Abstract
While most of the countries around the globe are combating the pandemic of COVID-19, the level of its impact is quite variable among different countries. In particular, the data from Nepal, a developing country having an open border provision with highly COVID-19 affected country India, has shown a biphasic pattern of epidemic, a controlled phase (until July 21, 2020) followed by an outgrown phase (after July 21, 2020). To uncover the effective strategies implemented during the controlled phase, we develop a mathematical model that is able to describe the data from both phases of COVID-19 dynamics in Nepal. Using our best parameter estimates with 95% confidence interval, we found that during the controlled phase most of the recorded cases were imported from outside the country with a small number generated from the local transmission, consistent with the data. Our model predicts that these successful strategies were able to maintain the reproduction number at around 0.21 during the controlled phase, preventing 442,640 cases of COVID-19 and saving more than 1,200 lives in Nepal. However, during the outgrown phase, when the strategies such as border screening and quarantine, lockdown, and detection and isolation, were altered, the reproduction number raised to 1.8, resulting in exponentially growing cases of COVID-19. We further used our model to predict the long-term dynamics of COVID-19 in Nepal and found that without any interventions the current trend may result in about 18.76 million cases (10.70 million detected and 8.06 million undetected) and 89 thousand deaths in Nepal by the end of 2021. Finally, using our predictive model, we evaluated the effects of various control strategies on the long-term outcome of this epidemics and identified ideal strategies to curb the epidemic in Nepal.
Keywords: Biphasic epidemic, COVID-19, Mathematical model, Nepal, Open border
2010 MSC: 92B05
1. Introduction
Since the first reported case in China in December 2019 as a case of pneumonia of unknown cause, the novel corona virus disease (COVID-19) has spread rapidly all over the world, and on March 11, 2020, the World Health Organization (WHO) declared COVID-19 a pandemic (Time, 2020). As of September 16, 2020, more than 29 million cases of COVID-19 and more than 900 thousand deaths due to the disease have been reported worldwide (WHO, 2020c). In its global devastating effects on all aspects of human lives, the impact of the epidemic quite varies from country to country, thus the study focused on a specific country can provide better understanding of the disease and its control strategies.
In Nepal, the first case of COVID-19 was confirmed on January 23, 2020, which was also the first COVID-19 case in South Asia (GoN, 2020). After this first case found to be an infected Nepali student who had recently returned from Wuhan, China (Wiki, 2020), no additional case was reported until March 23, 2020. On March 24, 2020, the Government of Nepal implemented a country-wide lockdown including business closures and restrictions on movement within the country and access to flights in and out of the country (UN, 2020). In addition, the Government of Nepal aggressively initiated a border screen policy to quarantine people traveling to Nepal from abroad, to test them, and to isolate them if the test is positive. Because of such timely and aggressively implemented control strategies, the number of COVID-19 cases in Nepal remained relatively low (only 4% of the total cases from local transmission) until mid of July, 2020 (EDCD, 2020c), when these policies ended. Since these policies were lifted, the new cases began to grow dramatically, and as of September 16, 2020 the total of 58,327 cases (mostly from local transmission) have been reported (EDCD, 2020a). We define the epidemic phase from March 22 to July 21 as the controlled phase, during which the daily recorded cases remained significantly low, and the epidemic phase from July 22 to September 16 (end of the study) as the outgrown phase, during which the daily recorded COVID-19 cases exponentially increased. A detailed study of the biphasic epidemic trend of COVID-19 appeared in Nepal provides us with an opportunity to identify and evaluate effects of control strategies in the context of countries like Nepal, which is uniquely characterized by an open border provision with India, one of the highest COVID-19 affected countries.
Mathematical modeling using nonlinear systems has been an important tool for describing the dynamics of infectious diseases and evaluating the control strategies to curb epidemics (He et al., 2020, Hiroshi et al., 2020, Keeling and Rohani, 2008, Martcheva, 2015, Okuonghae and Omame, 2020, Vaidya and Lindi, 2015, Yang et al., 2020, Zhang et al., 2012, Rahman et al., 2019, Van den Driessche and Watmough, 2020). Deterministic mathematical models, including the SEIR (Susceptible-Exposed-Infected-Recovered) model, have been widely used in quantitative studies of COVID-19 pandemics. While some models were used to estimate the parameters, such as incubation period and infectious period (Backer et al., 2020, Linton et al., 2020, Liu et al., 2020b, Wan et al., 2020), others examined the effectiveness of control strategies, such as lockdown, detection and isolation, border screening, and medical resources (Hellewell et al., 2020, Shayak et al., 2020, Sun et al., 2020, Xiao et al., 2020, Chanda, 2020, Cheng et al., 2020, Faal et al., 2020, Ferretti and Chris, 2020, Wang et al., 2020). The quarantine for the traveler and suspected cases were also studied as the effective control measures for mitigating COVID-19 (Armitage and Nellums, 2020, Hossain et al., 2020, Liu et al., 2020a, Yuan et al., 2020). Regarding COVID-19 in Nepal, previous studies (Bhandary, 2020, Bhuju et al., 2020, Pun et al., 2020, White et al., 2020) have provided some insights into doubling time of new infections, early transmission trend, and the timing of the daily incidence burden in Nepal. However, none of the previous models have considered the entry of cases through the Nepal-India open border and border-related control strategies, which can be important factors because the travel history of recorded infectious people shows that more than 80% infectious cases came from abroad, especially from India, during the early period of epidemics (EDCD, 2020b, Rijal, 2020). Also, despite the Nepal government’s effort of applying strategies, such as border screening, quarantine and isolation, poor handling policy at the border does exist, allowing many infected individuals to enter the community without quarantine (Shrestha, 2020).
In this study, we develop a deterministic mathematical model, which incorporates the imported as well as locally generated cases along with various policies implemented for the control of COVID-19 in Nepal. Using case data from both the controlled and outgrown phases of epidemics in Nepal, we estimated key parameters as well as the basic and effective reproductive numbers. Using our model, we evaluated the control strategies implemented in Nepal. Furthermore, we applied our model to predict the long-term dynamics of COVID-19 in Nepal, and provided the simulations to demonstrate how these control strategies can curb the epidemics in Nepal.
2. Method
2.1. Data source
The data used in this study was obtained from the Ministry of Health and Population, Epidemiology and disease control division (EDCD) of Nepal (EDCD, 2020a). Since March 22, 2020 is the last day of any single COVID-19 case in the country, we considered the data of COVID-19 from March 22. The government of Nepal started the countrywide lockdown and border screening from March 24 to July 21. Since the country returned into an almost no-policy state after the long route buses and national flights were fully opened on September 17, 2020 (WHO, 2020e), we considered the data until September 16, 2020. The data including quarantine, new cases, cumulative cases, and RT-PCR tests, were used in our model fitting and simulation. We note that during the initial phase of epidemic, most of the PCR tests performed were for the quarantined people and only a few for the community and front line workers (armed forces, hospital workers, civil workers, etc.). Therefore, we considered 80% of the PCR-tests performed were for the people who were quarantined.
