Abstract
Purpose
In some countries, telephone-based support is one of the key services used for supporting patients with cancer. However, there is a lack of research on the efficacy of this method in Iran. This study aimed to evaluate the effects of tele-nursing on supportive care needs (SCNs) of patients with cancer undergoing chemotherapy.
Methods
This randomized controlled trial was conducted on 60 patients with cancer undergoing chemotherapy who were randomly assigned and allocated to two groups, an intervention group and a control group. Patients’ SCNs were assessed in the baseline, and 1 and 2 months after commencement of the intervention using the SCNs Survey -Short Form 34. The data were analyzed through descriptive statistics, t-test, and repeated measure test, by SPSS version 16.
Results
There were no significant statistical differences in the mean score of dimensions and total SCNs between the two groups in baseline (p˃0.05). However, the results showed that the mean score of dimensions and total SCNs in the intervention group were significantly less than the control group, after the intervention (p˂0.05).
Conclusions
Telephone-based support is an effective method to address and reduce SCNs of patients with cancer undergoing chemotherapy through increasing access to support for this population especially who may be in rural and remote settings. During the COVID_19 pandemic and given the vulnerability of patients with cancer, telephone support can be used to avoid unnecessary visits to hospitals and reduced the risk of transmitting the virus to the patients.
Trial registration number
IRCT20170404033216N1
Keywords: Cancer, Supportive care needs, Tele-nursing, Quality of life
Introduction
Cancer is a chronic disease with recurrent and long-lasting stages [1]. According to global cancer statistics, about 110,000 cases of cancer occurred and about 56,000 patients died in Iran in 2018. The prevalence rate of cancer was 248.392 patients [2]. Depending on the type of cancer, its stage, and the patient’s condition, there are many types of cancer treatment such as surgery, radiotherapy, immunotherapy, and chemotherapy. Chemotherapy is still used as the primary or sole treatment for cancer. This treatment may damage or kill any rapidly dividing cell, tumor or normal cells. Damage to healthy cells leads to side effects including diarrhea, low blood pressure, drowsiness, constipation, nausea and vomiting, hair loss, fatigue, muscle aches, weight changes, and skin problems [3, 4].
However, most patients and their caregivers have little knowledge about the side effects associated with these cancer treatments, and how to manage them. Therefore, they incur high costs for frequent visits to hospital or their treatment provider due to a lack of information and knowledge about common or serious side effects, stopping the treatment, and worsening of symptoms [5]. These issues may be due to a lack of available and active supportive care for patient counseling and education which requires the effective teamwork of health care providers, especially nurses and access to the best available resources and technologies [6, 7].
Human resilience is about learning the knowledge and skills to cope with any life-altering situation. Dealing with a potentially life-limiting illness is one situation which poses an increased need for help and education. Patient education has emerged as one of the key roles of nurses in providing health care services [8, 9]. More than 70% of health care team are nurses who play an important role in educating clients because, they spend more time with patients. There is ample opportunity to educate them and evaluate the effectiveness of patient education [10]. Health care systems are providing better-quality educational programs for patient education [11], and educating patients with cancer can lead to achieving improved treatment outcomes and reduced the side effects of treatment (i.e., fatigue, nausea, vomiting and pain, anxiety, and depression). The significance of education and supporting patients at every stage of the cancer journey is well known. According to Dodd’s study on patients with cancer, the patients who were educated to deal with the side effects of chemotherapy and radiotherapy started self-care earlier than the patients who had not received education [12]. Due to the complexity of cancer treatment and patients’ knowledge level, various methods and educational materials are needed for patient education. The challenge therefore is to identify patients’ needs and select appropriate instructional methods and technology for different age ranges, level of literacy, and emotional and social characteristics to meet their needs [13].
Telephone communication is one of the educational and follow-up methods used for cancer care by nurses [14]. This communication is an effective method for providing low-cost supportive care and improving the relationship between patient and professionals, and removing time and space barriers to access to cancer care. Telephone communication reduces the number of hospitalizations, improves patient education, promotes patients’ self-management, and ultimately improves patient care quality.
The finding of a systematic review evaluating the efficacy of telephone interventions on heart failure, Clark et al. reported a 21% reduction in readmission rates and a 20% reduction in mortality of patients [15]. Another study showed that the patients were satisfied with asking questions during a phone conversation and sending a short message, which led to reduced medical expenses and improved patients’ quality of life [16]. A telephone communication allows savings in time, financial burdens imposed on patients due to frequent traveling for visiting health care professionals, and it reduces medical expenses. In addition, the number of referrals to hospitals, emergency wards and, consequently, hospital costs and personnel workload are also reduced. The telephone call, also, helps the patients and their families participate actively in self-care, caring for the patient at home and contact health care professionals as needed 24 h a day, 7 days a week, and patients do not require any special skills and access to certain facilities (such as the internet) [17].
