Abstract
Background
Immune thrombocytopenia (ITP) is a bleeding disorder. Helicobacter pylori is a Gram-negative bacterium that is presumed to be associated with ITP and therapeutic response of patients. To evaluate the effect of H. pylori eradication on platelet count of ITP patients, we analyzed the studies conducted on the association between H. pylori infection and response to therapy in ITP patients in Western Asia focusing on the Middle East region.
Methods
A systematic search of databases (PubMed/Medline, ISI Web of Science, Cochrane Central) and Google Scholar search engine results was conducted up until January 2020. The keywords included in the search were Helicobacter pylori and/or H. pylori, ITP and/or immune thrombocytopenia.
Results
Seven studies comprising a total of 228 H. pylori-infected patients (193 with successful eradication) were included in this study. The association between H. pylori eradication and ITP was expressed as odds ratios (OR) and 95% confidence intervals (CI). The findings showed that patients who received eradication treatment for H. pylori infection had significantly higher OR (OR, 8.83; 95% CI, 2.03‒38.35; P=0.004) than those in the non-eradicated group.
Conclusion
Our results indicate a significant therapeutic effect of H. pylori eradication on the platelet count of patients with chronic ITP. Given the inherent limitations of this study, including the small number of patients, further studies with more patients are recommended.
Keywords: Helicobacter pylori, H. Pylori, ITP, Immune thrombocytopenia
INTRODUCTION
Immune thrombocytopenia (ITP) is an acquired autoimmune disorder characterized by a decreased platelet count in peripheral blood and increased destruction of platelets and megakaryocytes in peripheral blood and bone marrow, respectively [1]. The incidence of ITP is estimated to be 100 cases per million years and increases with age [2]. Based on its duration, ITP can be categorized as newly diagnosed, persistent, or chronic infection [3]. Patients with platelet counts lower than 100×109/L may show different clinical findings, ranging from skin symptoms, such as petechiae, purpura, and ecchymosis, to life-threatening clinical complications, including intracranial bleeding [4, 5]. Children account for approximately 50% of ITP cases, and often recover spontaneously from the disease, while adults go through the chronic phase of the disorder [2]. Most ITP cases are primary infections, and only 20% percent of cases are secondary to underlying complications [6]. These complications include lymphoproliferative disorders (mainly chronic lymphoblastic leukemia), autoimmune disorders such as lupus erythematosus (SLE), infection with different viruses such as cytomegalovirus (CMV), Epstein-Barr virus (EBV), human immunodeficiency virus (HIV), hepatitis C virus (HCV), and infection with the bacterium Helicobacter pylori (H. pylori) [7]. Although the pathogenesis of ITP remains ambiguous, one can assume that due to impaired immunological tolerance following viral infection, immune cells recognize and attack platelet glycoproteins (GPs) (mainly GP IIb/IIIa and Ib/IX) as viral immunogens as a result of molecular mimicry, which ultimately results (including T lymphocytes) in the destruction of platelets [1, 6, 8, 9]. In parallel to the direct destruction of platelets by T lymphocytes, the immune system can produce autoantibodies against platelets. These auto-antibody-coated platelets are cleared by macrophages of the reticuloendothelial system (RES), which leads to increased destruction of platelets, and increased risk of bleeding [7]. Similar to other autoimmune disorders, ITP is subject to certain effective factors, including genetic factors such as mutations in human leukocyte antigens (HLAs) and polymorphisms of interferon-γ [10-12]. In addition to genetic factors, other factors, such as H. pylori infection, are presumed to be associated with the initiation of ITP and the response of patients to therapy. Different studies have reported an association between H. pylori infection eradication and improved platelet count in patients with ITP [13-16]. However, due to the difference in H. pylori infection prevalence rates in different countries and races, as well as the lack of sufficient evidence to determine the impact of H. pylori eradication on platelet count, such findings cannot be accepted with certainty. Therefore, to arrive at a definitive conclusion, previous studies conducted in different countries on various populations and races should be reconsidered and thoroughly reviewed. To this end, we analyzed the studies that have already been conducted on the association between H. pylori infection and response to therapy in patients with ITP in the Middle East to evaluate the effect of H. pylori eradication on platelet count.