2.2. Modeling basic transmission dynamics
We consider the transmission dynamics model based on the SEIR framework. We divide the whole population into five distinct compartments: S (susceptible), E (exposed), (recorded infectious), (non-recorded infectious), and R (recovered). In our model, susceptible individuals contract the virus when they come in contact with the non-recorded infectious individuals at the rate . These exposed individuals become infectious at per capita rate with the proportion being recorded and remaining non-recorded. Individuals from both and classes get recovered with the rate or die with the rate k. and represent the per capita rate of natural mortality and the natural recruitment rate into the susceptible class. We represent the entry of individuals from abroad, mainly across the Nepal-India border, by the time-dependent rate , among which the proportion are infected and the remaining are susceptible.
2.3. Modeling control strategies implemented in Nepal
The main control strategies implemented by the government of Nepal are: (i) Border screening and quarantine, (ii) Lockdown, and (iii) Detection and isolation.
Border screening and quarantine. To model the border screening and quarantine strategy, we introduce a quarantined class, Q, to which of individuals from abroad enter, where represents the rate of border screening. For these quarantined individuals PCR test is performed with rate and the tested individuals with positive result enter into the class and are isolated. As the expected rate of positive test in people entering into the country is , we assume that represents the portion of the tested population getting positive result, while the remaining portion of the tested population show negative result and enter the susceptible class, S. Due to the limitation of PCR test, there were cases of individuals, including some without onset of the symptoms, being released from the quarantine center without performing PCR test. We assume that individuals leave the quarantined class without PCR test at the rate of . Among them, the portion enters non-recorded infectious class and the remaining enters the susceptible class.
Lockdown. Lockdown strategy reduces the contact among individuals, and we assume the reduction of contact by resulting in the transmission rate . Since the strategy was altered in two different phases, the controlled and the outgrown, we consider two different reduction rates of contact as follows.
where represents the time when the epidemic phase changes corresponding to alteration of policies (July 21, 2020). As a result, the net infection rate becomes and before and after , respectively.
Detection and isolation. As mentioned above, recorded infected individuals, , in our model are isolated. Therefore, the detection and isolation strategy can be incorporated into our model by altering the rate . We introduce a parameter to represent the effect of the detection so that the rate of individuals in exposed class, who are detected and recorded, changes as . Since the strategy of testing for individuals in the general community was altered after the lockdown was lifted, we take two different detection rates for the controlled and outgrown phases as follows.
As a result, the net detection and isolation rate becomes and before and after , respectively.
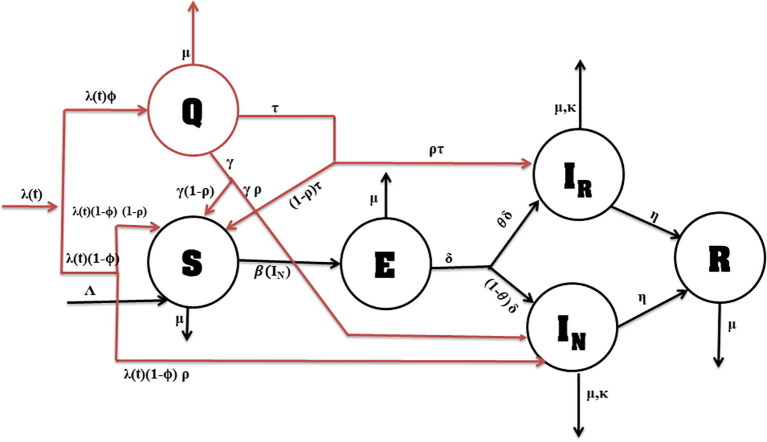
Combining all the control strategies implemented in Nepal into the basic transmission dynamics model, we obtain the model as shown in Fig. 1 . The model is described by the following system of ordinary differential equations.
| (1) |
| (2) |
| (3) |
| (4) |
| (5) |
| (6) |
Fig. 1.
Schematic diagram of the model. The arrow along with parameters shows the rate of flow from one compartment to another. The basic transmission dynamics of COVID-19 is shown in black color while the implemented control policies are indicated by red color.
Here, the total population is given by .
2.4. Estimation of population size and model parameters
Even though the first case of COVID-19 in Nepal was confirmed on January 23, 2020, no additional cases were reported until March 23, 2020. Therefore, we consider March 22, 2020 as the initial time for our dynamical system model. The total population of Nepal in the census year 2011 was 26,494,504, which was projected to reach 29,704,501 by the end of 2019 (CBS, 2011). There are about 3 to 4 million Nepalese working in India (Kunwar, 2015, TKP, 2020b) and about 1.5 million Nepalese working in the Gulf countries and Malaysia (MoL, 2020, IOM, 2019), making approximately the total of 5 million Nepalese as seasonal migrants. Therefore, deducting 5 million people as migrants from the total population of 29,704,501, we get = 25,000,000. Also, 63 people came from abroad were sent to Kharipati quarantine (a quarantine centre) on March 21 (TRN, 2020). Therefore, we take . The first case identified on January 23, 2020 had been recovered (GoN, 2020) by the beginning of our dynamics, and hence we take . Since the initial time of our dynamic model is the beginning of the epidemic, we assume , and .
Since the infected individuals remain in the exposed class for about 5.2 days until they become infectious (Stephen et al., 2020, Backer et al., 2020, WHO, 2020a), we take per day. Also, the infectious individuals get recovered in about 17 days (Time, 2020), implying the average recovery rate per day. We estimate the rate of death due to COVID-19 using the data taken from the official website of the Nepal government (GoN, 2020). Specifically, we take the average death rate from March 22 to September 16, 2020, and obtain the death rate per day. We take and in such a way that the natural birth rate and death rate remain equal for the period of this pandemic. In addition, we use the quarantine and PCR data along with the model to estimate parameters and , which are related to people leaving quarantine center. We estimate the remaining parameters and by using the least square fitting of the model to the daily recorded new case data.
2.5. Data fitting
We implemented the previous method (Rahman et al., 2019) to perform the data fitting and to identify a reasonable confidence interval of the estimated parameters. In brief, the method involves thorough process of consecutive reduction of number of parameters until the reasonable confidence intervals are identified. The process allowed us to identify the parameters , and that can be reasonably estimated from the available data. Further reduction of the number of parameters from the current six parameters provided a poor fit (F-test, p-value ).
For the model fitting the data available is the daily new cases of recorded infectious people. Using our model, the recorded new infections generated at time , can be computed using the following equation:
| (7) |
We solve the system of differential equations numerically using a fourth order Runge–Kutta method. We use the solutions to obtain the best-fit parameters via a nonlinear least squares regression method that minimizes the following sum of the squared residuals:
| (8) |
where , and are parameters to be estimated, and and are the new cases of recorded infectious people predicted by the model and those given in the available data, respectively. Here, n represents the total number of data points used for the model fitting. To obtain the confidence limits for the estimated parameters, we compute the standard errors from the sensitivity matrix (S) by using the complex-step derivative techniques described previously (Banks et al., 2014, Banks and Joyner, 2018, Rahman et al., 2019).
Furthermore, we use the sensitivity-based method (Miao et al., 2011) to analyze the identifiability of these parameters. In particular, we found the matrix to be of the full rank (rank = 6), which confirms the identifiability of the estimated parameters (Miao et al., 2011). In our study, all computations were carried out in MATLAB 2020a (The MathWorks, Inc.) using its various routines, including “ode45” (ODE solver) and “fmincon” (minimizer).
