Highlights
-
•
First study that directly compared Tai Ji Quan trials published in English and Chinese with meta-regression analysis in the largest sample to date
-
•
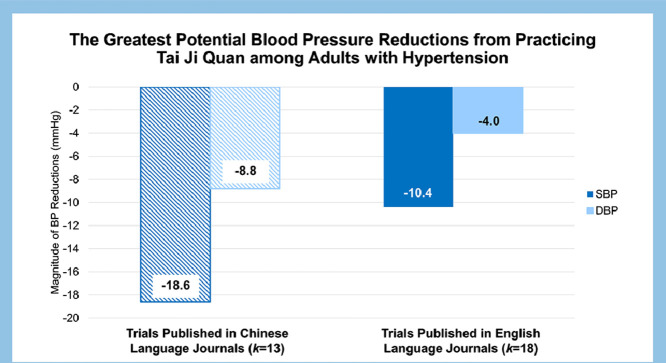
In trials published in English, Tai Ji Quan reduces systolic blood pressure by 10 mm Hg and diastolic blood pressure 4 mm Hg among adults with hypertension
-
•
In trials published in Chinese, Tai Ji Quan reduces systolic pressure by 19 mm Hg and diastolic pressure by 9 mm Hg among adults with hypertension
-
•
More confidence should be placed in Tai Ji Quan trials published in English due to their higher methodological quality compared to trials published in Chinese
Keywords: Blood pressure, Complementary medicine, Exercise training, Hypertension
Abstract
Background
Professional health organizations are not currently recommending Tai Ji Quan alongside aerobic exercise to treat hypertension. We aimed to examine the efficacy of Tai Ji Quan as antihypertensive lifestyle therapy.
Methods
Tai Ji Quan interventions published in English and Chinese were included when they involved healthy adults, reported pre- and post-intervention blood pressure (BP), and had a non-exercise/non-diet control group. We systematically searched 11 electronic databases for studies published through July 31, 2018, yielding 31 qualifying controlled trials. We (1) evaluated the risk of bias and methodological study quality, (2) performed meta-regression analyses following random-effects assumptions, and (3) generated additive models representing the largest possible clinically relevant BP reductions.
Results
Participants (n = 3223) were middle-aged (56.6 ± 15.1 years of age, mean ± SD) adults with prehypertension (systolic BP (SBP) = 136.9 ± 15.2 mmHg, diastolic BP (DBP) = 83.4 ± 8.7 mmHg). Tai Ji Quan was practiced 4.0 ± 1.4 sessions/week for 54.0 ± 10.6 min/session for 22.3 ± 20.2 weeks. Overall, Tai Ji Quan elicited significant reductions in SBP (–11.3 mmHg, 95%CI: –14.6 to –8.0; d+ = –0.75) and DBP (–4.8 mmHg, 95%CI: –6.4 to –3.1; d+ = –0.53) vs. control (p < 0.001). Controlling for publication bias among samples with hypertension, Tai Ji Quan trials published in English elicited SBP reductions of 10.4 mmHg and DBP reductions of 4.0 mmHg, which was half the magnitude of trials published in Chinese (SBP reductions of 18.6 mmHg and DBP reductions of 8.8 mmHg).
Conclusion
Our results indicate that Tai Ji Quan is a viable antihypertensive lifestyle therapy that produces clinically meaningful BP reductions (i.e., 10.4 mmHg and 4.0 mmHg of SBP and DBP reductions, respectively) among individuals with hypertension. Such magnitude of BP reductions can lower the incidence of cardiovascular disease by up to 40%.
Graphical Abstract
1. Introduction
Hypertension is the most common cardiovascular disease risk factor, affecting nearly 50% of adults in the United States according to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guidelines.1 The ACC/AHA recommends aerobic exercise as antihypertensive lifestyle therapy because it lowers blood pressure (BP) by 5–8 mmHg.1,2 Accordingly, adults with hypertension are encouraged to engage in moderate-to-vigorous intensity aerobic exercise on most, and preferably all, days of the week.1 Unfortunately, most adults (72%) with hypertension do not adhere to these exercise recommendations for hypertension.3
Tai Ji Quan is a safe, low-impact, enjoyable, and inexpensive form of exercise accessible to individuals who for various reasons can not or choose not to engage in aerobic exercise.4, 5, 6 Tai Ji Quan is a form of mind–body exercise that employs rhythmic physical motions while emphasizing relaxation and breathing techniques. Tai Ji Quan has numerous health benefits, with BP being one of the top health outcomes found in the literature.4,7,8 In fact, Tai Ji Quan has been reported to elicit systolic BP (SBP) reductions as large as 17–19 mmHg and diastolic BP (DBP) reductions as large as 11–13 mmHg in primary-level Tai Ji Quan intervention studies published in English and Chinese.9, 10, 11 Yet, due to limited evidence, professional committees and organizations such as the 2018 Physical Activity Guidelines Advisory Committee and ACC/AHA are not currently recommending Tai Ji Quan as antihypertensive lifestyle therapy alongside aerobic exercise, which is regarded as the standard of care.1,12,13
Three prior meta-analyses published in English have quantified the BP-lowering effects of Tai Ji Quan. Two of these meta-analyses reported clinically meaningful unstandardized mean effect sizes of –12.4 mmHg to –15.2 mmHg for SBP and –4.1 mmHg to –6.0 mmHg for DBP,14,15 while the 3rd meta-analysis reported medium-to-large standardized mean effect sizes of –0.93 for SBP and –0.54 for DBP.16 Despite these encouraging findings, these meta-analyses had the following limitations: (1) two of the 3 meta-analyses combined samples having various BP status, rendering it impossible to distinguish among adults who had normal BP from those who had hypertension;15,16 (2) all meta-analyses had small sample sizes (k = 9–12; n = 536–832) and only included Tai Ji Quan intervention studies published in 2014 and before; and (3) all 3 meta-analyses did not disclose the statistical procedures used for the effect-size calculations as required by contemporary standards for systematic reviews and meta-analyses.17 Furthermore, despite high heterogeneity (I2 ranged from 74% to 90% for the 2 meta-analyses that gauged it15,16), moderator analyses were not performed to investigate if any study (e.g., trial location), sample (e.g., baseline BP status), or Tai Ji Quan intervention (e.g., frequency) characteristics influenced the BP response to Tai Ji Quan.14, 15, 16
To address the limitations in the literature, we conducted the largest meta-analysis to date to examine the efficacy of Tai Ji Quan as antihypertensive lifestyle therapy, while examining moderators of the BP response to Tai Ji Quan with meta-regression analysis, a contemporary statistical technique that can examine multiple moderators simultaneously.18, 19, 20, 21 In addition, we investigated which combination of study, sample, and Tai Ji Quan intervention characteristics generated the largest possible BP reductions with additive regression models to provide insights into the clinical utility of Tai Ji Quan as antihypertensive lifestyle therapy.
2. Methods
2.1. Selection criteria
The systematic review and meta-analytic procedures are registered at PROSPERO (registration number: CRD42019124262) and were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses Statement.22 According to 5 a priori inclusion criteria, trials were eligible if they: (1) enrolled adults ≥18 years of age who were healthy other than their BP status, (2) explicitly stated that the intervention was Tai Ji Quan, (3) included a non-exercise/non-diet control group, (4) reported BP pre- and post-intervention for the Tai Ji Quan and control groups, and (5) were peer-reviewed articles published in either English- or Chinese-language journals. Trials were excluded if they (1) included samples with chronic disease (e.g., cardiovascular disease, diabetes mellitus, cancer); (2) prescribed drug/supplements, dietary interventions, or another type of exercise in addition to Tai Ji Quan; or (3) involved a single Tai Ji Quan session (i.e., an acute intervention).