MATERIALS AND METHODS
To conduct this systematic review and meta-analysis, the Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA) guidelines were used [17].
Literature search
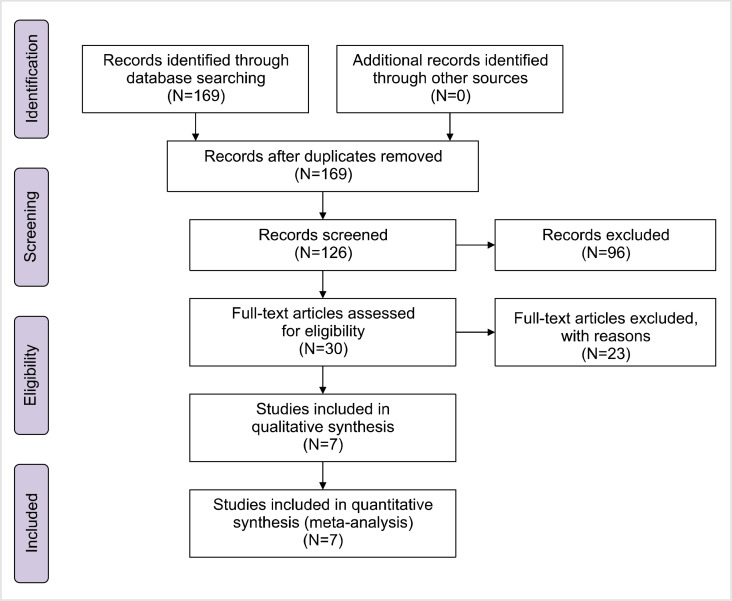
To find relevant papers published on the effect of H. pylori eradication on the platelet count of patients with ITP, we systematically searched three international indexing databases (PubMed/Medline, ISI Web of Science, Cochrane Central) and Google Scholar search engine up to January 2020. The keywords used in the search process included “helicobacter pylori” and/or “H. Pylori,” “ITP” and/or “Immune thrombocytopenia.” Two authors (S.M.S.P. and A.Y.A.) independently screened the article titles and abstracts for inclusion. The titles and abstracts of 126 articles were investigated thoroughly to determine the competency of the articles. Among the 30 full-text articles related to Asia, seven studies were compatible with our inclusion criteria and were reviewed for inclusion in the present study (Table 1). The inclusion criteria were as follows: i) definite diagnosis of ITP, ii) documented H. pylori infection with reliable tests such as stool antigen test or serologic test for antibody, iii) outcome of eradication (platelet count or response rate), and iv) Western Asia and Middle Eastern origin. The identification, screening, eligibility assessment, and final included studies are summarized in Fig. 1.
Table 1.
Summary of the characteristic of the included studies.
