Abstract
Introduction
Medical knowledge regarding preservation of fertility and pregnancy in patients with breast cancer (BC) is of interest. We, therefore, decided to conduct a survey on this issue among professionals involved in the treatment of BC in Argentina.
Materials and methods
A survey was conducted and sent by email to 3,412 contacts in the Argentine Mastology Society (Sociedad Argentina de Mastología, or SAM) database, with responses from 396 physicians. The survey design was based on the Lambertini 2017 survey. To the author’s knowledge, it is the first Argentine survey to address this issue.
Results
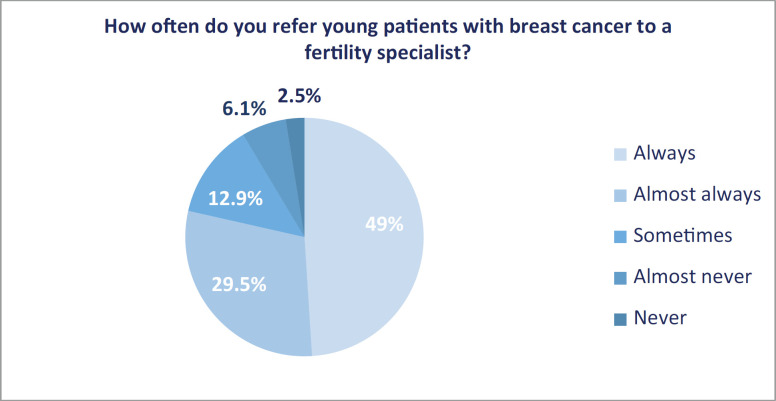
The frequency with which the impact of cancer treatment on the fertility of young patients was addressed by the respondent and referred to a fertility specialist was ‘always’ and ‘almost always’ in 86.8% and 78.5% of cases, respectively.
Conclusions
The level of knowledge is comparable to the data presented by other surveys. Membership in a Mastology Unit was associated with more current treatment. Continued work on the training of professionals is necessary to facilitate communication, information and guidance of patients of childbearing age who are going to have cancer treatment in order to advise them on fertility preservation, as well as the possibility of pregnancy after diagnosis of BC, and to be able to provide better care to those with BC associated with pregnancy.
Keywords: survey, medical knowledge, breast cancer, preservation of fertility, breast cancer associated with pregnancy
Introduction
In the United States from 2013 to 2017, the incidence of breast cancer (BC) in women aged 20–34 years represented 1.9% of diagnoses, and those aged 35–44 years represented 8.3%. The mortality rates were 0.9% in women aged 20–34 years and 4.6% for those between 35 and 44 years of age [1].
In a collaborative study published in 2016 that included 1,732 patients with BC in Argentina, the incidence by age was 7.4% for those between 30 and 39 years old and 8.5% for those between 40 and 44 years old [2]. According to data from the Breast Cancer Registry (Registro de Cáncer de Mama, or RCM) of the Argentine Mastology Society (SAM), 10.4% of infiltrating carcinomas were found in young women [3].
Globally, deaths from BC have been declining since the late 1980s in both young and older women [4]. According to the statistics published by the Surveillance, Epidemiology and End Results Program (SEER) [1], the age-adjusted rate of new BCs has increased 0.3% per year in the last 10 years, while mortality decreased 1.5% annually from 2008 to 2017. The 5-year survival rate has increased, reaching 91.27% in 2013.
Due to the increased survival of patients and the delay of motherhood for personal and social reasons, it is likely that young women diagnosed with BC have not fulfilled their plans for motherhood at the time of diagnosis, and are interested in their future fertility as well as the possibility of facing BC during pregnancy.
The first doctors to come into contact with young women with BC, whether they are mastologists, gynaecologists or oncologists, must know the needs and particular characteristics of this population. It is they who will have the opportunity to make a timely referral to a fertility specialist, as well as choosing the best therapeutic strategies for those with a diagnosis of BC during pregnancy to carry the foetus to term, without compromising the oncological safety of the mother or vitality and normal development of the foetus.
Today there are international guidelines with different algorithms for the management of young patients who wish to preserve their fertility [4–6], as well as the management of BC during pregnancy [7, 8], with the aim of providing up-to-date evidence to support medical practice.
According to a recent publication, using data from American Association of Clinical Oncology’s (ASCO) Quality in Oncology Practice Initiative [9], only 56% of women received fertility preservation counselling. According to the guidelines of the ASCO, the National Comprehensive Cancer Network and the European Society for Medical Oncology (ESMO) [5–7], consultations with pre-menopausal patients with BC should include fertility preservation counselling prior to beginning treatment, and no patient should be excluded.
Medical knowledge on these topics is of interest; therefore, surveys have been conducted on this topic in different countries in order to train and educate physicians, thereby improving the quality of advice and care for patients [10–13].
We, therefore, decided to conduct a survey of professionals involved in the treatment of BC in order to analyse the knowledge and current practice in the preservation of fertility and pregnancy in Argentina.
Materials and methods
A survey (Appendix A) was conducted and sent via email to 3,412 contacts in the Argentine Mastology Society (SAM) database. It was sent three times: 31 July, 25 October25 and 17 December 2019. Five hundred and sixty-one professionals (16.4%) clicked on the link, and 396 physicians completed the survey (11.6% of the total emails sent, and 70.5% of those who clicked on the link).