2.2. Search strategy
Aided by a medical librarian (JL), we systematically searched 6 electronic databases in English and 5 electronic databases in Chinese from their inception until July 31, 2018 (Supplementary Table 1, Full search strategy, for each of the electronic databases queried). The team screened potential reports in duplicate by trained coders (YW, SC, and YC), first by title and abstract and then by full text. The team also searched for additional reports in reference lists of included trials, and reference lists of relevant reviews and meta-analyses.
2.3. Data extraction and coded variables
Data were extracted using our standardized coding form and coder manual23,24 adapted according to a previously published scale. This scale was specially designed to evaluate the frequency, intensity, and time principle of exercise prescription and instructional methods (e.g., breathing techniques, credentials of the instructors) of Tai Ji Quan interventions aimed at improving balance for older adults.25
We coded the study characteristics (e.g., trial location, publishing language), sample characteristics (e.g., baseline BP, body mass index), and Tai Ji Quan intervention characteristics (i.e., the frequency, intensity, and time exercise prescription and instructional methods). In addition, we coded BP measurement methods, such as BP measurement equipment and body position during measurement. Notably, we extracted information regarding the time between the last session of Tai Ji Quan and the post-intervention BP measurement, which may suggest the existence of the acute BP effects of the last session of exercise (i.e., postexercise hypotension21,26) and/or detraining since the BP benefits of exercise dissipate rapidly upon the cessation of training.27 In our meta-analysis, we followed the Seventh Report of the Joint National Committee BP definitions of hypertension, prehypertension, and normal BP because the majority of research in this literature was conducted before release of the 2017 ACC/AHA Guidelines. Methodological study quality was assessed using an augmented version of the Downs and Black checklist (27 items) and was scored as the percentage of items satisfied out of a possible 32-point total.28 Overall methodological study quality scores were grouped into low (≤16 points, <50%), moderate (>16 to 25 points, 50%–79%), or high (>25 points, ≥80%).29,30 We used the Revised Cochrane Risk-of-Bias Tool for Randomized Trials (RoB 2.0)31 to assess risk of bias from domains including the randomization process, deviation from intended interventions, missing outcome data, measurement of outcomes, and selection of reported results for randomized controlled trials (RCTs). In addition, we used the Risk of Bias in Non-Randomized Studies of Interventions (ROBINS-I)32 to assess risk of bias from domains, including the confounding, selection of participants, intervention classification, deviation from intended interventions, missing outcome data, measurement of outcomes, and selection of reported results for non-RCTs (NRCTs).
All data extraction and assessments of methodological study quality and risk of bias of included Tai Ji Quan interventions were conducted by 3 trained coders (YW, SC, and YC) independently and a high reliability was achieved (mean Cohen's κ = 0.87 and Pearson's r = 0.88). All disagreements were resolved through discussion.
2.4. Outcome and effect size calculations
The main outcome of the current meta-analysis is the BP response to Tai Ji Quan, defined as the difference between the change of BP in the Tai Ji Quan group and in the control group. The BP response to Tai Ji Quan was quantified as the standardized mean difference effect size (d) by calculating the mean difference in resting SBP or DBP between the Tai Ji Quan group and the control group post- vs. pre-intervention, divided by the pooled standard deviation (SD), correcting for small sample size bias and baseline differences between the groups.33,34 When trials measured resting BP at multiple time points, we treated the BP value taken at the time point before and at the closest to the onset of the Tai Ji Quan intervention as the pre-intervention value, and the BP value taken at the time point after and closest to the end of the Tai Ji Quan intervention as the post-intervention value. Because we observed a large variation in the distribution of baseline SBP (the SD ranged from 3.3 to 25.3)35,36 and DBP (the SD ranged from 3.6 to 17.1)11,37 across the included trials, we chose to use standardized effect sizes, which are more robust, less biased, and have better efficiency compared to unstandardized effect sizes across many statistical circumstances.38 Negative d values indicate that Tai Ji Quan reduced BP more post- vs. pre-intervention compared to the control group. When reaching statistical significance (p < 0.05), d values were interpreted as insufficient (0 to –0.19), small (–0.20 to –0.49), medium (–0.50 to –0.79), and large (≤–0.80) BP reductions.39 Inconsistencies in d values were assessed with the Q statistic, which we transformed into the I2 statistic and its 95% confidence intervals (95%CIs).40,41 I2 values range from low heterogeneity (0%) to high heterogeneity (100%).
2.5. Moderator analyses
We examined characteristics related to the study, sample, and Tai Ji Quan interventions as moderators of the BP response to Tai Ji Quan. Weighted regression models with maximum likelihood estimation of the random-effects weights (i.e., the inverse of the variance for each d) was used to explain variability in d values for SBP and DBP. In multiple-moderator models, we examined significant or trending moderators (p ≤ 0.10) from bivariate meta-regression analyses42 in conjunction with the model coefficients and R2 values (i.e., between-study variance explained by a covariate) to determine the influence of individual moderators on the BP response to Tai Ji Quan.43 The moving constant technique44 estimated the magnitude of the weighted mean effect size (d+) and its 95%CI at different levels of interest for individual moderators while statistically controlling for the presence of other moderators held constant at their mean levels; the results are estimated, or predicted d+ values, denoted as .44
For SBP and DBP, additive regression models were generated from the final multiple-moderator models that represented the greatest potential antihypertensive benefit from Tai Ji Quan. Individual moderators were assessed within the same model at the level that yielded the greatest BP reduction (i.e., and 95%CI). To facilitate clinical interpretation for each moderator dimension and level of interest, we back-converted the standardized estimate (i.e., ) into mmHg of BP change by multiplying the by the SD of baseline SBP (i.e., 15) and the SD of baseline DBP (i.e., 9) calculated on the combined sample from all included Tai Ji Quan trials.24
2.6. Publication bias
We evaluated the potential for publication or other reporting biases in both SBP and DBP d values by (1) visually examining the distribution and asymmetry of funnel plots45 and (2) using the tests of Begg and Mazumdar46 and Egger et al.47 tests, in addition to performing the Precision-Effect Test and Precision-Effect Estimate with standard error (SE) analysis to determine if potential publication bias needed to be controlled by including the SE of the BP response to Tai Ji Quan in the multiple-moderator models for SBP and DBP.48
2.7. Sensitivity analyses
Notably, we did not restrict our sample to RCTs, and, in fact, there were more NRCTs (51.6%, k = 16) than RCTs (48.4%, k = 15). Accordingly, we performed sensitivity analyses to compare the d values from RCTs and NRCTs.49 There was no difference between the mean effect sizes of RCTs and NRCTs for SBP (p > 0.35) or DBP (p > 0.35), affirming the decision to combine RCTs and NRCTs for analyses. In addition, we paired study design with other variables included in the final multiple-moderator models and examined them as competing moderators of the BP response to Tai Ji Quan. Study design was the weaker, non-significant moderator when examined in tandem with the baseline SBP (p = 0.72), publishing language (p = 0.16), or the SE of the SBP response to Tai Ji Quan (p = 0.31) in the SBP multiple-moderator model. It was also the weaker, non-significant moderator when examined in tandem with baseline DBP (p = 0.59) or publishing language (p = 0.42) in the DBP multiple-moderator model. These results reinforced our decision to combine RCTs and NRCTs in our final analyses.
2.8. Statistical computing
Analyses were performed using Stata Version 14.1 (Stata Corp., College Station, TX, USA) with macros for meta-analysis42,50 and incorporated random-effects assumptions. Stata commands appear in Supplementary Table 2 (Stata commands). Descriptive statistics are reported as mean ± SD unless stated otherwise. Two-sided significance level was p < 0.05.