Therefore, telephone communication can be an appropriate option in providing supportive care and education by nurses for patients with cancer who have many unmet needs. Despite the importance of providing supportive care services for patients with cancer and their families, there are no systematic structures for providing supportive care in Iran. Although the usefulness of phone supports is clear, the efficiency of this method needs to be investigated in Iran due to cultural and social differences between countries and patients’ preference for face-to-face communication with professionals. This study aimed to evaluate the effects of tele-nursing on supportive care needs (SCNs) of patients with cancer undergoing chemotherapy.
Method
Design and participants
The study was a randomized controlled trial. The participants were patients with cancer who were undergoing chemotherapy and referred to a cancer hospital or clinic affiliated to Arak University of Medical Sciences, Arak, Iran. According to the study by Javadi et al., and with a type-I error of 0.05, and a power of 0.80, the sample size for each study group was estimated to be 30 and 60 in total [18]. The inclusion criteria were patients 18–80 years of age with a diagnosis of cancer from an oncologist, suffering from no metastasis, and who were undergoing chemotherapy, had awareness of the diagnosis, had access to a landline or cell phone, who had no hearing and speech impairments, and no mental illness. After signing a consent form, patients were randomly assigned to either an intervention or a control group through block randomization. A computerized random number generator performed the randomization of the assignment. Researchers began the randomization by assigning an identification number to each subject. Patients were excluded if they experienced unexpected events during the intervention (i.e., death, migration to other cities, changing telephone numbers) or were unable to continue the participation in the study.
Measures
The data were collected using the questionnaires of demographic (personal information including marital status, education level, gender, and age), clinical (the type of cancer, chemotherapy courses, and time from diagnosis), and the supportive care needs (SCNs-SF34). The SCNs-SF34 questionnaire assesses a cancer patient’s needs in 5 dimensions: psychological (10 items), health system and information (HIS) (11 items), patient care and support (5 items), physical and daily living (5 items), and sexuality (3 items). For each item, participants were asked to rate the level of their needs for help over the last month on a 5-point Likert-type scale as follows: (1) “Not applicable” (i.e., “This was not a problem for me as a result of having cancer”); (2) “Satisfied” (i.e., “I did need help with this, but my need for help was satisfied at the time”); (3) “Low need” (i.e., “This item caused me little concern or discomfort. I had little need for additional help”); (4) “Moderate need” (i.e., “This item caused me some concern or discomfort. I had some need for additional help”); and (5) “High need” (i.e., “This item caused me a lot of concern or discomfort. I had a strong need for additional help”). The first two responses are interpreted as “no need,” while the last three responses are interpreted as “some need.” The total score of SCNS-SF34 varies from 34 to 170, with a higher score indicating more need for help [19, 20]. The validity and reliability of the Persian version of SCNs-SF34 were reported acceptable with Cronbach’s alpha of 0.9 [21, 22].
Intervention
The intervention group received telephone support services for 2 months (two telephone calls per week of 15 to 30 min). The master’s prepared research nurse who was experienced in a cancer hospital, and skilled in communicating and caring for patients with cancer, made the telephone calls with participants. The content of the telephone calls was developed as a protocol based on the results of the latest studies and textbooks on cancer nursing [23] and supportive care [24]. The protocol was approved by the oncology department of Arak University of Medical Sciences. This protocol included explanations about cancer and type of treatment, side effects of chemotherapy, and managing the side effects (including nausea, vomiting, diarrhea, constipation, mucositis, and fatigue), and self-care in cancer in the fields of nutrition, physical activity, and sleeping.
The control group received routine face-to-face educational interventions provided to patients with cancer, about cancer and chemotherapy by physicians and nurses.
All participants in both groups completed SCNs-SF34 at the beginning of the study and 1 month and 2 months after starting the intervention via the telephone.
Data analysis
All data were evaluated for normality using the Kolmogorov-Smirnov test. Descriptive statistics (M, SD, N, %) were calculated to summarize this data on participant characteristics and disease-related information. Chi-square or Fisher’s exact tests were used for comparing the qualitative data of demographic and disease-related information. Also, a t-test was used for the quantitative data. The repeated measure test was used for comparing these two groups. Data analysis was performed by the Statistical Package for the Social Sciences (SPSS) software version 16.0 (SPSS Inc., Chicago, IL, USA). P value < 0.05 was considered to be statistically significant.