Participation was anonymous and voluntary; consent was implicit when choosing to open the link in the email, which indicated its content (Appendix B).
The survey design was based on Lambertini et al. 2017 [13]. It was modified and adapted, and was divided into four sections. The first section included 11 questions on demographic data. A second section included 11 questions on BC and fertility preservation. The third section included 6 questions about pregnancy after BC, and finally, a fourth included 11 questions about BC during pregnancy. The survey was directed to different specialists involved in the care of patients with BC.
To the author’s knowledge, this is the first Argentine survey that addresses issues in the management of and current practices in BC, preservation of fertility and pregnancy, by the professionals who care for these patients.
Statistical analysis
The category variables are described using the raw number and the percentage in each category. The Chi square test was performed with Mantel-Haenszel correction. The p value for statistical significance was <0.05. The OpenEpi program, version 3.01, was used to perform the calculations.
Results
Three hundred and ninety-six responses were received.
Demographic characteristics
62.4% of those surveyed were between 30 and 49 years of age. 87.7% were gynaecologists or mastologists, 4.5% were clinical oncologists and 91.4% said that they would be interested in receiving information on the topic (Table 1).
Table 1. Demographic characteristics of individuals polled.
| n | % | |
|---|---|---|
| Total population | 396 | 100% |
| Age | ||
| 20–29 years | 18 | 4.5 |
| 30–39 years | 121 | 30.6 |
| 40–49 years | 126 | 31.8 |
| 50–59 years | 67 | 16.9 |
| 60 or older | 64 | 16.2 |
| Gender | ||
| Women | 237 | 59.8 |
| Men | 159 | 40.2 |
| Speciality | ||
| Mastology | 172 | 43.5 |
| Gynaecology | 175 | 44.2 |
| Oncology | 18 | 4.5 |
| Obstetrics | 17 | 4.3 |
| General surgery | 8 | 2 |
| Other | 6 | 1.5 |
| Usual place of practice | ||
| Private practice | 77 | 19.4 |
| Hospital/sanatorium | 121 | 30.6 |
| Both | 195 | 49.2 |
| Other | 3 | 0.8 |
| Years in practice | ||
| 1–5 years | 71 | 17.9 |
| 6–10 years | 62 | 15.6 |
| 11–15 years | 67 | 16.9 |
| 16–20 years | 56 | 14.1 |
| 20 years or more | 140 | 35.5 |
| Work in a MU accredited by SAM | ||
| Yes | 109 | 27.5 |
| No | 287 | 72.5 |
| Patients <40 years seen annually | ||
| Under 10 | 218 | 55.1 |
| 10–50 | 147 | 37.1 |
| More than 50 | 31 | 7.8 |
| Patients with BC during pregnancy seen in the last 10 years | ||
| None | 81 | 20.5 |
| 1–5 | 219 | 55.3 |
| 6–10 | 69 | 17.4 |
| More than 10 | 27 | 6.8 |
| Interested in receiving information about the topic addressed | ||
| Yes | 362 | 91.4 |
| No | 11 | 2.8 |
| Maybe | 23 | 5.8 |
| Interested in attending a course about the topic addressed | ||
| Yes | 285 | 72 |
| No | 25 | 6.3 |
| Maybe | 86 | 21.7 |
MU: Mastology unit, ASM: Argentine Society of Mastology, PABC: pregnancy-associated BC
Fertility preservation
The impact of cancer treatment on the fertility of young patients was addressed and referred accordingly ‘always’ and ‘almost always’ in 344 respondents (86.8%) and 311 (78.5%), respectively (Figures 1 and 2).
Figure 1. Discussion of the impact of oncological treatment on future fertility.
Figure 2. Frequency of referral to a fertility specialist.
In 210 cases, a response was provided for the most frequent reasons why patients were not referred to a fertility specialist: the patient did not desire referral 112 (53.3%); factors related to the patient: age, parity, marital status, cancer prognosis 85 (40.5%); there are no fertility specialists in their area 65 (30.9%); and lack of information on available techniques 24 (11.4%) (Figure 3).
Figure 3. Reason for not referring patients to a fertility specialist. (n: 210). OS = Ovarian stimulation; pt = patient; BC = breast cancer.
We did not find statistically significant differences when evaluating the approach to the impact of cancer treatment on fertility (p = 0.6) and referral (p = 0.9), according to the speciality of the respondent: gynaecologist: always or almost always discuss 86.8% and provide referral 80.6%; mastologist: 90.1% and 79.6%; and oncologist: 94.4% and 77.8%.
Regarding fertility preservation techniques, the majority, 365 (92.2%) considered oocyte cryopreservation useful (Figure 4).
Figure 4. Knowledge regarding utility of different techniques of fertility preservation in patients with BC. BC = Breast cancer; CT = chemotherapy.
The responses regarding the safety of ovarian stimulation (OS) and the impact of cancer treatments on fertility are detailed in Table 2.
