Highlights
-
•
Middle school parents’ concussion-symptom knowledge scores were relatively high; however, parents struggled to identify emotional symptoms, such as feeling sadness, being more emotional, and feeling nervous or anxious, as concussion symptoms.
-
•
Parents generally had positive attitudes toward concussion care seeking, although they noted some difficulty in the perceived ease of seeking concussion care.
-
•
Numerous factors were found to be associated with greater concussion-symptom knowledge and more positive concussion care-seeking attitudes. For example, the odds of higher scores were associated with increased parental age and with being white or non-Hispanic vs. being from another racial or ethnic group.
Keywords: Pediatrics, Traumatic brain injury, Youth
Abstract
Background
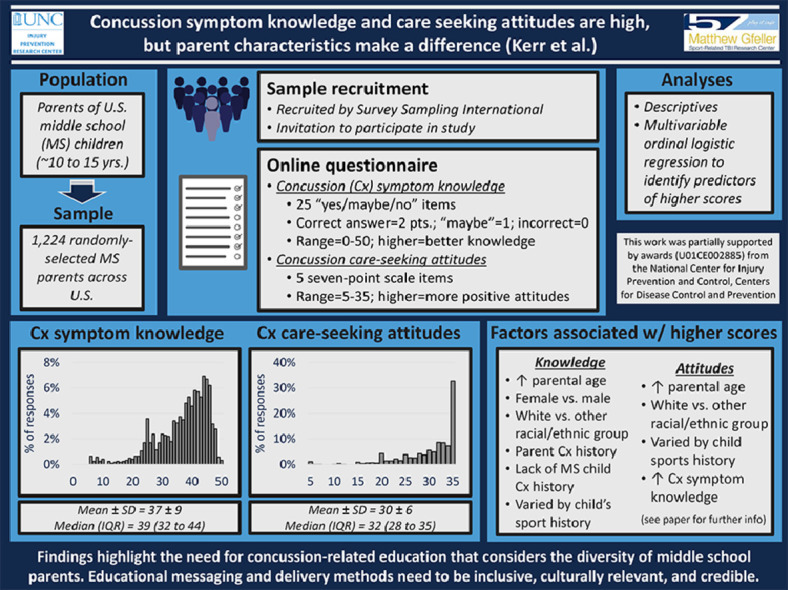
Developing appropriate concussion prevention and management paradigms in middle school (MS) settings requires understanding parents’ general levels of concussion-related knowledge and attitudes. This study examined factors associated with concussion-symptom knowledge and care-seeking attitudes among parents of MS children (aged 10–15 years).
Methods
A panel of 1224 randomly selected U.S. residents, aged ≥ 18 years and identifying as parents of MS children, completed an online questionnaire capturing parental and child characteristics. The parents’ concussion-symptom knowledge was measured using 25 questions, with possible answers being “yes”, “maybe”, and “no”. Correct answers earned 2 points, “maybe” answers earned 1 point, and incorrect answers earned 0 point (range: 0–50; higher scores = better knowledge). Concussion care-seeking attitudes were also collected using five 7-point scale items (range: 5–35; higher scores = more positive attitudes). Multivariable ordinal logistic regression models identified predictors of higher scores. Models met proportional odds assumptions. Adjusted odds ratios (aORs) with 95% confidence intervals (95%CIs) (excluding 1.00) were deemed statistically significant.
Results
Median scores were 39 (interquartile range: 32–44) for symptom knowledge and 32 (interquartile range: 28–35) for care-seeking attitude. In multivariable models, odds of better symptom knowledge were higher in women vs. men (aOR = 2.28; 95%CI: 1.71–3.05), white/non-Hispanics vs. other racial or ethnic groups (aOR = 1.88; 95%CI: 1.42–2.49), higher parental age (10-year-increase aOR = 1.47; 95%CI: 1.26–1.71), and greater competitiveness (10%-scale-increase aOR = 1.24; 95%CI: 1.13–1.36). Odds of more positive care-seeking attitudes were higher in white/non-Hispanics vs. other racial or ethnic groups (aOR = 1.45; 95%CI: 1.06–1.99) and in older parental age (10-year-increase aOR = 1.24; 95%CI: 1.05–1.47).
Conclusion
Characteristics of middle school children's parents (e.g., sex, race or ethnicity, age) are associated with their concussion-symptom knowledge and care-seeking attitudes. Parents’ variations in concussion knowledge and attitudes warrant tailored concussion education and prevention.
Graphical abstract
1. Introduction
Approximately 1.1–1.9 million sports- and recreation-related concussions are estimated to occur annually in United States (US) among children aged ≤ 18 years.1 Although the literature base exploring concussions among this age group has grown over the past few decades, most research still draws on data from emergency department settings,1, 2, 3, 4, 5 high school sports,6, 7, 8, 9 and club and recreational leagues.6,10, 11, 12, 13, 14, 15, 16 One less examined setting is middle school (MS); in the US, MS is an intermediary level of education between elementary and secondary school that typically includes 3 to 4 grade levels (ranging from the 5th to the 9th grades) and students aged 10–15 years. Previous efforts to understand concussions among this population have used primarily injury surveillance and include findings from 1 MS in Hawaii in 1998–2008,17 9 MS football teams in Oklahoma in 1998–1999,18 and 9 MS in Virginia in 2015–2016.19 Thus, more research needs to be conducted with MS populations, specifically in the school sports setting. It is important to examine MS sports settings because school sports may include participants who better represent the general population than some youth sports leagues, where fees and extra costs may inhibit participation by those with lower socioeconomic status. Importantly, as with other populations, MS students who do not participate in sports may be at risk for concussions from non-sport-related mechanisms, such as falls and car crashes.20 Although concussion-related educational resources may be available for families of youth athletes via national organizations or their sports programs, these resources may be less accessible to those not participating in sports.
When discussing the health and safety of MS students, it is important to consider the role that parents play in the wellness of their children because parents often make crucial and primary health care decisions for their children. Parents are also often direct drivers of concussion identification and care.21 Also, previous research has noted the negative impact of parental pressure on youth athletes (e.g., less enjoyment and motivation to play).22,23 Coupled with findings that athletes may face external pressure to not disclose concussions and play through injury,24 it is important to understand factors that affect parents’ concussion knowledge and attitudes toward seeking concussion care.