3. Results
3.1. Study search and study characteristics
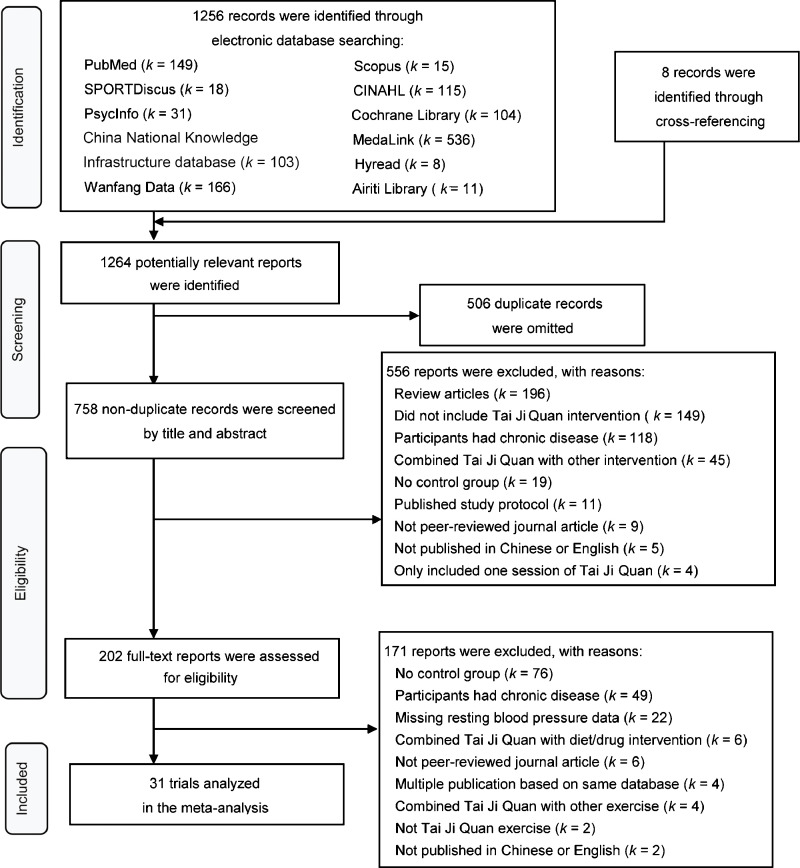
We identified 31 controlled Tai Ji Quan trials that satisfied the inclusion criteria (Fig. 1). A list of included trials is available in Supplementary Table 3 (Reference list of included Tai Ji Quan trials).
Fig. 1.
Flow chart detailing the systematic search of potential reports and selection process of included Tai Ji Quan trials.
The included Tai Ji Quan trials were published between 1997 and 2018 in English (k = 18, 58.1%) and Chinese (k = 13, 41.9%) language journals and each enrolled between 20 and 300 (n = 104 ± 74, mean ± SD) participants. Trials were RCTs (k = 15, 48.4%) or NRCTs (k = 16, 51.6%), and most examined BP as the primary outcome (k = 24, 77.4%). The attrition rate was reported or can be calculated for 18 of the Tai Ji Quan interventions (58.1%). On average, the attrition rate was 16.8% ± 8.8% (Supplementary Table 4, Study and Tai Ji Quan intervention characteristics). Among included Tai Ji Quan interventions, 24 interventions (77.4%) disclosed the content of the control groups (Supplementary Table 4), including routine daily activities (k = 14, 45.2%), usual care (k = 4, 12.9%), and attention control (k = 6, 19.4%) such as educational lectures. The remaining 7 (22.6%) interventions did not disclose the content of the control groups. On average, the included Tai Ji Quan trials achieved “moderate” methodological study quality on the augmented Downs and Black Checklist (50.1% ± 16.3%),27 despite widely varying scores (25.8%–87.1%). The risk-of-bias ratings for individual trials appear in Supplementary Table 5 (Risk of bias of RCTs) and Supplementary Table 6 (Risk of bias of NRCTs), respectively. The majority of the RCTs (k = 12, 80%) exhibited high levels of risk of bias based on RoB 2.0.31 In particular, deviation from intended interventions was the domain with the highest percentage of trials that were rated as high risk of bias (k = 11, 73.3%). In parallel, the majority of the NRCTs (k = 11, 68.8%) exhibited serious risk of bias based on ROBINS-I.32 In particular, confounding was the domain with the highest percentage of trials that were rated as serious risk of bias (k = 10, 62.5%); meanwhile, deviation from intended interventions was the domain with the highest percentage of trials that did not provide enough information for judgments to be made (k = 11, 68.8%).
3.2. Sample characteristics
Baseline sample characteristics were similar between the Tai Ji Quan (n = 1654) and control (n = 1569) groups (p > 0.05) (Supplementary Table 7, Baseline sample characteristics). On average, participants (n = 3223) were middle-aged (56.6 ± 15.1 years) adults with prehypertension (SBP = 136.9 ± 15.2 mmHg/DBP = 83.4 ± 8.7 mmHg) and were predominantly women (69.5% ± 21.6%). Among the included samples, based on baseline BP values and use of BP medications,51 16 trials (51.6%) involved samples (n = 1750) with hypertension (SBP = 148.4 ± 8.9 mmHg/DBP = 88.3 ± 8.3 mmHg). Meanwhile, 10 trials (32.3%) involved samples (n = 854) with prehypertension (SBP = 130.4 ± 5.6 mmHg/DBP = 80.9 ± 3.6 mmHg), and 5 trials (16.1%) involved samples (n = 619) with normal BP (SBP = 113.2 ± 5.4 mmHg/DBP = 72.5 ± 3.9 mmHg). A total of 8 trials (25.8%) provided information regarding medication use. Of these, 5 trials reported that no participants were taking BP medications, while all participants had hypertension.37,52, 53, 54, 55 Just 2 trials disclosed the percentage of participants who were taking specific categories of BP medications, with calcium channel blockers being the most popular (i.e., 52%–55%).56,57 In addition, 1 trial reported that all of its participants had dyslipidemia and were taking statins.58
3.3. Tai Ji Quan intervention characteristics
Table 1 provides the details of the Tai Ji Quan intervention characteristics. Tai Ji Quan was practiced, on average, 4.0 ± 1.4 sessions/week for 54.0 ± 10.6 min/session for 22.3 ± 20.2 weeks. Tai Ji Quan interventions included, on average, 30.4 ± 25.4 forms following Yang (k = 15, 48.4%), Chen (k = 1, 3.2%),52 or undisclosed (k = 15, 48.4%) styles; however, less than one-third of the trials disclosed the names of the Tai Ji Quan forms (k = 8, 25.8%) or adopted progression methods (Table 1) to facilitate the learning of Tai Ji Quan practice (k = 10, 32.3%). Few trials reported emphasis on the 3 fundamental elements of Tai Ji Quan practice, including movement principles (k = 4, 12.9%), breathing techniques (k = 6, 19.4%), or relaxation (k = 3, 9.7%). Only 1 trial (3.2%) reported that all 3 elements were emphasized.37
Table 1.
Tai Ji Quan intervention characteristics.
| Methods | k | Mean ± SD (range) | Reporting rate (%)a |
|---|---|---|---|
| Ex Rx methods items | |||
| Frequency (sessions/week) | 31 | 4.0 ± 1.4 (2.0–7.0) | 100.0 |
| Intensityb | 12 | — | 38.7 |
| Disclosed | 1 | — | |
| Monitored, not disclosed | 11 | — | |
| Time (min/session) | 29 | 54.0 ± 10.6 (30.0–65.0) | 93.5 |
| Length of intervention (weeks) | 31 | 22.3 ± 20.2 (6.0–104.0) | 100.0 |
| Instructional methods items | |||
| Styleb | 16 | — | 51.6 |
| Yang style | 15 | — | |
| Chen style | 1 | — | |
| Number of forms | 24 | 30.4 ± 25.4 (6.0–108.0) | 77.4 |
| Form names | 8 | — | 25.8 |
| Movement principles emphasized | 4 | — | 12.9 |
| Breathing techniques emphasized | 6 | — | 19.4 |
| Relaxation emphasized | 3 | — | 9.7 |
| Progressionb | 10 | — | 32.3 |
| Designated leaning phase | 8 | — | |
| Gradually increased duration | 2 | — | |
| Number of instructorsb | 14 | 1.4 ± 0.9 (1.0–4.0) | 45.2 |
| Single instructor | 10 | — | |
| Multiple instructors | 4 | — | |
| Credentials of instructorsb | 15 | — | 48.4 |
| Experienced | 4 | — | |
| Master or expert | 3 | — | |
| Professional | 5 | — | |
| Trained, qualified, or certified | 6 | — | |
| Unsupervised practice, encouraged, but did not disclose actual time spentb | 5 | — | 16.1 |
Notes: Summary statistics are based on 31 Tai Ji Quan trials (k) and are presented as mean ± SD, unless otherwise stated; Range represents the minimum, maximum values reported for the particular item. — indicates that an item is not applicable.
