Abstract
Objective
To characterize trends in cholesterol testing since the start of the COVID-19 pandemic.
Methods
We extracted testing for total cholesterol performed in adults ≥40 years old within the Mass General Brigham healthcare system between March and September 2020, as well those performed between March and September 2019 (reference period). Weekly cholesterol testing rates during the 2020 vs. 2019 study periods were compared using the paired samples t-test. Secondary analyses compared testing volumes and patient characteristics during the first vs. second half of the 2020 study period.
Results
The study sample included 296,599 tests for total cholesterol performed in 220,215 individuals. The mean (SD) weekly cholesterol tests performed were 6,361 (682) in 2019 vs. 3,867 (2,373) in 2020 (P = 2.6 × 10−5), representing an overall decline of 39.2%. However, weekly testing rates in 2020 were not uniform. Greatest reductions coincided with the “first wave” of the pandemic (March-May 2020), with up to 92% reductions in testing observed. In the first 14 weeks of each study period (March to mid-June), weekly testing rates were 71.8% lower in 2020. Among individuals tested in 2020, those tested between March and mid-June had substantially lower total cholesterol compared with individuals tested after mid-June (174.2 vs. 181.5 mg/dL, P<2.2 × 10−16).
Conclusions
In a large integrated healthcare system, cholesterol testing rates were 39% lower between March-September 2020 compared with the same time period in 2019. Mechanisms for safely facilitating cholesterol testing and management for high-risk patients will be important as COVID-19 re-surges across the U.S. until widespread vaccination and population immunity allow resumption of routine preventive care.
Keywords: Cardiovascular disease, Primary prevention, Secondary prevention, Risk factors, Lipids and cholesterol, Covid-19
The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) has led to reductions in outpatient medical care and routine preventive screening for cancer and diabetes mellitus [1], [2], [3]. Cardiovascular disease is the leading cause of mortality in the U.S. [4]. Primary and secondary cardiovascular disease prevention guidelines advise routine cholesterol screening and surveillance for individuals aged ≥40 years and particularly those with established atherosclerotic cardiovascular disease [5,6]. However, data on cholesterol testing since the start of the COVID-19 pandemic are limited. Here, we characterized trends in cholesterol testing since the start of the COVID-19 pandemic within the largest healthcare system in New England.
1. Methods
Mass General Brigham (MGB) is a large integrated healthcare system serving Massachusetts and its neighboring states. The present analysis used data from cholesterol and SARS-CoV2 testing performed at Massachusetts General Hospital, Brigham and Women's Hospital, and Brigham and Women's Faulkner Hospital (all in Boston, MA), North Shore Medical Center (Salem, MA), Wentworth-Douglass Hospital (Dover, NH), and their affiliated outpatient centers. Using the MGB Research Patient Data Registry, a centralized clinical data registry, we extracted all tests for total cholesterol performed among adults aged ≥40 years with ≥1 outpatient visit (including televisits) during the 29-week period of March 4, 2020 through September 22, 2020, a period for which complete laboratory data were available. The comparison sample was cholesterol testing performed among adults with ≥1 outpatient visit during the corresponding date range in 2019. We additionally extracted SARS-CoV2 polymerase chain reaction (PCR) tests performed at MGB sites.
Weekly volumes of cholesterol testing during the 2020 vs. 2019 study periods were compared using the paired samples t-test. Secondary analyses compared testing volumes and patient characteristics during the first vs. second half of the 2020 study period. Analyses were performed using R version 3.6.0 (R Foundation, Vienna, Austria). The Massachusetts General Hospital institutional review board approved these analyses and waived informed consent.
2. Results
The study sample included 296,599 tests for total cholesterol performed in 220,215 individuals (mean 1.35 cholesterol tests per individual) between March-September 2019 and March-September 2020. During the 2020 study period, 36,929 SARS-CoV2 PCR tests were performed within the MGB system, with mean (SD) SARS-CoV2 PCR testing volumes of 1319 (1022) tests per week (overall range 185–3407 tests per week).