Parents’ concussion knowledge and attitudes toward seeking care may be key factors in concussion management, but these factors are under-studied in MS settings. A recent systematic review found that most research examining parental knowledge of concussions examined parents of high school athletes,25 with other studies examining hospital samples26 and youth recreational and club leagues.27,28 Therefore, there is a need for concussion prevention within settings that include younger athletes, including MS settings.29 To develop appropriate prevention and management paradigms in MS settings, it is essential to first ascertain the parents’ general levels of concussion-related knowledge and attitudes. Accordingly, our study aimed to (1) describe concussion-symptom knowledge and care-seeking attitudes among parents of MS children and (2) identify factors associated with concussion-symptom knowledge and care-seeking attitudes.
2. Materials and methods
The current cross-sectional study surveyed parents of MS-aged children using an online questionnaire. The study was approved by the Institutional Review Board at The University of North Carolina at Chapel Hill. All participants provided written informed consent prior to participating in the study.
2.1. Participants and sampling
The study sample was obtained from Survey Sampling International (SSI). SSI recruits a pool of U.S. residents who have agreed to participate in online survey research. To ensure data quality, SSI uses certification processes, such as digital fingerprinting, Internet Protocol (IP) verification, and built-in quality-control questions. Upon recruitment, the participant pool provides demographic information from which SSI can identify those eligible for specific studies.
For this study, SSI surveyed only individuals who had previously self-reported being a parent of a child aged 10–15 years (the approximate age of MS students). Outside of the sampling pool, no additional exclusion criteria were used. Among this group of eligible participants, SSI randomly generated a sample who received an invitation to participate in this study. To avoid self-selection bias, specific study details were not included in the invitation. Instead, participants were invited to “take a survey”; study details were then provided upon accepting the invitation. Upon completion of the survey, SSI reimbursed participants with “reward points” that could be redeemed for cash, gift cards, or other incentives.
2.2. Data collection
The online instrument was hosted on Qualtrics and was based on a modified version of a previously validated questionnaire30,31 developed with input from parents of youth sport athletes, injury epidemiologists, athletic trainers, and other sports medicine professionals. The questionnaire included questions regarding characteristics of both the responding parents and their MS children. The questionnaire was piloted in a sample of parents of MS children and subsequently revised to ensure clarity. The finalized online questionnaire's URL was provided to SSI, which integrated it into their survey platform. In September and October 2018, 1362 randomly selected U.S. residents (aged ≥ 18 years) identifying as parents of children aged 10–15 years were invited and agreed to complete the online questionnaire. This age range aimed to ensure capture of any younger-aged legal guardians (although this study refers to participants as “parents”). Of these, 1224 (89.9%) confirmed having children currently enrolled in MS, completed all pertinent questionnaire items for this study, and were subsequently included in analyses (Table 1).
Table 1.
Descriptive profile of responding parents of middle school students (n = 1224).
| Sample characteristics | n | % |
|---|---|---|
| Sex | ||
| Male | 452 | 36.9 |
| Female | 772 | 63.1 |
| Age (year) | ||
| <30 | 133 | 10.9 |
| 30–39 | 508 | 41.5 |
| 40–49 | 367 | 30.0 |
| 50–59 | 169 | 13.8 |
| ≥60 | 47 | 3.8 |
| Race/ethnicity | ||
| White/non-Hispanic | 692 | 56.5 |
| Other racial/ethnic group | 532 | 43.5 |
| Black/African-American | 165 | 13.5 |
| Hispanic/Latino | 198 | 16.2 |
| Asian/Pacific-Islander | 90 | 7.4 |
| Mixed race/other | 79 | 6.5 |
| Highest level of education completed | ||
| Less than bachelor's degree | 643 | 52.5 |
| Less than high school | 14 | 1.1 |
| High school or GED | 229 | 18.7 |
| Some college, no degree | 243 | 19.9 |
| Associate's degree | 157 | 12.8 |
| Bachelor's degree or more | 581 | 47.5 |
| Bachelor's degree | 359 | 29.3 |
| Master's degree | 137 | 11.2 |
| Doctorate | 40 | 3.3 |
| Professional degree | 45 | 3.7 |
| Personal concussion history | ||
| No | 854 | 69.8 |
| Yes | 370 | 30.2 |
| MS child concussion history | ||
| No | 991 | 81.0 |
| Yes | 233 | 19.0 |
| MS child played organized sports within past year | ||
| No sports at all | 307 | 25.1 |
| Club sports only, including football | 25 | 2.0 |
| Club sports only, excluding football | 156 | 12.7 |
| MS sports only, including football | 32 | 2.6 |
| MS sports only, excluding football | 189 | 15.4 |
| Both sports settings, including football | 139 | 11.4 |
| Both sports settings, excluding football | 376 | 30.7 |
Note: Some categories do not meet total 100% because of rounding.Abbreviations: GED = tests of general educational development; MS = middle school.
2.3. Measures
Our outcomes of interest were concussion-symptom knowledge and concussion care-seeking attitudes. Concussion-symptom knowledge was measured by 25 items with “yes”, “no”, and “maybe” answers and gauged the parents’ recognition of concussion symptoms (Cronbach α = 0.90) (Table 2). Correct answers were scored as 2 points, “maybe” answers were scored as 1 point, and incorrect answers were scored as 0 point. The resulting scores ranged from 0 to 50 points, with higher scores indicating better knowledge. Concussion care-seeking attitudes were measured by 5 items using a 7-point Likert-type scale. These items assessed the parents’ feelings toward seeking medical care for their MS children if their children were concussed (Cronbach α = 0.90). The resulting scores ranged from 5 to 35, with higher scores indicating more favorable attitudes toward care seeking.
Table 2.
