Abstract
BACKGROUND & AIMS:
We estimated the prevalence of social determinants of health (SDH, food insecurity and social support) in adults with inflammatory bowel diseases (IBD) in the United States and evaluated associations with financial toxicity and healthcare use.
METHODS:
In the National Health Interview Survey 2015, we identified adults with IBD and estimated the prevalence of food insecurity and/or lack of social support. We evaluated associations with financial toxicity (financial hardship due to medical bills, personal and health-related financial distress, cost-related medication nonadherence, healthcare affordability) and emergency department use.
RESULTS:
Of estimated 3.1 million adults with IBD in the US, 42% or estimated 1,277,215 patients with IBD reported at least one negative SDH, with 12% reporting both food insecurity and lack of social support. On multivariable analysis adjusting for age, sex, race, family income and comorbidities, patients with food insecurity were significantly more likely to experience financial hardship due to medical bills (odds ratio [OR], 3.31; 95% CI, 1.48–7.39), financial distress (OR, 6.92; 95% CI, 2.28–21.0) and cost-related medication non-adherence (OR, 8.07; 95% CI, 3.16–20.6). Similarly, patients with inadequate social support were significantly more likely to experience financial hardship due to medical bills (OR, 2.98; 95% CI, 1.56–5.67), financial distress (OR, 3.05; 95% CI, 1.64–5.67) and cost-related medication non-adherence (OR, 2.71; 95% CI, 1.10–6.66). Food insecurity and/or lack of social support was not associated with increased risk of emergency department use.
CONCLUSIONS:
In an analysis of data from the National Health Interview Survey 2015, we found that 1 in 8 patients with IBD have food insecurity and lack social support, which is associated with higher financial toxicity. Patients with IBD should be assessed for SDH to tailor healthcare delivery and improve population health.
Keywords: societal factors, social environment, hunger, poverty, insurance
INTRODUCTION
Inflammatory bowel diseases (IBD) are associated with significant healthcare costs estimated to exceed $800 billion over a lifetime in the United States (US).1 Unplanned healthcare utilization, including emergency department (ED) visits and hospitalizations, and pharmacotherapy are primary drivers of cost in IBD care.2–5 Prior studies evaluating factors associated with unplanned healthcare utilization have focused on patient-specific clinical and behavioral characteristics such as disease severity, presence of depression and anxiety, surgery, etc.6 However, social environment plays a critical part in determining individual health and healthcare utilization. Social determinants of health (SDH) represent the entirety of social, economic and physical circumstances in which individuals are born and live that critically shape and impact health.7, 8 These conditions inherently create societal stratification and are responsible for health disparities among different groups of people based on social and economic class, education, and ethnicity. Prior studies have used surrogates such as race/ethnicity, insurance status and socioeconomic status/income to infer SDH in IBD.9–14 However, there has been very limited direct assessment of key SDH, particularly food insecurity and social and neighborhood support, in patients with IBD.
Food insecurity refers to limited or uncertain access to nutritionally adequate, safe, and acceptable foods. Nationally, the prevalence of food insecurity is approximately 11%, with wide geographic and socioeconomic variability, and it has been associated with depression, diabetes, cardiovascular disease, etc.15 Similarly, lack of social networks and social cohesion and living in unsafe neighborhoods have been associated with adverse healthcare outcomes.15–17 However, it is unclear how these SDH associate with financial toxicity and healthcare utilization in patients with IBD. A thorough understanding of the prevalence and impact of these SDH is important to facilitate optimal management of patients with IBD within their socioeconomic context.18
Hence, we performed a survey analysis in the National Health Interview Survey (NHIS) 2015, to estimate US national prevalence of two important SDH, food insecurity and lack of social support, and their association with healthcare-related financial toxicity (financial hardship due to medical bills, cost-related medication non-adherence [CRN], personal and/or health-related financial distress and healthcare affordability) and ED utilization.
METHODS
Data Source
We used the NHIS 2015 to estimate the national prevalence of SDH in patients with IBD.19 The NHIS is an annual household survey compiled by the National Center for Health Statistics/Center for Disease Control & Prevention that incorporate complex, multistage sampling to provide estimates on noninstitutionalized, U.S. population and draw a sample of nearly 35,000 households made up of 87,500 individuals. The NHIS collects data through questionnaires delivered by trained interviewers and collects information on demographic characteristics of each included family and information on health conditions and access to and use of health services from ≥1 randomly selected member adult from each family. NHIS data are publicly available as deidentified data from the National Center for Health Statistics, so this study was exempt from the institutional review board committee.
Study population
Patients were identified as having a diagnosis of IBD based on an affirmative response to the question, “Have you ever been told by a doctor or other health professional that you had Crohn’s disease or ulcerative colitis?” Our patient population was restricted to adults (age 18 or older). Based on these criteria, 454 patients had a self-reported diagnosis of IBD which represents an estimated 3.1 million adults with IBD nationally or 1.3% of US adults. Baseline demographics of this cohort has been described elsewhere.20 NHIS 2015 data are publicly available as deidentified data, so this study was exempt from the institutional review board committee.
Definitions
Our primary components of SDH were food insecurity and social support.
Food insecurity:
Food insecurity was defined based on the U.S. Department of Agriculture Economic Research Service’s 10-item questionnaire, which focuses on being worried about food running out, inability to afford a balanced meal, cutting portions or skipping meals due to costs, etc.21 Based on this, patients were classified as food secure (score 0 to 2), low food security (score 3 to 5), and very low food security (score 6 to 10).
