Abstract
Introduction
African descent populations in the United States have high rates of type 2 diabetes and are incorrectly represented as a single group. Current glycated hemoglobin A1c (HbA1c) cutoffs (5.7% to <6.5% for prediabetes; ≥6.5% for type 2 diabetes) may perform suboptimally in evaluating glycemic status among African descent groups. We conducted a scoping review of US-based evidence documenting HbA1c performance to assess glycemic status among African American, Afro-Caribbean, and African people.
Methods
A PubMed, Scopus, and Cumulative Index to Nursing and Allied Health Literature (CINAHL) search (January 2020) yielded 3,238 articles published from January 2000 through January 2020. After review of titles, abstracts, and full texts, 12 met our criteria. HbA1c results were compared with other ethnic groups or validated against the oral glucose tolerance test (OGTT), fasting plasma glucose (FPG), or previous diagnosis. We classified study results by the risk of false positives and risk of false negatives in assessing glycemic status.
Results
In 5 studies of African American people, the HbA1c test increased risk of false positives compared with White populations, regardless of glycemic status. Three studies of African Americans found that HbA1c of 5.7% to less than 6.5% or HbA1c of 6.5% or higher generally increased risk of overdiagnosis compared with OGTT or previous diagnosis. In one study of Afro-Caribbean people, HbA1c of 6.5% or higher detected fewer type 2 diabetes cases because of a greater risk of false negatives. Compared with OGTT, HbA1c tests in 4 studies of Africans found that HbA1c of 5.7% to less than 6.5% or HbA1c of 6.5% or higher leads to underdiagnosis.
Conclusion
HbA1c criteria inadequately characterizes glycemic status among heterogeneous African descent populations. Research is needed to determine optimal HbA1c cutoffs or other test strategies that account for risk profiles unique to African American, Afro-Caribbean, and African people living in the United States.
Summary.
What is already known on this topic?
Type 2 diabetes disproportionately affects African descent groups, yet contributing factors are often overlooked. Studies show that glycated hemoglobin A1c (HbA1c) underperforms as a screening and diagnostic tool among ethnic cohorts of this population.
What is added by this report?
This review demonstrates that current HbA1c cutoffs overestimate glycemic status in African Americans and underestimate glycemic status in Afro-Caribbeans and Africans. It identifies gaps in the scientific literature, especially among Afro-Caribbeans.
What are the implications for public health practice?
Type 2 diabetes screening and diagnostic tests must account for genetic, biochemical, and socioeconomic factors. To ensure early type 2 diabetes detection, heterogeneity within African descent groups must be recognized, and more reliable testing strategies must be identified.
Introduction
People of African descent in the United States have a disproportionate burden of type 2 diabetes; prevalence is higher in African descent populations, 14%, compared with White populations of European descent (White populations), 9% (1). Additionally, African descent populations are represented as a single group, despite being comprised of African American (91%), Afro-Caribbean (4.7%), and African (3.7%) people (2,3). Limited evidence examines how intraethnic differences in cardiometabolic risk criteria, social determinants of health, and genetic admixture affect diabetes risk in these 3 populations (4,5). Current glycated hemoglobin A1c (HbA1c) cutoffs (HbA1c 5.7% to less than 6.5% for prediabetes; HbA1c of 6.5% or higher for type 2 diabetes), determined from predominantly White population cohorts (4–8), may perform suboptimally in evaluating glycemic status in this diverse population of African American, Afro-Caribbean, and African populations (9–12). African American people may have higher HbA1c values across the glycemic spectrum (9,13), and African immigrants may have lower HbA1c values compared with White people (14). To ensure accurate detection of type 2 diabetes, there is a need to understand the ability of HbA1c to correctly classify type 2 diabetes status and to evaluate intraethnic variation among African American, Afro-Caribbean, and African people (15–17).
Compared with random glucose, fasting plasma glucose (FPG), and the 2-hour oral glucose tolerance test (OGTT), HbA1c has multiple benefits. It does not require fasting, tracks plasma glucose over the preceding 2 to 3 months, and better predicts complications such as cardiovascular disease (4,18). The HbA1c test is stable, unaffected by external variables (eg, exercise, recent meals, and environmental stressors), and easily added to blood tests (19,20). However, interpretation of HbA1c results is affected by the reduced lifespan of red blood cells in patients with type 2 diabetes, anemia, and hemoglobinopathies, conditions which disproportionately affect African descent populations (21–25).
The goal of our study was to conduct a scoping review of US-based peer-reviewed evidence documenting HbA1c performance in African American, Afro-Caribbean, and African populations in the United States with the objectives of 1) summarizing evidence on HbA1c performance in each subethnic group; 2) demonstrating variations in HbA1c performance by each subethnic group; and 3) identifying potential future areas of research.
Methods
Data sources
In early January 2020, we searched PubMed, Scopus, and Cumulative Index to Nursing and Allied Health Literature (CINAHL) for peer-reviewed studies published between January 1, 2000, and January 1, 2020, by using complex search strings that were tested and developed in partnership with our institution’s health sciences librarian (L.A.F.). The search string included medical subject headings (MeSH) terms and key words such as “African continental ancestry group,” “African Americans,” “Caribbean,” and “West Indian” to describe population groups and “Glycated Hemoglobin A,” “hemoglobin A1c,” and “hba1c” to describe the testing indicator of interest for type 2 diabetes (Appendix).
Study selection
Throughout the review process, we screened articles for studies meeting the following inclusion criteria:
Articles were original studies published between January 2000 and January 2020, that evaluated HbA1c performance in African descent groups.
Study populations included African Americans, Afro-Caribbeans, or Africans.
Study participants were living in the United States.
Study was a database analysis, epidemiologic study, or clinical study.
HbA1c performance was reported specifically in one or more of the African descent groups.
HbA1c performance was assessed in healthy populations or for screening or diagnosis of prediabetes or type 2 diabetes.
HbA1c performance was assessed by statistical methods (eg, sensitivity, specificity, and positive predictive value), compared with other tests in the same population, or compared African descent populations to other racial groups.
During the study selection process, we included studies that compared various diabetes screening tests against HbA1c, including the OGTT, FPG, and glycated protein tests, to avoid excluding major findings. Although the OGTT is considered optimal for comparison, it is far more costly, resource intensive, and time consuming than the FPG and glycated protein tests (6–8); additionally, research supports the use of other tests along with OGTT or in place of OGTT to enhance detection of diabetes (7,18–22). Because African descent populations are less likely to be adequately represented in clinical research and simultaneously experience health care inequities (4,19), we wanted to be inclusive of all the data, in comparison to HbA1c, that were available for the populations.
On the basis of the title and abstract review, we excluded articles that did not match the set inclusion criteria above (Figure). Two authors (L.K. and S.B.) conducted independent title and abstract reviews. In the full-text review, we excluded articles with insufficient data (eg, case studies), narrative reviews, and articles that fell under a previously set exclusion criterion not detected during the title and abstract review. Full-text articles for potential studies were reviewed by 2 authors (L.K. and S.B.) independently. When multiple exclusion criteria were met, we categorized the article by the exclusion criterion that appeared first in title, abstract, or full text review. A third author (M.H.R.) verified that the exclusion criteria were relevant throughout the article.
Figure.
