how social, structural and cultural factors facilitate or hinder the successful implementation of exercise during pregnancy.
Methods
Study design
The FitMum RCT is a single-site, three-arm randomised controlled trial study.
Setting
The study is carried out at the Department of Gynaecology and Obstetrics, Nordsjaellands Hospital (NOH), Hillerod, in the Capital region of Denmark, where approximately 4000 women give birth per year. NOH is a public hospital, and participation in FitMum is free of charge.
Participants
This study aims to include 220 healthy, pregnant women. Inclusion criteria are obtained written informed consent, maternal age of 18 years or older, gestational age (GA) of maximum 15 weeks, ultrasonic-confirmed viable intrauterine pregnancy, body mass index of 18.5–45 kg/m2 and body weight <150 kg (prepregnancy weight or first measured weight in pregnancy), ability to wear a wrist-worn activity tracker 24/7 until one year postpartum and having a smartphone. Exclusion criteria are structured exercise at moderate-to-vigorous intensity for more than one hour/week during early pregnancy, previous preterm delivery, obstetric or medical complications, multiple pregnancies, inability to speak Danish, or alcohol or drug abuse.
Recruitment and inclusion
Participants are recruited: (1) via booking confirmation of a first-trimester scan, (2) at face-to-face meetings during the first-trimester scan and (3) through posters, flyers and social media. Before inclusion, interested women answer an online, one-page prescreening questionnaire. Eligible participants and their partners are invited to the first visit at NOH as soon as possible and no later than GA of 14 weeks and 6 days. At visit 1, the woman is verbally informed about the study and screened according to inclusion and exclusion criteria. Women who have not had a first-trimester scan are vaginally scanned to confirm a singleton, viable intrauterine pregnancy. All eligible women are included, and written informed consent is obtained (online supplemental file 1). Written informed consent is also obtained from the partner as biological samples are collected from the offspring and from the partner (online supplemental file 2). After inclusion, we obtain anthropometric and demographic information, a blood sample as well as a short semistructured interview with the participant. The interview provides knowledge of the participant’s thoughts on participating in a research project, knowledge of prior and current PA level, and experiences with health technologies.
bmjopen-2020-043671supp001.pdf (84.9KB, pdf)
bmjopen-2020-043671supp002.pdf (83.8KB, pdf)
At the end of visit 1, the participant receives a commercial activity tracker, Garmin Vivosport. The participant is instructed to wear the tracker continuously 24/7 from the one week baseline period until one year postpartum, except during charging. The activity tracker is water resistant and determines the frequency, duration and intensity of activity periods on a minute-to-minute basis. The data from the activity tracker are wirelessly synced to the associated app, Garmin Connect, provided by Garmin International, and the research platform Fitabase (Small Steps Labs LLC), through which the compliance of wearing and synchronising the data from the tracker are continuously monitored during the study.
Baseline period and randomisation
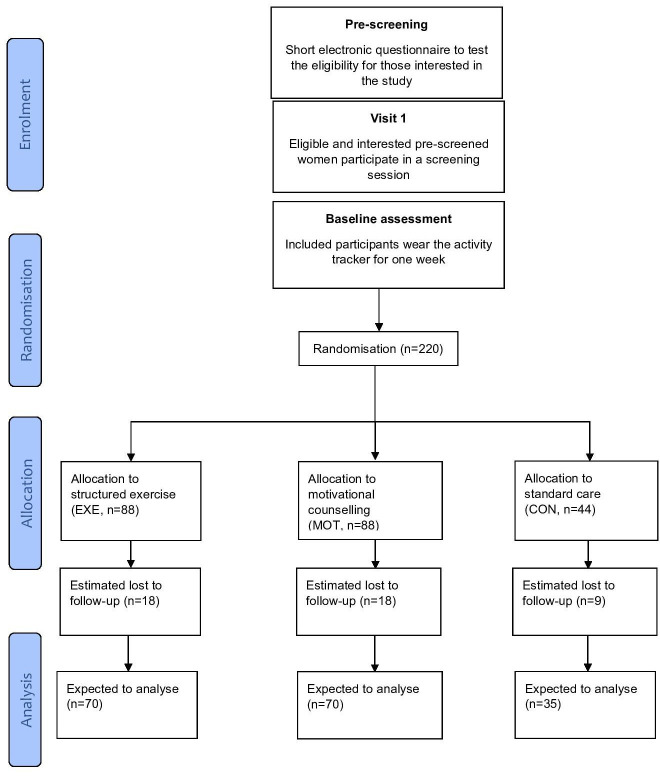
After inclusion, the baseline PA level of the participant is measured by the activity tracker for one week. After the baseline period, participants are randomised into the EXE, MOT and CON groups (figure 1). The target number of participants randomised to each group is 88, 88 and 44, respectively, in order to have more participants in the intervention groups. Randomisation is performed via a numbered randomisation list administered through the database Research Electronic Data Capture (REDCap), and the investigators are blinded to the procedure. Blinding of participants is considered impossible due to the inherent content of the exercise interventions. The participant is informed about the assigned group by email, and participants in EXE and MOT receive written information containing guidelines from the Danish Health Authorities about PA during pregnancy.
Figure 1.
Flow diagram of the FitMum RCT.
Patient and public involvement
Template for Intervention Description and Replication64 was used as inspiration for the development and description of the study. As a part of the development phase, stakeholders in the field were involved in discussions and sharing of knowledge. Additionally, 27 semistructured interviews with Danish pregnant women, midwives and obstetricians were performed to explore the feasibility of such a study as well as the motivational factors and barriers to PA during pregnancy. Participants are not directly involved in the recruitment and conduct of the study, but a process evaluation is conducted, and personal understandings of the participants are obtained via interviews (see further). The insights from the study will be shared with the participants at an information meeting after the end of the study.
Interventions
Standard care at the hospital
All three groups are offered the standard care that applies to women giving birth at NOH. This consists of three appointments with their general practitioner (GA weeks 6–10, 25 and 32), five to six midwife consultations (GA weeks 14–17, 29, 36, 38, 40 and if still pregnant around week 41 as well) and ultrasonic scans at GA weeks 12 and 20.
Standard care control group (CON)
Participants in CON wear an activity tracker to determine their activity level. The face of the tracker looks like a normal watch showing only time and battery life.