(Lack of) Social support:
Lack of social support was defined based on negative response to any of the following questions: (1) people in the neighborhood to help each other, (2) people in the neighborhood to count on, (3) people in the neighborhood to trust, or (4) neighborhood is close-knit; or being worried about paying rent/mortgage/housing costs.
Outcomes
We evaluated the association between food insecurity and/or lack of social support and measures of financial toxicity. Financial toxicity includes objective financial burden, such as medication nonadherence as a result of high costs and subjective financial distress, such as changes in treatment-related decision making based primarily on cost. It has been associated with negative effects on healthcare spending and patients’ quality of life and health outcomes. Financial toxicity was assessed across the following four domains.22–24
Financial hardship due to medical bills:
Patients were identified as having financial hardships due to medical bills if they (or anyone in their family) reported having problems paying medical bills in the past 12 months and/or currently having medical bills being paid off over time. For patients who reported problems paying medical bills, they were additionally asked if they had any medical bills they were unable to pay at all. Based on this, financial hardships due to medical bills was graded into 3 mutually exclusive categories: (1) no financial hardship from medical bills, (2) financial hardship from medical bills but able to pay, and (3) financial hardships and unable to pay bills at all.
Financial distress:
Financial distress was derived from five questions regarding the level of worry (4-point Likert scale, ranging from “not worried at all” to “very worried”) concerning personal and/or health-related financial matters including health-related financial distress: (1) ability to pay medical costs of illness/accident, (2) ability to pay medical costs of usual healthcare, (3) inability to afford prescription medicine in the past 12 months; and personal financial distress: (4) maintaining standard of living, and (5) inability to pay monthly bills.
Cost-related medication non-adherence:
CRN was defined based on self-reported behaviors in the last 12 months to save money: (1) skipping medication doses, (2) taking less medicine, or (3) delayed filling a prescription. In addition, we assessed whether patients had pursued cost-reducing strategies for prescription medications based on the following questions: during the past 12 months: (1) “have you asked your doctor for lower cost medication to save money?”, (2) “have you bought prescription drugs from another country to save money?” and (3) “have you used alternative therapies to save money?”
Healthcare affordability.
Inability to afford healthcare was defined based on (1) inability to afford to see a specialist, or (2) inability to afford follow-up care, within the past 12 months.
Besides financial toxicity, we evaluated the association between food insecurity and/or lack of social support and ED visits in the previous 12 months.
Covariates
We collected data on the following covariates: age, sex, body mass index (BMI), marital status, education, employment history in the past 12 months, family size, family income (calculated based on family income as a percentage of the federal poverty limit from the Census Bureau: high-income [≥400%], middle-income [200% to 400%], and low-income [<200%]), race/ethnicity, insurance status, geographical region, smoking status, and self-reported medical comorbidities (coronary artery disease, diabetes mellitus and chronic obstructive pulmonary disease).
Statistical analysis
To evaluate the association between SDH and outcomes, we classified individuals with IBD into three categories: being food secure and having social support, being either food insecure or lacking social support, or being both food insecure and lacking social support. We accounted for the complex survey design of the NHIS by using survey-specific descriptive statistics to provide weighted national estimates of food insecurity and/or lack of social support, and corresponding prevalence of financial toxicity across domains of SDH, with accompanying 95% confidence intervals (CI). We used Rao-Scott x2 test to compare categorical variables and survey-specific linear regression to compare continuous variables. Unadjusted and adjusted survey-specific logistic regression models were used to assess association between SDH factors and financial toxicity across the 4 domains, and ED visits and reported as odds ratio (OR) and accompanying 95% CI. All statistical analyses were performed with survey-specific tools using Stata, version 14 (StataCorp, College Station, Texas). The level of statistical significance was defined as a p-value <0.05.
RESULTS
Food insecurity
Approximately 14% of US adults with IBD, corresponding to estimated 422,614 patients (95% CI 282,767 – 562,461), were food insecure, of whom half reported very low food security (Table 1). Overall, 19% patients were worried food would run out before they got money to buy more, 16% reported food did not last before they had money to get more, and 13% could not afford to eat balanced meals (eFigure 1). Approximately 60% patients with food insecurity were receiving Supplemental Nutrition Assistance Program. Overall, 44% patients without high school education, 37% patients in poor-low income families, and 28% patients with private insurance were food insecure (Supplementary Table 1). Patients with IBD had 69% higher odds of food insecurity (95% CI, 1.15–2.49) as compared to patients without IBD after adjusting for comorbidities, age, sex, race, education, income and insurance status (Supplementary Table 2).
Table 1.
Characteristics of adults with IBD with varying degrees of food insecurity.