Table 2. Fertility preservation.
| Yes | No | NR | |
|---|---|---|---|
| OS is considered safe in all patients with BC | 180 (45.5%) | 101 (25.5%) | 115 (29%) |
| OS is considered safe in patients with ER positive BC | 168 (42.4%) | 98 (24.8%) | 130 (32.8%) |
| OS is considered safe in patients who have received neoadjuvant CT | 198 (50%) | 69 (17.4%) | 129 (32.6%) |
| OS in patients with a BC diagnosis should include letrozole or tamoxifen | 203 (51.3%) | 37 (9.3%) | 156 (39.4%) |
| The use of analogues during CT can be offered to all pre-menopausal patients with BC who wish to preserve their fertility independent of ER status | 249 (62.9%) | 52 (13.1%) | 95 (24%) |
| The impact of CT on future fertility depends on age, drugs and dosages used | 350 (88.4%) | 13 (3.3%) | 33 (8.3%) |
| The risk of amenorrhoea following CT is greater in women < 30 years compared to women > 40 years |
88 (22.2%) | 245 (61.9%) | 63 (15.9%) |
OS: Ovarian stimulation, pts: patients, BC: breast cancer, ER: oestrogen receptors, CT: chemotherapy, NR: no response
Pregnancy after BC
When evaluating the risk posed by pregnancy after BC, 66.2% of those surveyed affirmed that the risk does not increase, 45.2% considered that it does not do so within the first 2 years of diagnosis or with positive oestrogen receptor (ER) disease (58.3%) (Table 3).
Table 3. Pregnancy after BC.
| Yes | No | NR | |
|---|---|---|---|
| Pregnancy after BC increases RR | 77 (19.4%) | 262 (66.2%) | 57 (14.4%) |
| Pregnancy after BC increases RR only in the first 2 years following dx | 127 (32.1%) | 179 (45.2%) | 90 (22.7%) |
| Pregnancy after BC increases RR only in ER positive cancers | 64 (16.2%) | 231 (58.3%) | 101 (25.5%) |
| It is considered safe to temporarily interrupt HT after 18–30 months to allow a pregnancy | 203 (51.3%) | 79 (19.9%) | 114 (28.8%) |
| Lactation after BC is considered safe | 313 (79%) | 22 (5.6%) | 61 (15.4%) |
| ARTs are considered safe in patients who have had BC | 247 (62.4%) | 44 (11.1%) | 105 (26.5%) |
BC: breast cancer, RR: risk of recurrence, dx: diagnosis, ER: oestrogen receptors, HT: hormone therapy, ART: assisted reproduction techniques, NR: no response
51.3% considered it safe to temporarily interrupt hormone therapy (HT) after 18–30 months to attempt a pregnancy.
BC associated with pregnancy
39.9% of those surveyed answered that BC during pregnancy, even when treated properly, has a worse prognosis. 33.6% stated that patients diagnosed at 28–33 weeks should be indicated a preterm delivery (PD) to begin cancer treatment (Table 4).
Table 4. BC associated with pregnancy.
| Yes | No | NR | |
|---|---|---|---|
| PABC, even when adequately treated, has a worse prognosis | 158 (39.9%) | 205 (51.8%) | 33 (8.3%) |
| In patients diagnosed between 28 and 33 weeks, a PD is indicated | 133 (33.6%) | 208 (52.5%) | 55 (13.9%) |
| Mx may be used with abdominal protection | 368 (92.9%) | 18 (4.6%) | 10 (2.5%) |
| Conservative surgery may be considered, depending on the case | 331 (83.6%) | 45 (11.4%) | 20 (5%) |
| SNB with patent blue may be used, depending on the case | 113 (28.5%) | 221 (55.8%) | 62 (15.7%) |
| SNB with radiocolloids may be performed, depending on the case | 206 (52%) | 116 (29.3%) | 74 (18.7%) |
| RT during pregnancy is safe | 10 (2.5%) | 339 (85.6) | 47 (11.9%) |
| CT may be used safely in any trimester | 7 (1.8%) | 359 (90.6%) | 30 (7.6%) |
| CT may be used safely from the second trimester on | 263 (66.4%) | 72 (18.2%) | 61 (15.4%) |
| HT may be used safely | 28 (7.1%) | 296 (74.7%) | 72 (18.2%) |
| Anti-Her2 treatment may be used safely | 28 (7.1%) | 246 (62.1%) | 122 (30.8%) |
PABC: Pregnancy-associated BC, dx: diagnosis, PD: preterm delivery, Mx: mammogram, SNB: sentinel node biopsy, RT: radiation therapy, CT: chemotherapy, NR: no response
Regarding the identification of the sentinel node, 28.5% and 52% considered the use of patent blue and radiocolloids safe, respectively.
When evaluating the safety of the different adjuvant treatments, we see that 66.4% considered chemotherapy (CT) safe from the second trimester on; 85.6%, 74.7% and 62.1% did not consider the use of radiation treatment (RT), HT and anti-HER2 therapies to be safe.
Evaluation according to membership in a Mastology Unit (MU)
13.8% (n = 15) of the professionals who work in a Mastology Unit (MU) do not have fertility specialists in their area, nor do 17.4% (n = 50) of those who do not work in a MU; this difference was not statistically significant (p = 0.7) (Table 5).