| Reference (country) | N (F/M) Age mean±SD or median (range) |
Detection of HP infection (follow up period) |
Duration of ITP (type of ITP relapse) |
Platelet count at enrollment | Platelet after treatment | Response in all infected patients | Eradicated patients (non-eradicated patients) |
|---|---|---|---|---|---|---|---|
| Iran [18] | 29.2±7.0 (18–46) | 79 patients were infected & only 71 completed eradication | 61 mo (6–210 mo) | 58.32±17.74×109/L (range, 31–96×109/L) | Eradicated patients137.77×109/L | Response in 30 eradicated patients | 62 |
| 29.2±7.0 (18–46) | Chronic | 9 | |||||
| 1 yr | NR | P<0.001 | CR: 30 | ||||
| Iran [19] | 30 (67/33) | 5 patients were infected | NR | 20×109/L (10–30×109/L) | 81×109/L (69–89×109/L) | Response in 5 eradicated patients | 5 |
| 12 (9–16) | Chronic | PR: 4 | 0 | ||||
| 1 yr | 1 out of 5 eradicated patients (20%) | P=0.043 | CR: 0 | ||||
| PR+CR: 4 patients | |||||||
| Iran [20] | 52 (50/50 in 26 patients) | H. pylori eradication achieved in 89.5% (26/29) | NR | 57.9×109/L (22–96×109/L) | 104×109/L (26–196×109/L) | Response in 26 eradicated patients | 26 |
| NR | CR: 15 | 3 | |||||
| 38 (17–71) | NR | P<0.001 | PR: 0 | ||||
| 6 mo | PR+CR: 15 | ||||||
| Iran [21] | 92 (53/47) | Only 47 patients remained after excluding other patients | 2.2 mo (1–4.5 mo) | 34.6×109/L (21–48×109/L) | 52.8×109/L (23–86×109/L) | Response in 41 eradicated patients | 41 |
| 41 (19–71) | CR: 0 | 6 | |||||
| Chronic | (P<0.001) | PR: 3 | |||||
| 6 mo | NR | PR+CR: 3 | |||||
| Pakistan [22] | 197 (54.5/45.5 in 22 patient) | 22 patients were infected | NR | 53.36±24.5×109/L | 80.86±51.0×109/L | Response in 22 infected patients | 7 |
| NR | CR: 7 | 15 | |||||
| 43.18±12.5 yr | NR | NR | P=0.003 | PR: 10 | |||
| PR+CR: 17 | |||||||
| Pakistan [23] | 85 (62.3/37.6) | 34 patients were infected | NR | 48.56±21.7×109/L | 94.2±26.8×109/L | Response in 34 eradicated patients | 34 |
| Infected patients: 43.89±7.06 | Chronic | CR: 19 | 0 | ||||
| Uninfected patients: 44.75±7.91 | NR | NR | P=0.001 | PR: 10 | |||
| PR+CR: 29 | |||||||
| Turkey [24] | 34 (35.3/64.7) | 20 patients were infected | NR | 39.7±19.2×109/L | 164.2±63.2×109/L | Response in 18 eradicated patients | 18 |
| 52.5 yr (range, 16–93) | Chronic | CR: 5/18 | 2 | ||||
| 13 mo | NR | P<0.05 | PR: 3/18 | ||||
| PR+CR: 8 |
Abbreviations: CR, complete response; ITP, immune thrombocytopenia; NR, not reported; PR, partial response.
Fig. 1.
Identification, screening, eligibility assessment, and final included studies.
Statistical analysis
The association between H. pylori eradication and ITP, expressed as odds ratios (OR) and 95% confidence intervals (CI), was calculated using Comprehensive Meta-Analysis (CMA) software. If the OR was higher than 1, it was considered a better response for patients in the eradication group. The random-effects model was used for pooling the data, and the possibility of publication bias was evaluated using a funnel plot.