| Variable | Food secure, weighted % | Low food security, weighted % | Very low food security, weighted % | p-value |
|---|---|---|---|---|
| Sample, n | 381 | 35 | 34 | |
| Weighted sample, n (weighted %) | 2,650,943 (86%) | 222,833 (7%) | 192,097 (7%) | |
| Average Age, y | 53.1 (50.7 – 55.4) | 51.7 (43.2 – 60.3) | 42.3 (36.1 – 48.4) | 0.01 |
| Average BMI | 29.8 (27.8 – 31.7) | 27.1 (23.1 – 31.2) | 29.9 (24.1 – 35.8) | 0.75 |
| Female | 1,493,276 (56%) | 137,399 (62%) | 135,951 (68%) | 0.63 |
| Married | 1,458,549 (55%) | 93,322 (42%) | 48,607 (24%) | 0.07 |
| Less than high school education | 117,824 (4%) | 52,893 (24%) | 40,054 (20%) | <0.01 |
| Family size | ||||
| 1 | 594,341 (22%) | 58,404 (26%) | 64,250 (32%) | 0.22 |
| 2 | 1,058,787 (40%) | 38,572 (17%) | 80,732 (40%) | |
| ≥3 | 997,815 (38%) | 125,856 (56%) | 54,800 (27%) | |
| Minor children residing in the home | 719,996 (27%) | 81,423 (37%) | 56,598 (28%) | 0.72 |
| Family Income | ||||
| Poor/low income | 609,726 (24%) | 187,395 (85%) | 177,213 (89%) | <0.01 |
| Middle/high income | 1,908,761 (76%) | 33,329 (15%) | 22,644 (11%) | |
| Supplemental Nutrition Assistance Program (SNAP) | ||||
| Proportion receiving SNAP | 325,801 (12%) | 120,842 (54%) | 131,596 (66%) | <0.01 |
| Race/ethnicity | ||||
| Non-Hispanic white | 2,086,653 (80%) | 131,614 (60%) | 141,932 (71%) | 0.07 |
| Black | 137,980 (5%) | 33,986 (15%) | 16,108 (8%) | |
| Asian | 124,677 (5%) | 528 (1 %) | 0% | |
| Hispanic | 259,006 (10%) | 53,705 (24%) | 41,808 (21 %) | |
| Insurance status | ||||
| No insurance | 73,166 (3%) | 15,687 (7%) | 39,177 (20%) | <0.01 |
| Private | 805,091 (30%) | 173,565 (78%) | 142,963 (72%) | |
| Non-private | 1,772,686 (67%) | 33,581 (15%) | 17,641 (9%) | |
| Region | ||||
| Northeast | 519,320 (20%) | 48,890 (22%) | 27,850 (14%) | 0.48 |
| Midwest | 629,069 (24%) | 20,100 (9%) | 32,944 (16%) | |
| South | 944,266 (36%) | 122,046 (55%) | 103,866 (52%) | |
| West | 558,023 (21 %) | 31,798 (14%) | 35,142 (18%) | |
| Smoking status | ||||
| Never smoker | 1,448,379 (55%) | 110,342 (50%) | 86,663 (43%) | 0.02 |
| Current smoker | 339,766 (13%) | 65,563 (29%) | 79,593 (40%) | |
| Former smoker | 862,137 (33%) | 46,895 (21 %) | 33,475 (17%) | |
| Comorbidities | ||||
| Coronary heart disease | 208,364 (8%) | 9,270 (4%) | 21,017 (11%) | 0.60 |
| Diabetes mellitus | 341,441 (13%) | 57,847 (26%) | 6,593 (3%) | 0.06 |
| Chronic obstructive pulmonary disease | 186,096 (7%) | 28,790 (13%) | 36,360 (18%) | 0.11 |
| Emergency Department Visits | ||||
| Emergency Department Visits | 704,824 (27%) | 78,780 (35%) | 137,105 (72%) | <0.01 |
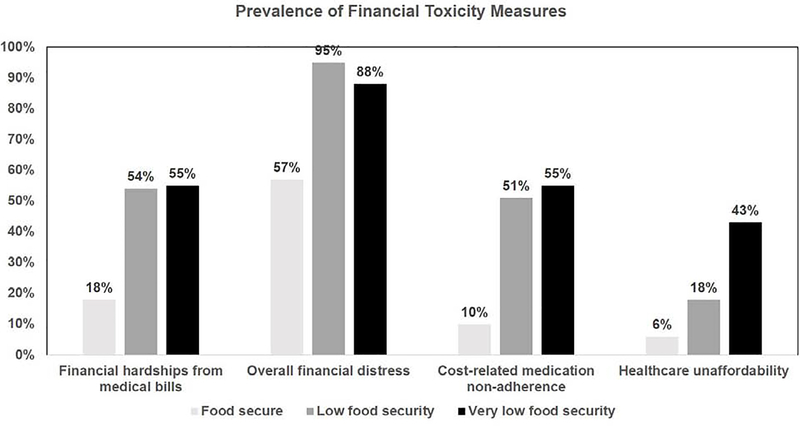
The prevalence of financial toxicity was significantly higher in patients with food insecurity, across all domains. Approximately 55% patients with very low food security experienced financial hardship due to medical bills, 43% were unable to afford healthcare, 55% experienced CRN, and 88% reports personal and/or healthcare-related financial distress (Figure 1). Food insecurity was associated with a higher burden of ED visits in the preceding 12 months (very low food security vs. low food security vs. food secure: 72% vs. 35% vs. 27%, p<0.01). On multivariable analysis, after adjusting for age, sex, race, family income and comorbidities, we observed that food insecurity was independently associated with higher risk of financial hardship due to medical bills (adjusted OR, 3.31; 95% CI, 1.48–7.39), financial distress (adjusted OR, 6.92; 95% CI, 2.28–21.0), CRN (adjusted OR, 8.07; 95% CI, 3.16–20.6), but not lack of affordable health care (adjusted OR, 2.63; 95% CI, 0.92–7.56) and ED visits (adjusted OR, 1.87; 95% CI, 0.78–4.46) (Supplementary Table 3).
Figure 1.
Prevalence of measures of financial toxicity by levels of food insecurity
(Lack of) Social support
Approximately 53% of patients, corresponding to 1,640,590 patients (95% CI, 1,446,707 – 1,835,707), reported lack of social support (with and without food insecurity) (Table 1, eFigure 2). Overall, 73% patients without high school education, 75% patients in poor-low income families, and 64% patients with private insurance lacked social support (Supplementary Table 4). Black (70%) and Hispanic (83%) patients were more likely to lack adequate social support compared to non-Hispanic White (47%) and Asian (51%) patients. IBD was not independently associated with lack of adequate social support (adjusted OR, 1.09; 95% CI, 0.85–1.40) on multivariable analysis (Supplementary Table 5).
