Abstract
Venous thromboembolism (VTE), which includes pulmonary embolism and deep vein thrombosis, is a condition characterized by abnormal blood clot formation in the pulmonary arteries and the deep venous vasculature. It is often serious and sometimes even fatal if not promptly and appropriately treated. Moreover, the later consequences of VTE may result in reduced quality of life. The treatment of VTE depends on various factors, including the type, cause, and patient comorbidities. Furthermore, bleeding may occur as a side effect of VTE treatment. Thus, it is necessary to carefully weigh the benefits versus the risks of VTE treatment and to actively monitor patients undergoing treatment. Asian populations are known to have lower VTE incidences than Western populations, but recent studies have shown an increase in the incidence of VTE in Asia. A variety of treatment options are currently available owing to the introduction of direct oral anticoagulants. The current VTE treatment recommendation is based on evidence from previous studies, but it should be applied with careful consideration of the racial, genetic, and social characteristics in the Korean population.
Keywords: Venous thromboembolism, Deep vein thrombosis, Pulmonary embolism, Anticoagulants
INTRODUCTION
Venous thromboembolism (VTE) includes pulmonary embolism (PE), which is potentially fatal and causes chronic thromboembolic pulmonary hypertension, and deep vein thrombosis (DVT), which causes leg swelling and postthrombotic syndrome. In addition, VTE may develop in a splanchnic vein and in other atypical locations. Currently, cancer-associated thrombosis (CAT) is highlighted due to the increased prevalence of cancer. Although the incidence of VTE in Asian populations, including that of Korea, is lower than that in Western populations [1], the age- and sex-standardized annual incidence rate (ASR) of VTE per 100,000 individuals in the Korean population has increased steadily starting in 2004 [2], and this increase has been maintained, leading to an ASR of 29.2% in 2013 [3].
Among cardiovascular diseases, PE is the third most common cause of death, after heart attack and stroke [4]. The fatality rate is approximately 6% after DVT and approximately 12% after PE [5].
Vitamin K antagonists (VKA; warfarin) and low-molecular-weight heparin (LMWH) have been used for the treatment of VTE. However, direct oral anticoagulant (DOAC) therapies have also been developed; DOACs have been commonly used for the treatment of VTE since the mid-2000s because they do not require regular hematologic monitoring, and fixed-dose oral intake is convenient. In Korea, dabigatran was first covered by the National Health Insurance System in May 2015, and rivaroxaban, apixaban, and edoxaban were subsequently approved for VTE treatment. Overall, VKA has been rapidly replaced by DOACs in the market [3]. Therefore, the development of Korean guidelines for VTE treatment is needed for Korean clinicians, although the results of clinical trials for Korean patients with VTE [6] are still scarce.
The members of the Thrombosis and Hemostasis Working Party under the Korean Society of Hematology decided to develop Korean recommendations for VTE treatment. All members are clinical or laboratory hematologists, and most are affiliated with tertiary teaching hospitals. The group divided the specific topics pertaining to VTE treatment among the members; subsequently, the members wrote the manuscript, referencing recent guidelines, meta-analyses, and the results of pivotal clinical trials while reflecting on domestic circumstances in Korea. After completion of the manuscript draft, independent members in the field of thrombosis and hemostasis reviewed the primary manuscript. All members reviewed the completed manuscript several times.
This recommendation is not a manual for VTE treatment. Physicians must consider each clinical situation and the patient’s condition or status when making decisions. The diagnosis or prophylaxis of VTE is beyond the scope of our recommendation. This recommendation may aid in clinical decision-making for Korean patients with VTE.
APPROPRIATE SELECTION OF TREATMENT MODALITIES AND ANTICOAGULANTS FOR VENOUS THROMBOEMBOLISM
General principle of anticoagulation
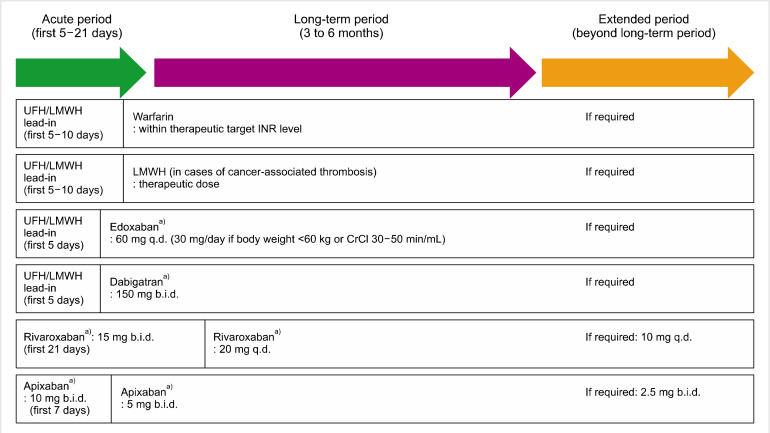
Medical anticoagulation consists of 3 periods: acute (the first 5–21 days), long-term (3–6 mo), and extended period (thereafter; Fig. 1). In the acute period, anticoagulants are loaded via parenteral heparin lead-in or a higher dose of oral anticoagulants is administered. For long-term treatment, the general anticoagulant treatment period for postoperative VTE is 3 months because of the low risk of recurrence, but is prolonged to 6 months for unprovoked VTE. Extended treatment can be considered in some cases with a high risk of VTE recurrence.
Fig. 1.
Overview of anticoagulant therapy for venous thromboembolism. a)Doses can be modified according to organ function, body weight, or concomitant medications. Abbreviations: INR, international normalized ratio; LMWH, low-molecular-weight heparin; UFH, unfractionated heparin.
Abbreviations: INR, international normalized ratio; LMWH, low-molecular-weight heparin; UFH, unfractionated heparin.
For the treatment of VTE, heparin and VKA have been used widely for a long time, although DOACs are quickly replacing them because of their convenience of use. However, in certain situations or for patients who have already been using older anticoagulants for a long time, heparin and VKA can continue to be used [7]. LMWH is also frequently used, especially in cases of CAT. Compared to unfractionated heparin (UFH), it is more likely to show a predictable dose-response relationship. It has a longer half-life, allowing it to be administered subcutaneously once a day or twice a day, with a lower risk of heparin-induced thrombocytopenia and osteoporosis. Because LMWH is excreted mainly by the kidney, it should not be used in patients with severe renal impairment. Conversely, UFH has a shorter half-life and can thus be useful in patients who require an immediate anticoagulant effect to support rapid conversion. VKA is absorbed in the gastrointestinal tract and metabolized in the liver. It exhibits moderate anticoagulant effects by inhibiting vitamin K between 48 and 72 h after the start of administration. Because protein C and protein S, which are considered natural anticoagulants, may also decrease during the priming of VKA, the risk of thrombosis and skin necrosis increases in the first 2 or 3 days of VKA use. Therefore, during this period, VKA should be administered with heparin. The effect of VKA is affected by the patient’s liver function, concurrent medication, and food intake; therefore, careful monitoring is required.
Dabigatran directly inhibits factor IIa, while rivaroxaban, apixaban, and edoxaban inhibit factor Xa. Several large-scale phase 3 studies have compared DOAC therapies with VKA, confirming that DOACs are not inferior in terms of antithrombotic efficacy and bleeding [8-11]. Thus, DOACs have been used instead of VKA for the treatment of VTE. The major drug absorption sites of rivaroxaban, dabigatran, and edoxaban are the stomach and the proximal small intestine. Therefore, in patients with previous total gastrectomy, these drugs should be taken with caution because they may not be absorbed efficiently. Unlike other DOACs, apixaban is mostly absorbed in the distal small intestine and ascending colon and can be safely used in patients who have undergone gastrectomy; however, it should be avoided in patients who have previously undergone resection of the ascending colon [12]. Dabigatran is produced as a capsule formulation. Thus, when the capsule of dabigatran is opened and the contents are taken alone, its bioavailability rises rapidly. Opening, crushing, or chewing dabigatran capsules is prohibited.