RESULTS
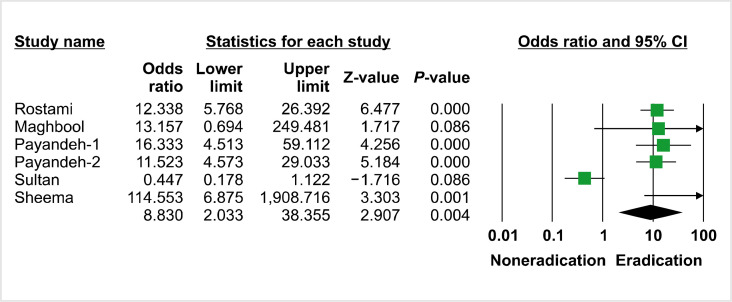
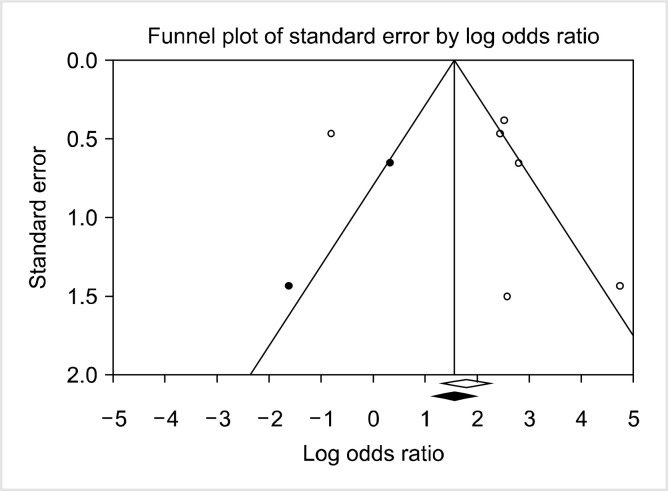
Among the articles reviewed, only seven studies concerning the association between H. pylori eradication and response to treatment in patients with ITP in the Middle East were included in this meta-analyze (Fig. 1) [18-24]. Table 1 summarizes the main characteristics and outcomes of the treatments used in the included studies. In all included studies, the authors used standard guidelines for the diagnosis of ITP, which are mainly based on ruling out other possible causes of thrombocytopenia (viral infections, lymphoproliferative disorders, and autoimmune disorders) and confirming a decreased platelet count (less than 100×109/L). However, most of these previous studies failed to report the duration of ITP in the patients examined. Moreover, all of the included studies, except two, reported that the participants were diagnosed with chronic ITP. For the two exceptions, after reviewing the description of patients (such as their mean age), we concluded that it was highly probable that they also studied chronic patients. The findings showed that among the seven included articles, three studies confirmed H. pylori infection using the Urea Breath Test (UBT) [20, 21, 24], three other studies [19, 22, 23] used the stool antigen enzyme immunoassay test, and one study [18] did not report the method used for H. pylori infection documentation. In the 228 patients included in these seven studies, the prevalence of H. pylori infection ranged from 16.6% [19] to 61.2% [18]. Moreover, all studies used standard triple therapy consisting of amoxicillin, clarithromycin, and a proton pump inhibitor (omeprazole in all studies) for 14 days to eradicate H. pylori infection. Three studies determined a complete response as a platelet count >100×109/L [18, 20, 22], while four studies considered platelet counts >150×109/L as a complete response in their patients [19, 21, 23, 24]. Furthermore, the highest rate of eradicated patients with increased platelet count was 85.3% [23], while the lowest rate was 7.3% [21]. The results also revealed that after eradication of H. pylori, ITP patients showed significantly increased platelet counts (P<0.05) in all studies (Table 1). Additionally, patients who received eradication treatment for H. pylori infection showed significantly higher OR (8.83; 95% CI, 2.03–38.35; P=0.004) than those who did not (Fig. 2). Overall, as the findings showed, there was significant heterogeneity among studies (I2=88.3%, P=0.00) (Table 2). In addition, as shown in Fig. 3, there is some evidence of publication bias due to the asymmetrical form of the funnel plot.
Fig. 2.
Odds ratios of the patients with eradication of H. Pylori.
Table 2.
Random-effects model for pooling data.
| Model | N of studies | Effect size and 95% interval | Test of null (2-tail) | Heterogeneity | Tau-squared | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Point estimate | Lower limit | Upper limit | z-value | P | q-value | df (Q) | P | I-squared | Tau squared | Standard error | Variance | Tau | |||||
| Fixed | 6 | 6.013 | 3.833 | 9.435 | 7.806 | 0.000 | 42.809 | 5 | 0.000 | 88.320 | 2.674 | 2.290 | 5.244 | 1.635 | |||
| Random | 6 | 8.830 | 2.033 | 38.355 | 2.907 | 0.004 | |||||||||||
Fig. 3.