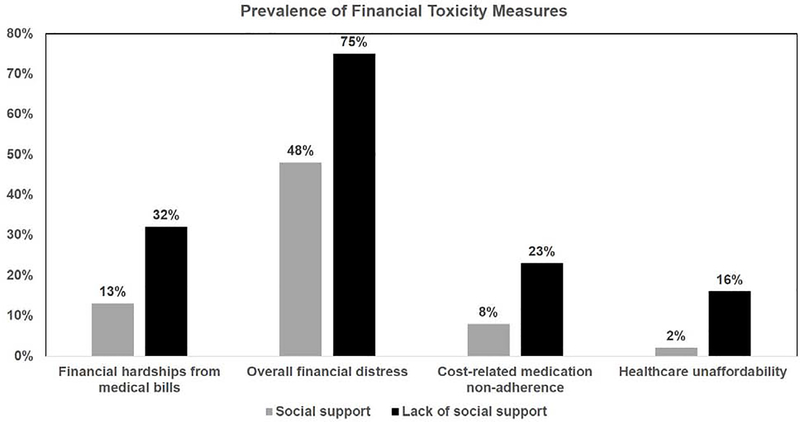
The prevalence of financial toxicity was significantly higher in patients with lack of social support, across all domains (Figure 2). On multivariable analysis, we observed that lack of social support was independently associated with higher risk of financial hardship due to medical bills (adjusted OR, 2.98; 95% CI, 1.56–5.67), financial distress (adjusted OR, 3.05; 95% CI, 1.64–5.67), CRN (adjusted OR, 2.71; 95% CI, 1.10–6.66) and lack of affordable health care (adjusted OR, 5.12; 95% CI, 1.57–16.8), but not ED visits (adjusted OR, 1.26; 95% CI, 0.70–2.25) (Supplementary Table 6).
Figure 2.
Prevalence of measures of financial toxicity by social support
Social Determinants of Health and Adverse Outcomes
An estimated 42% or 1,277,215 patients [95% CI, 1,078,084 –1,476,345]) nationally reported one negative SDH factor (either food insecure or lack of social support), while approximately 12% (378,194 patients [95% CI, 241,247 – 514,652]) were food insecure and lacked social support (Table 3, Supplementary Table 7).
Table 3.
Characteristics of adults with IBD with varying degrees of negative social determinants of health.
| Variable | Food secure and adequate social support, weighted % | Food insecure OR lack of social support, weighted % | Food insecure AND lack of social support, weighted % | p-value |
|---|---|---|---|---|
| Sample, n | 196 | 198 | 60 | |
| Weighted sample, n (weighted %) | 1,431,888 (46%) | 1,277,215 (42%) | 378,194 (12%) | |
| Average Age, y | 50.3 (47.3 – 53.3) | 55.6 (52.6 – 58.7) | 47.8 (41.9 – 53.8) | 0.67 |
| Average BMI | 29.8 (30.0 – 32.6) | 30.2 (27.5 – 32.9) | 26.7 (24.2 – 29.2) | 0.41 |
| Female | 780,809 (55%) | 757,133 (59%) | 234,556 (62%) | 0.70 |
| Married | 821,188 (57%) | 637,330 (50%) | 141,898 (38%) | 0.17 |
| Less than high school education | 62,143 (4%) | 74,654 (6%) | 84,654 (22%) | <0.01 |
| Family size | ||||
| 1 | 375,012 (26%) | 248,035 (19%) | 103,020 (27%) | 0.60 |
| 2 | 553,711 (39%) | 545,484 (40%) | 113,534 (30%) | |
| ≥3 | 503,166 (35%) | 513,696 (40%) | 161,602 (43%) | |
| Minor children residing in the home | 368,282 (26%) | 359,281 (28%) | 135,053 (36%) | 0.59 |
| Family Income | ||||
| Poor/low income | 230,631 (16%) | 430,186 (37%) | 324,138 (86%) | <0.01 |
| Middle/high income | 1,177,374 (84%) | 735,630 (63%) | 51,979(14%) | |
| Supplemental Nutrition Assistance Program (SNAP) | ||||
| Proportion receiving SNAP | 100,375 (7%) | 260,041 (20%) | 228,618 (60%) | <0.01 |
| Race/ethnicity | ||||
| Non-Hispanic white | 1,248,069 (89%) | 871,000 (69%) | 252,160 (67%) | <0.01 |
| Black | 52,097 (4%) | 92,890 (7%) | 43,203 (12%) | |
| Asian | 61,812 (4%) | 62,934 (5%) | 0% | |
| Hispanic | 46,042 (3%) | 231,847 (18%) | 79,462 (21%) | |
| Insurance status | ||||
| No insurance | 15,321 (1%) | 66,032 (5%) | 54,838 (15%) | <0.01 |
| Private | 379,594 (27%) | 472,697 (37%) | 275,060 (73%) | |
| Non-private | 1,036,974 (72%) | 738,613 (58%) | 48,295 (13%) | |
| Region | ||||
| Northeast | 338,642 (24%) | 184,430 (14%) | 74,126 (20%) | 0.21 |
| Midwest | 314,299 (22%) | 320,070 (25%) | 47,615 (13%) | |
| South | 527,508 (37%) | 447,919 (35%) | 207,553 (55%) | |
| West | 251,869 (18%) | 324,796 (25%) | 48,901 (13%) | |
| Smoking status | ||||
| Never smoker | 843,277 (59%) | 636,432 (50%) | 171,431 (45%) | <0.02 |
| Current smoker | 176,756 (12%) | 187,111 (15%) | 129,083 (34%) | |
| Former smoker | 411,048 (29%) | 453,664 (35%) | 77,624 (21%) | |
| Comorbidities | ||||
| Coronary heart disease | 109,539 (8%) | 98,856 (8%) | 30,293 (8%) | 0.99 |
| Diabetes mellitus | 151,637 (11%) | 201,928 (16%) | 60,208 (16%) | 0.46 |
| Chronic obstructive pulmonary disease | 99,659 (7%) | 99,495 (8%) | 52,115 (14%) | 0.27 |
| Emergency room visits | ||||
| Proportion with emergency room visits | 358,263 (26%) | 382,940 (30%) | 187,609 (50%) | 0.043 |