3. Results
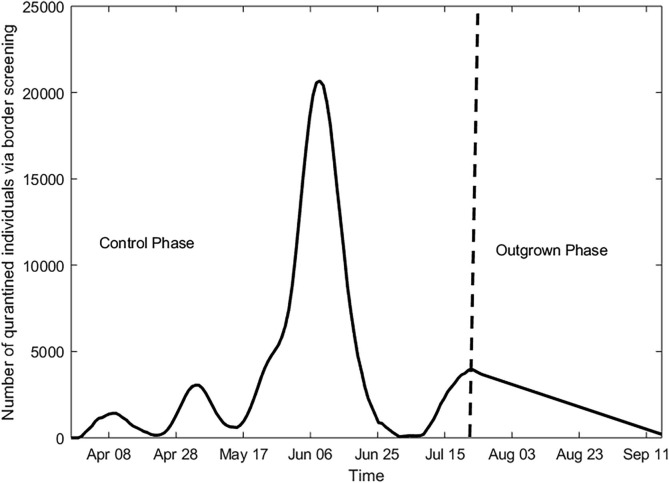
3.1. Estimation of border screen
Given the open border of Nepal with India, one of the most COVID-19 infected countries, and related border screen and quarantine policies implemented by the Nepal government, the rate of border screening and quarantine is important for accurate evaluation of the policy. However, the official data of this information is not available. We use our model to estimate the rate of border screen and quarantine, , from the data of the active quarantine population, , and the number of PCR-tests performed, .
Using the fact that the natural death is negligible during the short period of epidemic (i.e., ), we apply the model Eq. (1) at the data collected time to obtain the following approximation:
where day, as the data was recorded every day. In this expression, is given by , and represents those leaving quarantine center without PCR test (), implying
Since , we obtain the minimum estimate of as
Using data of active quarantine, , PCR tests, , and the estimated population leaving quarantine center without PCR, , we then estimated the daily number of people border screened and entered into the quarantine, , until July 21, 2020 (the controlled phase). Our estimates show that the rate of border screen and quarantine was relatively low (less than 2 thousand per day) until the mid of May, 2020, and then the rate increased rapidly reaching a peak of about 16 thousand per day around mid-June. After the peak, the rate began to fall and reached a low level by the end of the first phase of epidemic (Fig. 2 ). Data shows that, after July 21 (the outgrown phase), the active quarantined population continues to decrease indicating less impact of these individuals on the epidemic during the outgrown phase. Therefore, for simplicity, we assume that decreases linearly after July 21 (Fig. 2).
Fig. 2.
Estimation of border screen and quarantine. Estimated number of daily quarantined individuals using the border screening and quarantine policy.
Furthermore, we use our model to estimate the per capita rate of individuals leaving quarantine center with () and without () PCR test. We can approximate these rates as follows:
Our calculation shows that the individuals leave the quarantine center at the rate per day with PCR test and at the rate per day without PCR test.
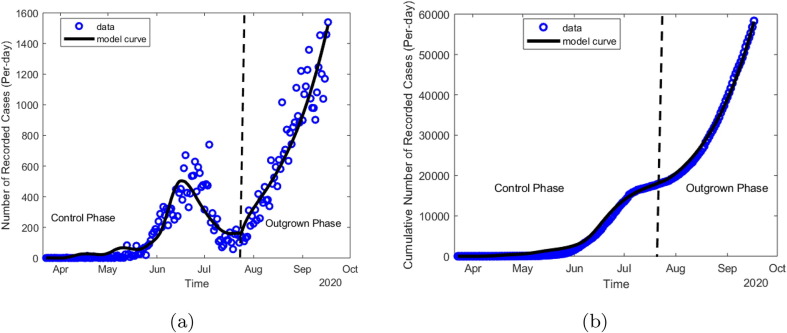
3.2. Epidemic pattern and model validation
We fitted our model to daily recorded new cases data of Nepal from both the controlled (March 22 to July 21) and the outgrown (July 21 to Sept 16) phases, and estimated six parameters , and . The values of the best estimates, along with their 95% confidence intervals, are provided in Table 1 . As shown in Fig. 3 a the model has an excellent agreement with the data of recorded new cases from both phases of the epidemic. In addition, we used our model to estimate the cumulative cases of COVID-19 during the entire period of study and compared our estimates with the data (Fig. 3b). Our model is capable of accurately predicting the cumulative cases of COVID-19 in Nepal for both epidemic phases, thereby validating our modeling approach.
Table 1.
Values of estimated and fixed parameters.
| Parameters | Value | 95% CI | Reference |
|---|---|---|---|
| 0.052 | [0.0085 0.0955] | Data fitting | |
| 0.248 | [0.20 0.29] | Data fitting | |
| 0.75 | [0.64 0.85] | Data fitting | |
| 0.57 | [0.49 0.65] | Data fitting | |
| 0.75 | [0.64 0.85] | Data fitting | |
| 0.052 | [0.04 0.063] | Data fitting | |
| k | 0.000281 | Fixed | Calculated |
| 0.00975 | Fixed | Calculated | |
| 0.06 | Fixed | Calculated | |
| 0.0588 | Fixed | (Li et al., 2020) | |
| 0.1923 | Fixed | Stephen et al., 2020, Backer et al., 2020, WHO, 2020a |
Fig. 3.
Data fitting and model validation. (a) Recorded daily new cases of COVID-19 data (circle) along with the best fit of the model prediction (line). (b) Cumulative cases over entire study period estimated using the model (line) along with the data (circle).
In consistence with the data, the epidemic trend of the COVID-19 in Nepal predicted by our model shows that the recorded COVID-19 cases increased slowly until the mid of May, attained the peak of the controlled phase during the mid-June, and then decreased until the end of the first phase (the controlled phase), when the policies were altered. After the controlled phase, the cases again started to rise with a higher rate until the end of the study, giving the outgrown phase following the controlled phase. It’s worth noting that the first peak observed during the controlled phase is around the same time when the maximum number of returned migrants were border-screened and quarantined (Fig. 2).
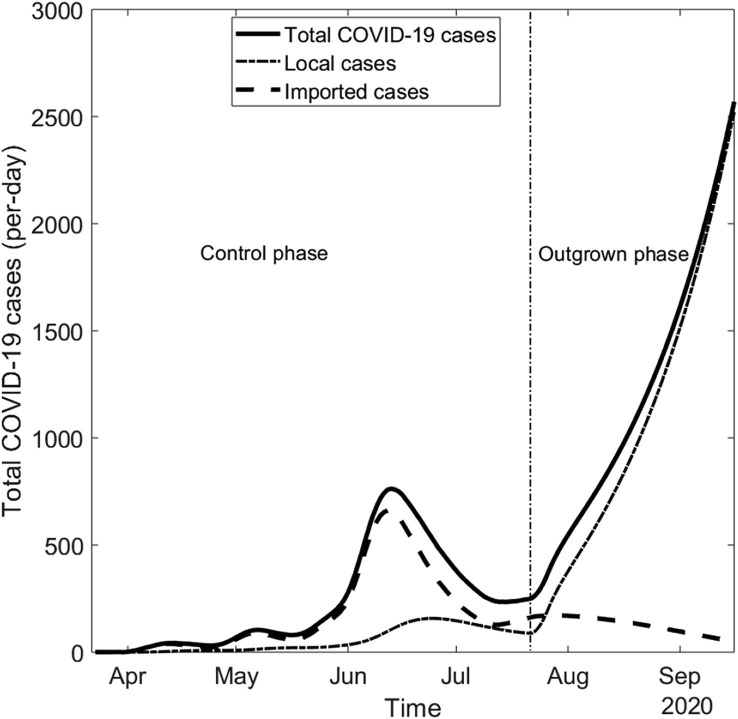
3.3. Importation vs local transmission of COVID-19 cases in Nepal
For countries like Nepal that shares open-border with another country (India) having one of the highest levels of COVID-19 cases, it is critical to identify the impact of importation through the border and the local transmission on the disease spread. We used our model to estimate the imported cases and the cases from local transmission, both recorded and non-recorded (Fig. 4 ). Our estimation shows that during the controlled phase of the epidemic, most of the COVID-19 cases in Nepal were imported, indicating the local transmission was well controlled. During this phase, the imported cases gradually increased while the local transmission remained significantly lower than the imported cases. The imported cases reached the maximum number (about 460) around July 01, consistent with the highest border screen (Fig. 2), and then gradually decreased for the entire period of our study.