Concussion-symptom knowledge and care-seeking attitudes descriptive statistics of parents of middle school students (n = 1224).
| Concussion-symptom knowledge (options of Yes, Maybe, No)a | |||
|---|---|---|---|
| Question: Do you think the following are signs and symptoms of a concussion? | |||
| Responses, n (%) |
|||
| Yes | Maybe | No | |
| Headache | 954 (77.9) | 217 (17.7) | 53 (4.3) |
| “Pressure in the head” | 869 (71.0) | 294 (24.0) | 61 (5.0) |
| Skin rash | 123 (10.0) | 290 (23.7) | 811 (66.3) |
| Nausea or vomiting | 886 (72.4) | 252 (20.6) | 86 (7.0) |
| Dizziness | 1020 (83.3) | 143 (11.7) | 61 (5.0) |
| Blurred vision | 982 (80.2) | 181 (14.8) | 61 (5.0) |
| Balance problems | 978 (79.9) | 184 (15.0) | 62 (5.1) |
| Sensitivity to light | 748 (61.1) | 360 (29.4) | 116 (9.5) |
| Neck pain | 715 (58.4) | 423 (34.6) | 86 (7.0) |
| Joint pain | 309 (25.2) | 546 (44.6) | 369 (30.1) |
| Feeling slowed down | 725 (59.2) | 402 (32.8) | 97 (7.9) |
| Feeling like “in a fog” | 855 (69.9) | 270 (22.1) | 99 (8.1) |
| “Don't feel right” | 861 (70.3) | 283 (23.1) | 80 (6.5) |
| Difficulty concentrating | 894 (73.0) | 252 (20.6) | 78 (6.4) |
| Difficulty remembering | 911 (74.4) | 228 (18.6) | 85 (6.9) |
| Fatigue or low energy | 711 (58.1) | 391 (31.9) | 122 (10.0) |
| Confusion | 957 (78.2) | 195 (15.9) | 72 (5.9) |
| Drowsiness | 844 (69.0) | 287 (23.4) | 93 (7.6) |
| Sensitivity to noise | 635 (51.9) | 449 (36.7) | 140 (11.4) |
| Trouble falling asleep | 443 (36.2) | 513 (41.9) | 268 (21.9) |
| More emotional | 419 (34.2) | 519 (42.4) | 286 (23.4) |
| Irritability | 508 (41.5) | 500 (40.8) | 216 (17.6) |
| Sadness | 349 (28.5) | 541 (44.2) | 334 (27.3) |
| Nervous or anxious | 434 (35.5) | 519 (42.4) | 271 (22.1) |
| Teeth pain | 296 (24.2) | 581 (47.5) | 347 (28.3) |
| Concussion care-seeking attitudes (rated on a 1–7 scale, with 7 being more favorable | |||
| Question: For the following, select the number closest to each word that describes how you feel about seeking medical care for your child(ren) in middle school when he/she may have a concussion. | |||
| Mean ± SD | |||
| Irresponsible … Responsible | 6.2 ± 1.4 | ||
| Harmful … Beneficial | 6.1 ± 1.5 | ||
| Extremely difficult … Extremely easy | 5.6 ± 1.5 | ||
| Bad … Good | 6.1 ± 1.4 | ||
| Unimportant … Important | 6.3 ± 1.3 | ||
Yes = correct answer, except for “skin rash”, “joint pain”, and “teeth pain”.
Some categories do not meet total 100% because of rounding.
Our explanatory variables of interest consisted of parent and child characteristics. Parent characteristics included age (in years), sex, race/ethnicity, education level, and concussion history. We also included a competitiveness index, which has been validated in previous research.32 Competitiveness was assessed using 20 items on a 5-point scale; the items focused on “interpersonal competitiveness in every context” (α = 0.85). The resulting scores ranged from 5 to 100, with higher scores indicating a more competitive nature.
Child characteristics included concussion history and participation in organized sports within the past year. Respondents were instructed to provide characteristics only for their children currently enrolled in MS. Respondents with MS children who played sports were asked to select whether their children played MS sports or club/rec sports, or both. Parents were also asked to list, from a preselected set of sports (with a fill-in option), the sports that their children played within each sports setting. A 7-category variable was created using this information, with “No sports played” as the referent group; the remaining 6 categories were based on a combination of whether the MS children played in specific sports settings (i.e., MS sports, club/recreational leagues, or both) and whether they played football (i.e., “including football” or “excluding football”). The resulting organized sports participation variable was intended to highlight both the settings and sports in which MS children participated. Football was retained as an element within each sports category, given findings that have identified football as having a higher concussion rate than other contact sports.9,19,33
2.4. Statistical analysis
Data were analyzed using SAS (Version 9.4; SAS Institute, Cary, NC, USA). Descriptive analyses, including frequencies and measures of central tendency and variability, were conducted for all measures of interest. Next, multivariable ordinal logistic regression models identified parent and child characteristics associated with higher levels of concussion-symptom knowledge and concussion care-seeking attitudes. Given the discrete nature of knowledge vs. attitudes, a decision was made to categorize scores into 3 ordinal levels based on ∼33% increments in the overall range of each score (i.e., knowledge = 0–16, 17–33, 34–50; attitudes = 5–15, 16–25, 26–35). This was done to represent meaningful elevations in the levels of the outcomes.
In the multivariable ordinal logistic regression models, adjusted odds ratios (aORs) related to parent characteristics were computed for age (maintained as a discrete variable; with the aORs examining the effect of 10-year increases), sex (female vs. male), race/ethnicity (other racial/ethnic group vs. white/non-Hispanic), education level (with vs. without at least a bachelor's degree), concussion history (yes vs. no), and competitiveness (maintained as a discrete variable, with the aORs examining the effect of 10% increases). The levels of increase in the discrete variables (i.e., 10-year increase in age and 10% increase in competitiveness) were chosen a priori. aORs related to child characteristics were computed for concussion history (yes vs. no) and sport participation (each sports participation category compared to the referent of “No sports played”). Given the potential for clustering of participants residing within the same zip code, empirical Wald tests based on the robust sandwich covariance estimator were used to evaluate statistical significance in these models. Last, the model for concussion care-seeking attitudes included the 3-category concussion-symptom knowledge variable as a predictor.
Both models met proportional odds assumptions (p = 0.18 and p = 0.15, respectively). All aORs with 95% confidence intervals (95%CIs), excluding 1.00, were deemed statistically significant.
3. Results
Of the 1224 participating parents, most were 30–49 years of age (71.5%), female (63.1%), white/non-Hispanic (56.5%), and had less than a bachelor's degree (52.5%) (Table 1). Overall, 30.2% of parents reported that they had a concussion history, and 19.0% reported that their MS children had concussion histories. Also, 74.9% reported that their MS children had played organized sports within the past year, with 16.0% of the entire sample reporting that their MS children played football, and 42.1% reporting that their MS children played in both MS and club/recreational sports (Table 1).