For the use of DOACs in cases of CAT, see the section ‘Treatment of cancer-associated venous thromboembolism’.
Anticoagulation in special situations
Anticoagulation in renal insufficiency: Because the main excretion site of DOACs is the kidney, the anticoagulant effect of DOACs increases in the presence of renal insufficiency, and the likelihood of bleeding complications also increases. Since patients with renal insufficiency were not included in the clinical trials of DOACs (for example, a creatinine clearance of <30 mL/min was an exclusion criterion for an edoxaban trial [13]), attention should be given to the use of DOACs in cases of renal insufficiency. Conversely, LMWH, such as dalteparin, can be used safely in patients with moderate renal impairment. The use of anticoagulants according to renal function is summarized in Table 1.
Table 1.
Use of anticoagulants for the treatment of venous thromboembolism in patients with renal insufficiency.
| Anticoagulant | Recommendationa) |
|---|---|
| Unfractionated heparin | CrCl ≥30 mL/min: no adjustment |
| CrCl <30 mL/min: no adjustment, use with caution | |
| LMWH | CrCl ≥30–80 mL/min: no adjustment, use with caution |
| CrCl <30 mL/min: enoxaparin - 1 mg/kg subcutaneously once a day, use with caution, anti-Xa monitoring is recommended if applicable; dalteparin - dose adjustment according to anti-Xa activity, use with caution | |
| Warfarin | No adjustment recommended |
| Edoxaban | CrCl ≥50 mL/min: no adjustment |
| CrCl 15–49 mL/min: 30 mg once daily | |
| CrCl <15 mL/min: not recommended | |
| Dabigatran | CrCl ≥50 mL/min: no adjustment |
| CrCl 30–49 mL/min: 110 mg twice daily | |
| CrCl <30 mL/min: not recommended | |
| Rivaroxaban/Apixaban | CrCl ≥30 mL/min: no adjustment |
| CrCl 15–29 mL/min: no adjustment, use with caution | |
| CrCl <15 mL/min: not recommended |
a)Detailed recommendations may differ slightly according to guidelines and in the context of clinical trials. The list above is based on the approval package of each drug from the Korean Food and Drug Safety (KFDS) for the treatment of venous thromboembolism.
Abbreviations: CrCl, creatinine clearance; LMWH, low-molecular-weight heparin.
Anticoagulation in thrombocytopenia: In cases of CAT with thrombocytopenia, mostly in hematologic malignancies, LMWH is the preferred anticoagulant because of its shorter half-life and better safety profile than VKA. DOACs may also be considered for these patients. However, the pivotal trials of DOACs for CAT excluded patients with a platelet count <50,000×109/L [13], or even <75,000×109/L [14]; thus, there is insufficient data on whether DOACs can replace LMWH in the setting of CAT combined with significant thrombocytopenia. Therefore, the use of DOACs in patients with thrombocytopenia requires caution, and decisions should be individualized until more robust evidence is gathered.
Thrombolytic therapy and inferior vena cava filter insertion: Sometimes, thrombolytic therapy can be administered either through systemic infusion via a vein or directly to the thrombus by inserting a catheter. However, as the risk of bleeding increases, this method should be considered only in cases of hemodynamically unstable PE. An inferior vena cava (IVC) filter can be considered in patients with DVT to prevent PE when anticoagulation is contraindicated (e.g., bleeding), but the general use of IVC filters or permanent indwelling hardware should be avoided [15].
TREATMENT OF VENOUS THROMBOEMBOLISM
Treatment of deep vein thrombosis
Treatment of proximal deep vein thrombosis: Proximal lower extremity DVT occurs when a thrombus is located in the popliteal, femoral, or iliac veins. Clinical symptoms vary according to the anatomy, extent, and degree of occlusion, and range from asymptomatic to extensive edema and gangrene. Anticoagulant therapy is indicated for all patients with proximal DVT [16]. In the case of active hemorrhage, lower platelet counts (<50,000×109/L) or prior intracerebral hemorrhage, an IVC filter is preferable. Recommendations for the treatment of provoked proximal DVT includes 3 months of anticoagulant therapy [16]. In patients with an unprovoked proximal DVT, extended anticoagulant therapy (at least 3 months and potentially indefinite) is preferred, while in patients with high bleeding risk, 3 months of anticoagulant therapy is recommended [16]. Therapeutic options for proximal DVT include VKA, LMWH or DOACs. A selection among these agents is usually made based on clinician experience, as well as the risks of bleeding, patient comorbidities, preferences, cost, and convenience. Thrombolytic therapy is not recommended, except for patients with massive iliofemoral or femoral DVT with a high risk of limb gangrene [16].
Treatment of isolated distal deep vein thrombosis: Isolated distal DVT is diagnosed when a thrombus forms below the popliteal vein without extension to the proximal veins. The decision of whether to treat isolated DVT is controversial, as the 3-month recurrent VTE risks of isolated distal DVT between the untreated and treated groups were discordant between studies [17-20], although the absolute risk of VTE recurrence is reportedly lower than that of proximal DVT or PE. In addition, in contrast to proximal DVT and PE, a guideline for the management of isolated DVT is not supported by high-level evidence. A meta-analysis of 24 studies involving 4,072 patients reported that anticoagulation reduced VTE recurrence rate compared to no anticoagulant treatment [odds ratio (OR), 0.50; 95% confidence interval (CI), 0.31–0.79], without increasing the rate of major bleeding (OR, 0.64; 95% CI, 0.15–2.73) [21]. In contrast, based on the evidence of a randomized placebo-controlled prospective trial [22], asymptomatic patients without high-risk features of VTE recurrence or extension (immobilization, active cancer, unprovoked VTE) and with a high risk of bleeding, may undergo surveillance with serial screening for DVT of the lower leg without anticoagulation. However, if patients are acutely symptomatic, have high-risk features for recurrence and extension, and are without bleeding risk, anticoagulation is recommended [16]. Aspirin is often used instead of an anticoagulant, considering the less aggressive nature of isolated distal DVT, but this method lacks firm evidence [23]. After the decision to anticoagulate, the choice of drugs and duration may follow the treatment strategies for proximal DVT of the lower extremities.
Treatment of pulmonary embolism
Treatment of hemodynamically unstable pulmonary embolism: Patients with life-threatening PE may require additional treatment beyond anticoagulation, including systemic thrombolysis, catheter-directed therapy, and embolectomy. A meta-analysis showed that the use of thrombolytics was associated with lower all-cause mortality. The reduction in mortality seems to be mainly accounted for by studies including hemodynamically unstable patients [24]. Anticoagulation should be started when the patient becomes stable, without bleeding complications after thrombolysis.
Treatment of hemodynamically stable pulmonary embolism: Anticoagulation is the mainstay of treatment for patients with confirmed PE and should be given to all patients with suspicion of the disease in the absence of active bleeding, even before a diagnosis of PE is confirmed. The anticoagulation of patients with PE has changed considerably in recent years, since DOACs were introduced. DOACs have shown similar efficacy and safety to those of conventional anticoagulants in patients with acute PE in several large randomized clinical trials [8-11, 25]. The risk reduction for recurrent VTE with different DOACs has not been directly compared, but based on indirect comparisons, it appears to be similar among all DOACs.
The recommended treatment duration for PE is usually 6 months but may range from 3 months in patients with a transient risk factor to indefinite in patients with ongoing major risk factors (e.g., cancer, recurrent unprovoked PE).