Table 5. Knowledge according to belonging to a MU.
| MU Yes (n: 109) | MU No (n: 287) | ||
|---|---|---|---|
| AE agreement | AE agreement | p | |
| Fertility preservation | |||
|
Discussion of the impact of treatments on fertility ASCO and BCY4 recommend addressing the subject of the impact that oncological have on the whole patient of childbearing age [4, 5] |
103 (94.5%) | 241 (84%) | 0.002 |
|
Referral to a fertility specialist BCY4 recommends that all women interested in preserving their fertility should be referred to a specialist [4] |
90 (82.6%) | 221 (77%) | 0.1 |
| OS is considered safe in all patients with BC [35] | 61 (56%) | 119 (41.5%) | 0.004 |
| OS is considered safe in all patients with ER+ BC [35] | 61 (56%) | 107 (37.3%) | 0.0003 |
| OS is considered safe in patients who have received neoadjuvant CT [35] | 69 (63.3%) | 129 (44.9%) | 0.0005 |
| OS in patients diagnosed with BC should include letrozole and tamoxifen [35] | 70 (64.2%) | 133 (46.3%) | 0.0007 |
| Use of analogues during CT may be offered to all pre-menopausal patients with BC who wish to preserve their fertility independent of their ER status [25] | 76 (69.7%) | 173 (60.3%) | 0.04 |
| Pregnancy after BC | |||
| Pregnancy after BC increases RR Pregnancy after BC does not increase RR [36] |
85 (78%) | 177 (61.7%) | 0.001 |
| Pregnancy after BC increases RR only in the first 2 years following dx The interval between BC dx and pregnancy does not impact patient prognosis [36] |
54 (49.5%) | 125 (43.5%) | 0.14 |
| Pregnancy after BC increases RR only in ER positive cancers Pregnancy after BC does not increase RR, even in ER+ cancers [36] |
80 (73.4%) | 151 (52.6%) | 0.00009 |
| It is considered safe to temporarily interrupt HT after 18–30 months to allow a pregnancy The BCY4 and Saint Gallen guides recommend a minimum 18 months of HT before considering pregnancy, although prospective date is lacking [4, 27] |
66 (60.5%) | 137 (47.7%) | 0.01 |
| PABC | |||
| PABC, even when adequately treated, has a worse prognosis Adequately treated PABC has the same prognosis as BC without pregnancy [37] |
71 (65.1%) | 134 (46.7%) | 0.0005 |
| In patients diagnosed between 28 and 33 weeks, a PD is indicated The ESMO guide [7] and different authors [8, 38] suggest that it is always preferable to carry a pregnancy to term |
69 (63.3%) | 139 (48.4%) | 0.004 |
| SNB with patent blue may be used, depending on the case The ESMO guide [7] and Loibl [8] note the contraindication for the use of patent blue during pregnancy |
79 (72.5%) | 142 (49.5%) | 0.00001 |
| SNB with radiocolloids may be performed, depending on the case [7, 8] | 81 (74.3%) | 125 (43.5%) | <0.0000001 |
| CT can be used safely from the second trimester on [7, 8] | 97 (89%) | 166 (57.8%) | <0.0000001 |
| HT may be used safely Tamoxifen is teratogenic and is found to be contraindicated during pregnancy [7, 8] |
96 (88.1%) | 200 (69.7%) | 0.00008 |
| Anti-Her2 treatment may be used safely Trastuzumab passes through the placenta from the second trimester on and is found to be associated with oligoamnios, and is therefore contraindicated [7, 8] |
81 (74.3%) | 165 (57.5%) | 0.001 |
MU: Mastology unit, AE: available evidence, tmts: treatments, OS: ovarian stimulation, PABC: pregnancy-associated BC, dx: diagnosis, PD: preterm delivery, Mx: mammogram, SNB: sentinel node biopsy, HT: hormone therapy, RT: radiation therapy, CT: chemotherapy
Eighteen questions were selected according to the clinical relevance of the knowledge. The responses were analysed, taking into consideration whether or not the respondent belonged to a MU and whether they were in accordance with current guidelines and recommendations [4–8].
We found a statistically significant difference in those professionals who belonged to these units in 16 of the 18 questions evaluated.
Discussion
The future fertility and oncological safety of a patient with a pregnancy following BC diagnosis are important issues for many young women [14]. The knowledge of the physicians who treat these patients is essential to provide adequate information in the decision-making process and improve the quality of care.
Fertility preservation
In our survey, we observed that 86.8% of treating physicians address the impact that cancer treatment will have on the fertility of young patients. Although it is an important percentage, it was lower than that published in the literature, which reports values between 91.6% and 98% [11–14].
Referral to a fertility specialist has evolved over time: in the surveys conducted by Quinn in 2009 [10] and Forman in 2010 [11], it was specified in only 47% and 39%. The inclusion of this topic in the guidelines surely contributed to a favourable change, as evidenced by Adams in 2013 [12], where referral reached 67%, reaching 97% according to Rosenberg in 2017 [14]. In our study, referrals were given in 78.5% of cases, and although this is an overall improvement, it remains sub-optimal.
The most frequent reason for lack of referral was that the patient did not want it (53.3%), and factors related to the patient: age, parity, marital status, cancer prognosis (40.5%), similar to that published by Lambertini et al [13], who found that these factors are the main barrier to accessing consultation with a fertility specialist (53.8%). However, according to Forman et al [11], these factors should not deprive a patient of the discussion regarding fertility preservation.
When evaluating patient surveys by Ruddy [15] and Partridge [16], future fertility is a matter of great concern, which may even impact their therapeutic decisions [17, 18]. Therefore, it is striking that one of the most frequent causes of lack of referral is that the patient does not want it. It is worth questioning how we inform patients on this topic, and how our beliefs, opinions or lack of knowledge impact that decision, as, according to that published by Peate et al [19], 75% of the patients base their decision on the opinion of their doctor.