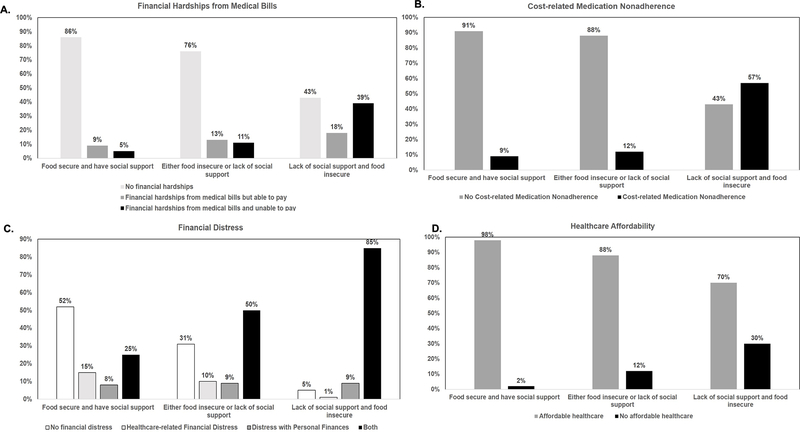
The prevalence of financial toxicity was significantly higher in patients with both negative SDH factors, across all domains (Figures 3A–D). On multivariable analyses, compared to patients who were food secure and with adequate social support, patients reporting food insecurity and lack of social support were significantly more likely to experience financial hardships due to medical bills (adjusted OR, 9.06; 95% CI, 2.70–30.35), financial distress (adjusted OR, 37.88; 95% CI, 8.43–170.13), CRN (adjusted OR, 12.28; 95% CI, 2.43–62.15) and lack affordable healthcare (adjusted OR, 12.23; 95% CI, 1.55–96.79) (Supplementary Table 8). Patients who were food insecure and lacked social support were significantly more likely have had ED visits in the preceding 12 months (both negative SDH factors vs. one negative SDH factor vs. none: 50% vs. 30% vs. 26%, p=0.04) (Table 3). However, on multivariate logistic regression, patients with both negative SDH factors did not have higher risk of ED visits as compared with patients who were food secure and had adequate social support (adjusted OR, 1.74; 95% CI, 0.63–4.80) (Supplementary Table 8).
Figure 3.
Prevalence of measures of financial toxicity by burden of negative social determinants of health (no negative SDH vs. only 1 negative SDH vs. 2 negative SDH): (A) financial hardship due to medical bills, (B) cost-related medication non-adherence, (C) personal and/or health-related financial distress, and (D) healthcare affordability
DISCUSSION
Health outcomes are driven by a wide array of factors, including underlying genetics, health behaviors, social and environmental factors, and health care. In a nationally representative sample of non-institutionalized US adults with IBD, we focused on the interaction of two understudied SDH, food insecurity and lack of social support, and their impact on financial toxicity and unplanned healthcare utilization. We observed that approximately one in seven adults with IBD was food insecure, one in two adults lacked adequate social support, and one in eight was at a significant social disadvantage with food insecurity and lacking social support. Patients who were both food insecure and lacked adequate social support experienced significant financial toxicity across multiple domains. This was closely associated with cost-related nonadherence to medications, resulting in maladaptive treatment-coping strategy. These findings have important implications for value-based healthcare and population health management, since these social determinants are not readily modifiable at an individual level and require policy and societal interventions to increase access to nutritionally adequate and safe foods access in socially acceptable ways, and to provide a safe social network for patients.18,25, 26
Prior studies have addressed the concepts of SDH in IBD using surrogates such as race/ethnicity, insurance status, income and education level.9–14 These studies have demonstrated lower utilization of advanced medical and surgical therapies, inferior healthcare access, lower adherence to therapy and inferior IBD-related outcomes in low-income patients, those without insurance, and African American patients. However, they have not been able to examine the complex interplay of social and economic factors that influence health outcomes. In our analysis, we observed that uninsured patients, African-American and Hispanic patients, patients belonging to lower income strata and those without high school education had higher prevalence of negative SDH factors. However, rates of social disadvantage were also considerable in other groups with >37–49% patients with private or non-private insurance, Asians or Caucasians, with at least high school education and with middle to high-income families, reporting food insecurity or lack of adequate social support.