Treatment of subsegmental pulmonary embolism: Subsegmental pulmonary embolism (SSPE) is diagnosed when PE does not involve the proximal pulmonary arteries. The decision on whether to treat asymptomatic SSPE patients remains to be an issue; a recommendation cannot be supported by high-quality randomized clinical trials, because computed tomographic (CT) angiography may result in a false-positive diagnosis (especially in cases with a single subsegmental involvement in 1 image and normal D-dimer), and the data with respect to whether SSPE could be progressive or recurrent without anticoagulation are still controversial [26, 27]. Patients with SSPE should undergo bilateral Doppler ultrasonography of the lower extremities [28], and high-risk DVT sites, such as upper extremities with indwelling central venous catheters. Patients who are asymptomatic, have no co-existing DVT or high-risk features [29] of recurrent or progressive VTE (immobilization, active cancer, unprovoked VTE), and are at high risk of bleeding may undergo surveillance with serial screening for DVT of the lower leg without anticoagulation. However, if patients are symptomatic, have co-existing DVT and/or high-risk features, and have no bleeding risk, anticoagulation should be suggested rather than surveillance only. When deciding on anticoagulation, the choice of drugs and duration may follow the treatment strategies recommended for PE in larger pulmonary arteries.
Incidental pulmonary embolism: Incidental PE is frequently reported on enhanced chest CT scans. Although the embolic load in incidental PE is usually lower than that in symptomatic PE, anticoagulation should be initiated if it involves a location proximal to the subsegmental vasculature [30]. In cases of incidental SSPE, the data are conflicting, as discussed in Section 4.2.3. Some investigators suggest observation without the use of anticoagulants in this group.
Treatment of cancer-associated venous thromboembolism
CAT is a common complication of cancer, associated with high morbidity and mortality rates. Once CAT is confirmed, physicians should consider anticoagulant therapy regardless of whether or not a patient has thrombosis-related symptoms. However, limited life expectancy with advanced cancer, high bleeding risks especially in severe thrombocytopenia, or thrombotic symptoms that cannot be expected to improve are factors that prevent the initiation of anticoagulation.
In accordance with major clinical trials comparing LMWH with VKA [14, 31], LMWH was previously the standard treatment for CAT, owing to its efficacy against thrombosis recurrence and improved safety profile compared to VKA. Recently, DOACs have emerged as potential alternative therapies to LMWH owing to their convenient route of administration and predictable pharmacokinetics. However, evidence for their use in CAT is inconclusive, as only a small fraction of the study populations in these trials had CAT [32]. Recently, a Korean phase IV study with rivaroxaban [6] and 2 phase III trials comparing DOACs to LMWH in patients with CAT [13, 33] reported comparable efficacies with slightly increased bleeding risk for DOACs. Based on the results of these 2 randomized controlled trials, the latest guidelines included rivaroxaban and edoxaban as options for VTE treatment [34]. Careful choice of treatment candidates and proper anticoagulant strategies are critical for the treatment of CAT [34, 35]. For anticoagulation in patients with CAT and thrombocytopenia, see the subsection ‘Anticoagulation in thrombocytopenia’.
Treatment of venous thrombosis of other sites
Treatment of superficial venous thrombophlebitis: Although superficial thrombophlebitis is considered benign and self-limiting, there is increasing recognition that a significant proportion of those presenting with this disorder will have concomitant DVT or PE or are at a significant risk of developing VTE [36]. The treatment of superficial thrombophlebitis remains controversial. However, therapeutic strategies must include symptomatic relief, limitation of thrombosis extension, and reduction in PE risk. A randomized controlled trial showed that anticoagulation with UFH, LMWH, and VKA were superior to compression therapy alone in reducing superficial thrombophlebitis extension [37, 38]. The SURPRISE study suggested the usability of an oral anticoagulant (rivaroxaban) in patients with superficial thrombophlebitis [39]. Current guidelines recommend treating superficial thrombophlebitis of at least 5 cm in length with prophylactic doses of fondaparinux or LMWH for 45 days, but guidelines state that for patients with less extensive superficial thrombophlebitis, anticoagulant treatment is not necessary [16].
Treatment of catheter-related venous thrombosis: Thrombotic complications associated with the use of catheters are common in patients with cancer, leading to patient distress, catheter dysfunction, and infection. There are no large, prospective, randomized trials of treatments for catheter-related thrombosis [40]. Symptomatic catheter-related thrombosis is treated with anticoagulation alone, generally without catheter removal. The optimal duration of anticoagulation for catheter-related thrombosis has not been investigated in clinical trials. The American College of Chest Physicians (ACCP) guidelines recommend anticoagulation for 3 months if the catheter has been removed and for as long as the catheter is in place if >3 months [16]. Recently, DOACs can reportedly be used in cancer patients with catheter-related thrombosis [41, 42]. Multiple reviews of strategies for preventing catheter-related thrombosis are available [43, 44].
Treatment of splanchnic vein thrombosis: Splanchnic vein thrombosis (SVT) is the most common form of unusual site thrombosis, comprising approximately 4% of all thrombotic events. SVT encompasses thrombosis in the portal, mesenteric, hepatic, and splenic veins [45]. Doppler ultrasonography is the first-line choice for the diagnosis of portal and hepatic vein thrombosis, and CT angiography is the diagnostic modality of choice for detecting mesenteric vein thrombosis [46]. The most common acquired risk factors for SVT are abdominal cancers (especially hepatobiliary, gastrointestinal, and pancreatic), liver cirrhosis, and myeloproliferative neoplasms (MPNs). Thus, in non-cirrhotic, non-malignant SVT patients, screening for MPNs (i.e., JAK2 mutation analysis) and paroxysmal nocturnal hemoglobinuria is recommended, even in patients with normal complete blood cell counts [47]. No high-quality randomized controlled trial has yet been reported, but several guidelines or reviews have suggested the management of SVTs [48-51]. Acute, symptomatic, extensive SVTs, and patients planning to undergo liver transplantation are recommended to undergo anticoagulation over surveillance. Esophageal or fundic varices, especially in cirrhotic patients, are not a contraindication for anticoagulation, but adequate prophylactic treatment (with β-blockers, endoscopic ligation, etc.) should precede anticoagulation. To date, there is no data on DOACs for the treatment of SVTs. UFH, LMWH, and heparin transition to VKA are recommended for SVTs. At least 3 months of anticoagulation is recommended for all SVT patients; patients with transient risk factors (surgery, infections) may discontinue treatment after 3 months of anticoagulation, but patients with cirrhosis, active cancer, MPNs, and other thrombophilic conditions should undergo extended anticoagulation while weighing its risks and benefits. In every circumstance, gastrointestinal bleeding should be monitored before or during anticoagulation and should be properly controlled.
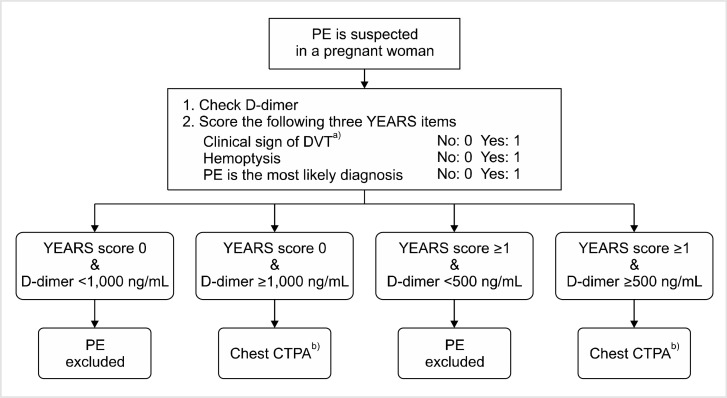
Venous thromboembolism associated with pregnancy
Although its absolute risk is low (0.6–1.2 of every 1,000 deliveries) [52], VTE is an important issue in pregnant women, as it is one of the most common causes of maternal morbidity and mortality [53]. Among VTE cases, PE is a particularly important cause of maternal death. For pregnant women with suspected PE, undergoing computed tomographic pulmonary angiography (CTPA) or ventilation-perfusion scan is often inevitable because of the limited diagnostic specificity and sensitivity of D-dimer. A recently published pregnancy-adapted YEARS algorithm for the diagnosis of suspected PE can be used to rule out PE safely; in a prospective study, 32–65% of patients avoided unnecessary CTPA scanning, with the highest efficiency during the 1st trimester (Fig. 2) [54].