Fig. 4.
Contribution of Importation vs local transmission in COVID-19 cases. Model estimation of the daily number of COVID-19 cases (solid line) along with the contributions from the importation through border (dashed line) and local transmission (dot-dashed line).
While the local transmission was quite controlled during the controlled phase (only 6,577 cases), during the outgrown phase the local cases dramatically increased outcompeting the imported cases at the end of July. The outgrown phase (July 22-September 16, 2020) resulted in 67,073 total cases (recorded and non-recorded), out of which 60,123 () are from local transmission, by the end of our study (September 16, 2020). Note that the timing of the dominance of the local transmission over importation is consistent with the alteration of policies by the government of Nepal, especially the lifting of the lockdown.
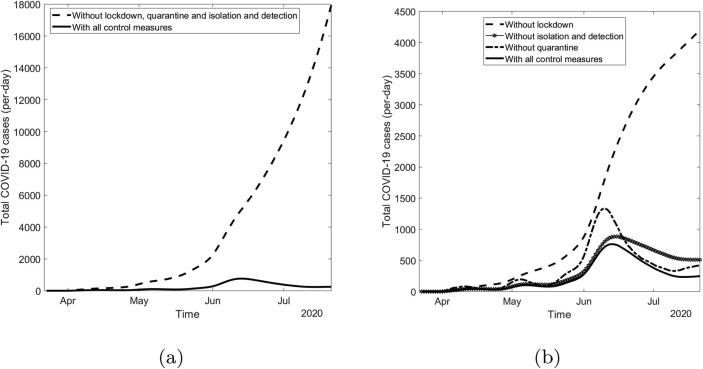
3.4. Effectiveness of control strategies
From the epidemic trend it can be clearly seen that the major policies implemented by the government of Nepal, namely border screening and quarantine, lockdown, and detection and isolation, were significantly effective because the disease spread was well-controlled while the policies were in place and became out of control once the policies were lifted. We can use our model parameters , and to quantify the effectiveness of these policies, border screen and quarantine, lockdown, and detection and isolation, respectively, on controlling COVID-19 epidemic in Nepal during the controlled phase. Our model shows that the epidemic dynamics would have been quite worse (19,090 new cases per day during the peak) if these policies were not implemented (Fig. 5 a). Through these policies, 442,640 cases were prevented and 1,216 lives were saved during the period of controlled phase (real scenario from the official data: 17,994 cumulative cases and 40 deaths).
Fig. 5.
Effect of control strategies. Daily new covid-19 cases (a) with (solid line) and without (dashed line) all control strategies in combination, and (b) with (solid line) and without one policy at a time, border screening and quarantine (dot-dashed line), lockdown (dashed line) and detection and isolation (star-line).
We also estimated the effectiveness of each of the policies individually (Fig. 5b). Removing each policy (border screen and quarantine, lockdown, and detection and isolation) at a time, our model predicts the peak infectious case of 1339, 4199, 884, respectively. As per our model estimation, in the absence of border screen and quarantine, lockdown, and detection and isolation, one at a time, the total cumulative cases would have reached 42050, 162400, 38920, respectively, taking the Nepalese lives of 162, 497, 138, respectively. Among these three policies lockdown was found to be the most significant, followed by the border screening and quarantine, and then by the detection and isolation. These results show that the detection and isolation does not seem to have significant impact on the reduction of infections and deaths on the early phase, compared to other two strategies, presumably because of the less local transmission due to the strict lockdown. However, the detection and isolation may have important role and significant impact during the outgrown phase when the local transmission becomes the leading cause of infection.
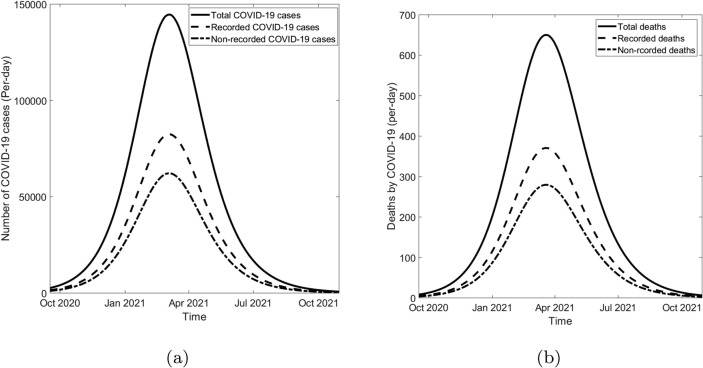
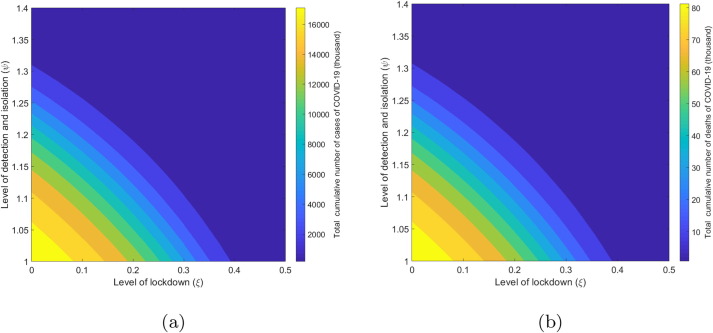
3.5. Long-term prediction and potential control in Nepal
In this section, we present our model prediction of epidemic outcome, especially the new cases, cumulative cases, and the total deaths, in Nepal by the end of the year 2021. If the current trend continues without any interventions, our model predicts that the peak value of daily new cases will reach 144,600 (82,420 recorded and 62,180 non-recorded) on March 4, 2021 (Fig. 6 a). With this epidemic trend, Nepal will suffer from the cumulative cases of 18.76 million (10.70 million recorded and 8.06 million non-recorded) and the total COVID-19-related deaths of 87 thousand by the end of 2021 (Fig. 6b).
Fig. 6.
Long-term dynamics of COVID-19 in Nepal. Long-term dynamics of (a) daily new cases and (b) daily deaths due to COVID-19, predicted by our model. Here, the current (Oct 2020) peak of the new cases and daily deaths are 1,127 and 4, respectively..
At the current situation of the limited pharmaceutical prevention, applying public health measures, including the ones the government of Nepal implemented during the controlled phase, are the most promising control mearues (MoHP, 2020; WHO, 2020b). We now assess the impact of these control measures on curbing COVID-19 epidemics from September 2020 to December 2021. Since the current trend (the outgrown phase) shows that the imported COVID-19 cases are not important compared to the local transmission, we particularly focus on two control strategies, the lockdown and the detection and isolation. Note that the current value of infection rates is and the detection rate is (Table 1). In our model, the level of lockdown and detection and isolation can be incorporated using the parameters and , respectively.