There is increasing patient and provider interest in dietary management of IBD.27, 28 However, most specialized diets are expensive.29 We observed that one in seven patients with IBD may not have access to nutritionally adequate, safe, and acceptable foods. It is imperative that providers recognize the problem of food insecurity when making dietary recommendations for patients with IBD. Similarly, patients with IBD frequently rely on family, friends and other caregivers to provide long-term medical and non-medical support.10, 30 A good social support system can significantly improve patients’ quality of life and positively impact self-management.31 We identified that approximately one in two adults with IBD have an inadequate social support system. Addressing the patient’s social support system may improve individual and population health in IBD.
With high prevalence of negative SDH, across various sociocultural and economic groups, it’s impact on financial toxicity and unplanned healthcare utilization, and evolution of health systems towards whole-person care and population health, our findings strongly support systematically screening for SDH in all patients with IBD.26, 32 Typical domains to cover within SDH include economic stability, food insecurity, neighborhood and physical environment, community and social context, and perceptions of healthcare, health-related behaviors, and access to and utilization of healthcare. Whether routine screening for SDH translates into improved health outcomes is unclear.33 While healthcare providers appreciate the connection between social factors and health outcomes, they have been reticent to ask about these factors due to limited confidence in their capacity to address the patients’ social needs. As health systems evolve, by choice or by mandate, the capacity of healthcare providers to respond to patients’ vital social needs will improve with anticipated improvement in population health.34,35 Evolving value-based payment models such as shared savings programs, insert social determinants into the financial equation facing healthcare systems, by prioritizing outcomes like 30-day readmissions and value-based payment reform. New programs, such as the Accountable Health Communities program by the Centers for Medicare and Medicaid services, explore bridges created between social services and the healthcare sector. As a low prevalence, high-cost condition, with very wide variability in quality and costs of healthcare, patients with IBD are likely to benefit from systematic efforts to measure, and respond to, negative SDH.
Although our study is the first to provide insights into the national burden and impact of key SDH on financial toxicity and healthcare utilizations in adult patients with IBD, it is not without limitations. First, NHIS relies on self-reported diagnoses of IBD, without adequate validation. However, it forms the basis for Centers for Disease Control official estimates of the burden of IBD in the US. Second, we are not able to evaluate the effect of IBD disease activity and complications on SDH, financial toxicity and vice versa. Third, due to the cross-sectional nature of the survey design, we are unable to infer a causal association between SDH and financial toxicity and ED visits. Finally, there may be an over-representation of older patients with IBD in our study limiting the generalizability of our findings on the prevalence and impact of SDH in younger patients with IBD.
In conclusion, patients with IBD have high prevalence of food insecurity and lack of adequate social support, and this negatively associates with high financial toxicity and unplanned healthcare utilization. Population health management strategies should incorporate universal screening for SDH, and empower healthcare teams to address social needs to improve the overall quality of healthcare delivery, and effectively manage clinical and financial risks.
Supplementary Material
eFigure 1. Response to different questions assessing food insecurity in adults with IBD from the National Health Interview Survey 2015
eFigure 2. (Lack of) social support in adults with IBD from the National Health Interview Survey 2015
Table 2.
Characteristics of adults with IBD with or without adequate social support.
| Variable | Social Support, weighted % | Inadequate Social Support, weighted % | p-value |
|---|---|---|---|
| Sample, n | 197 | 257 | |
| Weighted sample, n (weighted %) | 1,446,707 (47%) | 1,640,590 (53%) | |
| Average Age, y | 50.2 (47.2 – 53.1) | 54.0 (51.1 – 56.9) | 0.08 |
| Average BMI | 29.8 (27.0 – 32.6) | 29.4 (27.2 – 31.5) | 0.75 |
| Female | 799,595 (55%) | 972,870 (59%) | 0.54 |
| Married | 821,151 (57%) | 779,280 (48%) | 0.14 |
| Less than high school education | 59,458 (4%) | 162,088 (10%) | 0.03 |
| Family size | |||
| 1 | 372,527 (26%) | 353,383 (22%) | 0.66 |
| 2 | 554,812 (38%) | 627,854 (38%) | |
| ≥3 | 519,223 (36%) | 659,353 (40%) | |
| Minor children residing in the home | 363,702 (25%) | 498,903 (30%) | 0.42 |
| Income | |||
| Poor/low income | 244,366 (17%) | 740,265 (49%) | <0.01 |
| Middle/high income | 1,181,339 (83%) | 783,608 (51%) | |
| Race/ethnicity | |||
| Non-Hispanic white | 1,245,504 (88%) | 1,125,448 (70%) | <0.01 |
| Black | 56,051 (4%) | 132,120 (8%) | |
| Asian | 61,742 (4%) | 63,469 (4%) | |
| Hispanic | 59,323 (4%) | 298,079 (18%) | |
| Insurance status | |||
| No insurance | 7,234 (1%) | 128,786 (8%) | <0.01 |
| Private | 402,329 (29%) | 724,813 (44%) | |
| Non-private | 1,036,999 (71%) | 786,827 (48%) | |
| Region | |||
| Northeast | 337,662 (23%) | 259,705 (16%) | 0.50 |
| Midwest | 316,829 (22%) | 365,195 (22%) | |
| South | 524,576 (36%) | 658,369 (40%) | |
| West | 267,786 (19%) | 357,320 (22%) | |
| Smoking status | |||
| Never smoker | 857,646 (59%) | 793,505 (48%) | 0.13 |
| Current smoker | 174,537 (12%) | 318,419 (19%) | |
| Former smoker | 413,856 (29%) | 528,566 (32%) | |
| Comorbidities | |||
| Coronary heart disease | 109,516 (8%) | 129,114 (8%) | 0.93 |
| Diabetes mellitus | 147,853 (10%) | 265,940 (16%) | 0.18 |
| Chronic obstructive pulmonary disease | 102,427 (7%) | 148,801 (9%) | 0.43 |
| Emergency Department Visit | |||
| Emergency department visit | 322,130 (24%) | 555,808 (34%) | 0.10 |
WHAT YOU NEED TO KNOW.