Structured supervised exercise training intervention (EXE)
The targeted PA level for all participants in EXE and MOT is at least 30 min/day at a moderate intensity as recommended to healthy pregnant women,6 and all participants are informed hereof if randomised to EXE or MOT. In EXE, exercise training takes place in teams and is supervised by health professionals (exercise physiologists, physiotherapists and public health scientists). It consists of three weekly 1-hour exercise sessions at moderate intensity, including two exercise sessions in a gym and one in a public swimming pool. The gym sessions consist of a combination of aerobic and resistance training with 30 min stationary bike training (a combination of hill climbing and high cadence intervals) and 30 min of other exercise, for example, elastic bands, exercise balls, mats, dumbbells or body weight. In the swimming pool, participants do 15 min of swimming and 45 min of water exercises with plates, balls, dumbbells or body weight. Moderate intensity during training sessions is assessed using both heart rate monitoring of 65%–80% of age-predicted maximal heart rate (from the activity tracker) and perceived exertion in the range of 12–14 on Borg’s conventional 6–20 point scale,64 as recommended by the American College of Obstetricians and Gynaecologists.14 If a participant experiences any pain or needs to decrease intensity, the content of exercise sessions (repetitions and/or resistance) is individually adjusted accordingly. Special attention is paid to the newly recruited participants. Exercise sessions are offered at seven different times per week, and participants are recommended to sign up for three of these sessions. The sessions are held early mornings or late afternoons all weekdays and before noon on Fridays and Saturdays.
Motivational counselling supported by health technology (MOT)
This intervention is composed of four individual and three group counselling sessions as well as weekly SMS reminders. The overall focus of both the individual and group counselling sessions is based on what already motivates the participants to increase or maintain their PA level. The motivation technique applied is inspired by motivational interviewing,65 self-determination theory66 and behaviour change techniques.67
All four individual sessions last one hour and are led by professional health counsellors (exercise physiologists, physiotherapists and public health scientists). The sessions aim to discuss the participant’s barriers, wishes, needs, knowledge and former PA experiences to identify individual characteristics and motivation towards a more physically active lifestyle. Aside from measuring the PA level, the activity trackers are also used as an intervention element to motivate the participants to increase their PA levels.68 During individual sessions, feedback on recent PA performances is provided based on activity data acquired from the activity tracker, in order to give the participants insight into their PA level. The participants will, with guidance from the counsellor, set their own activity goals and make an individual action plan to increase the PA level, which may have a motivating effect on PA behaviour.68 69 Individual sessions are scheduled during the daytime as conveniently for the participant as possible.
The first group session lasts one hour and aims to inform the participants about guidelines for PA, benefits associated with PA during pregnancy and possible ways to increase PA during pregnancy. In the following two 2-hour group sessions, the interaction between the participants is used to create meaningful group processes such as support, experience exchange, reflection, learning and development. These sessions focus on the discussion of relevant topics concerning PA during pregnancy, and the counsellor acts as a facilitator through the session, with the topics of conversation chosen by the participants. Issues like postpartum PA, the pelvic floor, uterine contractions, abdominal muscles and diastasis recti, and myths about pregnancy PA are discussed. Group sessions are held late afternoons or before noon for those on maternity leave.
The weekly SMS reminders have supportive and motivating content and are used to encourage the participants to achieve a moderate PA level. The texts are chosen based on every participant’s PA level during the last week measured by the activity tracker. One example of the text: ‘You have been exercising regularly for an extended period of time. Well done. Good habits make it easier for you to continue as your belly gets bigger and heavier’.
Outcome measures
The data collection procedures are illustrated in table 1.
Table 1.
Procedures and measurements in FitMum RCT
| Visit number | Visit 1 | Email randomisation | Visit 2 | Visit 3 | Visit 4 | Visit 5 | One year after delivery |
| Gestational age (week+days) | Screening and baseline testing max. 15+0 | One week after inclusion | Week 28+0–6 | Week 34+0–6 | Delivery | 7–14 days after delivery | |
| Approximately week 40 | |||||||
| Ultrasound scan | × | ||||||
| Oral information about the study | × | ||||||
| Medical interview to assess inclusion and exclusion criteria | × | ||||||
| Demographic, anthropometric, sickness absence and pelvic/low back pain data | × | × | × | × | |||
| Medical history, concomitant disease and previous medication | × | ||||||
| Demographic and anthropometric data of the participant’s partner | × | ||||||
| Written informed consent | × | ||||||
| Activity tracker and associated oral and written information | × | ||||||
| Randomisation | × | ||||||
| Methodology for obtaining outcomes | |||||||
| Activity tracker | Continuously during the trial and one year after delivery | ||||||
| Maternal body weight | × | × | × | × | × | Six times at home during the first year postpartum | |
| Doubly labelled water | × | ||||||
| Questionnaires: PPAQ-DK, SF-36, PSQI, P-ESES, BREQ-2 | × | × | × | × | |||
| Maternal blood samples | × | × | × | × | |||
| Paternal blood sample | × | ||||||
| Umbilical cord blood sample | × | ||||||
| Placenta samples | × | ||||||
| DXA scan | × | ||||||
| Breastmilk sample | × | ||||||
| Qualitative interview | × | × | × | ||||
| Observation and autodocumentation | Recurring | ||||||
| ASQ-3 | × | ||||||
| Growth assessment at general practitioner | Five weeks, and five and 12 months | ||||||
| Parental mental well-being questionnaire | Six to eight weeks postpartum | ||||||
| 7-day child accelerometer | × | ||||||
| Safety | |||||||
| Record adverse events | × | × | |||||
| Symphysis-fundal height | × | × | |||||
ASQ-3, Ages and Stages Questionnaire 3; BREQ-2, Behavioural Regulations Exercise Questionnaire; DXA, dual-energy X-ray absorptiometry; PA, physical activity; P-ESES, Pregnancy Exercise Self-efficacy Scale; PPAQ-DK, Pregnancy Physical Activity Questionnaire (Danish version); PSQI, Pittsburgh Sleep Quality Index; SF-36, The Medical Outcomes Study Short Form 36.
Primary outcome: moderate-to-vigorous intensity physical activity
The primary outcome of FitMum RCT is min/week of MVPA measured continuously from randomisation to GA of 28 weeks and 0-6 days as determined by a wrist-worn activity tracker, Garmin Vivosport, with a built-in heart rate monitor and accelerometer.
Secondary outcome: gestational weight gain
Body weight of the participant before pregnancy is self-reported. The body weight during pregnancy is measured four times from inclusion until delivery on the same scale (Seca 799) with the participant in light clothes and without shoes.
Additional outcomes
Complementary measures of physical activity
Complementary measures of PA are obtained by the Danish version of ‘Pregnancy Physical Activity Questionnaire’ (PPAQ)70 named PPAQ-DK and by the doubly labelled water technique.71
PPAQ is a semiquantitative and subjective instrument, which has been validated70 and is considered one of the most valid and reliable questionnaires for the assessment of PA level in pregnant women.72 Our research group has translated PPAQ to Danish and validated it in a Danish pregnant population.73
The doubly labelled water technique is the ‘gold standard’ technique to measure free-living energy expenditure objectively and is safe, even for pregnant women, as it relies on stable, non-radioactive isotopes.74–77 The participants are administered a glass of water for oral intake containing 0.1 g of 99.8% 2H2O and 1.6 g of 10% 18O per kg body weight. In total, five postdose urine samples are collected in the morning (not the first urine void of the day); on the day after oral water dosage; and after four, seven, 11 and 14 days. The urine samples are stored in the participant’s freezer and later at −80°C.