The study was performed adhering to the standards as outlined in the Declaration of Helsinki [25]. This study was registered in the Ethics and Research Center of Arak University of Medical Sciences with the code of ethics (IR.ARAKMU.REC.1396.159), and in the Iranian Clinical Trial Center under the code (IRCT20170404033216N1).
Results
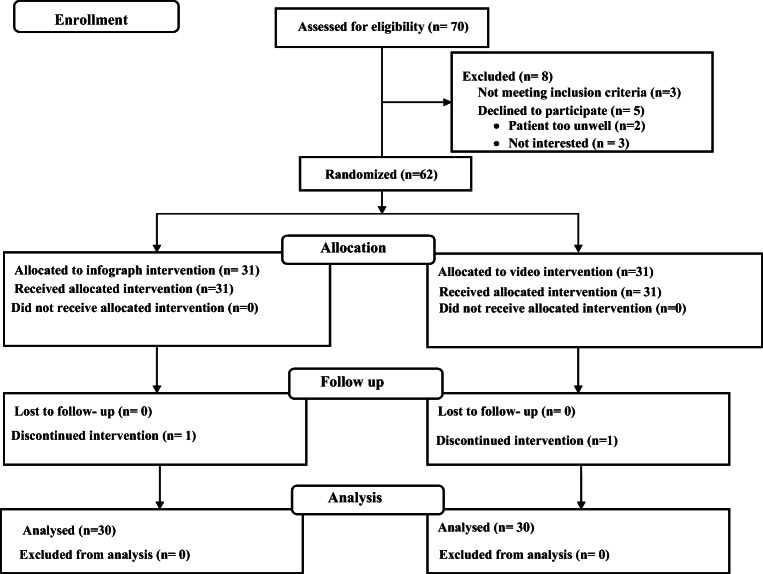
A total of 70 patients with cancer were screened for eligibility, of which 3 patients did not meet the inclusion criteria, 5 refused to participate in the study (2 patients were too unwell and 3 patients were not interested), and 2 passed away during the study (Fig. 1).
Fig. 1.
The CONSORT flow diagram of the participants’ recruitment
The study finished with 60 patients (30 in each group). The participants’ mean age in the intervention and control groups was 47.9 ± 17.44 and 54.6 ± 17.09 years, respectively, indicating no significant statistical difference (P > 0.05). Table 1 shows demographic and clinical information. There was no significant statistical difference in the mean scores of HIS, psychological, physical and daily living, patient care and support, and sexuality dimensions in the baseline between the two groups (P > 0.05).
Table 1.
Comparison of demographic and clinical characteristics in the control and intervention groups
| Control group (N %) | Intervention group (N %) | P valuea | ||
|---|---|---|---|---|
| Gender | Males | 21 (70) | 13 (43.3) | 0.067 |
| Females | 9 (30) | 17 (56.7) | ||
| Marital status | Single | 4 (13.3) | 6 (20) | 0.825 |
| Married | 23 (76.7) | 22 (73.3) | ||
| Widow | 3 (10) | 2 (6.7) | ||
| Educational level | Illiterate | 6 (20) | 4 (13.3) | 0.217 |
| Primary | 15 (50) | 8 (26.7) | ||
| Guidance | 3 (10) | 4 (13.3) | ||
| High school | 3 (10) | 8 (26.7) | ||
| Academic | 3 (10) | 6 (20) | ||
| Type of cancer | Liver | 0 | 2 (6.7) | 0.057 |
| Breast | 1 (3.3) | 8 (26.7) | ||
| CML | 3 (10) | 0 | ||
| Lymphomas | 1 (3.3) | 5 (16.7) | ||
| CRC | 5(16.7) | 3 (10) | ||
| ALL | 3 (10) | 1 (3.3) | ||
| Lung | 3 (10) | 2 (6.7) | ||
| Esophagus | 2 (6.7) | 0 | ||
| Gastric | 3 (10) | 1 (3.3) | ||
| Prostate | 2 (6.7) | 1 (3.3) | ||
| Bone marrow | 1 (3.3) | 0 | ||
| Small intestine | 0 | 1 (3.3) | ||
| AML | 2 (6.7) | 3 (10) | ||
| Sarcoma | 1 (3.3) | 1 (3.3) | ||
| Thyroid | 0 | 1 (3.3) | ||
| Brain | 1 (3.3) | 1 (3.3) | ||
| Pancreatic | 2 (6.7) | 0 | ||
| Age (years) | Mean (SD) | Mean (SD) | P valueb | |
| 54.66 (17.09) | 47.93 (17.44) | 0.137 | ||
| Time from diagnosis (years) | 1.93 (1.85) | 2.54 (2.85) | 0.333 | |
| Chemotherapy course | 8.7 (8.25) | 4.83 (3.24) | 0.02 | |
aChi-square and Fisher’s exact tests
bt-test
CML chronic myelogenous leukemia, CRC colorectal cancer, AML acute myeloid leukemia
Furthermore, the results of the repeated measure test between the groups showed that the mean scores of all dimensions of HIS (F = 9.801, P = 0.003), psychological (F = 4.835, P = 0.032), physical and daily living (F = 4.816, P = 0.032), patient care and support (F = 6.636, P = 0.013), and sexuality (F = 11.933, P = 0.001) in the intervention group were significantly lower than those of the control group (Table 2).