Reporting rate is expressed as a percentage of trials that reported the specific item out of the total number of trials (k = 31).
For these Tai Ji Quan intervention characteristics, the subcategories are listed with the frequency they appeared among those trials that reported the item. Authors used 1 or multiple keyword(s) to describe the credentials of the instructors.
Abbreviation: Ex Rx = exercise prescription.
Among included Tai Ji Quan trials, only 1 trial (3.2%) disclosed the average heart rate (HR) during Tai Ji Quan practice (i.e., 63.7% of the age-predicted maximum HR.59 Meanwhile, 10 trials (32.3%) monitored and instructed participants to exercise at various HR ranges that ranged from 40% to 85% of the age-predicted maximum HR, or between 110 beats/min and 130 beats/min, but they did not disclose the actual HR values. Only 1 trial stated that HR was recorded during Tai Ji Quan exercise but provided no further information.60 All trials (k = 31, 100.0%) included supervised Tai Ji Quan exercise; yet, only about one-half of the trials disclosed the number (k = 14, 45.2%) or the credentials (k = 18, 58.1%) of the instructors (Table 1). In addition, 5 trials (k = 5, 16.1%) recommended unsupervised home practice without disclosing the actual time spent practicing. Last, in our sample, 2 trials (6.5%) specified that there were no adverse events; 1 trial (3.2%) indicated that no subjects withdrew from the study due to injuries from Tai Ji Quan practice. The rest of the trials (k = 28, 90.3%) did not provide any information regarding adverse events (Supplementary Table 4).
3.4. Resting BP assessment
Most trials (k = 21, 67.7%) reported the BP measurement instrument used. These included automated/digital units (k = 10, 32.3%) or manual sphygmomanometers (k = 11, 35.5%). About one-third of the trials (k = 10, 32.3%) reported the body position during the BP measurements, which included the seated (k = 9, 29.0%) or supine (k = 1, 3.2%) position. Yet, 11 trials (35.5%) did not report any details of the resting BP measurement procedures. In addition, none of the Tai Ji Quan trials specified the time between the post-intervention BP measurements and the last Tai Ji Quan session.
3.5. Tai Ji Quan as stand-alone antihypertensive therapy and potential mechanisms
Overall, Tai Ji Quan elicited moderate to large reductions in SBP (–11.3 mmHg, 95%CI: –14.6 to –8.0; d+ = –0.75) and DBP (–4.8 mmHg, 95%CI: –6.4 to –3.1; d+ = –0.53) compared to controls (p < 0.001) (Supplementary Fig. 1, Funnel plots of the SBP and DBP response to Tai Ji Quan vs. control; Supplementary Fig. 2, Forest plots of the SBP and DBP response to Tai Ji Quan vs. control). Of note, the standardized effect sizes for SBP (I2 = 88.3%, 95%CI: 84.6%–91.2%) and DBP (I2 = 83.9%, 95%CI: 78.1%–88.2%) lacked homogeneity. In addition, the mean effect sizes of RCTs and NRCTs were similar for SBP (–0.72 vs. –0.78, p = 0.83) and DBP (–0.45 vs. –0.60, p = 0.41), which supported our decision to combine RCTs with NRTCs in our final analyses.
In relation to the mechanisms of the BP-lowering effects of Tai Ji Quan (Supplementary Table 4), 15 trials (48.4%) discussed potential mechanisms of the BP-lowering effects of Tai Ji Quan. However, only 5 trials (16.1%) measured one or more of the mechanisms discussed or proposed. In addition, only 1 trial (3.2%) examined the relationship between the change of BP in response to Tai Ji Quan and the measured mechanism. Specifically, Pan and colleagues61 found that the change of plasma NO, CO, and H2S levels were negatively correlated with the change of SBP and mean arterial pressure.
3.6. Publication bias
The funnel plot (Supplementary Fig. 1), test of Begg, and test of Egger all suggested that there was significant publication or other reporting bias for the SBP response to Tai Ji Quan (test of Begg: z = –2.97, p = 0.003; test of Egger: t = –3.91, p = 0.001).45, 46, 47 Meanwhile, both the funnel plot and the test of Egger suggested that there was significant publication or other reporting bias for the DBP response to Tai Ji Quan (t = –2.37, p = 0.03), but the test of Begg did not (z = –1.41, p = 0.16).45, 46, 47 Following the Precision-Effect Test and Precision-Effect Estimate with SE48 analysis, potential publication bias was apparent (p = 0.02) only for the SBP response to Tai Ji Quan; thus, publication basis was controlled for in the multiple-moderator model for SBP.
3.7. Multiple-moderator models
When controlling for publication bias, SBP reductions were greater among Tai Ji Quan trials published in Chinese (16.7 mmHg, 95%CI: 12.5–20.9) than those published in English (8.4 mmHg, 95%CI: 4.8–11.9; p = 0.005) (Table 2). In addition, SBP was reduced more in samples with the highest baseline SBP (p = 0.04): 14.4 mmHg (95%CI: 11.3–17.7) for samples with hypertension, 11.3 mmHg (95%CI: 8.3–14.1) for samples with prehypertension, and 8.3 mmHg (95%CI: 3.3–13.2) for samples with normal BP. Collectively, these moderators accounted for 45.3% of the variance in the SBP response to Tai Ji Quan. The additive regression model revealed that, when controlling for publication bias among samples with hypertension, Tai Ji Quan trials published in Chinese elicited SBP reductions of 18.6 mmHg (95%CI: 14.1–23.1), nearly twice the magnitude of the SBP reductions of 10.4 mmHg (95%CI: 6.2–14.4) for Tai Ji Quan trials published in English (Table 2).
Table 2.
Moderator and additive models: SBP response to Tai Ji Quan (k = 31)a.
| Moderator dimension/level | (95%CI) | β | p | ∆ SBP (mmHg, 95%CI) |
|---|---|---|---|---|
| Publishing language | ||||
| Published in Chinese (k = 13) | –1.11 (–1.39 to –0.83) | –0.391 | 0.005 | –16.7 (–20.9 to –12.5) |
| Published in English (k = 18) | –0.56 (–0.79 to –0.32) | –8.4 (–11.9 to –4.8) | ||
| Baseline SBP of sample (mmHg) | –0.258 | 0.045 | ||
| Normal: 113 ± 5 (k = 5) | –0.55 (–0.88 to –0.22) | –8.3 (–13.2 to –3.3) | ||
| Prehypertension: 130 ± 6 (k = 10) | –0.75 (–0.94 to –0.55) | –11.3 (–14.1 to –8.3) | ||
| Hypertension: 148 ± 9 (k = 16) | –0.96 (–1.18 to –0.75) | –14.4 (–17.7 to –11.3) | ||
| Publication bias (SE of the SBP response to Tai Ji Quan) | –0.329 | 0.017 | ||
| Additive regression model: (1) among samples with hypertension and (2) controlling for publication bias | ||||
| Published in Chinese | –1.24 (–1.54 to –0.94) | –18.6 (–23.1 to –14.1) | ||
| Published in English | –0.69 (–0.96 to –0.41) | –10.4 (–14.4 to –6.2) |
Note: Baseline SBP is presented as mean ± SD.