In addition, the PA of the participants is determined from GA week 29 until delivery and in the first year postpartum by the activity tracker. The measures of PA include active calories, active time, steps, heart rate, moderate-intensity and vigorous-intensity activity, floors climbed, MET-min/week and type of activity, which is recognised automatically by the tracker.
Clinical and psychological health parameters in participant, partner and offspring
A variety of clinical and psychological health parameters are obtained from the participant, her partner and her offspring. Clinical data regarding pregnancy, delivery and neonatal outcomes are collected from medical records. Health-related quality of life is determined in the participant by the Danish version of the Medical Outcomes Study Short Form 36,78 79 which has also been validated in pregnant women.80 Exercise self-efficacy is determined by the Danish version of the Pregnancy Exercise Self-Efficacy Scale (P-ESES).81 P-ESES has been translated into Danish and validated in a Danish pregnant population by our research group.82 PA motivation is determined by the Danish version of the Behavioural Regulation in Exercise Questionnaire (BREQ-2),83–85 which is the most widely used measure of the continuum of behavioural regulation in exercise psychology research. Sleep quantity and quality are assessed in the participant by the activity tracker and by the Danish version of the self-administered questionnaire Pittsburgh Sleep Quality Index (PSQI).86 87 The PSQI is considered a valid and reliable tool to assess sleep metrics among pregnant women.88 In addition, a validation of activity trackers to measure sleep will be conducted using polysomnography in a subgroup of women already participating in the FitMum study. Sick leave and pelvic and low back pain are registered by asking the participant whether she has been absent from work/study and on sick leave during her pregnancy and whether she has experienced pelvic and/or low back pain before and during her pregnancy. Maternal body composition is determined from total body water measured by doubly labelled water technique and by a postpartum dual-energy X-ray absorptiometry (DXA) scan. Offspring growth: head circumference, length and weight is measured at birth and by general practitioners at five weeks, five months and 12 months postpartum. Participants receive an electronic questionnaire and fill out the anthropometric data along with information on offspring dietary habits and vaccine status. Parental mental well-being is assessed six to eight weeks after birth. Both parents or holders of custody receive a questionnaire consisting of the Edinburgh Postnatal Depression Score and Gotland Depression Scale, which are combined as a screening tool for postnatal depression89–92 in Danish postnatal care. Psychomotor development of the offspring is assessed by the validated Ages and Stages Questionnaire 3 (ASQ-3), which is administered electronically to participants 12 months after the due date. ASQ-3 pinpoints developmental progress in the fields of communication, gross motor, fine motor, problem solving and personal-social skills. The administration of ASQ-3 relative to due date and not to birth date aims to correct for variance in cognitive and motor skills due to premature birth. Offspring physical activity is assessed for seven days by an infant activity tracker (Actigraph GT3X+) 12 months after the due date. The tracker detects level, intensity and pattern of physical activity.
Analyses of blood, placenta and breastmilk samples
Plasma metabolites and hormones are assessed in maternal and paternal venous blood. The blood samples will be analysed for concentrations of glucose, cholesterol (total, high and low density), triglyceride, free fatty acids, amino acids, interleukin-6, and C reactive protein. Venous blood is obtained from the umbilical cord within 30 min after delivery of the placenta. The blood will be analysed for concentrations of glucose, cholesterol (total, high and low density), triglyceride, insulin, c-peptide, free fatty acids, amino acids, adiponectin and leptin. Furthermore, epigenetic profiling at the level of DNA methylation will be performed in maternal, paternal and umbilical cord blood mononuclear cells. Bioinformatic comparison of DNA methylomes from parents and offspring will infer on the DNA methylation marks that are modulated by maternal exercise and transmitted to the offspring. Information on DNA methylomes from each parent will allow us to distinguish between maternally and paternally epigenetic profiles transmitted to the offspring. Principal component analyses will be used to identify the specific metabolic or anthropometric features of the mother that are associated with a specific DNA methylation footprint transmitted to the offspring. Placental function is assessed from samples taken within 30 min after delivery of the placenta. The samples are immediately frozen on dry ice and stored at −80°C. Analyses will include RNA-seq, non-targeted metabolomics, RT-qPCR, Western blot, histology and immunohistochemistry. Breastmilk is obtained from a single feed at the day of visit 5 and stored at −80°C for later metabolomic and lipidomic analyses.
Process evaluation of interventions
A process evaluation is made using quantitative and qualitative methods to provide insight into mechanisms through which interventions bring about change, assess fidelity and quality of implementation, clarify causal mechanisms and identify contextual factors associated with variations in outcomes.93–95 Integrating process evaluations alongside outcome data is recommended by the UK Medical Research Council guidelines in order to develop and evaluate complex interventions to improve the interpretation of the outcomes, design more effective interventions and apply interventions appropriately across groups and settings by understanding the implementation and functioning of interventions in a given context.94 96 The Reach, Effectiveness, Adoption, Implementation, and Maintenance framework is used to improve reporting on key issues related to the implementation and external validity of FitMum RCT.97
Personal understandings of physical activity
The qualitative dataset is composed of 220 short standardised screening interviews, 30 semistructured interviews, 70 observations, five sets of autoethnographies, visual material, as well as drop-out and follow-up interviews. This subproject will explore the physical and mental health and well-being of the participants, their social relations, PA levels and their experience of pregnancy to identify the challenges and barriers of PA during pregnancy. Personal understandings of PA in the everyday life of participants are determined at inclusion, GA week 34 and one year postpartum, in approximately ten participants from each of the three study groups.
Changes during the COVID-19 pandemic
Due to the COVID-19 pandemic (present in Denmark from 11 March 2020), supplies of interventions (EXE and MOT) and visits are periodically changed. During the lockdown period in spring 2020, all visits (except birth) are converted into online versions using Zoom Cloud Meetings or telephone. From 11 March 2020, in EXE, the swimming pool sessions are replaced with online land exercises and all land exercise sessions consist of 30 min of aerobic exercise where the participants exercise on their own (eg, biking, power-walking, dancing and aerobics) followed by 30 min of supervised online group resistance training. All individual and group MOT sessions are held online.
As much data as possible are collected during the pandemic, but some clinical data have not been possible to obtain in all participants due to limitations on non-urgent visits to the hospital. No blood samples are obtained at the virtual ‘visits’, women are weighed at home and symphysis-fundal height measurements are not obtained. No doubly labelled water is administered at the virtual ‘visit’ 2. The participant’s body weight at visit 4 is noted by the midwives on the day of giving birth, but biological samples are not collected. No DXA scans or breastmilk samples are collected at ‘visit’ 5.