Table 2.
Comparison of repeated measure test results with respect to the mean scores of supportive care needs
| SCNS subscales | Groups | Mean ± SD | Mean ± SD | Mean ± SD | Repeated measure test (pairwise comparisons Bonferroni) | Means ± SD | Repeated measure test (Between groups) |
Time * group | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Before and 1 month after | Before and 2 months after | 1 month after and 2 months after | ||||||||
| Before | 1 month after | 2 months after | ||||||||
| Psychological | Control | 29.86 ± 9.08 | 29.56 ± 9.35 | 29.2 ± 9.62 | 0.999 | 0.999 | 0.999 | 29.54 ± 1.41 |
F = 4.835 P value = 0.032 |
F = 95.98 P value = 0.0001 |
| Intervention | 32.6 ± 8.66 | 23.4 ± 5.42 | 19.46 ± 4.16 | 0.0001 | 0.0001 | 0.0001 | 25.15 ± 1.41 | |||
| Health systems and Information | Control | 37.9 ± 9.93 | 36.7 ± 10.11 | 36.6 ± 10.10 | 0.193 | 0.201 | 0.999 | 37.06 ± 1.39 |
F = 9.801 P value = 0.003 |
F = 235.88 P value = 0.0001 |
| Intervention | 40.83 ± 5.59 | 30.03 ± 4.75 | 21.83 ± 3.48 | 0.0001 | 0.0001 | 0.0001 | 30.9 ± 1.39 | |||
| Physical and daily living | Control | 14.76 ± 5.11 | 14.83 ± 4.69 | 14.83 ± 4.48 | 0.999 | 0.999 | 0.999 | 14.81 ± 0.723 |
F = 4.816 P value = 0.032 |
F = 74.049 P value = 0.0001 |
| Intervention | 16.56 ± 4.62 | 11.46 ± 3.15 | 9.66 ± 2.26 | 0.0001 | 0.0001 | 0.0001 | 12.56 ± 0.723 | |||
| Patient care and support | Control | 14.5 ± 4.67 | 14.26 ± 4.81 | 14.03 ± 4.82 | 0.999 | 0.999 | 0.999 | 14.26 ± 0.683 |
F = 6.636 P value = 0.013 |
F = 34.108 P value = 0.0001 |
| Intervention | 14.43 ± 3.6 | 11.4 ± 2.41 | 9.5 ± 2.41 | 0.0001 | 0.0001 | 0.0001 | 11.77 ± 0.683 | |||
| Sexuality | Control | 8.23 ± 3.68 | 8.13 ± 3.46 | 7.93 ± 3.48 | 0.999 | 0.582 | 0.552 | 8.1 ± 0.514 |
F = 11.933 P value = 0.001 |
F = 27.11 P value = 0.0001 |
| Intervention | 7.03 ± 2.79 | 5.23 ± 1.75 | 4.5 ± 1.41 | 0.0001 | 0.0001 | 0.0001 | 5.58 ± 0.514 | |||
| Total | Control | 105.26 ± 21.66 | 103.5 ± 21.96 | 102.6 ± 22.7 | 0.773 | 0.434 | 0.999 | 103.78 ± 3.32 |
F = 14.329 P value = 0.0001 |
F = 255.79 P value = 0.0001 |
| Intervention | 111.46 ± 19.35 | 81.53 ± 13.2 | 64.96 ± 10.23 | 0.0001 | 0.0001 | 0.0001 | 85.98 ± 3.32 | |||
In the total mean score of the baseline of both groups, no significant statistical difference was found (P > 0.05). Also, the results of the repeated measure test (intergroup) showed that the total mean score of the two groups were significantly different (F = 14.329, P = 0.0001) while that of the intervention group was lower than that of the control group.