Evaluation of publication bias by funnel plot.
DISCUSSION
As a Gram-negative bacterium, H. pylori is responsible for most cases of peptic ulcers and gastric cancer worldwide. It is also associated with mucosa-associated lymphoid tissue (MALT) lymphoma, although the transmission pattern of this pathogen is not completely understood [25, 26]. Overall, it is widely known that H. pylori is transmitted through oral-oral, fecal-oral, and gastro-oral routes [27]. As a highly prevalent infection, H. pylori is commonly acquired in early stages of life and grows in digestive tract and stays in the host’s body for the rest of its life [28, 29]. The most common manifestation of H. pylori is gastritis, although its clinical manifestations vary from case to case [26, 29, 30]. Interestingly, the prevalence of H. pylori infection also varies from country to country, indicating the probable role of genetics and race in the prevalence of infection. For instance, Hooi et al. [31] estimated the prevalence of H. pylori infection to be 81%, 59%, and 77.2% in Pakistan, Iran, and Turkey, respectively, while they estimated the prevalence for Egypt and Denmark to be 40.9% and 22.1%, respectively. The significant difference in the reported prevalence of H. pylori infection might be due to factors such as access to clean water, population density, and the level of social health in the country. Gasbarrini et al. [32] reported an association between H. pylori and ITP for the first time in 1998; since then, different studies have several proposed possible mechanisms for this association. Using different mechanisms, it is believed that H. pylori escapes from innate immune mediators and attaches to gastric epithelial cells. After attachment, one of the important virulence factors of H. pylori, cytotoxin-associated gene A (CagA), induces inflammation through NF-κB signaling and interleukin (IL)-8 stimulation [33, 34]. In addition, CagA activates SHP-2 phosphatase and ERK (a mediator of the MPK signaling pathway), which results in the perturbation of gastric epithelial cell signaling [33]. CagA is an immunogenic protein that stimulates the production of antibodies. Because of the molecular mimicry between CagA and GP IIb/IIIa on platelets, it is possible that antibodies against CagA cause increased destruction of antibody-coated platelets by the reticuloendothelial system in patients with chronic ITP [35, 36]. Another aspect of this association is mediated by the vacuolating cytotoxin A gene (VacA), which is another important virulence factor of H. pylori. VacA perturbs IL-2 signaling, inhibits proliferation of helper T cells, and mediates adherence to platelets [33]. In addition, H. pylori can use the von Willebrand factor (VWF) to increase adherence to platelets [37], resulting in the activation and consumption of platelets, which is another possible cause of thrombocytopenia in H. pylori-induced ITP. Several meta-analyses and random clinical trials have already reported a positive outcome of H. pylori eradication on the platelet count of patients with ITP. For instance, the systemic reviews and meta-analyses of seventeen studies involving 788 ITP patients showed statistically significant increases in platelet counts in successfully eradicated patients compared to controls, and untreated and non-eradicated patients [weighted mean difference (WMD), 40.77×109/L (95% CI, 20.92–60.63), 52.16×109/L (95% CI, 34.26–70.05), and 46.35×109/L (95% CI, 27.79–64.91), respectively] [38]. Furthermore, a review of 25 studies involving 1,555 patients reported an overall response rate of 35.2% (95% CI, 28.0–42.4) [39]. Similarly, by reviewing six studies with 241 patients in the eradication group, Kim et al. [36] reported a significantly higher overall platelet response rate than the control group (OR, 1.93; 95% CI, 1.01–3.71; P=0.05).
In summary, despite the overall acceptance of the positive role of H. pylori eradication on platelet count in patients with ITP, important questions remain unanswered. For instance, the pathophysiology of H. pylori-induced chronic ITP, the mechanisms of response to infection, and the reason for the difference in infection prevalence in different populations remain unknown.