Abbreviations: ∆ = change; β = standardized coefficient represents unique variance explained by moderator; CI = confidence interval; = standardized estimate; SBP = systolic blood pressure; SE = standard error.
Multiple R2 (variance explained by model, adjusted for number of moderators) = 45.3%.
DBP reductions were greater among Tai Ji Quan trials published in Chinese (–7.7 mmHg, 95%CI: –9.4 to –6.0) than those published in English (–2.9 mmHg, 95%CI: –4.1 to –1.6; p <0.001) (Table 3). In addition, DBP was reduced more in samples with the highest baseline DBP (p < 0.001): 6.4 mmHg (95%CI: 5.3–7.5) for samples with hypertension, 4.8 mmHg (95%CI: 3.7–5.8) for samples with prehypertension, and 2.8 mmHg (95%CI: 1.2–4.4) for samples with normal BP. Collectively, these moderators accounted for 65.9% of the variance in the DBP response to Tai Ji Quan. The additive regression model revealed that, among samples with hypertension, Tai Ji Quan interventions published in Chinese elicited DBP reduction of 8.8 mmHg (95%CI: 7.2–10.4), more than twice the magnitude of the DBP reductions of 4.0 mmHg (95%CI: 2.5–5.5) for Tai Ji Quan trials published in English (Table 3).
Table 3.
Moderator and additive models: DBP response to Tai Ji Quan (k = 31)a.
| Moderator dimension/level | (95%CI) | β | p | ∆ DBP (mmHg, 95%CI) |
|---|---|---|---|---|
| Publishing language | ||||
| Published in Chinese (k = 13) | –0.85 (–1.04 to –0.67) | –0.495 | <0.001 | –7.7 (–9.4 to –6.0) |
| Published in English (k =18) | –0.32 (–0.46 to –0.18) | –2.9 (–4.1 to –1.6) | ||
| Baseline DBP of sample (mmHg) | –0.464 | <0.001 | ||
| Normal: 73 ± 4 (k = 5) | –0.31 (–0.49 to –0.13) | –2.8 (–4.4 to –1.2) | ||
| Prehypertension: 81 ± 4 (k = 10) | –0.53 (–0.64 to –0.41) | –4.8 (–5.8 to –3.7) | ||
| Hypertension: 88 ± 8 (k = 16) | –0.71 (–0.83 to –0.59) | –6.4 (–7.5 to –5.3) | ||
| Additive Model: (1) among samples with hypertension | ||||
| Published in Chinese | –0.98 (–1.15 to –0.80) | –8.8 (–10.4 to –7.2) | ||
| Published in English | –0.44 (–0.61 to –0.28) | –4.0 (–5.5 to –2.5) |
Note: Baseline DBP is presented as mean ± SD.
Abbreviations: ∆ = change; β = standardized coefficient represents unique variance explained by moderator; CI = confidence interval; = standardized estimate; DBP = diastolic blood pressure.
Multiple R2 (variance explained by model, adjusted for number of moderators) = 65.9%.
4. Discussion
Our meta-analysis examined the efficacy of Tai Ji Quan as antihypertensive lifestyle therapy with the largest sample size examined to date. We found that Tai Ji Quan practiced ∼4 sessions/week for ∼60 min/session for ∼22 weeks, on average, produced BP reductions of 5–11 mmHg. Our novel finding, after controlling for publication bias among samples with hypertension, was that Tai Ji Quan trials published in English elicited SBP reductions of 10 mmHg and DBP reductions of 4 mmHg; for those published in Chinese, Tai Ji Quan trials elicited SBP reductions of 19 mmHg and DBP reductions of 10 mmHg. Even the more conservative magnitude of BP reductions reported in the literature published in English would reduce the risk of heart disease by ∼22% and stroke by ∼41%62 and may lower the BP of adults with hypertension into normal ranges.63,64 These large and clinically meaningful BP reductions support the use of Tai Ji Quan as an alternative to aerobic exercise as antihypertensive lifestyle therapy based on the literature, whether published in English or Chinese.
Aerobic exercise is the primary exercise modality that professional organizations throughout the world recommend to prevent and treat hypertension.64 However, less than one-third (28%) of adults with high BP adhere to the current aerobic exercise recommendations for hypertension.3 Therefore, in order to improve exercise adherence, other exercise options with comparable BP benefits, such as Tai Ji Quan, hold promise as viable alternatives to aerobic exercise, especially when people are unwilling or unable to engage in aerobic exercise to lower their high BP. Indeed, adults with hypertension may show better adherence to Tai Ji Quan than aerobic exercise because it is a safe, low-impact, enjoyable, and inexpensive form of exercise that requires minimal equipment and space.4, 5, 6, 7,65 Tai Ji Quan also provides various other physiological (e.g., managing arthritis symptoms, especially pain) and psychological health benefits (e.g., alleviating fear of falling, reducing stress), some of which (e.g., improving balance) are distinct from more traditional forms of exercise.8,66
Our meta-analysis also identified several moderators of the BP response to Tai Ji Quan that warrant further comment. Our most novel finding was that when controlling for other moderators, the magnitude of BP reductions was significantly larger among trials published in Chinese than trials published in English for both SBP (∼17 mmHg vs. ∼8 mmHg) and DBP (∼8 mmHg vs. ∼3 mmHg). This finding suggests that it is not appropriate to use 1 mean effect size calculation based on trials combined from the English and Chinese literature to represent the efficacy of Tai Ji Quan as antihypertensive lifestyle therapy,67,68 as all 3 previous meta-analyses did.14, 15, 16 As a result, in our additive regression models, we estimated the greatest potential BP reductions separately for Tai Ji Quan trials published in Chinese and English (Tables 2 and 3). In addition, the larger BP reduction reported among Tai Ji Quan trials published in Chinese than trials published in English emphasizes that further investigation is needed to explain the large discrepancies in the magnitude of the antihypertensive effects of Tai Ji Quan between trials published in Chinese and English.
Accordingly, we compared differences in the samples, Tai Ji Quan interventions, and study characteristics (Table 4) between Tai Ji Quan trials published in Chinese and English. In relation to sample characteristics, the sole difference we found was that trials published in Chinese had samples with higher DBP at baseline (p = 0.03), which may have contributed to the greater DBP reductions reported.64 Overall, we did not identify any differences in Tai Ji Quan intervention characteristics that may have contributed to the greater BP reductions reported in trials published in Chinese rather than in English. In relation to the study characteristics, Tai Ji Quan trials published in Chinese differed from trials published in English in that they (1) tended to have smaller sample sizes (p = 0.052), (2) had lower methodological study quality evaluated by using the Downs and Black Checklist (p < 0.001),28 and (3) had greater publication bias in relation to SBP indicated by the SE of the SBP response to Tai Ji Quan (p = 0.048). They also tended to have greater publication bias in relation to DBP, as indicated by the SE of the DBP response to Tai Ji Quan (p = 0.06). These findings indicate that Chinese-language journals are more likely to publish Tai Ji Quan trials showing significant BP reductions, but the trials have noticeable limitations in their study methodology is compared to those published by English-language journals. These limitations likely contributed to the overall greater BP reductions reported in Tai Ji Quan trials published in Chinese.68,69 We also acknowledge there could be other factors that contributed to the greater BP reductions reported in Tai Ji Quan trials published in Chinese, such as the participants’ expectations and the Tai Ji Quan instructors’ teaching skills.70 However, none of these factors were adequately reported to allow for quantitative comparisons.
Table 4.