Data management and analysis
Data management
The activity tracker data are collected by Fitabase, which regularly backs up the data. A participant who does not synchronise the tracker for seven days or more is reminded by email, text message or phone call. All tracker data are exported from Fitabase to R98 for data analysis. Tracker data are used to calculate non-wear time; a week is included in the analysis if the week has four or more days with complete data. A day that has six hours or more of non-wear time is excluded and considered a missing day. An electronic case report form (e-CRF) is used to collect all clinical data related to the trial. Data are stored in coded form according to the rules of the Danish Data Protection Agency. Personal data processing complies with the Act on Processing of Personal Data. Data are owned by NOH and University of Copenhagen. Use of data generated in FitMum RCT in new contexts must be agreed and approved by the Steering group. Technical University of Denmark and Aarhus University must have access to the data they have collected and are free to use it in new contexts. The e-CRF is completed by the investigators at the time of the participant’s visits at NOH so that it always reflects the latest observations of the participant. Data will be stored for ten years, after which they will be transferred to the Danish National Archives ‘Rigsarkivet’ in an anonymised format.
Sample size
FitMum RCT has been powered to detect an overall significant difference in the primary outcome between the three groups as well as a significant difference between the two intervention groups (EXE vs MOT) with average activity levels of 210 (EXE), 150 (MOT) and 60 (CON) min/week. The SD was set at 116 min/week and based on the results from Oostdam et al.51 The required sample size is determined to obtain a power of 80% with a family-wise significance level of 5%. The sample size calculation showed that the required number of participants is 35 in CON and 70 in each of the two intervention groups due to the randomisation ratio of 1:2:2 to CON, EXE and MOT, respectively. Based on an expected lost to follow-up rate of 20%, as seen in similar exercise studies in pregnant women,28 32 33 51 we plan to include 44 participants in CON and 88 participants in each of the two intervention groups, making a total of 220 participants.
Statistical methods
Data analyses of both primary and secondary outcomes will be performed using intention-to-treat analyses. In addition, a dose–response model will be estimated to quantify the relationship between adherence to the intervention (proportion of attendances in the planned EXE and MOT sessions, respectively) and the activity level. Moreover, analyses describing associations between the level of physical activity (as measured by the activity tracker) and the secondary and additional outcomes will be performed. Baseline data will be reported as averages and SDs (medians and IQRs) or frequencies and proportions as appropriate. No interim analyses will be performed on the primary and secondary outcomes. The analysis of the primary outcome will be performed using a linear model with the randomisation group as a categorical covariate and with adjustment for baseline PA level. Hypothesis tests will be performed using likelihood ratio tests. Statistical analysis will be conducted using R.98 Analyses of the primary outcome will be performed by a statistician blinded from the intervention allocations. Investigators will perform analyses of baseline data and secondary and additional outcomes under the supervision of a statistician. A full statistical analysis plan is published in ClinicalTrials.gov.99
Trial status
The recruitment of participants began in September 2018 and ended in October 2020. Data collection of the primary outcome is completed in spring 2021. Full data collection is expected to be complete in 2022.
Ethics and dissemination
The FitMum study adheres to the principles of the Helsinki declaration. The study is approved by the Danish National Committee on Health Research Ethics (# H-18011067) and the Danish Data Protection Agency (# P-2019-512).
All participants consent in written form before inclusion and are informed that participation in the FitMum study is voluntary. Participants are informed that they may withdraw from the study at any time and that withdrawal of consent will not affect any subsequent pregnancy and delivery processes at NOH. The participant has time to ask questions and is allowed 24 hours to deliberate on study participation before the obtainment of written informed consent.
FitMum RCT is designed based on recommendations of appropriate PA during pregnancy,14 45 100 101 and although anatomic and physiological changes occur during pregnancy, PA during an uncomplicated pregnancy is safe.14 22 29 40 60 102–105 All information about adverse events and serious adverse events are documented consecutively and will be reported. Participants will be discontinued from the intervention if they are at risk of preterm birth, if a cervical length below 25 mm is measured, if serious obstetric or medical complications occur, if investigators’ assessment reveals that continuation in the trial would be detrimental to the participant’s well-being or if intolerable adverse events occur.
The FitMum study will provide evidence-based knowledge that can contribute to improving national and international recommendations of PA during pregnancy and to new, effective and simple guidance to implement health technology-supported exercise programmes to pregnant women. Based on the results and process evaluation, the knowledge and tools from the FitMum study can be transformed into initiatives in municipalities and hospitals to improve the health and quality of life for both mother and child and can be used for preventing the development of lifestyle-related diseases across generations.
Findings will be submitted for publication in peer-reviewed scientific journals and disseminated at national and international conferences. In addition, results will be disseminated to the public in relevant media and to health professionals via science theatre performances.
Discussion
The FitMum study aims to evaluate the effects of structured supervised exercise training and motivational counselling supported by health technology on PA level during pregnancy to generate evidence about how to implement PA in everyday life in healthy pregnant women. Previous studies have investigated the effect of different lifestyle interventions on various health outcomes in normal weight,23 24 26 28 50–57 overweight and obese pregnant women.20 21 32 33 58–61 However, none of these studies have focused primarily on investigating the effect of PA interventions on actual PA level determined by novel objective methods. In addition, the FitMum study compares the effect of two very different PA interventions to explore strategies to implement PA programmes into pregnant women’s everyday life. Moreover, offspring of FitMum participants will be studied for one year after birth, whereby knowledge on the effect of PA during pregnancy on offspring health will be obtained. A limitation of the study is that the true effect of motivational counselling is not identified, as technology is an integral part of the MOT intervention.
Consumer-based wearable activity trackers tend to increase PA level when they are used as an intervention tool or as part of an intervention.106 Activity trackers are often relatively light weight, comfortable to wear and rechargeable.107 In addition, using an activity tracker to measure PA during pregnancy is feasible, recommended108 and has a reasonable compliance rate during pregnancy and after giving birth.109 However, there are some challenges and limitations of using activity trackers in a long-term intervention study. First, the participants must recharge the device and synchronise their data approximately once per week, which burdens participants and challenges adherence and compliance. Second, we cannot control the interaction of CON participants with the tracker. Third, the main goal for the tracker’s design is a comfortable wear, yet wearing the tracker for extended periods of time may cause skin irritation and discomfort.110 Moreover, the unavailability of the raw data and algorithms used by the manufacturer creates a limitation in the validation of PA metrics.107 Therefore, measuring PA by a variety of methods, and comparing these methods with the doubly labelled water technique (a gold standard method), will be used in order to obtain comprehensive measures of PA behaviours in FitMum participants.
Supplementary Material
Acknowledgments
We would like to thank the technical staff, especially Susanne Månsson, from the Clinical Research Unit, Department of Research, NOH, for their contribution in planning the practical work involved in the collection of data.