Our model predicts that both the lockdown (reduction on ) and the detection and isolation (increment in ) are significantly impactful on curbing COVID-19 epidemic burden in Nepal (Fig. 7 ). For example, 50% reduction of contact through lockdown (i.e., ) can reduce the cumulative number from the base-case of 18.7 million to 426 thousand and the total deaths from 87 thousand to 20 thousand. Similarly, 1.4 times increment in the detection and isolation rate (i.e., ) can bring the cumulative cases down to 494 thousand and the total death down to 13 thousand.
Fig. 7.
Long-term impact of control policies. Model prediction of (a) the cumulated cases and (b) the cumulative deaths due to COVID-19 by December 2021, under the different levels of lockdown and detection and isolation.
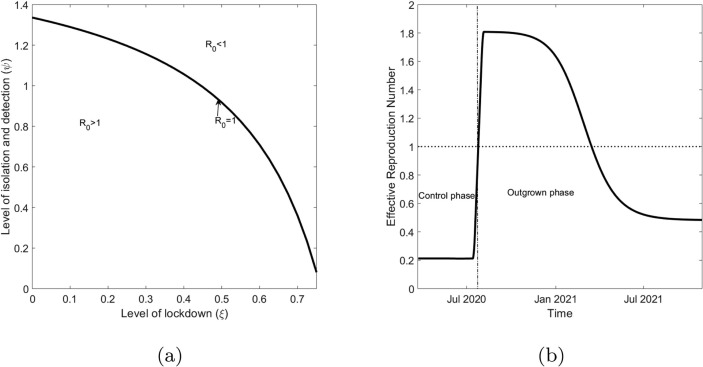
3.6. Reproduction number
The basic reproduction number, , is an average number of secondary infections generated by a single infectious individual in a completely susceptible population. For infectious diseases, it is an important threshold, which helps determine whether outbreak occurs or is avoided () (Martcheva, 2015). We used the Next Generation Matrix method (Diekmann et al., 1990, Van den Driessche and Watmough, 2020) to derive the expression of for our model (see Appendix) and obtained
where
As expected, we are able to theoretically establish as the outbreak threshold for our model, as stated in the following theorem:
Theorem 1
Disease free equilibrium point of the system of Eqs.(1), (2), (3), (4), (5), (6)is asymptotically stable ifand unstable if.
The proof of the theorem is given in Appendix. Using the estimated parameters, we found the value of for Nepal. implies that the outbreak was avoided at the time the locally infected case was introduced in March 2020. The successful control is consistent with the fact that the local transmission during early epidemic period was negligible with the majority of infections coming from abroad. Furthermore, we found that if the government of Nepal had not timely implemented policies (i.e., if we replace by and by ), the basic reproduction number would have been . Using our model, we also performed analysis to identify the level of lockdown () and the level of detection and isolation () required to assure the value of less than unity so that the epidemic is avoided. The resulting combinations of these two policies, which can avoid the epidemic, are shown in Fig. 8 a. For example, a policy with combination of 22% reduction in contact due to lockdown () and 1.2 times increase in detection and isolation () can make less than unity, thereby avoiding epidemic to occur.
Fig. 8.
Reproduction numbers. (a) Parameter space showing the level of lockdown () and the level of detection and isolation () that make less than or greater than 1. (b) Effective reproduction number of COVID-19 () in Nepal until December 2021.
While the basic reproduction number provides the important information about the beginning of the epidemic, the average number of the secondary infections varies over time, mainly due to alteration of implementation of policies over the epidemic period. To describe the time varying average number of secondary cases more accurately, we considered the effective reproduction number, . The value of allows us to track whether the epidemic at time t is in increasing () or decreasing () trend. For our model, the effective reproduction number is given by
Using the estimated parameters, we observed that the value of effective reproduction number remains about 0.21 until July 21 (Fig. 8b), indicating that the local transmission is under control during the controlled phase. However, around July-21 (the date of end of policies), the effective reproduction number rapidly increased and reached 1.80 indicating the rapid local transmission during the outgrown phase. The long-term prediction of our model shows that the value of remains greater than unity until March 2021 (increasing trend). After March 2021, the epidemic will observe the decreasing trend (i.e, ).
4. Discussion
In this study, we focused on modeling COVID-19 epidemic in Nepal, which shares an open border with India, one of the most affected countries in the world. Since a large number of Nepalese, especially male labor migrants, work in India, the mobility across the Nepal-India open border has directly affected COVID-19 cases in Nepal, causing considerable number of imported cases through the migrant workers coming from India (EDCD, 2020c). Despite a large number of inflow of COVID-19 cases from India, the timely implementation of the Nepal Government’s policies, namely (i) border screen and quarantine, (ii) lockdown, and (iii) detection and isolation, was successful in controlling the epidemic for about four months until these policies were lifted on July 21, 2020. After the policies were lifted, the cases surged uncontrollably, resulting in a biphasic trend of COVID-19 in Nepal, the controlled phase (until July 21, 2020) and the outgrown phase (after July 21, 2020). In order to evaluate these successful control policies, here we took advantage of modeling and data of unique epidemic in Nepal with biphasic trend resulting from the combination of case-inflow through the Nepal-India border and control policy implementation. Our novel model, which is capable of excellently describing the COVID-19 data from Nepal, has provided number of important insights into transmission dynamics and related effective control policies.
Using our model and the available data from the ministry of health and population, we estimated the key parameters related to COVID-19 transmission and control in Nepal. Based on our model, we identified quite distinct transmission rate and distinct rate of detection and isolation between two phases of epidemics, showing that the policies implemented were indeed significantly effective. The timely implementation of policies was able to maintain the low level of effective reproduction number () while the polices were in place, and upon lifting the policies the effective reproduction number rapidly rose to 1.80. As per our model evaluation, with these policies the government of Nepal was able to prevent more than 444 thousand cases and save more than 1,200 lives. Among these three policies, “lockdown” was found to be the most effective, followed by “border screen and quarantine” and then by “detection and isolation”.
Consistent with the data based on the travel history of recorded infectious people (more than 80% came from aboard, especially from India) (EDCD, 2020b, Rijal, 2020), our result also shows that about 70% of COVID-19 cases in Nepal were imported during the controlled phase. Despite inflow of significant number of COVID-19 cases from India, the local transmission remains well controlled during the controlled phase of epidemic, implying that the “border screening and quarantine” policy in combination with other policies implemented by the government of Nepal was key to avoid a potential early surge of cases from local transmission. Our model predicts a high rate of local transmission, consistent with the data, during the outgrown phase (i.e., after the policies were lifted on July 21, 2020). As a result, the contribution of the local transmission to epidemics became significantly high outcompeting the importation after July 21, 2020. We note that along the line of our results, various reports and updates on the situation of Nepal (Pun et al., 2020, NIE, 2020, EDCD, 2020b, TKP, 2020a, WHO, 2020d, WHO, 2020e, WHO, 2020g) also claim that there were small number of local transmissions before July 21, 2020 and the mass community transmission has become noticeable only after lifting the policies on July 21, 2020.