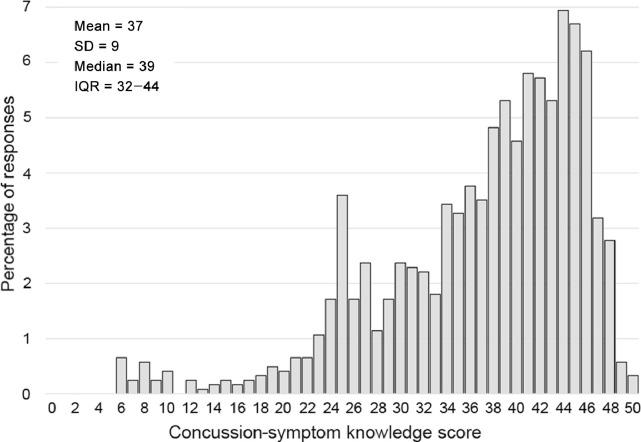
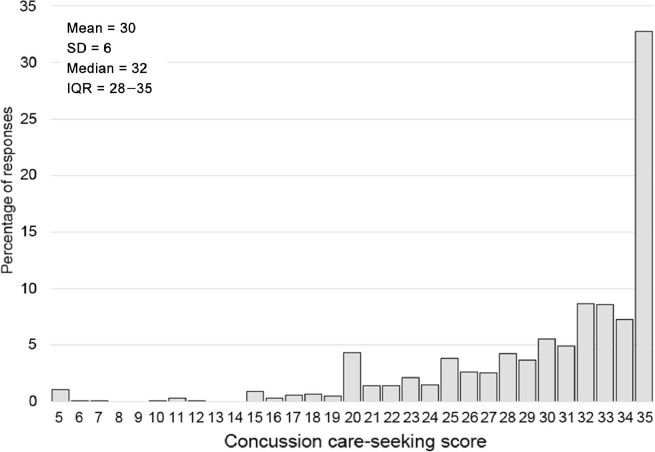
The median score for concussion-symptom knowledge was 39 (inter-quartile range (IQR): 32–44) (Fig. 1). Many parents were less familiar with emotional symptoms, including sadness (28.5% of respondents gave a “yes” response), more emotional (34.2%), and feeling nervous or anxious (35.5%) (Table 2). In addition, parents also struggled to correctly identify incorrect symptoms, such as joint pain (25.2% answered “yes” and 44.6% answered “maybe”) and teeth pain (24.2% answered “yes” and 47.5% answered “maybe”) (Table 2). The median score for concussion care-seeking attitude was 32 (IQR: 28–35) (Fig. 2). For each item in the scale, the mean scores were high, ranging from 5.6 to 6.3 (on a 7-point scale). Attitudes toward concussion care seeking along the continuum of “extremely difficult … extremely easy” were the lowest among all items (Table 2).
Fig. 1.
Distribution of scores of concussion-symptom knowledge in a sample of 1224 parents of middle school children in the US. IQR = interquartile range.
Fig. 2.
Distribution of scores of concussion care-seeking attitudes among sample of 1224 parents of middle school children in the US. IQR = interquartile range.
In the multivariable ordinal logistic regression models, various factors were found to be associated with higher levels of concussion-symptom knowledge and concussion care-seeking attitudes (Table 3). After covariate adjustment, odds of better symptom knowledge were higher among women vs. men (referent) (aOR = 2.28; 95%CI: 1.71–3.05), white/non-Hispanics vs. other racial/ethnic groups (referent) (aOR = 1.88; 95%CI: 1.42–2.49), with higher parental age (10-year-increase aOR = 1.47; 95%CI: 1.26–1.71), and higher competitiveness (10% scale-increase aOR = 1.24; 95%CI: 1.13–1.36). Also, personal concussion history was associated with higher odds of better symptom knowledge (aOR = 1.69; 95%CI: 1.25–2.29), and MS child concussion history was associated with lower odds of better symptom knowledge (aOR = 0.37; 95%CI: 0.27–0.52). Last, effect estimates indicated generally higher odds of better symptom knowledge among parents with MS children playing sports within the past year vs. those who played no sports; however, the only statistically significant finding was that parents with MS children playing non-football sports in both club/recreational leagues and MS sports had higher odds of better symptom knowledge than parents with MS children playing no sports (referent) (aOR = 1.51; 95%CI: 1.05–2.18) (Table 3).
Table 3.
Multivariable ordinal logistic regression analyses for models predicting higher levels of concussion-symptom knowledge and care-seeking attitudes among parents of middle school children.
| Variable | Odds ratio (95%CI)a |
|
|---|---|---|
| Concussion-symptom knowledge | Concussion care-seeking attitudes | |
| Age (10-year increase) | 1.47 (1.26–1.71)* | 1.24 (1.05–1.47)* |
| Sex | ||
| Male | 1.00 | 1.00 |
| Female | 2.28 (1.71–3.05)* | 1.16 (0.84–1.61) |
| Race/ethnicity | ||
| Other racial/ethnic group | 1.00 | 1.00 |
| White/non-Hispanic | 1.88 (1.42–2.49)* | 1.45 (1.06–1.99)* |
| Highest level of education completed | ||
| Less than bachelor's degree | 1.00 | 1.00 |
| Bachelor's degree or more | 0.85 (0.64–1.13) | 1.15 (0.84–1.58) |
| Personal concussion history | ||
| No | 1.00 | 1.00 |
| Yes | 1.69 (1.25–2.29)* | 1.23 (0.86–1.75) |
| Competitiveness index (10% increase) | 1.24 (1.13–1.36)* | 1.03 (0.94–1.14) |
| Concussion-symptom knowledge tier | ||
| Low (0–16) | – | 1.00 |
| Medium (17–33) | – | 2.50 (1.30–4.79)* |
| High (34–50) | – | 6.00 (3.08–11.66)* |
| MS child concussion history | ||
| No | 1.00 | 1.00 |
| Yes | 0.37 (0.27–0.52)* | 0.82 (0.55–1.24) |
| MS children sports history within past year | ||
| No sports played | 1.00 | 1.00 |
| Played club/rec leagues, including football | 1.04 (0.39–2.73) | 0.63 (0.28–1.42) |
| Played club/rec leagues, excluding football | 1.56 (0.96–2.53) | 1.84 (1.07–3.17)* |
| Played MS sports, including football | 2.18 (0.78–6.05) | 2.75 (0.80–9.44) |
| Played MS sports, excluding football | 1.26 (0.81–1.96) | 1.50 (0.95–2.38) |
| Played in both settings, including football | 1.34 (0.82–2.17) | 2.18 (1.20–3.96)* |
| Played in both settings, excluding football | 1.51 (1.05–2.18)* | 1.93 (1.27–2.94)* |
Abbreviation: CI = confidence interval.