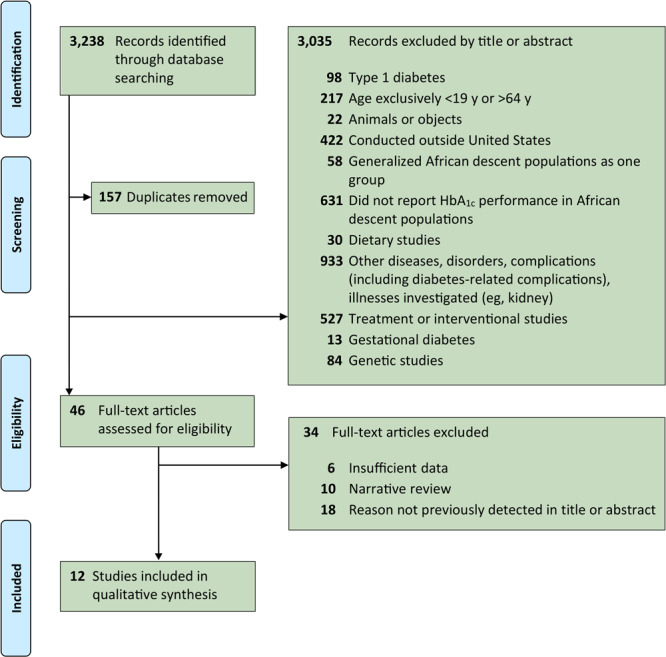
Flow diagram of the study selection process for glycated hemoglobin A1c (HbA1c) testing performance in African descent populations in the United States, using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses). Studies were published January 1, 2000, to January 1, 2020.
During the identification process, 3,238 records were identified through database searching. In the screening phase, 3,081 records were screened after 157 duplicates were removed. Records were excluded by using a title and abstract review (n = 3,035) by the following exclusion criteria: topic was type 1 diabetes (n = 98); age was exclusively less than 19 years or greater than 64 years (n = 217); topic was animals or objects (n = 22); study was conducted outside the United States (n = 422), study generalized African descent populations as one group (n = 58); study did not report HbA1c performance in African descent populations (n = 631); topic was a dietary study (n = 30); topic was other diseases, disorders, complications (including diabetes-related complications), or illnesses (eg, kidney) (n = 933); topic was a treatment or interventional study (n = 527); topic was gestational diabetes (n = 13); or topic was a genetic study (n = 84). After this screening process, the remaining 46 full-text articles were assessed for eligibility. Of these, 34 full-text articles were excluded based on the following exclusion criteria: insufficient data (n = 6); being a narrative review (n = 10); or for a reason not previously detected in the title or abstract (n = 18). The inclusion stage yielded 12 studies to be included in qualitative synthesis.
Data extraction
We created a data extraction sheet to record the study author and name, populations (sample size, male/female breakdown, race/ethnicity distribution, age, and study location), HbA1c laboratory methods, study design, HbA1c evaluation methods, findings, and HbA1c performance. We successfully retrieved any missing information by 1) searching through cited articles from which the studies retrieved data; 2) identifying parent studies and protocol descriptions given in prior publications; and 3) emailing corresponding authors. HbA1c performance was classified using 2 labels: 1) greater risk of false positive (GRFP) label indicated that the HbA1c test may result in overdetection of glycemic status (eg, type 2 diabetes) that the study is measuring or 2) greater risk of false negatives (GRFN) label indicated that the HbA1c test may result in underdetection of glycemic status. This classification system (GRFP or GRFN) was based on text analysis of the language used by the authors of each study in the way they interpreted their results (eg, lower sensitivity, lower specificity, more misdiagnoses). This allowed for standardization of labeling findings from different study designs. GRFP was assigned if studies reported 1) higher HbA1c values in African descent participants compared with other ethnic groups (eg, White participants) at the same glycemic level; 2) lower sensitivity because of less true positives; or 3) lower specificity because of more false positives. GRFN was assigned if studies reported 1) lower HbA1c values in participants compared with other ethnic groups at same glycemic level; 2) lower sensitivity because of more false negatives; or 3) or lower specificity because of less true negatives. Discrepancies in the review process and data extraction were resolved with input from a third author (M.H.R.).
Included studies were grouped based on study population (African American, Afro-Caribbean, and African) and then organized in alphabetical order by the first author’s last name. Studies were labeled numerically as 1 through 12 based on this ordering.
Results
Of the 12 articles that met the inclusion criteria, studies numbered 1 through 7 analyzed HbA1c performance among African American people (26–32), study number 8 analyzed HbA1c performance among Afro-Caribbean people (33), and studies numbered 9 through12 analyzed HbA1c performance among African people (34–37). All studies were conducted with people living in the United States (Table 1).
Table 1. Study Characteristics for Articles Reporting on Glycated Hemoglobin A1c (HbA1c) Performance Among African Descent Populations Living in the United States, 2010–2019.
| Study | First Author (Year); Study | N; Sex | Race/Ethnicitya (%) | Age, y | Location | Study Design | HbA1c Laboratory Analysis Method |
|---|---|---|---|---|---|---|---|
| African American | |||||||
| 1 | Bleyer (2010) (26) | N = 885; 43.2% male and 56.8% female | 43.5% African American; 56.5% White | ≥18 | Winston-Salem, North Carolina | Clinical; retrospective study | Cation-exchange column chromatography on an automated HPLC instrument (Variant II Turbo, Bio-Rad Laboratories). |
| 2 | Carson (2016); CARDIA study (27) | N = 2,692; 45.5% male and 54.5% female | 44% African American; 56% White | Mean (SD): 45.3 (3.6) | Minneapolis, Minnesota; Chicago, Illinois; Birmingham, Alabama; Oakland, California | Database analysis | Whole blood aliquot by ion-exchange HPLC using a Tosoh G7 (Tosoh Bioscience). |
| 3 | Cutrona (2015); FACHS (28) | N = 312; 100% female | 100% African American | 26–92; Mean (SD): 47 (7) | Ames, Iowa; Athens, Georgia | Database analysis | Whole blood aliquot by turbidimetric immunoinhibition (University of Iowa Clinical Pathology Laboratories). |
| 4 | Getaneh (2011); NHANES III and DIAMOND Study (29) | N = 16,056b; 48.1% male and 51.9% female | 4.3% Dominican; 28.9% Hispanic; 26.9% African American; 39.9% White | Range of mean ages: 38.2–63.3 | NHANES III: United States. DIAMOND: New York, New York |
Database analysis | Diamat HPLC from Bio-Rad Laboratories.c |
| 5 | Hivert (2019); DPP (30) | N = 2,658; 33% male and 67% female | 55.5% White; 20.2% African American; 17.0% Hispanic; 4.4% Asian; 2.9% American Indian | ≥25; Mean (SD): 50.7 (10.7) | 27 US clinical centersd | Clinical | Ion-exchange HPLC instrument (Variant; Bio-Rad Laboratories). |
| 6 | Homko (2012) (31) | N = 83; 7.2% male and 92.8% female | 100% African American | Mean (SD): 53 (10.4) | Philadelphia, Pennsylvania | Clinical | CDC-approved automated point-of-care analyzer (DCA 2000, Bayer Corporation): monoclonal antibody recognizes glycated N terminus of β chain of hemoglobin. |
| 7 | Meigs (2014); BACH Prediabetes Study (32) | N = 1,387; 37.4% male and 62.6% female | 27.3% African American; 29.6% Hispanic; 43.0% White | 34–87 | Boston, Massachusetts | Clinical | Tina-Quant HbA1c generation 2 assay with analytic measurement range of 3.4%–18% (Quest Diagnostics). |
| Afro-Caribbean | |||||||
| 8 | Exebio (2012) (33) | N = 128e | 100% Haitian American | ≥35 | Miami, Florida | Clinical | Whole blood with close tube sampling, in duplicate (coefficient of variation <1.7%), with Roche Tina Quant Second Generation A1c immunoassay method of Laboratory Corporation of America. |
| African | |||||||
| 9 | Briker (2019); The AIA Study (34) | N = 430; 65% male and 35% female | 100% African immigrants in the United States | Mean (SD): 38 (10) | Bethesda, Maryland | Clinical | NGSP-certified instruments: BioRad Laboratories Classic Variant (n = 32), Bio-Rad Laboratories Variant II (n = 158), and BioRad Laboratories D10 (n = 240) used sequentially by the NIH Clinical Center for HPLC. |
| 10 | Sumner 1 (2015); The AIA Study (35) | N = 216; 68% male and 32% female | 100% African immigrants in the United States | 20–64; mean (SD): 37 (10) | Bethesda, Maryland | Clinical | NGSP-certified instruments: Classic Variant, Variant II, and D10 for HPLC (Bio-Rad Laboratories). Whole blood samples in 90 participants analyzed by boronate affinity chromatography method on NGSP-certified Premier Hb9210 analyzer (Trinity Biotech). |
| 11 | Sumner 2 (2016); The AIA Study (36) | N = 236; 69% male and 31% female | 100% African immigrants in the United States | 20–64; Mean (SD): 39 (10) | Bethesda, Maryland | Clinical | NGSP-certified instruments: Variant II and D10 for HPLC (Bio-Rad Laboratories). |
| 12 | Sumner 3 (2016); The AIA Study (37) | N = 217; 69% male and 31% female | 100% African immigrants in the United States | 20–64; Mean (SD): 39 (10) | Bethesda, Maryland | Clinical | NGSP-certified instruments: Variant II and D10 for HPLC (Bio-Rad Laboratories). |
Abbreviations: AIA, Africans in America; BACH, Boston Area Community Health; CARDIA, Coronary Artery Risk Development in Young Adults; CDC, Centers for Disease Control and Prevention; DIAMOND, Diabetes Among Dominicans and Other Minorities in Northern Manhattan; DPP, Diabetes Prevention Program; FACHS, Family and Community Health Study; HPLC, high performance liquid chromatography; NHANES III, the third National Health and Nutrition Examination Survey; NIH, National Institutes of Health; NGSP, National Glycohemoglobin Standardization Program.