Footnotes
Twitter: @jakobeglarsen
Contributors: BS initiated the FitMum study together with LT and is the principal investigator of FitMum RCT. ECLL is the clinical trial manager. A steering group consisting of BS, ECLL, TDC, JEL and HTM oversees trial status and progression. CBR, SdPK and BS led the protocol development with contribution from SAA, ADA, JB, TDC, SM, AKJ, GT, APJ, JEL, GvH, EA, RB, OHM, HTM, LT and ECLL. CBR, SdPK, SAA, ADA, JB, TDC, SM, ECLL and BS constitute the clinical core group that guides the practical performance of FitMum RCT. CBR, SdPK and ADA conduct intervention activities together with research assistants and master’s students. CBR, SdPK, SAA and ADA will perform most of the data analysis along with AKJ. Analyses of the primary outcome will be performed by AKJ. All authors read, contributed to and approved the final version of the manuscript.
Funding: The FitMum study has been financially supported by the Independent Research Fund Denmark (8020-00353B and 0218-00014B), TrygFonden (128509), Copenhagen Center for Health Technology (061017), Beckett-Fonden (17-2-0883), Aase and Ejnar Danielsens Fond (10-002052) and Familien Hede Nielsens Fond (2017-1142).
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Craike M, Hill B, Gaskin CJ, et al. Interventions to improve physical activity during pregnancy: a systematic review on issues of internal and external validity using the RE-AIM framework. BJOG: Int J Obstet Gy 2017;124:573–83. 10.1111/1471-0528.14276 [DOI] [PubMed] [Google Scholar]
- 2.Thangaratinam S, Rogozińska E, Jolly K, et al. Interventions to reduce or prevent obesity in pregnant women: a systematic review. Health Technol Assess 2012;16:1–8. 10.3310/hta16310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organisation (who) . Good maternal nutrition. The best start in life, 2016. [Google Scholar]
- 4.Adamo KB, Ferraro ZM, Brett KE. Can we modify the intrauterine environment to halt the intergenerational cycle of obesity? Int J Environ Res Public Health 2012;9:1263–307. 10.3390/ijerph9041263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jelsma JGM, van Leeuwen KM, Oostdam N, et al. Beliefs, barriers, and preferences of European overweight women to adopt a healthier lifestyle in pregnancy to minimize risk of developing gestational diabetes mellitus: an explorative study. J Pregnancy 2016;2016:1–11. 10.1155/2016/3435791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hill B, McPhie S, Moran LJ. Lifestyle intervention to prevent obesity during pregnancy: implications and recommendations for research and implementation. Midwifery 2016;2017:13–18. [DOI] [PubMed] [Google Scholar]
- 7.Bønnelycke J, Sandholdt CT, Jespersen AP. Household collectives: resituating health promotion and physical activity. Sociol Health Illn 2019;41:533–48. 10.1111/1467-9566.12832 [DOI] [PubMed] [Google Scholar]
- 8.Borodulin K, Evenson KR, Herring AH. Physical activity patterns during pregnancy through postpartum. BMC Womens Health 2009;9:32. 10.1186/1472-6874-9-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santo EC, Forbes PW, Oken E, et al. Determinants of physical activity frequency and provider advice during pregnancy. BMC Pregnancy Childbirth 2017;17:1–11. 10.1186/s12884-017-1460-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hegaard HK, Damm P, Hedegaard M, et al. Sports and leisure time physical activity during pregnancy in nulliparous women. Matern Child Health J 2011;15:806–13. 10.1007/s10995-010-0647-y [DOI] [PubMed] [Google Scholar]
- 11.Owe KM, Nystad W, Bø K. Correlates of regular exercise during pregnancy: the Norwegian mother and child cohort study. Scand J Med Sci Sports 2009;19:637–45. 10.1111/j.1600-0838.2008.00840.x [DOI] [PubMed] [Google Scholar]
- 12.Richardsen KR, Falk RS, Jenum AK, et al. Predicting who fails to meet the physical activity guideline in pregnancy: a prospective study of objectively recorded physical activity in a population-based multi-ethnic cohort. BMC Pregnancy Childbirth 2016;16:1–11. 10.1186/s12884-016-0985-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barrès R, Zierath JR. The role of diet and exercise in the transgenerational epigenetic landscape of T2DM. Nat Rev Endocrinol 2016;12:441–51. 10.1038/nrendo.2016.87 [DOI] [PubMed] [Google Scholar]
- 14.Committee on Obstetric Practice . Committee opinion: physical activity and exercise during pregnancy and the postpartum period. Am Coll Obstet Gynecol 2015;650:1–8. [Google Scholar]
- 15.Evenson KR, Barakat R, Brown WJ. Guidelines for physical activity during pregnancy: comparisons from around the world. Am J Lifestyle Med 2014;8:102–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perales M, Artal RLA. Exercise during pregnancy. JAMA 2017;317:1113–4. 10.1001/jama.2017.0593 [DOI] [PubMed] [Google Scholar]
- 17.Moyer C, Reoyo OR, May L. The influence of prenatal exercise on offspring health: a review. Clin Med Insights Womens Health 2016;9:CMWH.S34670. 10.4137/CMWH.S34670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.U.S. Department of Health and Human Services . 2018 Physical Activity Guidelines Advisory Committee Scientific Report To the Secretary of Health and Human. 2018 Phys Act Guidel Advis Comm Sci Report To Secr Heal Hum Serv [Internet]., 2018. Available: https://health.gov/paguidelines/second-edition/report/pdf/PAG_Advisory_Committee_Report.pdf
- 19.Mottola MF, Davenport MH, Ruchat S-M, et al. 2019 Canadian guideline for physical activity throughout pregnancy. Br J Sports Med 2018;52:1339–46. 10.1136/bjsports-2018-100056 [DOI] [PubMed] [Google Scholar]
- 20.Ruiz JR, Perales M, Pelaez M, et al. Supervised exercise-based intervention to prevent excessive gestational weight gain: a randomized controlled trial. Mayo Clin Proc 2013;88:1388–97. 10.1016/j.mayocp.2013.07.020 [DOI] [PubMed] [Google Scholar]
- 21.Leung Hui A, Back L, Ludwig S. Effects of lifestyle intervention on dietary intake, physical activity level, and gestational weight gain in pregnant women with different pre-pregnancy body mass index in a randomized control trial. BMC Pregnancy Childbirth 2014;14:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wiebe HW, Boulé NG, Chari R, et al. The effect of supervised prenatal exercise on fetal growth. Obstet Gynecol 2015;125:1185–94. 10.1097/AOG.0000000000000801 [DOI] [PubMed] [Google Scholar]
- 23.Poston L, Bell R, Croker H, et al. Effect of a behavioural intervention in obese pregnant women (the upbeat study): a multicentre, randomised controlled trial. Lancet Diabetes Endocrinol 2015;3:767–77. 10.1016/S2213-8587(15)00227-2 [DOI] [PubMed] [Google Scholar]