Dependent variables were categorized into 3 ordinal levels using ∼33% increments (i.e., knowledge = 0–16, 17–33, 34–50; attitudes = 5–15, 16–25, 26–35); assumptions for proportional odds were met for both models (knowledge p = 0.18; attitudes p = 0.15).
p < 0.05, denotes statistical significance (i.e., 95%CI does not include 1.00).
After covariate adjustment, the odds of more positive care-seeking attitudes were higher for white/non-Hispanic persons vs. other racial/ethnic groups (referent) (aOR = 1.45; 95%CI: 1.06–1.99) and for older parental age (10-year-increase aOR = 1.24; 95%CI: 1.05–1.47) (Table 3). Greater concussion-symptom knowledge was also associated with higher odds of more positive care-seeking attitudes. Last, higher odds of more positive care-seeking attitudes were found among parents whose MS children played in non-football club/rec league sports (aOR = 1.84; 95%CI: 1.07–3.17), compared to those with MS children not playing sports within the past year (referent). Also, using the same referent group, higher odds of more positive care-seeking attitudes were found among parents whose MS children played in both settings, regardless of whether it included football (aOR = 2.18; 95%CI: 1.20–3.96) or excluded football (aOR = 1.93; 95%CI: 1.27–2.94) (Table 3).
4. Discussion
To our knowledge, our study is the first to consider concussion-symptom knowledge and concussion care-seeking attitudes of a national sample of parents of MS children. Although this topic has been examined in other settings,25 the need for focus on MS settings is important, given recent findings that have estimated concussion rates in MS sports to be potentially comparable to rates in high school sports.19,34 Additionally, assessing parents of MS children is important because they are typically responsible for seeking and directing medical care for their minor children. Our study found that, generally, concussion-symptom knowledge and concussion care-seeking attitudes scores among parents of MS students were high. However, we identified various deficiencies in our sample's knowledge base, and various factors were also found to be associated with higher levels of each outcome. These findings help to provide a baseline for interpreting the current state of MS parents’ understanding of concussions and may help to identify areas of need for future educational interventions that aim to improve parents’ concussion recognition and management.
4.1. Concussion-symptom knowledge and care-seeking attitudes among a national sample of MS parents
As found in previous studies with other samples of parents of youth athletes,30,35, 36, 37 concussion-symptom knowledge scores in our study were relatively high, although with some variability. Our sample struggled to identify emotional symptoms, such as sadness, being more emotional, and feeling nervous or anxious, as symptoms of concussion, a rate that is similar to previous findings for other populations.27,36,38 In our study, such difficulties with symptom recognition were made particularly evident by the large percentages of respondents who selected “maybe” as the response to each item in our concussion-symptom knowledge measure. However, a literature review by Register-Mihalik et al.39 suggested that increasing concussion knowledge among parents may not necessarily lead to parents’ being better able to identify potential concussions when they occur. Furthermore, parents may struggle, in general, to identify concussions because children may struggle to describe their symptoms or to may confuse their concussion-related symptoms with symptoms caused by other conditions such as dehydration.40,41 Thus, future research should identify education initiatives that support parents in better recognizing (and, additionally, responding to) concussions when they occur in their children.
Historically, measurements for assessing an individual's concussion-symptom knowledge have used a series of items that could be answered “yes” or “no”.27,30,37 However, these items are limited in their ability to capture the true existence of concussion-symptom knowledge because a respondent has a default 50% probability of correctly identifying a symptom. We added a “maybe” option that allowed respondents to express uncertainty. (Pilot-testing efforts examined the use of a scale-based measure that allowed for varying degrees of uncertainty; however, that measure was found to be confusing and not intuitive to our target population.) The continued development of measurements that assess concussion-symptom knowledge, allow for the expression of uncertainty, and retain simplicity are recommended.
As with our findings on concussion-symptom knowledge, our findings regarding attitudes toward concussion care seeking were similar to those of previous research;26,27 parents generally had positive attitudes toward concussion care seeking. The item in our survey with the lowest mean score pertained to the ease of seeking concussion care. Although this mean score was still generally high, it highlights the need to examine further the reasons why seeking concussion care may be difficult. Potential reasons could include a lack of understanding of the resources that are available both in the MS setting and elsewhere, particularly for those parents who may lack health care resources and health insurance. Previous research has shown that parents who lack access to affordable health care may be less likely to seek care for their children for trauma.42,43 Efforts to increase concussion knowledge among MS parents should include not only recognition of concussion-related symptoms but also how to respond to suspected concussions, including the provision of care to their children. Future efforts should focus on the importance of providing timely and affordable health care to ensure medical care for children.
To aid in concussion-prevention efforts, MS should use school nurses, who can help to educate children and their parents.44,45 It is also important to note that although a large proportion of high school student athletes have access to athletic training services,46 other youth sport settings, such as those in MS, often have very limited or no access to athletic trainers. Barriers to hiring athletic trainers at the high school level also exist at the MS level, including budget concerns and lack of community support.47 Nevertheless, the presence of on-site medical professionals is important for all injuries and not solely for concussions; school-based medical professionals can help manage safe environmental playing conditions, identify and begin immediate management of suspected injuries, and evaluate injured athletes for safe return to play.