For all studies, White refers to Caucasian, Non-Hispanic White, and/or European White.
Participant data extracted from Table 1, “Sociodemographic Characteristics of Dominicans and the Third National Health and Nutrition Examination Survey Populations, Stratified by Hemoglobin A1c-Based Diabetes Diagnosis” (29).
Laboratory analysis data extracted from “Plan and Operation of the Third National Health and Nutrition Examination Survey, 1988–94. Series 1: Programs and Collection Procedures” (38).
Location data extracted from “The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes” (39).
Breakdown for sex/gender not available.
The population size of the studies varied from 83 to 16,056 participants, with the sex representation ranging from 69% male/31% female to 0% male/100% female (Table 1). The study cohorts consisted of 20.2% to 100% African descent populations. The overall age range across the different studies was 18 to 92 years and the mean age was between 37 and 64 years when reported (Table 1).
HbA1c laboratory analysis methods were high performance liquid chromatography (HPLC) for studies 1, 2, 4, 5, and 9 through 12 (26,27,29,30,34–37), or immunoassays for studies 3 and 6 through 8 (28,31–33) (Table 1).
The study designs included either clinical data collection (studies 1 and 5 through 12) (26,30–37) or analyses of established databases (studies 2 through 4) (27–29), with publication dates ranging from 2010 to 2019 (Table 1). Study 1 was a retrospective study of patients who underwent HbA1c testing from May 2008 to February 2009 (Table 1) (26). Study 2 was a cross cross-sectional analysis within the longitudinal Coronary Artery Risk Development in Young Adults (CARDIA) study (Table 1) (27).
In these studies, HbA1c performance was evaluated by comparing HbA1c results in African descent populations to HbA1c results in other ethnic groups (eg, White people) (studies 1, 2, 5, and 7) (26,27,30,32), evaluating HbA1c test results against the 2-hour OGTT, FPG, glycated plasma proteins test results, or previous diagnosis in the same participants (studies 3, 6, and 8–12) (28,31,33–37), or both (study 4) (29) (Table 2). Studies conducted among African American people showed that the HbA1c test almost always had a GRFP in this population. Studies 1, 2, 4, 5, and 7 demonstrated that HbA1c values were higher in African Americans when compared with Whites across a range of glycemic states (26,27,29,30,32). Additionally, Study 7 showed that HbA1c values were higher in African American people when compared with both White people and Hispanic people, leading to the potential of overdiagnosis of type 2 diabetes in African American people (32). Using OGTT as a standard test for diagnosis of glycemic status, studies 4 and 6 demonstrated that using HbA1c results in overdiagnosis of type 2 diabetes when HbA1c is 6.5% or higher (29,31). Study 3 showed that African American people may experience an overdiagnosis of prediabetes or type 2 diabetes at HbA1c of 5.7% to less than 6.5%; however, study 6 showed that an HbA1c cutoff of less than 5.7% does not eliminate the possibility of a type 2 diabetes diagnosis (28,31) (Table 2).
Table 2. Evaluation of Glycated Hemoglobin A1c (HbA1c) Performance: Greater Risk of False Positives Versus Greater Risk of False Negatives Among African Descent Populations Living in the United States, 2010–2019.
| Study | HbA1c Evaluation Method | Findings | Performance |
|---|---|---|---|
| African American | |||
| 1 | Compared with other ethnic groups (ie, White people) | Main finding: Higher HbA1c values for African American than for White people at all fasting glucose levels (26). |
Greater risk of false positives |
Additional findings:
| |||
| 2 | Compared with other ethnic groups (ie, White people) | Main finding: African American people without previous diagnosis of type 2 diabetes by OGTT had higher mean values of HbA1c than White people (β = 0.19% points; 95% CI = 0.14–0.24) (27). |
Greater risk of false positives |
| Additional finding: HbA1c values were compared for participants free of type 2 diabetes based on the OGTT. | |||
| 3 | Compared with other measures (ie, previous diagnosis)a | Main finding: Chronic financial strain increased sIL-6R, an inflammatory marker, and HbA1c (28). |
Greater risk of false positives |
| Additional finding: Although African American women had no previous prediabetes or type 2 diabetes diagnosis, 54% had HbA1c >5.7%. | |||
| 4 | Compared with other ethnic groups (ie, White people); Compared with other measures (ie, FPG and OGTT) | Main findings:
|
Greater risk of false positives |
| 5 | Compared with other ethnic groups (ie, White people) | Main finding: HbA1c was higher in African American (mean [SD], 6.2% [0.6]) than in White people (mean [SD], 5.8% [0.4]) (30). |
Greater risk of false positives |
Additional findings:
| |||
| 6 | Compared with other measures (ie, OGTT) | Main findings:
|
Greater risk of false positives at HbA1c ≥6.5% and greater risk of false negatives at HBA1c ≤5.6% |
Additional findings:
| |||
| 7 | Compared with other ethnic groups (ie, Hispanic and White people) | Main finding: Mean HbA1c levels were higher in African American (5.68%) than in Hispanic (5.57%) and White people (5.47%) (32). |
Greater risk of false positives |
Additional findings:
| |||
| Afro-Caribbean | |||
| 8 | Compared with other measures (ie, FPG) | Main findings:
|
Greater risk of false negatives |
| Additional finding: The area under the ROC curve for HbA1c as a diagnostic indicator of type 2 diabetes was 0.86. | |||
| African | |||
| 9 | Compared with other measures (ie, OGTT) | Main findings:
|
Greater risk of false negatives |
| Additional finding: Using HbA1c alone missed a diagnosis of type 2 diabetes in 60% of African people and a prediabetes diagnosis in 40% of African people (34). | |||
| 10 | Compared with other measures (ie, FPG and OGTT) | Main finding: Among subjects with IGT by OGTT, HbA1c ≥5.7% had sensitivity of 53%, 54%, and 47% for the total, normal, and variant hemoglobin groups, respectively (35). |
Greater risk of false negatives |
Additional findings:
| |||
| 11 | Compared with other measures (ie, OGTT and glycated albumin) | Main finding: Among subjects with prediabetes by OGTT, HbA1c of 5.7% to less than 6.5% had 37% sensitivity in nonobese African immigrants and 64% sensitivity in obese African immigrants (36). |
Greater risk of false negatives |
| Additional finding: For HbA1c of 5.7% to less than 6.5% combined with glycated albumin ≥13.77%, sensitivity increased to 72% for nonobese African immigrants. | |||
| 12 | Compared with other measures (ie, OGTT and glycated albumin) | Main findings:
|
Greater risk of false negatives |
Additional findings:
| |||
Abbreviations: OGTT, 2-hour oral glucose tolerance test; FPG, fasting plasma glucose; IGT, impaired glucose tolerance; PCA, principal component analysis; GRS, genetic risk score; SCT, sickle cell trait; ROC, receiver operating characteristic.