- 24.Harrison CL, Lombard CB, Strauss BJ, et al. Optimizing healthy gestational weight gain in women at high risk of gestational diabetes: a randomized controlled trial. Obesity 2013;21:904–9. 10.1002/oby.20163 [DOI] [PubMed] [Google Scholar]
- 25.Vinter CA, Jensen DM, Ovesen P. The lip (lifestyle in pregnancy) study. Diabetes Care 2011;34:2502–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Renault KM, Nørgaard K, Nilas L, et al. The treatment of obese pregnant women (top) study: a randomized controlled trial of the effect of physical activity intervention assessed by pedometer with or without dietary intervention in obese pregnant women. Am J Obstet Gynecol 2014;210:134.e1–134.e9. 10.1016/j.ajog.2013.09.029 [DOI] [PubMed] [Google Scholar]
- 27.Russo LM, Nobles C, Ertel KA. Physical activity interventions in pregnancy and risk of gestational diabetes mellitus a systematic review and meta-analysis. Obstet Gynecol 2015;125:576–82. [DOI] [PubMed] [Google Scholar]
- 28.Wang C, Wei Y, Zhang X. A randomized clinical trial of exercise during pregnancy to prevent gestational diabetes mellitus and improve pregnancy outcome in overweight and obese pregnant women. Am J Obstet Gynecol 2017:1–30. [DOI] [PubMed] [Google Scholar]
- 29.Di Mascio D, Magro-Malosso ER, Saccone G, et al. Exercise during pregnancy in normal-weight women and risk of preterm birth: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol 2016;215:561–71. 10.1016/j.ajog.2016.06.014 [DOI] [PubMed] [Google Scholar]
- 30.Sanabria-Martínez G, García-Hermoso A, Poyatos-León R, et al. Effectiveness of physical activity interventions on preventing gestational diabetes mellitus and excessive maternal weight gain: a meta-analysis. BJOG: Int J Obstet Gy 2015;122:1167–74. 10.1111/1471-0528.13429 [DOI] [PubMed] [Google Scholar]
- 31.Koivusalo SB, Rönö K, Klemetti MM, et al. Gestational diabetes mellitus can be prevented by lifestyle intervention: the Finnish gestational diabetes prevention study (RADIEL): a randomized controlled trial. Diabetes Care 2016;39:24–30. 10.2337/dc15-0511 [DOI] [PubMed] [Google Scholar]
- 32.Barakat R, Perales M, Cordero Y. Influence of land or water exercise in pregnancy on outcomes: a cross-sectional study. Med Sci Sports Exerc 2017;49:1397–403. [DOI] [PubMed] [Google Scholar]
- 33.Backhausen MG, Tabor A, Albert H, et al. The effects of an unsupervised water exercise program on low back pain and sick leave among healthy pregnant women – a randomised controlled trial. PLoS One 2017;12:e0182114. 10.1371/journal.pone.0182114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barakat R, Pelaez M, Lopez C, et al. Exercise during pregnancy reduces the rate of cesarean and instrumental deliveries: results of a randomized controlled trial. J Matern Fetal Neonatal Med 2012;25:2372–6. 10.3109/14767058.2012.696165 [DOI] [PubMed] [Google Scholar]
- 35.Nielsen EN, Andersen PK, Hegaard HK, et al. Mode of delivery according to leisure time physical activity before and during pregnancy: a multicenter cohort study of low-risk women. J Pregnancy 2017;2017:1–8. 10.1155/2017/6209605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dumith SC, Domingues MR, a M-SR. Physical activity during pregnancy and its association with maternal and child health indicators. Rev Saude Publica 2012;46:327–33. [DOI] [PubMed] [Google Scholar]
- 37.Owe KM, Nystad W, Stigum H, et al. Exercise during pregnancy and risk of cesarean delivery in nulliparous women: a large population-based cohort study. Am J Obstet Gynecol 2016;215:791.e1–e13. 10.1016/j.ajog.2016.08.014 [DOI] [PubMed] [Google Scholar]
- 38.Ferrari N, Bae-Gartz I, Bauer C. Exercise during pregnancy and its impact on mothers and offspring in humans and mice. J Dev Orig Health Dis 2017:1–14. [DOI] [PubMed] [Google Scholar]
- 39.Huang L, Fan L, Ding P. Maternal exercise during pregnancy reduces the risk of preterm birth through the mediating role of placenta. J Matern Neonatal Med 2017;7058:1–21. [DOI] [PubMed] [Google Scholar]
- 40.Magro-Malosso ER, Saccone G, Di Mascio D. Exercise during pregnancy risk of preterm birth in overweight and obese women: a systematic review and meta-analysis of randomized controlled trials. Acta Obstet Gynecol Scand 2017;215:561–71. [DOI] [PubMed] [Google Scholar]
- 41.Pomeroy J, Renström F, Gradmark AM, et al. Maternal physical activity and insulin action in pregnancy and their relationships with infant body composition. Diabetes Care 2013;36:267–9. 10.2337/dc12-0885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Harrod CS, Chasan-Taber L, Reynolds RM. Physical activity in pregnancy and neonatal body composition: the healthy start study. Obs Gynecol 2014;124:257–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Clapp JF. Influence of endurance exercise and diet on human placental development and fetal growth. Placenta 2006;27:527–34. 10.1016/j.placenta.2005.07.010 [DOI] [PubMed] [Google Scholar]
- 44.Jackson MR, Gott P, Lye SJ, et al. The effects of maternal aerobic exercise on human placental development: placental volumetric composition and surface areas. Placenta 1995;16:179–91. 10.1016/0143-4004(95)90007-1 [DOI] [PubMed] [Google Scholar]
- 45.The Danish Health Authorities . Recommendations for pregnant women [online], 2014. Available: https://www.sst.dk/en/health-and-lifestyle/physical-activity/recommendations/pregnant-women
- 46.Broberg L, Ersbøll AS, Backhausen MG, et al. Compliance with national recommendations for exercise during early pregnancy in a Danish cohort. BMC Pregnancy Childbirth 2015;15:317. 10.1186/s12884-015-0756-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Weir Z, Bush J, Robson SC, et al. Physical activity in pregnancy: a qualitative study of the beliefs of overweight and obese pregnant women. BMC Pregnancy Childbirth 2010;10:1–7. 10.1186/1471-2393-10-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bauer C, Graf C, Platschek AM. Reasons, motivational factors and percieved personal barriers to engagement in physical activity during pregnancy vary within the bmi classes - the prenatal prevention project Germany. J Phys Act Heal 2017;32:1–44. [DOI] [PubMed] [Google Scholar]
- 49.Lindqvist M, Persson M, Mogren I. "Longing for individual recognition" - Pregnant women's experiences of midwives' counselling on physical activity during pregnancy. Sex Reprod Healthc 2018;15:46–53. 10.1016/j.srhc.2017.12.003 [DOI] [PubMed] [Google Scholar]