4.2. Factors associated with concussion-symptom knowledge and care-seeking attitudes
Among our sample of MS parents, numerous factors were found to be associated with higher levels of concussion-symptom knowledge and care seeking. For both outcomes, the odds of having higher concussion-symptom knowledge and more positive concussion care-seeking attitudes were associated with older parental age and with being white/non-Hispanic vs. being from another racial/ethnic group. Additional factors were associated with concussion-symptom knowledge, including being female vs. being male and having a higher competitive nature (as measured by the competitiveness index). Similar results have been found in previous research,26,36 which also emphasizes that concussion education must consider the inherent variability within target audiences or populations. Specifically, previous research has indicated that social and equity issues exist in the use of current educational strategies and tools.48,49 These inequities may range from a lack of community resources to cultural and language barriers that prevent pro-equity considerations in interventions and result in further social disparity in outcomes.
To improve care seeking and other key aspects of concussion care for all age groups, there is a need for interventions that are data driven and that are targeted to specific subpopulations. In an effort to reach a wide range of parents and address equity considerations, concussion education must be easily accessible and modified to meet varying needs. This may include strategies such as making materials and messaging available in different languages and making them representative of various cultures and populations. However, messaging must remain accurate and consistent, particularly because previous research has found that concussion information available from websites and news articles may include incorrect statements (e.g., same-day return to play is possible with medical clearance).50,51 Additional research has also noted that parents’ perceived trustworthiness of concussion information varies by information source, with doctors or health care providers’ being considered the most trustworthy.52
Given these findings, we can highlight additional areas of focus for future research. First, although in our study we observed that parents with personal concussion histories had higher concussion-symptom knowledge compared to parents without personal concussion histories, we found that the opposite was true for parents whose MS children had concussion histories vs. the parents of children who did not. It is important that future studies investigate this surprising finding. Second, it is important to note the large percentage of parents (approximately 75%) who reported that their MS children participated in sports within the past year. In general, compared to parents of MS children who did not participate in sports in the past year, these parents were generally found to have greater concussion-symptom knowledge and more positive concussion care-seeking attitudes, although these results were not statistically significant. Such findings may be associated with the passage of state legislation in all 50 U.S. states and the District of Columbia regarding youth concussion,53 with many states including parent-education directives in their legislation. Even so, parents of children not involved in organized sports need access to concussion-related prevention education because concussions can occur from non-sport-related mechanisms, such as falls and motor vehicle crashes.20 Thus, education efforts should also acknowledge non-sport-related mechanisms.
To date, there has been a dearth of data-driven concussion education and prevention interventions in high school and youth sport settings. This may partially explain why many assessments have not indicated improvement in care-seeking outcomes. Given this situation, our study provides data that can inform future intervention development. Specifically, our study's findings indicate the need for developing varied parental educational materials and intervention messaging and strategies that are culturally relevant and that consider potential gender, racial/ethnic, and personal experience with concussion. The development of videos, images, and specific messaging strategies should include adequate representation of different genders, racial/ethnic groups, and concussion experiences.
4.3. Limitations
Our findings may not be generalizable to the parents of all MS athletes or to the parents of any individual youth athlete, although some of these concerns might be partially mitigated by the nationwide sampling pool that SSI used to recruit participants for this study. It is also important to note that inferences regarding our constructs of knowledge and attitudes should be restricted to concussion-symptom knowledge and care-seeking attitudes. Also, our analyses were unable to account for additional parental, child, and community-level factors, including parent occupation, parent insurance status, concussion histories of older and younger siblings of the MS children, the presence of sports medicine staff at the children's sport settings, or the rural or urban character of the community. Finally, concerns about statistical power inhibited our ability to conduct multivariable modeling with more specific categories for variables, such as race or ethnicity. Although it is difficult for a single study to account for all factors potentially associated with the outcomes, future studies should consider additional factors when examining concussion-related knowledge and attitudes.
5. Conclusion
Generally, concussion-symptom knowledge and concussion care-seeking attitude scores were relatively high (as assessed by our measurement tools) in our sample of parents of MS students. However, some parents were unsure of a number of concussion symptoms. Coupled with the multitude of factors associated with our outcomes, our findings highlight the need for concussion-related education that considers the diversity of the MS parent population. Further investigation into educational messaging and delivery methods may help to ensure that concussion-related education and prevention materials for parents of MS children are credible, culturally relevant, and inclusive of both sport and non-sport mechanisms.
Acknowledgments
Acknowledgments
The authors thank the research participants for their participating in the study. Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. This work was funded by a grant from the Division of Unintentional Injury, Centers for Disease Control and Prevention (5U01CE002885-02). The University of North Carolina Injury Prevention Research Center is also partly supported by an Injury Control Research Center award (R49/CE002479) from the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. There are no other financial relationships relevant to the development of this article.