Comparisons of the sample, Tai Ji Quan intervention, and study characteristics between Tai Ji Quan trials published in Chinese and English.
| Published in Chinese (k = 13) |
Published in English (k = 18) |
|||
|---|---|---|---|---|
| k | Mean ± SDa | k | Mean ± SDa | |
| Sample characteristics | ||||
| Age (year) | 8 | 51.9 ± 14.9 | 15 | 59.2 ± 16.3 |
| Female (%) | 10 | 78.3 ± 23.9 | 16 | 64.0 ± 18.7 |
| BMI (kg/m2) | 6 | 24.4 ± 1.6 | 12 | 24.6 ± 1.7 |
| Baseline SBP (mmHg) | 13 | 139.1 ± 16.0 | 18 | 135.3 ± 14.8 |
| Baseline DBP (mmHg) | 13 | 87.4 ± 10.3 | 18 | 80.5 ± 6.0⁎ |
| No Tai Ji Quan practice in the past 6 months (%) | 1 | 7.7 | 6 | 33.3 |
| Tai Ji Quan intervention characteristics | ||||
| Time (min/session) | 12 | 47.9 ± 13.7 | 17 | 58.4 ± 4.5⁎ |
| Weekly time (min) | 12 | 210.0 ± 77.4 | 18 | 215.3 ± 90.1 |
| Total time of intervention (min) | 12 | 4016.7 ± 2760.1 | 18 | 4481.5 ± 3135.3 |
| Frequency (sessions/week) | 13 | 4.6 ± 1.2 | 17 | 3.6 ± 1.5 |
| Intervention length (week) | 13 | 21.8 ± 25.2 | 18 | 22.6 ± 16.6 |
| Reported intensity of Tai Ji Quan practice (%) | 0 | 0 | 1 | 5.5 |
| Did emphasize movement principles (%) | 1 | 7.7 | 3 | 16.7 |
| Did emphasize breathing (%) | 4 | 30.8 | 2 | 11.1 |
| Did emphasize relaxation (%) | 1 | 7.7 | 2 | 11.1 |
| Study characteristics | ||||
| Sample size | 13 | 73.8 ± 35.1 | 18 | 125.8 ± 87.1 |
| Publication year | 13 | 2011.1 ± 3.8 | 18 | 2011.4 ± 5.7 |
| Methodological study quality (%) | 13 | 37.0 ± 10.8 | 18 | 60.0 ± 12.6⁎ |
| Adopted RCT design (%) | 4 | 30.8 | 11 | 61.1 |
| BP was primary outcome (%) | 12 | 92.3 | 12 | 66.7 |
| SE of the SBP response to Tai Ji Quan | 13 | 0.28 ± 0.08 | 18 | 0.22 ± 0.08⁎ |
| SE of the DBP response to Tai Ji Quan | 13 | 0.27 ± 0.08 | 18 | 0.22 ± 0.08 |
Abbreviations: BP = blood pressure; BMI = body mass index; DBP = diastolic blood pressure; RCT = randomized controlled trials; SBP = systolic blood pressure; SE = standard error.
For categorical variables, Means and SDs were not applicable; instead, percentages of the number of observations in the identified categories in relation to the total sample (i.e., 13 and 18 for trials published in Chinese and English, respectively) were reported.
p < 0.05, based on analysis of variance test for continuous variables and Pearson's χ2 test for categorical variables.
The 2nd moderator we identified was baseline BP status. When controlling for other moderators, BP reductions were the largest among interventions that involved samples with hypertension (SBP ∼14 mmHg/DBP ∼6 mmHg), prehypertension (SBP ∼11 mmHg/DBP ∼5 mmHg), and normal BP (SBP ∼8 mmHg/DBP ∼3 mmHg).51 This finding is consistent with the law of initial values,26 which states that the magnitude of the response is directly related to the initial level of the health outcome being measured.64
It should be noted that overall the included Tai Ji Quan trials were of moderate methodological study quality (i.e., 50.1% of items on the Downs and Black Checklist were satisfied28). Following the Grading of Recommendations, Assessment, Development, and Evaluation Approach,71,72 we recommend that readers place moderate certainty in our findings because the included Tai Ji Quan trials exhibited (1) a high/serious risk of bias evaluated by RoB 2.0 and ROBINS-I (Supplementary Tables 5 and 6), (2) high levels of heterogeneity (i.e., I2 ranged from 83.9% to 88.3%, although some heterogeneity was explained with moderators), and (3) some evidence of publication bias, especially in relation to SBP. In addition, we recommend that readers place more certainty in Tai Ji Quan trials published in English than in Chinese for the reasons discussed previously (Table 4).
Although our multiple-moderator models explained a clinically meaningful portion of the variance of the SBP (45.3%) and DBP (65.9%) responses to Tai Ji Quan, it was surprising that these models left a large amount of variance in effects unexplained. We evaluated 20 other potential sources of influence and found that these factors were unrelated to the BP responses to Tai Ji Quan among included trials (Supplementary Table 8, variables tested but not significant as the moderator of the BP response to Tai Ji Quan). Notably, it remains possible that some authors of the included Tai Ji Quan trials inadvertently omitted details of their studies due to space limitations or other unknown reasons, which limited our ability to extract such information and perform analyses. As a result, we acknowledge that additional unidentified moderators may exist in this literature (Supplementary Table 4), such as the intensity of Tai Ji Quan practice (3.2% reported), the emphasis on relaxation (9.7% reported) and breathing techniques (22.7% reported) during Tai Ji Quan practice, the credentials of instructors (48.4% reported various credentials) and whether they corrected the techniques of Tai Ji Quan practice (22.6% reported), the experience of Tai Ji Quan practice among subjects (25.8% reported), adherence to prescribed Tai Ji Quan practice (16.1% reported), medication use at baseline (25.8% reported) and during the intervention (12.9% reported), and maintenance of diet (9.7% reported) and physical activity levels other than Tai Ji Quan practice (9.7% reported) during the intervention. In addition, no intervention (0%) disclosed the time between the last session of Tai Ji Quan and the post-intervention BP measurement. Therefore, it was unclear whether the BP response was confounded by the post-exercise hypotension21,26 or by detraining.27 Finally, another limitation of our meta-analysis was that we did not search for the grey literature or Tai Ji Quan trials published in languages other than Chinese and English.
Our meta-analysis also had several strengths. First, we performed meta-regression analysis, allowing us to examine multiple moderators of the BP responses to Tai Ji Quan simultaneously.18, 19, 20 Second, the use of contemporary statistical strategies, in particular the moving constant technique,44 allowed us to estimate the magnitude of BP reduction at different clinically significant levels of the individual moderators (Tables 2 and 3). Third, although all previous meta-analyses that examined the BP benefits of Tai Ji Quan included trials published in both Chinese and English, ours was the first to examine publishing language as a moderator of the BP response to Tai Ji Quan. Importantly, our results suggest that more confidence should be placed in the Tai Ji Quan trials published in English due to the more noticeable limitations in study methodologies and greater publication bias in the Tai Ji Quan trials published in Chinese.
5. Conclusion
Our new and noteworthy findings are that Tai Ji Quan interventions published in English elicited SBP reductions of 10.4 mmHg and DBP reductions of 4.0 mmHg, while trials published in Chinese elicited SBP reductions of 18.6 mmHg and DBP reductions of 8.8 mmHg among samples with hypertension. Tai Ji Quan may be another viable exercise option to treat hypertension because even the more conservative magnitude of BP reductions among individuals with hypertension reported in the English literature would reduce the risk of cardiovascular disease by up to 40%.62 The current review also calls attention to the fact that future Tai Ji Quan intervention studies need to (1) improve the reporting of potential moderators of the BP response to Tai Ji Quan and (2) investigate the notable discrepancies we found between trials published in Chinese and English literature.
Acknowledgments
Acknowledgment
This study was supported, in part, by the National Institutes of Health (NIH) Science of Behavior Change Common Fund Program through an award administered by the National Institute on Ageing (5U24AG052175) and the University of Connecticut Center for Excellence in Teaching and Learning (KFS 4612560).