Exact temporality between the previous diagnosis and HbA1c testing was not provided within the study, with an estimate of less than 12 months extrapolated from the study design. Findings from this study may represent new onset diabetes. This provides a limitation in the conclusive findings for HbA1c performance in this study.
In the Afro-Caribbean population, HbA1c testing at the 6.5% or higher cutoff has a GRFN (33). Using FPG as a standard for diagnosis of type 2 diabetes, study 8 showed that more participants were correctly diagnosed as having type 2 diabetes if the cutoff was lowered to 6.26% or higher, suggesting that HbA1c values are generally lower in Afro-Caribbean people (Table 2).
The Africans in America studies 9 through 12 all showed that HbA1c has a GRFN in African people at the HbA1c cutoff of 5.7% to less than 6.5% for prediabetes and HbA1c cutoff of 6.5% or higher for type 2 diabetes (34–37). Using OGTT as a diagnostic standard for glycemic status, studies 9 through 12 demonstrated that using an HbA1c cutoff of 5.7% to less than 6.5% will lead to underdiagnosis of prediabetes in Africans. Additionally, study 9 showed that using an HbA1c cutoff of 6.5% or higher will lead to an underdiagnosis of type 2 diabetes in Africans (34) (Table 2).
Discussion
We assessed 12 studies that evaluated the ability of HbA1c to correctly identify African American, Afro-Caribbean, and African people with prediabetes or type 2 diabetes. Studies among African American people found that HbA1c of 5.7% to less than 6.5% or HbA1c of 6.5% or higher led to overdiagnosis. In one study of Afro-Caribbean people, HbA1c of 6.5% or higher had a greater risk of false negatives (GRFN). Among African people, HbA1c of 5.7% to less than 6.5% or HbA1c of 6.5% or higher led to greater risk of underdiagnosis.
Overdiagnosis of diabetes was likely among African American people in 3 ways. African American people had consistently higher HbA1c levels than White people regardless of glycemic status (26,27,29,30,32). Furthermore, half of normoglycemic African American people had HbA1c values greater than 5.7% (28); and lastly, African American people were more likely to be diagnosed with type 2 diabetes by HbA1c of 6.5% or higher alone but not by OGTT (29,31). Although study 6 did suggest a GRFN at HbA1c less than 5.7%, by misdiagnosing some participants as having normal glycemic status if their HbA1c was less than 5.7% (31), the finding is limited by the smaller sample size of 83 participants when compared with the other studies. This finding must be investigated further.
In Afro-Caribbean people, the HbA1c cutoff of 6.5% is likely to result in underdiagnosis of type 2 diabetes because study 8 showed that more participants were correctly diagnosed as having type 2 diabetes if the cutoff was lowered to 6.26% (33). However, this finding may not be generalizable to other Afro-Caribbean populations because of the smaller sample size and limitation of the study population to Haitian American people. Additionally, because only 1 study provided this conclusion, generalizability is further limited. For African people, underdiagnosis of prediabetes and type 2 diabetes is also likely at the standard HbA1c cutoffs because diagnosis was missed by HbA1c despite being detected by OGTT (34–37). The findings among African people hold true regardless of hemoglobin variant or obesity status (35,36).
Genetics are often thought to be responsible for the differences of HbA1c performance in African descent populations (24,40–43). In fact, genetic analysis in study 5 shows that the HbA1c difference was primarily because of the genomic principal component analysis (PCA) factor in African American people when compared with White people (30). The study demonstrated that the PCA factor was associated with increased HbA1c values in African American people. However, genetics do not fully explain HbA1c differences among African American people (44), because increases in HbA1c may be mediated by social determinants of health (eg, chronic financial strain as seen in study 3) or chronic inflammation (sIL-6R) (28,45). Additionally, G6PD variant or deficiency is often correlated with lower HbA1c values in various populations (40), especially in African American people and African people because of its higher prevalence in these groups (14,46,47). Similarly, the sickle cell trait is associated with lower HbA1c values in African descent populations (21,25). However, study 1 showed that the sickle cell trait may not actually correlate to changes in HbA1c values for African American people (26). Findings regarding associations of genetics with HbA1c are still being researched in this population. Research accounting for genetically linked HbA1c differences in Afro-Caribbean people is also lacking. Genetic polymorphisms between African American people and Haitian people have been researched and show that differences in the PPARGC1A gene will correlate to risk of type 2 diabetes in African American people as opposed to protective associations with type 2 diabetes in Haitian people, suggesting that other genetic associations may explain differences in diabetes for Haitian people (48). Although little research explains the role of genetics in HbA1c differences for Haitian people, one likely contributor to lower HbA1c values may be the G6PD variant because of its higher prevalence in populations of African descent (47). Nevertheless, opposing findings regarding the role of genetics in influencing HbA1c values (eg, PCA factor is associated with higher HbA1c whereas the sickle cell trait is associated with lower HbA1c) make it difficult to ascertain the overall impact genetics has in causing the differences in HbA1c that were found for the African descent populations and therefore require further evaluation.
Socioeconomic factors and health behaviors such as diet, smoking, and exercise may explain some differences in glycemic control and HbA1c values among the 3 groups. Higher income and educational attainment appear to decrease the odds of diabetes among African immigrants, whereas only higher education lowers the odds for African American people (5). Neither education nor income appear to affect diabetes risk among Afro-Caribbean people (5,49). Additionally, study 3 found that financial stress and chronic inflammation were associated with higher HbA1c. Chronic inflammation resulting from social and environmental stressors, including experiences of racism, correlate to higher HbA1c in nondiabetic adults (50). In terms of health behaviors, compared with African American people, African and Afro-Caribbean people are less likely to smoke. As African and Afro-Caribbean immigrants settle in the United States, they are affected by dietary acculturation often characterized by increased caloric intake and diets higher in refined carbohydrates, animal protein, fat, and sodium (5). Although diet may affect glycemic control, it is unlikely that diet explains the differences in HbA1c performance illustrated in this study. These socioeconomic factors highlight the diversity of experience within African descent groups, which is often overshadowed by perceived homogeneity of the “Black” experience in the United States. Since immigration to the United States presents unique socioeconomic circumstances that can affect factors like HbA1c (4), impacts of these circumstances are important to analyze distinctly from global concerns.
With these factors affecting HbA1c performance, results must be interpreted with caution. Some alternative diagnostic tests are suggested to aid or replace HbA1c for classification of glycemic status. For example, FPG in combination with HbA1c increases the sensitivity for type 2 diabetes diagnosis in African people (study 10) (35). A stronger relationship between HbA1c and FPG at higher FPG levels in most ethnic groups has been suggested as well (51). Study 8 suggests that FPG may be a better measure of glycemic status than HbA1c in Afro-Caribbean people (33). At the same time, studies 3, 6, and 9 through 12 suggest that OGTT more accurately measures glycemic status than HbA1c in both African American and African people (28,31,34–37). Comparisons between HbA1c and OGTT in Afro-Caribbean people are lacking and should be studied further.
Convenient nonfasting alternatives for type 2 diabetes testing are other glycated proteins (eg, glycated albumin, fructosamine, and other advanced glycation end products) either in combination with or in place of HbA1c (36,37,52–55). Although this approach is supported in multiethnic studies, these glycated proteins should be evaluated specifically in African descent groups.
Several limitations exist for the findings of our review. Despite constructing a comprehensive search, articles published in peer reviewed journals that were not indexed in PubMed, Scopus, and CINAHL may have been missed. The search contained nouns and adjectives as identification for African descent countries and regions of origin and HbA1c testing. However, study participant groups may be based on self or researcher categorization rather than actual region, country, or ethnic group of the participant. Findings must be interpreted with caution because of this subjective labeling within studies. Additionally, we did not use a specific protocol to evaluate the quality of the included studies, as this is not a part of scoping review methodologies and can increase risk of bias (56,57). Another limitation that must be considered is that time may pass between HbA1c testing and alternate testing in some studies and glycemic status of individuals can change in that time; this limitation will usually exist in this nature of clinical research methodology and therefore must be recognized when evaluating the conclusions from those studies.