Fig. 2.
Pregnancy-adapted YEARS algorithm for suspected acute pulmonary embolism in pregnant patients. a)If a woman has clinical sign of DVT, check compression ultrasonography of the symptomatic leg and initiate anticoagulant if DVT is confirmed. b)Initiate ant-icoagulant if chest CTPA indicates PE.
Abbreviations: CTPA, computed pulmonary angiography; DVT, deep vein thrombosis; PE, pulmonary embolism.
Pregnant women with acute VTE should receive anticoagulation. VKA is contraindicated due to the risk of fetal malformations. The safety of DOACs is not supported by the literature, and concerns have been raised regarding fetal safety in some studies [55]. LMWH is preferred over UFH in terms of convenience.
In times of delivery, a scheduled delivery is suggested if a therapeutic dose of LMWH is administered, based on a 1.9-fold increased risk of bleeding in spontaneous labor compared to planned delivery [56]. In contrast, spontaneous labor is allowed if a woman receives only a prophylactic dose of LMWH [53]. For breastfeeding women, UFH, LMWH, and VKA are considered safe anticoagulants, while DOACs are not yet recommended because of insufficient data [53].
Venous thromboembolism in children
Cause and risk factors of venous thromboembolism in children: Venous thrombosis in children is rare and is mostly associated with multifactorial medical conditions [57]. The incidence of symptomatic VTE in neonates is 0.51 per 10,000 [58], and in children, 0.07 to 0.14 per 10,000 [59, 60]. In the Canadian registry, 96% of DVT/PE cases were associated with medical conditions, including cancer, congenital heart disease, or trauma. The single most important and frequent risk factor for VTE is a central venous catheter (CVC) [61], found in 33–48% of VTE cases in children [59, 61]. The rate of CVC as a risk factor is as high as 94% in neonates [59]. In contrast, inherited thrombophilia was reported in only 8.8% of the cohort [61]. Factor V Leiden and prothrombin gene mutations are frequent in Caucasian patients but not in those of Asian ethnicity. The incidence of protein C deficiency is 0.2–0.5% in the general population but 2–5% in VTE individuals [62-65]. Measurement of protein S is very challenging, and the incidence of deficiency is thought to be as low as 0.9% [66]. The prevalence of hereditary antithrombin III deficiency is estimated to be 0.03–0.8% [67].
The utility of diagnostic tests for inherited thrombophilia in children: A panel of tests for thrombophilia should include factor V Leiden mutations; prothrombin 20210 mutations; deficiencies of antithrombin, protein C, and protein S; homocysteine levels; factor VIII levels; lipoprotein levels; and detection of antiphospholipid antibodies [68]. The developmental stage of the hemostatic system in children, physiologically lower levels of coagulant and anticoagulant proteins, and other confounding factors, such as concomitant use of drug, infection, or inflammation, should be addressed [68-70]. Generally, the tests for thrombophilia do not change decisions about the initiation and duration of acute management, except for specific patients with purpura fulminans complicating severe protein C or S deficiency or cases with VKA-induced skin necrosis [71-73].
Testing in patients with unprovoked, spontaneous, or recurrent thrombotic events, which are rare in children and adolescents, may help to identify inherited thrombophilia and guide management [57, 68]. Up to half of VTE events at unusual sites, such as the cerebral or splanchnic veins, and stroke are associated with inherited thrombophilia, and the patients are candidates for testing [74, 75]. Therefore, testing after the 1st episode of CVC-related VTE without a strong family history (a first-degree relative with VTE in patients under 40 years old) is not generally recommended [76].
Treatment of venous thromboembolism in children: Treatment recommendations for pediatric VTE are based on studies from adult populations, as scarce evidence exists in children [77]. Treatment options for VTE in children include anticoagulation, thrombolysis, surgery, and observation [78]. Potential benefits must be weighed against risks in premature neonates and critically ill children who are at high risk of bleeding [79]. Options for acute anticoagulation include UFH or LMWH, but LMWH is more frequently used because of the ease of dosing and the low need for monitoring [79]. After an acute period of anticoagulation with UFH or LMWH, patients may continue to receive LMWH, or a transition may be made to VKA [77]. When starting a patient on VKA, UFH or LMWH, admnistration should be continued until the international normalized ratio (INR) reaches the therapeutic range and remains there for 2 days. In most cases, this process takes 5 to 7 days [77]. Anticoagulation with LMWH or VKA, rather than no anticoagulation, is recommended in children with symptomatic DVT or PE [77, 78]. It is suggested to use anticoagulation for ≤3 months in children with provoked DVT or PE and for 6 to 12 months in unprovoked DVT or PE [77]. Patients with recurrent thrombosis and antiphospholipid antibody syndrome often require indefinite anticoagulation [72]. Therapeutic UFH in children is titrated to achieve an activated partial thromboplastin time range (aPTT) of 1.5 to 2.5 times the upper limit of normal [77]. For neonates and children receiving either once- or twice-daily therapeutic LMWH, the drug needs to be monitored with a target anti-Xa activity range of 0.5 to 1.0 unit/mL in a sample taken 4 to 6 h after subcutaneous injection [77]. For children receiving VKA, the drug needs to be monitored to a target INR of 2.5 (range, 2.0–3.0), except for those with prosthetic cardiac valves, who are recommended to adhere to the adult guidelines [77]. Symptomatic CVC-related thrombi can be treated without removal if the catheter is functioning. A nonfunctioning or unnecessary catheter should be removed after 3 to 5 days of therapeutic anticoagulation. The total recommended anticoagulant duration is between 6 weeks and 3 months [77]. Thrombolytic therapy should be used only for life- or limb-threatening thrombosis [78]. Thrombectomy followed by anticoagulation or IVC filter insertion is not recommended except in specific, limited circumstances; rather, anticoagulation alone should be used in children with symptomatic DVT or PE [78]. DOACs have potential benefits for children, including oral administration, and possibly no need for monitoring. Many clinical trials of DOACs are underway, but the routine use of DOACs is not yet recommended in children [80].
TREATMENT AFTER AN INITIAL FAILURE OF ANTICOAGULATION
To date, there has been no randomized trial or prospective cohort study to guide treatment after an initial failure of anticoagulation. Inadequate anticoagulation (inadequate dosage, poor compliance, discontinuation for an anticipated procedure, malabsorption) is the most common cause of recurrent VTE during therapy. However, recurrent VTE should be confirmed by radiologic testing and should be examined for other etiologies, such as malignancy, May-Thurner syndrome, inherited thrombotic disorders, or antiphospholipid antibody syndrome. Treatment options for initial failure include increasing the dose or administration frequency of the anticoagulants or alternate agents. In patients receiving VKA (with an INR of 2.0 to 3.0) or an adequate dose of a DOAC, the guideline recommends changing to LMWH at least temporarily [16]. In patients receiving LMWH, the guidelines recommend increasing the LMWH dose by 25 to 33% [16]. The efficacy of DOACs in this population has not yet been studied.
REVERSAL OF ANTICOAGULATION
In VTE patients, anticoagulation reversal is required in times of bleeding, invasive procedures or surgery, and over-anticoagulation. Reversal should be decided according to the situation of an individual patient, balancing the benefits and risks [81]. Table 2 summarizes the key pharmacokinetic features and the approved or potential antidotes for anticoagulants.