Authors’ contributions
YW participated in the design of the study and contributed to data collection, analysis, and interpretation; BTJ contributed to data analysis and interpretation; SC, YC, and JL contributed to data collection; LSP participated in the design of the study and contributed to data interpretation; all authors contributed to manuscript writing. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jshs.2020.03.007.
Appendix. Supplementary materials
References
- 1.Whelton P.K., Carey R.M., Aronow W.S. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–e148. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Lewington S., Clarke R., Qizilbash N., Peto R., Collins R. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. The Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services . Healthy People; 2020. Topics & objectives - physical activity.www.healthypeople.gov/2020/topics-objectives/topic/physical-activity Available at: [accessed 20.08.2019] [Google Scholar]
- 4.Guo Y., Qiu P., Liu T. Tai J Quan: an overview of its history, health benefits, and cultural value. J Sport Health Sci. 2014;3:3–8. [Google Scholar]
- 5.Wayne P.M., Berkowitz D.L., Litrownik D.E., Buring J.E., Yeh G.Y. What do we really know about the safety of Tai Chi? A systematic review of adverse event reports in randomized trials. Arch Phys Med Rehabil. 2014;95:2470–2483. doi: 10.1016/j.apmr.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen K.M., Snyder M., Krichbaum K. Facilitators and barriers to elders' practice of t'ai chi. A mind-body, low-intensity exercise. J Holist Nurs. 2001;19:238–255. doi: 10.1177/089801010101900305. [DOI] [PubMed] [Google Scholar]
- 7.Wayne P.M., Kaptchuk T.J. Challenges inherent to t'ai chi research: part I–t'ai chi as a complex multicomponent intervention. J Altern Complement Med. 2008;14:95–102. doi: 10.1089/acm.2007.7170a. [DOI] [PubMed] [Google Scholar]
- 8.Solloway M.R., Taylor S.L., Shekelle P.G. An evidence map of the effect of tai chi on health outcomes. Syst Rev. 2016;5:126. doi: 10.1186/s13643-016-0300-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang K.H. The influence of Tai Ji Quan on the physical function of middle-aged and older women. J Yichun Univ. 2009;31:168–190. [in Chinese] [Google Scholar]
- 10.Zhao X.M., Wu G.S., Li G.L. The influence of simplified Tai Chi exercise on the physical function of middle-aged women. Chinese J Rehabil Theory Pract. 2006;12:167–168. [in Chinese] [Google Scholar]
- 11.Lee Y.M. The effects of tai chi on waist circumference and blood pressure in the elderly. J Phys Ther Sci. 2017;29:172–175. doi: 10.1589/jpts.29.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brook R.D., Appel L.J., Rubenfire M. Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the American Heart Association. Hypertension. 2013;61:1360–1383. doi: 10.1161/HYP.0b013e318293645f. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Department of Health and Human Services. 2018 Physical Activity Guidelines Advisory Committee. 2018 physical activity guidelines advisory committee scientific report. Available at: www.hhs.gov/fitness/be-active/physical-activity-guidelines-for-americans/index.html#:∼:text=For% 20substantial%20health%20benefits%2C%20adults,and%20vigorous%2 Dintensity%20aerobic%20activity. [accessed 20.08.2019].
- 14.Wang J., Feng B., Yang X. Tai chi for essential hypertension. Evid Based Complement Alternat Med. 2013;2013 doi: 10.1155/2013/215254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zheng G., Huang M., Liu F., Li S., Tao J., Chen L. Tai chi chuan for the primary prevention of stroke in middle-aged and elderly adults: a systematic review. Evid-Based Complement Alternat Med. 2015;2015 doi: 10.1155/2015/742152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zheng G., Li S., Huang M., Liu F., Tao J., Chen L. The effect of tai chi training on cardiorespiratory fitness in healthy adults: a systematic review and meta-analysis. PLoS One. 2015;10 doi: 10.1371/journal.pone.0117360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shea B.J., Reeves B.C., Wells G. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacCallum R.C., Zhang S., Preacher K.J., Rucker D.D. On the practice of dichotomization of quantitative variables. Psychol Methods. 2002;7:19–40. doi: 10.1037/1082-989x.7.1.19. [DOI] [PubMed] [Google Scholar]
- 19.Steel P.D., Kammeyer-Mueller J.D. Comparing meta-analytic moderator estimation techniques under realistic conditions. J Appl Psychol. 2002;87:96–111. doi: 10.1037/0021-9010.87.1.96. [DOI] [PubMed] [Google Scholar]
- 20.Viswesvaran C., Sanchez J.I. Moderator search in meta-analysis: a review and cautionary note on existing approaches. Educ Psychol Meas. 1998;58:77–87. [Google Scholar]
- 21.Pescatello L.S., Corso L.M.L., MacDonald H.V. Small sample sizes confound understanding of cardiometabolic responses to exercise. Exerc Sport Sci Rev. 2017;45:173–180. doi: 10.1249/JES.0000000000000115. [DOI] [PubMed] [Google Scholar]
- 22.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 23.Corso L.M., Macdonald H.V., Johnson B.T. Is concurrent training efficacious antihypertensive therapy? A meta-analysis. Med Sci Sports Exerc. 2016;48:2398–2406. doi: 10.1249/MSS.0000000000001056. [DOI] [PubMed] [Google Scholar]
- 24.MacDonald H.V., Johnson B.T., Huedo-Medina T.B. Dynamic resistance training as stand-alone antihypertensive lifestyle therapy: a meta-analysis. J Am Heart Assoc. 2016;5 doi: 10.1161/JAHA.116.003231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu Y., MacDonald H.V., Pescatello L.S. Evaluating exercise prescription and instructional methods used in tai chi studies aimed at improving balance in older adults: a systematic review. J Am Geriatr Soc. 2016;64:2074–2080. doi: 10.1111/jgs.14242. [DOI] [PubMed] [Google Scholar]
- 26.Pescatello L.S., Kulikowich J.M. The aftereffects of dynamic exercise on ambulatory blood pressure. Med Sci Sports Exerc. 2001;33:1855–1861. doi: 10.1097/00005768-200111000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Moker E.A., Bateman L.A., Kraus W.E., Pescatello L.S. The relationship between the blood pressure responses to exercise following training and detraining periods. PLoS One. 2014;9 doi: 10.1371/journal.pone.0105755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Downs S.H., Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chudyk A.M., Jutai J.W., Petrella R.J., Speechley M. Systematic review of hip fracture rehabilitation practices in the elderly. Arch Phys Med Rehabil. 2009;90:246–262. doi: 10.1016/j.apmr.2008.06.036. [DOI] [PubMed] [Google Scholar]
- 30.Samoocha D., Bruinvels D.J., Elbers N.A., Anema J.R., van der Beek A.J. Effectiveness of web-based interventions on patient empowerment: a systematic review and meta-analysis. J Med Internet Res. 2010;12:e23. doi: 10.2196/jmir.1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sterne J.A.C., Savović J., Page M.J. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 32.Sterne J.A., Hernan M.A., Reeves B.C. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Becker B.J. Synthesizing standardized mean‐change measures. Br J Math Stat Psychol. 1988;41:257–278. [Google Scholar]
- 34.Hedges L.V., Olkin I. Academic Press, Inc.; Orlando, FL: 1985. Statistical methods for meta-analysis. [Google Scholar]
- 35.Wolf S.L., O'Grady M., Easley K.A., Guo Y., Kressig R.W., Kutner M. The influence of intense tai chi training on physical performance and hemodynamic outcomes in transitionally frail, older adults. J Gerontol A Biol Sci Med Sci. 2006;61:184–189. doi: 10.1093/gerona/61.2.184. [DOI] [PubMed] [Google Scholar]