According to our review process, there is only 1 study protocol in the United States that examines performance of diabetes screening tests among African immigrants to the United States (34–37). However, studies 9 through 12 demonstrate distinct comparisons within this cohort that illustrate significant conclusions about HbA1c performance. This is because the protocol is ongoing, and the number of participants increased over time. In turn, this also lends strength to the findings, because the similarity in protocol is balanced by the increasing diversity of the sample for each study design.
Finally, the lack of existing studies for Afro-Caribbean people in the United States presents a substantial limitation; our findings for this group must be interpreted cautiously. Further research is needed to understand the performance of HbA1c and evaluate alternate tests in place of the HbA1c in specific African descent populations, especially Afro-Caribbean people. Unique settings like New York City, where 32% of the African descent population is Afro-Caribbean and 4% is African (58), may serve as key locations for public health researchers to investigate type 2 diabetes screening and diagnostics.
Our review also has several strengths. In partnership with our institution’s research librarian, we tested several search constructions and selected the searches that provided the broadest selection within the scope of our topic. Additionally, we searched 3 databases without limiting article type or study designs on title and abstract review and had 2 reviewers independently screen the articles. This improved the selection of articles available for review and reduced selection bias. Finally, we were able to provide clear findings by constructing a label categorization scheme (GRFP/GRFN) that allowed for grouping of studies that used different comparative analytic and statistical methods to analyze HbA1c.
In African descent populations in the United States, the utility of HbA1c is limited in screening for glycemic status, determining care methods, assessing risk of type 2 diabetes complications, or analyzing health disparities. Current HbA1c cutoffs for prediabetes and type 2 diabetes may overestimate glycemic status in African American people and underestimate glycemic status in Afro-Caribbean and African people. Reasons for variations in HbA1c have been attributed to genetic, biochemical, and socioeconomic factors. Alternate testing such as OGTT, FPG, and other glycated blood proteins in place of or in combination with HbA1c may better assess glycemic status in African descent populations. Intraethnic HbA1c heterogeneity within the African descent groups must be recognized, and identification of more reliable type 2 diabetes screening and diagnostic tests is urgent.
Acknowledgments
This research did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector. The authors have no conflict of interest to report. No copyrighted materials, surveys, instruments, or tools were used in our study.
Institution where work was completed: Brooklyn College, City University of New York.
Appendix. Search Strings Used in a Scoping Review of HbA1c Performance in African Descent Populations in the United States With Normal Glucose Tolerance, Prediabetes, and Diabetes
| Database | Search String |
|---|---|
| PubMed | (africa[tiab] OR african[tiab] OR africans[tiab] OR “africa”[MeSH Terms] OR afro[tiab] OR black[tiab] OR “african continental ancestry group”[MeSH Terms] OR “african americans”[MeSH Terms] OR Angola[tiab] OR Angolan[tiab] OR Benin[tiab] OR Beninese[tiab] OR Botswana[tiab] OR Motswana[tiab] OR Batswana[tiab] OR “Burkina Faso”[tiab] OR Burkinabe[tiab] OR Burundi[tiab] OR Burundian[tiab] OR Cameroon[tiab] OR Cameroonian[tiab] OR “Cape Verde”[tiab] OR “Cape Verdean”[tiab] OR “Central African Republic”[tiab] OR “Central African”[tiab] OR Chad[tiab] OR Chadian[tiab] OR Comoros[tiab] OR Comorian[tiab] OR “Republic of the Congo”[tiab] OR Congolese[tiab] OR Djibouti[tiab] OR Djiboutian[tiab] OR “Equatorial Guinea”[tiab] OR “Equatorial Guinean”[tiab] OR Equatoguinean[tiab] OR Eritrea[tiab] OR Eritrean[tiab] OR Ethiopia[tiab] OR Ethiopian[tiab] OR Gabon[tiab] OR Gabonese[tiab] OR Gambia[tiab] OR Gambian[tiab] OR Ghana[tiab] OR Ghanaian[tiab] OR Guinea[tiab] OR Guinean[tiab] OR “Guinea-Bissau”[tiab] OR “Bissau-Guinean”[tiab] OR “Ivory Coast”[tiab] OR Ivorian[tiab] OR Kenya[tiab] OR Kenyan[tiab] OR Lesotho[tiab] OR Mosotho[tiab] OR Basotho[tiab] OR Liberia[tiab] OR Liberian[tiab] OR Madagascar[tiab] OR Malagasy[tiab] OR Malawi[tiab] OR Malawian[tiab] OR Mali[tiab] OR Malian[tiab] OR Mauritania[tiab] OR Mauritanian[tiab] OR Mauritius[tiab] OR Mauritian[tiab] OR Mozambique[tiab] OR Mozambican[tiab] OR Namibia[tiab] OR Namibian[tiab] OR Niger[tiab] OR Nigerien[tiab] OR Nigeria[tiab] OR Nigerian[tiab] OR Rwanda[tiab] OR Rwandan[tiab] OR “Sao Tome and Principe”[tiab] OR Senegal[tiab] OR Senegalese[tiab] OR Seychelles[tiab] OR Seychellois[tiab] OR “Sierra Leone”[tiab] OR “Sierra Leonean”[tiab] OR Somalia[tiab] OR Somalian[tiab] OR “South Africa”[tiab] OR “South African”[tiab] OR “South Sudan”[tiab] OR “South Sudanese”[tiab] OR Sudan[tiab] OR Sudanese[tiab] OR Swaziland[tiab] OR Swazi[tiab] OR Tanzania[tiab] OR Tanzanian[tiab] OR Togo[tiab] OR Uganda[tiab] OR Ugandan[tiab] OR Zambia[tiab] OR Zambian[tiab] OR Zimbabwe[tiab] OR Zimbabwean[tiab] OR anguilla[tiab] OR anguillian[tiab] OR “Antigua and Barbuda”[tiab] OR antiguan[tiab] OR barbudan[tiab] OR aruba[tiab] OR aruban[tiab] OR bahamas[tiab] OR bahamian[tiab] OR barbados[tiab] OR barbadian[tiab] OR belize[tiab] OR belizean[tiab] OR bermuda[tiab] OR bermudian[tiab] OR “British Virgin Islands”[tiab] OR caribbean[tiab] OR “Cayman Islands”[tiab] OR “Costa Rica”[tiab] OR “Costa Rican”[tiab] OR cuba[tiab] OR cuban[tiab] OR curacao[tiab] OR curacaoans[tiab] OR dominica[tiab] OR “Dominican Republic”[tiab] OR dominican[tiab] OR grenada[tiab] OR grenadine[tiab] OR guadeloupe[tiab] OR guadeloupean[tiab] OR guyana[tiab] OR guyanese[tiab] OR haiti[tiab] OR haitian[tiab] OR honduras[tiab] OR honduran[tiab] OR jamaica[tiab] OR jamaican[tiab] OR martinique[tiab] OR martiniquais[tiab] OR montserrat[tiab] OR montserratian[tiab] OR nevis[tiab] OR nicaragua[tiab] OR nicaraguan[tiab] OR panama[tiab] OR panamanian[tiab] OR “Puerto Rico”[tiab] OR “Puerto Rican”[tiab] OR “St. Barts”[tiab] OR “St. Christopher”[tiab] OR “St. Croix”[tiab] OR “St. Johns”[tiab] OR “St. Kitts and Nevis”[tiab] OR “St. Lucia”[tiab] OR “St. Martin”[tiab] OR “St. Thomas”[tiab] OR “St. Vincent”[tiab] OR vincentian[tiab] OR suriname[tiab] OR surinamese[tiab] OR “Trinidad and Tobago”[tiab] OR trinidadian[tiab] OR trini[tiab] OR tobagonian[tiab] OR “US Virgin Islands”[tiab] OR venezuela[tiab] OR venezuelan[tiab] OR “Virgin Islands”[tiab] OR “West Indies”[tiab] OR “West Indian”[tiab]) AND (“Glycated Hemoglobin A”[mesh] OR “hemoglobin A1c”[tiab] OR “hba1c”[tiab] OR “A1C”[tiab]) AND (“2000/01/01”[PDAT]: “2020/01/01”[PDAT]) |