This study has several limitations, including the following: i) The number of studies and patients involved was small; ii) the included studies only examined chronic ITP in adults, and therefore, the results cannot be generalized to patients with acute ITP, especially children; iii) the studies showed heterogeneity in the method used for H. pylori infection; iv) the thresholds for complete response (CR) and partial response (PR) varied among the included studies; and v) some data were missing (such as the duration of ITP). In conclusion, the results indicated a significant therapeutic effect of H. pylori eradication on the platelet count in patients with chronic ITP. It is recommended that other studies be conducted to further explore the effect of H. pylori eradication on children with ITP, and the difference between H. pylori eradication in both acute and chronic forms of the infection.
Footnotes
Authors’ Disclosures of Potential Conflicts of Interest
No potential conflicts of interest relevant to this article were reported.
REFERENCES
- 1.Andrès E. Primary immune thrombocytopenia: a translational research model for autoimmune diseases. J Clin Med. 2019;8:1971. doi: 10.3390/jcm8111971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cines DB, Blanchette VS. Immune thrombocytopenic purpura. N Engl J Med. 2002;346:995–1008. doi: 10.1056/NEJMra010501. [DOI] [PubMed] [Google Scholar]
- 3.Provan D, Stasi R, Newland AC, et al. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood. 2010;115:168–86. doi: 10.1182/blood-2009-06-225565. [DOI] [PubMed] [Google Scholar]
- 4.Cines DB, Bussel JB, Liebman HA, Luning Prak ET. The ITP syndrome: pathogenic and clinical diversity. Blood. 2009;113:6511–21. doi: 10.1182/blood-2009-01-129155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper N, Ghanima W. Immune thrombocytopenia. N Engl J Med. 2019;381:945–55. doi: 10.1056/NEJMcp1810479. [DOI] [PubMed] [Google Scholar]
- 6.Zufferey A, Kapur R, Semple JW. Pathogenesis and therapeutic mechanisms in immune thrombocytopenia (ITP) J Clin Med. 2017;6:16. doi: 10.3390/jcm6020016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pezeshki SMS, Jalali MT, Amin Asnafi A, Jaseb K, Saki N. HLA-B5, 7, 8, 27, and 51 antigens and immune thrombocytopenic purpura: is there an association? J Pediatr Hematol Oncol. 2020;42:e32–7. doi: 10.1097/MPH.0000000000001543. [DOI] [PubMed] [Google Scholar]
- 8.Kashiwagi H, Kuwana M, Hato T, et al. Reference guide for management of adult immune thrombocytopenia in Japan: 2019 revision. Int J Hematol. 2020;111:329–51. doi: 10.1007/s12185-019-02790-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Audia S, Mahévas M, Samson M, Godeau B, Bonnotte B. Pathogenesis of immune thrombocytopenia. Autoimmun Rev. 2017;16:620–32. doi: 10.1016/j.autrev.2017.04.012. [DOI] [PubMed] [Google Scholar]
- 10.Rezaeeyan H, Jaseb K, Kaydani GA, Asnafi AA, Masbi MH, Saki N. Involvement of interferon-γ + 874A/T polymorphism in the pathogenesis of and therapeutic response to immune thrombo-cytopenia. Lab Med. 2019;50:e42–9. doi: 10.1093/labmed/lmz010. [DOI] [PubMed] [Google Scholar]
- 11.Rajaei E, Jalali MT, Shahrabi S, Asnafi AA, Pezeshki SMS. HLAs in autoimmune diseases: dependable diagnostic biomarkers? Curr Rheumatol Rev. 2019;15:269–76. doi: 10.2174/1573397115666190115143226. [DOI] [PubMed] [Google Scholar]