- 36.Song B.Y. Effect of Tai Ji Quan exercise on middle-aged and older women with hypertension. National Traditional Sports. 2018;8:159–160. [in Chinese] [Google Scholar]
- 37.Pan X., Zhang Y., Tao S. Effects of tai chi exercise on blood pressure and plasma levels of nitric oxide, carbon monoxide and hydrogen sulfide in real-world patients with essential hypertension. Clin Exp Hypertens. 2015;37:8–14. doi: 10.3109/10641963.2014.881838. [DOI] [PubMed] [Google Scholar]
- 38.Johnson BT, Huedo-Medina TB. Meta-analytic statistical inferences for continuous measure outcomes as a function of effect size metric and other assumptions. Available at: www.ncbi.nlm.nih.gov/books/NBK140575/. [accessed 20.08.2019]. [PubMed]
- 39.Cohen J Statistical power analysis for the behavioral sciences. 2nd, ed. Hillsdale, NJ: Lawrence Erlbaum Associations; 1988 [Google Scholar]
- 40.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Huedo-Medina T.B., Sánchez-Meca J., Marín-Martínez F., Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I² index? Psychol Methods. 2006;11:193–206. doi: 10.1037/1082-989X.11.2.193. [DOI] [PubMed] [Google Scholar]
- 42.Lipsey M.W., Wilson D. Sage; Thousand Oaks, CA: 2000. Practical meta-analysis (applied social research methods) [Google Scholar]
- 43.Viechtbauer W. Accounting for heterogeneity via random-effects models and moderator analyses in meta-analysis. Z Psychol. 2007;215:104–121. [Google Scholar]
- 44.Johnson B.T., Huedo-Medina T.B. Depicting estimates using the intercept in meta‐regression models: the moving constant technique. Res Synth Methods. 2011;2:204–220. doi: 10.1002/jrsm.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Higgins J.P.T., Thomas J., Chandler J., editors. Cochrane handbook for systematic reviews of interventions. 2nd ed. John Wiley & Sons; Chichester: 2019. [Google Scholar]
- 46.Begg C.B., Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 47.Egger M., Davey Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stanley T.D., Doucouliagos H. Meta-regression approximations to reduce publication selection bias. Res Syn Methods. 2014;5:60–78. doi: 10.1002/jrsm.1095. [DOI] [PubMed] [Google Scholar]
- 49.Johnson B.T., Low R.E., MacDonald H.V. Panning for the gold in health research: incorporating studies’ methodological quality in meta-analysis. Psychol Health. 2015;30:135–152. doi: 10.1080/08870446.2014.953533. [DOI] [PubMed] [Google Scholar]
- 50.Harbord R.M., Higgins J. Meta-regression in Stata. Stata J. 2008;8:493–519. [Google Scholar]
- 51.Chobanian A.V., Bakris G.L., Black H.R. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 52.Chang M., Yeh S.J., Chu M., Wu T., Huang T. Associations between tai chi chung program, anxiety, and cardiovascular risk factors. Am J Health Promot. 2013;28:16–22. doi: 10.4278/ajhp.120720-QUAN-356. [DOI] [PubMed] [Google Scholar]
- 53.Qi D.L., Li Y.M., Yan X.H. Influence of eight form Tai Chi Quan on individuals with hypertension. Sichuan Sports Med. 2015;5:24–39. [in Chinese] [Google Scholar]
- 54.Tsai J.C., Wang W.H., Chan P. The beneficial effects of tai chi chuan on blood pressure and lipid profile and anxiety status in a randomized controlled trial. J Altern Complement Med. 2003;9:747–754. doi: 10.1089/107555303322524599. [DOI] [PubMed] [Google Scholar]
- 55.Shi Z.B., Miao Z.L. Traditional Chinese exercise medicine on stage1 hypertension. Chinese Manip Rehabil Med. 2017;8:51–52. [in Chinese] [Google Scholar]
- 56.Thomas G.N., Hong A.W.L., Tomlinson B. Effects of tai chi and resistance training on cardiovascular risk factors in elderly Chinese subjects: a 12-month longitudinal, randomized, controlled intervention study. Clin Endocrinol (Oxf) 2005;63:663–669. doi: 10.1111/j.1365-2265.2005.02398.x. [DOI] [PubMed] [Google Scholar]
- 57.Ma C., Zhou W., Tang Q., Huang S. The impact of group-based tai chi on health-status outcomes among community-dwelling older adults with hypertension. Heart Lung. 2018;47:337–344. doi: 10.1016/j.hrtlng.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 58.Lan C., Su T.C., Chen S.Y., Lai J.S. Effect of T'ai chi chuan training on cardiovascular risk factors in dyslipidemic patients. J Altern Complement Med. 2008;14:813–819. doi: 10.1089/acm.2008.0143. [DOI] [PubMed] [Google Scholar]
- 59.Tsai J., Wang W., Chan P. The beneficial effects of tai chi chuan on blood pressure and lipid profile and anxiety status in a randomized controlled trial. J Altern Complement Med. 2003;9:747–754. doi: 10.1089/107555303322524599. [DOI] [PubMed] [Google Scholar]
- 60.Duan L.M. Effect of Yang style Taiji push hands and routine on cardiovascular function of middle-aged and older women. J Phys Educ Inst Shanxi Normal Univ. 2008;23:87–90. [in Chinese] [Google Scholar]
- 61.Pan X., Zhang Y., Tao S. Effects of tai chi exercise on blood pressure and plasma levels of nitric oxide, carbon monoxide and hydrogen sulfide in real-world patients with essential hypertension. Clin Exp Hypertens. 2015;37:8–14. doi: 10.3109/10641963.2014.881838. [DOI] [PubMed] [Google Scholar]
- 62.Law M.R., Morris J.K., Wald N.J. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pescatello L.S., Franklin B.A., Fagard R. American college of sports medicine position stand. exercise and hypertension. Med Sci Sports Exerc. 2004;36:533–553. doi: 10.1249/01.mss.0000115224.88514.3a. [DOI] [PubMed] [Google Scholar]
- 64.Pescatello L.S., MacDonald H.V., Ash G.I. Assessing the existing professional exercise recommendations for hypertension: a review and recommendations for future research priorities. Mayo Clin Proc. 2015;90:801–812. doi: 10.1016/j.mayocp.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 65.Wayne P.M., Kaptchuk T.J. Challenges inherent to t'ai chi research: part II-defining the intervention and optimal study design. J Altern Complement Med. 2008;14:191–197. doi: 10.1089/acm.2007.7170b. [DOI] [PubMed] [Google Scholar]
- 66.Huston P., McFarlane B. Health benefits of tai chi: what is the evidence. Can Fam Physician. 2016;62:881–890. [PMC free article] [PubMed] [Google Scholar]
- 67.Bangdiwala S.I., Bhargava A., O'Connor D.P. Statistical methodologies to pool across multiple intervention studies. Transl Behav Med. 2016;6:228–235. doi: 10.1007/s13142-016-0386-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vickers A., Goyal N., Harland R., Rees R. Do certain countries produce only positive results? A systematic review of controlled trials. Control Clin Trials. 1998;19:159–166. doi: 10.1016/s0197-2456(97)00150-5. [DOI] [PubMed] [Google Scholar]
- 69.Schulz K.F., Chalmers I., Hayes R.J., Altman D.G. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273:408–412. doi: 10.1001/jama.273.5.408. [DOI] [PubMed] [Google Scholar]
- 70.Cramer H., Lauche R., Langhorst J., Dobos G. Are Indian yoga trials more likely to be positive than those from other countries? A systematic review of randomized controlled trials. Contemp Clin Trials. 2015;41:269–272. doi: 10.1016/j.cct.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 71.Hultcrantz M., Rind D., Akl E.A. The GRADE working group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017;87:4–13. doi: 10.1016/j.jclinepi.2017.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Murad M.H. Clinical practice guidelines: a primer on development and dissemination. Mayo Clin Proc. 2017;92:423–433. doi: 10.1016/j.mayocp.2017.01.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.