Based on the current epidemic trend identified by our model, we predict that without any interventions about 18 million Nepalese ( of the total population) will be infected with COVID-19 by the end of 2021. The model predicts that the current increasing trend of daily new cases will continue to increase reaching the peak level of about 144 thousand new cases per day on March 04, 2021. However, we also acknowledge that there is a possibility for the peak time to occur earlier, as projected by some studies (White et al., 2020), if the government reduces the testing of asymptomatic cases (i.e., reduces the detection and isolation in our model) as mentioned in OLK (2020). Because Nepal is in the high risk zone of COVID-19 due to its poor health system and porous borders with India, potential epidemic outcomes predicted by our model strongly recommend the urgent implementation of control strategies.
Since the pharmaceutical control of COVID-19 is not widely available, most of the countries have been implementing the non-pharmaceutical approaches, including the ones implemented by the government of Nepal, for mitigating COVID-19 transmissions. As identified by our model in the context of Nepal, many countries, such as China, Taiwan, and South Korea, which have been successful to control the epidemics, also applied the strict lockdown, meticulous testing and tracking, and massive isolation of people, precise and widespread contact tracing and testing (Azman and Luquero, 2020, Choi, 2020, Trevisan et al., 2020, Cheng et al., 2020) as effective means of epidemic control. Therefore, we also evaluated the local transmission related control strategies “Lockdown” and ”Detection and isolation” in the context of Nepal, and identified the level of these policies required for successful mitigation of potential COVID-19 surge in Nepal. For example, our result shows that the lockdown level that can reduce the contact rate by 50% will decrease the peak of new cases of COVID-19 below 2,600, significantly less than the predicted base-case of 144 thousand. In this level of lockdown, the cumulative cases will also reduce from 18 million to less than 200 thousand. Similarly, the total COVID-19 cases can be reduced to 494 thousand if the detection and isolation policy is increased by 1.4 times the base case. Importantly, our model has identified that for a significantly large level of the detection and isolation (for example, greater than 1.6 time the base case), the disease spread can be avoided without needing a high level of lockdown.
We acknowledge several limitations of our study. We used the limited data sets available publicly from the ministry of health and population of Nepal. Because of poor policy at the border, the data related to border screen need to be carefully considered. The detailed data with accurate border screening and quarantine will improve the predictions of our model. While the testing program for border screened population was better documented, the testing for local community is less understood, which may have slightly impacted on our estimates of detection and isolation rate. However, we conducted sensitivity of this parameter over the wider range. We have ignored the spatial heterogeneity on the dynamics and policy implementation, especially among seven provinces of Nepal. Not all provinces equally share border with India and also cases distribution is not uniform. For example, Gandaki province has sporadic transmission (WHO, 2020f) while other six provinces (Province 1, Province 2, Bagmati, Lumbini, Karnali and Sudurpaschim) show clusters of cases. Therefore, future studies on province-wise analysis of COVID-19 transmission along with inter-province mobility will help for better implementation of effective control strategies.
In summary, we developed a novel mathematical model to uncover effective control strategies that were implemented in unique biphasic epidemic trend in Nepal, under the influence of human mobility across the open-border with India, one of the most COVID-19 affected countries in the world. Quantification of these successful control strategies through distinct two phases of epidemic in Nepal (the controlled phase and the outgrown phase) has provided us with opportunity to evaluate the impact of these strategies to curb potential surge in Nepal. Our results may provide important policy guidance for devising the appropriate control strategies for bringing Nepal out from the devastating pandemic.
CRediT authorship contribution statement
Khagendra Adhikari: Formal analysis, Investigation, Methodology, Writing - original draft. Ramesh Gautam: Formal analysis, Investigation, Methodology, Writing - original draft. Anjana Pokharel: Formal analysis, Investigation, Methodology, Writing - original draft. Kedar Nath Uprety: Formal analysis, Supervision, Writing – review and editing. Naveen K. Vaidya: Conceptualization, Formal analysis, Supervision, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
KA acknowledges Nepal Academy of Science and Technology (NAST) for Ph.D. Fellowship. AP acknowledges the financial support from International Mathematical Union (IMU) through the Graduate Research Assistantships in Developing Countries (GRAID) award 2020. KA, RG and AP acknowledge the Nepal Mathematical Society (NMS) for the NMS Ph.D. Fellowship Award 2020. The work of NKV was supported by NSF grants DMS-1951793, DMS-1616299, DMS-1836647, and DEB-2030479 from National Science Foundation of USA and the UGP award from San Diego State University.
Appendix A.
A.1. Derivation of basic reproduction number, , using the next generation matrix
We first obtain the disease free equilibrium, , of the model system. Using the pre-pandemic condition and the disease-free conditions , we obtain . Then the model system provides the following disease free equilibrium:
where
According to the next generation matrix method, we divide the compartments used in the model into two groups: infected and non-infected group . Then the model system can be written as:
We now write the right hand side of the system of infected compartments as , where contains the terms representing the new infections in compartment i and contains the terms containing the difference between the transfer of individuals out of and into the compartment i:
We now take the values and corresponding to the beginning of the epidemic, and construct the following two matrices using and .
These matrices allow use to compute the second generation matrix as follows:
whose eigenvalues are 0, 0, and . Then the basic reproduction number is given by the dominant eigenvalue. Therefore,
A.2. Proof of Theorem 1
Jacobian of the system of Eqs. (2), (3), (4), (5), (6) evaluated at the disease free equilibrium, , is
The eigenvalues of this Jacobian are given by
and
We can clearly observe that all the eigenvalues are negative if . Therefore, the disease free equilibrium, , is asymptotically stable if and unstable if .
References
- Armitage R., Nellums L.B. COVID-19 and the Gypsy, Roma and Traveller population. Public Health. 2020;185:48. doi: 10.1016/j.puhe.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azman A.S., Luquero F.J. From China: hope and lessons for COVID-19 control. Lancet Infect Dis. 2020;20(7):756–757. doi: 10.1016/S1473-3099(20)30264-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backer, J.A., Klinkenberg, D., Wallinga, J., 2020. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20-28 January 2020. Euro Surveill 25(5). 10.2807/1560-7917.ES.2020.25.5.2000062. [DOI] [PMC free article] [PubMed]
- Banks H.T., Joyner M.L. Information content in data sets: A review of methods for interrogation and model comparison. Journal of Inverse and Ill-Posed Problems. 2018;26 doi: 10.1515/jiip-2017-0096. [DOI] [Google Scholar]
- Banks H.T., Hu S., Tompson W.C. CRC Press; Boca Raton London: 2014. Modeling and Inverse Problems in the Presence of Uncertainty. [Google Scholar]
- Bhandary S. Effectiveness of lockdown as COVID-19 intervention: official and computed cases in Nepal. Journal of Patan Academy of Health Sciences. 2020;7(1):37–41. doi: 10.3126/jpahs.v7i1.28861. [DOI] [Google Scholar]
- Bhuju G., Phaijoo G., Gurung D. Modeling transmission dynamics of COVID-19 in Nepal. Journal of Applied Mathematics and Physics. 2020;8(10):2167–2173. doi: 10.4236/jamp.2020.810162. [DOI] [Google Scholar]
- CBS, 2011. National Population and Housing Census 2011 (Population Projection 2011-2031), Central Bureau of Statistics, Nepal, Volume 08, NPHC 2011. URL: https://cbs.gov.np/wp-content/upLoads/2018/12/PopulationProjection2011-2031.pdf (Accessed: 2020-09-10).