Discussion
The results of the present study showed that patients with cancer undergoing chemotherapy have supportive care needs in different aspects, with some needs being higher than others. This result is inconsistent with the findings of other studies conducted in the world and Iran [26–28].
The highest level of supportive care needs in both groups in this study was the HIS dimension, which was in line with the findings of some studies [29, 30]. Hwang et al. argued that the patients with cancer in Asian countries had a lower education level and thus they needed more information on different aspects of supportive care [31]. Similarly, more than half of the participants in this study were illiterate or had education at the level of elementary school. It is predicted that one of the issues that require more information on this dimension is the participant’s education level.
The psychological dimension, in both groups, ranked as the second factor with a high need for supportive care. Many studies have shown that patients with cancer have a strong need for this dimension [32–34]. However, Wendy et al. found that the patient’s priority in Hong Kong was not in this dimension of needs [35]. This discrepancy can be attributed to the unknown of chemotherapy for patients and their fears and anxieties about the side effects of this type of treatment, especially physical aspects such as hair loss [36]. Cultural differences, coping strategies, the types of services provided in different countries or health centers, and even religious beliefs can affect the psychological needs [37]. When providing telephone supports, the psychological needs in the intervention group were reported to be lower than those of the control group. Through telephone support, many of the questions asked by patients on this dimension can be answered sooner and their worries can be mitigated. Alfred et al. reported that a variety of psychological supports can be provided to patients with breast cancer through telephone support and counseling [10]. Meanwhile, the results of another study showed that telephone support did not affect supportive care needs and depression [6]. This result may be due to the patient characteristics in addition to caregivers’ features and capabilities.
The physical and daily living in both groups were placed in the third priority. However, the results of another study showed that this need has not been classified as one of the first three priorities [38]. Chemotherapy can cause many side effects such as nausea, vomiting, fatigue, and the loss of physical ability to do daily activities. Undoubtedly, these patients can better control these conditions if they receive the required support and training to manage the side effects of chemotherapy by a professional care team, especially nurses. The results of the present study demonstrated that telephone support can reduce participants’ needs on this dimension. This finding is in keeping with other studies which identified the relevance and applicability of this method in reducing or resolving physical needs and daily activities [14, 39–41].
The patient care and support for the participants of this study were in fourth place. Most people live with family when they are sick and there are sincere and responsible connections between family members. This paves the way to provide support to the patient in different forms of physical, nutritional, and financial care by the family. In this context, the cancer patient is likely to identify needs in this dimension. Fatmawati et al. found that different types of family (nuclear and extended) lead to improving the performance indicators and thus reduce the cancer patient’s need for support [42].
Sexuality was the last need identified for both groups, which is consistent with other studies [18, 32, 43], while it was one of the highest priorities reported in other studies [35]. Sexuality may be considered a taboo subject in Iran [44]. It is possible that the participants may not have willing to express these needs despite some sexual and marital problems [18].
The limitations of this study were the telephone support was provided for patients who were receiving chemotherapy, and investigating the effectiveness of the intervention in a short period. Short follow-up period a further limitation is that the study was only in one province. Therefore, the findings of this study may have limited generalizability in different societies and may not be generalizable to patients at other phases of cancer.
It is recommended further longitudinal research is undertaken to assess the effects of telephone-based support on patients with cancer during different phases of cancer, including at the time of diagnosis, undertaking other treatment options, and with those undergoing rehabilitation. Furthermore, considering cultural diversity in different provinces of Iran is important to reflect different types of remote supportive care services.
Conclusions
Telephone-based support can be an effective method and appropriate alternative for providing supportive care services for patients with cancer, especially those who often have no easy access to health services. This method can be considered by policymakers to inform the development holistic supportive care programs and, by nurses, to reduce the SCNs for patients with cancer and improve both health care access and their quality of life. The strengths of this study were having a wide range of participants with different types of cancer and following up the effect of the intervention 1 and 2 months after the intervention.
Acknowledgements
The authors would like to thank the patients who actively participated in the study. The authors also thank the Student Research Committee and Office of the Vice-Chancellor for Research, Arak University of Medical Sciences (IR).
Availability of data and material
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Code availability
N/A.