| Scopus | (TITLE-ABS-KEY ((africa OR african OR africans OR afro OR black OR “african americans” OR blacks OR angola OR angolan OR benin OR beninese OR botswana OR motswana OR batswana OR “Burkina Faso” OR burkinabe OR burundi OR burundian OR cameroon OR cameroonian OR “Cape Verde” OR “Cape Verdean” OR “Central African Republic” OR “Central African” OR chad OR chadian OR comoros OR comorian OR “Republic of the Congo” OR congolese OR djibouti OR djiboutian OR “Equatorial Guinea” OR “Equatorial Guinean” OR equatoguinean OR eritrea OR eritrean OR ethiopia OR ethiopian OR gabon OR gabonese OR gambia OR gambian OR ghana OR ghanaian OR guinea OR guinean OR “Guinea-Bissau” OR “Bissau-Guinean” OR “Ivory Coast” OR ivorian OR kenya OR kenyan OR lesotho OR mosotho OR basotho OR liberia OR liberian OR madagascar OR malagasy OR malawi OR malawian OR mali OR malian OR mauritania OR mauritanian OR mauritius OR mauritian OR mozambique OR mozambican OR namibia OR namibian OR niger OR nigerien OR nigeria OR nigerian OR rwanda OR rwandan OR “Sao Tome and Principe” OR senegal OR senegalese OR seychelles OR seychellois OR “Sierra Leone” OR “Sierra Leonean” OR somalia OR somalian OR “South Africa” OR “South African” OR “South Sudan” OR “South Sudanese” OR sudan OR sudanese OR swaziland OR swazi OR tanzania OR tanzanian OR togo OR uganda OR ugandan OR zambia OR zambian OR zimbabwe OR zimbabwean OR anguilla OR anguillian OR “Antigua and Barbuda” OR antiguan OR barbudan OR aruba OR aruban OR bahamas OR bahamian OR barbados OR barbadian OR belize OR belizean OR bermuda OR bermudian OR “British Virgin Islands” OR caribbean OR “Cayman Islands” OR “Costa Rica” OR “Costa Rican” OR cuba OR cuban OR curacao OR curacaoans OR dominica OR “Dominican Republic” OR dominican OR grenada OR grenadine OR guadeloupe OR guadeloupean OR guyana OR guyanese OR haiti OR haitian OR honduras OR honduran OR jamaica OR jamaican OR martinique OR martiniquais OR montserrat OR montserratian OR nevis OR nicaragua OR nicaraguan OR panama OR panamanian OR “Puerto Rico” OR “Puerto Rican” OR “St. Barts” OR “St. Christopher” OR “St. Croix” OR “St. Johns” OR “St. Kitts and Nevis” OR “St. Lucia” OR “St. Martin” OR “St. Thomas” OR “St. Vincent” OR vincentian OR suriname OR surinamese OR “Trinidad and Tobago” OR trinidadian OR trini OR tobagonian OR “US Virgin Islands” OR venezuela OR venezuelan OR “Virgin Islands” OR “West Indies” OR “West Indian”)) AND DOCTYPE (ar OR re) AND PUBYEAR > 1999) AND (TITLE-ABS-KEY ((hba1c OR “glycosylated hemoglobin A” OR “glycated hemoglobin” OR “hemoglobin A1c” OR “glycated hemoglobin A”))) AND (LIMIT-TO (SUBJAREA, “MEDI”) OR LIMIT-TO (SUBJAREA, “NURS”) OR LIMIT-TO (SUBJAREA, “HEAL”) OR LIMIT-TO (SUBJAREA, “SOCI”)) AND (LIMIT-TO (LANGUAGE, “English”)) |
| Cumulative Index to Nursing and Allied Health Literature (CINAHL) | (hba1c OR glycosylated hemoglobin A OR glycated hemoglobin OR “hemoglobin A1c” OR “glycated hemoglobin A”) AND (africa OR african OR africans OR afro OR black OR african americans OR blacks OR caribbean OR Angola OR Angolan OR Benin OR Beninese OR Botswana OR Motswana OR Batswana OR “Burkina Faso” OR Burkinabe OR Burundi OR Burundian OR Cameroon OR Cameroonian OR “Cape Verde” OR “Cape Verdean” OR “Central African Republic” OR “Central African” OR Chad OR Chadian OR Comoros OR Comorian OR “Republic of the Congo” OR Congolese OR Djibouti OR Djiboutian OR “Equatorial Guinea” OR “Equatorial Guinean” OR Equatoguinean OR Eritrea OR Eritrean OR Ethiopia OR Ethiopian OR Gabon OR Gabonese OR Gambia OR Gambian OR Ghana OR Ghanaian OR Guinea OR Guinean OR “Guinea-Bissau” OR “Bissau-Guinean” OR “Ivory Coast” OR Ivorian OR Kenya OR Kenyan OR Lesotho OR Mosotho OR Basotho OR Liberia OR Liberian OR Madagascar OR Malagasy OR Malawi OR Malawian OR Mali OR Malian OR Mauritania OR Mauritanian OR Mauritius OR Mauritian OR Mozambique OR Mozambican OR Namibia OR Namibian OR Niger OR Nigerien OR Nigeria OR Nigerian OR Rwanda OR Rwandan OR “Sao Tome and Principe” OR Senegal OR Senegalese OR Seychelles OR Seychellois OR “Sierra Leone” OR “Sierra Leonean” OR Somalia OR Somalian OR “South Africa” OR “South African” OR “South Sudan” OR “South Sudanese” OR Sudan OR Sudanese OR Swaziland OR Swazi OR Tanzania OR Tanzanian OR Togo OR Uganda OR Ugandan OR Zambia OR Zambian OR Zimbabwe OR Zimbabwean OR anguilla OR anguillian OR “Antigua and Barbuda” OR antiguan OR barbudan OR aruba OR aruban OR bahamas OR bahamian OR barbados OR barbadian OR belize OR belizean OR bermuda OR bermudian OR “British Virgin Islands” OR caribbean OR “Cayman Islands” OR “Costa Rica” OR “Costa Rican” OR cuba OR cuban OR curacao OR curacaoans OR dominica OR “Dominican Republic” OR dominican OR grenada OR grenadine OR guadeloupe OR guadeloupean OR guyana OR guyanese OR haiti OR haitian OR honduras OR honduran OR jamaica OR jamaican OR martinique OR martiniquais OR montserrat OR montserratian OR nevis OR nicaragua OR nicaraguan OR panama OR panamanian OR “Puerto Rico” OR “Puerto Rican” OR “St. Barts” OR “St. Christopher” OR “St. Croix” OR “St. Johns” OR “St. Kitts and Nevis” OR “St. Lucia” OR “St. Martin” OR “St. Thomas” OR “St. Vincent” OR vincentian OR suriname OR surinamese OR “Trinidad and Tobago” OR trinidadian OR trini OR tobagonian OR “US Virgin Islands” OR venezuela OR venezuelan OR “Virgin Islands” OR “West Indies” OR “West Indian”) |
Footnotes
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions.
Suggested citation for this article: ZKhosla L, Bhat S, Fullington LA, Horlyck-Romanovsky MF. HbA1c Performance in African Descent Populations in the United States With Normal Glucose Tolerance, Prediabetes, or Diabetes: A Scoping Review. Prev Chronic Dis 2021;18:200365. DOI: https://doi.org/10.5888/pcd18.200365.