- Chanda, A., 2020. COVID-19 in India: transmission dynamics, epidemiological characteristics, testing, recovery and effect of weather. Epidemiology and Infection 148, e182, 1–10. 10.1017/S09. [DOI] [PMC free article] [PubMed]
- Cheng H.Y., Jian S.W., Liu D.P., Ng T.C., Huang W.T., Lin H.H., et al. Contact tracing assessment of COVID-19 transmission dynamics in Taiwan and risk at different exposure periods before and after symptom onset. JAMA Intern Med. 2020;180(9):1156–1163. doi: 10.1001/jamainternmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J.Y. Covid-19 in South Korea. Postgrad. Med. J. 2020;96:399–402. doi: 10.1136/postgradmedj-2020-137738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diekmann, O., Heesterbeek, J.A.P., Metz, J.A.J., 1990. On the definition and the computation of the basic reproduction ratio in models for infectious diseases in heterogeneous populations. J. Math. Biol. 28 (4), 365–382. 10.1007/BF00178324 hdl:1874/8051. PMID 2117040. S2CID 22275430. [DOI] [PubMed]
- EDCD, 2020a. COVID-19 Statistics: Nepal. Epidemiology and Disease Control Division. URL: https://portal.edcd.gov.np/covid19/. Accessed: 2020-09-17.
- EDCD, 2020b. Detail epidemiological update COVID-19-National and Provinces, 11 August 2020. Epidemiology and diseases control Division, Nepal. URL: http://edcd.gov.np/news/download/epidemiological-update-on-covid-19-11-aug-2020. Accessed: 2020-09-26.
- EDCD, 2020c. Epidemiological Update on COVID 19. Epidemiology and diseases control Division. Nepal, (17 July 2020). URL: http://edcd.gov.np/news/download/epidemiological-update-on-covid-19-17-july-2020. Accessed:2020-09-27.
- Faal N., Ivn A., Delfim F.M.T., Juan J.N. Mathematical modeling of COVID-19 transmission dynamics with a case study of Wuhan. Chaos Solitons Fract. 2020;135:109846. doi: 10.1016/j.chaos.2020.109846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferretti L., Chris W. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science. 2020;368(6491):eabb6936. doi: 10.1126/science.abb6936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GoN, 2020. COVID-19 Nepal. Government of Nepal, URL: https://covidnepal.org. Accessed: 2020-09-18.
- He S., Peng Y., Sun K. SEIR modeling of the COVID-19 and its dynamics. Nonlinear Dyn. 2020;101:1667–1680. doi: 10.1007/s11071-020-05743-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellewell J., Abbott S., Gimma A., Bosse N.K., Jarvis C.I., Russell T.W., et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020;8(4):e488–e496. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiroshi N., Natalie M.L., Andrei R.A. Serial interval of novel corona virus (COVID-19) infections.International. J. Infect. Dis. 2020;93:284–286. doi: 10.1016/j.chaos.2020.109846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossain, M.P., Junus, A., Zhu, X., Jia, P., Pfeiffer, D., Yuan, H.Y., 2020. The effects of border control and quarantine measures on the spread of COVID-19. Epidemics 32,100397. 10.1016/j.epidem.2020.100397. [DOI] [PMC free article] [PubMed]
- IOM, 2019. Migration in Nepal -A COUNTRY PROFILE 2019. Kathmandu, Nepal. International Organization for Migration. URL: https://publications.iom.int/system/files/pdf/mp_nepal_2019.pdf.
- Keeling M.J., Rohani P. Modeling Infectious Diseases in Humans and Animals. Princeton University Press. 2008 doi: 10.2307/j.ctvcm4gk0. 41 William Street Princeton, NJ 08540-5237 USA. http://www.jstor.org/stable/j.ctvcm4gk0. [DOI] [Google Scholar]
- Kunwar S.K. Emigration of Nepalese People and Its Impact. Econ. J. Develop. Issue. 2015;19(20):77–82. [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linton N.M., Kobayashi T., Yang Y., Hayashi K., Akhmetzhanov A.R., Jung S.M., Yuan B., Kinoshita R., Nishiura H. Incubation period and other epidemiological characteristics of 2019 novel coronavirus infections with right truncation: a statistical analysis of publicly available case data. J. Clin. Med. 2020;9:538. doi: 10.3390/jcm9020538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Tang J.W., Lam T.Y. Cold Spring Harbor Laboratory Press; 2020. Transmission Dynamics of the COVID-19 Epidemics in England. [DOI] [Google Scholar]
- Liu, Z., Magal, P., Seydi, O., Webb, G.A, 2020. COVID-19 epidemic model with latency period. Infect. Dis. Model. 5, 323–337. 10.1016/j.idm.2020.03.003 [DOI] [PMC free article] [PubMed]
- Martcheva M. Texts in Applied Mathematics. Springer; 2015. An Introduction to Mathematical Epidemiology, ISSN 2196-9949. [Google Scholar]
- MoHP, 2020. Critical preparedness, readiness and response actions for COVID-19, 2020. Ministry of Health and Population, Government of Nepal. URL: https://www.who.int/publications/i/item/critical-preparedness-readiness-and-response-actions-for-covid-19. Accessed: 2020-09-18.
- MoL, 2020. Nepal Labour Migration Report,2020. Government of Nepal, Ministry of Labour, Employment and Social Security. URL: https://moless.gov.np/wp-content/uploads/2020/03/Migration-Report-2020-English.pdf. Accessed: 2020-09-17.
- Miao H., Xia X., Perelson A.S., Wu H. On identifiability of nonlinear ODE models and applications in viral dynamics. SIAM Rev. 2011;53(1):3–39. doi: 10.1137/090757009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIE, 2020. Coronavirus infection in Nepal enters community transmission phase. The New Indian Express. URL: https://www.newindianexpress.com/world/2020/sep/02/coronavirus-infection-in-nepal-enters-community-transmission-phase-2191464.html. Accessed: 2020-09-26.
- Okuonghae D., Omame A. Analysis of a mathematical model for COVID-19 population dynamics in Lagos, Nigeria. Chaos Solitons Fract. 2020;139 doi: 10.1016/j.chaos.2020.110032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OLK, 2020. Poor contract tracing in Kathmandu- Two per infectious. Onlinekhabr. URL: https://www.onlinekhabar.com/2020/09/894783. Accessed: 2020-09-27.
- Pun S.B., Mandal S., Bhandari L., Jha S., Rajbhandari S., Mishra A.K., Chalise B.S., Shah R. Understanding COVID-19 in Nepal. J. Nepal Health Res. Counc. 2020;18(1):126–127. doi: 10.33314/jnhrc.v18i1.2629. [DOI] [PubMed] [Google Scholar]
- Rahman, M., Bekele-Maxwell, K., Cates, L.L., Banks, H.T., Vaidya, N.K., 2019. Modeling Zika virus transmission dynamics: parameter estimates, disease characteristics, and prevention. Sci. Rep. 9 (1), 10575. doi:10.1038/s41598-019-46218-4. [DOI] [PMC free article] [PubMed]
- Rijal, A., 2020. 99% COVID-19 cases in Nepal asymptomatic, 97% Imported. The Rising Nepal. URL: https://risingnepaldaily.com/main-news/99-covid-19-cases-in-nepal-asymptomatic-97-imported. Accessed: 2020-09-27.