Table 2.
Characteristics of common anticoagulants and its approved or potential antidotes.
| Anticoagulants | Metabolism and excretion | Plasma half-life | Antidotes |
|---|---|---|---|
| UFH | Rapid endothelial internalization | 40–90 minutes | Protamine sulfate |
| Slow renal clearance | |||
| LMWH | Renal excretion | 4 hours | Protamine sulfate (ciraparantaga)) |
| VKA | Hepatic metabolism | 40 hours | Oral or IV Vitamin K |
| Fresh frozen plasma | |||
| Dabigatran | 80% renal, 20% hepatic | 13 hours | Idarucizumab (ciraparantaga)) |
| Apixaban | 27% renal, 73% hepatic | 12 hours | Andexanet alfa (ciraparantaga)) |
| Edoxaban | 50% renal, 50% hepatic | 10–14 hours | (andexanet alfa, ciraparantaga)) |
| Rivaroxaban | 35% renal, 65% hepatic | 5–9 hours | Andexanet alfa (ciraparantaga)) |
a)Under investigation.
Abbreviations: IV, intravenous; LMWH, low-molecular-weight heparin; UFH, unfractionated heparin; VKA, vitamin K antagonist.
Oral or intravenous vitamin K can be used for severe prolongation (>8) or moderate prolongation (5–8) of the INR with bleeding or significant risk of bleeding [82]. Fresh frozen plasma is commonly used because of its low cost and ease of use. Protamine sulfate is an approved drug for the reversal of UFH. It should be slowly infused with doses of 1 mg per 80–100 U of UFH for neutralization [83]. Although LMWH has a stronger inhibitory effect on Xa than on thrombin, protamine sulfate can be considered as an antidote for LMWH at a dose of 1 mg per 100 U of LMWH [83].
Novel antidotes for DOACs are currently available in some countries or under clinical trials. Idarucizumab is an engineered antibody fragment with a structure similar to that of thrombin; it binds to dabigatran. It showed good reversal efficacy in a pivotal phase III trial [84] and was approved by the United States (U.S.) Food and Drug Administration (FDA) in 2015. Andexanet alfa is a modified, recombinant human factor Xa protein that binds to factor Xa inhibitors and LMWH but is catalytically inactive. It received U.S. FDA accelerated approval for patients taking rivaroxaban or apixaban who require reversal. Recently, full data from a multicenter, open-label study were published; among patients taking factor Xa inhibitors suffering from major bleeding, andexanet alfa resulted in 82% excellent or good hemostatic efficacy at 12 hours with remarkably reduced anti-Xa activity [85]. Ciraparantag is another broad-spectrum reversal agent under investigation. It is a synthetic small molecule that binds to and inhibits Xa inhibitors, UFH, LMWH, and fondaparinux [86].
MONITORING AND DRUG-DRUG INTERACTION OF DOACS
DOACs can be used at fixed doses without testing levels in most patients, and this feature is obviously an advantage of DOACs compared to VKA. However, emerging data suggest that measuring the DOAC concentration would be beneficial in certain critical circumstances [87]. If done properly, monitoring of DOACs can guide decision-making regarding the pursuit of invasive procedures or the use of costly reversal agents. In conventional laboratory testing, thrombin time and aPTT can reflect the activity of dabigatran [88] but are imperfect and often result in false-negative findings, particularly for aPTT [89]. Prothrombin time and/or aPTT are often prolonged after the use of Xa inhibitors, but the degree of prolongation does not correlate with DOAC levels, and the results vary according to the reagents used [90]. Chromogenic assays for anti-Xa are reliable and relatively cost-effective, with proper calibration [91]. Liquid chromatography/tandem mass spectrometry is the gold standard method for monitoring DOACs, but it is not practical for clinical laboratory use [92]. Future development of DOAC-specific tests with good test reliability, faster turnaround time, and affordable cost are necessary to monitor DOACs more accurately and provide clinical benefits.
Drug-drug interactions involving DOACs can arise either via pharmacokinetic or pharmacodynamic mechanisms [93]. DOACs are pharmacokinetically dependent on varying degrees of cytochrome CYP3A and P-glycoprotein. Therefore, concomitant administration of commonly used drugs can alter DOAC activity. The pharmacodynamics of DOACs can be augmented by some classes of drugs, such as antiplatelet compounds, nonsteroidal anti-inflammatory drugs, and selective serotonin or noradrenaline reuptake inhibitors [93]. The use of other drugs should be carefully checked, and the prescription should be adjusted by a professional pharmacist while considering potential drug-drug interactions, especially in the elderly with polypharmacy or cancer patients undergoing active treatment.
CONCLUSION
The treatment of VTE has changed significantly in recent years, after the insurance coverage of DOACs began. The emergence of anticoagulants with a lower risk of bleeding and easy use has led to the replacement of warfarin and heparin by DOACs in most situations where anticoagulation is indicated.
In the future, 2 factors need to be considered to improve the Korean VTE treatment guidelines. First, studies examining whether lower doses of anticoagulants can maintain their therapeutic effects while reducing bleeding side effects are a worldwide issue. These studies are necessary, particularly for Korean VTE patients with a high risk of bleeding. Second, the diagnosis of asymptomatic incidental VTE is increasing due to a changing medical environment, and updated treatment guidelines are urgently required. The current recommendations are based not only on insufficient evidence, but also mostly on Western data. Therefore, recommendations need to be amended based on Korean data in the future.
Footnotes
Authors’ Disclosures of Potential Conflicts of Interest
No potential conflicts of interest relevant to this article were reported.