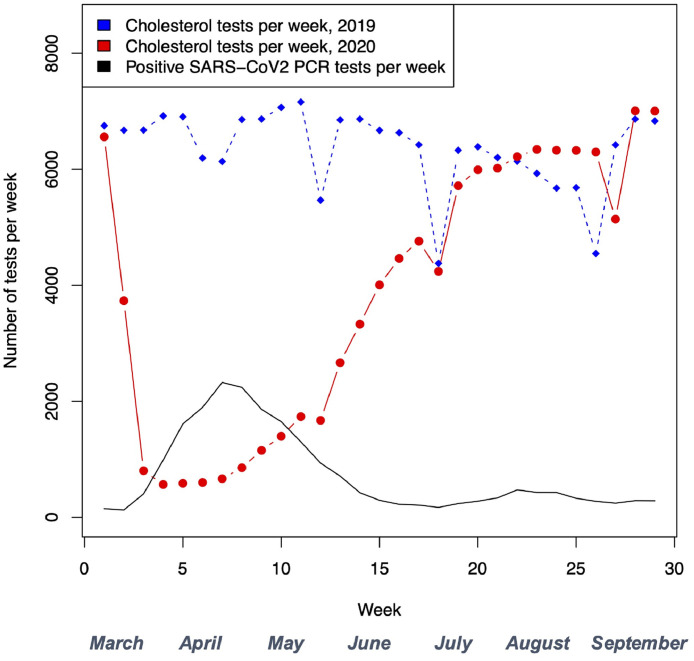
The mean (SD) weekly cholesterol tests performed were 6361 (682) in 2019 vs. 3867 (2373) in 2020 (P = 2.6 × 10−5), representing an overall decline of 39.2%. However, testing rates were not uniform throughout 2020. Greatest reductions coincided with the “first wave” of the pandemic (March-May 2020), with up to 92% reductions in weekly testing observed (Fig. 1). In the first 14 weeks of each study period (March through mid-June), mean (SD) weekly testing rates were 6669 (449) in 2019 vs. 1879 (1700) in 2020 (P = 1.0 × 10−7), representing a 71.8% decline in 2020. Beginning in June 2020, weekly testing increased, returning to 2019 levels by August 2020. There was no difference in weekly cholesterol testing volumes during the latter 15 weeks of each study period (mid-June through September) (6072 [747] per week in 2019 vs. 5722 [968] in 2020, P = 0.26).
Fig. 1.
Cholesterol testing during the 2019 and 2020 study periods, in comparison with positive SARS-CoV2 polymerase chain reaction tests during the 2020 study period.
Compared with individuals tested in 2019, those tested in 2020 were older (64.1 vs 63.4 years, P<2.2 × 10−16) and had lower mean total cholesterol levels (179.8 vs. 183.3 mg/dL, P<2.2 × 10−16) (Table 1). Among individuals tested in 2020, those tested between March and mid-June 2020 were less likely to be female (48.9% vs. 55.3%, P <2.2 × 10−16), more likely to be non-White (19.4% vs 17.5%, P = 4.4 × 10−13), and had substantially lower total cholesterol (174.2 vs. 181.5 mg/dL, P<2.2 × 10−16) compared with individuals tested after mid-June 2020.
Table 1.
Characteristics of individuals undergoing cholesterol testing.
| Characteristic | Individuals tested March-September 2019 (n = 169,825) | Individuals tested March-September 2020 (n = 104,087) | P-value* | Individuals tested in first 14 weeks of 2020 study period (n = 25,116) | Individuals tested only in latter 15 weeks of 2020 study period (n = 78,971) | P-value+ |
|---|---|---|---|---|---|---|
| Age, y | 63.4 (12.4) | 64.1 (11.9) | <0.001 | 63.9 (12.0) | 64.2 (11.9) | 0.009 |
| Age ≥75 y,% | 33,306 (19.6%) | 21,001 (20.2%) | <0.001 | 5042 (20.1%) | 15,959 (20.2%) | 0.65 |
| Female,% | 91,525 (53.9%) | 55,964 (53.8%) | 0.52 | 12,292 (48.9%) | 43,672 (55.3%) | <0.001 |
| Race | <0.001 | <0.001 | ||||
| • Asian | 7726 (4.5%) | 4047 (3.8%) | 961 (3.8%) | 3087 (3.9%) | ||
| • Black | 9492 (5.6%) | 6001 (5.7%) | 1644 (6.5%) | 4357 (5.5%) | ||
| • Hispanic | 4071 (2.4%) | 2364 (2.2%) | 587 (2.3%) | 1777 (2.3%) | ||
| • White | 138,539 (81.6%) | 85,365 (82.2%) | 20,249 (80.6%) | 65,116 (82.5%) | ||
| • Other or not reported | 9997 (5.9%) | 6310 (6.1%) | 1675 (6.7%) | 4634 (5.9%) | ||
| Primary language | <0.001 | <0.001 | ||||
| • English | 156,510 (92.2%) | 95,997 (92.2%) | 22,896 (91.2%) | 73,112 (92.6%) | ||
| • Spanish | 6470 (3.8%) | 4194 (4.0%) | 1170 (4.7%) | 3023 (3.8%) | ||
| • Other | 6845 (4.0%) | 3896 (3.7%) | 1050 (4.2%) | 2836 (3.6%) | ||
| Cholesterol, mg/dL^ | 183.3 (43.9) | 179.8 (46.7) | <0.001 | 174.2 (47.2) | 181.5 (46.2) | <0.001 |
| Cholesterol ≥200 mg/dL,%^ | 62,957 (34.1%) | 35,832 (32.0%) | <0.001 | 7343 (27.9%) | 28,489 (33.2%) | <0.001 |
P-value for comparison of individuals tested in 2019 vs. individuals tested in 2020.