- Shayak B., Sharma M.M., Rand R.H., Singh A.K., Misra A. Transmission dynamics of COVID-19 and impact on public health policy. medRxiv. 2020 doi: 10.1101/2020.03.29.20047035. [DOI] [Google Scholar]
- Shrestha, S., 2020. Hundreds of Nepalese stuck at India border amid COVID-19 lockdown. ALJAZERA. URL: https://www.aljazeera.com/news/2020/04/01/hundreds-of-nepalese-stuck-at-india-border-amid-covid-19-lockdown/. Accessed: 2020-06-26.
- Stephen A.L., Kyra H.G., Qifang B.I., Forrest K.J., Qulu Z., Hannah R.M., Andrew S.A., Nicholas G.R., Justin L. The Incubation Period of Coronavirus Disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020;172:577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun G.Q., Wang S.F., Li M.T., Li L., Zhang J., Zhang W., Jin Z., Feng G.L. Transmission dynamics of COVID-19 in Wuhan, China: effects of lockdown and medical resources. Nonlinear Dynamics. 2020;Jun 24:1–13. doi: 10.1007/s11071-020-05770-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Time, 2020. World Health Organization Declares COVID-19 a `Pandemic’ Here’s What That Means. URL: https://time.com/5791661/who-coronavirus-pandemic-declaration/. Accessed:2020-08-04.
- TKP, 2020. No evidence of Covid community transmission yet but infection cases could rise, WHO Nepal representative says.THE KATHMANDU POST. 10 June, 2020. URL: https://tkpo.st/2YkDnKV. Accessed:2020: 09-26.
- TKP, 2020. With hundreds of thousands of migrants predicted to return home, Nepal needs to brace for a crisis. THE KATHMANDU POST (22 April, 2020). URL: https://tkpo.st/2xNRgYL. Accessed: 2020-08-02.
- Trevisan M., Le L.C., Le A.V. The COVID-19 pandemic: a view from Vietnam. Am. J. Public Health. 2020;110:1152–1153. doi: 10.2105/AJPH.2020.305751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TRN, 2020. Sixty three People Sent To Kharipati Quarantine. The Rising Nepal. URL: https://risingnepaldaily.com/mustread/63-people-sent-to-kharipati-quarantine. Accessed: 2020-05-10.
- UN, 2020. COVID-19 Nepal: Preparedness and Response Plan (NPRP) April-2020. UNITED NATIONS, Nepal. URL: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/covid-19-nepal-preparedness-and-response-plan-(nprp)-draft-april-9.pdf?sfvrsn=808a970a_2.
- Vaidya N.K., Lindi M.W. Avian influenza dynamics under periodic environmental conditions. SIAM J. Appl. Math. 2015;75(2):443–467. doi: 10.1137/140966642. [DOI] [Google Scholar]
- Van den Driessche, P., Watmough, J., 2020. Reproduction numbers and sub-threshold endemic equilibria for compartmental models of disease transmission. Mathematical Biosciences 180, 29–48. 10.1016/S0025-5564(02)00108-6. PMID 12387915. [DOI] [PubMed]
- Wan, H., Cui, J., Yang, G., 2020. Risk estimation and prediction of the transmission of coronavirus disease-2019 (COVID-19) in the mainland of China excluding Hubei province. Infect. .Dis Poverty 9 (116). 10.1186/s40249-020-00683-6. [DOI] [PMC free article] [PubMed]
- Wang, L., Wang, J., Zhao, H., Shi, Y., Wang, P., Wu, Shi, L.. 2020. Modeling and assessing the effects of medical resources on transmission of novel corona virus (covid19) in Wuhan, China. Math. Biosci. Eng. 17 (4), 2936–2949. 10.3934/mbe.2020173. [DOI] [PubMed]
- White, L., Letchford, N., Pokharel, S., Lata, D., Zaman, R. 2020. Modelling of COVID-19 Strategies in Nepal Final Report, Oxford Policy Management Limited Registered in England. URL: https://reliefweb.int/sites/reliefweb.int/files/resources/Nepal_COVID-19_modelling_-_final_published.pdf. Accessed: 2020-08-17.
- WHO, 2020a. Coronavirus disease 2019 (COVID-19) Situation Report. 2 April, 2020. World Health Organization (WHO). URL: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200402-sitrep-73-Covid-19.pdf/. Accessed: 2020-06-04.
- WHO, 2020b. COVID-19 Strategy Update. World Health Organization (WHO). URL: https://www.who.int/docs/default-source/coronaviruse/covid-strategy-update-14april2020.pdf?sfvrsn=29da3ba0_12. Accessed: 2020-08-12.
- WHO, 2020c. WHO Coronavirus Disease (COVID-19) Dashboard URL: https://covid19.who.int/. Accessed: 2020-09-21.
- WHO, 2020d. Situation Update Report 19 (26 August, 2020), Coronavirus disease 2019 (COVID-19), WHO Country Office for Nepal. URL: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/19-who-nepal-sitrep-covid-19.pdf?sfvrsn=c9fe7309_2. Accessed: 2020-09-26.
- WHO, 2020e. Situation Update Report 22 (16 September, 2020), Coronavirus disease 2019 (COVID-19), WHO Country Office for Nepal. URL: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/22-who-nepal-sitrep-covid-19.pdf?sfvrsn=df7c946a_2. Accessed: 2020-09-26.
- WHO, 2020f. Situation Update Report 23 (23 September, 2020), Coronavirus disease 2019 (COVID-19), WHO Country Office for Nepal. URL: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/23-who-nepal-sitrep-covid-19.pdf?sfvrsn=1c07f023_2. Accessed: 2020-09-25
- WHO, 2020g. Situation Update Report 18 (19 Aug 2020), Coronavirus Diseases 2019 Nepal, WHO Country Office for Nepal. URL: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/18-who-nepal-sitrep-covid-19-23082020.pdf?sfvrsn=6fb20500_2. Accessed: 2020-09-16.
- Wiki, 2020. COVID-19 pandemic in Nepal. URL:https://en.wikipedia.org/wiki/COVID-19_pandemic_in_Nepal. Accessed: 2020-09-26.
- Xiao Y., Tang B., Wu J., Cheke R.A., Tang S. Linking key intervention timings to rapid decline of the COVID-19 effective reproductive number to quantify lessons from mainland China. Int. J. Infect. Dis. 2020;97:296–298. doi: 10.1016/j.ijid.2020.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z., Zeng Z., Wang K., Wong S.S., Liang W., Zanin M., et al. Modified SEIR and AI prediction of the epidemics trend of COVID-19 in China under public health interventions. J. Thorac. Dis. 2020;12:165–174. doi: 10.21037/jtd.2020.02.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan H.Y., Mao A., Han G., Yuan H., Pfeiffer D. medRxiv 2020.04.09.20059006; doi: https://doi.org/10.1101/2020.04.09.20059006; 2020. Effectiveness of quarantine measure on transmission dynamics of COVID-19 in Hong Kong. [Google Scholar]
- Zhang H., Small M., Fu X., Sun G., Wang B. Modeling the influence of information on the coevolution of contact networks and the dynamics of infectious diseases. Physica D: Nonlinear Phenom. 2012;241(18):1512–1517. doi: 10.1016/j.physd.2012.05.011. [DOI] [Google Scholar]