REFERENCES
- 1.Lee CH, Lin LJ, Cheng CL, Kao Yang YH, Chen JY, Tsai LM. Incidence and cumulative recurrence rates of venous thrombo-embolism in the Taiwanese population. J Thromb Haemost. 2010;8:1515–23. doi: 10.1111/j.1538-7836.2010.03873.x. [DOI] [PubMed] [Google Scholar]
- 2.Jang MJ, Bang SM, Oh D. Incidence of venous thromboembolism in Korea: from the Health Insurance Review and Assessment Service database. J Thromb Haemost. 2011;9:85–91. doi: 10.1111/j.1538-7836.2010.04108.x. [DOI] [PubMed] [Google Scholar]
- 3.Hong J, Lee JH, Yhim HY, et al. Incidence of venous thrombo-embolism in Korea from 2009 to 2013. PLoS One. 2018;13:e0191897. doi: 10.1371/journal.pone.0191897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goldhaber SZ, Bounameaux H. Pulmonary embolism and deep vein thrombosis. Lancet. 2012;379:1835–46. doi: 10.1016/S0140-6736(11)61904-1. [DOI] [PubMed] [Google Scholar]
- 5.White RH. The epidemiology of venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I4–8. doi: 10.1161/01.CIR.0000078468.11849.66. [DOI] [PubMed] [Google Scholar]
- 6.Yhim HY, Choi WI, Kim SH, et al. Long-term rivaroxaban for the treatment of acute venous thromboembolism in patients with active cancer in a prospective multicenter trial. Korean J Intern Med. 2019;34:1125–35. doi: 10.3904/kjim.2018.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boon GJAM, Van Dam LF, Klok FA, Huisman MV. Management and treatment of deep vein thrombosis in special populations. Expert Rev Hematol. 2018;11:685–95. doi: 10.1080/17474086.2018.1502082. [DOI] [PubMed] [Google Scholar]
- 8.EINSTEIN-PE Investigators, author. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012;366:1287–97. doi: 10.1056/NEJMoa1113572. [DOI] [PubMed] [Google Scholar]
- 9.Agnelli G, Buller HR, Cohen A, et al. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369:799–808. doi: 10.1056/NEJMoa1302507. [DOI] [PubMed] [Google Scholar]
- 10.Hokusai-VTE Investigators, author. Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med. 2013;369:1406–15. doi: 10.1056/NEJMoa1306638. [DOI] [PubMed] [Google Scholar]
- 11.Schulman S, Kearon C, Kakkar AK, et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361:2342–52. doi: 10.1056/NEJMoa0906598. [DOI] [PubMed] [Google Scholar]
- 12.Hakeam HA, Al-Sanea N. Effect of major gastrointestinal tract surgery on the absorption and efficacy of direct acting oral anticoagulants (DOACs) J Thromb Thrombolysis. 2017;43:343–51. doi: 10.1007/s11239-016-1465-x. [DOI] [PubMed] [Google Scholar]
- 13.Raskob GE, van Es N, Verhamme P, et al. Edoxaban for the treatment of cancer-associated venous thromboembolism. N Engl J Med. 2018;378:615–24. doi: 10.1056/NEJMoa1711948. [DOI] [PubMed] [Google Scholar]
- 14.Lee AY, Levine MN, Baker RI, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349:146–53. doi: 10.1056/NEJMoa025313. [DOI] [PubMed] [Google Scholar]
- 15.Galanaud JP, Laroche JP, Righini M. The history and historical treatments of deep vein thrombosis. J Thromb Haemost. 2013;11:402–11. doi: 10.1111/jth.12127. [DOI] [PubMed] [Google Scholar]
- 16.Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149:315–52. doi: 10.1016/j.chest.2015.11.026. [DOI] [PubMed] [Google Scholar]
- 17.Horner D, Hogg K, Body R, Nash MJ, Baglin T, Mackway-Jones K. The anticoagulation of calf thrombosis (ACT) project: results from the randomized controlled external pilot trial. Chest. 2014;146:1468–77. doi: 10.1378/chest.14-0235. [DOI] [PubMed] [Google Scholar]
- 18.Lagerstedt CI, Olsson CG, Fagher BO, Oqvist BW, Albrechtsson U. Need for long-term anticoagulant treatment in symptomatic calf-vein thrombosis. Lancet. 1985;2:515–8. doi: 10.1016/S0140-6736(85)90459-3. [DOI] [PubMed] [Google Scholar]
- 19.Pinede L, Ninet J, Duhaut P, et al. Comparison of 3 and 6 months of oral anticoagulant therapy after a first episode of proximal deep vein thrombosis or pulmonary embolism and comparison of 6 and 12 weeks of therapy after isolated calf deep vein thrombosis. Circulation. 2001;103:2453–60. doi: 10.1161/01.CIR.103.20.2453. [DOI] [PubMed] [Google Scholar]
- 20.Schwarz T, Buschmann L, Beyer J, Halbritter K, Rastan A, Schellong S. Therapy of isolated calf muscle vein thrombosis: a randomized, controlled study. J Vasc Surg. 2010;52:1246–50. doi: 10.1016/j.jvs.2010.05.094. [DOI] [PubMed] [Google Scholar]
- 21.Franco L, Giustozzi M, Agnelli G, Becattini C. Anticoagulation in patients with isolated distal deep vein thrombosis: a meta-analysis. J Thromb Haemost. 2017;15:1142–54. doi: 10.1111/jth.13677. [DOI] [PubMed] [Google Scholar]
- 22.Righini M, Galanaud JP, Guenneguez H, et al. Anticoagulant therapy for symptomatic calf deep vein thrombosis (CACTUS): a randomised, double-blind, placebo-controlled trial. Lancet Haematol. 2016;3:e556–62. doi: 10.1016/S2352-3026(16)30131-4. [DOI] [PubMed] [Google Scholar]
- 23.Ho P, Lim HY, Chua CC, et al. Retrospective review on isolated distal deep vein thrombosis (IDDVT) - a benign entity or not? Thromb Res. 2016;142:11–6. doi: 10.1016/j.thromres.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 24.Chatterjee S, Chakraborty A, Weinberg I, et al. Thrombolysis for pulmonary embolism and risk of all-cause mortality, major bleeding, and intracranial hemorrhage: a meta-analysis. JAMA. 2014;311:2414–21. doi: 10.1001/jama.2014.5990. [DOI] [PubMed] [Google Scholar]
- 25.Schulman S, Kakkar AK, Goldhaber SZ, et al. Treatment of acute venous thromboembolism with dabigatran or warfarin and pooled analysis. Circulation. 2014;129:764–72. doi: 10.1161/CIRCULATIONAHA.113.004450. [DOI] [PubMed] [Google Scholar]
- 26.Carrier M, Righini M, Le Gal G. Symptomatic subsegmental pulmonary embolism: what is the next step? J Thromb Haemost. 2012;10:1486–90. doi: 10.1111/j.1538-7836.2012.04804.x. [DOI] [PubMed] [Google Scholar]
- 27.Goy J, Lee J, Levine O, Chaudhry S, Crowther M. Sub-segmental pulmonary embolism in three academic teaching hospitals: a review of management and outcomes. J Thromb Haemost. 2015;13:214–8. doi: 10.1111/jth.12803. [DOI] [PubMed] [Google Scholar]
- 28.Raskob GE. Importance of subsegmental pulmonary embolism. Blood. 2013;122:1094–5. doi: 10.1182/blood-2013-06-508440. [DOI] [PubMed] [Google Scholar]
- 29.den Exter PL, van Es J, Klok FA, et al. Risk profile and clinical outcome of symptomatic subsegmental acute pulmonary embolism. Blood. 2013;122:1144–9. quiz 1329. doi: 10.1182/blood-2013-04-497545. [DOI] [PubMed] [Google Scholar]
- 30.O'Connell C. Incidentally found pulmonary embolism: what's the clinician to do? Hematology Am Soc Hematol Educ Program. 2015;2015:197–201. doi: 10.1182/asheducation-2015.1.197. [DOI] [PubMed] [Google Scholar]
- 31.Lee AYY, Kamphuisen PW, Meyer G, et al. Tinzaparin vs warfarin for treatment of acute venous thromboembolism in patients with active cancer: a randomized clinical trial. JAMA. 2015;314:677–86. doi: 10.1001/jama.2015.9243. [DOI] [PubMed] [Google Scholar]
- 32.Vedovati MC, Germini F, Agnelli G, Becattini C. Direct oral anticoagulants in patients with VTE and cancer: a systematic review and meta-analysis. Chest. 2015;147:475–83. doi: 10.1378/chest.14-0402. [DOI] [PubMed] [Google Scholar]
- 33.Young AM, Marshall A, Thirlwall J, et al. Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: results of a randomized trial (SELECT-D) J Clin Oncol. 2018;36:2017–23. doi: 10.1200/JCO.2018.78.8034. [DOI] [PubMed] [Google Scholar]