Background:
This study estimated the prevalence of social determinants of health (SDH, food insecurity and social support) in adults with inflammatory bowel diseases (IBD) in the United States and evaluated associations with financial toxicity (such as financial hardship due to medical bills, medication nonadherence due to high costs) and healthcare use.
Findings:
An analysis of data from the National Health Interview Survey 2015 found that 1 in 8 patients with IBD have food insecurity and lack social support, which is associated with higher financial toxicity.
Implications for Patient Care:
Patients with IBD should be assessed for SDH to personalize healthcare delivery and improve population health.
Acknowledgments
Conflicts of Interest:
NHN – None to declare
RK – None to declare
LOM – None to declare
WJS – research grants from Atlantic Healthcare Limited, Amgen, Genentech, Gilead Sciences, Abbvie, Janssen, Takeda, Lilly, Celgene/Receptos, Pfizer, Prometheus Laboratories (owned by Precision IBD); consulting fees from Abbvie, Allergan, Amgen, Arena Pharmaceuticals, Avexegen Therapeutics, BeiGene, Boehringer Ingelheim, Celgene, Celltrion, Conatus, Cosmo, Escalier Biosciences, Ferring, Forbion, Genentech, Gilead Sciences, Gossamer Bio, Incyte, Janssen, Kyowa Kirin Pharmaceutical Research, Landos Biopharma, Lilly, Oppilan Pharma, Otsuka, Pfizer, Precision IBD (owns Prometheus Laboratories), Progenity, Prometheus Laboratories (owned by Precision IBD), Reistone, Ritter Pharmaceuticals, Robarts Clinical Trials (owned by Health Academic Research Trust, HART), Series Therapeutics, Shire, Sienna Biopharmaceuticals, Sigmoid Biotechnologies, Sterna Biologicals, Sublimity Therapeutics, Takeda, Theravance Biopharma, Tigenix, Tillotts Pharma, UCB Pharma, Ventyx Biosciences, Vimalan Biosciences, Vivelix Pharmaceuticals; and stock or stock options from BeiGene, Escalier Biosciences, Gossamer Bio, Oppilan Pharma, Precision IBD (owns Prometheus Laboratories), Progenity, Ritter Pharmaceuticals, Ventyx Biosciences, Vimalan Biosciences. Spouse: Opthotech - consultant, stock options; Progenity - consultant, stock; Oppilan Pharma - employee, stock options; Escalier Biosciences - employee, stock options; Precision IBD (also owns Prometheus Laboratories) - employee, stock options; Ventyx Biosciences – employee, stock options; Vimalan Biosciences – employee, stock options.
SS – research grants from AbbVie, Janssen
Disclosures: Dr. Nguyen is supported by NIH/NIDDK (T32DK007202). Dr. Sandborn is partially supported by NIDDK-funded San Diego Digestive Diseases Research Center (P30 DK120515). Dr. Singh is supported by NIH/NIDDK (K23DK117058), ACG Junior Faculty Development Award and the Crohn’s and Colitis Foundation Career Development Award (#404614).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Lichtenstein GR, Shahabi A, Seabury SA, et al. Lifetime Economic Burden of Crohn’s Disease and Ulcerative Colitis by Age at Diagnosis. Clin Gastroenterol Hepatol 2020;18:889–897. [DOI] [PubMed] [Google Scholar]
- 2.Dieleman JL, Cao J, Chapin A, et al. US Health Care Spending by Payer and Health Condition, 1996–2016. JAMA 2020;323:863–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park KT, Ehrlich OG, Allen JI, et al. The Cost of Inflammatory Bowel Disease: An Initiative From the Crohn’s & Colitis Foundation. Inflamm Bowel Dis 2020;26:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peery AF, Crockett SD, Murphy CC, et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2018. Gastroenterology 2019;156:254–272 e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen NH, Khera R, Ohno-Machado L, et al. Annual Burden and Costs of Hospitalization for High-Need, High-Cost Patients With Chronic Gastrointestinal and Liver Diseases. Clin Gastroenterol Hepatol 2018;16:1284–1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nguyen NH, Koola J, Dulai PS, et al. Rate of Risk Factors for and Interventions to Reduce Hospital Readmission in Patients With Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol 2019; doi: 10.1016/j.cgh.2019.08.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health 2011;32:381–98. [DOI] [PubMed] [Google Scholar]
- 8.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep 2014;129 Suppl 2:19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernstein CN, Kraut A, Blanchard JF, et al. The relationship between inflammatory bowel disease and socioeconomic variables. Am J Gastroenterol 2001;96:2117–25. [DOI] [PubMed] [Google Scholar]
- 10.Sewell JL, Velayos FS. Systematic review: The role of race and socioeconomic factors on IBD healthcare delivery and effectiveness. Inflamm Bowel Dis 2013;19:627–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Basu D, Lopez I, Kulkarni A, et al. Impact of race and ethnicity on inflammatory bowel disease. Am J Gastroenterol 2005;100:2254–61. [DOI] [PubMed] [Google Scholar]