- 12.Amin Asnafi A, Jalali MT, Pezeshki SMS, Jaseb K, Saki N. The association between human leukocyte antigens and ITP, TTP, and HIT. J Pediatr Hematol Oncol. 2019;41:81–6. doi: 10.1097/MPH.0000000000001381. [DOI] [PubMed] [Google Scholar]
- 13.Kim H, Lee WS, Lee KH, et al. Efficacy of Helicobacter pylori eradication for the 1st line treatment of immune thrombo-cytopenia patients with moderate thrombocytopenia. Ann Hematol. 2015;94:739–46. doi: 10.1007/s00277-014-2268-9. [DOI] [PubMed] [Google Scholar]
- 14.Aljarad S, Alhamid A, Sankari Tarabishi A, Tarabishi AS, Suliman A, Aljarad Z. The impact of helicobacter pylori eradication on platelet counts of adult patients with idiopathic thrombocytopenic purpura. BMC Hematol. 2018;18:28. doi: 10.1186/s12878-018-0119-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hwang JJ, Lee DH, Yoon H, Shin CM, Park YS, Kim N. The effects of helicobacter pylori eradication therapy for chronic idiopathicthrombocytopenic purpura. Gut Liver. 2016;10:356–61. doi: 10.5009/gnl14483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brito HS, Braga JA, Loggetto SR, Machado RS, Granato CF, Kawakami E. Helicobacter pylori infection & immune thrombo-cytopenic purpura in children and adolescents: a randomized controlled trial. Platelets. 2015;26:336–41. doi: 10.3109/09537104.2014.911836. [DOI] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group, author. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 18.Rostami N, Keshtkar-Jahromi M, Rahnavardi M, Keshtkar-Jahromi M, Esfahani FS. Effect of eradication of Helicobacter pylori on platelet recovery in patients with chronic idiopathic thrombo-cytopenic purpura: a controlled trial. Am J Hematol. 2008;83:376–81. doi: 10.1002/ajh.21125. [DOI] [PubMed] [Google Scholar]
- 19.Maghbool M, Maghbool M, Shahriari M, Karimi M. Does Helicobacter pylori play a role in the pathogenesis of childhood chronic idiopathic thrombocytopenic purpura? Pediatr Rep. 2009;1:e2. doi: 10.4081/pr.2009.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Payandeh M, Sohrabi N, Zare ME, Kansestani AN, Hashemian AH. Platelet count response to helicobacter pylori eradication in Iranian patients with idiopathic thrombocytopenic purpura. Mediterr J Hematol Infect Dis. 2012;4:e2012056. doi: 10.4084/mjhid.2012.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Payandeh M, Raeisi D, Sohrabi N, et al. Poor platelet count response to helicobacter pylori eradication in patients with severe idiopathic thrombocytopenic purpura. Int J Hematol Oncol Stem Cell Res. 2013;7:9–14. [PMC free article] [PubMed] [Google Scholar]
- 22.Sultan S, Irfan SM, Kaker J, Hasan M. Efficacy of helicobacter pylori eradication as an upfront treatment of secondary immune thrombocytopenia: an experience from Pakistan. Med J Malaysia. 2016;71:53–6. [PubMed] [Google Scholar]
- 23.Sheema K, Ikramdin U, Arshi N, Farah N, Imran S. Role of Helicobacter pylori eradication therapy on platelet recovery in chronic immune thrombocytopenic purpura. Gastroenterol Res Pract. 2017;2017:9529752. doi: 10.1155/2017/9529752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sayan O, Akyol Erikci A, Ozturk A. The efficacy of Helicobacter pylori eradication in the treatment of idiopathic thrombo-cytopenic purpura--the first study in Turkey. Acta Haematol. 2006;116:146–9. doi: 10.1159/000093648. [DOI] [PubMed] [Google Scholar]