References
- 1. Mendola ND, Chen TC, Gu Q, Eberhardt MS, Saydah S. Prevalence of total, diagnosed, and undiagnosed diabetes among adults: United States, 2013–2016. NCHS Data Brief 2018;(319):1–8. [PubMed] [Google Scholar]
- 2. Anderson M. Rising share of the U.S. Black population is foreign born. Pew Research Center; 2015. https://www.pewsocialtrends.org/2015/04/09/a-rising-share-of-the-u-s-black-population-is-foreign-born/. Accessed July 20, 2020.
- 3. Anderson M, López G. Key facts about Black immigrants in the U.S. Pew Research Center; 2018. https://www.pewresearch.org/fact-tank/2018/01/24/key-facts-about-black-immigrants-in-the-u-s/. Accessed July 20, 2020.
- 4. Chung ST, Sumner AE. Diabetes: T2DM risk prediction in populations of African descent. Nat Rev Endocrinol 2016;12(3):131–2. 10.1038/nrendo.2016.2 [DOI] [PubMed] [Google Scholar]
- 5. Commodore-Mensah Y, Matthie N, Wells J, B Dunbar S, Himmelfarb CD, Cooper LA, et al. African Americans, African immigrants, and Afro-Caribbeans differ in social determinants of hypertension and diabetes: evidence from the National Health Interview Survey. J Racial Ethn Health Disparities 2018;5(5):995–1002. 10.1007/s40615-017-0446-x [DOI] [PubMed] [Google Scholar]
- 6. International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009;32(7):1327–34. 10.2337/dc09-9033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010;33(Suppl 1):S62–9. 10.2337/dc10-S062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Edelman D, Olsen MK, Dudley TK, Harris AC, Oddone EZ. Utility of hemoglobin A1c in predicting diabetes risk. J Gen Intern Med 2004;19(12):1175–80. 10.1111/j.1525-1497.2004.40178.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cavagnolli G, Pimentel AL, Freitas PA, Gross JL, Camargo JL. Effect of ethnicity on HbA1c levels in individuals without diabetes: systematic review and meta-analysis. PLoS One 2017;12(2):e0171315. 10.1371/journal.pone.0171315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bergenstal RM, Gal RL, Connor CG, Gubitosi-Klug R, Kruger D, Olson BA, et al. Racial differences in the relationship of glucose concentrations and hemoglobin A1c levels. Ann Intern Med 2017;167(2):95–102. 10.7326/M16-2596 [DOI] [PubMed] [Google Scholar]
- 11. Bloomgarden Z. Beyond HbA1c. J Diabetes 2017;9(12):1052–3. 10.1111/1753-0407.12590 [DOI] [PubMed] [Google Scholar]
- 12. Spanakis EK, Golden SH. Race/ethnic difference in diabetes and diabetic complications. Curr Diab Rep 2013;13(6):814–23. 10.1007/s11892-013-0421-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ziemer DC, Kolm P, Weintraub WS, Vaccarino V, Rhee MK, Twombly JG, et al. Glucose-independent, black–white differences in hemoglobin A1c levels: a cross-sectional analysis of 2 studies. Ann Intern Med 2010;152(12):770–7. 10.7326/0003-4819-152-12-201006150-00004 [DOI] [PubMed] [Google Scholar]
- 14. Paterson AD. HbA1c for type 2 diabetes diagnosis in Africans and African Americans: personalized medicine NOW! PLoS Med 2017;14(9):e1002384. 10.1371/journal.pmed.1002384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA 2015;314(10):1021–9. 10.1001/jama.2015.10029 [DOI] [PubMed] [Google Scholar]
- 16. Chung ST, Sumner AE. Diabetes: T2DM risk prediction in populations of African descent. Nat Rev Endocrinol 2016;12(3):131–2. 10.1038/nrendo.2016.2 [DOI] [PubMed] [Google Scholar]
- 17. Mugeni R, Aduwo JY, Briker SM, Hormenu T, Sumner AE, Horlyck-Romanovsky MF. A review of diabetes prediction equations in African descent populations. Front Endocrinol (Lausanne) 2019;10:663. 10.3389/fendo.2019.00663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cox ME, Edelman D. Tests for screening and diagnosis of type 2 diabetes. Clin Diabetes 2009;27(4):132–8. 10.2337/diaclin.27.4.132 [DOI] [Google Scholar]
- 19. Leal S, Soto-Rowen M. Usefulness of point-of-care testing in the treatment of diabetes in an underserved population. J Diabetes Sci Technol 2009;3(4):672–6. 10.1177/193229680900300409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bode BW, Irvin BR, Pierce JA, Allen M, Clark AL. Advances in hemoglobin A1c point of care technology. J Diabetes Sci Technol 2007;1(3):405–11. 10.1177/193229680700100314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cavagnolli G, Comerlato J, Comerlato C, Renz PB, Gross JL, Camargo JL. HbA1c measurement for the diagnosis of diabetes: is it enough? Diabet Med 2011;28(1):31–5. 10.1111/j.1464-5491.2010.03159.x [DOI] [PubMed] [Google Scholar]
- 22. Kramer CK, Araneta MR, Barrett-Connor E. A1C and diabetes diagnosis: the Rancho Bernardo Study. Diabetes Care 2010;33(1):101–3. 10.2337/dc09-1366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Huang Z, Liu Y, Mao Y, Chen W, Xiao Z, Yu Y. Relationship between glycated haemoglobin concentration and erythrocyte survival in type 2 diabetes mellitus determined by a modified carbon monoxide breath test. J Breath Res 2018;12(2):026004. 10.1088/1752-7163/aa9081 [DOI] [PubMed] [Google Scholar]
- 24. Lacy ME, Wellenius GA, Sumner AE, Correa A, Carnethon MR, Liem RI, et al. Association of sickle cell trait with hemoglobin A1c in African Americans. JAMA 2017;317(5):507–15. 10.1001/jama.2016.21035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Little RR, Roberts WL. A review of variant hemoglobins interfering with hemoglobin A1c measurement. J Diabetes Sci Technol 2009;3(3):446–51. 10.1177/193229680900300307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bleyer AJ, Vidya S, Sujata L, Russell GB, Akinnifesi D, Hire D, et al. The impact of sickle cell trait on glycated haemoglobin in diabetes mellitus. Diabet Med 2010;27(9):1012–6. 10.1111/j.1464-5491.2010.03050.x [DOI] [PubMed] [Google Scholar]
- 27. Carson AP, Muntner P, Selvin E, Carnethon MR, Li X, Gross MD, et al. Do glycemic marker levels vary by race? Differing results from a cross-sectional analysis of individuals with and without diagnosed diabetes. BMJ Open Diabetes Res Care 2016;4(1):e000213. 10.1136/bmjdrc-2016-000213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cutrona CE, Abraham WT, Russell DW, Beach SRH, Gibbons FX, Gerrard M, et al. Financial strain, inflammatory factors, and haemoglobin A1c levels in African American women. Br J Health Psychol 2015;20(3):662–79. 10.1111/bjhp.12120 [DOI] [PubMed] [Google Scholar]
- 29. Getaneh A, Andres R, Brillon DJ, Findley SE. Hemoglobin A1C criterion for diabetes diagnosis among Hispanic and non-Hispanic populations. Endocr Pract 2011;17(2):210–7. 10.4158/EP10119.OR [DOI] [PubMed] [Google Scholar]
- 30. Hivert MF, Christophi CA, Jablonski KA, Edelstein SL, Kahn SE, Golden SH, et al. Genetic ancestry markers and difference in A1c between African American and White in the Diabetes Prevention Program. J Clin Endocrinol Metab 2019;104(2):328–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Homko CJ, Zamora LC, Kerper MM, Mozzoli M, Kresge K, Boden G. A single A1C >= 6.5% accurately identifies type 2 diabetes/impaired glucose tolerance in African Americans. J Prim Care Community Health 2012;3(4):235–8. 10.1177/2150131911435526 [DOI] [PubMed] [Google Scholar]