The absence of fertility specialists and the lack of information on available techniques were other causes of the lack of referral, data that coincide with that published by Lambertini (30.9% versus 28.2% and 11.4% versus 17.9%) [13]. It must be mentioned that in Argentina, public and private institutions have their own fertility services or access these services following the concept of MUs without borders.
It is encouraging that 91.4% of the respondents wish to receive information on the subject and 72% would attend a course, similar to that published by Forman [11].
In the study conducted by Masciello et al [20], 78% of mastologists prefer to defer the discussion about fertility preservation for the Oncologists to address. On the other hand, we did not find statistically significant differences between the different professionals involved.
Nearly all of the respondents (92.2%) considered oocyte cryopreservation, one of the currently most recommended techniques, to be useful [5]. However, a lack of knowledge of different techniques, between 7.8% and 50.3%, is observed.
More than half of those surveyed did not consider OS safe or were unaware of it, especially in those with ER positive BC, similar to the 43.2% published by Lambertini et al [13]. Regarding OS protocols in BC patients, 51.3% stated that they should include letrozole or tamoxifen, similar to that described by Sanada et al [21], who used aromatase inhibitors in up to 68.3% of patients with BC. The results of the prospective STIM trial (NTR4108) confirming the safety of these protocols are awaited [22].
62.9% considered that the use of gonadotropin-releasing hormone (GnRH) analogues during CT could be offered to all pre-menopausal patients with BC who wish to preserve their fertility, regardless of ER status. Randomised studies [23, 24] and meta-analyses [25] evaluated the efficacy of this procedure even in ER positive patients. ASCO 2018 [5] and the Consensus of Breast Cancer in young women (BCY4) [4] consider that this method should be offered to patients who are interested in fertility preservation, and who cannot or do not wish to use other methods. Lambertini et al [25] suggests that they would not be exclusive and could be offered to patients who have already used other preservation techniques. Ovarian suppression was the best known strategy 82.4%, in the Lambertini survey [13]; however, in our study, only 54.8% considered it useful. This could be related to the lack of coverage of other techniques in some countries.
It is not necessary for all professionals to have a thorough understanding of every fertility preservation procedure. However, the patient of childbearing age who is going to receive cancer treatment should be informed about safety and the possibility of consultation with a fertility specialist to advise her on the different options available. It is important to acknowledge to the patient that it is desirable to preserve her fertility and to make a rapid referral.
Pregnancy after BC
In evaluating the risk posed by pregnancy after BC, 66.2% of those surveyed stated that it does not increase, 45.2% considered that it does not do so within the first 2 years of diagnosis, or in ER positive disease (58.3%). In his survey, Lambertini [13], reported similar data: 69.6%, 50.5% and 63%, respectively. Current evidence suggests that pregnancy after BC does not increase the risk of relapse [4]. Some 62.4% of the professionals considered assisted reproductive techniques safe in a patient with a history of BC, similar to the 57.5% reported in the literature [13].
The best time to become pregnant remains controversial. Experts suggest waiting 2 years after diagnosis to start trying become pregnant [26].
In our survey, 51.3% responded that it is safe to temporarily interrupt hormone treatment after 18–30 months to allow a pregnancy, as did the 50.5% reported by Lambertini [13]. This behaviour is supported by the BCY4 Consensus [4] and Saint Gallen 2019 [27]; however, it will be the results of the POSITIVE study (IBCSG 48-14 NCT02308085) that provides the answer on regarding its safety [28].
BC during pregnancy
Despite the fact that BC during pregnancy does not represent a worse prognosis for women [8, 29], 39.9% of those surveyed answered yes, even when it is treated appropriately, similar to the 31.5% reported in the literature [13]. It is worth mentioning that distinct publications found that a postpartum BC diagnosis may be associated with a worse prognosis than a diagnosis during pregnancy [30].
33.6% stated that in patients diagnosed at 28–33 weeks, a preterm birth is indicated at the start of oncological treatment; however, the greatest risk to consider is prematurity. The best option, when possible, is to carry out treatments during pregnancy and carry to term [7, 8].
In accordance with current evidence, sentinel node biopsy (SNB) is a procedure that can be carried out in a safe manner during pregnancy [7, 8]. For studies using radiocolloids, some 52% of the respondents considered the use of radiocolloids safe during pregnancy; on the other hand, 55.8% contraindicated patent blue due to the potential for anaphylactic reactions [7, 8, 31].
In evaluating the safety of different adjuvant treatments, it is seen that 66.4% considered CT to be safe to start in the second trimester, which is correct, and that its use during the first trimester is associated with foetal malformations and miscarriage [7, 8].
85.6%, 74.7% and 62.1%, respectively, responded that radiation therapy, HT and anti-Her2 treatment should be avoided during pregnancy. Lambertini [13] published similar numbers—76.6%, 76.2% and 61.9%.
Knowledge according to belonging to a MU
MUs are created to optimise the quality of patient care through better coordination and communication between different disciplines, and for advances in knowledge to be applied in a uniform manner, benefiting every patient and professional in the MU.
In 2015 [32], the SAM developed an accreditation programme based on international guidelines [33, 34]. In the completed survey, it is evident that belonging to a MU leads to enrichment and continuing education, such that the responses of the professionals who engaged in these were in accordance in a statistically significant manner with available evidence [4, 5, 7, 8, 27, 35–38].
In order to carry out this work, the SAM database of professionals was used. The response rate was low, though similar to other surveys [10, 12]; thus conclusions could not be extrapolated to what is happening throughout Argentina. Other limitations of the study were selection bias, which is possible given that only those professionals who are interested in the topic decided to answer.