P-value for comparison of individuals tested in first vs. second half of 2020 study period.
Proportions are displayed as a percentage of total cholesterol tests. A total of 296,599 cholesterol tests were performed in the study sample, including 184,456 tests in 2019 and 112,143 in 2020.
3. Discussion
In a large integrated healthcare system, cholesterol testing volume was 39% lower between March-September 2020 compared with the same time period in 2019. Weekly testing volume was lowest during the first spike in COVID-19 cases, then returned to pre-pandemic levels as cases abated in New England. Patients tested during the first wave of the COVID-19 pandemic had more optimal lipid control compared with individuals tested later in 2020. Study limitations include lack of data on patients’ background medical therapy (including lipid-lowering therapy) and primary vs. secondary prevention status. Trends in New England may not generalize uniformly to other U.S. states and regions. As chronically poor cholesterol control may compound future cardiovascular disease risk [7], mechanisms for safely facilitating cholesterol testing and management for high-risk patients will be important as COVID-19 re-surges across the U.S. until widespread vaccination and population immunity allow resumption of routine preventive care.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Dr. Natarajan has received grant support from Amgen, Apple, AstraZeneca, Boston Scientific, and Novartis, is a scientific advisor to Apple, AstraZeneca, Blackstone Life Sciences, Genentech, and Novartis, and reports spousal employment at Vertex, all unrelated to the present work. The other authors report no disclosures.
Acknowledgments
Funding
P.N. is supported by grants from the National Heart, Lung, and Blood Institute (R01HL142711, R01HL148050, R01HL151283, R01HL148565, R01HL135242) and Foundation Leducq (TNE-18CVD04), and a Hassenfeld Scholar Award from the Massachusetts General Hospital. M.C.H. is supported by a grant from the National Heart, Lung, and Blood Institute (T32HL094301-07).
Disclosures
P.N. has received grant support from Amgen, Apple, AstraZeneca, Boston Scientific, and Novartis, is a scientific advisor to Apple, AstraZeneca, Blackstone Life Sciences, Genentech, and Novartis, and reports spousal employment at Vertex, all unrelated to the present work. The other authors report no disclosures.
References
- 1.Patel S.Y., Mehrotra A., Huskamp H.A. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Internal Med. 2020 doi: 10.1001/jamainternmed.2020.5928. [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alexander G.C., Tajanlangit M., Heyward J., Mansour O., Qato D.M., Stafford R.S. Use and content of primary care office-based vs telemedicine care visits during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.21476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heintzman J., O'Malley J., Marino M., Todd J.V., Strange K.C., Huguet N. SARS-CoV-2 testing and changes in primary care services in a multistate network of community health centers during the COVID-19 pandemic. JAMA. 2020;324:1459–1462. doi: 10.1001/jama.2020.15891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Virani S.S., Alonso A., Benjamin E.J., Bittencourt M.S., Callaway C.W., Carson A.P. Heart disease and stroke statistics—2020 update: a report from the American heart association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 5.Bibbins-Domingo K., Grossman D.C., Curry S.J., Davidson K.W., Epling J.W., Garcia F.A.R. Statin use for the primary prevention of cardiovascular disease in adults: US preventive services task force recommendation statement. JAMA. 2016;316:1997–2007. doi: 10.1001/jama.2016.15450. [DOI] [PubMed] [Google Scholar]
- 6.Grundy S.M., Stone N.J., Bailey A.L., Beam C., Birtcher K.K., Blumenthal R.S. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. 2019;139:e1082–e1143. doi: 10.1161/CIR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Silverman M.G., Ference B.A., Im K., Wiviott S.D., Giugliano R.P., Grundy S.M. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA. 2016;316:1289–1297. doi: 10.1001/jama.2016.13985. [DOI] [PubMed] [Google Scholar]