Author contribution
Conceptualization: [Maryam Ebrahimabadi], [Nazi Nejat]; methodology: [Nazi Nejat], [Maryam Ebrahimabadi]; formal analysis and investigation: [Fatemeh Rafiei], [Maryam Ebrahimabadi]; writing - original draft preparation: [Maryam Ebrahimabadi]; writing - review and editing: [Maryam Ebrahimabadi], [Nazi Nejat]; funding acquisition: [Nazi Nejat]; resources: [Maryam Ebrahimabadi], [Nazi Nejat]; supervision: [Nazi Nejat]. All authors read and approved the final manuscript.
Funding
This study was financially supported and approved by Arak University of Medical Sciences (grant no. 2817).
Declarations
Ethics approval
The study received ethical approval from Arak University of Medical Sciences with the code of ethics (IR.ARAKMU.REC.1396.159).
Consent to participate
All participants provided informed consent prior to enrolling onto the study.
Consent for publication
All authors consent to the publication of this manuscript in Supportive Care in Cancer.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Maryam Ebrahimabadi, Email: mebrahimi141@gmail.com.
Fatemeh Rafiei, Email: f.rafiei87@yahoo.com.
Nazi Nejat, Email: n.nejat@arakmu.ac.ir, Email: nazinejat@gmail.com.
References
- 1.Heydarzadeh L, Alilu L, Habibzadeh H, RasouIi J. The effect of peer education on knowledge, comprehension, and knowledge application of patients regarding chemotherapy complications. Iran J Nurs Midwifery Res. 2020;25(1):40–46. doi: 10.4103/ijnmr.IJNMR_69_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kazem Z (2019) Cancer Statistics in I.R. Iran in 2018. Basic Clin Cancer Res 11(1). 10.18502/bccr.v11i1.1645
- 3.Nayeri ND, Bakhshi F, Khosravi A, Najafi Z. The effect of complementary and alternative medicines on quality of life in patients with breast cancer: a systematic review. Indian J Palliat Care. 2020;26(1):95–104. doi: 10.4103/IJPC.IJPC_183_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abbasi A, Mirhosseini S, Basirinezhad MH, Ebrahimi H. Relationship between caring burden and quality of life in caregivers of cancer patients in Iran. Support Care Cancer. 2020;28(9):4123–4129. doi: 10.1007/s00520-019-05240-y. [DOI] [PubMed] [Google Scholar]
- 5.Benor DE, Delbar V, Krulik T. Measuring impact of nursing intervention on cancer patients’ ability to control symptoms. Cancer Nurs. 1998;21(5):320–334. doi: 10.1097/00002820-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 6.White VM, Macvean ML, Grogan S, D’Este C, Akkerman D, Ieropoli S, et al. Can a tailored telephone intervention delivered by volunteers reduce the supportive care needs, anxiety and depression of people with colorectal cancer? A randomised controlled trial. Psychooncology. 2012;21(10):1053–1062. doi: 10.1002/pon.2019. [DOI] [PubMed] [Google Scholar]
- 7.Leydon GM, Ekberg K, Drew P. “How can I help?” Nurse call openings on a cancer helpline and implications for call progressivity. Patient Educ Couns. 2013;92(1):23–30. doi: 10.1016/j.pec.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 8.Ebrahimabadi M, Rezaei K, Moini A, Fournier A, Abedi A. Infographics or video; which one is more effective in asthmatic patients’ health? A randomized clinical trial. J Asthma. 2019;56(12):1306–1313. doi: 10.1080/02770903.2018.1536143. [DOI] [PubMed] [Google Scholar]
- 9.Rankin SH, Stallings KD, London F. Patient education in health and illness. Philadelphia: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 10.Marcus AC, Garrett KM, Cella D, Wenzel L, Brady MJ, Fairclough D, Pate-Willig M, Barnes D, Powell Emsbo S, Kluhsman BC, Crane L, Sedlacek S, Flynn PJ. Can telephone counseling post-treatment improve psychosocial outcomes among early stage breast cancer survivors? Psycho-oncology. 2010;19(9):923–932. doi: 10.1002/pon.1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davis TC, Bocchini JA, Fredrickson D, Arnold C, Mayeaux E, Murphy PW, et al. Parent comprehension of polio vaccine information pamphlets. Pediatrics. 1996;97(6):804–810. [PubMed] [Google Scholar]