Its strength is that it is the first study to permit evaluation of current knowledge and practices in relation to the topics in this field and the great interest that they generate.
Conclusion
Based on these results, we can conclude that the level of knowledge is comparable to the data presented in other surveys. Belonging to a MU was associated with being more up-to-date on this topic. It is necessary to continue working to train professionals in facilitating communication, information and advising patients of childbearing age who are going to receive oncological treatment so they can be informed about fertility preservation as well as the possibility of pregnancy following a BC diagnosis, and providing better care to those with BC during pregnancy.
Conflicts of interest
The authors declare no conflict of interest related to the present work.
Funding
Nothing of a financial nature was received for the execution of the present work.
Appendix A. Survey of current practices in BC, fertility preservation and pregnancy
A) Demographic data
1. Age: __________ years.
2. Gender: ____Female ____Male
3. What is your speciality?
____ Mastology ____ Oncology
____ Gynaecology ____ Imaging
____ General surgery ____ Radiotherapy
____ Obstetrics ____ Anatomical pathology
4. Are you a member of the ASM?
____Yes ____ Subscriber ____Member ____ Honorary ____ Lifetime Member
____ No
5. How would you define your regular practice?
____ Hospital/sanatorium
____ Private practice
____Both
____ Other (please specify): _____________
6. How long have you been in practice? ____________ years.
7. Do you work in a MU certified/accredited by AMS?
____ Yes
____ No
8. How many patients under 40 with BC do you treat annually?
____ fewer than 10
____ 10–50
____more than 50
9. How many patients with PABC have you seen in the last 10 years of practice?
____ 0
____ 1–5
____ 6–10
____ more than 10
10. Are you interested in receiving information on the topics in this survey?
____ Yes
____ No
____ Maybe
11. Are you interested in attending a course on the topics in this survey?
____ Yes
____ No
____ Maybe
B) BC and fertility preservation
1. How often do you discuss with the impact oncological treatment can have on future fertility with young patients with BC?
____ Always ____ Almost always ____ Sometimes ____ Almost never____ Never
2. How often do you refer young patients with BC to a fertility specialist?
____ Always ____ Almost always ____ Sometimes ____ Almost never____ Never
3. In cases wherein patients are not referred to a fertility specialist. Check ALL of the reasons you consider to be correct.
____ Lack of Information on available methods.
_____ No availability of fertility specialists in your work area.
____ You would not consider ovulation stimulation to be appropriate in these patients.
____ Consider that these procedures would delay starting cancer treatments.
____ You do not believe that it is advisable for patients with BC to attempt future pregnancies.
____ Patient-related factors: age, parity, marital status, cancer prognosis.
____ The patient does not want it.
____ Other reasons: Specify __________________________________________
4. Which of the following fertility preservation techniques are considered useful in patients with BC? Check ALL that you consider:
____ Embryo cryopreservation.
____ Oocyte cryopreservation
____ Ovarian tissue cryopreservation.
Use of GnRH analogues during CT.
____ None.
5. Check ALL statements with which you agree:
| Yes | No | No response | |
|---|---|---|---|
| OS is considered safe in all patients with BC | |||
| OS is considered safe in patients with ER positive BC | |||
| OS is considered safe in patients who have received neoadjuvant CT | |||
| OS in patients with a BC diagnosis should include letrozole or tamoxifen | |||
| The use of analogues during CT can be offered to all pre-menopausal patients with BC who wish to preserve their fertility independent of ER status | |||
| The impact of CT on future fertility depends on age, drugs and dosages used | |||
| The risk of amenorrhoea following CT is greater in women < 30 years compared to women > 40 years |
OS; Ovarian stimulation, pts; patients, BC; breast cancer, ER; oestrogen receptors, CT; chemotherapy, NR; no response
C) Pregnancy after BC
| Yes | No | NR | |
|---|---|---|---|
| Pregnancy after BC increases RR | |||
| Pregnancy after BC increases RR only in the first 2 years following dx | |||
| Pregnancy after BC increases RR only in ER+ cases | |||
| It is considered safe to temporarily interrupt HT after 18–30 months to allow a pregnancy | |||
| Lactation after BC is considered safe | |||
| ARTs are considered safe in patients who have had BC |
BC: Breast cancer, RR: risk of recurrence, dx: diagnosis, ER: oestrogen receptors, HT: hormone therapy, ART: assisted reproduction techniques, NR: no response
D) PABC
| Yes | No | NR | |
|---|---|---|---|
| PABC, even when adequately treated, has a worse prognosis | |||
| In patients diagnosed between 28 and 33 weeks, a PD is indicated | |||
| Mx may be used with abdominal protection | |||
| Conservative surgery may be considered, depending on the case | |||
| The SNB with patent blue may be performed, depending on the case | |||
| SNB with radiocolloids may be performed, depending on the case | |||
| RT during pregnancy is safe | |||
| CT may be used safely in each trimester | |||
| CT may be used safely from the second trimester on | |||
| HT may be used safely | |||
| Anti-Her2 treatment may be used safely |
PABC: Pregnancy-associated BC, dx: diagnosis, PD: preterm delivery, Mx: mammogram, SNB: sentinel node biopsy, RT: radiation therapy, CT: chemotherapy, NR: no response
Thank you very much for your responses and time.