Authors’ contributions
ZYK conceived the study, led its design and coordination, and led the drafting of the manuscript; JKRM assisted in the conception of the study, led its design and coordination, and assisted in the drafting of the manuscript; AKN, MCK, AC, PG, and KHB assisted in the conception of the study, assisted in its design, and helped draft the manuscript; JKHK assisted in the design of the study and helped draft the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Appendix. Supplementary materials
References
- 1.Bryan MA, Rowhani-Rahbar A, Comstock RD, Rivara F, Seattle Sports Concussion Research Collaborative Sports-and recreation-related concussions in US youth. Pediatrics. 2016;138 doi: 10.1542/peds.2015-4635. [DOI] [PubMed] [Google Scholar]
- 2.Bakhos LL, Lockhart GR, Myers R, Linakis JG. Emergency department visits for concussion in young child athletes. Pediatrics. 2010;126:e550–e556. doi: 10.1542/peds.2009-3101. [DOI] [PubMed] [Google Scholar]
- 3.Jacobson NA, Buzas D, Morawa LG. Concussions from youth football results from NEISS hospitals over an 11-year time frame, 2002–2012. Orthop J Sports Med. 2013;1 doi: 10.1177/2325967113517860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coronado VG, Haileyesus T, Cheng TA. Trends in sports-and recreation-related traumatic brain injuries treated in US emergency departments: the National Electronic Injury Surveillance System-All InjuryProgram (NEISS-AIP) 2001–2012. J Head Trauma Rehabil. 2015;30:185–197. doi: 10.1097/HTR.0000000000000156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buzas D, Jacobson NA, Morawa LG. Concussions from 9 youth organized sports results from NEISS hospitals over an 11-year time frame, 2002–2012. Orthop J Sports Med. 2014;2 doi: 10.1177/2325967114528460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dompier TP, Kerr ZY, Marshall SW. Incidence of concussion during practice and games in youth, high school, and collegiate American football players. JAMA Pediatr. 2015;169:659–665. doi: 10.1001/jamapediatrics.2015.0210. [DOI] [PubMed] [Google Scholar]
- 7.Lincoln AE, Caswell SV, Almquist JL, Dunn RE, Norris JB, Hinton RY. Trends in concussion incidence in high school sports: a prospective 11-year study. Am J Sports Med. 2011;39:958–963. doi: 10.1177/0363546510392326. [DOI] [PubMed] [Google Scholar]
- 8.Powell JW, Barber-Foss KD. Traumatic brain injury in high school athletes. JAMA. 1999;282:958–963. doi: 10.1001/jama.282.10.958. [DOI] [PubMed] [Google Scholar]
- 9.Kerr ZY, Chandran A, Nedimyer AK, Arakkal A, Pierpoint LA, Zuckerman SL. Concussion incidence and trends in 20 high school sports. Pediatrics. 2019;144 doi: 10.1542/peds.2019-2180. [DOI] [PubMed] [Google Scholar]
- 10.Kerr ZY, Yeargin SW, Valovich McLeod TC. Comprehensive coach education and practice contact restriction guidelines result in lower injury rates in youth American football. Orthop J Sports Med. 2015;3 doi: 10.1177/2325967115594578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kerr ZY, Marshall SW, Simon JE. Injury rates in age-only versus age-and-weight playing standard conditions in American youth football. Orthop J Sports Med. 2015;3 doi: 10.1177/2325967115603979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pfister T, Pfister K, Hagel B, Ghali WA, Ronksley PE. The incidence of concussion in youth sports: a systematic review and meta-analysis. Br J Sports Med. 2016;50:292–297. doi: 10.1136/bjsports-2015-094978. [DOI] [PubMed] [Google Scholar]
- 13.Kerr ZY, Lincoln AE, Dodge T. Epidemiology of youth boys' and girls' lacrosse injuries in the 2015 to 2016 seasons. Med Sci Sports Exerc. 2018;50:284–291. doi: 10.1249/MSS.0000000000001422. [DOI] [PubMed] [Google Scholar]
- 14.Kontos AP, Elbin RJ, Fazio-Sumrock VC. Incidence of sports-related concussion among youth football players aged 8–12 years. J Pediatr. 2013;163:717–720. doi: 10.1016/j.jpeds.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 15.Kontos AP, Elbin R, Sufrinko A. Incidence of concussion in youth ice hockey players. Pediatrics. 2016;137 doi: 10.1542/peds.2015-1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Kane JW, Spieker A, Levy MR, Neradilek M, Polissar NL, Schiff MA. Concussion among female middle-school soccer players. JAMA Pediatr. 2014;168:258–264. doi: 10.1001/jamapediatrics.2013.4518. [DOI] [PubMed] [Google Scholar]
- 17.Beachy G, Rauh M. Middle school injuries: a 20-year (1988–2008) multisport evaluation. J Athl Train. 2014;49:493–506. doi: 10.4085/1062-6050-49.2.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Turbeville SD, Cowan LD, Asal NR, Owen WL, Anderson MA. Risk factors for injury in middle school football players. Am J Sports Med. 2003;31:276–281. doi: 10.1177/03635465030310022001. [DOI] [PubMed] [Google Scholar]
- 19.Kerr ZY, Cortes N, Caswell AM. Concussion rates in U.S. middle school athletes, 2015–2016 school year. Am J Prev Med. 2017;53:914–918. doi: 10.1016/j.amepre.2017.05.017. [DOI] [PubMed] [Google Scholar]
- 20.Haarbauer-Krupa J, Arbogast KB, Metzger KB. Variations in mechanisms of injury for children with concussion. J Pediatr. 2018;197:e241–e248. doi: 10.1016/j.jpeds.2018.01.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wahlin T, Deane F. Discrepancies between parent-and adolescent-perceived problem severity and influences on help seeking from mental health services. Aust N Z J Psychiatry. 2012;46:553–560. doi: 10.1177/0004867412441929. [DOI] [PubMed] [Google Scholar]
- 22.Knight CJ, Dorsch TE, Osai KV, Haderlie KL, Sellars PA. Influences on parental involvement in youth sport. Sport Exerc Perfor Psychol. 2016;5:161. doi: 10.1037/spy0000053. [DOI] [Google Scholar]
- 23.Sánchez-Miguel PA, Leo FM, Sánchez-Oliva D, Amado D, García-Calvo T. The importance of parents’ behavior in their children's enjoyment and amotivation in sports. J Hum Kinet. 2013;36:169–177. doi: 10.2478/hukin-2013-0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kerr ZY, Register-Mihalik JK, Marshall SW, Evenson KR, Mihalik JP, Guskiewicz KM. Disclosure and non-disclosure of concussion and concussion symptoms in athletes: review and application of the socio-ecological framework. Brain Inj. 2014;28:1009–1021. doi: 10.3109/02699052.2014.904049. [DOI] [PubMed] [Google Scholar]
- 25.Feiss RS, Lutz M, Moody JR, Pangelinan MM. A systematic review of coach and parent knowledge of concussion. J Concussion. 2020 doi: 10.1177/2059700219900053. [DOI] [Google Scholar]