- 34.Key NS, Khorana AA, Kuderer NM, et al. Venous thrombo-embolism prophylaxis and treatment in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2020;38:496–520. doi: 10.1200/JCO.19.01461. [DOI] [PubMed] [Google Scholar]
- 35.Kim SA, Yhim HY, Bang SM. Current management of cancer-associated venous thromboembolism: focus on direct oral anticoagulants. J Korean Med Sci. 2019;34:e52. doi: 10.3346/jkms.2019.34.e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scott G, Mahdi AJ, Alikhan R. Superficial vein thrombosis: a current approach to management. Br J Haematol. 2015;168:639–45. doi: 10.1111/bjh.13255. [DOI] [PubMed] [Google Scholar]
- 37.Di Nisio M, Wichers I, Middeldorp S. Treatment of lower extremity superficial thrombophlebitis. JAMA. 2018;320:2367–8. doi: 10.1001/jama.2018.16623. [DOI] [PubMed] [Google Scholar]
- 38.Maddox RP, Seupaul RA. What is the most effective treatment of superficial thrombophlebitis? Ann Emerg Med. 2016;67:671–2. doi: 10.1016/j.annemergmed.2015.10.018. [DOI] [PubMed] [Google Scholar]
- 39.Beyer-Westendorf J, Schellong SM, Gerlach H, et al. Prevention of thromboembolic complications in patients with superficial-vein thrombosis given rivaroxaban or fondaparinux: the open-label, randomised, non-inferiority SURPRISE phase 3b trial. Lancet Haematol. 2017;4:e105–13. doi: 10.1016/S2352-3026(17)30014-5. [DOI] [PubMed] [Google Scholar]
- 40.Debourdeau P, Farge D, Beckers M, et al. International clinical practice guidelines for the treatment and prophylaxis of thrombosis associated with central venous catheters in patients with cancer. J Thromb Haemost. 2013;11:71–80. doi: 10.1111/jth.12071. [DOI] [PubMed] [Google Scholar]
- 41.Barco S, Atema JJ, Coppens M, Serlie MJ, Middeldorp S. Anticoagulants for the prevention and treatment of catheter-related thrombosis in adults and children on parenteral nutrition: a systematic review and critical appraisal. Blood Transfus. 2017;15:369–77. doi: 10.2450/2016.0031-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baumann Kreuziger L, Jaffray J, Carrier M. Epidemiology, diagnosis, prevention and treatment of catheter-related thrombosis in children and adults. Thromb Res. 2017;157:64–71. doi: 10.1016/j.thromres.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 43.Kahale LA, Tsolakian IG, Hakoum MB, et al. Anticoagulation for people with cancer and central venous catheters. Cochrane Database Syst Rev. 2018;6:CD006468. doi: 10.1002/14651858.CD006468.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kahn SR, Lim W, Dunn AS, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e195S–e226S. doi: 10.1378/chest.141.5.1369b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.De Stefano V, Martinelli I. Splanchnic vein thrombosis: clinical presentation, risk factors and treatment. Intern Emerg Med. 2010;5:487–94. doi: 10.1007/s11739-010-0413-6. [DOI] [PubMed] [Google Scholar]
- 46.Riva N, Ageno W. Approach to thrombosis at unusual sites: splanchnic and cerebral vein thrombosis. Vasc Med. 2017;22:529–40. doi: 10.1177/1358863X17734057. [DOI] [PubMed] [Google Scholar]
- 47.Smalberg JH, Arends LR, Valla DC, Kiladjian JJ, Janssen HL, Leebeek FW. Myeloproliferative neoplasms in Budd-Chiari syndrome and portal vein thrombosis: a meta-analysis. Blood. 2012;120:4921–8. doi: 10.1182/blood-2011-09-376517. [DOI] [PubMed] [Google Scholar]
- 48.Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e419S–e96S. doi: 10.1378/chest.141.5.1369b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.DeLeve LD, Valla DC, Garcia-Tsao G American Association for the Study Liver Diseases, author. Vascular disorders of the liver. Hepatology. 2009;49:1729–64. doi: 10.1002/hep.22772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ageno W, Riva N, Schulman S, et al. Long-term clinical outcomes of splanchnic vein thrombosis: results of an international registry. JAMA Intern Med. 2015;175:1474–80. doi: 10.1001/jamainternmed.2015.3184. [DOI] [PubMed] [Google Scholar]
- 51.Ageno W, Beyer-Westendorf J, Garcia DA, Lazo-Langner A, McBane RD, Paciaroni M. Guidance for the management of venous thrombosis in unusual sites. J Thromb Thrombolysis. 2016;41:129–43. doi: 10.1007/s11239-015-1308-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kourlaba G, Relakis J, Kontodimas S, Holm MV, Maniadakis N. A systematic review and meta-analysis of the epidemiology and burden of venous thromboembolism among pregnant women. Int J Gynaecol Obstet. 2016;132:4–10. doi: 10.1016/j.ijgo.2015.06.054. [DOI] [PubMed] [Google Scholar]
- 53.Bates SM, Rajasekhar A, Middeldorp S, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: venous thromboembolism in the context of pregnancy. Blood Adv. 2018;2:3317–59. doi: 10.1182/bloodadvances.2018024802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.van der Pol LM, Tromeur C, Bistervels IM, et al. Pregnancy-adapted YEARS algorithm for diagnosis of suspected pulmonary embolism. N Engl J Med. 2019;380:1139–49. doi: 10.1056/NEJMoa1813865. [DOI] [PubMed] [Google Scholar]
- 55.Lameijer H, Aalberts JJJ, van Veldhuisen DJ, Meijer K, Pieper PG. Efficacy and safety of direct oral anticoagulants during pregnancy; a systematic literature review. Thromb Res. 2018;169:123–7. doi: 10.1016/j.thromres.2018.07.022. [DOI] [PubMed] [Google Scholar]
- 56.Knol HM, Schultinge L, Veeger NJ, Kluin-Nelemans HC, Erwich JJ, Meijer K. The risk of postpartum hemorrhage in women using high dose of low-molecular-weight heparins during pregnancy. Thromb Res. 2012;130:334–8. doi: 10.1016/j.thromres.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 57.Klaassen IL, van Ommen CH, Middeldorp S. Manifestations and clinical impact of pediatric inherited thrombophilia. Blood. 2015;125:1073–7. doi: 10.1182/blood-2014-05-536060. [DOI] [PubMed] [Google Scholar]
- 58.Nowak-Göttl U, von Kries R, Göbel U. Neonatal symptomatic thromboembolism in Germany: two year survey. Arch Dis Child Fetal Neonatal Ed. 1997;76:F163–7. doi: 10.1136/fn.76.3.F163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van Ommen CH, Heijboer H, Büller HR, Hirasing RA, Heijmans HS, Peters M. Venous thromboembolism in childhood: a prospective two-year registry in The Netherlands. J Pediatr. 2001;139:676–81. doi: 10.1067/mpd.2001.118192. [DOI] [PubMed] [Google Scholar]
- 60.Chalmers EA. Epidemiology of venous thromboembolism in neonates and children. Thromb Res. 2006;118:3–12. doi: 10.1016/j.thromres.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 61.Andrew M, David M, Adams M, et al. Venous thromboembolic complications (VTE) in children: first analyses of the Canadian Registry of VTE. Blood. 1994;83:1251–7. doi: 10.1182/blood.V83.5.1251.1251. [DOI] [PubMed] [Google Scholar]
- 62.Miletich J, Sherman L, Broze G., Jr Absence of thrombosis in subjects with heterozygous protein C deficiency. N Engl J Med. 1987;317:991–6. doi: 10.1056/NEJM198710153171604. [DOI] [PubMed] [Google Scholar]
- 63.Tait RC, Walker ID, Reitsma PH, et al. Prevalence of protein C deficiency in the healthy population. Thromb Haemost. 1995;73:87–93. doi: 10.1055/s-0038-1653730. [DOI] [PubMed] [Google Scholar]