Appendix B. E-mail format used to request participation in the survey
Dear colleague:
We would like to request your assistance by responding to this anonymous survey about current practices in breast cancer, fertility preservation and pregnancy, the results of which will be used to conduct a scientific study. It will not take longer than 10 minutes to complete.
We appreciate your time and collaboration.
Sincerely,
Dr Gabriela Candás
Dr Alejandra García
Link to the survey
If you have already completed the survey, please disregard this message. Thank you very much.
References
- 1.SEER. [26/05/20]. [ https://seer.cancer.gov/statfacts/html/breast.html]
- 2.Meiss Kress RP, Chuit R, Novelli JE, et al. Breast cancer in Argentina: analysis from a collaborative group for the study of female breast cancer. J Cancer Epi Treat. 2016;1(2):5–16. doi: 10.24218/jcet.2016.10. [DOI] [Google Scholar]
- 3.Fabiano V, Mando P, Rizzo M, et al. Breast cancer in young women presents with more aggressive pathologic characteristics: retrospective analysis from an argentine national database. JCO Global Oncol. 2020;6:639–646. doi: 10.1200/JGO.19.00228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paluch-Shimon S, Cardoso F, Partridge AH, et al. ESO-ESMO 4th International Consensus Guidelines for Breast Cancer in Young Women (BCY4) Ann Surg Oncol. 2020;31(6):674–696. doi: 10.1016/j.annonc.2020.03.284. [DOI] [PubMed] [Google Scholar]
- 5.Oktay K, Harvey BE, Partridge AH, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;36:1994–2001. doi: 10.1200/JCO.2018.78.1914. [DOI] [PubMed] [Google Scholar]
- 6.National Comprehensive Cancer Network (NCCN) [26/05/20]. [ www.nccn.org]
- 7.Peccatori FA, Azim HA, Jr, Orecchia R, et al. Cancer, pregnancy and fertility: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24(6):vi160–vi170. doi: 10.1093/annonc/mdt199. [DOI] [PubMed] [Google Scholar]
- 8.Loibl S, Schmidt A, Gentilini O, et al. Breast cancer diagnosed during pregnancy: adapting recent advances in breast cancer care for pregnant patients. JAMA Oncol. 2015;1(8):1145–1153. doi: 10.1001/jamaoncol.2015.2413. [DOI] [PubMed] [Google Scholar]
- 9.Patel P, Kohn T, Cohen J, et al. Evaluation of reported fertility preservation counseling before chemotherapy using the quality oncology practice initiative survey. JAMA Network Open. 2020;3(7):e2010806. doi: 10.1001/jamanetworkopen.2020.10806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quinn GP, Vadaparampil ST, Lee J-H, et al. Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol. 2009;27(35):5952–5957. doi: 10.1200/JCO.2009.23.0250. [DOI] [PubMed] [Google Scholar]
- 11.Forman EJ, Anders CK, Behera MA. A nationwide survey of oncologists regarding treatment-related infertility and fertility preservation in female cancer patients. Fertil Steril. 2010;94:1652–1656. doi: 10.1016/j.fertnstert.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 12.Adams E, Hill E, Watson E. Fertility preservation in cancer survivors: a national survey of oncologists’ current knowledge, practice and attitudes. Br J Cancer. 2013;108:1602–1615. doi: 10.1038/bjc.2013.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lambertini M, Di Maio M, Pagani O, et al. The BCY3/BCC 2017 survey on physicians’ knowledge, attitudes and practice towards fertility and pregnancy-related issues in young breast cancer patients. Breast. 2018;42:41–49. doi: 10.1016/j.breast.2018.08.099. [DOI] [PubMed] [Google Scholar]
- 14.Rosenberg SM, Gelber S, Gelber RD, et al. Oncology physicians’ perspectives on practices and barriers to fertility preservation and the feasibility of a prospective study of pregnancy after breast cancer. J Adolesc Young Adult Oncol. 2017;6(3):429–434. doi: 10.1089/jayao.2017.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ruddy KJ, Gelber SI, Tamimi RM, et al. Prospective study of fertility concerns and preservation strategies in young women with breast cancer. J Clin Oncol. 2014;32(11):1151–1156. doi: 10.1200/JCO.2013.52.8877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Partridge AH, Gelber S, Peppercorn J, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004;22:4174–4183. doi: 10.1200/JCO.2004.01.159. [DOI] [PubMed] [Google Scholar]
- 17.Llarena NC, Estevez SL, Tucker SL, et al. Impact of fertility concerns on tamoxifen initiation and persistence. J Natl Cancer Inst. 2015;107(10):dvj202. doi: 10.1093/jnci/djv202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruggeri M, Pagan E, Bagnardi V, et al. Fertility concerns, preservation strategies and quality of life in young women with breast cancer: baseline results from an ongoing prospective cohort study in selected European centers. Breast. 2019;47:85–92. doi: 10.1016/j.breast.2019.07.001. [DOI] [PubMed] [Google Scholar]
- 19.Peate M, Meiser B, Friedlander M, et al. It’s now or never: fertility-related knowledge, decision-making preferences, and treatment intentions in young women with breast cancer-An Australian Fertility Decision Aid Collaborative Group Study. J Clin Oncol. 2011;29(10):1670–1677. doi: 10.1200/JCO.2010.31.2462. [DOI] [PubMed] [Google Scholar]