- 50.Hawkins M, Chasan-Taber L, Marcus B, et al. Impact of an exercise intervention on physical activity during pregnancy: the behaviors affecting baby and you study. Am J Public Health 2014;104:e74–81. 10.2105/AJPH.2014.302072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Oostdam N, van Poppel MNM, Wouters M, et al. No effect of the FitFor2 exercise programme on blood glucose, insulin sensitivity, and birthweight in pregnant women who were overweight and at risk for gestational diabetes: results of a randomised controlled trial. BJOG An Int J Obstet Gynaecol 2012;119:1098–107. 10.1111/j.1471-0528.2012.03366.x [DOI] [PubMed] [Google Scholar]
- 52.Seneviratne SN, Jiang Y, Derraik JGB, et al. Effects of antenatal exercise in overweight and obese pregnant women on maternal and perinatal outcomes: a randomised controlled trial. BJOG 2016;123:588–97. 10.1111/1471-0528.13738 [DOI] [PubMed] [Google Scholar]
- 53.Ussher M, Lewis S, Aveyard P, et al. Physical activity for smoking cessation in pregnancy: randomised controlled trial. BMJ 2015;350:h2145. 10.1136/bmj.h2145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gaston A, Prapavessis H. Using a combined protection motivation theory and health action process approach intervention to promote exercise during pregnancy. J Behav Med 2014;37:173–84. 10.1007/s10865-012-9477-2 [DOI] [PubMed] [Google Scholar]
- 55.Vinter CA, Jensen DM, Ovesen P, et al. The lip (lifestyle in pregnancy) study: a randomized controlled trial of lifestyle intervention in 360 obese pregnant women. Diabetes Care 2011;34:2502–7. 10.2337/dc11-1150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kong KL, Campbell CG, Foster RC, et al. A pilot walking program promotes moderate-intensity physical activity during pregnancy. Med Sci Sports Exerc 2014;46:462–71. 10.1249/MSS.0000000000000141 [DOI] [PubMed] [Google Scholar]
- 57.Smith KM. The blossom project online: use of a behaviorally-based website to promote physical activity and prevent excessive gestational weight gain in previously sedentary pregnant women. ProQuest Dissertations Theses 2014. [Google Scholar]
- 58.Cavalcante SR, Cecatti JG, Pereira RI, et al. Water aerobics II: maternal body composition and perinatal outcomes after a program for low risk pregnant women. Reprod Health 2009;6:1–7. 10.1186/1742-4755-6-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Haakstad LAH, Bo K. Exercise in pregnant women and birth weight: a randomized controlled trial. BMC Pregnancy Childbirth 2011;11:1–7. 10.1186/1471-2393-11-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tomić V, Sporiš G, Tomić J, et al. The effect of maternal exercise during pregnancy on abnormal fetal growth. Croat Med J 2013;54:362–8. 10.3325/cmj.2013.54.362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.de Oliveria Melo AS, Silva JLP, Tavares JS, et al. Effect of a physical exercise program during pregnancy on uteroplacental and fetal blood flow and fetal growth: a randomized controlled trial. Obstet Gynecol 2012;120:302–10. 10.1097/AOG.0b013e31825de592 [DOI] [PubMed] [Google Scholar]
- 62.Currie S, Sinclair M, Murphy MH, et al. Reducing the decline in physical activity during pregnancy: a systematic review of behaviour change interventions. PLoS One 2013;8:e66385. 10.1371/journal.pone.0066385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pearce EE, Evenson KR, Downs DS, et al. Strategies to promote physical activity during pregnancy. Am J Lifestyle Med 2013;7:38–50. 10.1177/1559827612446416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982;14:377???381. 10.1249/00005768-198205000-00012 [DOI] [PubMed] [Google Scholar]
- 65.Miller BG, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. New York: Guilford press. J Community Appl Soc Psychol [online] 1991;2:299–300. [Google Scholar]
- 66.Markland D, Ryan RM, Tobin VJ, et al. Motivational interviewing and Self–Determination theory. J Soc Clin Psychol 2005;24:811–31. 10.1521/jscp.2005.24.6.811 [DOI] [Google Scholar]
- 67.Michie S, Ashford S, Sniehotta FF, et al. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 2011;26:1479–98. 10.1080/08870446.2010.540664 [DOI] [PubMed] [Google Scholar]
- 68.de Vries HJ, Kooiman TJM, van Ittersum MW, et al. Do activity monitors increase physical activity in adults with overweight or obesity? A systematic review and meta-analysis. Obesity 2016;24:2078–91. 10.1002/oby.21619 [DOI] [PubMed] [Google Scholar]
- 69.Cadmus-Bertram LA, Marcus BH, Patterson RE, et al. Randomized trial of a Fitbit-Based physical activity intervention for women. Am J Prev Med 2015;49:414–8. 10.1016/j.amepre.2015.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chasan-Taber L, Schmidt MD, Roberts DE, et al. Development and validation of a pregnancy physical activity questionnaire. Med Sci Sports Exerc 2004;36:1750–60. 10.1249/01.MSS.0000142303.49306.0D [DOI] [PubMed] [Google Scholar]
- 71.Santini De Oliveira C, Dos Santos Imakawa T. Physical activity during pregnancy: recommendations and assessment tools. Rev Bras Ginecol Obs 2017;39:424–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schuster S, Šklempe Kokić I, Sindik J. Measuring physical activity in pregnancy using questionnaires: a meta-analysis. Acta Clin Croat 2016;55:440–51. 10.20471/acc.2016.55.03.13 [DOI] [PubMed] [Google Scholar]
- 73.Holmberg Krøner F, de Place Knudsen S, Borup Roland C. Validity and reliability of the Danish version of the pregnancy physical activity questionnaire to assess levels of physical activity during pregnancy, 2020. Journal of Maternal-Fetal and neonatal medicine [DOI] [PubMed]
- 74.Abeysekera MV, Morris JA, O’Sullivan AJ. Techniques to measure free-living energy expenditure during pregnancy - A guide for clinicians and researchers. Obstet Med 2014;7:60–5. 10.1177/1753495X14528324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.van Hees VT, Renström F, Wright A, et al. Estimation of daily energy expenditure in pregnant and non-pregnant women using a wrist-worn tri-axial accelerometer. PLoS One 2011;6:e22922–10. 10.1371/journal.pone.0022922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lof M, Forsum E. Activity pattern and energy expenditure due to physical activity before and during pregnancy in healthy Swedish women. Br J Nutr 2006;95:296–302. 10.1079/BJN20051497 [DOI] [PubMed] [Google Scholar]
- 77.Wong WW, Roberts SB, Racette SB, et al. The doubly labeled water method produces highly reproducible longitudinal results in nutrition studies. J Nutr 2014;144:777–83. 10.3945/jn.113.187823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Health Assessment Lab . Medical outcomes trust and QualityMetric incorporated. SF-36v2 health survey 2004.