- 25.Burucoa C, Axon A. Epidemiology of Helicobacter pylori infection. Helicobacter. 2017;Suppl 1:12403. doi: 10.1111/hel.12403. [DOI] [PubMed] [Google Scholar]
- 26.Guevara B, Cogdill AG. Helicobacter pylori: a review of current diagnostic and management strategies. Dig Dis Sci. 2020;65:1917–31. doi: 10.1007/s10620-020-06193-7. [DOI] [PubMed] [Google Scholar]
- 27.Xie Y, Song C, Cheng H, et al. Long-term follow-up of Helicobacter pylori reinfection and its risk factors after initial eradication: a large-scale multicentre, prospective open cohort, observational study. Emerg Microbes Infect. 2020;9:548–57. doi: 10.1080/22221751.2020.1737579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thorell K, Lehours P, Vale FF. Genomics of Helicobacter pylori. Helicobacter. 2017;22 Suppl 1:12409. doi: 10.1111/hel.12409. [DOI] [PubMed] [Google Scholar]
- 29.Diaconu S, Predescu A, Moldoveanu A, Pop CS, Fierbințeanu-Braticevici C. Helicobacter pylori infection: old and new. J Med Life. 2017;10:112–7. [PMC free article] [PubMed] [Google Scholar]
- 30.Versalovic J. Helicobacter pylori. Pathology and diagnostic strategies. Am J Clin Pathol. 2003;119:403–12. doi: 10.1309/5DTF5HT7NPLNA6J5. [DOI] [PubMed] [Google Scholar]
- 31.Hooi JKY, Lai WY, Ng WK, et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastro-enterology. 2017;153:420–9. doi: 10.1053/j.gastro.2017.04.022. [DOI] [PubMed] [Google Scholar]
- 32.Gasbarrini A, Franceschi F, Tartaglione R, Landolfi R, Pola P, Gasbarrini G. Regression of autoimmune thrombocytopenia after eradication of Helicobacter pylori. Lancet. 1998;352:878. doi: 10.1016/S0140-6736(05)60004-9. [DOI] [PubMed] [Google Scholar]
- 33.Zain MA, Zafar F, Ashfaq A, Jamil AR, Ahmad A. Helicobacter pylori: an underrated cause of immune thrombocytopenic purpura. A comprehensive review. Cureus. 2019;11:e5551. doi: 10.7759/cureus.5551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Frydman GH, Davis N, Beck PL, Fox JG. Helicobacter pylori eradication in patients with immune thrombocytopenic purpura: a review and the role of biogeography. Helicobacter. 2015;20:239–51. doi: 10.1111/hel.12200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fukuda T, Asou E, Nogi K, Yasuda M, Goto K. Association between Helicobacter pylori infection and platelet count in mice. Exp Anim. 2018;67:487–92. doi: 10.1538/expanim.18-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim BJ, Kim HS, Jang HJ, Kim JH. Helicobacter pylori eradication in idiopathic thrombocytopenic purpura: a meta-analysis of randomized trials. Gastroenterol Res Pract. 2018;2018:6090878. doi: 10.1155/2018/6090878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Byrne MF, Kerrigan SW, Corcoran PA, et al. Helicobacter pylori binds von Willebrand factor and interacts with GPIb to induce platelet aggregation. Gastroenterology. 2003;124:1846–54. doi: 10.1016/S0016-5085(03)00397-4. [DOI] [PubMed] [Google Scholar]
- 38.Franchini M, Cruciani M, Mengoli C, Pizzolo G, Veneri D. Effect of Helicobacter pylori eradication on platelet count in idiopathic thrombocytopenic purpura: a systematic review and meta-analysis. J Antimicrob Chemother. 2007;60:237–46. doi: 10.1093/jac/dkm195. [DOI] [PubMed] [Google Scholar]
- 39.Stasi R, Sarpatwari A, Segal JB, et al. Effects of eradication of Helicobacter pylori infection in patients with immune thrombocytopenic purpura: a systematic review. Blood. 2009;113:1231–40. doi: 10.1182/blood-2008-07-167155. [DOI] [PubMed] [Google Scholar]