- 26.Lin AC, Salzman GA, Bachman SL. Assessment of parental knowledge and attitudes toward pediatric sports-related concussions. Sports Health. 2015;7:124–129. doi: 10.1177/1941738115571570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kay MC, Register-Mihalik JK, Ford CB, Williams RM, Valovich McLeod TC. Parents’ and child's concussion history as predictors of parental attitudes and knowledge of concussion recognition and response. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117742370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rieger B, Lewandowski L, Potts H, Potter K, Chin LS. Parent knowledge and perceptions of concussion related to youth football. Cureus. 2018;10:e2268. doi: 10.7759/cureus.2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kerr ZY, Register-Mihalik JK, Haarbauer-Krupa J. Using opinion leaders to address intervention gaps in concussion prevention in youth sports: key concepts and foundational theory. Inj Epidemiol. 2018;5:28. doi: 10.1186/s40621-018-0158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Register-Mihalik JK, Guskiewicz KM, Valovich McLeod TC, Linnan LA, Mueller FO, Marshall SW. Knowledge, attitude, and concussion-reporting behaviors among high school athletes: a preliminary study. J Athl Train. 2013;48:645–653. doi: 10.4085/1062-6050-48.3.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Register-Mihalik JK, Williams RM, Marshall SW. Demographic, parental, and personal factors and youth athletes' concussion-related knowledge and beliefs. J Athl Train. 2018;53:768–775. doi: 10.4085/1062-6050-223-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smither RD, Houston JM. The nature of competitiveness: the development and validation of the competitiveness index. Educ Psychol Meas. 1992;52:407–418. [Google Scholar]
- 33.Marar M, McIlvain NM, Fields SK, Comstock RD. Epidemiology of concussions among United States high school athletes in 20 sports. Am J Sports Med. 2012;40:747–755. doi: 10.1177/0363546511435626. [DOI] [PubMed] [Google Scholar]
- 34.Kerr ZY, Cortes N, Ambegaonkar JP. The epidemiology of injuries in middle school football, 2015-2017: the Advancing Healthcare Initiatives for Underserved Students project. Am J Sports Med. 2019;47:933–941. doi: 10.1177/0363546518825361. [DOI] [PubMed] [Google Scholar]
- 35.Kim S, Connaughton DP, Leeman RF, Lee JH. Concussion knowledge of youth sport athletes, coaches, and parents: a review. J Amateur Sport. 2018;4:82–107. [Google Scholar]
- 36.Cusimano MD, Zhang S, Topolovec-Vranic J, Hutchison MG, Jing R. Factors affecting the concussion knowledge of athletes, parents, coaches, and medical professionals. SAGE Open Med. 2017;5 doi: 10.1177/2050312117694794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wallace J, Covassin T, Nogle S, Gould D, Kovan J. Concussion knowledge and reporting behavior differences between high school athletes at urban and suburban high schools. J Sch Health. 2017;87:665–674. doi: 10.1111/josh.12543. [DOI] [PubMed] [Google Scholar]
- 38.Mannings C, Kalynych C, Joseph MM, Smotherman C, Kraemer DF. Knowledge assessment of sports-related concussion among parents of children aged 5 years to 15 years enrolled in recreational tackle football. J Trauma Acute Care Surg. 2014;77(Suppl. 1):S18–S22. doi: 10.1097/TA.0000000000000371. [DOI] [PubMed] [Google Scholar]
- 39.Register-Mihalik J, Baugh C, Kroshus E, Kerr Z, Valovich McLeod TC. A multifactorial approach to sport-related concussion prevention and education: application of the socioecological framework. J Athl Train. 2017;52:195–205. doi: 10.4085/1062-6050-51.12.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patel AV, Mihalik JP, Notebaert AJ, Guskiewicz KM, Prentice WE. Neuropsychological performance, postural stability, and symptoms after dehydration. J Athl Train. 2007;42:66–75. [PMC free article] [PubMed] [Google Scholar]
- 41.Chrisman SP, Quitiquit C, Rivara FP. Qualitative study of barriers to concussive symptom reporting in high school athletics. J Adolesc Health. 2013;52:330–335. doi: 10.1016/j.jadohealth.2012.10.271. [DOI] [PubMed] [Google Scholar]
- 42.Overpeck MD, Kotch JB. The effect of US children's access to care on medical attention for injuries. Am J Pub Health. 1995;85:402–404. doi: 10.2105/ajph.85.3.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lohr KN, Brook RH, Kamberg CJ. Use of medical care in the RAND Health Insurance Experiment: diagnosis-and service-specific analyses in a randomized controlled trial. Med Care. 1986;24(Suppl. 9):S1–87. [PubMed] [Google Scholar]
- 44.Diaz AL, Wyckoff LJ. NASN position statement: concussions–the role of the school nurse. NASN Sch Nurse. 2013;28:110–111. doi: 10.1177/1942602X12473949. [DOI] [PubMed] [Google Scholar]
- 45.Welch Bacon CE, Erickson CD, Kay MC, Weber ML, Valovich McLeod TC. School nurses’ perceptions and experiences with an interprofessional concussion management team in the secondary school setting. J Interprof Care. 2017;31:725–733. doi: 10.1080/13561820.2017.1345873. [DOI] [PubMed] [Google Scholar]
- 46.Pryor RR, Casa DJ, Vandermark LW. Athletic training services in public secondary schools: a benchmark study. J Athl Train. 2015;50:156–162. doi: 10.4085/1062-6050-50.2.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mazerolle SM, Raso SR, Pagnotta KD, Stearns RL, Casa DJ. Athletic directors' barriers to hiring athletic trainers in high schools. J Athl Train. 2015;50:1059–1068. doi: 10.4085/1062-6050-50.10.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kroshus E, Kerr ZY, Lee JG. Community-level inequalities in concussion education of youth football coaches. Am J Prev Med. 2017;52:476–482. doi: 10.1016/j.amepre.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 49.Kroshus E, Gonzalez LA, Chrisman SP, Jimenez N. Availability of concussion information in Spanish for parents of youth athletes. Health Promot Pract. 2019;20:372–380. doi: 10.1177/1524839918790231. [DOI] [PubMed] [Google Scholar]
- 50.Ahmed OH, Sullivan SJ, Schneiders AG, McCrory PR. Concussion information online: evaluation of information quality, content and readability of concussion-related websites. Br J Sports Med. 2012;46:675–683. doi: 10.1136/bjsm.2010.081620. [DOI] [PubMed] [Google Scholar]
- 51.Ahmed OH, Hall EE. “It was only a mild concussion”: exploring the description of sports concussion in online news articles. Phys Ther Sport. 2017;23:7–13. doi: 10.1016/j.ptsp.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 52.Kerr ZY, Chandran A, Nedimyer AK. Use of sport-related concussion information sources among parents of United States middle school children. J Sport Health Sci. 2020 doi: 10.1016/j.jshs.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yang J, Comstock RD, Yi H, Harvey HH, Xun P. New and recurrent concussions in high-school athletes before and after traumatic brain injury laws, 2005–2016. Am J Pub Health. 2017;107:1916–1922. doi: 10.2105/AJPH.2017.304056. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.