- 79.Bjorner JB, Thunedborg K, Kristensen TS, et al. The Danish SF-36 Health Survey: Translation and preliminary validity studies. J Clin Epidemiol. 1998;51(11):991–9. 1998:5–10. [DOI] [PubMed]
- 80.Jomeen J, Martin CR. The factor structure of the SF-36 in early pregnancy. J Psychosom Res 2005;59:131–8. 10.1016/j.jpsychores.2005.02.018 [DOI] [PubMed] [Google Scholar]
- 81.Bland HW, Melton BF, Marshall ES, et al. Measuring exercise self-efficacy in pregnant women: psychometric properties of the Pregnancy-Exercise self-efficacy scale (P-ESES). J Nurs Meas 2013;21:349–59. 10.1891/1061-3749.21.3.349 [DOI] [PubMed] [Google Scholar]
- 82.Bendix EJ, Holmberg Krøner F, de Place Knudsen S, et al. Cross-Cultural adaption, translation and reliability tests of the Danish version of the pregnancy exercise self-efficacy scale. Sex Reprod Healthc 2020;26:100542. 10.1016/j.srhc.2020.100542 [DOI] [PubMed] [Google Scholar]
- 83.Mullan E, Markland D, Ingledew DK. A graded conceptualisation of self-determination in the regulation of exercise behaviour: development of a measure using confirmatory factor analytic procedures. :. 23. Pergamon Person, 1997. [Google Scholar]
- 84.Mullan E, Markland D, Mullan E. Variations in Self-Determination across the stages of change for exercise in adults. Vol. 21, motivation and emotion. Markland & Hardy 1997. [Google Scholar]
- 85.Markland D, Tobin V. A modification to the behavioural regulation in exercise questionnaire to include an assessment of Amotivation. J Sport Exerc Psychol 2004;26:191–6. 10.1123/jsep.26.2.191 [DOI] [Google Scholar]
- 86.Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 87.University of Pittsburgh . Pittsburgh sleep quality index (PSQI) 1988;3:6. [Google Scholar]
- 88.Qiu C, Gelaye B, Zhong Q-Y, et al. Construct validity and factor structure of the Pittsburgh sleep quality index among pregnant women in a Pacific-Northwest cohort. Sleep Breath 2016;20:293–301. 10.1007/s11325-016-1313-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cox JL. Perinatal mental health : a guide to the Edinburgh Postnatal Depression Scale (EPDS). Gaskell, 2003: 125. [Google Scholar]
- 90.Zierau F, Bille A, Rutz W, et al. The Gotland male depression scale: a validity study in patients with alcohol use disorder. Nord J Psychiatry 2002;56:265–71. 10.1080/08039480260242750 [DOI] [PubMed] [Google Scholar]
- 91.Magovcevic M, Addis ME. The masculine depression scale: development and psychometric evaluation. Psychol Men Masc 2008;9:117–32. 10.1037/1524-9220.9.3.117 [DOI] [Google Scholar]
- 92.Madsen SA. Spædbarnet i faderens verden (Infants’ within the world of the father). Psyke & Logos [online] 2008;29:669–87. [Google Scholar]
- 93.Craig P. Developing and evaluating complex interventions.
- 94.Moore G, Audrey S, Barker M, et al. Process evaluation in complex public health intervention studies: the need for guidance. J Epidemiol Community Health 2014;68:101–2. 10.1136/jech-2013-202869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hoffmann TC, Erueti C, Glasziou PP. Poor description of non-pharmacological interventions: analysis of consecutive sample of randomised trials. BMJ 2013;347:f3755. 10.1136/bmj.f3755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.F. Moore G, Raisanen L, Moore L, et al. Mixed-method process evaluation of the Welsh national exercise referral scheme. Health Educ 2013;113:476–501. 10.1108/HE-08-2012-0046 [DOI] [Google Scholar]
- 97.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework, 1999 [DOI] [PMC free article] [PubMed]
- 98.R Core Team . R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2020. https://www.r-project.org/ [Google Scholar]
- 99.Statistical Analysis Plan (SAP) for the FitMum randomized controlled trial [online], 2020. Available: https://clinicaltrials.gov/ProvidedDocs/30/NCT03679130/SAP_000.pdf
- 100.UK Chief Medical Officers . Uk chief medical officers recommendations 2017. Physical Activity in Pregnancy, 2017. [Google Scholar]
- 101.UK Chief Medical Officers . UK chief medical officers recommendations 2017: physical activity in pregnancy, guidance 2017:1–7.
- 102.Verdiere S, Guinhouya BC, Salerno D. Should physical activity be contraindicated during pregnancy in relation to its potentially related risks? 2017;45:104–11. [DOI] [PubMed] [Google Scholar]
- 103.Melo A, Silva JLP, Tavares JS. Effect of a physical exercise program during pregnancy on Uteroplacental and fetal blood flow and fetal growth 2012;120:302–10. [DOI] [PubMed] [Google Scholar]
- 104.Rêgo AS, Alves MTSSdeBe, Batista RFL. Physical activity in pregnancy and adverse birth outcomes 2016;32:1–10. [DOI] [PubMed] [Google Scholar]
- 105.Charlesworth S, Foulds HJ, Burr J, et al. Evidence-based risk assessment and recommendations for physical activity clearance: pregnancy. Appl Physiol Nutr Metab 2011;36:S154–89. [DOI] [PubMed] [Google Scholar]
- 106.Brickwood K-J, Watson G, O’Brien J, et al. Consumer-based wearable activity trackers increase physical activity participation: systematic review and meta-analysis. JMIR Mhealth Uhealth 2019;7:e11819. 10.2196/11819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wright SP, Hall Brown TS, Collier SR, et al. How consumer physical activity monitors could transform human physiology research. Am J Physiol Regul Integr Comp Physiol 2017;312:R358–67. 10.1152/ajpregu.00349.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Guérin E, Ferraro ZM, Adamo KB, et al. The need to objectively measure physical activity during pregnancy: considerations for clinical research and public health impact. Matern Child Health J 2018;22:637–41. 10.1007/s10995-018-2475-4 [DOI] [PubMed] [Google Scholar]
- 109.Grym K, Niela-Vilén H, Ekholm E, et al. Feasibility of smart wristbands for continuous monitoring during pregnancy and one month after birth. BMC Pregnancy Childbirth 2019;19:1–9. 10.1186/s12884-019-2187-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wear and care tips for garmin watches [online]. Available: https://support.garmin.com/en-US/?faq=yAgOpDYLCe4ftSa9k0dQx7&searchType=noProduct&sas_source=grmn [Accessed 8 Sep 2019].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-043671supp001.pdf (84.9KB, pdf)
bmjopen-2020-043671supp002.pdf (83.8KB, pdf)