- 12.Nahon S, Lahmek P, Saas C, et al. Socioeconomic and psychological factors associated with nonadherence to treatment in inflammatory bowel disease patients: results of the ISSEO survey. Inflamm Bowel Dis 2011;17:1270–6. [DOI] [PubMed] [Google Scholar]
- 13.Nguyen GC, Bayless TM, Powe NR, et al. Race and health insurance are predictors of hospitalized Crohn’s disease patients undergoing bowel resection. Inflamm Bowel Dis 2007;13:1408–16. [DOI] [PubMed] [Google Scholar]
- 14.Nguyen GC, LaVeist TA, Harris ML, et al. Racial disparities in utilization of specialist care and medications in inflammatory bowel disease. Am J Gastroenterol 2010;105:2202–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gundersen C, Ziliak JP. Food Insecurity And Health Outcomes. Health Aff (Millwood) 2015;34:1830–9. [DOI] [PubMed] [Google Scholar]
- 16.De Jesus M, Puleo E, Shelton RC, et al. Associations between perceived social environment and neighborhood safety: Health implications. Health Place 2010;16:1007–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Slonim-Nevo V, Sarid O, Friger M, et al. Effect of Social Support on Psychological Distress and Disease Activity in Inflammatory Bowel Disease Patients. Inflamm Bowel Dis 2018;24:1389–1400. [DOI] [PubMed] [Google Scholar]
- 18.Figueroa JF, Frakt AB, Jha AK. Addressing Social Determinants of Health: Time for a Polysocial Risk Score. JAMA 2020; doi: 10.1001/jama.2020.2436 [DOI] [PubMed] [Google Scholar]
- 19.Parsons VL, Moriarity C, Jonas K, et al. Design and estimation for the national health interview survey, 2006–2015. Vital Health Stat 2 2014:1–53. [PubMed] [Google Scholar]
- 20.Dahlhamer JM, Zammitti EP, Ward BW, et al. Prevalence of Inflammatory Bowel Disease Among Adults Aged ≥18 Years — United States, 2015. MMWR Morb Mortal Wkly Rep 2016; 65:1166–1169. [DOI] [PubMed] [Google Scholar]
- 21.National Research Counci. Research Opportunities Concerning the Causes and Consequences of Child Food Insecurity and Hunger: A Workshop Summary. Washington (DC), 2013. [PubMed] [Google Scholar]
- 22.Caraballo C, Valero-Elizondo J, Khera R, et al. Burden and Consequences of Financial Hardship From Medical Bills Among Nonelderly Adults With Diabetes Mellitus in the United States. Circ Cardiovasc Qual Outcomes 2020;13:e006139. [DOI] [PubMed] [Google Scholar]
- 23.Khera R, Valero-Elizondo J, Das SR, et al. Cost-Related Medication Nonadherence in Adults With Atherosclerotic Cardiovascular Disease in the United States, 2013 to 2017. Circulation 2019;140:2067–2075. [DOI] [PubMed] [Google Scholar]
- 24.Valero-Elizondo J, Khera R, Saxena A, et al. Financial Hardship From Medical Bills Among Nonelderly U.S. Adults With Atherosclerotic Cardiovascular Disease. J Am Coll Cardiol 2019;73:727–732. [DOI] [PubMed] [Google Scholar]
- 25.Joynt Maddox KE, McClellan MB. Toward Evidence-Based Policy Making to Reduce Wasteful Health Care Spending. JAMA 2019; doi: 10.1001/jama.2019.13977.. [DOI] [PubMed] [Google Scholar]
- 26.Maani N, Galea S. The Role of Physicians in Addressing Social Determinants of Health. JAMA 2020; doi: 10.1001/jama.2020.1637. [DOI] [PubMed] [Google Scholar]
- 27.Levine A, Rhodes JM, Lindsay JO, et al. Dietary Guidance for Patients With Inflammatory Bowel Disease from the International Organization for the Study of Inflammatory Bowel Disease. Clin Gastroenterol Hepatol 2020;18:1381–1392. [DOI] [PubMed] [Google Scholar]
- 28.Sasson AN, Ananthakrishnan AN, Raman M. Diet in Treatment of Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol 2019; doi: 10.1016/j.cgh.2019.11.054. [DOI] [PubMed] [Google Scholar]
- 29.Lee AR, Wolf RL, Lebwohl B, et al. Persistent Economic Burden of the Gluten Free Diet. Nutrients 2019;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shukla R, Thakur E, Bradford A, et al. Caregiver Burden in Adults With Inflammatory Bowel Disease. Clin Gastroenterol Hepatol 2018;16:7–15. [DOI] [PubMed] [Google Scholar]
- 31.Kamp KJ, West P, Holmstrom A, et al. Systematic Review of Social Support on Psychological Symptoms and Self-Management Behaviors Among Adults With Inflammatory Bowel Disease. J Nurs Scholarsh 2019;51:380–389. [DOI] [PubMed] [Google Scholar]
- 32.Dulai PS, Singh S, Ohno-Machado L, et al. Population Health Management for Inflammatory Bowel Disease. Gastroenterology 2018;154:37–45. [DOI] [PubMed] [Google Scholar]
- 33.Andermann A Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Rev 2018;39:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chaiyachati KH, Grande DT, Aysola J. Health systems tackling social determinants of health: promises, pitfalls, and opportunities of current policies. Am J Manag Care 2016;22:e393–e394. [PubMed] [Google Scholar]
- 35.Young GJ, Chou CH, Alexander J, et al. Provision of community benefits by tax-exempt U.S. hospitals. N Engl J Med 2013;368:1519–27. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Response to different questions assessing food insecurity in adults with IBD from the National Health Interview Survey 2015
eFigure 2. (Lack of) social support in adults with IBD from the National Health Interview Survey 2015