- 32. Meigs JB, Grant RW, Piccolo R, López L, Florez JC, Porneala B, et al. Association of African genetic ancestry with fasting glucose and HbA1c levels in non-diabetic individuals: the Boston Area Community Health (BACH) Prediabetes Study. Diabetologia 2014;57(9):1850–8. 10.1007/s00125-014-3301-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Exebio JC, Zarini GG, Vaccaro JA, Exebio C, Huffman FG. Use of hemoglobin A1C to detect Haitian-Americans with undiagnosed type 2 diabetes. Arq Bras Endocrinol Metabol 2012;56(7):449–55. 10.1590/S0004-27302012000700007 [DOI] [PubMed] [Google Scholar]
- 34. Briker SM, Aduwo JY, Mugeni R, Horlyck-Romanovsky MF, DuBose CW, Mabundo LS, et al. A1C underperforms as a diagnostic test in Africans even in the absence of nutritional deficiencies, anemia and hemoglobinopathies: insight from the Africans in America Study. Front Endocrinol (Lausanne) 2019;10:533. 10.3389/fendo.2019.00533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sumner AE, Thoreson CK, O’Connor MY, Ricks M, Chung ST, Tulloch-Reid MK, et al. Detection of abnormal glucose tolerance in Africans is improved by combining A1C with fasting glucose: the Africans in America Study. Diabetes Care 2015;38(2):213–9. 10.2337/dc14-1179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sumner AE, Duong MT, Bingham BA, Aldana PC, Ricks M, Mabundo LS, et al. Glycated albumin identifies prediabetes not detected by hemoglobin A1C: the Africans in America Study. Clin Chem 2016;62(11):1524–32. 10.1373/clinchem.2016.261255 [DOI] [PubMed] [Google Scholar]
- 37. Sumner AE, Duong MT, Aldana PC, Ricks M, Tulloch-Reid MK, Lozier JN, et al. A1C combined with glycated albumin improves detection of prediabetes in Africans: the Africans in America Study. Diabetes Care 2016;39(2):271–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Plan and operation of the Third National Health and Nutrition Examination Survey, 1988–94. Series 1: programs and collection procedures. Vital Health Stat 1 1994;(32):1–407. [PubMed] [Google Scholar]
- 39. The Diabetes Prevention Program Research Group. The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care 1999;22(4):623–34. 10.2337/diacare.22.4.623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wheeler E, Leong A, Liu CT, Hivert MF, Strawbridge RJ, Podmore C, et al. Impact of common genetic determinants of hemoglobin A1c on type 2 diabetes risk and diagnosis in ancestrally diverse populations: a transethnic genome-wide meta-analysis. PLoS Med 2017;14(9):e1002383. 10.1371/journal.pmed.1002383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Franklin CS, Aulchenko YS, Huffman JE, Vitart V, Hayward C, Polašek O, et al. The TCF7L2 diabetes risk variant is associated with HbA1c levels: a genome-wide association meta-analysis. Ann Hum Genet 2010;74(6):471–8. 10.1111/j.1469-1809.2010.00607.x [DOI] [PubMed] [Google Scholar]
- 42. Paré G, Chasman DI, Parker AN, Nathan DM, Miletich JP, Zee RY, et al. Novel association of HK1 with glycated hemoglobin in a non-diabetic population: a genome-wide evaluation of 14,618 participants in the Women’s Genome Health Study. PLoS Genet 2008;4(12):e1000312. 10.1371/journal.pgen.1000312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Soranzo N, Sanna S, Wheeler E, Gieger C, Radke D, Dupuis J, et al. Common variants at 10 genomic loci influence hemoglobin A1c levels via glycemic and nonglycemic pathways. Diabetes 2010;59(12):3229–39. Erratum in: Diabetes 2011;60(3):1050–1. 10.2337/db10-0502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cohen RM, Franco RS, Smith EP, Higgins JM. When HbA1c and blood glucose do not match: how much is determined by race, by genetics, by differences in mean red blood cell age? J Clin Endocrinol Metab 2019;104(3):707–10. 10.1210/jc.2018-02409 [DOI] [PubMed] [Google Scholar]
- 45. Maruthur NM, Kao WHL, Clark JM, Brancati FL, Cheng CY, Pankow JS, et al. Does genetic ancestry explain higher values of glycated hemoglobin in African Americans? Diabetes 2011;60(9):2434–8. 10.2337/db11-0319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sarnowski C, Hivert MF. Impact of genetic determinants of HbA1c on type 2 diabetes risk and diagnosis. Curr Diab Rep 2018;18(8):52. 10.1007/s11892-018-1022-4 [DOI] [PubMed] [Google Scholar]
- 47. Sarnowski C, Leong A, Raffield LM, Wu P, de Vries PS, DiCorpo D, et al. Impact of rare and common genetic variants on diabetes diagnosis by hemoglobin A1c in multi-ancestry cohorts: the Trans-Omics for Precision Medicine Program. Am J Hum Genet 2019;105(4):706–18. 10.1016/j.ajhg.2019.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cheema AK, Li T, Liuzzi JP, Zarini GG, Dorak MT, Huffman FG. Genetic associations of PPARGC1A with type 2 diabetes: differences among populations with African origins. J Diabetes Res 2015;2015:921274. 10.1155/2015/921274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bidulescu A, Ferguson TS, Hambleton I, Younger-Coleman N, Francis D, Bennett N, et al. Educational health disparities in hypertension and diabetes mellitus among African descent populations in the Caribbean and the USA: a comparative analysis from the Spanish town cohort (Jamaica) and the Jackson heart study (USA). Int J Equity Health 2017;16(1):33–9. 10.1186/s12939-017-0527-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Liu S, Hempe JM, McCarter RJ, Li S, Fonseca VA. Association between inflammation and biological variation in hemoglobin A1c in U.S. nondiabetic adults. J Clin Endocrinol Metab 2015;100(6):2364–71. 10.1210/jc.2014-4454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Guan X, Zheng L, Sun G, Guo X, Li Y, Song H, et al. The changing relationship between HbA1c and FPG according to different FPG ranges. J Endocrinol Invest 2016;39(5):523–8. 10.1007/s40618-015-0389-1 [DOI] [PubMed] [Google Scholar]
- 52. Yazdanpanah S, Rabiee M, Tahriri M, Abdolrahim M, Rajab A, Jazayeri HE, et al. Evaluation of glycated albumin (GA) and GA/HbA1c ratio for diagnosis of diabetes and glycemic control: a comprehensive review. Crit Rev Clin Lab Sci 2017;54(4):219–32. 10.1080/10408363.2017.1299684 [DOI] [PubMed] [Google Scholar]
- 53. Welsh KJ, Kirkman MS, Sacks DB. Role of glycated proteins in the diagnosis and management of diabetes: research gaps and future directions. Diabetes Care 2016;39(8):1299–306. 10.2337/dc15-2727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. George JA, Erasmus RT. Haemoglobin A1c or glycated albumin for diagnosis and monitoring diabetes: an African perspective. Indian J Clin Biochem 2018;33(3):255–61. 10.1007/s12291-018-0755-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Loomis SJ, Li M, Maruthur NM, Baldridge AS, North KE, Mei H, et al. Genome-wide association study of serum fructosamine and glycated albumin in adults without diagnosed diabetes: results from the Atherosclerosis Risk in Communities Study. Diabetes 2018;67(8):1684–96. 10.2337/db17-1362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Tricco AC, Lillie E, Zarin W, O’Brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol 2016;16(1):15. 10.1186/s12874-016-0116-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5(1):69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lobo A, Salvo J, Alvarez J, Hurley D, Levin W, Sears W, et al. The newest New Yorkers: characteristics of the city’s foreign-born population. New York (NY): NYC Office of Immigrant Affairs; 2013. https://www1.nyc.gov/assets/planning/download/pdf/data-maps/nyc-population/nny2013/nny_2013.pdf. Accessed July 20, 2020.