- 64.Mateo J, Oliver A, Borrell M, Sala N, Fontcuberta J. Laboratory evaluation and clinical characteristics of 2,132 consecutive unselected patients with venous thromboembolism--results of the Spanish Multicentric Study on Thrombophilia (EMET-Study) Thromb Haemost. 1997;77:444–51. doi: 10.1055/s-0038-1655986. [DOI] [PubMed] [Google Scholar]
- 65.Heijboer H, Brandjes DP, Büller HR, Sturk A, ten Cate JW. Deficiencies of coagulation-inhibiting and fibrinolytic proteins in outpatients with deep-vein thrombosis. N Engl J Med. 1990;323:1512–6. doi: 10.1056/NEJM199011293232202. [DOI] [PubMed] [Google Scholar]
- 66.Pintao MC, Ribeiro DD, Bezemer ID, et al. Protein S levels and the risk of venous thrombosis: results from the MEGA case-control study. Blood. 2013;122:3210–9. doi: 10.1182/blood-2013-04-499335. [DOI] [PubMed] [Google Scholar]
- 67.Tait RC, Walker ID, Perry DJ, et al. Prevalence of antithrombin deficiency in the healthy population. Br J Haematol. 1994;87:106–12. doi: 10.1111/j.1365-2141.1994.tb04878.x. [DOI] [PubMed] [Google Scholar]
- 68.Raffini L. Thrombophilia in children: who to test, how, when, and why? Hematology Am Soc Hematol Educ Program. 2008;2008:228–35. doi: 10.1182/asheducation-2008.1.228. [DOI] [PubMed] [Google Scholar]
- 69.Andrew M, Paes B, Milner R, et al. Development of the human coagulation system in the full-term infant. Blood. 1987;70:165–72. doi: 10.1182/blood.V70.1.165.165. [DOI] [PubMed] [Google Scholar]
- 70.Appel IM, Grimminck B, Geerts J, Stigter R, Cnossen MH, Beishuizen A. Age dependency of coagulation parameters during childhood and puberty. J Thromb Haemost. 2012;10:2254–63. doi: 10.1111/j.1538-7836.2012.04905.x. [DOI] [PubMed] [Google Scholar]
- 71.Gavva C, Sarode R, Zia A. A clinical audit of thrombophilia testing in pediatric patients with acute thromboembolic events: impact on management. Blood Adv. 2017;1:2386–91. doi: 10.1182/bloodadvances.2017009514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Young G. How I treat pediatric venous thromboembolism. Blood. 2017;130:1402–8. doi: 10.1182/blood-2017-04-742320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Manco-Johnson MJ, Grabowski EF, Hellgreen M, et al. Laboratory testing for thrombophilia in pediatric patients. On behalf of the Subcommittee for Perinatal and Pediatric Thrombosis of the Scientific and Standardization Committee of the International Society of Thrombosis and Haemostasis (ISTH) Thromb Haemost. 2002;88:155–6. doi: 10.1055/s-0037-1613169. [DOI] [PubMed] [Google Scholar]
- 74.Ageno W, Dentali F, Squizzato A, et al. Evidence and clinical judgment: treatment of cerebral vein thrombosis. Thromb Haemost. 2010;103:1109–15. doi: 10.1160/TH09-12-0827. [DOI] [PubMed] [Google Scholar]
- 75.De Stefano V, Rossi E. Testing for inherited thrombophilia and consequences for antithrombotic prophylaxis in patients with venous thromboembolism and their relatives. A review of the Guidelines from Scientific Societies and Working Groups. Thromb Haemost. 2013;110:697–705. doi: 10.1160/TH13-01-0011. [DOI] [PubMed] [Google Scholar]
- 76.Neshat-Vahid S, Pierce R, Hersey D, Raffini LJ, Faustino EV. Association of thrombophilia and catheter-associated thrombosis in children: a systematic review and meta-analysis. J Thromb Haemost. 2016;14:1749–58. doi: 10.1111/jth.13388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Monagle P, Chan AKC, Goldenberg NA, et al. Antithrombotic therapy in neonates and children: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e737S–e801S. doi: 10.1378/chest.11-2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Monagle P, Cuello CA, Augustine C, et al. American Society of Hematology 2018 Guidelines for management of venous thromboembolism: treatment of pediatric venous thrombo-embolism. Blood Adv. 2018;2:3292–316. doi: 10.1182/bloodadvances.2018024786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Raffini LJ, Scott JP. Thrombotic disorders in children. In: Kliegman RM, Stanton BF, St Geme JW, Schor N, eds. Nelson textbook of pediatrics. 20th ed. Philadelphia, PA: Elsevier, 2016:2394–7. [Google Scholar]
- 80.Male C, Thom K, O'Brien SH. Direct oral anticoagulants: what will be their role in children? Thromb Res. 2019;173:178–85. doi: 10.1016/j.thromres.2018.06.021. [DOI] [PubMed] [Google Scholar]
- 81.Thomas S, Makris M. The reversal of anticoagulation in clinical practice. Clin Med (Lond) 2018;18:314–9. doi: 10.7861/clinmedicine.18-4-314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Keeling D, Baglin T, Tait C, et al. Guidelines on oral anticoagulation with warfarin - fourth edition. Br J Haematol. 2011;154:311–24. doi: 10.1111/j.1365-2141.2011.08753.x. [DOI] [PubMed] [Google Scholar]
- 83.Hirsh J, Bauer KA, Donati MB, Gould M, Samama MM, Weitz JI. Parenteral anticoagulants: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008;133(6 Suppl):141S–59S. doi: 10.1378/chest.08-0689. [DOI] [PubMed] [Google Scholar]
- 84.Pollack CV, Jr, Reilly PA, van Ryn J, et al. Idarucizumab for dabigatran reversal - full cohort analysis. N Engl J Med. 2017;377:431–41. doi: 10.1056/NEJMoa1707278. [DOI] [PubMed] [Google Scholar]
- 85.Connolly SJ, Crowther M, Eikelboom JW, et al. Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Engl J Med. 2019;380:1326–35. doi: 10.1056/NEJMoa1814051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ansell JE, Bakhru SH, Laulicht BE, et al. Single-dose ciraparantag safely and completely reverses anticoagulant effects of edoxaban. Thromb Haemost. 2017;117:238–45. doi: 10.1160/TH16-03-0224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Connors JM. Testing and monitoring direct oral anticoagulants. Blood. 2018;132:2009–15. doi: 10.1182/blood-2018-04-791541. [DOI] [PubMed] [Google Scholar]
- 88.van Ryn J, Stangier J, Haertter S, et al. Dabigatran etexilate--a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity. Thromb Haemost. 2010;103:1116–27. doi: 10.1160/TH09-11-0758. [DOI] [PubMed] [Google Scholar]
- 89.Hawes EM, Deal AM, Funk-Adcock D, et al. Performance of coagulation tests in patients on therapeutic doses of dabigatran: a cross-sectional pharmacodynamic study based on peak and trough plasma levels. J Thromb Haemost. 2013;11:1493–502. doi: 10.1111/jth.12308. [DOI] [PubMed] [Google Scholar]
- 90.Hillarp A, Baghaei F, Fagerberg Blixter I, et al. Effects of the oral, direct factor Xa inhibitor rivaroxaban on commonly used coagulation assays. J Thromb Haemost. 2011;9:133–9. doi: 10.1111/j.1538-7836.2010.04098.x. [DOI] [PubMed] [Google Scholar]
- 91.Seiffge DJ, Traenka C, Polymeris AA, et al. Intravenous thrombolysis in patients with stroke taking rivaroxaban using drug specific plasma levels: experience with a standard operation procedure in clinical practice. J Stroke. 2017;19:347–55. doi: 10.5853/jos.2017.00395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schmitz EM, Boonen K, van den Heuvel DJ, et al. Determination of dabigatran, rivaroxaban and apixaban by ultra-performance liquid chromatography - tandem mass spectrometry (UPLC-MS/MS) and coagulation assays for therapy monitoring of novel direct oral anticoagulants. J Thromb Haemost. 2014;12:1636–46. doi: 10.1111/jth.12702. [DOI] [PubMed] [Google Scholar]
- 93.Forbes HL, Polasek TM. Potential drug-drug interactions with direct oral anticoagulants in elderly hospitalized patients. Ther Adv Drug Saf. 2017;8:319–28. doi: 10.1177/2042098617719815. [DOI] [PMC free article] [PubMed] [Google Scholar]