- 12.Dodd MJ, Cho MH, Miaskowski C, Painter PL, Paul SM, Cooper BA, Duda J, Krasnoff J, Bank KA. A randomized controlled trial of home-based exercise for cancer-related fatigue in women during and after chemotherapy with or without radiation therapy. Cancer Nurs. 2010;33(4):245–257. doi: 10.1097/NCC.0b013e3181ddc58c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Omidi Z, Kheirkhah M, Abolghasemi J, Haghighat S (2020) Effect of lymphedema self-management group-based education compared with social network-based education on quality of life and fear of cancer recurrence in women with breast cancer: a randomized controlled clinical trial. Qual Life Res:1–12 [DOI] [PMC free article] [PubMed]
- 14.Javanmardifard S, Ghodsbin F, Kaviani MJ, Jahanbin I. The effect of telenursing on self-efficacy in patients with non-alcoholic fatty liver disease: a randomized controlled clinical trial. Gastroenterol Hepatol Bed Bench. 2017;10(4):263–271. [PMC free article] [PubMed] [Google Scholar]
- 15.Clark RA, Inglis SC, McAlister FA, Cleland JG, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. Bmj. 2007;334(7600):942. doi: 10.1136/bmj.39156.536968.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patimah I (ed) (2019) Telenursing outcome for management of chronic illness. The 3rd International Seminar on Global Health
- 17.Shohani M, Mozafari M, Khorshidi A, Lotfi S. Comparing the effects of face-to-face and telenursing education on the quality of family caregivers caring in patients with cancer. J Fam Med Prim Care. 2018;7(6):1209–1215. doi: 10.4103/jfmpc.jfmpc_317_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Javadi P, Nejat N, Golaghaie F, Sharifi M. The effects of nurse-led telephone-based support on supportive care needs among women with breast cancer: a randomized clinical trial. Nurs Midwifery Stud. 2019;8(1):7–13. doi: 10.4103/nms.nms_94_17. [DOI] [Google Scholar]
- 19.Boyes A, Girgis A, Lecathelinais C. Brief assessment of adult cancer patients’ perceived needs: development and validation of the 34-item Supportive Care Needs Survey (SCNS-SF34) J Eval Clin Pract. 2009;15(4):602–606. doi: 10.1111/j.1365-2753.2008.01057.x. [DOI] [PubMed] [Google Scholar]
- 20.Lyu J, Yin L, Cheng P, Li B, Peng S, Yang C, et al. Reliability and validity of the mandarin version of the supportive care needs survey short-form (SCNS-SF34) and the head and neck cancer-specific supportive care needs (SCNS-HNC) module. BMC Health Serv Res. 2020;20(1):1–9. doi: 10.1186/s12913-020-05793-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nejat N (2015) Supportive care needs of patients with colorectal cancer and their families in Iran and New Zealand: A Thesis Submitted for the Degree of Doctor of Philosophy, University of Otago, Christchurch, New Zealand.: University of Otago
- 22.Rahmani A, Ferguson C, Jabarzadeh F, Mohammadpoorasl A, Moradi N, Pakpour V. Supportive care needs of Iranian cancer patients. Indian J Palliat Care. 2014;20(3):224–228. doi: 10.4103/0973-1075.138400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yarbro CH, Wujcik D, Gobel BH. Cancer nursing: principles and practice. 8. Jones & Bartlett Learning: Burlington, Massachusetts, United States; 2016. [Google Scholar]
- 24.Ettinger DS. Supportive care in cancer therapy. United States: Humana Press; 2014. [Google Scholar]
- 25.Declaration H. Human experimentation: code of ethics of World Medical Association Br. Br Med J. 1964;2:18. doi: 10.1136/bmj.2.5402.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park HY, Kim MJ, Kim JY, Kim S, Choi JY, Kim JH, Jeong HY. Could peer support programs be a good resource for managing the unmet needs of cancer patients? J Cancer Educ. 2019;34(5):950–957. doi: 10.1007/s13187-018-1399-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Okediji PT, Salako O, Fatiregun OO (2017) Pattern and predictors of unmet supportive care needs in cancer patients. Cureus 9(5) [DOI] [PMC free article] [PubMed]