- 20.Masciello MC, Bartolomew AJ, Haslinger M, et al. Physician perspectives on fertility preservation discussions with premenopausal breast cancer patients: results from a multihospital health care system. Ann Surg Oncol. 2019;26(10):3210–3215. doi: 10.1245/s10434-019-07563-w. [DOI] [PubMed] [Google Scholar]
- 21.Sanada Y, Harada M, Kunitomi C, et al. A Japanese nationwide survey on the cryopreservation of embryos, oocytes and ovarian tissue for cancer patients. J Obstet Gynaecol Res. 2019;45(10):2021–2028. doi: 10.1111/jog.14073. [DOI] [PubMed] [Google Scholar]
- 22.Dahhan T, Balkenende EME, Beerendonk CCM, et al. Stimulation of the ovaries in women with breast cancer undergoing fertility preservation: alternative versus standard stimulation protocols; the study protocol of the STIM-trial. Contemp Clin Trials. 2017;61:96–100. doi: 10.1016/j.cct.2017.07.009. [DOI] [PubMed] [Google Scholar]
- 23.Moore HCF, Unger JM, Phillips K-A, et al. Goserelin for ovarian protection during breast-cancer adjuvant chemotherapy. N Engl J Med. 2015;372(10):923–932. doi: 10.1056/NEJMoa1413204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leonard RCF, Adamson DJA, Bertelli G, et al. GnRH agonist for protection against ovarian toxicity during chemotherapy for early breast cancer: the Anglo Celtic Group OPTION trial. Ann Oncol. 2017;28(8):1811–1816. doi: 10.1093/annonc/mdx184. [DOI] [PubMed] [Google Scholar]
- 25.Lambertini M, Moore HCF, Leonard RCF, et al. Gonadotropin-releasing hormone agonists during chemotherapy for preservation of ovarian function and fertility in premenopausal patients with early breast cancer: a systematic review and meta-analysis of individual patient-level data. J Clin Oncol. 2018;36(19):1981–1990. doi: 10.1200/JCO.2018.78.0858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cardoso F, Loibl S, Pagani O, et al. The European Society of Breast Cancer Specialists recommendations for the management of young women with breast cancer. Eur J Cancer. 2012;48(18):3355–3377. doi: 10.1016/j.ejca.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 27.Burstein HJ, Curigliano G, Loibl S, et al. Estimating the benefits of therapy for early-stage breast cancer: The St. Gallen International Consensus guidelines for the primary therapy of early breast cancer 2019. Ann Oncol. 2019;30(10):1541–1557. doi: 10.1093/annonc/mdz235. [DOI] [PubMed] [Google Scholar]
- 28.Pregnancy Outcome and Safety of Interrupting Therapy for Women with Estrogen Responsive Breast Cancer (POSITIVE) [22/03/20]. [ https://clinicaltrials.gov/show/NCT02308085]
- 29.Amant F, Minckwitz G, Han SN, et al. Prognosis of women with primary breast cancer diagnosed during pregnancy: results from an international collaborative study. J Clin Oncol. 2013;31:2532–2539. doi: 10.1200/JCO.2012.45.6335. [DOI] [PubMed] [Google Scholar]
- 30.Azim Jr HA, Santoro L, Russell-Edu W, et al. Prognosis of pregnancy-associated breast cancer: a meta-analysis of 30 studies. Cancer Treat Rev. 2012;38:834–842. doi: 10.1016/j.ctrv.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 31.Peccatori FA, Lambertini M, Scarfone G, et al. Biology, staging, and treatment of breast cancer during pregnancy: reassessing the evidences. Cancer Biol Med. 2018;15(1):6–13. doi: 10.20892/j.issn.2095-3941.2017.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McLean I, Terrier F, Elizalde R, et al. Unidades de Mastología. Fundamentos, Certificación y Acreditación. Sociedad Argentina de Mastología V01–2015. 2015.
- 33.Chicago: American College of Surgeons; National Accreditation Program For Breast Centers Standards Manual. 2018 Edition [ https://accreditation.facs.org/accreditationdocuments/NAPBC/Portal%20Resources/2018NAPBCStandardsManual.pdf] [Google Scholar]
- 34.Biganzoli L, Fatima Cardoso F, Marc Beishon M, et al. The requirements of a specialist breast centre. Breast. 2020;51:65–84. doi: 10.1016/j.breast.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim J, Turan V, Oktay K. Long-Term safety of letrozole and gonadotropin stimulation for fertility preservation in women with breast cancer. J Clin Endocrinol Metab. 2016;101(4):1364–1371. doi: 10.1210/jc.2015-3878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lambertini M, Kroman N, Ameye L, et al. Long-term safety of pregnancy following breast cancer according to estrogen receptor status. J Natl Cancer Inst. 2018;110(4):426–429. doi: 10.1093/jnci/djx206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Amant F, Minckwitz G, Han SN, et al. Prognosis of women with primary breast cancer diagnosed during pregnancy: results from an international collaborative study. J Clin Oncol. 2013;31(20):2532–2539. doi: 10.1200/JCO.2012.45.6335. [DOI] [PubMed] [Google Scholar]
- 38.Amant F, Vandenbroucke T, Verheecke M, et al. Pediatric outcome after maternal cancer diagnosed during pregnancy. N Engl J Med. 2015;373(19):1824–1834. doi: 10.1056/NEJMoa1508913. [DOI] [PubMed] [Google Scholar]