- 28.So WK, Chow KM, Chan HY, Choi KC, Wan RW, Mak SS, et al. Quality of life and most prevalent unmet needs of Chinese breast cancer survivors at one year after cancer treatment. Eur J Oncol Nurs. 2014;18(3):323–328. doi: 10.1016/j.ejon.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 29.Cheng KK, Darshini Devi R, Wong WH, Koh C. Perceived symptoms and the supportive care needs of breast cancer survivors six months to five years post-treatment period. Eur J Oncol Nurs. 2014;18(1):3–9. doi: 10.1016/j.ejon.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 30.Park BW, Hwang SY. Unmet needs of breast cancer patients relative to survival duration. Yonsei Med J. 2012;53(1):118–125. doi: 10.3349/ymj.2012.53.1.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hwang SY, Park BW. The perceived care needs of breast cancer patients in Korea. Yonsei Med J. 2006;47(4):524–533. doi: 10.3349/ymj.2006.47.4.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schmid-Buchi S, Halfens RJ, Muller M, Dassen T, van den Borne B. Factors associated with supportive care needs of patients under treatment for breast cancer. Eur J Oncol Nurs. 2013;17(1):22–29. doi: 10.1016/j.ejon.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 33.Boyes AW, Girgis A, D’Este C, Zucca AC. Prevalence and correlates of cancer survivors’ supportive care needs 6 months after diagnosis: a population-based cross-sectional study. BMC Cancer. 2012;12:150. doi: 10.1186/1471-2407-12-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McDowell ME, Occhipinti S, Ferguson M, Dunn J, Chambers SK. Predictors of change in unmet supportive care needs in cancer. Psychooncology. 2010;19(5):508–516. doi: 10.1002/pon.1604. [DOI] [PubMed] [Google Scholar]
- 35.Lam WW, Au AH, Wong JH, Lehmann C, Koch U, Fielding R, et al. Unmet supportive care needs: a cross-cultural comparison between Hong Kong Chinese and German Caucasian women with breast cancer. Breast Cancer Res Treat. 2011;130(2):531–541. doi: 10.1007/s10549-011-1592-1. [DOI] [PubMed] [Google Scholar]
- 36.Hesketh PJ, Batchelor D, Golant M, Lyman GH, Rhodes N, Yardley D. Chemotherapy-induced alopecia: psychosocial impact and therapeutic approaches. Support Care Cancer. 2004;12(8):543–549. doi: 10.1007/s00520-003-0562-5. [DOI] [PubMed] [Google Scholar]
- 37.Tarakeshwar N, Vanderwerker LC, Paulk E, Pearce MJ, Kasl SV, Prigerson HG. Religious coping is associated with the quality of life of patients with advanced cancer. J Palliat Med. 2006;9(3):646–657. doi: 10.1089/jpm.2006.9.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liao YC, Liao WY, Shun SC, Yu CJ, Yang PC, Lai YH. Symptoms, psychological distress, and supportive care needs in lung cancer patients. Support Care Cancer. 2011;19(11):1743–1751. doi: 10.1007/s00520-010-1014-7. [DOI] [PubMed] [Google Scholar]
- 39.Larson JL, Rosen AB, Wilson FA. The effect of telehealth interventions on quality of life of cancer patients: a systematic review and meta-analysis. Telemed J e-health. 2018;24(6):397–405. doi: 10.1089/tmj.2017.0112. [DOI] [PubMed] [Google Scholar]
- 40.Chen YY, Guan BS, Li ZK, Li XY. Effect of telehealth intervention on breast cancer patients’ quality of life and psychological outcomes: a meta-analysis. J Telemed Telecare. 2018;24(3):157–167. doi: 10.1177/1357633x16686777. [DOI] [PubMed] [Google Scholar]
- 41.Hintistan S, Nural N, Cilingir D, Gursoy A. Therapeutic effects of nurse telephone follow-up for lung cancer patients in Turkey. Cancer Nurs. 2017;40(6):508–516. doi: 10.1097/ncc.0000000000000461. [DOI] [PubMed] [Google Scholar]
- 42.Pradjatmo H, Nisman WA, Fatmawati Y. Quality of life of cervical cancer patient with support from nuclear family and extended family in Dr. Sardjito general hospital, Yogyakarta Indonesia: a comparative study. Int J Res Med Sci. 2017;5(8):3554–3559. doi: 10.18203/2320-6012.ijrms20173561. [DOI] [Google Scholar]
- 43.Edib Z, Kumarasamy V, Binti Abdullah N, Rizal A, Al-Dubai SAR. Most prevalent unmet supportive care needs and quality of life of breast cancer patients in a tertiary hospital in Malaysia. Health Qual Life Outcomes. 2016;14(1):26. doi: 10.1186/s12955-016-0428-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rashidian M, Minichiello V, Knutsen SF, Ghamsary M. Effect of attitudes towards patients on sexual history taking: a survey of Iranian–American physicians in California, USA. Sexual Health. 2017;14(6):514–522. doi: 10.1071/SH17016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.